

|
Chapter 3:
The Cervical Spine
From R. C. Schafer, DC, PhD, FICC's best-selling book:
“Motion Palpation”
Second Edition ~ The Motion Palpation Institute & ACAPress
The following materials are provided as a service to our profession. There is no charge for individuals to copy and file these materials. However, they cannot be sold or used in any group or commercial venture without written permission from ACAPress.
All of Dr. Schafer's books are now available on CDs, with all proceeds being donated
to chiropractic research. Please review the complete list of available books.Applied Anatomy Considerations See the Pierce Analyis of films The Apophyseal Joints of the Spine Regional Structural Characteristics The Cervical Apophyseal Joints The Cervical Intervertebral Foramina The Contents of the Intervertebral Foramina The Cervical Nerves Pertinent Neurovascular Considerations Cerebrospinal Fluid Circulation: Pertinent Considerations Biomechanical Considerations Action and Brake Mechanisms in the Spine as a Whole The Upper Cervical Region The Lower Cervical Region Diagnostic Considerations Dynamic Palpation of the Cervical Region Assessing Segmental Mobility Objectively Differential Diagnosis Therapeutic Approach Adaptability to Partial Mobility Adjusting Occipitoatlantal Articular Fixations Adjusting Atlantoaxial Fixations Adjusting Middle and Lower Cervical Fixations Adjusting Muscular Fixations in the Cervical Spine BibliographyChapter 3: The Cervical Spine
This chapter describes the basic biomechanical, diagnostic, and therapeutic considerations related to motion palpation and the cervical spine. Emphasis will be on relating the general concepts previously explained about the chiropractic fixation-subluxation complex to specific entities that can be revealed by motion palpation and frequently corrected by dynamic chiropractic. Some aids to differential diagnosis are also included.
APPLIED ANATOMY CONSIDERATIONSThere are seven sites of possible "articular" fixation in the cervical spine. They are at the bilateral apophyseal joints, the bilateral covertebral joints, the superior and inferior intervertebral disc (IVD) interfaces, and the odontal-atlantal articulation (Table 3.1).
Table 3.1. The 27 Sites of Possible Spinopelvic Articular Fixation
In the cervical spine (7 possible sites of fixation) Bilateral apophyseal joints 2 Bilateral covertebral joints 2 Superior and inferior IVD interfaces 2 Odontal-atlantal articulation 1 In the thoracic spine (8 possible sites of fixation) Bilateral apophyseal joints 2 Superior and inferior IVD interfaces 2 Bilateral costovertebral joints 2 Bilateral costotransverse joints 2 In the lumbar spine (4 possible sites of fixation) Bilateral apophyseal joints 2 Superior and inferior IVD interfaces 2 In the pelvis (8 possible sites of fixation) Bilateral superior sacroiliac joints 2 Bilateral inferior sacroiliac joints 2 Sacrococcygeal joint 1 Pubic joint 1 Bilateral acetabulofemoral joints 2 The Apophyseal Joints of the Spine
Throughout the spine, paired diarthrodial articular processes (zygapophyses) project from the vertebral arches. The superior processes (prezygapophyses) of the inferior vertebra contain articulating facets that face somewhat posteriorly. They mate with the inferior processes (postzygapophyses) of the vertebra above that face somewhat anteriorly. Each articular facet is covered by a layer of hyaline cartilage that faces the synovial joint. The angulation of vertebral facets normally varies with the level of the spine and can be altered by wear and pathology.
In visualizing the motion of any joint, it is helpful to keep in mind that the hyaline-coated articulating surface is not the shape of the often flat bony surface exhibited on an x-ray film. Most apophyseal joints of the spine have a convex-concave shape.
Fisk states that the posterior joints of the spine are more prone to osteoarthritic changes than any other joint in the body: "Evidence of disc degeneration precedes this arthritis in the lumbar spine, but there is no such relationship in the cervical spine." However, most authorities agree with Grieve that the presence of arthrotic changes in the facet planes does not, of itself, necessarily have any effect on ranges of movement, neither does the presence of osteophytosis.
Inserted from the Pierce Technique Page (for clarification)
Neutral Lateral View:
This x-ray on the left is a section from a neutral lateral cervical film, displaying C3 through C5.
The vertebral body is on the right. Protruding directly off the back of the body is the pedicle, which is where the ring of bone that houses the spinal cord attaches.
Directly behind the pedicle is the trapezoidal-shaped articular pillar. You will note the flat facet (zygapophysis) on the top and the bottom of each pillar. In the cervical region, they face backwards at a 45° angle.
You will also note (see below) in the following flexion and extension views that the principal motions take place at the facets. The only motion that should occur at the vertebral discs is anterior compression during flexion, and posterior compression during extension. No translation (forward or backwards motion) of the vertebral bodies should occur during these motions as long as the disc and the longitudinal ligaments retain their integrity.
You may also refer to the The “Spinal Motion Unit” section of Spinal Anatomy 101 Page
for an in-depth review of these biomechanical phenomena.
Flexion Film Analysis:
NOTE: When pre-positioning the patient for this view, it's KEY to have them first lower their chin, before they flex their spine, otherwise you may not observe motion at occiput. The picture on the left demonstrated nutation at occiput.
When the spine flexes, it should fully reverse the cervical curve. Three primary motions should occur in flexion:(1) The zygapophyses (facets) should slide upwards and forwards. Because of this motion,
(2) the IVF's should open (more) fully. And lastly,
(3) the spinous processes should “fan out”, or separate. Occiput should also nutate forwards, and the C1 posterior arch should approximate the back of occiput.
A segment which has lost the ability to flex would be labelled a “flexion lock”. Please note that in flexion (as in the neutral view), George's posterior body line should still be one curved line, with all segments on that line. If you require more than one line to connect all the segments, the subluxated segment will reside in the portion of the spine which is straightened. In flexion lock, typically the segment just below the intersection of these 2 lines is the subluxated segment. The most obvious indicator would be that the segment fails to flex and thus, increase the size of it's IVF.
Extension Film Analysis:
NOTE: When pre-positioning the patient for this view, it's KEY to have them first raise their chin, before they extend their spine, otherwise you may not observe motion at occiput.
As with flexion, 3 thing should occur. The facets should slide backwards and down, the IVF's close down, and all the spinous processes should approximate. Unusual findings may include a segment which remains in flexion (or moves into flexion while the other segments extend). This abnormal motion is referred to as “paradoxic motion”, and is considered a sign of abnormal function of the cervical spine.
Again, all segments should remain on one curved line. A segment which fails to extend is locked in flexion. Two or more lines would be needed to connect all segments, and the subluxated vertebra will be located in the straight section of the spine.
The obvious segment to adjust would be the one BELOW the one which fails to extend. The Logic is: You can't adjust the upper one from the front, to drive it back and down, but you can adjust the lower one P-A, to drive it forwards and up. Remember, the subluxation occurs at the facets beneath the segment which fails to extend. So moving the segment directly below it (the sub-adjacent segment) will break up the fixation that exists between them, thus permitting the upper segment to extend, and for that segments IVF to close down.
In this particular extension film, observe that C7 FAILS to extend on T1. Note the IVF size, and the fact that the spinous process fails to approximate with T1. It's hard to see in this view, due to the overlapping of shoulder tissue, but the inferior facet of C7 fails to slide down on the superior facet of T1. A "spot view" with increased penetration could easily display this loss of function, BUT that is NOT necessary...the IVF and spinous process clearly tell the story...this is classic "paradoxic motion".
You may also want to review Schafer's Radiologic Manifestations of Spinal Subluxations
Regional Structural Characteristics
Nature has made many structural adaptations in the cervical region because of the relatively small weight-bearing structures, the required range of motion, and the enlarged spinal cord in this region as compared to other spinal regions. The laminae are slender and overlap, and this shingling design increases with age. The osseous elevations on the posterolateral aspect of most cervical vertebrae (that form the uncovertebral pseudojoints) tend to protect the spinal canal from lateral IVD herniation, but hypertrophy of these joints added to IVD degeneration can readily lead to intervertebral foramen (IVF) encroachment.
The IVDs are broader anteriorly than posteriorly to accommodate the cervical lordosis. It is helpful to know the location of the nucleus pulposus of a region because it indicates the normal site of maximum load, but authorities differ on the normal location of the nucleus in the cervical region. Kapandji locates it centrally. Cailliet places it slightly posterior (further anterior than a lumbar nucleus), and Jeffreys says it is distinctly posterior from the midline. Thus, such conflicting reports are no better than no data at all.
Because the atypical atlas has no centrum, there is no IVD between the occiput and atlas or the atlas and axis.
The Cervical Apophyseal Joints
The articular processes of the mid and lower cervical spine incline medially in the coronal plane and obliquely in the sagittal plane so that they are approximately at a 45°angle to the vertical. This is an important fact to remember when adjusting this region. The bilateral articular surface area of the segments, which shares a good part of head weight with the vertebral body, is about 67% of that of the vertebral body.
The short, thick, dense capsular ligaments bind the articulating processes together (Figure 3.1), enclosing the articular cartilage and synovium. Their fibers are firmly bound to the periosteum of the superior and inferior processes and arranged at a 90°angle to the plane of the facet. This allows maximum laxity when the facets are in a position of rest. They normally allow no more than a few millimeters of movement from the neutral position per segment, and possibly provide more cervical stability than any other ligament complex of this region.
Capsulitis from overstretch in acute traumatic subluxation complex or excessive compensatory hypermobility is common. Within the capsule, small tongues of meniscus-like tissue flaps project from the articular surfaces into the synovial space. They are infrequently nipped" in severe jarring at an unguarded moment during the end of extension, rotation, or lateral bending, establishing a site of apophyseal bursitis.
The posterior joint capsules and the perivertebral supporting ligaments enjoy an abundance of nociceptors and mechanoreceptors, far more than any other area of the spine. The IVDs are almost void of such receptors.
The Cervical Intervertebral Foramina
The foramina in the cervical region are shaped more like rounded gutters than orifices, averaging 1 cm in length. There is no true IVF between the atlas and the occiput or between the atlas and the axis. The C1 nerve exits over the superior aspect of the posterior arch of the atlas in the vertebral artery sulcus (Figure 3.2). The C2 nerve exits between the inferior aspect of the posterior arch of the atlas and the superior aspect of the pedicle of the axis. It then, in a vulnerable position, transverses the lateral atlantoaxial joint, anterior to the ligamentum flava for a short while, then exits (Figure 3.3). The C3–C8 nerves exit through short oval canals that increase in size as they progress caudally.
In contrast with the dorsal and lumbar regions, the boundaries of the cervical IVFs are designed more for motion than they are for stability. The greatest degree of functional IVF-diameter narrowing occurs ipsilaterally in lateral bending with simultaneous extension.
Thus, this position should be avoided whenever possible during cervical adjustments and manipulation.
The Contents of the Intervertebral Foramina
Cervical nerves, especially, fill the transverse diameter of the their IVFs. Thus, any disorder that reduces this dimension structurally or functionally (eg, subluxation, osteophytes, disc herniation, edema, vascular engorgement) will undoubtedly compromise the integrity of the IVF contents (Figure 3.4).
Each IVF of the cervical, thoracic, and lumbar spine is dynamic; widening and expanding with spinal motion, serving as a channel for nerve and vascular flow egress and ingress, and allowing for massage-like compression and expansion of the conduits and lipoareolar bed. From one-third to one-half of the foraminal opening is occupied by the spinal nerve root and its sheath, with the remaining portion filled essentially by fat, connective tissue, and various vessels. The following structures are found in the IVF:
- Anterior nerve root
- Posterior nerve root
- Part of the dorsal nerve root ganglion
- A bilaminar sleeve of dura and arachnoid membrane to the ganglion
- A short continuation of the subarachnoid space with cerebrospinal fluid that ends just after the ganglion
- Recurrent meningeal nerve
- Spinal ramus artery
- Intervertebral vein
- Lymphatic vessels
- Fat, fascia, and areolar tissue.
The Cervical Nerves
The cervical nerves coalesce into the cervical plexus (C1–C4) and brachial plexus (C5–T1). See Table 3.2. The cervical nerves are named after the vertebra below; the IVDs, the vertebra above.
Table 3.2. Segmental Function of the Cervical Nerves
CERVICAL PLEXUS (C1–C4) Segment Function C1 Motor to head and neck extensors, infrahyoid, rectus capitis anterior and lateral, and longus capitis. C2 Sensory to lateral occiput and submandibular area; motor, same as C1 plus longus colli. C3 Sensory to lateral occiput and lateral neck, overlapping C2 motor to head and neck extensors, infrahyoid, longus capitis, longus colli, levator scapulae, scaleni, and trapezius. C4 Sensory to lower lateral neck and medial shoulder area; motor to head and neck extensors, longus colli, levator scapulae, scaleni, trapezius, and diaphragm. BRACHIAL PLEXUS (C5–T1) C5 Sensory to clavicle level and lateral arm (axillary nerve); motor to deltoid, biceps; biceps tendon reflex. Primary root in shoulder abduction, exits under the C4 vertebra. C6 Sensory to lateral forearm, thumb, index and half of 2nd finger (sensory branches of musculocutaneous nerve); motor to biceps, wrist extensors; brachioradialis tendon reflex. Primary root in wrist extension, exits under the C5 vertebra. C7 Sensory to second finger; motor to wrist flexors, finger extensors, triceps; triceps tendon reflex. Primary root in finger extension, exits under the C6 vertebra. C8 Sensory to medial forearm (medial antebrachial nerve), ring and little fingers (ulnar nerve); motor to finger flexors, interossei; no reflex applicable. Primary root in finger flexion, exits under the C7 vertebra. T1 Sensory to medial arm (medial brachial cutaneous nerve); motor to interossei; no reflex applicable. Primary root in finger abduction, exits under the T1 vertebra.
Dynamics of the Cervical Cord
During forward flexion of the neck, the cervical spinal canal is lengthened so that the posterior wall of the spinal canal lengthens relative to the anterior wall. The opposite occurs during backward extension. During flexion and extension, the cord itself does not appreciably ascend or descend, but the accordion-like folds within its dural sheath deepen during extension and almost disappear during forced flexion owing to the tension developed by the tensile force.
Dynamics of the Cervical Roots
It is highly controversial whether the nerve root sleeves normally adhere to the IVFs (ie, if they ingress or egress within the IVFs during spinal movements) (See Figure 3.5). Most authorities, however, agree that the roots are normally held high within their respective IVFs in the neutral position and especially so during flexion. During extension, the dura mater and arachnoid around the spinal cord relax and the roots descend to a more mid-IVF position. It is well to keep this in mind when one or more segments are found to be severely locked in flexion or extension.
The nerve roots themselves occupy about a quarter of the contents of the IVF, the remaining area is occupied by the tissues previously listed. The motor root runs close to the clefts (the covertebral joints of Luschka) and the sensory root lies close to the articular processes. Soon after the nerves exit the IVF, their epineural sheaths become attached to the transverse processes, posterior longitudinal ligament, and scalenii fascia. Thus, the roots are not as free as some have reported. [See Clinical Comment 3.1]
Cutaneous Branches of the Cervical Plexus
Extensions of the cervical plexus divide into deep muscular (primarily motor) and superficial (primarily sensory) branches. These latter branches are frequently involved (tender) in subluxation syndromes of C1–C4, especially when the disorder is complicated by advanced spondylosis. The four common resulting neuralgias are:
Lesser occipital neuralgia, which usually manifests in the occipitalis muscle, tissues around the mastoid process, and upper posterior aspect of the pinna.
Greater auricular neuralgia, which expresses over the front and back of the pinna, the skin over the parotid gland, and otherwise parallels the distribution of the auriculotemporal branch of the trigeminus and is thus often mistaken for trifacial neuralgia.
Cervical cutaneous neuralgia, which primarily involves the zone of the middle third of the platysma. It may spread to involve an area extending from the chin to the sternum.
Supraclavicular neuralgia. The anterior, middle, and posterior rami of the lower cervical plexus (C3–C4) have the following cutaneous distribution, respectively: (a) skin over the upper portion of the sternum, (b) skin over the pectoralis major, and (c) skin over the deltoid. Thus, C4 and/or C5 vertebral lesions may produce neuralgia in and refer hyperesthesia to these areas.
The Greater Occipital Nerve
The posterior primary divisions of C2 are by far the largest of all spinal nerve posterior rami. They divide into several terminal branches that ramify in the superficial fascia of the occiput and supply the skin of the scalp above the superior nuchal line as far as the vertex. Kinetic disturbances of the upper cervical segments are notorious in their contribution to mechanical etiologic patterns of cervical neuralgia (migraine), which is typically unilateral and referred along the distribution of the greater occipital nerve. This common disorder will be described later in this chapter.
The Brachial Plexus
The brachial plexus is formed by the anterior primary divisions of C1–T1. Chronic mid- and lower-cervical subluxation complexes and/or traumatic tensile or compression injuries may produce a wide variety of upper-extremity motor and sensory signs and symptoms that often lead to peripheral degenerative changes (eg, frozen shoulder, tendinitis, bursitis, cubital and carpal tunnel syndromes).
The Sympathetic Nerves
Two major components of the sympathetic nervous system are located in the neck: the bilateral sympathetic chains and the vertebral nerves. The vertebral nerves course along the vertebral arteries as they pass through the foramina of the cervical transverse processes thus easily subjected to torsion and shear stresses. Although it is not fully understood how these sympathetic system components cause certain symptoms, the symptoms attributed to them are generally accepted.
The cervical cord contains neither lateral horn cells or preganglionic fibers. Preganglionic fibers of the neck arise from the upper thoracic spine and ascend to the cervical ganglia. Postganglionic fibers from the cervical ganglia course in three directions:(1) branches accompanying the distribution of the anterior roots;
(2) branches that synapse into postganglionic fibers that travel with the cranial nerves and arteries of the neck and head and to the cardiac plexus; and
(3) branches that re-enter the IVFs with the recurrent meningeal nerve to supply the dura and internal longitudinal ligaments. [See Clinical Comment 3.2]The superior cervical ganglion is the largest of the cervical sympathetic chain and lies just below the base of the skull: in front of the axis and C3, between the internal jugular vein and the internal carotid artery. Thus, upper-?cervical kinetic disturbances of any of the upper cervical vertebral joints may cause irritation of this important ganglion leading to symptoms of hypersympathicotonia or to compression leading to Horner's syndrome.
The Vagus
In its bilateral descent through the neck, the vagus passes laterally to the superior cervical ganglion, lying in almost immediate contact with the transverse process of the atlas. Thus, upper-cervical kinetic disturbances (eg, atlanto-occipital and/or atlantoaxial fixations) may cause irritation leading to signs and symptoms of hypervagotonia or pressure leading to hypovagotonia.
Pertinent Neurovascular Considerations
The Recurrent Meningeal Nerve (Nervus Sinu Vertebralis)
The thread-like recurrent meningeal nerve is composed of unmyelinated sensory and sympathetic fibers. It is given off from each spinal nerve at a point just beyond the ganglion and returns through the IVF to supply the dural sheath of the nerve root, the vessels passing through the IVF, and the anterior surface of the dura mater of the spinal cord. Some authorities also state that it sends sensory fibers into the posterior aspect of the anulus of the IVD.
The Vascular BedThe Vertebral Arteries. The vertebral arteries arise bilaterally from the subclavian arteries, pass through the foramina of the cervical transverse processes, and then ascend into the cranium. Each artery is surrounded by a plexus of sympathetic postganglionic neurons (the vertebral plexus) and a venous plexus formed by the vertebral vein. Any external factor that can obstruct a vertebral artery is thus likely to interfere with the drainage of the vertebral vein and the function of the sympathetic vertebral plexus. Typical examples are bony encroachments narrowing the transverse foramina; vertebral artery deflection, torsion, or tension as the result of severe degenerative changes and misalignment of the motion unit (especially the occipito-atlantal unit); severe upper-cervical muscle spasm; or an expanding space-occupying perivertebral mass. The most common cause of intraluminal obstruction is artherosclerosis. The resulting syndromes, which may forewarn an impending stroke, will be described later in this chapter.
The Vertebral Veins. The vertebral veins begin in the posterior vertebral venous plexus in the suboccipital triangle, from which it communicates with the internal vertebral venous plexuses.
The Deep Cervical Veins. These veins, larger than the vertebral veins, course down the neck behind the transverse processes of the cervical vertebrae. They begin in the posterior vertebral venous plexus, receive tributaries from the deep muscles of the neck, and communicate with the occipital veins by a branch that perforates the upper trapezius muscles. For this latter reason, prolonged spasm of the deep suboccipital muscles may produce a congestive stasis leading to a throbbing discomfort and suboccipital pain. Such symptoms, which may be unilateral or bilateral, are often associated with tender nodules within the suboccipital musculature.Cerebrospinal Fluid Circulation: Pertinent Considerations
The intracranial pressure of the cerebrospinal fluid (CSF) system must be sustained within fine limits. An increase in pressure as in hydrocephalus leads to papilledema, cerebral pressure ischemia necrosis, and cerebellar symptoms. A decrease in pressure such as follows a spinal tap of 5 cc or more may lead to intractable headache with possible convulsions and coma.
The posterior medullary velum, which forms the posteroinferior wall of the 4th ventricle and which is perforated by the foramina of Luschka and Magendie, extends well into the foramen magnum. It is separated from the posterior ramus of the foramen magnum by the subarachnoid space and the contained dura mater. It is at this point that one of two possible structural impediments to CSF circulation may occur because of fixed occipitoatlantal shifting, tilting, or rotation:
The cerebral subarachnoid space may become constricted, inhibiting the amount of cerebrospinal fluid flow into the spinal canal and ultimately to the spinal roots and cauda equina. This would result in increased intracranial pressure and possibly decreased intraspinal pressure.
An occipitoatlantal disrelationship may be sufficient enough to press the dura mater constituting the floor of the cisterna cerebellaris (subarachnoid space of the cerebellum) against the posterior medullary velum and partially occlude the exit of the foramina of Luschka and Magendie, thus interfering with CSF egress from the 4th ventricle and increasing intracranial pressure. Early symptoms may include intractable pressure headache, frequent and otherwise unexplainable feelings of nausea with tendencies toward projectile vomiting (especially on exertion), unpredictable protopathic ataxias, and/or bizarre visual disturbances.
BIOMECHANICAL CONSIDERATIONSThe head mechanically teeters on the occipitoatlantal joints, which are shaped like cupped palms tipped slightly medially. Because the line of gravity falls anterior to these articulations, an automatic force must be constantly provided in the upright posture by the posterior neck muscles to hold the head erect. Added to this gravitational stress is the action of the anterior muscles of the neck (essentially the masticatory, suprahyoid, and infrahyoid groups), which serve as a muscle chain to join the anterior cranium to the shoulder girdle.
The biomechanical efficiency of any one of the 26 vertebral motion units from occiput to sacrum can be described as that condition (individually and collectively) in which each gravitationally dependent segment above is:(1) free to seek its normal resting position in relation to its supporting structure below,
(2) free to move efficiently through its normal ranges of motion, and
(3) free to return to its normal resting position after movement.Flexion, extension, rotation, lateral flexion, and circumduction are the basic movements of the cervical region. Movements of the head on the neck are generally confined to the occiput-atlas-axis complex and can be described separately from movements of the neck on the trunk.
Action and Brake Mechanisms in the Spine as a Whole
Flexion
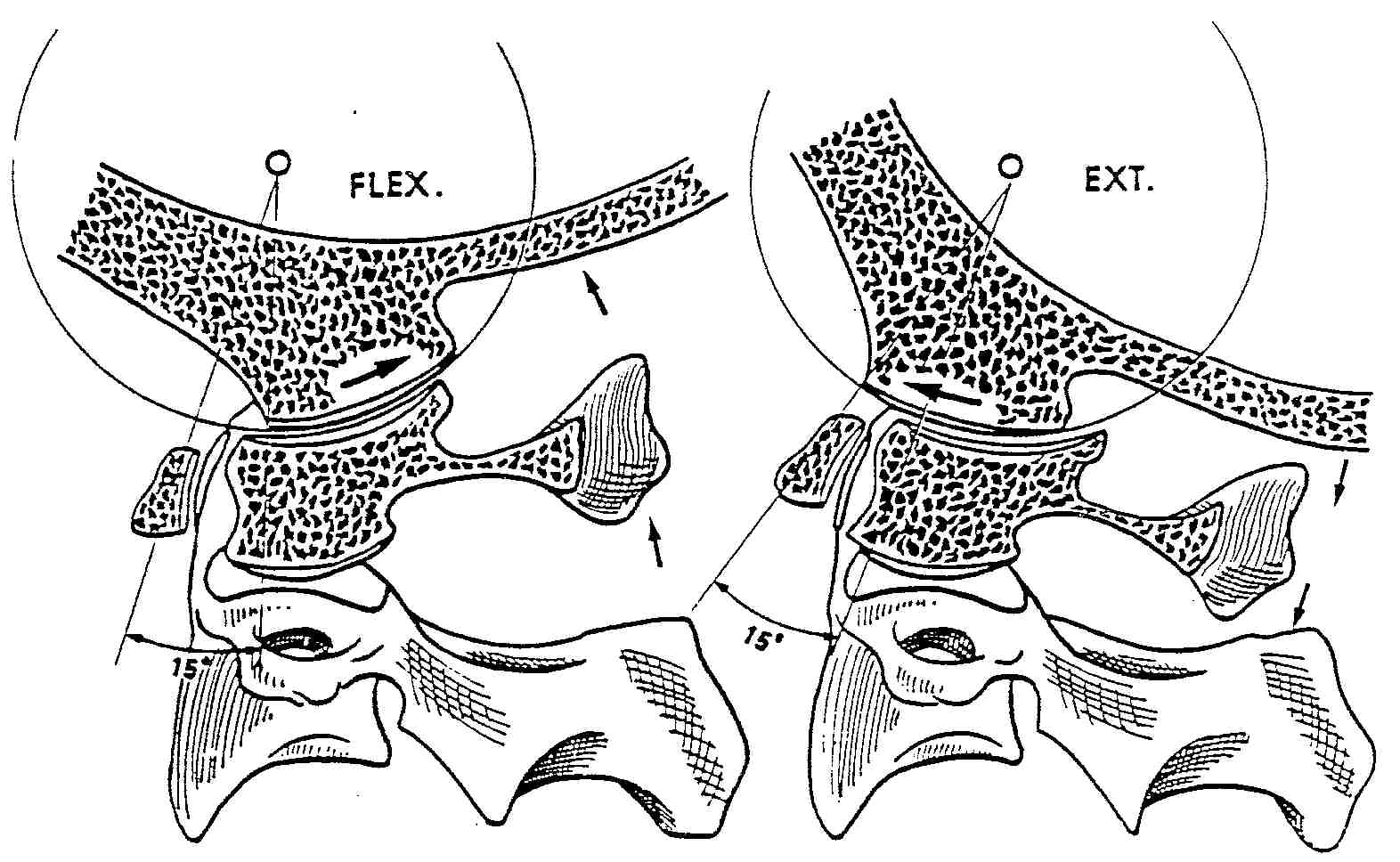
During flexion, the IVDs tend to compress at their anterior aspect, the inferior set of articular facets glide anterosuperiorly on the mating set of superior facets of the vertebra below, and the normal range of motion is checked by the posterior anulus of the disc, posterior longitudinal ligament, intertransverse ligaments, supraspinous ligament, nuchal ligament, and extensor muscle tendons. See Figure 3.6. Slight z-axis translation occurs anteriorly.
Extension
Extension has a much lower magnitude than flexion throughout the spine. The IVDs tend to compress and bulge at their posterior aspect, and the inferior set of articular facets glide posteroinferiorly on the mating superior facets below. The motion is checked by the anterior anulus of the disc, the anterior longitudinal ligament, all the anterior and lateral tendons that contribute in flexion, the anterior fascia and visceral attachments, and probably spinous process and/or laminae jamming at maximum extension. Slight z-axis translation occurs posteriorly.
Rotation
Spinal rotation is limited by the planes of the articular facets, the thickness of the associated IVDs, and the resistance offered by the fibers of the disc's anulus and the vertebral ligaments under torsion.
Lateral Bending
Sideward abduction involves a degree of tilting of vertebral bodies on their discs. The anterior aspect of the vertebral bodies in the upper spine also rotate toward the side of convexity, the posterior aspect swings in the opposite direction, and the facets tend to slide open on the convex side and override on the concave side. The motion is checked by the intertransverse ligaments and intercostal tissues on the convex side, behind the fulcrum, and the apposition of ribs on the concave side in the thoracic region.
Coupling and Related Effects
Some motions restrict other motions and enhance still others. For example, flexion and extension restrict rotation and lateral bending ranges. Rotation decreases A-P and P-A glide and is accompanied by a degree of lateral flexion. Lateral flexion inhibits A-P and P-A glide and enhances cervical rotation toward the concave side and lumbar rotation toward the convex side.
The Upper Cervical Region
All movements in the cervical spine are relatively free because of the saddle-like joints. The cervical spine is most flexible in flexion and rotation. The latter occurs most freely in the upper cervical area and is progressively restricted downward.
An understanding of the basic kinematics of the cervical spine is important to accurate clinical diagnosis and therapeutic applications. Our major concern in this section will be the motion between the occiput and the atlas and the atlas upon the axis. Normal ranges of motion are shown in Table 3.3. It should be noted that the specific ranges of cervical motion differ widely among so many authorities that any range described here should be considered hypothetical depending on individual planes of articulation, other variances in structural design (eg, congenital, aging degeneration, posttraumatic), and soft-tissue integrity. This wide variance in opinion is also true for the centers of motion described. Such guidelines should not prejudice your clinical findings.
Table 3.3. Normal Ranges of Upper Cervical Motion
| Motion Unit | Movement | |
| Occipitoatlantal | Flexion | |
| Extension | ||
| Lateral bending | ||
| Rotation | ||
| Atlantoaxial | Flexion | |
| Extension | ||
| Lateral flexion | ||
| Rotation | ||
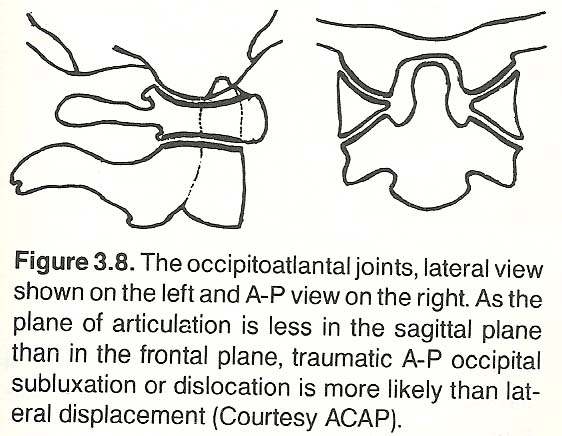 |
The oblique cup-and-saucer occipitoatlantal joints are designed for a limited range of flexion-extension nodding movement (Figure 3.7). Translatory movements are slight; most action is a rolling movement. The long axes of the joints are obliquely set, but a slight curve in the coronal plane allows some end play for lateral tilt.
The frontal plane angle of the joint axes for the occipital condyles can be determined on a radiograph by drawing lines that are parallel to the articulating surfaces of the condyles. Normally, this angle is 124°in males and 127°in females. However, anomalies (congenital or pathogenic) such as basilar impression or condylar hypoplasia will increase this angle. Faye points out that this angle does not really exist as the joint's hyaline cartilage (invisible on film) has a different contour than that of the bone shadows.
Occipitoatlantal Flexion
Much cervical motion is concentrated in specific spinal areas. For example, about half of flexion and extension occurs at the occipitoatlantal joints (Figure 3.8), with the other half distributed among the remaining cervical joints. As the nucleus of the disc is nearer the anterior of a complete cervical vertebra, flexion-extension is more discernible at the spinous process than at the anterior aspect of the vertebral body.
 |
Without any participation of the neck below the atlas, the head can be moved about 10°in flexion between the occiput and atlas. During strict upper neck flexion, the condyles roll backward and slide slightly posterior on the atlas while the atlas rolls anteriorly and somewhat superiorly on the occiput, with the atlas taking the odontoid of the axis with it so that the dens slightly approaches the clivus of the basiocciput. As the atlas slides anteriorly from the condyles, the occiput and posterior arch of the atlas separate just slightly, but this is exaggerated if movement is virtually isolated at the occipitoatlantal joint (eg, in ankylosing spondylitis).
The prime mover of occipitoatlantal flexion is the rectus capitis anterior, aided by the longus capitis. The range is limited primarily by the elasticity of the posterior ligaments and by the tip of the dens meeting the bursa below the anterior rim of the foramen magnum. See Figure 3.9.
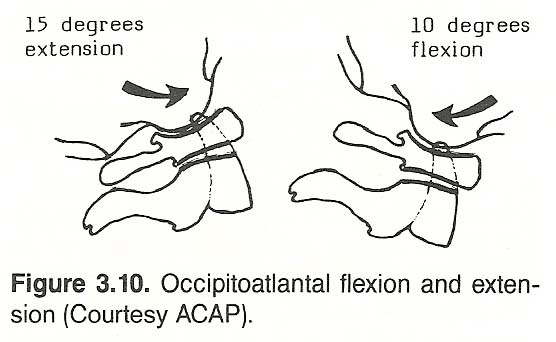
Occipitoatlantal Extension
Upper cervical flexion-extension usually occurs before any lower cervical motion; thus initial visual examination can often help to discern dysfunction of the upper cervical spine solely by observation of active motion. The skull can be extended on the atlas for about 15°without participation by any other cervical vertebra (Figure 3.10). During normal extension of the neck, the condyles slide anteriorly on the atlas and the atlas rolls upward so that its posterior arch approximates the occiput. Slight opening of the inferior aspect of the atlanto-odontoid space occurs, but it is limited by the tectorial membrane.
 |
Upper cervical extension is powered by the rectus capitis posterior group. Extension and lateral tilt of the upper cervical region is restricted by tension of the tectorial membrane and the posterior arch of the atlas becoming trapped between the occiput and the axis. During clinical observation, the chin should move before the neck moves in active cervical flexion and extension.
Occipitoatlantal Lateral Bending
Cervical lateral flexion is performed by the unilateral contraction of the neck flexors and extensors with motion occurring in the coronal plane. Such flexion is accompanied by rotational torsion below C2, distributed fairly equally in the normal cervical joints. That is, when the cervical spine as a whole bends laterally, it also tends to rotate anteriorly on the side of the concavity so that the vertebral bodies arc further laterally than the spinous processes.
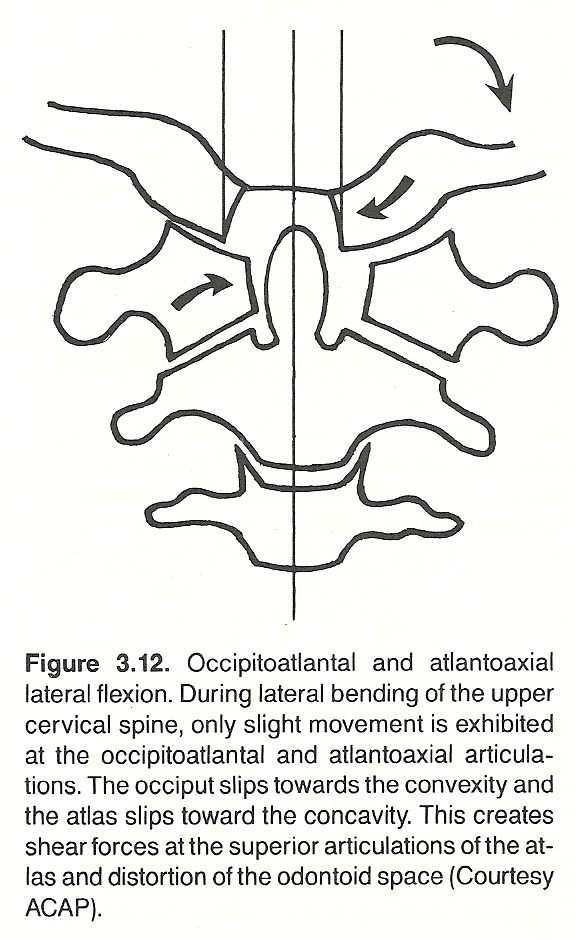
Normally, about a 45° tilt can be observed between the skull and the shoulder. About 7°of this occurs at the occipitoatlantal joint, following the arc of the condyles on the superior facets of the atlas (Figure 3.11). As the occiput and atlas shift laterally as one unit towards the concavity during lateral bending, the space between the dens and lateral mass of the atlas widens on the concave side. At the same time, the occipital condyles translate slightly laterally on the superior facets of the atlas toward the convexity and the atlas slips slightly toward the side of concavity. These movements are slight unless there is a degree of instability involved. If the occipito-atlantal capsular ligaments are weakened, the condyle on the side of lateral bending may strike the tip of the odontoid. The body of the axis tends to rotate towards the concavity while its spinous process shifts toward the convexity owing to the coupling mechanism.
Occipitoatlantal lateral bending is produced by the rectus capitis lateralis, which is helped by the semispinalis, splenius capitis, sternomastoideus, and trapezius. The range is limited primarily by the alar ligaments. In mild coronal lateral flexion and transverse rotation of the head and neck, the occiput and atlas move as a unit because of the planes of the articular facets. Close observation will show that the occiput specifically abducts on the atlas without rotation about a vertical axis. Thus, the atlas is caught between trying to follow the motion of the occiput or the axis. (Figure 3.12). This stress, according to Gillet, forces a slight amount of rotational end play of the occiput on the atlas even though the design of the condyles is not conducive to rotation.
Occipitoatlantal Rotation
 |
During rotation, the occipital condyles and the atlas initially move as one unit on the axis. Approaching the end of the range of motion, the condyles can rotate a few degrees on the atlas in the direction of movement. Some authorities contest this fact, thus the range is often listed as 0°.
Atlantoaxial Flexion
In addition to the side-rolling motion of the atlas on the occiput, the atlas is capable of some tilting where the anterior ring of the atlas moves upward on the odontoid and the posterior arch rides downward, or vice versa.
During severe flexion, there could be considerable separation of the anterior arch of the atlas from the odontoid, but it is checked by the weak transverse arms of the cruciate and by tension of the stronger tectorial membrane.
During cervical flexion, the inferior lateral masses of the atlas roll upward posteriorly and slide backward on the superior facets of the axis. Opening of the superior aspect of the atlanto-odontoid space is not appreciably restricted by the delicate transverse cruciate ligament (Figure 3.13). Movement is restricted mainly by the apophyseal capsules, the ligamentum flavum, the interspinous ligament, the posterior nuchal muscles, and apposition of the chin against the sternum.
Atlantoaxial Extension
Similar to the motion described between the occiput and atlas during cervical extension, the posterior arches of the atlas and axis also approximate. The range of pure extension of C1 on C2 is minimal. The reason for this is that all other segments of the spine tip and translate posteriorly during extension from the neutral. The atlas cannot do this because of the odontoid process of the axis (Figure 3.14). All that it can do during extension of the neck is tip downward at its posterior aspect and tip upward at its anterior aspect, a rotatory motion. During forced extension, the posterior arch of the atlas is caught as in a vise between the occiput and axis. Extension is even more resisted when the anterior arch meets the odontoid and the interarticular tissues compress. These facts are important to remember when someone speaks of extension of the atlas on the axis.
Atlantoaxial Lateral Bending
Some authors report that no motion occurs between C1 and C2 during lateral bending; however, motion palpation typically reveals slight motion (joint play) that follows the arc of the inferior facets of the atlas on the superior facets of the axis. Thus, if a major fixation is found at this point, it should be released because it is an extremely symptom-producing fixation.
When lateral flexion is restricted to the upper cervical area, the articulating facet spaces open on the side of convexity and compress on the side of concavity. However, when lateral flexion is generalized throughout the cervical region, the lateral masses of the atlas sideslip towards the side of concavity so that the space between the lateral mass and the odontoid increases on the side of the concavity. Obviously, this is limited by the size of the bony crescent about the dens unless the cruciate is torn.
Atlantoaxial Rotation
During normal movement, the occiput and atlas move as one about the odontoid process of the axis (Figure 3.15). [See Clinical Comment 3.3] Keep in mind that the odontoid of the axis is usually firmly attached to the occiput via the ligament complex. These ligaments (especially the alar ligaments, transverse cruciate, and the apophyseal capsules of the axis) tend to restrict C2 rotation on C3 as compared to the wide range allowed by the atlas. Although the inferior facets of the atlas and the superior facets of the axis may both be concave (as viewed on film), their articular cartilages are biconvex.
The inferior facets of the atlas are the flattest of any in the spine, and the superior facets of the axis are convex and slope slightly downward laterally. This pivotal design offers a gap anteriorly and posteriorly between the facets as much as 2 5 mm. In addition, the extremely loose and wide articular capsules of the C1-C2 joint, which enter the articular space on each side to form a meniscus-like fold of synovium, probably allow the greatest degree of inherent instability present in the cervical spine. It is for these reasons that misdiagnosis of axial instability is a common orthopedic error. During ineroentgenographic studies, the atlas appears to almost fall off the superior facets of the axis during maximum rotation.
About half of active cervical rotation takes place at the atlantoaxial joints about the odontoid process, with the remaining half distributed fairly evenly among the other cervical joints. During rotation, the odontoid represents a peg encased within an enclosed ring or a stake surrounded by a horseshoe. C1 rotation normally occurs about the dens of C2, which serves as a pivot.
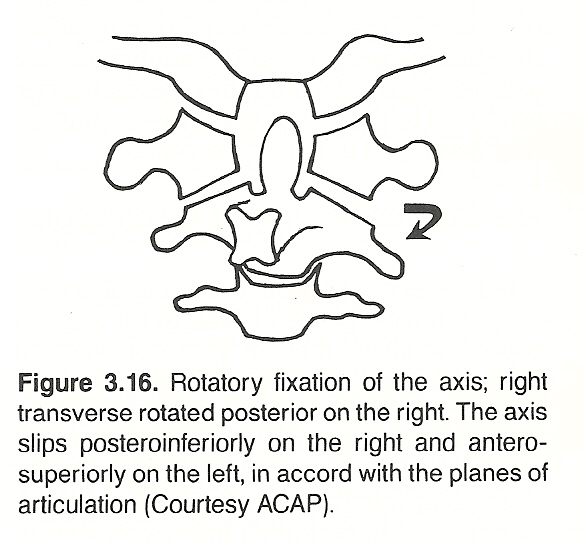 |
As mentioned, 50% of total neck rotation occurs between C1 and C2 before any rotation is noted from C2 to C7 or at the occipitoatlantal joint. After about 30°of atlas rotation on the dens, the body of the axis begins to rotate (Figure 3.16), followed by progressively diminishing rotation in the remaining cervical segments. Because the occipitoatlantal and atlantoaxial apophyseal articulations are not horizontal, rotation must be accompanied by a degree of coupled tilting.
Atlantoaxial rotation is powered by the obliquus capitis and rectus capitis posterior major, with help offered by the ipsilateral splenius capitis (Figure 3.17) and the contralateral sternocleidomastoideus. During maximum atlantoaxial rotation in a supple spine, there is considerable kinking or stretching of the contralateral vertebral artery. Remembering this may save you from a malpractice suit.
If a complete fixation occurs between C1 and C2, the remaining cervical segments tend to become hypermobile in compensation. Thus, gross inspection of neck rotation (or other motions) should never be used to evaluate the function of individual segments. Specific segmental motion palpation is always required. [See Clinical Comment 3.4]
The Lower Cervical Region
The IVDs of the lower cervical region normally contain an exceptional amount of elastin, which allows them to conform to the many possible planes of movement. Excessive flexion is limited by the ligamentous and muscular restraints on the separating posterior arches, and overextension is limited by bony apposition. Other factors include the resistance of the anular fibers to translation, the stiffness property of the anulus relative to its vertical height, and the physical barrier produced by the uncinate processes that are
fully developed in late adolescence.
The Cervical Planes of Articulation
In the cervical region, the plane of articulation is almost perpendicular to the sagittal plane and inclined about 45°to the vertical plane. The lateral cervical gravity line extends from the apex of the odontoid process through the anterior portion of T2. The stable base between T1–T2 progressively changes upward so that the planes of articulation tend to be forced inferior, posterior, but not medially as in the thoracic and lumbar regions of the spine.
A horizontal locking-type base of support at the atlantoaxial articulation is similar to that found at the lumbosacral area. The inferior articular surfaces of the atlas offer a bilateral, medial, and inferior slant that forces the atlas to move inward toward the odontoid to allow rotary movements of the head. Excessive A-P and P-A movement is stabilized by the anterior and posterior rings and check ligaments. The posteromedially slanted cup-like superior articular surfaces of the atlas help stabilize the occipital articulating surfaces. These concave facets allow free rocking for flexion-extension nodding of the head.
From C3 to C7, the almost flat and thus freely mobile articular processes are found at the junction of the pedicles and laminae. The inferior facets face downward and forward, and glide on the superior facets of the vertebra below which face upward and backward. Maximum cervical A-P and P-A motions usually take place between C4 and C5. It should also be noted that it is almost impossible to actively flex the normal neck without causing some flexion in the upper thoracic region.
Facet Action
In the mid- and lower-cervical areas, A-P and P-A motion is a distinctly gliding translation because of the 45°facet planes and the biconcave vertebral bodies (Figure 3.18). During flexion and extension, the superior vertebra's inferior facets slide anterosuperiorly during flexion and postero-inferiorly during extension on the inferior vertebra's superior facets. During full flexion, the facets may be almost if not completely separated. Thus, an adjustment force is usually contraindicated in the fully flexed position. The center of motion is often described as being within the superior aspect of the body of the subjacent vertebra.
Some pivotal tilting of the superior facets, backward in extension and forward in flexion, is also normal near the end of the range of motion. The facets also tend to separate (open) on the contralateral side of rotation and lateral bending. They appose (compress) during extension and on the ipsilateral side of rotation and lateral bending.
Likewise, the foramina normally open on flexion, narrow on extension, close on the concave side of lateral bending, and open on the convex side of lateral bending. Because of the anterosuperior slant of the lower cervical facets, an inferior facet that moves downward must also slide posteriorly, and vice versa.
Any corrective adjustment must take into consideration the general extent of cervical lordosis, the existing planes of articulation, the facet tilt present, and the amount of interfacet opening, as well as any underlying pathologic process(es) involved, and applying just enough force during correction to overcome the resistance of the fixation into the direction of the resistance.
Coupling Patterns
In the cervical spine, rotation about the Z axis is coupled to rotation about the Y axis, and vice versa; ie, during cervical lateral bending the cervical centra tend to rotate toward the concavity while the spinous processes swing in a larger arc towards the convexity.
Note that this is exactly opposite to the coupling action that occurs in the lumbar spine. During cervical bending to the right, for example, the right facet of the superior vertebra slides down the facet plane and toward the posterior and the left facet slides up the facet incline and toward the anterior. This coupling phenomenon is exaggerated in circumstances in which an unusual ratio of axial rotation and lateral bending produces a subluxation or unilateral facet dislocation.
The amount of cervical rotation that is coupled with lateral flexion varies with the segmental level. At C2, for example, there is 1°of rotation with every 1.5°of lateral flexion. This 2:3 ratio changes caudally so that the degree of coupled rotation decreases. At C7, there is 1°of rotation for every 7.5°of lateral flexion, a 2:15 ratio.
Ranges of Motions
All cervical vertebrae from C2 to C7 partake in flexion, extension, rotation, and lateral bending, but some segments are more active in certain movements than others. In the C3 C7 area, flexion and extension occur as mild gliding translation of the upper on the lower facets, accompanied by appropriate disc distortion. The site of greatest movement in flexion is at the C4–C5 interface (Table 3.4), while extension movement is fairly well diffused. This fact probably accounts for the high incidence of arthritis at the midcervical area. Rotation below the axis is greatest near the C5–C6 level, slightly less above and considerably less below. Lateral bending in greatest at the C2–C5 levels and diminishes caudally. The arc of lateral motion is determined by the planes of the covertebral joints (if they are present). Faye points out that, for cervical lateral flexion, the first rib costotransverse joint must be mobile because it is an important component of the kinematic chain.
| Motion Unit | Movement | |
| C2–C3 | Flexion/extension | |
| Lateral bending | ||
| Rotation | ||
| C3–C4 | Flexion/extension | |
| Lateral bending | ||
| Rotation | ||
| C4–C5 | Flexion/extension | |
| Lateral bending | ||
| Rotation | ||
| C5–C6 | Flexion/extension | |
| Lateral bending | ||
| Rotation | ||
| C6–C7 | Flexion/extension | |
| Lateral bending | ||
| Rotation | ||
| C7–T1 | Flexion/extension | |
| Lateral bending | ||
| Rotation | ||
Lower Cervical Instability
Instability in the lower cervical region is rarely obvious in the ambulatory patient. The most important stabilizing agents in the mid- and lower-cervical spine are the anulus fibrosis, the anterior and posterior ligaments, and the muscles, especially, which serve as important contributing stabilizers. During dynamic palpation, states Faye, any segmental joint play found to be more than a "spinginess" should arouse suspicions of lack of ligament restraint. This is often accompanied by an audible click (similar to that heard during knuckle cracking).
Motion of the Transitional Cervicothoracic Area
In the cervicothoracic area, normal movement is somewhat similar to that in the lumbosacral area insofar as the type of stress (but not magnitude of load) to which both areas are subjected is similar. L5 has poor mobility on the sacrum and C7 has poor mobility on T1, with the major amount of movement in the cervicothoracic junction being at the C6–C7 interface and primarily that of rotation. Faye mentions that diminished cervicothoracic joint play is clinically significant in many chronic, stubborn cases.
Reversal of the Normal Cervical Curve
As opposed to the primary thoracic kyphosis which is a structural curve, the cervical and lumbar lordoses are functional arcs produced by their wedge-shaped IVDs (developed in the upright position).
The cervical and lumbar curves normally flatten in the non-weight-bearing supine position. Likewise, they adapt comparatively fast to changes involving the direction of force. Adaptation in the thoracic spine takes much longer.
The force of gravity on the cervical lordosis normally falls just anterior to the support of the posterior cervical musculature. When the cervical curve flattens, a larger workload is placed on the musculature of the neck to maintain biomechanical integrity. A pathologic straightening of the normal anterior curve of the cervical spine, as viewed in a lateral weight-bearing x-ray film, results in mechanical alteration of normal physiologic and structural integrity. The normal vertical line of gravity, as viewed laterally, falls near or through the odontoid and touches the anterior border of T2. As the cervical spine tends to flatten in the erect position, the gravity line passes closer to the center of the cervical discs.
While the cervical curve is the first secondary curve to develop in the infant, its maintenance in the erect posture is primarily determined by the integrity of the lumbar curve when the spine is supple. Faye considers the angle of the thorax an equally important factor; ie, the sternum should face slightly upward. A flattened cervical spine that is not compensatory to a flattened lumbar spine is usually the result of a local disorder such as a subluxation syndrome caused by facets fixed in flexion, posterior shifting of one or more disc nuclei, hypertonicity of the anterior musculature, or anterior ligamentous shortening as the result of local overstress, inflammation, occupational posture, or congenital anomaly.
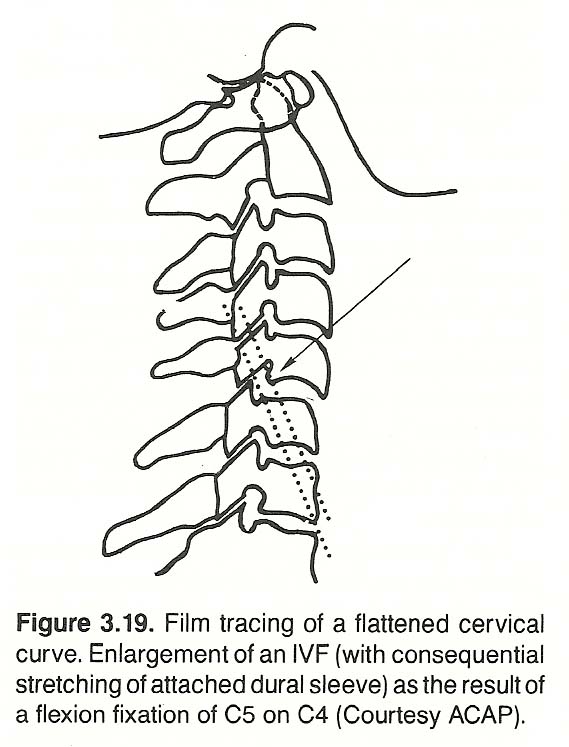 |
A flattened cervical spine in the erect posture resembles a normal spine during flexion. To appreciate the mechanisms involved, it is well to review the biomechanics involved: The nucleus of the disc serves as a fulcrum during flexion and return extension. When the spine is subjected to bending loads during flexion, half of the disc on the convex side suffers tension, widens, and contracts, while the other half of the disc on the concave side suffers compression, thins, and bulges. Concurrently, the nucleus bulges on the side of tension and contracts on the side of compression, which increases tension on the adjacent anulus. This creates a self-stabilizing counteracting flexion force to the motion unit that aids a return to the resting position.
In a reduced curve (cervical hypolordosis), Bergmann reminds us that more weight has to be born on the vertebral bodies and discs; while in an increased curve (hyperlordosis), more weight must be borne by the facets. The shape of the vertebra and angles of the facet and disc determine the degree of lordosis. If through degenerative changes and/or stress responses these are altered, the "normal" arc of the curve will be changed.
Numerous studies relating ideas of what the normal curve should be have been conducted, and most seem to be in agreement that the cervical lordosis extends down to T2, with C5 being the midpoint or "stress" vertebra (See Figure 3.19). Flattening of the cervical curve is often the result of perispinal spasm secondary to an underlying injury, irritation, or inflammatory process. The latter may be the result of a lower primary fixation.
Symptomatology. The acute clinical picture can be torticollis. Other manifestations may include headaches (occipital, occipitofrontal, or supraorbital), vertigo, tenderness elicited on lateral C4–C6 nerve roots, neuritis involving branches of the brachial plexus owing to nerve root irritation, hyperesthesia of one or more fingers, and loss or lessening of the biceps reflex on the same or contralateral side. In less frequent situations, the triceps reflex may be involved. One or more symptoms are frequently aggravated by an abnormal position of the head such as during reading in bed, an awkward sleeping position, prolonged typing, or long-distance driving.
Effect of Atlas Position. It has been postulated by several authorities that the cervical curvature directs the position of the atlas; ie, a hyperlordotic cervical spine is compensated by the atlas moving superiorly and that a flattened curve is compensated for by the atlas moving inferiorly. After studying the lateral cervical films of 109 patients, however, Ng has shown statistically that malposition of the atlas in the A-P plane does not necessarily accompany an alteration of the cervical curve. No significant correlation could be found between the atlantopalatal angle and the degree of cervical curvature, thus indicating that an anterosuperior atlas does not necessarily accompany cervical hyperlordosis or vice versa.
Dynamic Palpation of the Cervical Region
The objectives of dynamic palpation are to note:
(1) normal and abnormal segmental motion and
(2) motion restrictions, "jumps," erratic gliding, and motion smoothness. Bilateral motion quantity and quality are primary concerns because of their influence of the health of the individual, biomechanically and neurologically.
During motion palpation, each cervical motion unit is palpated during flexion, extension, rotation, and lateral flexion to assess segmental mobility and end play. The amount of motion in any particular joint primarily depends on:
(1) the shape of the joint surface,
(2) the laxity or tautness of supporting ligaments, and
(3) the tone of the related musculature. See Figure 3.20. The extent of movement below the axis is primarily dependent upon ligamentous and muscular laxity and the distortion and compressibility of the IVDs. On this point, Faye includes the joints of Lushka.
The "joints" of Lushka (or uncovertebral joints) are not found in a large percentage of the population. Jeffrey's points out that an academic controversy has existed for many years of whether these clefts on the cervical segments are true synovial joints. The current orthodox teaching is that they begin as stress fissues of the annular fibers, which appear in the second decade of life, and are later converted into cartilage-lined joint surfaces.
Cervical Muscle Considerations
Gillet's investigations have shown that several deep short muscles are found in the cervical region that have a tendency toward hypertonicity and therefore fixation. It must be emphasized, however, that most of them are reflexively influenced by lower primary fixations and, thus, not necessarily in need of manipulation. They often require trigger-point therapy and/or massage for the fibrotic changes, states Faye who adds that this is a difficult area for electrotherapy.
The Intertransversarii. The cervical muscles most involved in a muscular fixation, according to Gillet, are the anterior and posterior intertransversaii that assist lateral bending, usually working reciprocally. When hypertonic, however, they often act separately. Acting together unilaterally, they pull the top vertebra of a motion unit into lateral flexion with a certain amount of rotation because of the plane of articulation of the cervical segments. When acting bilaterally, then assist forward flexion. When fixed in flexion, they tend to produce a segmental or area hypolordosis or, at times, kyphosis.
Chronic hypertonicity of the anterior intertransversaii forces flexion even when the spine is in the neutral resting position. The involved segments will be hypolordotic, hypermobility will be found at the extreme posterior elements of the vertebrae, and segmental extension will be restricted. The same state can occur in reverse when the posterior transversarii become fixed in extension; ie, flexion will be restricted. At times, intertransversaii fixation will be found both anteriorly and posteriorly. Both of these pairs of muscles can limit motion (lateral bending especially, and rotation partially), although they do so to a lesser degree than the rotatores and multifidi.
Because these muscles are so small, deep, and so close to each other, it is often difficult to determine which are responsible for any given restriction or dysfunction. Fortunately, hypertonic muscles can often be palpated as abnormal bulges, and this is especially true when they are put under tension. In many cases, they are secondary and recur if primary fixations in the subluxation complex are not adjusted.
The Multifidi and Rotatores. In the mid and lower cervical region, it seems that the multifidus muscles are more apt to be abnormal. Around the axis and C3, however, Gillet has found that the rotatores are often found to be responsible. Each type of fixation has, fortunately, its type of motion in which it is felt more easily during motion palpation. The multifidi arise from the transverse processes of the cervical vertebrae and insert on the spinous process of the segment above, assisting in extension and rotation. The rotatores are a series of small muscles that span deep in a groove between the spinous and transverse processes of each vertebrae, assisting in extension and rotation toward the opposite side.
The Interspinales. The interspinal muscles are short bands of well-developed muscle fibers that extend bilaterally between the spinous processes of contiguous vertebrae, assisting in extension. Hypertonicity contributes to hyperlordosis. This exaggerated lordosis may be short, and the hypertonic muscles involved are usually easily discernible. It becomes especially visible when the patient's neck is passively moved into maximum forward flexion. Although this type of fixation is common, Gillet believes it is rarely pathogenic.
The Oblique Muscles of the Head. The obliquus capitis superior arises from the transverse processes of the atlas and insert broadly on the occiput, helping to extend and move the head laterally. The obliquus capitis inferior arises from the spinous process of the axis and inserts on the transverse processes of the atlas, assisting in rotating the atlas and head. When these muscles are hypertonic on one side, the axis can be pulled laterally. See Figure 3.21.
The Rectus Capitis Group. The rectus capitis posterior major arises from the spinous process of the axis and inserts broadly on the occiput, assisting in extension of the head (Figure 3.22). When hypertonic, the occiput is rotated backward upon the spinous process of the axis, obliterating the space over the posterior tubercle of the atlas and thus producing atlantal hyperlordosis. It is usually caused by a primary fixation found much lower in the spine, according to Gillet (eg, anterior thoracic body fixation). The rectus capitis posterior minor arises from the posterior tubercle of the atlas and broadly inserts on the occiput, assisting in extension of the head. The rectus capitis lateralis originates on the transverse process of the atlas and inserts on the jugular process of the occiput (Figure 3.23), assisting in flexion and stabilization of the occiput on the atlas. The rectus capitis anterior arises from the lateral masses of the atlas and broadly insert on the basilar part of the occiput, also assisting in flexion and stability of the cranium.
The Longus Colli. The superior oblique portions of the long muscles of the neck arise from the C3–C5 transverse processes and insert on the anterior tubercle of the atlas, assisting in cervical flexion and stabilization. Spasm or chronic contraction of the cervical longus colli produces a clinical picture that is opposite to that of rectus capitis major fixations. The head is pulled down and forward, opening the space between the occiput and the axis, thus producing atlantal kyphosis.
The Longus Capitis. The long muscles of the head arise from the C3–C6 transverse processes and insert at the occiput, assisting in flexion of the head. Hypertonicity contributes to flattening of the cervical curve.
The Occipito-Atlanto-Axial Complex
The occipital condyles, atlas, and axis function as a unit with unique characteristics. The normally ball-and-socket-type articulations at the occipitoatlantal joint allow flexion, extension, slight lateral flexion, and rotation end play. The facets of the atlas and axis are both convex. This allows considerable rotation and minimal lateral flexion, and their loose capsules and ligamentous straps allow significant flexion and extension. The axis, however, has more ligamentous attachments with the skull than does the atlas. Dove describes how many of these attachments bypass the atlas as does the spinal dura. The muscles that attach to the axis extend widely to the skull and atlas above, and to all the lower cervicals, upper five thoracics, first rib, and scapulae.
Craton reports that differences in area size of the two condyle-glenoid groove surfaces results in different articular mobility. The least mobile articulation exhibits the least erosion of the cartilage plates, and he suggests that a condyle sideslip with a counterclockwise rotation is the cause of the variable erosion and size.
Occipital-Atlantal Palpation
The occipitoatlantal junctions are typically described as ball-and-socket-type joints, where the condyle "ball" is elipsoid and its axis is transverse. This, states Dove, permits flexion-extension and a slight amount of rotation and lateral flexion. However, Rude, a German investigator, has shown that the occipital condyles vary greatly in shape, and the specific design of the facets determines their movement. While typically convex, many condyles have been found to be square, rhomboidal, rectangular, flat, prismatic, concave (rare), and some have split forms. Flattened and angular condyle facets allow great slipping and tipping during motion. A convex condyle facet allows only rotary slippage if the corresponding atlantoid facet has a similar radius. These facts should be kept in mind during occipitoatlantal motion palpation.
 |
NOTE: All motion-palpation procedures described in this chapter are conducted with the patient in the standard sitting posture and the doctor sitting directly behind the patient. As previously mentioned, a motion palpation station is used to allow the doctor to swing sideways for greater leverage and ease.
Rotation of the Occiput on the Atlas. Place the pad of your palpating finger on the tip of a transverse process of the patient's atlas (Figure 3.24). With your stabilizing hand on the patient's skull, rotate the patient's head slowly to one side, then to the other side (Figure 3.25). Avoid any flexion, extension, or lateral bending of the patient's neck. This is enhanced by using your palpating finger as a fulcrum. Repeat with your palpating finger on the patient's contralateral transverse process. You will be able to feel the transverse process glide behind the mandible when the patient's head is fully rotated to the side of palpation. If the joint is fixed, this motion will be absent. Occipital rotational end play is sometimes a difficult motion to palpate because of the bulging of the srnocleidomastoideus tendon. Obviously, Gillet and Faye support those authors who rport ocipital rotation on the atlas because it is palpable.
Flexion-Extension of the Occiput on the Atlas. This is a remarkable two-phase process. During the first phase, the occiput anteflexes on the atlas. During the second phase of flexion, however, Snijders/Timmerman state that the occiput retroflexes relative to the atlas and axis during flexion-extension of the neck.
With your stabilizing hand supporting the patient's vertex, place your palpating finger into the small space between the lateral tip of a transverse process of the atlas and the ramus of the patient's jaw (Figure 3.26). Push the patient's head with your stabilizing hand so that the patient's chin moves directly forward, parallel to the floor. Have patience in your practice of this palpation, as the skill can be difficult to master. If there is no unilateral fixation, you should feel the space between the transverse process and the jaw open wider. (The pushing hand on the crown of the patient's head should feel for the springy end feel, states Faye.) Then bring the patient's occiput backward, tucking the patient's chin inward against the throat (Figure 3.27). If there is no unilateral fixation in flexion, the space being palpated will narrow and sometimes become lost to the touch. Repeat this procedure on the contralateral side.
During this evaluation, the ramus of the jaw may be felt to flip distinctly superior rather than rolling anterior. Gillet believes that this hinge-type motion (rather than a rolling motion) is the result of hypertonicity of the rectus posterior minor muscle, either unilateral or bilateral, that produces restricted motion of the posterior atlas but free motion of the anterior atlas. If this is the case, forced motion will produce a shear force. On the other hand, if the anterior muscles are hypertonic, the anterior aspect of the condyle will be compressed against the anterior lateral mass of the atlas, while the posterior aspect opens. This can be palpated on forced motion by placing the palpating finger in the posterior aspect of the transverse mastoid space while the patient's head is moved into maximum extension and flexion.
Lateral Bending of the Occiput on the Atlas. Place your palpating finger over the tip of a transverse process of the patient's atlas. Place your stabilizing hand on the patient's vertex and flex the crown laterally (Figure 3.28), first toward one side and then toward the other, taking care to localize motion at the occipitoatlantal level. Avoid midcervical motion by using your palpating finger as a fulcrum. If fixation is absent, you will be able to feel the space above the transverse process open and close as you laterally flex the patient's head away and toward your palpating finger. Again, states Faye, the hand stabilizing the patient's crown feels for joint end play.
Differentiating Occipitoatlantal Muscular and Articular Fixations. The tip of the palpating finger is placed under the posterior occiput, midway between the occipital notch and the mastoid process (Figure 3.29). Some examiners prefer to cup the atlas in the web of the palpating hand so that the thumb palpates one side while the middle finger palpates the other side. The supporting hand rocks the patient's head into flexion and extension. If a stubborn articular fixation exists, the fibrous tissues will feel like a hard mass that does not change texture during motion. This feeling is characteristic and different from the softness of the tissues surrounding a freely or partially movable atlas. You also have an opportunity here of changing hands and palpating the same spot on the other side. Keep in mind that if a total fixation is evident unilaterally, the atlas will not be able to move on the contralateral side even if all tissues there feel normal.
An important exception to the rule that the amount of irritation decreases with the degree of fixation is found with total fixation of the occipitoatlantal joints. Here, for some unknown reason, there is almost never degeneration in the soft tissues and the fixation remains in an acute stage, according to Gillet. Thus, in this disorder, the amount of signs of irritation increases with the degree of fixation.
Atlantal-Axial Palpation
Rotation of the Atlas on the Axis. The pads of the first three fingers are placed horizontally in the suboccipital space so that the first finger firmly presses against the occipital notch, the second finger rests in the space over the posterior tubercle of the atlas, and the third finger rests lightly on the tip of the C2 spinous process. The free hand is used to rotate the head. During passive rotation, several degrees of atlas rotation should take place before the axis begins to move. Normally, the third finger will slip on the spinous process of the axis as the head is rotated because the head moves 1 cm or more prior to axial motion. Bilateral atlantoaxial fixation is indicated if the axis immediately follows the movement of the head (primarily the atlas), noted by the third finger not gliding over the process of the axis. If unilateral (pivotal) fixation is present, this situation will occur during rotation to one side but not to the other, and the center of movement will be at the point of fixation rather than at the odontoid. If the axis is fixed unilaterally, rotary movement will also be felt on the free side during A-P motion.
Faye also checks the mobility of atlas-axis rotation by placing the pads of the palpating fingers against the pillars of the upper cervical vertebra. He pronates his wrist and palm and holds his elbow horizontal during this palpation (Figure3.30). At the extreme of passive rotation, he uses an end push to judge the integrity of end play. During atlantal-axial A-P rotation, facet translation is judged with the fingertips placed on the anterolateral aspect of the transverse process of the atlas (Figure 3.31). These P-A and A-P motions, as all motions, must be checked bilaterally.
Lateral Bending of the Atlas on the Axis. Active lateral bending of the atlas on the axis is questioned by some authorities, but an important and distinct end play can be palpated in healthy spines. It has been Gillet's experience that abnormal lateral flexion of the atlas on the axis is affected most by hypertonicity of the intertransversarii and/or the upper part of the longus colli. Motion restriction can be determined by placing the tip of the palpating finger in the posterolateral space between the transverse processes of the atlas and axis and making contact on the atlas close to the rim of the occiput posterolaterally (Figure 3.32). It is often necessary to slip off the occiput to contact the atlas. The fulcrum for lateral bending is at the palpating finger, and a springy end feel is tested before any lower cervicals begin movement. Remember, in this type of motion palpation, we are palpating for fixation at the end of the passive range of motion. We are not palpating the gross motion available. Our palpation is a joint challenge, and we try to determine if the resistance is(1) more than normal but a springy muscular fixation exists,
(2) more than normal with an abrupt end feel, or
(3) abrupt with an end feel in all directions.While intertransversarii hypertonicity restricts lateral bending, a small degree of lateral gliding of the atlas on the axis is usually allowed. This does not appear to be true when hypertonicity of the longus colli exists or if articular fixation is present.
Flexion-Extension of the Atlas on the Axis. Palpate between the transverse processes of the atlas and axis during passive flexion-extension of the patient's head. During normal motion, you should feel the transverse process of the atlas glide forward (anteriorly) during flexion and return (posteriorly) to neutral during extension (Figure 3.33). [See Clinical Comment 3.5] Keep in mind that there cannot be true posterior extension translation of the atlas on the axis from the neutral position because of the odontoid process. Only tipping can occur.
Another method is to place the palpating finger in the space between the posterior tubercle of the atlas and the spinous of the axis. This space should open on flexion and close on extension of the neck, and the posterior tubercle should become more apparent on flexion and be lost to touch on extension of the neck.
Occipital and Lower Cervical Relationships
The occiput and axis are not structually adjacent, thus cannot articulate, but, as previously described, they are combined into a function unit by ligaments, fascia, and several deep cervical muscles, which, when shortened, pull the occiput and lower cervicals into hyperlordosis. This type of fixation is sensed by putting the pads of the palpating fingers into the interspinous spaces, placing your stabilizing hand on the patient's vertex, and then conducting the patient's head into full upper-cervical flexion and extension.
For example, hypertonicity of the rectus capitis posterior major and minor produces extension of the occiput toward the spinous process of the axis in the neutral resting position. The upper- and mid-cervical interspinous spaces will feel closed even during passive flexion of the neck. Hypertonicity of the superior oblique portion of the longus colli and/or rectus capitis anterior and lateralis pull the cervical spine into flexion. The interspinous spaces will feel open even on forced passive extension of the neck. [See Clinical Comment 3.6]
Lower Cervical Palpation
All cervical vertebrae from C2 to C7 partake in flexion, extension, rotation, and lateral flexion, but some segments (eg, C5) are more active than others. Refer to Table 3.4.
Lateral Flexion of C2–C7. The mid and lower cervicals are palpated in lateral bending as moving away from the side of flexion. To evaluate lateral gliding, place your thumb or the pad of your pronated middle finger firmly against the posterolateral aspect of the spinous processes or on the articular pillars of the segments being evaluated, while your supporting hand moves the patient's head in wide lateral flexion (refer to Figure 3.32). Laterally flex the patient's head over your palpating finger, which will serve as a fulcrum, and check for additional joint play at the end of passive motion.
The importance of palpable asymmetry in response to passive cervical sidebending has been clearly brought out by Johnston and associates who concluded that it appears to be an early indicator of a measurable impairment of cervical function, even in the absence of pain or other complaints. Thus, the role of segmental motion palpation in preventive health-care is underscored.
Segmental motion studies should not be confused with gross motion studies. When a motion-unit becomes dysfunctional, it exhibits asymmetric behavior that is palpable. In addition, secondary (compensatory) effects spread to adjacent units, usually within three segments, which does not necessarily limit regional function. Only in advanced stages where multiple units are involved will overt regional motion be affected.
Flexion-Extension of C2–C7. To check P-A motion and joint play of any mid- or lower-cervical vertebra, place the pad of your pronated middle finger on the articular pillars of the motion unit being examined (refer to Figure 3.33). With your other hand (the stabilizer), cup the patient's forehead in your palm. Place the patient's neck in full passive extension, using the palpating finger as a fulcrum at each level, and check for additional joint play at the end of each motion by applying a digital push with your contact finger. Also note the separation and closure of the spinous process on P-A and A-P motion. A-P motion is checked in a similar manner as P-A motion except that the pad of the palpating finger is placed against the anterolateral surface of the transverse processes and the patient's neck is flexed. You will have to pull the sternocleidomastoideus slightly back and lateral to make contact. Be gentle, as the tissues are normally tender in this area.
In the cervical spine, flexion and extension occur around a horizontal axis that lies in the body of the vertebra below. For C2, Bergmann locates it in the posteroinferior area of the body of C3 and states that it progressively moves anteriorly and superiorly for each segment caudally.
Anterior Rotation of C2–C7. Areas of P-A rotatory fixation are easily determined except in the individual with extremely heavy neck muscles. In evaluating rotation to the anterior, the palpating finger is slid down the posterolateral aspect of the neck as the patient's neck is passively rotated with the stabilizing hand. The palpation is made with the pad of the pronated middle finger after pushing the sternocleidomastoideus anterior and the upper trapezius backward (refer to Figure 3.30. The palpation is against the posterolateral tissues between the transverse processes or along the apophyses. In checking motion, rotate the patient's head to one side and then to the other, checking for additional joint play at the end of full passive rotation. A firm "bulge" will be evident over the restricted transverse, and this is usually attributed to a hypertonic multifidus or intertransversarii muscle. Palpation in the middle and lower cervical region can be difficult because the palpating finger can be against tender nerves. Because of this, some examiners prefer lamina palpation.
Posterior Rotation of C2–C7. In evaluating rotation to the posterior, the pad of the palpating finger is moved down the anterolateral side of the cervical transverse processes while the neck is rotated posteriorly on the same side by the stabilizing hand on the patient's crown (refer to Figure 3.31). During this palpation, the palpating finger tugs slightly upward and backward to pull the sternocleidomastoideus muscle out of the way. Such palpation must be extremely gentle as the underlying tissues are normally highly sensitive. Avoid contact with the carotid artery.
Simultaneous Extension, Lateral Bending, and Posterior-to-Anterior Rotation of C2–C7. A posterior contact is taken with the pad of the middle or index finger against the articular processes being examined. These fingers are also used as a fulcrum during passive movement of the patient's head to control the level of extension, lateral bending, and rotation. The palpating hand is pronated, and the elbow is raised to the horizontal during this procedure. The stabilizing hand, placed on the forehead or vertex of the patient, extends the patient's neck backward while your palpating finger checks segmental extension motion. With the patient's head still in extension, the neck is rotated first toward one side and then toward the other to check posterior-to-anterior rotation. The patient's head is then returned to the neutral position, the palpating fingers are slid to an adjacent motion unit, and the procedure is repeated. This polymotion procedure should only be used after all standard cervical orthopedic, vertebral artery patency, and thoracic outlet tests have proved negative.
Simultaneous Flexion and Anterior-to-Posterior Rotation of C2–C7. Contact is taken with the pad of the palpating finger against the anterolateral aspect of the transverse processes being examined. This finger is also used as a fulcrum during passive movement of the patient's head to control the level of flexion-rotation. The stabilizing hand, placed on the forehead or vertex of the patient, rolls the patient's head down and forward, tucking in the patient's chin, to check segmental forward flexion. With the patient's head still in forward flexion, the patient's neck is turned toward the side of palpation to check A-P rotation. During this maneuver, the palpating finger must be controlled by bringing it backward and upward, tugging against the sternocleidomastoideus muscle so that it will not hinder the palpation. After a motion unit has been checked, the patient's head is returned to the neutral position, the palpating fingers are slid to an adjacent motion unit, and the procedure is repeated.
Long-Axis Tension (Elongation). To evaluate the degree of distraction available between the facets of the segments of the cervical spine and the adaptability of the IVDs to tensile forces, place the patient in the supine position. Stand or sit facing the head of the table. Take a bilateral index or middle finger contact on the lamina of each segment, one at a time, and apply moderate traction, keeping the patient's neck in the neutral position by avoiding flexion or extension. The patient's skull should be supported by your palms. You should be able to feel a slight separation at each level.
Common Types of Mid- and Lower-Cervical Fixations. The two most common types of fixation in this area, states Faye, are those involving(1) simultaneous extension, lateral bending, and P-A rotation, and
(2) simultaneous flexion and A-P rotation. [See Clinical Comment 3.7]Interspinous fixation. Hypertonicity of one or more extensors tends to bind spinous processes together so that a segmental lordosis is formed. This condition, often found at the C3–C4 level, is palpable when the spinous processes refuse to open during passive flexion. It is also often evident on lateral stress films during forward flexion where two or more vertebrae do not follow the curve of the neck as a whole.
Covertebral articular fixation. Fixation is common at the lips of the joints of Luschka by longus colli hypertonicity, ligamentous shortening, and exostosis. See Figure 3.34. If it is found during passive motions that the patient's neck stops sharply at a point far short of normal motion, Gillet refers to this "brick wall" sign of strong restriction as an indication of cervical osteophytes. This is a classic sign of chronic degeneration found in the cervical joints of the elderly exhibiting a "dry" cervical spine. These fixations often produce chronic brachialgia.
The joints (or fissures) of Luschka (the uncovertebral joints of the cervical spine) are located on the anterolateral surfaces of the vertebral body and act as tracts that guide the motion of coupled rotation and lateral flexion and limit sidebending. These saddle-like joints, states Bergmann, begin development between the ages of 6 and 9 and are complete at 18 years. Whether they are true synovial joints is highly controversial. Gehweiler and associates feel that they represent functional adaptation by the cervical IVDs to the increased mobility of the cervical vertebrae at the time that the uncinate processes are reaching their full height.
However, as these joints are not found in a large percentage of the population, some authorities feel that they are strictly an effect of degeneration.
Compensation in Lumbopelvic Scoliosis. During any type of lumbopelvic distortion where the sacral base has assumed an unnatural position, cervical accommodation normally occurs to maintain the eyes horizontally forward and near the midline. However, because the occipito-atlanto-axial complex allows only slight lateral bending, scoliotic compensation must occur below the axis. If this does not occur in habitually maintaining the axis on the horizontal plane, stress on the dura mater above will be produced. Thus, it can be acknowledged that any problem from above or below that interferes with the role of the axis will produce problems with considerable scope because of the extensive myofascial relationships. For this reason, Dove recommends that the function of the axis be checked in each case where problems manifest in the head, cervical area, upper thoracic area, and shoulder girdle.
Assessing Segmental Mobility Objectively
Physical Mensuration
Gillet's system of measurement has always recognized that there could be possibilities by which hypermobile segments could take up the motion that did not occur in hypomobile motion units. The actual occurrence of this in a particular patient may or may not be true. For those who desire to collect objective data, following are some techniques to show unequal ranges of motions:
1. Lateral bending. The head of a sitting patient is flexed to the side, taking care to prevent the shoulders from following this movement. With the patient in this position, a dot is placed on the tip of the C7 spinous process. A short plumb line is then dropped from the posterior-superior aspect of the ear, and the point where it strikes the shoulder is marked. The same is done during lateral bending to the other side. The distance from these two shoulder points to the midline dot over C7 are then compared to note discrepancies in the ROM of cervical lateral bending.
2. Rotation. Gillet prefers to measure rotation rather than lateral bending because it appears that the influence of hypermobile vertebrae shows up less in this movement. Rotate the head of the sitting patient to the maximum with one hand, taking care that the patient's shoulders do not move from the neutral position. With the patient in this position, drop a short plumb line from the tip of the patient's ipsilateral ear and mark where it strikes the shoulder on a level with the C7. Do the same after rotating the patient's head toward the other side. The distance from these two shoulder points to the midline dot over C7 are then compared to note discrepancies in the ROM of cervical rotation.
3. Extension and flexion. To measure cervical extension, stand to the side of the sitting patient. With your stabilizing hand on the patient's scalp, slowly rotate the patient's head into extension on the neck without disturbing the neutral position of the patient's shoulders. Drop a short plumb line from the back of the patient's ear to the patient's shoulder. Obviously, the greater the degree of backward flexibility, the farther posterior the line will strike the patient's shoulder girdle. In extremely flexible patients, the line may fall posterior to the patient's spine. This same process can be reversed to evaluate cervical flexion.
The above measurements evaluate only gross cervical motion. They do not show specific sites of segmental hypomobility and/or hypermobility. These must be determined by motion palpation and roentgenographic analyses. Such plumb line measurements, however, are helpful in judging the gross effects corrective therapy has on restricted and unstable conditions.
Applied Roentgenography
The Davis series (seven views of the cervical spine) is the standard for assessing the osseous architecture of the cervical spine and to rule out osseous pathology. On the lateral exposures during cervical flexion and extension, considerable information can be gained about intersegmental mobility. Once significant pathology has been ruled out and an evaluation of A-P and P-A function is the remaining objective, immobilization devices should not be used.
Pre- and post-therapy studies using overlays have much merit, and various authors have suggested several methods to gather helpful data. As each vertebra serves as the fundation for the one below, each vertebra becomes the established reference point for the movement of the segment above. Faye advises tracing the vertebral bodies and spinous processes. The neutral spine is traced on clear acetate in black as it appears on the standard Davis lateral view. Once this is done, it can be used to compare flexion and extension ROMs of each motion unit. Jackson's stress lines are another excellent method of demonstrating abnormal flexion and extension arcs.
Roentgenographic Analysis of Cervical Hypolordosis
Rehberger reports the typical radiographic findings to include loss of the normal lordotic curve by the straightened cervical spine (78% cases), anterior and posterior subluxation on flexion and extension views, narrowing of IVD spaces at C4–C6 in 46% cases, discopathy at the affected vertebral level as the injury progresses, and osteoarthritic changes that are often accompanied by foraminal spurring.
In his monograph, Bergmann mentions the radiographic studies of Jochumsen who measured the distance from the anterior body of C5 to a line running from the anterior arch of the atlas to the anterosuperior aspect of the body of C7. He then set up a classification of cervical curves as follows:
1. Hyperlordosis over +9 mm
2. Mean lordosis +3 to +8 mm
3. Hypolordosis +1 to +2 mm
4. Alordosis +1 to -3 mm
5. Kyphosis under -3 mmv
Another approach used by some roentgenologists is to draw one line through the anterior and posterior tubercles of the atlas and another line through the inferior plate of C7. Secondary lines are then drawn at right angles from each of these base lines, and the angle created by the perpendicular lines is measured. From 35°to 40°is considered normal, less than 35°indicates hypolordosis, and an amount greater than 40°is classified as hyperlordosis.
Other methods can also be used. Pettibon states that mechanically the strongest and most resilient curve is an arc which has a radius of curvature equal to the chord across the arc, and he uses the Delmas index as described by Kapandji. As the radius increases, the curve increases (flattens, as in hypolordosis).
Differential Diagnosis
No where else in the spine are the bones, nerves, arteries, and veins so intimately associated as they are in the cervical region.
Tissue Sites of Pain Production
The neck contains an abundance of pain sensitive tissues within a relatively small and compact area of the body. Neck pain may be the result of trauma, irritation, prolonged tension, infection, or degenerative processes. The muscles, ligaments, glandular capsules, vessel walls, and skin of the anterior neck contain networks of nociceptors. Within the spinal complex, pain is primarily elicited from the perivertebral muscles and ligaments, sensory fibers the of nerve root and recurrent meningeal nerve, root dural sleeves and lining of the cord, vascular walls, and apophyseal capsules. Some investigators have traced a few sensory fibers to the posterior aspect of the IVD.
Typical causes of posterior neck pain are shown in Table 3.5.
Neurologic
Traumatic Inflammatory Psychologic Vascular
Compression Abscess Brachial neuritis Angina pectoris
Contusion Dental infection Cervical subluxa- Dissecting aor-
Dislocation Fibrositis tion syndrome tic aneurysm
Fracture Lymphadenitis Multifidi trigger Subarachnoid
Hematoma Meningitis point hemorrhage
IVD syndrome Myalgia Postural subluxa- Temporal arteritis
Subluxation Rheumatoid arth- tion complex
ritis Psychoneurosis
Riedel's struma Scalenus anticus
Trichinosis syndrome
Tuberculosis Sternocleidomas-
toid trigger point
TMJ dysfunction
Trapezius trigger Point
Degenerative
Neoplastic Deficiency Congenital
Carcinoma Cervical spondylosis Branchial cyst
Cyst Osteoarthritis Cervical rib
Hodgkin's disease Pott's disease of Congenital di-
Metastasis bone verticulum
Pancoast tumor Platybasia
Spinal cord tumor Other anomalies
Significant Neurologic and Orthopedic Tests
Evaluating vital signs and such procedures as inspection, static palpation, light touch/pain tests, muscle strength grading, and range of gross motion tests are so standard within chiropractic physical examination that there is no need to describe them here. This is also true for the evaluation of reflexes pertinent to cervical syndromes such as the biceps, ciliospinal, deltoid, infraspinatus, pectoral, radial, scapulohumeral, and triceps reflex. When suspicions arise of possible cranial nerve deficits, facial (VII), glossopharyngeal (IX), hypoglossal (XII), trigeminal (V), and vagus (X) nerve tests are especially pertinent. Besides these standard tests, the following orthopedic and neurologic tests are helpful in the differential diagnosis of cervical syndromes.
Cervical Compression Tests. Two tests are involved. First, with the patient sitting, stand behind the patient. The patient's head is laterally flexed and rotated about 45°toward the side being examined. Interlocked fingers are placed on the patient's scalp and gently pressed caudally. If an IVF is narrowed, this maneuver will further insult the foramen by compressing the disc and further narrowing the foramen, causing radiating pain and reduplication of other symptoms. In the second test, the patient's neck is passively extended and your interlocked fingers are placed on the patient's scalp and gently pressed caudad. If an IVF is narrowed, this maneuver mechanically compromises the foraminal diameters bilaterally and causes radiating pain and reduplication of other symptoms. Pain at the spine only is proably facetal in origin.
Cervical Distraction Test. With the patient sitting, stand to the side of the patient and place one hand under the patient's chin and your other hand under the base of the patient's occiput (Figure 3.35). Slowly and gradually the patient's head is lifted to remove weight from the cervical spine. This maneuver elongates the IVFs, decreases the pressure on the joint capsules around the facet joints, and stretches the perivertebral musculature. If the maneuver decreases pain and relieves other symptoms, it is a likely indication of narrowing of one or more IVFs or cervical facet syndrome. When stretched, spastic perivertebral muscles are painful.
Cervical Active Rotary Compression Test. With the patient sitting, observe while the patient voluntarily laterally flexes the head toward the side being examined. With the neck flexed, the patient is then instructed to rotate the chin toward the same side, which narrows the IVF diameters on the side of concavity. Pain or reduplication of other symptoms suggests a physiologic narrowing of one or more IVFs.
Shoulder Depression Test. With the patient sitting, stand behind the subject and bend the patient's neck laterally away from the side being examined. Stabilize the patient's shoulder with one hand and apply pressure alongside the patient's head with the palm of your other hand; stretching the dural root sleeves and nerve roots or aggravating radicular pain if the nerve roots adhere to the foramina. Extravasations, edema, encroachments, and the conversion of fibrinogen into fibrin may result in interfascicular, foraminal, and articular adhesions and inflammations that will restrict fascicular glide and the ingress and egress of the foraminal contents. Thus, radiating pain and reduplication of other symptoms during this test suggest adhesions between the nerve's dura sleeve and other structures around the IVF.
Swallowing Test. The sitting patient is asked to drink some water. If a pharyngeal lesion is ruled out (eg, tonsillitis), painfully difficult swallowing may suggest a space-occupying lesion at the anterior aspect of the cervical spine (eg, abscess, tumor, osteophytes, etc). See Figure 3.36.
Valsalva's Maneuver. The sitting patient is asked to bear down firmly (abdominal push), as if straining at the stool. This act increases intrathecal pressure, which tends to elicit localized pain in the presence of a space-occupying lesion (eg, IVD protrusion, cord tumor, bony encroachment) or of an acute inflammatory disorder of the cord (eg, arachnoiditis) or possibly the nerve root (radiculitis). Deep coughing will produce the same effect under like circumstances.
Cervical Percussion Test. The neck of the sitting patient is flexed to about 45°while you percuss each of the cervical spinous processes and adjacent superficial soft tissues with a rubber-tipped reflex hammer or the side of a closed fist. Evidence of point tenderness suggests a fractured or acutely subluxated vertebra or localized severe sprain or strain, while symptoms of radicular pain suggest IVF radiculitis or an IVD lesion.
Following are some common tests that are helpful in the differentiation of a thoracic outlet syndrome.
Adson's Test. With the patient sitting or standing, palpate the patient's radial pulse and advise the patient to bend the head obliquely backward toward the side being examined, to take a deep breath, and then to tighten the neck and chest muscles on the side tested. This maneuver decreases the interscalene space and increases any existing compression of the subclavian artery and lower components (C8 and T1) of the brachial plexus against the 1st rib. Marked weakening of the pulse or increased paresthesias is a positive sign of pressure on the neurovascular bundle, particularly of the subclavian artery as it passes between or through the scaleni musculature (Figure 3.37), thus suggesting a probable cervical rib or scalenus anticus syndrome. This test is sometimes called the scalene maneuver.
Allen's Test. The sitting patient elevates the arm and is instructed to make a tight fist to express blood from palm. You should then occlude the radial and ulnar arteries by finger pressure. The patient lowers the hand and relaxes the fist, while you release the arteries one at a time. Some examiners prefer to test the radial and ulnar arteries individually in two tests. The sign is negative if the pale skin of the palm flushes immediately when the artery is released. The patient should be instructed not to hyperextend the palm as this will constrict skin capillaries and render a false positive sign. The sign is positive if the skin of the palm remains blanched for more than 4 seconds. This test, which should be performed before Wright's test, is significant in vascular occlusion of the artery tested.
Eden's Test. With the patient seated, the examiner palpates the radial pulse and instructs the patient to pull the shoulders backward, throw the chest out in a "military posture," and hold a deep inspiration as the pulse is examined. The test is positive if weakening or loss of the pulse occurs, indicating pressure on the neurovascular bundle as it passes between the clavicle and the 1st rib, and thus a costoclavicular syndrome.
Wright's Test. With the patient sitting, palpate the radial pulse from the posterior in the downward position and as the patient's arm is passively moved through an 180°arc. If the pulse diminishes or disappears in this arc or if neurologic symptoms develop, it may indicate pressure on the axillary artery and vein under the pectoralis minor tendon and coracoid process or compression in the retroclavicular spaces between the clavicle and 1st rib, and thus be a hyperabduction syndrome.
Costoclavicular Maneuver. With the patient sitting, stand behind the patient and monitor the patient's radial pulse on the side being examined. Bring the patient's shoulder and arm posterior and then depresses the shoulder on the side being examined. This maneuver narrows the costoclavicular space by approximating the clavicle to the first rib, tending to compress the neurovascular structures between. When the shoulder is retracted, the clavicle moves backward on the sternoclavicular joint and rotates in a counterclockwise direction. An alteration or obliteration of the radial pulse or a reduplication of other symptoms suggests compression of the neurovascular bundle passing between the clavicle and the first rib (costoclavicular syndrome).
In addition to the tests described above, there are occasions when Bradburne's, Branham's, Brudzinski's cheek and neck, Klippel-Weil, and Rust's signs should be sought. This is also true for the application of Bakody's, Bikele's, Kernig's neck, Naffziger's, O'Donoghue's, Ruggeri's reflex, Soto-Hall's, and Spurling's tests. These tests are described in comprehensive texts on physical and differental diagnosis.
Vertebral Artery Deflection
The vertebral arteries are the major source of blood supply to the cervical spinal cord and brain stem, including the medulla oblongata, pons, and midbrain. They also supply the visual cortex of the cerebrum and cerebellum via the basilar artery. For an unexplained reason, one artery is usually smaller than its mate. In visualizing the course and distribution of the vertebral arteries, we should realize that they are captive vessels from C6 upward (Figure 3.38). Severe deflection may be caused by any stretching or twisting of the artery during neck injury or cervical manipulation. In later years, chronic deflection is commonly associated with bony spurs from the covertebral joints or grossly hyperplastic apophyses from arthrosis.
The vertebral arteries are unique in their course through several bony foramina, and in this intermittently channeled course they must make four nearly right-angle turns (forming a half square) in just 20–30 mm between entering the C2 transverse and entering the foramen magnum. Adding to this tortuous course are the anomalous loops that occur in about one in every 5 people. In addition, the C2 area is a common site for aneurysm.
With rotation, C1 moves forward from C2. On the side opposite to which the head is turned, the portion of the artery between the two segments is narrowed and stretched first being affected near 30° rotation and markedly kinked at 45°.
Extension of the cervical spine allows the tip of the superior articular process of the motion unit to glide forward and upward. If sufficient, this motion may cause encroachment on the vertebral artery and/or the IVF. Deflection of the artery and any resulting symptoms are especially exaggerated by rotation plus extension of the neck. As a result of pressure against the artery, there may be temporary lessening in the volume of blood flow. Atheromatous changes may occur later within the vascular wall. The major symptoms include headache, vertigo, nausea, vomiting, nystagmus, and suboccipital tenderness, which may be exaggerated by cervical extension with or without added rotation. Sometimes the symptoms are aggravated by dorsal extension and relieved by forward flexion with cervical traction.
Vertebral-Basilar Artery Insufficiency Syndrome
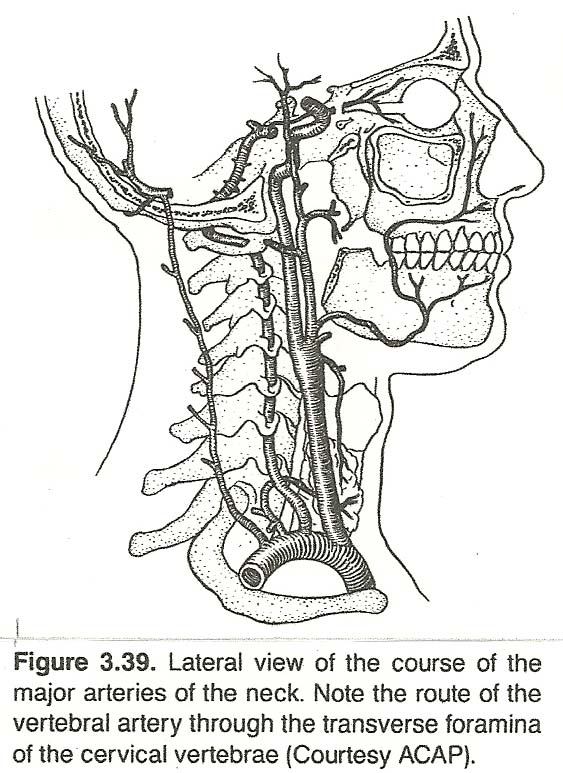 |
The vertebral arteries also exhibit special features for particular sites of predilection for degeneration by the change of fixed and unfixed vessel parts, increased vulnerability to bone and muscle movements, and the occlusion of peripheral arteries in their circulation area by difficult to diagnose pathologic changes of the vascular walls. See Figure 3.39. These factors suggest the probability of advanced degenerative or inflammatory process. Trauma to the vertebral artery has even been reported after emergency resuscitation procedures where passive extension of the neck is necessary to insert an airtube.
Because cervical rotation may approach 47°or more, the vertebral artery can easily be stretched and twisted to the point of occlusion. Thus, the integrity of the vertebral arteries should always be evaluated before cervical manipulation or mobilization. Youth is no exception to this rule. It is often young patients that experience transient ischemic attacks or a serious vascular accident after misapplied cervical manipulation.
Symptoms can usually be attributed to involvement of the plexus around the vertebral artery or intermittent disruption of the blood flow. Any compromise (eg, compression, atherosclerosis, thrombosis, vasospasm, kinking, longus colli and scalenus anticus spasm) producing an insufficiency of blood flow can lead to a singular symptom or a wide number of seemingly unrelated cranial manifestations such as occipital headaches, memory lapses, dizziness, tinnitus, nausea and vomiting, lightheadedness or syncope, intermittent blurred vision, suboccipital tenderness, and, sometimes, retro-occular pain (episodic), speech impairment, extremity paresthesia and weakness, drop attacks, and gait defects all of which can be generally grouped under the title of Barr-Lieou syndrome, especially when cervical trauma and an underlying spondylosis are involved. These signs and symptoms, which sometimes fluctuate from side to side, can mimic a posttraumatic syndrome, multiple sclerosis, amyotrophic lateral sclerosis, or a tumor within the posterior fossa.
Severe interference (eg, advanced atherosclerosis, osteophytic kinking, spondylotic foraminal impingement, or extension effects of IVD degeneration) leads to involvement of the nucleus ambiguous of the vagus (eg, dysphagia, ipsilateral palatal weakness), descending root and nucleus of cranial V (ipsilateral facial hypesthesia, especially around the lips), descending sympathetic fibers (Horner's syndrome), vestibular nuclei (rotary nystagmus), midbrain and cerebellum (ipsilateral arm/leg malcoordination, intention tremor, ataxia), spinothalamic tract (contralateral hypesthesia), and the effects from impaired venous drainage and CSF flow, which is often referred to as Wallenberg's syndrome.
It can be projected that the many cranial-oriented symptoms that have been relieved by chiropractic adjustments to the cervical region can be attributed to normalization of vertebral artery blood flow. Here we have a clinical paradox in that the same treatment may cause possible distress if unusual precautions are not taken with some patients.
Several clinical tests that have only minor variations are portrayed in the literature. The six most commonly used are Barr-Lieou's, George's, Hautant's, Maigne's, DeKleyn's, and Unterberger's tests.
Barr-Lieou Test. The sitting patient is asked to slowly but firmly rotate the head first to one side and then to the other. Transient mechanical occlusion of the vertebral artery may be precipitated by this simple turning of the head, and this phenomenon is attributed to the compressive action of the longus colli and scalene muscles (Figure 3.40) on the vertebral artery, just before coursing through the IVF of C6. A positive sign is exhibited if dizziness, faintness, nausea, nystagmus, vertigo, and/or visual blurring result suggesting buckling, torsion, or compression of the vertebral artery. This mild test should be used before any others because if it is positive, there is no need to apply greater stress.
George's Tests. With the patient sitting, blood pressure and the radial pulse rate are taken bilaterally and recorded. Stenosis or occlusion of the subclavian artery is suggested when a difference of 10 mm Hg between the two systolic blood pressures and a feeble or absent pulse is found on the involved side. Even if these signs are absent, a subclavian deficit may be exhibited by finding auscultated bruits in the supraclavicular fossa.
Hautant's Test. Place the sitting patient's upper limbs so that they are abducted forward with the palms supinated. The patient is instructed to close the eyes while you extend and rotate the patient's head. This position is held between 20–30 seconds on each side. A positive sign is for one or both arms to drop into a pronated position.
Maigne's Test. Place the sitting patient's neck in extension and contralateral rotation. This position is held for about 30–60 seconds on each side. A positive sign is shown by nystagmus or symptoms of vertebrobasilar ischemia. In this and DeKleyn's test, unusual care must be exercised as each of these tests is designed to stress the vertebral arteries, which may be weakened.
DeKleyn's Test. Place the patient supine with the head rest lowered a few notches. Extend and rotate the patient's head, and hold this position for about 15–30 seconds on each side. A positive sign is the same as that in Maigne's test. Faye recommends that the position be held for 45–60 seconds and that it must be held long enough to cause brain ischemia owing to loss of patency of an arterial deficit (eg, compression, atherosclerosis, kink, etc).
Underburger's Test. Ask the patient to stand with the upper limbs out-stretched, the eyes closed, and then to march in place with the head extended and rotated. The examiner should stand close to the patient during the test because a positive sign is a loss of balance. For this reason, it is not one of the most commonly used.
Other signs that help to determine a patient at risk include arteriosclerotic optic fundi changes, a subclavian or carotid bruit, positive Doppler ultrasound tracings, and positive roentgenographic changes.
Headaches of Cervical Origin: General Considerations
Markovich, the renowned neurologist, found that the most common headache is the type caused by neuromuscular skeletal imbalance. He points out that "the head in the human species has changed its position from the quadruped to the erect, thereby changing the basic relationship between the cervical spine and the head, with its important functional structures, and the rest of the body." He calls attention to the delicate interaction and highly sensitive biofeedback or servo-mechanisms that continually make adjustments in body balance, vision, and hearing with head and neck posture. "These regulatory, homeostatic mechanisms can be disturbed by a variety of conditions, originating at any level, including the inflammation and/or irritation of the cephalic projection of the upper cervical nerves (cervico-occipital neuralgias)."
Abnormal contraction of the muscles at the occipitocervical area appears to generate a type of "ischemic irritation" that includes the entrapment of the C2 nerves (greater and lesser occipital) as they pierce the thick muscle and ascend to the back of the head. Differentiation of various types of headaches is shown in Table 3.6, adapted from Markovich's findings. However, keep in mind that a patient may not exhibit such a clear picture. For example, vascular migraine may be superimposed on occipitocervical neuralgia or episodes may be interposed, depending on the causes involved.
| Symptom/Sign | Occipito-cervical Neuralgia | Trigeminal Neuralgia | Vascular Migraine | Temporo-mandibular Traction |
| Pain | Throbbing, paroxysmal | Excruciating, paroxysmal | Severe, paroxysmal | Severe, dull |
| Quality | Muscle spasms | Stabbing | Throbbing | Dull ache |
| Location | Occipital | Facial | Unilateral | Facial |
| Aura | None | None | Visual | None |
| Duration | Days | Brief | Hours | Chronic |
| Associated symptoms and signs | Earache, Eye pain, Neck pain, Paresthesias, Anxiety, Tinnitus, Nausea | Trigger zones | Vomiting, Photophobia, Irritability | Bruxism, Malocclusion, Earache, Joint clicks |
Localized headaches may point to causative subluxations. Pioneer chiropractic was specific in relating certain types of headache with to specific spinal areas. Firth, then president of Lincoln Chiropractic College, taught that: "A headache located in the forehead or over the eyes (frontal or eye headache) is often caused by a local subluxation in the upper or middle cervical region. A headache located in the region of the temples (temporal headache) is usually caused by a subluxation in the region of T4. A headache in the back of the head (occipital headache) may be caused by an atlas or axis subluxation, but it is more frequently caused by a lumbar subluxation. A vertigo or sick headache may be the result and symptom of gastric indigestion that is frequently relieved by an adjustment in the T6 T8 region. A headache at the crown of the head is more rarely encountered than any of the others and frequently indicates kidney trouble. It can often be relieved by an adjustment to the T10–T12 region. Such subluxations may be primary subluxations or in compensation to a structural fault elsewhere in the spine or a reflex from a distant part."
Kraus states: "It has been my experience that the most common cause of headaches originates in the 'vicious circle' generated by the abnormal and painful contraction of the cervical-nuchal muscles, mainly the trapezius muscle. These contractions generate a type of 'ischemic irritation' that includes the entrapment of the second cervical nerves (greater occipital and lesser occipital) as they travel through the bulk of the muscle, ascending into the back of the head to innervate the posterior scalp region, temporal areas, and lobes of the ears, and sending terminal branches into the angle of the jaw, back of the eye, and vertex of the head. This creates a distinct clinical syndrome that is easily confused with atypical 'vascular migraine' because of the unilaterality of the symptoms and frequent complaints of pain in the back of the eye with or without visual disturbance."
Kraus goes on to say that the second common entity is the TMJ pain dysfunction syndrome that has been proven to be more common than many expect and has many protean manifestations to the extent that it has become known as The Great Imposter. "The fact that a cervical nerve irritation can create a painful condition in the angle of the jaw or in the temple explains the possible common 'irritative' source of both syndromes." [See Clinical Comment 3.8]
True Migraine
With any type of vascular headache (migraine, cluster, hypertension), a patient will feel more relief in the upright position. The recumbent position is more beneficial to patients with sinusitis and tension headaches. In addition, vascular headaches are commonly associated with a prodromal aura (usually visual) that is thought to be the result of an initial arterial spasm and local ischemia in the area affected. In females, attacks are more frequent just before the onset of menstruation.
In true migraine headaches, there is an initial vasoconstriction (amine release) that produces prodromal neurologic symptoms (eg, visual aura, motor or sensory perversions) in 10% of the cases from the ischemia, which initiates a period of vasodilation (vasoactive substance release) that, in turn, produces the headache. The initial site of pain is usually orbital, frontal, or temporal; unilateral and localized; and then radiates to the parietal and occipital areas. The side of the headache may at one time occur on the left and the next time on the right. Bilateral types, however, are not rare. An attack may last several days, but the typical attack lasts less than 24 hours. Bouts of a throbbing headache arise in late adolescence or early adult life. They are more common in females and frequently associated with a family tendency, but some type of stress usually precipitates an attack. They usually first occur before adulthood.
Prodromal neurologic manifestations (usually accentuated contralaterally) such as amblyopia, hemianopsia, hemiparesis, numbness, ophthalmoplegia, paresthesia, speech disturbances, and weakness may or may not be associated. Listlessness, social withdrawal, dejection, nausea and vomiting, and anorexia are frequently related. Scintilating scotomata are commonly associated with migraine but rarely with other types of chronic headaches. Birth control pills (attributed to the periodic withdrawal of exogenous progestogens) and excessive noise and/or light increase the pain and number of attacks. Attacks usually reduce in severity and rate during pregnancy. [See Clinical Comment 3.9]
Cervical Migraine
The generally accepted etiology of cervical migraine is upper-cervical angiospasm of the vertebral artery.
As with true migraine, cervical migraine may be preceded by an aura. Neurologic examination during a pain-free interval reveals nothing pertinent except a tender spot in the upper neck over the site where the occipital nerve pierces the aponeurosis of the upper neck muscles. See Figure 3.41.
According to Faye and associates, if the occipital nerve is cut, the pain of cervical migraine may be stopped. However, sometimes the pain may persist, suggesting that it can be elicited from any segmental level of the cervical spine. An even more puzzling observation is that cervical migraine is often relieved when a cervical rib producing brachialgia is removed. This might indicate a vertebral artery or sympathetic involvement.
Cervical migraine may be suspected if the headache is always localized on the same side during every attack. A history of cervical trauma is also important. Seek signs of cervical dysfunction. In cervical migraine, it has been Schafer's experience that the site of involvement will usually be in the C4– C6 area. Pressure over and around the spinous processes may elicit extreme tenderness. Cervical motions in various directions may start an attack, especially if the positions are held for 30– 60 seconds.
Cluster Headaches
In cluster migraine (Horton's histamine cephalgia), the intense pain is unilateral. It may have an evening onset, but more commonly it awakens the patient after a few hours of sleep. The paroxysmal and localized pain begins initially in the temporal-supraorbital area and progresses to the occipital area, or the opposite may appear: occiput to temple.
Attacks, which are invariably associated with adult males, are more common in the spring and fall, thus making an allergic or hormonal reaction a possible precipitating factor. A familial tendency is rarely involved. The pain may be so intense that suicide is contemplated. It usually lasts 30– 90 minutes but may continue for several hours, reappearing in clusters that last from a day or two to several months, then it may remiss for several years. In both cluster and migraine headaches, severe bouts of pain are interspersed with pain-free episodes lasting several months. The reason for this pattern is
not clear.
Nasal stuffiness, flush, injected conjunctiva, and other ipsilateral signs of vasodilation may be found. Rhinorrhea, profuse lacrimation, tenderness of the carotid arteries, and pupillary constriction commonly manifest. In addition, cluster headaches are frequently found associated with "silent" peptic ulcers, in which the duration of severe pain may be extended to several hours. Such conditions are frequently aggravated by huge consumption of aspirin to relieve the pain but increase the gastritis that is producing the reflex mechanism. The patient will often report that everything is tried to gain relief, but nothing appears to help until the pain runs its course. Medication of any type, even morphine, has little effect; yet treatment to the hidden gastrointestinal fault will show immediate relief within a few days. It has been Schafer's experience that an occipitoatlantal fixation is usually involved in cluster headaches.
Occipital Neuralgia
Occipital neuralgia is caused by involvement of the greater and lesser occipital nerves, the greater nerve being affected with more frequency. These nerves are derived from the C2 and C3 segments of the spinal cord.
Typical occipital neuralgia displays paroxysms of pain provoked by movement of the head, suggesting that the nerve roots are under the influence of some type of mechanical pressure or irritation. The patient complains of pain in the back of the head and behind the ear. At time, the pain is strictly occipital, unilateral or bilateral. Sometimes it radiates toward the mandible. The character of the pain varies from a dull aching soreness to a sharp shooting pain. Turning the head often increases the pain, and brushing the hair is annoying because of an hyperesthetic scalp. Attacks may arise with short-intervals of relief or the pain may be continuous.
Examination usually reveals a tender point, which aids the diagnosis, that is located:
(1) midway between the tip of the mastoid and the atlas (greater occipital nerve),
(2) at a point behind the mastoid, or
(3) between the insertion of the sternocleidomastoideus muscle and that of the trapezius muscle.
Vascular Tension Headache
Tension headaches, which frequently have an emotional base (eg, stress, anxiety, depression), are rarely present on arising but increase in severity as the day progresses and stress accumulates. The onset is typically gradual and may last from hours to months without relief. Attacks, which may be unilateral or bilateral, may occur daily or be constant for several days and then not recur for several weeks or months (similar to cluster headaches). Facial pain and cheek paresthesias and/or a sense of pressure behind an eyeball may be associated. Tension headaches must be differentiated from the referred pain of sinus disease, which may manifest in the occipital area, especially if the maxillary or sphenoid sinuses are involved.
Examination usually reveals suboccipital tenderness at a point midway between the tip of the mastoid and the midcervical vertebrae. Firm pressure on this tender point may sometimes ease the pain referred to the temple, face, or eyeball. Palpation or percussion of a temporal artery may reveal abnormal unilateral tenderness. This must be differentiated from arteritis.
Two types of tension headaches are reported: the "hat-band" type and the occipital type:
1. In the "hat-band" type with a history of a constriction feeling around the circumference of the scalp, the cause can usually be found in a history of emotional stress. Symptoms of chronic anxiety or depression and unusual fatigue may also be associated.
2. The occipital type exhibits severe contraction in the muscles of the neck and scalp that can be palpated and demonstrated in electromyography. The pain is typically bilateral or general, with radiation over the entire cranium and sometimes down the neck into a shoulder. Cervical stiffness, tension, and tingling in the occipitoparietal region are commonly associated. Trigger points can often be found in the suboccipital area and other cervical muscles. Anxiety symptoms and hyperactive deep reflexes are usually associated. The occipitoatlantal joint is inevitably hypomobile, suggesting a motion-unit fixation. During suboccipital spasm, the nerves in the area are vulnerable to irritation from C1 or C2 subluxations. Passive upper-cervical stretching reproduces the pain and possibly the paresthesia, and palpation of the area elicits deep tenderness.
Differential Diagnosis
Besides a pathologic intracranial lesion, facial pain may have its origin in a fixation-subluxation of the occiput or in the upper cervical spine. The pain may be referred to any or all distributions of the 5th cranial nerve so that, in some instances, it suggests tic douloureux. Some of the characteristic signs of trigeminal neuraglia, however, are absent. For example, the paroxysmal peripheral projection of pain is not present, and, in trigeminal neuralgia, the pain is described as being in the skin, gums, or tongue. In atypical facial neuralgia, the pain may be continuous. The history may reveal that the attack was preceded by some type of physical or emotional stress. It may be associated with true migraine, and an associated tender point is often identical to that found in occipital neuralgia. Spinal examination usually elicits extreme tenderness over the articular processes of C2 and C3. An adjustment on this side is usually successful. Particularly seek signs of impaired flexion and A-P rotation motion, advises Faye.
Interscapulovertebral Pain Syndrome
Faye and associates have found that about 70% of common posterior upper thoracic pain is of lower cervical origin, is predominant in the interscapular region, and has a higher incidence in women. It is usually localized between the scapula and the spine, almost always unilateral, and radiates at times to the lateral (sometimes superior) border of the scapula. It may give the patient the impression of being deep seated, internal, or feel as a weighty, burning, or painful tension between the scapulae. Sharp pain may occur within 3-4 hours after working or it may arise a few minutes after the patient begins work. In other cases, it is episodic and elicited by faulty movement such as extremely abducting the arm backward.
The history will usually trace the cause to:
(1) occupations during which the hands are used at the level of where the elbows are not supported;
(2) domestic activities such as ironing, cleaning, sewing, or carrying heavy packages; or
(3) wearing a heavy overcoat, especially during prolonged standing, which may precipitate symptoms. Sometimes the pain occurs only at night, depending upon the position of the head on a pillow, the height and firmness of the pillow, and the side on which the patient habitually rests.
The presence of a positive anterior cervical "doorbell sign" (described later in this chapter) confirms the origin of the upper thoracic pain. A moderate pressure maintained for 2 or 3 seconds reproduces the pain of the patient's complaint. Palpation also reveals the presence of a fixed tender point that is invariably found about 2 cm lateral to the spinous processes of T5 or T6. This interscapular point is extremely tender. When pressure is applied, it also reproduces the pain that formed the basis of the patient's complaint. This tender point is over the site where the posterior branch of T2 emerges. The medial ramus becomes superficial at the T5 level, and from there it fans out horizontally to supply a large area of skin on the back. The fact that the posterior branch of T2 may be responsible for the pain does not explain why the cervical doorbell sign is positive. However, close study will show that there are anastomoses between the lower cervical and upper thoracic nerves. Also, T2 is an important segment as far as the cervical sympathetic nerves are concerned.
Posterior Nerve Branch Syndrome
The posterior rami of the spinal nerves innervate all the formations dependent on the posterior vertebral arch. Their motor distribution is in the muscles acting on the axial skeleton, and their segmental sensory distribution covers a large area of skin that extends without interruption from the vertex to the coccyx. Their role in the rich innervation of the posterior articulations of the spine is not well known. These nerve branches closely adhere to the articular structures, being fixed by fibrous attachments, and are affected by acute or chronic derangements of the posterior joints. In chronic fixations, there is pericapsular fibrosis of the posterior apophyses and marginal osteophytosis that may irritate the nerve root. See Figure 3.42.
The posterior branches of a spinal nerve can be injured or inflamed near the IVF. When this occurs, the pain is limited to the perivertebral region and relatively localized. The pain may often be elicited by movements that especially slide the posterior articulations (eg, rotation). Perivertebral spasm, usually pronounced, is another consequence of irritation of a posterior ramus. When prolonged, such complications as torticollis or other deformities arise.
Lower Cervical Radicular Syndrome
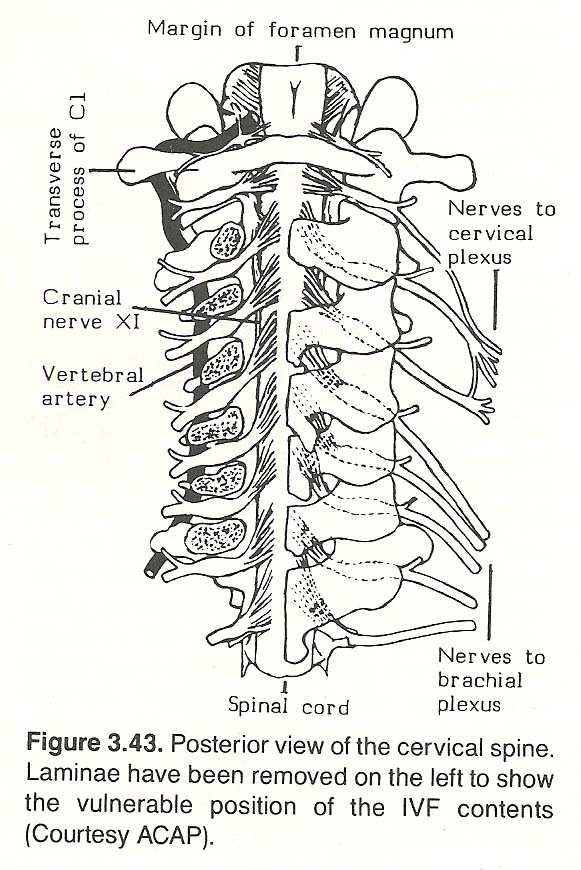 |
This neuralgia features pain along the upper extremity from cervical nerve root compression or irritation (C5 C8). Either mechanical and/or inflammatory etiologies may be involved. See Figure 3.43. Pain constitutes almost the entire symptomatology. It may involve the entire dermatome supplied by the root or be isolated to a smaller area such as the shoulder, elbow, or wrist. The patient almost always complains of simultaneous interscapular pain, which often precedes the radicular symptoms. It is usually increased when the patent is in bed and alleviated by certain movements such as placing a hand behind the head. In this position, the roots of the brachial plexus are relaxed.
An anterior doorbell sign is usually found. This sign contributes to the segmental localization and reveals the cervical origin of the symptoms. Keep in mind, however, the possibility that interspinal ligament pain and tenderness may alone be responsible for lower neck pain or pain referred to the posterior aspect of the shoulder or arm. In such cases, the anterior cervical doorbell will be absent.
After a thorough motion palpation examination, multidirectional pressure applied to the spinous process of the involved segment can help to analyze more precisely the level of the intervertebral block. When lateral pressure is applied, a counterpressure should be applied to the adjacent inferior spinous process. The related findings contribute to the determination of the most appropriate adjustive technic. Faye advises his students to remember that the major fixation is often above or below the level of radicular neuropathy. Other objective physical findings are present in only half the cases. For example, reflex changes are not often found, and motor changes are found in still fewer cases.
Anterior Doorbell Sign. The examiner faces the sitting patient. Mild pressure is applied over the emerging ventral roots of the cervical spine at the anterolateral aspect of the neck, under the sternocleidomastoideus muscle. Contact is made with the thumbs held horizontally. A positive sign is the reproduction or exaggeration of patient symptoms (eg, upper-extremity pain, paresthesia).
Adjustive Considerations. Manipulation is effective in many cases of cervical radiculitis. In the hyperalgesic forms in which neck movements are absent, one should not manipulate the cervical spine until palliative procedures have produced some substantial degree of pain-free motion. At times, adjustments are effective in the T3 T5 area when fixations, spontaneous pain, and point tenderness are located there. Pressure in this area may elicit brachial pain. In such cases, the pain does not show a typical radicular distribution; it resembles a sympathetic disturbance. Conversely, many interscapular neuralgias are improved by adjustments of the lower cervicals if fixated. After signs of inflammation and symptoms subside, reports Faye, gentle adjustments at the symptom level clears up the postinflammatory fixations.
Cervical IVD Syndrome
According to Grieve, the clinical picture of cervical disc disorders is typically a combination of "a hard osseocartilaginous spur, produced by the disc together with the adjacent margins of the vertebral bodies." Furthermore, "the mechanism by which pain and disability originate in the neck region," contends Cailliet, "can be considered broadly to result from encroachment of space or faulty movement in the region of the neck through which the nerves or blood vessels pass." This encroachment of space or faulty movement commonly comprise apophyseal subluxation with osteophyte formation, contributing to, or superimposed upon disc degeneration and/or protrusion. This occurs most frequently in the C4 C6 area. When a cervical disc protrusion is toward the posterior, Lhermitte's test will be positive.
Lhermitte's Test. With the patient seated, flexing the patient's neck and hips simultaneously with the patient's knees in full extension may produce sharp pain or shock-like sensations radiating down the spine and/or into the upper extremities. When this is elicited, it is a sign of cervical pathology suggesting spinal cord myelopathy by a protruded cervical disc, tumor, fracture, or multiple sclerosis.
The discs below C3 exhibit a higher incidence and the greatest severity of herniation. The C5 disc is the most frequently involved, followed by the C6 disc. The C2 disc is the least frequently involved of any in the neck.
The specific neurovascular manifestations of acute cervical disc herniation are:
C2 disc protrusion (C3 nerve root level):
posterior neck numbness and pain radiating to the mastoid and ear. The reflexes test normal.
C3 disc protrusion (C4 nerve root level):
posterior neck numbness and pain radiating along the levator scapulae muscle and sometimes to the pectorals. The reflexes test normal.
C4 disc protrusion (C5 nerve root level):
lateral neck, shoulder, and arm pain and paresthesia, deltoid weakness and possible atrophy, hypesthesia of C5 root distribution
over middle deltoid area (axillary nerve distribution). The reflexes test normal.
C5 disc protrusion (C6 nerve root level):
pain radiating down the lateral arm and forearm into the thumb and index finger, hypesthesia of the lateral forearm and thumb,
decreased biceps reflex, biceps and supinator weakness.
C6 disc protrusion (C7 nerve root level):
pain radiating down the middle forearm to the middle fingers, hypesthesia of the middle fingers, decreased triceps
and radial reflexes, triceps and grip weakness.
C7 disc protrusion (C8 nerve root level):
possible pain radiating down the medial forearm and hand, ulnar hypesthesia, intrinsic muscle weakness of the hand.
However, these symptoms are uncommon. The reflexes test normal.
The above symptoms vary depending on the direction of the disc bulge; eg, on the nerve root, IVF vessels, spinal cord, or combinations of involvement. In some acute and many chronic cases, peripheral numbness may manifest without pain. In some cervical disc herniations, the features may be confused with those of shoulder or elbow bursitis, epicondylitis, or subluxation, especially when no local cervical symptoms exist.
To repeat for emphasis, no where else in the spine are the structures as vulnerable to the effects of a poorly controlled adjustment than in the cervical region. Because of the possibility of a subclinical vertebral artery lesion, an adjustment with a shallow depth is a must in the cervical spine. We need only to open a joint less than an eighth of an inch to obtain an audible release of a fixation.
(1) the chronic state of the articular and periarticular soft tissues requires time to adapt to the renewed mobility, and
In rare occurrences, it may be found that the amount of correction achieved during the initial adjustment was so slight that the fixation returned to its state of total fixation within a few days. If this occurs, consideration should be given to using a more efficient technic. On this point, Faye states that the technic should utilize more than one adjustive thrust into a motion unit. "Often three or more specific thrusts are necessary to release a total fixation in all its directions of fixation."
Patient Supine. Place the patient supine on an adjusting table with the head-piece level with the floor. Stand at the head of the table, facing the patient. Turn the patient's head so that the fixation is upward and the contralateral side of the occiput can be cradled within your stabilizing hand. The middle finger of this hand should firmly contact the rim of the patient's occiput. Shift your position slightly so that it will be more lateral to the patient. With your active hand, apply a pisiform contact on the rim of the occiput on the side of fixation, fingers pointing toward the patient's vertex. Widen your stance for stability, raise the patient's head to slightly laterally bend the occipitoatlantal area, shift your body weight slightly forward from the patient to apply axial traction, and then deliver a quick shallow distracting impulse to just separate the locked occipitoatlantal joint. See Figure 3.45. This same procedure can be adapted to the patient in the prone position (Figure 3.46).
Another common technic applied with the patient in the prone position and the head turned so that the site of fixation is upward is to take a double knife-edge contact: one under the patient's occipital rim and the other just above the patient's vertebra prominens (viz, C7 or T1 spinous process). Your fingers will be entwined, and your hands will be placed in somewhat of a pyramidal design. In this position, apply opposing forces for long-axis cervical elongation (by opening the pyramidal base of your hands), then add a short distracting impulse (by dropping body weight slightly) at the end of resistance.
Patient Supine. Although active rotation of the occiput on the atlas is usually slight in degree, there should be distinct end play. If not, all other motions of the condyles will be affected. To correct this restriction, place the patient supine with the head level (Figure 3.48). Turn the patient's head so that the fixated side is upward. Stand at the head of the table facing the patient, and place your stabilizing under the patient's head. Apply a light thumb contact anteriorly against the patient's zygomatic arch and a firm index finger contact posteriorly against the rim of the occiput. Avoid pressure against the patient's ear. Slowly rotate the patient's head a little farther with your stabilizing hand until firm resistance is felt, then deliver a short quick dynamic impulse to further this rotation.
With slight modification, an occipital anterior rotation on the atlas fixation can be corrected by applying the technic described above on the contralateral side.
Patient Supine. Place the patient supine with the head-piece of the adjusting table level with the floor. Stand at the head of the table, obliquely facing the patient on the side of fixation. Rotate the patient's head so that the side of fixation is upward. Reach under the patient's head, and cup the patient's ear with your stabilizing hand. Bend forward over the patient, and with your active hand, apply an index finger or pisiform contact on the posterior arch of the atlas. Slowly rotate the patient's head farther with your stabilizing hand until firm resistance is felt, then add a short dynamic rotatory impulse with your active hand. This adjustment is delivered with the whole body, not just the contact point.
Atlantal Lateral Flexion on Axis Fixation
Patient Supine. If a lateral bending fixation is found between the atlas and axis, place the patient supine, stand at the head of the table and face the patient, turn the patient's head away from the side of fixation, and place your stabilizing hand under the patient's head. With your active hand, apply a pisiform contact on either the tip of the transverse process or the posterior arch, with your little finger extended along the ramus of the patient's jaw. Lift upward with your stabilizing hand to slightly laterally flex the upper cervical area. Apply counterpressure with your contact hand, and, when firm resistance is felt, add a short dynamic impulse to increase the lateral flexion (Figure 3.49).
Atlantal Anterior Rotation on Axis Fixation
Patient Supine. Stand at the head of the table facing the patient. Turn the patient's head toward the side of fixation. With your contact hand, cup the patient's atlas in the web of your active hand so that the tip of your index finger can contact the anterior aspect of the transverse process of the patient's atlas on the side of fixation. The patient's occiput will be supported by your palm. Cup the patient's uppermost ear with your stabilizing hand. Increase the rotation of the patient's head against the fixation with your stabilizing hand. Once firm resistance is obtained, apply traction with your stabilizing hand and deliver an impulse against the fixation by rotating the atlas posteriorly on the side of fixation with your contact fingers (Figure 3.50). It should be noted that during this adjustment the active hand also laterally flexes toward the stabilizing hand.
Adjusting Middle and Lower Cervical Fixations
Patient Supine. The patient is placed face up on the adjusting table, with the head-piece of the table level or up a notch. Stand at the head of the table facing the patient. Your stabilizing hand should support the patient's head and turn it away from the side of fixation. With your contact hand, push the trapezius laterally and take contact on the lamina or articular process of the involved segment, using either an index finger contact (straight or crooked) or a pisiform contact. Shift your weight slightly to the side of fixation, increase the rotation of the patient's neck to firm resistance, and deliver a short quick impulse directed along the plane of articulation to mobilize the blocked P-A motion (Figure 3.51).
An alternative technic is the classic cervical rotatory adjustment with the patient in the prone position. Stand on the same side as the fixation, turn the patient's face away from the side of fixation, so that the involved side will be facing the floor. Take contact on the lamina of the involved segment with the side of your index finger, elbow almost perpendicular to the patient's neck, and stabilize the patient's occiput by placing the heel of your stabilizing hand on the patient's temporal area above the ear. Remove any tissue slack under your contact finger, apply slight traction with your stabilizing hand, and deliver a short quick impulse with your contact hand against the blocked P-A motion of the segment.
Patient Supine. With the patient facing the ceiling and the head-piece of the table level or dropped a notch, stand at the head of the table and face the patient. Support the patient's head on the opposite side of the fixation with the fingers and palm of your stabilizing hand. With your active hand, place an index finger contact on the lamina of the superior segment of the involved motion unit. Raise both hands a little so that the patient's head will roll backward slightly and the cervical spine will be placed into extension. Your elbows will be low and pointing obliquely to the floor. Take up any tissue slack under your contact finger, and when firm resistance is felt, apply a short quick impulse with your contact finger that is directed anteriorly (upward) and slightly medial to release the extension block. The slight medial direction is added only to avoid contact slippage.
Anterior Rotation Fixations: C3–C7
Patient Supine. Position the patient face up on an adjusting table with the head-piece level. Stand at the head of the table and face the patient. Lift the patient's occiput with your stabilizing hand so that you can reach under the back of the patient's neck and apply a web contact with your active hand around the posterior aspect of the superior segment of the involved motion unit. The tip of your active index or middle finger should be on the anterolateral aspect of the segment's transverse process. Once firm contact is made, place the palm or heel of your stabilizing hand against the patient's ipsilateral temporal area, and rotate the patient's face away from the side of fixation. Remove all tissue slack under your active finger by adding mild counterpressure with your stabilizing hand. The adjustment is made by simultaneously pulling your active contact so that the segment will rotate from the anterior to the posterior while your stabilizing hand applies some tensile force.
Long-Axis Elongation Fixations: C3–C7
Vague autonomic symptoms may also be exhibited such as dizziness, blurred vision, and hearing difficulties. These can usually be attributed to a complicating involvement of the sympathetic plexus around the vertebral artery or intermittent disruption of the blood flow of the vertebral artery. Horner's syndrome (ptosis, meiosis, hypohidrosis) often occurs in diseases affecting the cervical cord. According to Faye, autonomic symptoms also occur when flexion and A-P cervical rotation fixations stress the sympathetic ganglion chain.
Shoulder-Hand Syndrome
This reflex dystrophy is often referred to as Steinbrocker's syndrome. It is a condition that simulates many of the common lesions about the shoulder joint and often erroneously diagnosed as periarthritis, bursitis, tendinitis, or frozen shoulder.
The signs and symptoms that involve the shoulder and hand include pain, swelling, stiffness, restricted motion, trophic changes of the soft tissues, and osteoporosis in some cases. It may start with a burning causalgic-type pain in the shoulder joint, followed by joint stiffness and trophic changes. The first sign in the hand may be stiffness and swelling of the fingers, with an inability to close the fist. The palmar fascia may contract. In its early stages, it resembles bursitis, neuritis, or any of the so-called rheumatic conditions that affect the shoulder.
Steinbrocker's syndrome is usually an aftermath of trauma or disease involving the upper-extremity, neck, or cranium.
Symptoms may not appear for days, weeks, or even months following the cause. It is also common following myocardial vascular damage. Regardless, the condition is regarded as a motor and neurovascular symptom complex that primarily affects the upper extremity.
Various etiologic theories have been proposed, but none have been widely confirmed. One again, advises Faye, pay close attention to the flexion and A-P rotation cervical fixations.
One widely held theory states that the reflex starts from an area of local tissue disturbance. Impulses from these areas travel centrally along the usual afferent pathways and enter the internuncial system of spinal cord neurons, which is an interconnected and widely ramified network of CNS nerve fibers. In shoulder-hand syndrome, the noxious impulses apparently set up a central disturbance in the nature of a widespread continuous agitation of the internuncial pool. Impulses spread steadily to fire the anterior and lateral horn cells, which are not ordinarily affected by afferent impulses from the periphery. This incessant stimulation is expressed peripherally by motor and neurovascular symptoms. Spasm and vasomotor imbalance result and produce the characteristic clinical features of the shoulder-hand syndrome.
A variety of seemingly unrelated clinical disturbances have been described for many years as separate entities. These disorders include causalgia, Sudeck's atrophy, posttraumatic osteoporosis, painful shoulder disability following coronary occlusion, postinfarctional sclerodactylia, palmar and digital contractures, the swollen atrophic hands associated with cervical osteoarthritis, and certain changes in the limbs of hemiplegics. Increasing evidence suggests that, although the etiology of these various syndromes may be different, many of their clinical characteristics, and probably the neurophysiologic mechanisms underlying their development, are extremely similar if not identical.
THERAPEUTIC APPROACH
Before making a proper adjustment, the doctor must be well armed with a sound knowledge of anatomy, pathophysiology, and be able to visualize the tissues involved and the plane of articulation of the segment(s) to be mobilized. This is true for all articulations to assure that the correction is made most efficiently and with the least discomfort to the patient. Faye recommends that the DC administer an impulse at the point of lock, into the fixation, assures adequate velocity with minimal amplitude.
Adaptability to Partial Mobility
For reasons not fully explained, Gillet only adjusts total fixations in the upper cervical area. He rarely adjusts partial fixations. One reason he gives is because they are so easily relieved spontaneously by the correction of more caudad total fixations. When it is deemed beneficial to adjust an upper-cervical partial fixation, a rotatory-type adjustment is preferred by Schafer because he believes that a recoil-type thrust is usually too traumatic on muscular fixations in this area, tending to enhance the fixed state at a later date because of the superimposed irritation. Gillet mentions that the rotary technic in such cases is one of his favorites. Faye states that it is important to adjust into the direction of each restricted direction of motion.
It is rarely possible to produce an immediate complete correction in a chronic upper-cervical total fixation because:
(2) the six occipitoatlantal muscles are especially affected by conditions more caudad in the spine. The fixation will either normalize itself after release, little by little, as the articulations are used or be encouraged to do so when the remainder of spinal fixations are mobilized.
Adjusting Occipitoatlantal Articular Fixations
The most important total fixation found in the spine appears to be at the occipitoatlantal articulations. In adjusting a total occipitoatlantal fixation, Gillet applies a forward thrust (P A) on the readily palpable posterior arch of the atlas while holding a firm contact just posterior to the lateral masses. This places the contact point on the largest and strongest aspect of the atlas.
An occipital lift, taught by Faye, is also an extremely effective technic for releasing total occipitoatlantal fixations and jammed facets (Figure 3.44).
Occipital Lift
Patient Sitting. Stand directly behind the sitting patient. The patient should be sitting erect, with the feet flat against the floor, and exhibiting the normal sitting lumbar lordosis. Take a moderately wide stance for stability. Rotate the patient's head away from the side of fixation. Reach around in front of the patient with your active hand, and apply a contact with your middle finger under the rim of the occiput, posterior to the mastoid process. Your index finger and thumb should avoid contact with the patient's ear. Reach around the other side of the patient with your stabilizing hand, and place it over your active hand for reinforcement. Bend over slightly and flex your knees so that the patient's skull can be firmed against your sternum. Your shoulders should be parallel with the patient's shoulders. With these contacts held firm, lean forward slightly more to produce a few degrees of lateral flexion of the patient's upper cervical spine and straighten your knees slightly to apply a slight vertical lift (distraction). At the end of resistance, apply a short dynamic impulse directed upward to separate the occipital condyle from the atlas. The thrust is delivered simultaneously with your contact hands and torso, assisted by quickly extending your knees (Figure 3.47). Take care not to apply any pressure against the patient's mandible. If a bilateral fixation has been found, reverse the procedure for the contralateral side.
Patient Prone. Place the patient prone on an adjusting table with the head-piece lowered about 15°. Rotate the patient's head away from you so that the side of fixation is upward. Apply a knife edge contact with the medial edge of your active hand on the rim of the occiput, and grasp your active wrist with your stabilizing hand. Slowly apply pressure to the point of firm resistance, and deliver an impulse thrust directed forward against the occiput.
Occipital Posterior Rotation on Atlas Fixation
Adjusting Atlantoaxial Fixations
Atlantal Posterior Rotation on Axis Fixation
Patient Sitting. If a posterior rotation fixation between the atlas and axis is found on the right, for example, stand behind the patient and turn the patient's head away from the side of fixation. The patient should be sitting erect, with the feet flat on the floor. Take contact on the right posterior arch of the patient's atlas with your supinated right index finger, other fingers pointing slightly downward and your palm cupping the patient's right ear. Cup your stabilizing hand over the patient's left ear, and just slightly extend the patient's neck. Avoid lateral flexion. Slowly rotate the patient's head a little farther, and shift your position so that it follows the back of the patient's head. Once firm resistance is felt, add a short dynamic impulse to continue the rotation.
Patient Prone. With the patient positioned face down on the adjusting table, stand on the side of involvement. Bend down so that you can apply a thumb contact against the posterior arch of the atlas. Reinforce this contact with the thumb of your stabilizing hand. Apply pressure horizontally. Your fingers will be extended over the back of the patient's neck, and your arms should be almost parallel to the floor. Increased contact pressure until firm resistance is felt, then add a short dynamic recoil-type of impulse by extending your elbows. This is an excellent technic to use with the elderly when a lateral fixation exists and there is mild suspicion of but no overt signs of vertebral artery insufficiency.
Patient Sitting. This fixation is usually attended by a degree of flexion fixation. Stand facing the sitting patient, oblique to the side of fixation. The stabilizing hand cradles the patient's head firmly enough to apply a slight degree of distraction. Slide the pisiform of your active hand up the angle of the scalenus anticus attachments until it contacts the anterior aspect of the transverse process of the patient's atlas. Slightly lift, rotate, and tilt the patient's upper cervical area with both hands to produce tension of the scaleni attachments. When firm resistance is felt, add a quick dynamic impulse with your pisiform that will produce a short anterior-to-posterior movement of the atlas on the axis. A variation of this technic is to use a thumb contact rather than a pisiform contact.
Posterior Rotation Fixations: C3–C7
Patient Sitting. Stand directly behind the sitting patient. Locate the fixed processes with the thumb of your contact hand by sliding the trapezius laterally, then take contact with your index finger, palm supinated. Your stabilizing hand should be supporting the contralateral side of the patient's neck at the same level as your active contact. Rotate the patient's head away from the side of fixation, let the neck extend slightly, and shift your weight slightly to the side of contact. Take up the tissue slack with your contact, rotate the neck a little farther until firm resistance is felt, and deliver a short quick impulse against the blocked articulation (Figure 3.52). Your line of drive should be alone the plane of the articulation, designed to release the blocked P-A motion.
An alternative technic is a slight variation on the classic rotatory adjustment with the patient in the sitting position. Stand at the side of the patient, contralateral to the side of the fixation. Reach around in front of the patient with your contact hand so that your middle finger can firmly grip the lamina of the involved segment on the side of fixation. Pronate the palm of your stabilizing hand, and raise the elbow high so that you can grasp your fingers around the rim of the patient's occiput on the contralateral side of the fixation. Rotate the patient's face away from the side of fixation, take up any tissue slack under your contact finger, increase the rotation to firm resistance, and give a short quick impulse with your contact hand along the plane of articulation to release the blocked P-A motion (Figure 3.53). It often helps if both the contact hand and the stabilizing hand simultaneously apply a slight vertical distraction pull during the adjustment.
Patient Prone. Place the patient face down on the adjusting table with the head-piece level. Stand on the side of fixation, facing perpendicular to the patient. Take contact on the involved articular process with your thumb, fingers relaxed horizontally over the back of the patient's neck. Place your stabilizing thumb over your contact thumb in a like manner for reinforcement. Shift your weight so that it is centered over the patient, relax your elbows, take up the tissue slack under your contact thumb, and deliver a short quick recoil-type impulse by quickly adducting your elbows. The line of drive should be towards the floor and slightly headward to be in line with the plane of articulation.
Lateral Bending Fixations: C3–C7
The suggested technics used for releasing lateral bending fixations are similar to those described above for posterior rotation fixations with the major exception that the line of drive is directed perpendicularly against the block processes rather than directed to rotate the superior segment of the involved motion unit anteriorly (Figure 3.54).
Extension Fixations: C3–C7
Patient Sitting. Stand directly behind the sitting patient, supinate the palm of your active hand and place an index finger contact over the inferior articulating process of the fixated process. Your stabilizing hand should support the patient's neck in a similar manner and be positioned at the same level. Keep the patient's head near your sternum for good control. Shift your body weight slightly to the side of fixation, extend and slightly distract the patient's neck with both hands to a point of firm resistance, and administer a short quick impulse directed anterosuperiorly against the extension block (Figure 3.55).
Patient Prone. Position the patient face down. The head-piece can be either level or raised a notch or two. Stand at the head of the table, obliquely facing the patient, on the side opposite the fixation. With your active hand, make contact on the lamina of the superior segment of the involved motion unit with your index finger so that the thumb of this hand can be placed on the contralateral lamina. Place your stabilizing hand upon your active hand for reinforcement. Shift your torso over your hands, relax your elbows, but increase pressure until firm resistance is felt. The adjustment is made by delivering a short recoil-type of impulse by quickly adducting your elbows. The line of drive is downward (anteriorly) and slightly cephalad to mobilize the extension block.
An alternative technic with the patient supine is to apply contact on the anterolateral aspect of the involved transverse process with the side of the index finger of your active ipsilateral hand. Turn the patient's face away from the side of fixation, and countersupport the patient's head or neck with your stabilizing hand. The correction is made by delivering an anterior-to-posterior impulse with your contact finger.
Patient Sitting. With the patient sitting, stand directly behind. Support the patient's neck contralaterally with your stabilizing hand and make contact with the side of your active hand's supinated index finger on the anterolateral aspect of the transverse process of the superior segment of the involved motion unit. Shift your weight slightly toward the side of fixation, laterally bend the patient's head toward the side of fixation (over your active contact finger), and apply slight extension of the patient's neck with both hands. Apply A-P motion until firm resistance is felt, and then administer a short quick rotatory anterior-to-posterior impulse with your active finger against the anterior rotation block, while lifting upward with your stabilizing hand to add some traction to open the facets.
After all cervical flexion-extension, rotation, and lateral bending fixations have been mobilized, check the integrity of motion-unit distraction. Restriction here sometimes remains after all other corrections have been made. To make this correction, assume the same doctor-patient positions as used during long-axis elongation palpation (Figure 3.56). If no or distinctly subnormal separation is felt between certain segments during traction, hold the traction and apply a short quick mild additional long-axis pull (a faint release should be palpable or heard), and sustain mild traction for several seconds to allow for tissue adaptation. Release the tension slowly. The prior traction before the correcting stretch is important to avoid tearing some tissue. Never "snap" the spine. This is often an extremely effective maneuver, but gentleness, the utmost of control, and sound clinical judgment are necessary in its application.
Adjusting Muscular Fixations in the Cervical Spine
Some major biomechanical effects of cervical hypertonicity are shown in Table 3.7. Should the practitioner wish to adjust muscle fixations in the cervical spine rather than allowing them to correct themselves spontaneously by relieving primary fixations found elsewhere, Gillet offers the following comments.
Table 3.7. Selected Effects of Cervical Area Hypertonicity
| Muscle | Effect of Prolonged Hypertonicity |
| Interspinales | Excessive muscle tone between the spinous processes tends to hyperextend the motion unit. |
| Obliquus capitis inferior | Increased tone tends to produce a rotary torque of the atlas-axis motion unit. |
| Obliquus capitis superior | Contraction tends to roll the occiput anterior and inferior and pull the atlas posterior and superior to produce a lateral occiput tilt and condyle jamming. |
| Rectus capitis posterior major | Hypertonicity tends to pull the occiput posterior, inferior, and medial and the spinous of the axis superior, lateral, and anterior. Strong hypertonicity will lock the occiput and axis together so that they appear to act as one unit even though they are not contiguous. |
| Scalenus anterior | Contraction tends to pull the C3-C6 transverse processes inferior, lateral, and anterior and the 1st rib superior and medial. |
| Scalenus medius | Excessive tone tends to pull the C1-C7 transverse processes inferior, lateral, and anterior and the 1st rib superior and medial. |
| Scalenus posterior | Hypertonicity tends to pull the C4-C6 transverse processes inferior, lateral, and anterior and the 2nd rib superior and medial. |
| Splenius capitis | Increased tone tends to pull the C5-T3 spinous processes lateral, superior, and anterior and to subluxate the occiput inferior, medial, and posterior. |
| Sternocleidomastoideus | Contraction tends to pull the sternum and clavicle posterior and superior and the occiput inferior and anterior. |
| Upper trapezius | Hypertonicity tends to pull the occiput posteroinferior, the C7-T5 spinous processes lateral, and the shoulder girdle medial and superior. |
Bailey RW:
The Cervical Spine.
Philadelphia, Lea & Febiger, 1974, pp 91-97.
Bard G, and Jones M:
Cineradiographic recording of traction of the cervical spine.
Archives of Physical Medicine and Rehabilitation, August 1964.
Bergmann T:
Integrated chiropractic methods.
Oklahoma seminar, April 23, 1983, NWCC, pp 8 12.
Bovee ML:
The Essentials of the Orthopedic & Neurological Examination.
Place of publication not shown, published by author, 1977, p 7.
Brodin H:
Cervical pain and mobilization.
Manuelle Medizin, 20:90-94, 1982.
Cailliet R:
Neck and Arm Pain.
Philadelphia, F.A. Davis, 1974, p 37.
Cailliet R:
Soft Tissue Pain and Disability.
Philadelphia, F.A. Davis, 1980, pp 61, 107-124, 128-130, 135-140, 142-148.
Chusid JG:
Correlative Neuroanatomy & Functional Neurology, ed 19.
Los Altos, CA, Lange Medical, pp 68, 297.
Craton EF:
Cranial vertebral junction autopsy.
Today's Chiropractic, pp 29-30. September-October 1985.
De Rusha JL:
Upper cervical technic correlated with neurodiagnosis.
ACA Journal of Chiropractic, September 1961.
Dimnet J, Pasquet A, Krag MH, Panjabi MM:
Cervical spine motion in the sagittal plane: Kinematic and geometric parameters.
Journal of Biomechanics, 15:959-969, 1982.
Dove CI:
The occipito-atlanto-axial complex.
Manuelle Medizin, 20:11-15, 1982.
Duckworth JAW:
Dissection seminar conducted at the Canadian Chiropractic Memorial College.
Toronto, CMCC, 1983.
Dvorak J, Orelli FV:
How dangerous is manipulation of the cervical spine? Case report and results of an inquiry.
Manuelle Medizin, 20:44-48, 1982.
Epstein BS: The Spine:
A Radiological Text and Atlas.
Philadelphia, Lea & Febiger, 1962, pp 268-269.
Faye LJ, et al:
Spine II: Motion Palpation and Clinical Considerations of the Cervical and Thoracic Spine.
Huntington Beach, CA, Motion Palpation Institute, 1986, pp 1-2, 4-9, 12-15, 18-21, 24-41.
Faye LJ:
Motion Palpation and Manipulation of the Lower Cervicals [Videotape].
Dynaspine, Inc, 10780 Santa Monica Blvd, Suite 400, Los Angeles, CA 90025.
Faye LJ:
Motion Palpation and Manipulation of the Upper Cervicals [Videotape].
Dynaspine, Inc, 10780 Santa Monica Blvd, Suite 400, Los Angeles, CA 90025.
Faye LJ:
Motion Palpation: Spine 2, Cervicals and Thoracics [Cassette tape program].
Huntington Beach, CA, Motion Palpation Institute, 1986, 6 tapes.
Felding JW, Francis WR, Hawkins RJ:
The upper cervical spine.
In Feldman F (ed): Radiology, Pathology, and Immunology of Bones and Joints: A Review of Current Concepts,
New York, Appleton-Century-Crofts, 1978, pp 303-312.
Fisk JW:
The Painful Neck and Back. Springfield, IL,
Charles C. Thomas, 1977, pp 28-37.
Gehweiler JA Jr, Osborne RL Jr, Becker RF:
The Radiology of Vertebrae Trauma.
Philadelphia, W.B. Saunders, 1980, p 74.
Gemmell HA:
Biomechanics and function examination of the cervical spine.
Journal of the Chiropractic Association of Oklahoma, 6(2):12-13, Spring 1988.
George AW:
A method for more accurate study of injuries to the atlas and axis.
ACA Journal of Chiropractic, pp 41-51, December 1983.
George PE:
New techniques to identify the potential stroke victim.
International Review of Chiropractic, p 23, January/March 1981.
Gillet H, Liekens M:
Belgian Chiropractic Research Notes. Huntington Beach, CA,
Motion Palpation Institute, 1984, pp 5-7, 19-20, 27-28, 38-43, 70-71, 107-108, 142-144.
Gillet H:
Normal and abnormal cervical mobility.
Bulletin of the European Chiropractic Union, 28(4):47-49, 1980.
Gillet H:
Occiput-atlas-axis fixation.
Journal of Clinical Chiropractic, 1(12): 30-33, 1976.
Glerak RA:
Vertebral artery compression and vascular insufficiency of the brain.
Archives of California Chiropractic Association, 2:28-39, 1972.
Goodheart GL:
Collected Published Articles and Reprints.
Montpellier, OH, Williams County Publishing, 1969, pp 15, 59-60, 65.
Gregory R:
Biomechanics of the upper cervical spine.
The Digest of Chiropractic Economics, September/October 1983.
Grice AS:
A biomechanical approach to cervical and dorsal adjusting.
In Haldeman S (ed): Modern Developments in the Principles and Practice of Chiropractic.
New York, Appleton-Century-Crofts, 1980, pp 331-349.
Grieve GP:
Common Vertebral Joint Problems. London,
Churchill Livingstone, 1981, pp 41, 125-134, 312-314, 319-324.
Grove AB:
Chiropractic Technique A Procedure of Adjusting.
Madison, WI, Straus Printing & Publishing, 1979, p 40.
Hadler NM:
Medical Management of the Regional Musculoskeletal Diseases.
New York, Grune & Stratton, 1984, pp 123-126.
Hadley LA:
Anatomico-Roentgenographic Studies of the Spine.
Springfield, IL, Charles C. Thomas, 1981, pp 160-162.
Henderson DJ:
Significance of vertebral dyskinesia in relation to the cervical syndrome.
Journal of Manipulative and Physiological Therapeutics, 2:1, 1979.
Herbst RW:
Gonstead Chiropractic Science and Art.
Sci-Chi Publishers. Other publication data not shown.
Hohl M, Baker HR:
The atlantoaxial joint, roentgenographic and anatomical study of normal and abnormal motion.
Journal of Bone & Joint Surgery, 46A:1739, 1964.
Jackson R:
The Cervical Syndrome, ed 4.
Springfield, IL, Charles C. Thomas, 1978.
Jeffreys E:
Disorders of the Cervical Spine.
Boston, Butterworths, 1980, pp 2-14.
Jirout J:
Changes in the atlas-axis relations on lateral flexion of the head and neck.
Neuroradiology, 6:215, 1973.
Johnston WL, Hill JL:
Spinal segmental dysfunction: incidence in the cervico-thoracic region.
Journal of the American Osteopathic Association, 81:67-76, September 1981.
Johnston WL, Vorro J, Hubbard RP:
Clinical/biomechanic correlates for cervical function: part I, a kinematic study.
Journal of the American Osteopathic Association, 85(7):429-436, July 1985.
Kapandji IA:
Physiology of the Joints: The Trunk and Vertebral Column, ed 2.
New York, Churchill Livingstone, 1980, vol three, pp 20-21, 154, 172-244.
Kale M:
The upper cervical specific.
Today's Chiropractic, part 1, pp 28-29, July/August 1984; part 2, pp 27-30, September/October 1984.
Keggi, Granger, Southwick:
Vertebral artery insufficiency secondary to trauma and osteoarthritis of the cervical spine. Yale Journal of Biology and Medicine, 38:471-478, 1966.
Kos J: The cervical spine.
Toronto, Canadian Memorial Chiropractic College, CMCC continuing education program.
Kraus H:
Muscular aspects of oral dysfunction.
In Gelb H (ed): Clinical Management of Head, Neck and TMJ Pain and Dysfunction.
Philadelphia, W.B. Saunders, 1977, pp 117-124.
Lombardi G:
The occipital vertebra.
American Journal of Roentgenology, 86:260, 1961.
Lysell E:
Motion in the cervical spine.
Acta Orthopaedia Scandinavia (Supplement), 123:1, 1969,
Macnab I:
Symptoms in cervical disc degeneration. In The Cervical Spine Research Society: The Cervical Spine.
Philadelphia, Lippincott, 1983, pp 388-394.
Mapstone T, Spetzler RF:
Vertebrobasilar insufficiency secondary to vertebral artery occlusion.
Journal of Neurosurgery, 56:581-583, 1982.
Markovich SE:
Painful neuro-muscular dysfunction syndromes in the head: a neurologist's view.
Paper presented to the American Academy of CranioMandibular Orthopedics Meeting, New Orleans, September 1976.
Markovich SE:
Pain in the head: A neurological appraisal.
In Gelb H (ed): Clinical Management of Head, Neck and TMJ Pain and Dysfunction.
Philadelphia, W.B. Saunders, 1977, pp 125-139.
McRae DL:
The significance of abnormalities of the cervical spine.
American Journal of Roentgenology, 84:3, 1960.
Mertz JA:
Videofluoroscopy of the cervical and lumbar spine.
ACA Journal of Chiropractic, pp 74-75, August 1981.
Meyermann R:
Possibilities of injury to the artery vertebralis.
Manuelle Medizin, 20:105-114, 1982.
Mumenthaler M:
Neurology, ed 2. Translated by EH Burrows.
New York, Thieme-Stratton, 1983, pp 157-158.
Murphy C, Rankin I, Jones BE, Jayson MIV:
Continuous recording of neck rotation: preliminary observations.
Spine, 9:657-658, 1984.
Nash CL, Moe JH:
A study of vertebral rotation.
Journal of Bone & Joint Surgery, 51:223, 1969.
Nelson JM:
Conservative approaches to the management of thoracic outlet syndrome.
In Coyle BA, Martinez DP (eds): Proceedings of the Second Conference on Current Topics in Chiropractic: Reviews of the Literature; May 4-5, 1985.
Sunnyvale, CA, Palmer College of Chiropractic West, 1985, section B1.
Ng SY:
The relationship between atlas deposition and cervical curvature.
ACA Journal of Chiropractic, 13:79-83, September 1979.
Ng SY:
Upper cervical vertebrae and occipital headache.
Journal of Manipulative and Physiological Therapeutics, 3 (3):137-141, September 1980.
Pettibon Bio-Mechanics Institute:
Pettibon Spinal Bio-Mechanics: Theory and Implications, ed 2.
Vancouver, WA, Pettibon BioMechanics, 1976, pp 44-46, 94-99.
Phillips RB:
Upper cervical biomechanics.
ACA Journal of Chiropractic, October 1976.
Rehberger LP:
Reversal of the normal cervical curve. Roentgenological Briefs,
Council on Roentgenology of the American Chiropractic Association, Des Moines, IA, date not shown.
Reid JD:
Effects of flexion-extension movements of the head and spine upon the spinal cord and nerve roots.
Journal of Neurology, Neurosurgery and Psychiatry (British), 23:214. 1960.
Reinert OC:
Anatomical characteristics of subluxation: C2 through C7.
ACA Journal of Chiropractic, pp 62-69, May 1984.
Rude J:
Morphology of the occipital condyles and movement of the atlanto-occipital joint.
Manuelle Medizin, 22:101-106, 1984.
Sandoz R:
A classification of luxation, subluxation and fixation of the cervical spine.
Annals of the Swiss Chiropractors Association, 6:219-276, 1976.
Saternus KS, Fuchs V:
Is the artery vertebralis endangered in resuscitation.
Manuelle Medizin, 20:101-104, 1982.
Schafer RC:
Chiropractic Management of Sports and Recreational Injuries.
Baltimore, Williams & Wilkins, 1982, pp 331, 340-341, 357.
Schafer RC:
Chiropractic Physical and Spinal Diagnosis.
Oklahoma City, American Chiropractic Academic Press, 1980, pp VI:24-26, VIII:9-32.
Schafer RC:
Clinical Biomechanics: Musculoskeletal Actions and Reactions.
Baltimore, Williams & Wilkins, 1983, pp 175, 177, 183, 184-186, 194, 264-271, 279-285.
Schafer RC:
Physical examination of the TMJ, posterior neck, and cervical spine.
In Schafer RC: Physical Diagnosis: Procedures and Methodology in Chiropractic Practice.
Arlington, VA, American Chiropractic Association. Scheduled to be released in 1988. Chapter 15.
Schafer RC:
Symptomatology and Differential Diagnosis.
Arlington, VA, American Chiropractic Association, 1986, pp 228, 455, 552-555, 569-570.
Schmorl G, Junghanns H:
The Human Spine in Health and Disease.
New York, Grune & Stratton, 1971.
Sheehan S, Bauer RB, Meyer JS:
Vertebral artery compression in cervical spondylosis, arteriographic demonstration during life of vertebral artery insufficiency due to rotation and extension of the neck.
Neurology, 10:968-986, 1960.
Smith DM:
Vertebral artery. Roentgenological Briefs.
Council on Roentgenology of the American Chiropractic Association, date and number not shown.
Snijders CJ,
Timmerman P: Motions and forces in the atlanto-occipital joint during flexion of the cervical spine.
Manuelle Medizin, 20:51-58, 1982.
Stonebrink RD:
Palpation for vertebral motoricity.
ACA Journal of Chiropractic, III:S11-14, February 1969.
Sutherland S:
Anatomical perivertebral influences on the intervertebral foramen.
In Goldstein M (ed): The Research Status of Spinal Manipulative Therapy, NINCDS Monograph No. 15, DHEW Publication No. (NIH) 76-998, Stock No. 017-049-0-0060-7,
Washington, DC, U.S. Government Printing Office, 1975.
Sweat RW:
Scanning palpation: cervical spine.
Today's Chiropractic, pp 23-24, January/February 1985.
Sweat RW, Sievert T:
Chiropractic and the vertebral arteries.
Today's Chiropractic, part 1, pp 45-48, September/October 1984; part 2, pp 23-24, Novem=- ber/December 1984.
Telford ED, Mottershead S:
Pressure at the cervical brachial junction: an operative and anatomical study.
Journal of Bone & Joint Surgery, 30B:249-250, 1948.
Toole J, Tucker SH:
Influence of head position upon cerebral circulation.
Archives of Neurology (AMA), 2:616-623, 1960.
VonTorklus D, Gehle W:
The Upper Cervical Spine.
New York, Grune & Stratton, 1972, p 22.
West HG:
Vertebral artery considerations in cervical trauma.
ACA Journal of Chiropractic, pp 18-19, December 1968.
White AA, Panjabi MM:
Clinical Biomechanics of the Spine.
Philadelphia, J.B. Lippincott, 1978, pp 65-74, 82-87, 123-166, 183-184, 196-218, 235, 271, 294-296.