

|
Chapter 1
Introduction To the Dynamic Chiropractic Paradigm
From R. C. Schafer, DC, PhD, FICC's best-selling book:
“Motion Palpation”
Second Edition ~ The Motion Palpation Institute & ACAPress
The following materials are provided as a service to our profession. There is no charge for individuals to copy and file these materials. However, they cannot be sold or used in any group or commercial venture without written permission from ACAPress.
All of Dr. Schafer's books are now available on CDs, with all proceeds being donated
to chiropractic research. Please review the complete list of available books.
Overview of the Dynamic Chiropractic Approach Introduction to Fixation Terminology Dr Henri Gillet's Fixation Theory Effects of Common Trauma Joint Play and Its Restrictions Normal Movements of Spinal Articulations The Planes of the Body and Related Considerations Structural Motion Motion Barriers and Their Significance in Manipulation The Different Types of Fixations Muscular (Class I) Fixations Ligamentous (Class II) Fixations Articular (Class III) Fixations Bony Restrictions Adaptive Therapy Significant Physiologic and Biomechanical Mechanisms The Mechanisms of Equilibrium The Mechanisms of Irritation Potential Effects of the Summation of Irritation Differentiating Joint Dysfunction from Joint Disease Practicing the Modern Subluxation Complex Paradigm Pertinent Biomechanical Terminology Movement Terms Arthrokinematic Terms Notation Symbols Used in Motion Palpation Fundamentals of Chiropractic Adjustment Technics Background Different Types of Adjustive Technics Low-Velocity Technics (LVTs) High-Velocity Technics (HVTs) Indirect (Functional) Approches Different Types of Adjustive Thrusts Different Approaches to Adjusting Bibliography
This chapter presents an overview of the background and basic concepts of
Dynamic Chiropractic. The normal motions of spinal and related articulations,
general considerations of spinal fixations, the different types of fixations,
the significant physiologic mechanisms associated, a comparison of traditional
and modern definitions of the vertebral subluxation complex, and other basic
concepts are summarized. Facts of Position. It was determined that a subluxated vertebra has not
"slipped out of place." It is not displaced from its physiologic boundary, nor
has it exceeded its normal limits of motion. Thus, when a "subluxation" is
adjusted, it is not really replaced, relocated, or reduced in the same context
as would be a complete or partial dislocation for it is usually "freed" to
function normally (made mobile).
Facts of Movements. Vertebral movements describe an arc around a center
of motion, from one extreme to the other. It was found that the basic movements of spinal segments are rotation about the longitudinal axis, lateral
flexion (side bending, tipping) toward the right or left, posterior-anterior
flexion, anterior-posterior extension, and long-axis distention. Factors may
arise that can inhibit movement within any one or more of these directions,
setting up a state of abnormal biomechanical translation and rotation leading
to biomechanical and subsequent physiologic dysfunction.
(1) if a subluxation (a malfunction less than that produced by a dislocation)
exists, a fixation also exists, and
Although this holding mechanism is commonly called a fixation, this term
too can be the cause of confusion if it infers a state of complete immobility.
In this text, the term fixation is used in its traditional sense in motion
palpation referring to any physical, functional, or psychic mechanism that
produces a loss of segmental mobility within its normal physiologic range of
motion. Thus, ankylosis would be considered a fixation in its purest sense
a 100% fixation. However, most fixations found clinically will be far less
(eg, in the 20%–80% range of normal mobility).
(1) the superior and inferior posterior articular facets constantly glide on one another, establishing a barrage of complex proprioceptive signals to higher central nervous system (CNS) centers;
This dynamic action is also thought to
help "milk" cerebrospinal fluid both around the spinal cord and peripherally
along the spinal nerves. Normally, these dynamic compressing and stretching
actions only occur for a few seconds at each event of movement and only within
physiologic limits. These momentary actions, which can be likened to mild
massage, should not be confused with prolonged or severe compressing and
stretching actions.
(1) overworked tissues (eg, unaccustomed activity of chopping wood or shoveling),
The basic direction of case management can be considered as progressing
through two phases. The first goal is to reduce the swelling and relieve the
associated pain and soreness by R-I-C-E (rest, ice, compression, and elevation) and other physiotherapeutic measures when appropriate. The second
objective is to promote healing and movement (eg, by manipulation, massage,
stretching, passive and active exercise, and other standard regimens. It is
also imperative to relieve any attending neurologic disorder in the spine, as
this often cuts the reflex feedback cycle that facilitates prolonging the
effect and also eliminates a possible source of a secondary or contributing
subluxation complex.
1. Total joint movement is the voluntary range of movement plus or minus
the joint play present.
DR. FAYE'S CLINICAL COMMENT #1.1
The pain experienced by the patient when joint play is restricted is sharp and only lasts as long as the doctor presses into the restriction during
the examination. This must not be confused with the joint pain associated with an inflamed joint that produces a lingering type of pain when challenged.
Many basic considerations in biomechanics involve time, mass, center of
mass, movement, force, and gravity which operate in accordance with the laws
of physics. However, while numerous parameters of movement are interrelated,
no one factor is capable of completely describing movement by itself.
(1) flexion/extension rotation is rotation about the X axis,
All Z points in front of the X-Y plane are positive, while those behind
are negative (Fig. 1.2). By using X, Y, and Z coordinates, any point in space
can be located and depicted. However, a minimum of six coordinates is necessary to specify the position of a rigid body (eg, a vertebra).
Chapter 1: Introduction to the Dynamic Chiropractic Paradigm
Overview of the Dynamic Chiropractic Approach
In 1936, a small group of Belgium chiropractors began what was to be a
long research project. Its aim was to study what chiropractors refer to as a
subluxation, which is traditionally defined as an incomplete dislocation, a
displacement in which the articular surfaces have not lost contact, or a partially reduced (spontaneously) dislocation.
Outstanding within the Belgium group were Drs. H. Gillet and M. Liekens.
These investigators, who have been involved in this study for more than half a
century, soon found that the clinical phenomenon of subluxation was a great
deal more complicated than the effects of the oversimplified picture of "a
bone out of place" that has been commonly proposed since the turn of the century. Their findings reported in the Belgium Research Notes are a testimony to
their skillful observations. Although the theory of "a displaced vertebra"
contained enough truth within it to constitute a basic therapeutic approach
that could be justified by large numbers of positive benefits witnessed
empirically, it was not sufficient to serve as a scientific hypothesis.
This investigative group did not have the advantage of any but personal
funding and their own office facilities, it was decided to concentrate their
studies on the normal and abnormal mobility of articular segments, especially
those of the vertebral column and pelvis. As the findings of their investigations were reported, some basic assumptions of the profession were confirmed
and others had to be discarded in light of the new knowledge obtained. For
example, it was found that two basic concepts withstood the assault of the
knowledge obtained year after year. These concepts involved vertebral position
and motion:
Introduction to Fixation Terminology
The design of the spinal column's bony processes and its ligaments tend to
stop the zygapophyses from exceeding their inherent range of motion. When this
range is exceeded (eg, severe trauma, predisposing gross pathology), the
articular surfaces lose contact and are in a state of dislocation.
Bones Do Not Subluxate
A single vertebra cannot become subluxated or fixated. Only an articulation can subluxate or become fixated. As fixation-subluxations occur between two normally articulating surfaces, we speak about adjusting or mobilizing
vertebral motion units (two apposing vertebral segments), not a single vertebra. Thus, articulations subluxate, not bones.
The Perpetuation of a Misnomer
A state of "subluxation," in the surgical sense of the word, is difficult
to achieve in gliding joints, and all zygapophyseal joints are gliding in
nature. This is said to be one reason given why chiropractic theory has had
such a difficult time being accepted by the general scientific community. It
is thus paradoxical that the term subluxation, in the chiropractic sense, has
forced its presence on all the health-care professions and is becoming widely
used in circles beyond the chiropractic profession, while at the same time
chiropractors have begun to understand that the term is a misnomer when all
its pathophysiologic components are considered. For example, a vertebra may be
in a hypomobile state of "fixation," unilaterally or bilaterally, that is well
within its normal range of motion during the resting position yet be considered an articular aberration that can cause or contribute to many pathologic
expressions.
Articular Fixation Defined
For an articulation to remain in an abnormal state of "subluxation," something must be holding it there to restrict its mobility otherwise it would
spontaneously reduce itself and produce little clinical concern. This "holding" or "mobility hindrance" mechanism is commonly called a "fixation." Thus,
(2) a fixation can exist even when the
articular surfaces are in an ideal relationship during the static resting
posture.
Dr. Henri Gillet's Fixation Theory
The ability of a doctor of chiropractic to detect restricted articular
motion or hypermobility may mean the difference between success and failure
with many patients. The study of motion palpation offers the examining physician far greater insight and confidence in why, where, when, how, and how
often to administer appropriate therapy especially a corrective adjustment.
In evaluating the state of the periarticular and intra-articular soft tissues (eg, muscles, ligaments, capsules, synovia, articular cartilages)
involved in an articular fixation, it will generally be found that it is some
abnormal state of these soft tissues that is preventing the articular surfaces
from moving in a particular plane. Common examples are muscle spasm and fibrosis, ligament shortening, intra-articular adhesions, scar development, cartilage hardening and malformation, cartilaginous chips and fragmented loose
bodies, and cartilage erosion that restrict motion. Subsequent bone erosion
and exostoses may also be involved. Osteopaths established many years ago that
the soft tissues involved in a "vertebral lesion" can vary from the simplest
muscle contraction to degenerative fibrosis of the muscles or even further to
complete ossification of the involved ligaments and bursae.
After years of study, Gillet and his associates concluded that abnormal
spinal muscle tone and changes within periarticular ligaments and intraarticular soft tissues were the primary factors responsible for the subluxation complex. These elements were also found to be the ones most influenced by
the "chiropractic adjustment." Gillet showed that the dynamic chiropractic
adjustment does not replace a vertebra or realign a bone; rather, it tends to
eliminate the reason for its so called "abnormal position." Once adjusted
(mobilized), the vertebral motion unit readapts itself, rapidly or slowly
depending on its state of adaptability, to its full range of motion often
without further necessity of the doctor's intervention.
Because bony segments have not actually slipped out of place, an explanation is offered on why postadjustment static x-ray films frequently fail to
show anatomical changes after the patient becomes symptom free. A freely
mobile joint will rest in its most ideal midrange of motion possible a position of readiness. If structural changes have occurred that have altered the
articular surfaces or otherwise impaired its dynamic motion and/or static
position in anyway, the adaptive or compensating resting position may appear
as a misalignment during roentgenographic analysis. This is the typical
"malpositioned vertebra" so often described in chiropractic literature.
Gillet's studies of vertebral fixation do not amend basic chiropractic
concepts regarding the potential effects of subluxation complex (eg, neurologic, myologic, circulatory, inflammatory, and/or cerebrospinal and axoplasmic
fluid changes). They only place them in a more dynamic perspective. This will
become clearer within the following sections of this chapter.
Spinal Dynamics
In general, it would seem that a spine will not remain normal if it is not
kept in a good state of mobility. This supports the necessity for voluntary
exercise of normal joints as a prophylaxis to disease.
During normal spinal motion, cineroentgenographic and surgical animal studies have shown that
(2) the intervertebral foramina (IVFs) are constantly opening and closing, and thus compressing and stretching the contents of the IVFs (viz, the spinal nerves, recurrent meningeal nerves, arteries, and veins).
Acute vs Chronic Spinal Fixations
The physiologic stretching, compression, and stimulation of the contents
of the IVFs is normal and quite necessary to maintain a healthy state of the
structures involved. To not occur would produce in the spine or any extraspinal synovial joint effects similar to those seen following prolonged immobilization of a limb such as disuse atrophy, ligament shortening, circulatory
stasis, neurotrophic changes, etc. It is well recognized that the atrophy of
disuse is one of degeneration; it is a pathologic state that produces minimal
nerve excitability (irritation). This is undoubtedly why we find that an acute
subluxation-fixation produces far more clinical expressions than a chronic
subluxation-fixation and its effects tend to reflect signs of hyperactivity
(eg, spasm, warmth, hyperesthesia, visceral hyperfunction). On the other hand,
a chronic subluxation-fixation tends to express signs of hypoactivity (eg,
weakness, coolness, numbness, visceral hypofunction, musculoskeletal
degeneration).
Some authorities relate these changes with either the effects of neural
facilitatory or inhibitory effects within the anterior, lateral, and posterior
columns of the spinal cord. For example, facilitation would respectively manifest as motor excitation (eg, hypertonicity, spasm), sympathetic vasomotor
excitation (eg, warmth), and sensory excitation (eg, pain, hyperesthesia). In
contrast, inhibition would exhibit as motor depression (eg, hypotonicity,
weakness), sympathetic vasomotor depression (eg, coolness, trophic changes),
and sensory depression (eg, anesthesia).
The Compensatory Factor
Whenever an articulation is deprived of carrying out its normal function
(motion), at least one other articulation is forced to take upon itself the
burden of compensatory excessive motion, which may include eccentric and/or
out-of-plane movement. This additional role within the counterpart joint or an
adjacent articulation in the kinematic chain leads to irritation to the degree
of inflammation once its homeostatic reserves are surpassed. Therefore, it is
often seen that a site of fixation is asymptomatic, while the compensating
hypermobile joint is highly expressive. In such a situation, it would be
contraindicated to adjust the already hypermobile segment even if it is the
focal site of clinical symptoms and signs.
Because of this compensatory factor, vertebral position derangements are
often only of the dynamic variety; ie, they only exist in compensation to
motion stress applied to an adjacent articulation. If the stress applied on
the compensatory hypermobile segment is prolonged, the greater the degree of
related neuromuscular stress. We often see this with the neuromuscular complaints of someone who has engaged in an unaccustomed activity such as shoveling, painting the ceiling, weekend gardening, or after exercise by an unconditioned person.
The question arises that if this is true, why have results appeared to
have been achieved in adjusting the symptomatic joint when it was not the
basic cause of the symptoms? One possible answer is because a specific contact
is extremely difficult to obtain on a specific vertebra as three motion units
have been shown to be affected by a specific thrust. If a broader contact is
used, the force of the adjustment is undoubtedly distributed to a larger
number of neighboring fixated segments. Another possible explanation is that a
major function of all perispinal ligaments is to serve as straps to prevent
excessive motion; thus, if a force is applied to one end of these straps, they
tend to move the adjacent structures to which they are attached (eg, a fixated
adjacent articulation). Other biomechanical and possibly somatosomatic reflex
mechanisms may also be involved.
It is important to remember that a partial unilateral fixation (eg, muscular, early ligamentous) produces symptoms on the opposite side because of the
induced compensatory hypermobility. Thus, contrary to previous thought,
correction is made by applying the adjustment (mobilizing the fixation) on the
contralateral side of symptom expression.
The Interrelationship of Fixations
Many speculations have been made in chiropractic of what has appeared to
be certain vertebrae or areas in the spine having a dominating influence on
the spine as a whole. Such topics as primary subluxations, secondary subluxations, "key" vertebrae, majors vs minors, etc have been discussed since the
early years of chiropractic. Many DCs have been taught that because the sacrum
is the base of the spine, it is almost solely responsible for the mechanical
state of the whole spinal superstructure. Conversely, many others have been
taught that because of its unique position near the brain stem, once the atlas
is correctly adjusted the whole spine will automatically realign itself. Lieb,
a dentist, shows pre- and post-therapy full-spine radiographs exhibiting that
correction of a TMJ syndrome has resulted in the spontaneous correction of
overt scoliosis, kyphosis, and lordosis. There is no doubt that there is both
truth and some misinterpretations in these concepts. Nevertheless, they do, in
part, help to explain many commonly witnessed clinical phenomena.
Gillet often observed that so-called lesser fixations frequently became
spontaneously mobile after he adjusted what was felt to be the most fixated
segment in the spine and/or extremities. It has also been the observation of
Gillet and his associates that, as a general rule, any correction made in any
part of the spine will help the whole spine to correct itself to a degree in
relation to the importance of the local correction. A hypothesis for this phenomenon will be given later in this chapter.
Normal Intervertebral Relationships
Because of our training in postural analysis, many of us have developed
the habit of mentally picturing a healthy spine as one in which each vertebra
is stacked upon its neighbor, with the ends of the spinous processes representing a dotted vertical line when the patient is standing or sitting and
facing forward. While this is generally true, this viewpoint of the spine in
such static attitudes is far removed from its role in daily living in which
the spinal segments (motion units) are constantly rotating, bending, flexing,
and extending. Except for possibly a few seconds at a time, the spine and its
associated tissues are never at rest.
In any given movement, a joint will assume the position demanded of it by
its anatomical plane and the gravitational and muscular forces directed on it.
This is obvious in a "short leg" syndrome when the spine is examined in the
upright position, where the hip, sacroiliac, and lumbar articulations must
attempt to accommodate themselves functionally to compensate for the unlevel
base of support. This mechanism is evident during all normal body motions, for
a movement of any body part requires a compensatory reciprocal action by other
body parts to maintain equilibrium. The same biomechanical process is true in
every case in which a vertebra is fixed at or near its extreme range of normal
motion, causing other articulations to "displace" themselves in adaptation to
the fixation during some or all motions, depending on the site and extent of
the fixation. Thus, an "abnormal segmental position" by itself is not pathognomonic of subluxation. It is for this reason that the editor of the ACA's
Basic Chiropractic Procedural Manual chose to take several pages to just summarize the criteria indicative of a subluxation.
Effects of Common Trauma
Ligaments are never tender unless they are in a pathologic state. Trauma
far less than that causing fracture or dislocation produces an inflammatory
reaction similar to that caused by a bacterial invasion. The reaction to bacterial invasion is designed to contain and wall off the bacteria to prevent
further spreading of the infection. After trauma, localization serves to contain the products of the injured tissues. Unfortunately, the resolution of
inflammation (scarring) can be especially harmful if the joint has not returned to normal mobility. This occurs because normal periarticular soft tissues
are flexible, elastic, plastic, and generally richly vascular. Scar tissue, on
the other hand, tends to be stiff, unyielding, and poorly vasculated. For this
reason, reinjured joints that were not properly attended initially are extremely slow to heal. Every individual has sustained numerous bumps, strains,
and sprains within his life.
Acute inflammation can develop into chronic inflammation that may continue
for decades. Therefore, it is necessary to treat each trauma until all pain,
tenderness, swelling, immobility, etc, are eliminated. Partial treatment is
not adequate.
The diagnosis should be accurate and comprehensive. More than one tissue
is usually affected by a single traumatic incident, and the treatment should
be specific for each tissue affected. Determining the cause is not an easy
task. For example, tender hypertonic perivertebral tissues found in the upper
thoracic region of the spine may be from:
(2) unusual sustained postures (eg, prolonged spinal extension as in painting a ceiling),
(3) a viscerosomatic reflex (eg, heavy smoking, lung or heart disease),
(4) excessive compensatory segmental hypermobility owing to one or more fixated lower cervical or
midthoracic vertebral motion units, or
(5) a combination of two or more of these factors.
Joint Play and Its Restrictions
In addition to the normal active and passive ranges of motion, there is a
third type of motion called "joint play." This small but precise accessory
movement within synovial joints cannot be influenced except passively. Although joint play is necessary for normal joint function, it is not influenced
by a patient's volition. Thus, joint play can be defined as that degree of end
movement or distention allowed passively that cannot be achieved through
voluntary effort. In other words, total joint motion is the sum of the voluntary range of movement plus or minus any joint play exhibited.
Joint play occurs because normal joint surfaces do not appose tightly. Because joint surfaces are of varying radii, movement cannot occur about a rigid
axis. The capsule must allow some extra play for full motion to occur. In
addition to translatory and rotational joint play, a degree of distraction
must exist. If any one of these involuntary movements is impaired for some
reason, the articular surfaces become closely packed (compressed) and motion
will be restricted. Added to this is the factor that there are small spaces
created by articular incongruence necessary for hydrodynamic lubrication. Prolonged compression would lead to poor lubrication and possible ischemia,
likely progressing to degenerative joint disease due to abrasion irritation.
Joint play cannot be produced by phasic muscle contraction. However,
voluntary action is greatly influenced by normal joint play. The loss of joint
play results in a painful joint that becomes involuntarily protected by secondary muscle spasm. Thus, motion palpation to detect restricted joint play is
an important part of the biomechanical examination of any painful and spastic
axial or appendicular joint. Pain and spasm result when a joint is moved
(actively or passively) in the direction in which normal joint end-play is
lacking. Once normal joint play is restored, the associated pain and spasm
subside.
Joint play should exist in all ranges of motion that are normal for a particular joint. That is, if a joint functions in flexion, extension, abduction,
and adduction, the integrity of joint play in all these directions plus distraction should be evaluated. It is not unusual for joint play to be restricted in some planes but not others.
A common cause of articular fixation and the resulting motion restriction
is disuse. Many occupations require that certain joints move only in one or
two planes but not all planes available. For example, a joint that is continually flexed but rarely extended will exhibit normal or abnormal joint play in
flexion and frequently restricted joint play in extension. A similar situation
occurs in a joint that is frequently abducted but rarely adducted or frequently rotated toward the left but rarely to the right.
The importance of freeing articular fixations (eg, by chiropractic adjustments, mobilization) is brought out by Mennell. Normal muscle function depends
on normal joint function, and vice versa. If joint motion is not free, the
involved muscles that move it cannot function and cannot be restored to normal. Thus, impaired muscle function leads to impaired joint function, and,
conversely, impaired joint function leads to impaired muscle function. In this
clinical cycle, muscle and joint function cannot be functionally separated
from each other.
In summary, Faye emphasizes the following major points of joint play:
2. Voluntary action depends on normal joint play, but voluntary motion and
exercise cannot produce or restore joint play. The presence or absence of
joint play can only be demonstrated by an examiner; ie, passively.
3. Loss of joint play produces pain on testing; ie, whenever that direction of joint play is challenged. When restricted joint play is restored by
manipulation, the related pain abates. A painful joint produces secondary
muscular changes; ie, spasm, which is nature's way of preventing injurious
joint movement. If painful joint movement occurs because of joint play
restriction, the joint play must be restored to near normal to obtain a permanent reduction of the spasm. [See Clinical Comment 1.1]
4. Muscles that move a joint with joint dysfunction become hypertonic in
response to the pain from irritation; therefore, the active range of motion is
also restricted.
5. Joint play can only be restored by a mobilizing force (maneuver,
thrust, impulse) delivered satisfactorily; ie, in line with the plane of articulation and against the motion resistance (fixation).
The force of gravity is always directed toward the earth's center. Thus,
the gravity line of action and direction are constants. In the upright "rigid"
body posture, the gravitational force on the entire mass can be considered a
single vector through the center of mass that represents the sum of many
parallel positive and negative coordinates (Fig. 1.1).
Describing Positions in Space
In a two-dimensional reference system, the plane is simply divided into
four quadrants by a perpendicular vertical ordinate line (Y axis) and a horizontal abscissa line (X axis). A third axis (usually labeled Z) can be used to locate points in three dimensions. The Z axis crosses the origin and is perpendicular to planes X and Y.
There are several reference systems. This particular system is the Cartesian coordinate system in which:
(2) axial rotation is rotation about the Y axis, and
(3) lateral flexion rotation is rotation about the Z axis.
In biomechanics, the body's reference origin is located at the body's
center of mass. This is usually just anterior to the S2 segment. When this
point is known, gross body space can be visualized as being in the sagittal
(right-left) Y-Z plane, frontal or coronal (anterior-posterior) X-Y plane, or
horizontal or transverse (superior-inferior) X-Z plane. With such a reference
system, movement of any body segment in these planes can be described by
placing a coordinate system at the axis of a joint and projecting the action
lines of the muscles involved.
Axes
An axis is a straight line around which an object rotates, a line serving
to orient a space or object (about which the object is symmetrical), or a
reference line in a system of coordinates. Most body movements are rotations
about joint axes and are rarely confined to a simple arc. Such motions vary to
compensate for muscle-joint restrictions, bones twisting about their axes, and
the transfer of power from one set of muscles to another within the range of
movement. The joint surfaces of spinal joints are usually convexo-concave in
design; ie, the convex surface is larger than the concave surface. This relationship is exaggerated in all extraspinal ball-and-socket joints.
If the anatomical position is used as a reference point, joint movements
occur in a definite plane and around a definite axis. Flexion, extension, and
hyperextension are movements in the sagittal plane about a frontal axis. Abduction and adduction are movements in the frontal plane about a sagittal axis. Rotation, pronation, and supination are movements in the transverse
plane about a vertical axis. And circumduction is movement in both the sagittal and frontal planes. See Table 1.1.
Table 1.1. Joint Movement Planes and Their Axes
Movement Plane Axis Flexion Sagittal Frontal Extension Sagittal Frontal Abduction Frontal Sagittal Adduction Frontal Sagittal Rotation Transverse Vertical Pronation Transverse Vertical Supination Transverse Vertical
Linear and Circular Motion
The two basic types of body movement are linear movement and circular
movement. Linear movement is that in which the body as a whole or one of its
parts can be moved as a whole from one place to another in a straight line.
One example of linear (sliding, gliding, translation) movement without any
circular motion is long axis distraction of a finger joint.
Circular movement (angular, rotational) is that in which the body or a
part can be moved around the arc of a circle. An example of circular motion is
seen between the long bones of the extremities and in the spinal column. Circular movements occur in definite planes and around a definite axis (center of
rotation). They comprise an important diagnostic viewpoint in musculoskeletal
disorders, and, as previously described, each of these three axes of rotation
is perpendicular to the plane in which motion occurs.
Structural Motion
From a clinical viewpoint, structural motion can be defined as a body
segment's relative change of place or position in space within a time frame
and about some other object in space. Thus, motion may be determined and
illustrated by knowing and showing its position before and after an interval
of time. While linear motion is readily demonstrated in the body as a whole as
it moves in a straight line, most joint motions are combinations of translation and angular movements that are more often than not diagonal rather than
parallel to the cardinal planes. For example, a vertebra cannot move in the A-P plane because its articulating facets are slanted obliquely. In addition to
muscle force, joint motion is governed by factors of movement freedom, axes of
movement, and range of motion.
Degrees of Joint Movement Freedom
The body is composed of numerous uniaxial, biaxial, and multiaxial joints.
Joints with one axis have one degree of freedom to move in one plane such as
pivot and hinge joints, joints with two axes have two degrees of freedom to
move in two different planes, and joints with three axes have three degrees of
freedom to move in all three planes (eg, ball-and-socket joints). Thus, that
motion in which an object may translate to and fro along a straight course or
rotate one way or another about a particular axis equals one degree of
freedom.
To know the actual degrees of freedom (ranges of motions) available to a
part of the body, one must sum the degrees available of adjacent joints to
appreciate the amount of free motion of one part about another part. The
degrees of freedom of a fingertip about the trunk, for example, are the sum of
the degrees of freedom of all the joints from the distal phalanges to the
shoulder girdle. While the distal phalanges have only one degree of freedom
(flexion-extension), the entire upper extremity has 17 degrees in total. This
summation process is an example of a living, open kinematic chain.
Combined Movements
Simple translatory motions of a body part invariably involve movements of
more than one joint. This requires reciprocating actions of three or more segments at two or more joints if parallel lines are to be followed. For example,
a fingertip cannot be made to follow the straight edge of a ruler placed in
front when the wrist, elbow, and shoulder joints are locked. The fingertip
must follow an arc and not a straight line. Thus, human motion can be described as translation that gains major contributions from linear, angular, and
curvilinear motions. The terms general or three-dimensional body motion infer
that a body part may move in any direction by combining multidirectional
translation and multiaxial rotation.
Plane Motion
Any motion in which all coordinates of a rigid body move parallel to a
fixed point is referred to as plane motion. Such motion has three degrees of
freedom (ranges of motions); viz,
(1) moving toward the anterior or posterior,
(2) laterally moving toward the right or left, and
(3) spinning in one direction or the other.
In other words, plane motion has two translatory degrees of
motion along two mutually perpendicular axes and one rotational degree of
motion around an axis perpendicular to the translatory axes. Thus, when an
individual flexes his spine forward, the vertebrae flex and rotate in a single
plane about an axis that is perpendicular to the sagittal plane. In such plane
motion, various points on a particular vertebra will always move in parallel
planes.
The Instantaneous Axis of Rotation
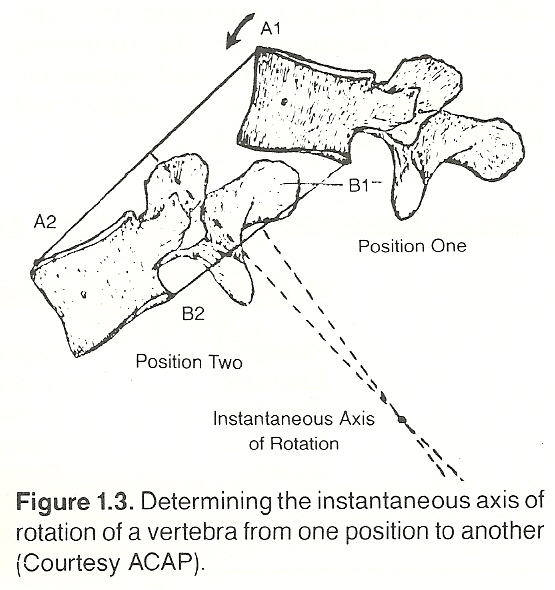 |
Plane motion is described by the position of its instantaneous axis of
rotation and the motion's rotational magnitude about this axis. In the above
example of spinal flexion, for instance, as a vertebra moves in a plane, there
is a point at every instant of motion somewhere within or without the body
that does not move. If a line is drawn from that point so it perpendicularly
meets the line of motion, the point of intersection is called the instantaneous axis of rotation for that motion at that particular point in time (Fig.
1.3). Most joint movement is to a great extent rotational motion, but the axis
of motion may change its location and/or its orientation during a complete
range of motion.
Out-of-Plane Motion
As contrasted to plane motion, out-of-plane motion is a type of general
body motion with three degrees of freedom: two rotations about mutually perpendicular axes and translation perpendicular to the plane formed by the axes.
Thus, in out-of-plane motion, the body as a whole or a segment can move more
than in a single plane. For example, if a person bends laterally, a midthoracic vertebral body translates from the sagittal plane towards the horizontal
plane (Fig. 1.4). This is not plane motion because various points on the
vertebra do not move in parallel planes.
Motion Barriers and Their Significance in Manipulation
All types of joint manipulation impose static and dynamic forces across
joint surfaces. Within its anatomical range of motion, a normal joint exhibits
in all planes of motion:
(1) a large voluntary active range,
(2) an involuntary stress-less passive range, and
(3) a slight paraphysiologic range that is determined by ligamentous plasticity, elasticity, and viscoelasticity (joint play). These ranges are used in voluntary exercise, mobilization, and adjustive techniques, respectively. To appreciate this more fully, an understanding of the barrier concept is necessary.
If a joint is tested passively to determine its range of motion, the
examiner will note increasing end resistance to motion referred to as a
"bind," the physiologic motion barrier, or the elastic barrier. If the joint
is slowly carried past this point, the added motion becomes uncomfortable to
the patient. If carried still further to a point just short of injury, this
point is the anatomical motion barrier. That slight range of motion between
the elastic barrier and the anatomical limit is the involuntary paraphysiologic space or range, the area of passive joint play. At the end of joint play,
the anatomical barrier, the joint tissues are stretched to their structural
limits.
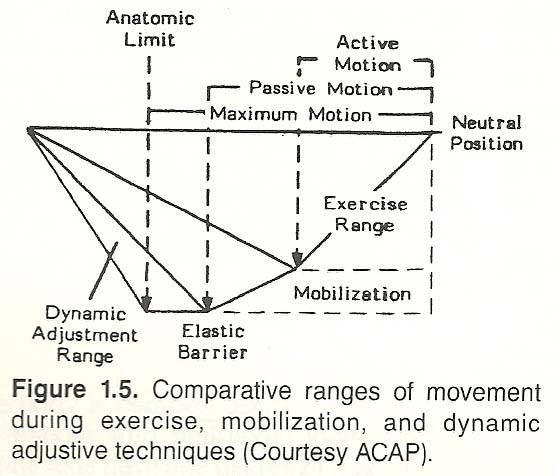 |
The gross evaluation of passive joint movement is normally conducted to or
within the elastic barrier (Fig. 1.5). Thus, joint motion evaluation is accomplished by passively carrying the joint through a range of motion until the
physiologic motion barrier is firmly encountered, and then noting the degrees
of movement achieved.
A spinal fixation has been previously defined as some abnormal factor that
blocks or inhibits passive motion. It has also been described that the term
fixation is not synonymous with the term subluxation; fixation is only one,
but highly necessary, characteristic of the subluxation complex.
(1) muscular,
1. Spasms and cramps that occur in other parts of the body (eg, calf
"Charley horse," intestinal colic, diaphragmatic spasm of "windedness") are
acute contractions that are extremely painful. In contrast, the spasms associated with spinal fixations are usually only sensitive to deep pressure and
otherwise go unnoticed by the patient.
There is no doubt that these perivertebral spasms exist because they can
be palpated. The most common ones found are of the rotatores, multifidi,
interspinales, intertransversarii (cervical), obliquus capitis (atlas-axis),
levatores costarum, spinalis groups, and different portions of the quadratus
lumborum. While areas of spasm can sometimes be palpated in the large-long
muscles of the back, they are rarely found to be responsible for individual
fixations. Gillet's findings to date have tended to confirm Palmer's concept
of a single segmental subluxation (the "major" concept) rather than Carver's
hypothesis of abnormal curves of the spine (summation of the whole area) being
the focus for pathologic expression. Regardless, further research is necessary
for uncontested confirmation of either theory.
(1) The sustaining or resting tone (tension, firmness) of a muscle (an involuntary mechanism) is controlled by the sympathetic
nervous system through low-frequency asynchronous impulses from the spinal
cord. Its purpose is to keep the muscular system in a neurochemical and functional state of readiness to act and maintain static postural equilibrium
(sustained by the stretch reflex). It is active during both rest and work, and
is especially developed in the antigravity muscles.
It is electrically silent during rest and relatively
silent during the relaxed upright position if the body is well balanced over
weight-bearing joints. Voluntary muscle contraction is always superimposed on
the involuntary intrinsic tone of the muscles involved in any musculoskeletal
action. They are usually palpated as taut tender muscle fibers underneath hyperesthetic skin. If the overlying skin and subcutaneous tissues near the related
spinous process are rolled between the skin and index finger, acute tenderness
will be reported by the patient.
They exhibit restricted mobility from the start when challenged, and the
end feel exhibits a little "give" and a rubbery end block.
They are completely released and almost immediately become nontender,
relaxed, and the segment to which they are attached becomes mobile with the
proper adjustment.
They are usually secondary to another area of fixation or the result of
a reflex (somatosomatic or viscerosomatic); thus, they will likely recur if
the primary fixation or some other focus of irritation is not corrected.
Unilaterality and Acuteness Factors. Besides being the most numerous,
muscular fixations are the most pathognomonic of overt symptoms yet the most
open to change by either direct or indirect methods according to Gillet. They
also are the type in which the "displacement" factor is the most visible
because the spasm or hypertonicity involved is usually unilateral. This can
often be seen with the axis, where unilateral hypertonicity of an obliquus
capitis inferior muscle pulls the spinous of the axis laterally. This
unilaterality is frequently a sign of its acute state. The more acute the
condition, the less degeneration will be found in the muscle responsible and
the greatest change can be observed after an adjustment either locally or
through the correction of more chronic major fixations.
Remote Effects. Muscular fixations are frequently secondary facilitated
"reflex" responses to more chronic fixations elsewhere or an activated
viscerosomatic reflex. If the result of a somatosomatic reflex, many of them
disappear spontaneously after the correction of primary ligamentous and
articular fixations. Furthermore, Gillet reports that there seems to be an
important specificity between primary chronic fixations and acute muscular
(reflex) fixations. This specificity is often surprising in its remote location, sometimes going from L5 to the lower cervicals without an apparent
neurologic or biomechanical explanation. Another common example is an upper-cervical major fixation that produces low-back muscular fixations which, in
turn, results in low-back pain and dysfunction.
Etiologic Questions. The inquiry commonly arises: Which comes first, fixation or postural distortion? There are two general answers (possibilities) to
this question:
1. Muscular contraction can pull a vertebra out of normal resting alignment.
The first type (1 above) takes in all traumatic subluxations in which one
or more muscles react to the trauma by a vigorous defensive contraction (nociceptive reflex). If this contraction exceeds an individual's limits, a noxious
nerve-muscle cycle can be established that tends to remain until a counter-
acting force (eg, adjustment) interrupts the cycle. This type of fixation-mal-placement syndrome would also include situations resulting from a feedback
mechanism from a unilateral peripheral irritation (eg, a viscerospinal
reflex), including those of the upper cervical area from excessive mentalemotional stimulation, visual fatigue, and other reflex fixations. As these
fixations are of a muscular nature, they are usually unilateral, or
predominantly so, and acute.
(1) a short leg,
In all these
conditions, we would have what could be called "microtraumatism," the most
typical being the anatomical short-leg syndrome in which the associated lumbar
scoliosis is a normal adaptation as long as the scoliosis is flexible to the
degree that the spine will straighten in the sitting and recumbent positions.
On this subject, Faye mentions that Lynton G. Giles has shown that a leg length difference of approximately 15 mm is necessary before appreciable adaptation occurs.
(1) the fixation comes first, or
Both types may sometimes be
found in the same area, in which case it is more often the acute type that
adds itself to the chronic type. In the chronic type, states Faye, degenerative changes within the three-joint complex of the motion unit must be present
for true displacement to exist.
Most patients have more than one major ligamentous or articular fixation. We try to adjust the most fixated (least "springy") motion unit first. As the muscular fixations spontaneously normalize, a second or third motion unit is adjusted to influence other muscular fixations. As the biomechanics improve and there are less aberrant joint insults to the spine and locomotor system, the inflamed joints begin to heal.
Effects of Adjustive Therapy The reflection of a degenerating chronic muscular fixation or the effect
of ligament trauma.
Overlaid with atrophied subcutaneous tissues.
Palpated as an abrupt, hard block within the normal range of motion that
exhibits no end play.
Bilateral (with one side tighter than the other) or else are in the
median line.
Improved only slightly immediately after each corrective treatment.
During this phase of treatment, stretching exercises at home should be recommended to the patient. A 30-second stretch into the fixation, just short of inducing pain, is my suggestion. This stretching should be repeated two or three times a day. The last few seconds of the stretch is done while exhaling.
The Intervertebral Discs Are motion palpated as being completely immobile in all directions and
asymptomatic.
Are painful when challenged by the palpator.
Progress to ankylosis; thus, irreversible in the terminal stage.
Articular fixations, which are always considered major faults, should
usually be corrected first, and ligamentous fixations should be given priority
consideration over muscular fixations because the latter are often secondary
(compensatory, reflexively produced). [See Clinical Comment 1.4]
I have found it a clinical advantage to adjust one major at one office visit. However, I attempt multiple adjustments in different ranges of motion in the motion unit selected. Some will produce audible releases, others will effect only a mobilization.
It has been my clinical experience that if chronic changes are present the gross ranges of motion can be restored to the spine with repeated mild adjustments directed to the least fixated areas. Gradually, over a long period of time (often 12-16 months), the doctor can adjust the most fixated areas. The change of flexibility is greatly appreciated by the older patient. I see these patients twice a week for 1-2 years and have recorded many remarkable improvements in range of motion.
Flatfoot. The flattening of the arch (pes planus or valgus) on the long
extremity could be a natural adaptation process to diminish the leg of the
relatively long leg. If we examine pelvic equilibrium, it will be found that
the long extremity has rotated externally because of movement of the related
ilium, when the weight of the body during gait falls abnormally at an angle
over the arch of the foot (forcing it downward). When such a mechanism occurs,
it would appear to be contraindicated to attempt to raise the compensatory
fallen arch with an arch support.
The Trochanter Phenomenon. The trochanter phenomenon, a term coined by
Illi, refers to the lateral sway of the whole pelvis towards the side of the
short leg. Gillet explains that this mechanism would not be able to influence
pelvic level if the lower extremities were simply straight vertical structures
and if the feet were placed exactly beneath the heads of the femurs because
this would constitute a parallelogram in which the upper horizontal arm would
always be parallel to the floor. The influence of lateral sway is achieved
because the femoral head projects at an angle from the surgical neck and, as
the femur is usually slanted exteriorly, each femur slants to a different
degree during lateral sway. This makes one femur shift slightly superior on
the long side and the other slightly inferior on the short side.
Compensatory Thoracic Rotation. The mechanisms of pelvic sway and lumbar
rotation described above attempt to swing L3 sideward for 1 3 cm, but this
cannot be tolerated because it places greater weight on that side. The long
muscles of the legs and lower back are forced to remain tensed to restrain
this sway from increasing. So it is at this point that equilibratory forces
begin to return the spine toward the median line, which it usually reaches in
the region of the lower thoracic spine, to distribute body weight more equal
bilaterally. While the perimeters of the lumbar vertebrae may appear to have
rotated considerably, it should be noted that the vertebral canal has only
distorted slightly because each vertebra has rotated only slightly in
relationship to its adjacent vertebrae: the spine is not only designed for
segmental motion, it is also designed for protection of the contents of the
vertebral canal. Furthermore, if the lumbar spine is normally flexible, the
lower thoracic vertebrae are progressively less so because of their attachment
to the thoracic cage. The necessary counterrotation of the thoracic vertebrae,
in compensation to the contralateral lower lumbar rotation, is usually
complete by the level of T8, at which point the vertebrae thereafter rest on a
relatively level plane. Another curve is then produced to return the spine to
the midline near the level of C7 or C6.
Gillet believes that the pathogenicity of any agent or act that is detrimental to health is summed with others present until they accumulate to the
point where the reserve forces and defenses (eg, neurologic, hormonal, immunologic) of the body become overpowered. He proposes that each individual has a
certain hereditary or acquired health-index (ie, a threshold of dysfunction).
The Physiologic Stress Factor in Illness
(1) the symptoms are overanxious reactions of the body to rid itself of a new or chronic irritation; and
According to this
classification, a majority of symptoms belong to the first category. Normal
defensive reactions (eg, fever, tachycardia, hypertension) may become so
poorly integrated or out of control that the overreaction progresses to an
action that kills the individual.
(1) the patient's faith in the doctor's
ability/honesty and
Although women appear to have a higher threshold for pain than men, Gillet
points out that nature appears to also have provided them with a compensatory
lower threshold for worry. It is likely for this that females seem to suffer
with cancer phobia more than males.
Joint dysfunction implies the loss of one or more movements within the
normal range of motion and associated pain, but it is only one possible
problem that must be differentiated from other causes of joint pain. There may
be many clues within a history of joint pain that point to the diagnosis of
joint disease and many may strongly suggest joint dysfunction. This may represent separate overlapping problems or one complex problem. For example, joint
pain may be the chief complaint in such systemic diseases as polyarteritis
nodosa, systemic lupus erythematosus, dermatomyositis, erythema nodosum, and
scleroderma. It is also sometimes associated with kidney or pulmonary diseases, ulcerative colitis, acromegaly, and hemorrhagic dyscrasias. It should
be remembered that gout may occur in any limb joint and is occasionally found
in the spine. It is not always associated with tophi or limited to the feet
and hands.
(1) gout affects the metacarpophalangeal joints,
(1) the pain has
a sudden onset and is sharp,
(1) joint dysfunction pain does not occur at night and is relieved by rest,
The word paradigm means a pattern, model, or viewpoint. In pioneer chiropractic, this viewpoint was usually restricted to considering a subluxation
complex as being the result of a static articular displacement; viz, a bone
out of place. This concept has led to frequent puzzlement when a patient
became symptom free and yet posttherapy static radiographs of the spine showed
little change in the original static malpositioning of certain segments. It
also failed to explain why patients with well aligned segments in a static
radiograph were expressing obvious signs and symptoms of a subluxation
complex. In modern chiropractic, the emphasis is on some factor that is interfering with normal articular mobility; thus, a dynamic impairment of mobility
rather than a static positional impairment.
(1) the hypermobile state, which obviously
needs no further mobilization, adjustment, or manipulation;
(1) where to adjust,
Thus, one major reason for mastering the art of motion palpation is to determine the quality of existing fixations. After such areas have been found and
classified as muscular, ligamentous, articular, or bony fixations, a rational
approach to adjustive therapy can be outlined. During this process, in which
the doctor should be constantly attempting to verify whether a fixation is
primary or secondary, the following general rules should be kept in mind: Only primary and possibly minor nonsecondary fixations require adjustment, and they should be mobilized in all directions of restricted mobility.
Primary fixations feel the most blocked, and restricted mobility is
demonstrable in more than one direction. Primary fixations are not particularly tender in contrast to secondary fixations except when they are stressed by
an examiner into the direction of restriction.
The adjustment of a secondary fixation will exhibit short-lived benefits
or possibly an adverse reaction unless the primary fixation is corrected
first.
The adjustment of a primary fixation will produce changes both locally
and elsewhere in the spine (eg, normalization of signs and symptoms expressed
at the site of a secondary fixation).
If the primary fixation(s) have been correctly determined and adjusted,
the treated articulation(s) should exhibit increased mobility on the next
office visit, and fixations judged as secondary should have spontaneously
improved or disappeared. There should be general improvement in general spinal
mobility, equilibrium, and related symptomatology. However, if the site of a
primary subluxation was misdiagnosed, the patient will likely report no improvement or an increase in symptoms on the next visit, and the fixations previously adjusted will be found to be in the same state as they were during
examination on the previous visit. When this latter situation occurs, a determination must be made whether the previous diagnosis was correct or not.
It has been a common experience for me to treat a chronically fixated spine in patients over the age of 35 on a twice-a-week schedule over a period of 6-18 months. The constantly imposed demand of spinal manipulation being applied to the most fixated motion units eventually is met by a specific adaptation of joint motion and elastic connective tissue.
Motion. A continuous change (displacement) of position.
Angular Motion.
This term is used to indicate an increase or decrease in
the angle formed between two bones; eg, flexion-extension at the elbow or
knee.
It may come as a surprise to some that there is no standardization of
chiropractic technic. Many of us have assumed that the chiropractic adjustive
procedures we were taught in chiropractic college were similar to those taught
in other chiropractic colleges. This assumption is false. There is a wide
variance in instruction among chiropractic colleges, and this instruction
varies when one instructor is replaced by another at the same college. This is
not unusual in teaching a manual art. Chiropractic technic, like a surgical
skill, is an art and not a science. Regardless of the variance in methodology,
each method taught is valuable; and the more variances we know, the more we
can refine, expand, and diversify our personal applications. Perfection of an
art is a constantly expanding process. The quest of perfection in our profession is the basis of the diligent practice of chiropractic.
"In discussing chiropractic techniques, it is only proper to note that
chiropractic holds no monopoly on manipulation. Manipulation for the purpose of setting and replacing displaced bones and joints, including spinal
articulations, is one of the oldest therapeutic methods known. It has been
and still is an integral part of the armamentarium of healers of all times
and cultures.
Each chiropractor has a number of contact points he or she uses, but
usually one or two are used whenever possible because of personal preference.
The most commonly applied contact points are shown in Figure 1.12. The force applied may be low, medium, or high.
The duration of the force may be brisk or sustained.
The amplitude (distance of articular motion) may be short, medium, or
long.
The direction of the force may be straight or curving and/or perpendicular, parallel, or oblique to the articular plane.
Overlying soft-tissue tension may be mild, medium, or strong. Primary or secondary leverage may be applied early, synchronized, or
late.
Contralateral stabilization may or may not be necessary.
Thrust onset may be slow, medium, or abrupt.
Fixations may be produced by perivertebral fascial adhesions, ligamentous
contractures, IVD dehydration, fibrosed muscle tissue, spondylosis, or meningeal sclerosis and adhesions. An excessively forceful dynamic thrust to these
conditions may result in increased mobility by stretching shortened tissues
and breaking adhesions, but there is always some danger of osseous avulsion or
tearing of meninges as scar tissue has a much higher tensile strength than
osseous or nerve tissue. Because of this, professional training is mandatory. The mobilization of fixated articular surfaces. The apophyseal joints
can become fixated because of the effects of joint locking (eg, traumatic),
muscle spasm, degeneration, an entrapped meniscoid or other loose body, capsular fibrosis, intra-articular "gluing" or adhesions (eg, postsynovitis,
chronic rheumatoid conditions), bony ankylosis, facet tropism, etc.
The relaxation of the perivertebral musculature. While a high-velocity
force that suddenly stretches muscles spindles in primary muscle spasm
increases the spasm, the same force applied to a segment where its related
muscles are in secondary or protective spasm tends to produce relaxation if
the thrust succeeds in removing the focal stimulus for the reflex.
The shock-like effect on the CNS. Shock-like forces
(1) are known to
frequently have a normalizing effect on self-sustaining CNS reflexes;
Balduc HA: Overview of contemporary chiropractic science for the Chiropractic
Association of Oklahoma. Northwestern College of Chiropractic, Convention
notes, April 24, 1983.
Active motion normally swings between the neutral position to the point of
tissue resistance, while passive motion extends past this to within the
elastic barrier. The usual objective of most mobilization techniques is to
restore the normal range of passive joint motion from the neutral position to
the normal elastic barrier. Thus, it is slightly longer in range than that of
active motion and to the maximum point of slow passive motion. The objective
of most stretching techniques is to restore motion from the neutral position
to the elastic barrier. Many osteopathic "leverage" techniques are conducted
within this range, as are many chiropractic extremity techniques. In contrast,
specific dynamic chiropractic adjustments are usually carried a step further
deep into the paraphysiologic range, often to the anatomical limit, but the
duration of the application of maximum force is only a fraction of a second.
Wyke has shown that forced active motion on a joint whose mobility has
been restricted will rapidly become painful and its periarticular muscles will
be hypertonic or spastic. For example, loss of joint play in the sacroiliac
joints can cause the gluteals and hamstrings to tighten. If a sudden strong
contraction is required by the quadriceps, the unrelaxed antagonistic hamstrings are likely to tear if the primary motion is accomplished. Various
degrees of this phenomenon are seen in sports and occupational injuries associated with fixations.
THE DIFFERENT TYPES OF FIXATIONS
There are four general types of fixations:
(2) ligamentous,
(3) articular, and
(4) bony. It is clinically important to attempt to judge
the degree of fixation and the nature of the fixative element to evaluate the
minimum amount of force necessary during an adjustive thrust to "break down"
the fixation if it is logical to do so (breaking an ankylosis, for example,
would usually be contraindicated). This is true whether the cause is a spasm,
a shortened ligament, an interarticular adhesion, or some other amelioratable
factor.
Muscular (Class I) Fixations
In relation to spinal fixations, the term muscular spasm is used by Gillet
to describe the state of a muscle or muscles that fixate vertebrae and hinder
their normal movement. Yet, he does this with misgivings because he states
that such contractions are somewhat different from the spasms and cramps which
occur in other muscles of the body. For example:
2. Except for spastic paralysis (eg, poststroke), spasms in other parts of
the body have a short duration. In contrast, the spasms associated with spinal
fixations may endure for months or years without change. In spite of the chronicity, the muscles involved do not necessarily degenerate or become fibrotic
as other muscles normally do under such conditions.
Muscle Tonicity vs Phasic Contractions
In all healthy skeletal muscles, there is a combination of two major
neurologic factors at work:
(2) The voluntary and
involuntary gross contraction of a muscle, under the control of both the
cerebrospinal motor system and cord reflexes, directs all postural, ballistic,
and tension movements.
Gillet postulates that the palpable spasm associated with a vertebral
fixation could be an involuntary state of abnormal hypertonus rather than a
cord reflex initiating a spasm via a phasic contraction as seen in typical
spasms and protective "splinting." This theory could explain why the hypertonic muscles associated with fixations are tender to palpation but not otherwise painful.
Gillet's Theory of the Cause of Fixation-Related Hypertonicity
It is empirically evident that "subluxations" are often caused by trauma
(direct or indirect) such as in blows, falls, and strains or indirect micro-trauma such as from the various effects of biomechanical imbalance. The neuromuscular response to trauma is either contraction to a degree that varies with
the severity of the trauma either a strong rapid contraction or a slow
contraction of long duration. In this context, paraphrasing Gillet, let us
suppose that as soon as the contraction goes beyond a certain limit in force
or duration the autonomic fibers controlling muscle tonicity become abnormally
stimulated. As any neural stimulation of high intensity tends to "jump"
impulses from sensory to motor tracts, via internuncial neurons in the spinal
cord, instead of or before traveling up the cord, it is possible that such a
mechanism could be established as a fixed pattern of behavior, a vicious self-
perpetuating neuromuscular cycle.
If such a hypertonicity is sufficient enough and if it is unilateral, the
motion unit involved will tend to be pulled into a sustained position of
action. This appears likely as each vertebral segment is "balanced" at rest
in a state of physiologic equilibrium between its extremes of motion. The
spine is not a stiff column of segments. The structural properties of its
discs, ligaments, and cartilages are relatively plastic, flexible, elastic,
and viscoelastic. We can now add to this picture the neurologic mechanism of
reciprocal inhibition; viz, phasic agonist contractions are accompanied by a
reciprocal decrease in action in its antagonists. For example, when flexors
act, extensors relax, and vice versa. Reciprocal inhibition is usually thought
of as a temporary mechanism, but is this always true?
General Characteristics of Muscular Fixations
Muscular fixations are the most numerous type of fixation, and their
potential number may appear great in any given patient. They are, however,
usually minor or secondary. Although all possible muscular fixations will not
necessarily exist in each patient, they are all possible and should be recorded with each patient. If no ligamentous or articular fixations are found,
muscular fixations can be corrected. However, if a secondary muscular fixation
is adjusted before mobilization of its primary focus, it will return quickly
(in minutes) because it is an adaptation to the site of primary ligamentous or
articular fixation.
The major characteristics of perivertebral muscular fixations are as
Postural Changes Related to Muscular Fixations
These secondary reflex fixations just described appear to be primarily due
to hypertonicity of the short spinal muscles, but certain long muscles are
sometimes involved. When they are, they produce the characteristic postural
distortions and antalgic positions that are so often seen in clinical practice
and measured by grids, plumb line analyses, etc. Certain methods of spinal
examination use these abnormal postures to deductively reason to the causative
fixation, and some therapeutic techniques work on the long muscles in an
attempt to bring the body back into normal balance. Such procedures may easily
lead to erroneous conclusions and misinterpretations. [See Clinical Comment
1.2]
It is possible to change human posture by working on these long muscles
because it is almost always possible to provide a centripetal effect on a primary condition by influencing the secondary half of the cycle. This can often
be seen in the effects of medical treatment, and it is true with many chiropractic procedures. To perpetuate this effect, however, will require a greater
repetition of the therapeutic agent. It can be stated as a general rule that
each time a correction has to be repeated several times within a short period,
this attempt at correction is being applied to an abnormality which is secondary to another located somewhere else, originating either within the body or
its immediate external environment.
Another difficulty in using gross posture as a sign of fixation is that
not all fixations produce a related hypertonus of long body muscles capable of
altering gross posture. This effect is a characteristic of fixations that produce irritation of the cerebrospinal nerves and far less of those which can
irritate the sympathetic nerves. Specific long muscles that are involved in
postural changes and fixations will be described in subsequent chapters.
2. Because the spine is forced to remain for long periods in a position of
"unrest," the soft tissues of the spine will slowly adapt to the action demanded by the patient's daily activities and positions. The vertebrae involved
can be considered to be "normally" misaligned as long as the reason for this
malposition exists.
The second type of fixation-subluxation (2 above) is of the spinal balance
class, including any vertebral articulation that would be forced to adapt
itself to:
(2) malformed vertebrae,
(3) the imbalancing effect
of acute subluxations,
(4) poor posture caused by unusual working conditions,
and
(5) unilateral imbalancing "specialized" movements in work.
Thus, we have two possible etiologies:
(2) the "displacement" is the primary element.
DR. FAYE'S CLINICAL COMMENT #1.2
If two spinal motion segments are in a state of "malposition" because of
unilateral hypertonicity or spasm of one or more intervertebral muscles, the
structures to which the involved muscles have their origin and insertion will
be drawn towards one another during most types of adjustments. Thus, a dynamic
thrust that has as its objective "realignment" of the segments will obviously
stretch the contracted muscles (increase the distance between muscle origin
and insertion). It is probably for this that a chiropractic dynamic thrust, as
contrasted to a simple slow pull or push, has proved to be more successful in
practice.
While Gillet does not propose that this hypothesis offers a complete ex-
planation, he does believe that it answers more questions than others projected in the past. In addition, this explanation is only rational for those
muscular fixations that remain in a state of prolonged abnormal function and
which are not associated with myodegeneration. He also adds that for some
still unknown reason, other fixations (possibly those in which we have two or
more hypertonic muscles between adjacent vertebrae) sometimes do undergo the
usual degenerative process in a fixation-subluxation syndrome.
Ligamentous (Class II) Fixations
One early physiologic change seen with chronically fixated vertebral
articulations is the shortening of ligaments. This is true because ligaments
always tend to adapt themselves to the range of motion used. That is, they
will shorten to the degree necessary to remove any slack. Thus, in complete or
multimuscular fixations, the associated ligaments and related soft tissues
will have distinctively shortened. The type of thrust used here must be one
designed to lengthen ligamentous tissues (eg, repeated nontraumatic traction
on the insertions of the involved ligaments). Total multimuscular and multiligamentous fixations are frequently found at the sacroiliac joints and the
occipital-atlantal area and are associated with the thoracic spine.
The most pertinent characteristics of ligamentous fixations, which are
often major fixations, are that they are usually:
Shortening of Capsular Ligaments
Gillet and associates have found few spinal fixations that can be explained by shortening of the capsular ligaments, although practically all the other
spinal ligaments seem to be involved in fixations.
When apophyseal capsular shortening occurs, one might think that it would
result in an articular-like fixation. However, this has not been found to be
true: there is still a certain amount of torsion possible. This is especially
evident in the extraspinal joints; eg, when there are many fixations in the
feet involving the calcaneus, tarsals, and metatarsals. Similar fixations can
frequently be found in the proximal articulation of the fibula with the tibia,
in sternoclavicular and acromioclavicular joints, and among the metacarpals.
Such extraspinal fixations can have noxious effects either locally or in the
spine (reflex fixation). These manifestations will be described in Chapters 8
and 9.
Musculotendinous Fixations Resembling Ligamentous Fixations
In certain purely muscular fixations, the spastic or hypertonic muscles
involved tend to degenerate and become fibrotic. For all practical purposes,
such fibrotic muscles resemble ligaments in function and structure. As most of
the deep spinal muscles are underlaid and/or overlaid with ligaments, it is
often difficult to determine which structure is responsible for the fixation.
Fortunately, the type and direction of a corrective thrust is nearly the same,
and even the amount of demonstrable change that can be expected from a
fibrosed muscle or a shortened ligament is the same. Thus, from a clinical
viewpoint, a fibrotic muscle fixation can be classed as a ligamentous fixa-
tion. Gillet believes that this type of fixation is the most common but not
the most irritative.
Several authors have described the shortening or tension found in certain
fascia and tendons as being responsible for the restriction of joint motion,
either by themselves or by hindering the action of their associated muscles.
One example of this is the fascia lata in fixations of the proximal femur. The
Belgium researchers, however, have not been able to confirm this as yet.
Muscular vs Ligamentous Postadjustment Effects
While the adjustive technique need be modified only slightly with either
muscular or ligamentous fixations, the postadjustive reaction is quite different. In muscular fixations, an immediate near-normal range of motion should be
expected. In ligamentous fixations, however, the immediate gain in mobility is
only slight with each treatment. This does not mean, however, that the
increased movements during everyday activities between office visits are not
another important factor in restoring mobility. [See Clinical Comment 1.3]
DR. FAYE'S CLINICAL COMMENT #1.3
Gillet gives no more importance to the intervertebral disc (IVD) in the
production of spinal fixations than any other ligamentous structure. He
believes the integrity of the IVD is generally more of a passive factor than
an active factor. A few exceptions to this general rule will be described in
subsequent chapters, but motion palpation studies have not confirmed that true
IVD lesions are as common as generally accepted in the medical community and
to a great extent within our own profession. Faye states that disc degeneration, with its internal disruption and posterior joint gapping, causes more
hypermobility and instability.
Articular (Class III) Fixations
True articular or total fixations are common manifestations in the human
spine, and they have been the subject of several studies that arrive at conflicting conclusions. Regardless of cause, they appear to be the result of
intra-articular joint "gluing" similar to that seen in adhesive capsulitis and
multiple ligamentous shortenings. Overt pathology does not appear to be
related as the fixation is eventually made mobile by repeated chiropractic
adjustments.
In any total articular fixation, one lateral pair of articulations
(inferior and superior facets) of the bilateral posterior articulations may be
the seat of fixation and the other not. The contralateral pair may be normal
initially, but as the inferior and superior zygapophyses become more immobilized because of the fixation of their contralateral counterparts, they also
become functionally incapable of motion. In time, the pathologic effects of
disuse can be expected in the initially normal pair of articulations.
In total fixations in which the fixative element is the product of
degeneration of the interarticular and periarticular soft tissues, with the
probable development of "adhesions," the major corrective effect of the
chiropractic adjustment is produced by the forced opening of the apposed
facets.
Gillet points out that this type of unilateral total fixation can be
demonstrated when reflex-fixations are searched for and found. This procedure
will be described in a following chapter. It should be mentioned, however,
that total unilateral fixations in the spine function differently than total
unilateral fixations in the sacroiliac joints. In total unilateral fixation of
a sacroiliac joint, the contralateral articulation is not restricted in movement and typically adapts by becoming hypermobile and acutely overstressed in
a prolonged attempt to serve the role of both joints.
This reciprocity of immobility and hypermobility is found in all types of
fixations. In total fixations found between vertebrae, Illi states that the
adaptive hyperkinesis takes place in the articulation above and below, or in
the opposite articulations exceptionally. In partial fixations, it takes place
on the still mobile side of segments unilaterally fixated (Figs. 1.6 and 1.7).
In summary, the major characteristics of articular (total) fixations are
that they:
DR. FAYE'S CLINICAL COMMENT #1.4
Bony Restrictions
Bony outgrowths may be obvious, but if they are near the periphery of a
joint, they may be recognized only by the sudden arrest of an otherwise free
motion. In true ankylosis, there is no mobility whatever and adjacent joints
are often hypermobile in compensation. Roentgenography is usually necessary
for diagnosis.
During physical examination, bony outgrowths within a joint are sometimes
recognized by the sudden arrest of an otherwise free joint motion at a certain
point. That is, an abrupt hard halt in motion usually signifies bone-to-bone
contact, signifying that further movement should not be conducted. Such an
approximation will be felt before the end of normal motion occurs when hypertrophic bone growth (eg, an osteophyte, a malunited fracture, or myositis
ossificans) has developed. If force that is continued beyond the point of a
bony block is painless, neuropathic arthropathy is likely.
True bony ankylosis is one type of total fixation. It has been Gillet's
experience that ankylosis is invariably the result of a local bone disease process or severe trauma and practically never correctable by adjustive therapy.
On the other hand, he feels that a fibrous type of pseudoankylosis is far more
frequent, especially in the midthoracic area during middle age or in the elderly. This is likely the result of a general degeneration of the perivertebral
muscles and ligaments. Although this fibrous condition can be manipulated, it
takes months or years to produce a pale picture of normal motion. Gillet also
states, "Unfortunately, as long as it exists, the rest of the spine will never
remain free from recurrent fixations." [See Clinical Comment 1.5]
Muscle spasm is distinguished from bony outgrowth as a cause of limited
joint motion by several features. Bony outgrowths allow perfectly free motion up
to a certain point, after which motion is arrested suddenly, completely, and
without great pain. Muscular spasm, on the contrary, checks motion slightly from
the onset. Resistance and pain gradually increase until the examiner's efforts
are arrested at some point.
DR. FAYE'S CLINICAL COMMENT #1.5
Adaptive Therapy
We have described that there are four different types of fixations: muscu-
lar, ligamentous, articular, and bony. Granted, these are crude classifications
and closer evaluations made in subsequent chapters will show that these phenomena are much more complicated than they appear on the surface. Each region of
the spine, nearly each motion unit, has its peculiar characteristics in a
fixation-subluxation complex. Certain muscles and ligaments have a greater tendency to become hypertonic or shortened than others, while certain articular
soft tissues also have a greater probability of becoming atrophied or eroded by
articular pressure. Furthermore, some of these fixations show a greater predisposition toward degeneration than others.
It should also be evident to the reader that chiropractic adjustive technics
should be adapted to the type(s) of fixation present if a maximum corrective
effect in quality and duration is to be achieved. An understanding of the
various types of fixation possible will also help to explain why certain other
physical or medical forms of treatment may have a direct or indirect influence
on the spine. In this context, we are in a better position to appreciate the
effects that rest, warmth, counterirritation, acupuncture, mental relaxation,
biofeedback training, or even psychotherapy may have on enhancing muscle
relaxation (hypotonus) and indirectly encouraging the spontaneous correction of
muscular fixations, which, according to Gillet, are the more irritative ones.
SIGNIFICANT PHYSIOLOGIC AND BIOMECHANICAL MECHANISMS
The Mechanisms of Equilibrium
Most practitioners will agree that many patients will present with one
lower limb anatomically shorter than the other limb. Although the term short
leg is used to describe this phenomenon, the length of all structures contributing to the structural distance between the head of the femur and the
floor is being considered. Thus, more structures can contribute to this
"shortness" than just the weight-bearing tibia of the leg; viz, the pelvis,
femur, ankle, and foot.
When a short leg exists, the crests of the pelvis will not be level and
the superimposed spine will try to adapt through various curvatures in an
attempt to keep the eyes level and at the same time keep various body parts
balanced relative to the body's line of gravity. This usually occurs in the
same manner as the biomechanical adaptation of a person walking on the side of
a hill.
All people do not adapt to walking on a horizontally slanted surface in
the same manner, nor do all people adapt to a short leg in the same manner.
Some spines will regain an equilibrium imbalance due to a short leg within a
few lumbar segments (eg, L3), while others will not achieve this until the
upper cervical area is reached. The reasons for this variance may be structural, functional, or just habitual.
Cabot, the famous diagnostician, constantly admonished his students that
"to recognize the abnormal, one must be completely familiar with the normal
and its many variations." Several mechanisms will be described in this section
that are normal responses to the commonly seen anatomical short leg.
The "Flatfoot" Factor
Some authorities consider a unilateral flattened longitudinal arch in the
foot to be one factor that will cause a measurable lowering of one femur.
Gillet feels that this is true in a way, but not in the oversimplified manner
that is often given in explanation. When the Belgium researchers measured the
influence of the height of the arch on the total length of a lower extremity,
they found it to be not more than 1 mm. As anatomical short legs usually have
a discrepancy of at least 5 mm, it is obvious that other causes must be found.
It has been the experience of Gillet that a fallen arch frequently appears
on the side of the long leg. After adding a heel lift on the short side, the
fallen arch may spontaneously correct itself within a few days to become near
normal. He offers the following possible explanations for this phenomenon.
Foot Eversion. Another mechanism, which in a way is part of the one
described above, is foot eversion. This usually occurs simultaneously on the
side of the fallen arch and also tends to bring the head of the femur (and the
structures supported) a little closer to the ground. Gillet contends that the
wearing of a wedge-shaped heel in such a case could aggravate the situation
because it would hinder intrinsic adaptation mechanisms from shortening the
long extremity, thus forcing the pelvis and superimposed spine to distort
further. Such foot eversion (toe-out, ankle pronation) is also part of other
adaptive mechanisms.
Other Efforts to Achieve Equilibrium with an Anatomical Short Leg
Compensatory Sacroiliac Rotational Misalignment. The next articulations
that try to align themselves in an abnormal fashion to achieve equilibrium in
a short-leg syndrome are the sacroiliac joints. Even with the compensatory
trochanter phenomenon, the whole pelvis will still be tilted downwards on the
side of the short leg so the ilia attempt to rotate anteriorly and superiorly
on the low side to lift its articulation with the sacrum and rotate posteriorly and inferiorly on the high side to lower its articulation (Fig. 1.8). This
is possible because the sacroiliac joints lie somewhat posteriorly in relation
to the head of the femur. This motion permits another gain of 1 2 mm, but
unfortunately, it is achieved at the expense of other joints.
Compensatory Sacral Tilt. Intrinsic adaptive mechanisms also attempt to
tip the sacrum itself into a position normally seen during lateral bending;
ie, upward on the short-leg side and downward on the long-leg side in order to
provide a more stable base for the spinal column.
Compensatory Inferior-Superior Sacroiliac. At times, in addition to the
iliac rotation and sacral tilting described, inferior translation of the
sacrum on the ilium on the long side and superior translation of the ilium on
the side of the short leg may be found as an aid to sacral leveling.
Compensatory Lumbar Rotation. The area where postural deformation and compensation is greatest is within the lower lumbar region. The vertebral bodies
and IVDs of the lumbar vertebrae are thicker anteriorly than they are posteriorly, exhibiting the shape of a wedge. During adaptation to a short leg, the
lower lumbars rotate posteriorly on the shortened side in an attempt to compensate for the slanted sacral base. Unfortunately, this rotation produces a
prolonged deformation of the lower lumbar IVFs that tends to encroach on the
nerve roots on the side of posteriority and add tension on the nerve roots on
the contralateral side. Although the sacrum also tries to rotate to adapt to
the position of the rotated L5, the attempt is in vain because the sacrum is
held in a vise-like grip by the ilia assisted by the strong sacroiliac ligaments and superimposed body weight. The lumbar vertebrae above L5 also rotate
and laterally bend in accordance to their respective base of support. In a
typical spine, it is rare to find levelness achieved below the interface of
the disc of L2 and the superior surface of L3.
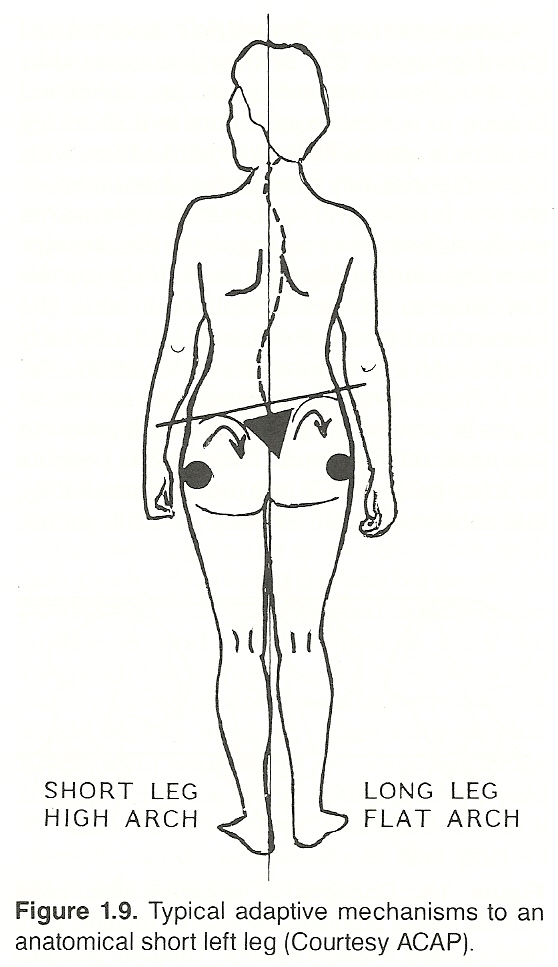
Although the compensatory shifting mechanisms described above are slight,
each in its own way attempts to contribute a benefit to the overall adaptation
to an anatomical short leg (Fig. 1.9). It should also be noted that the mechanisms described and their effects are the ideal and the result of an extremity
deficit likely acquired at birth or during childhood when the spine was supple
enough to regain balance easily and completely. Such ideal adaptation could
also be achieved during puberty or early adulthood if the spine is supple
enough.
Maladaptation Attempts. During the aging process, connective tissues tend
to lose their youthful degree of flexibility, elasticity, viscoelasticity, and
plasticity. The rib cage especially tends to become tough and tight, and the
spine is forced to use whatever compensatory mechanisms are available. When
the forces of adaptability are meager, we may see the unfortunate picture of a
cervical spine that has had to distort itself to a great degree to "catch up"
the lost balance which stopped at the lower thoracic spine. Fortunately, like
the lumbar vertebrae and discs, the cervical segments are also wedge shaped
and this helps considerably. There is also the biologic necessity to maintain,
if possible, level eyes. This sometimes forces a high degree of lateral
flexion at the occipitoatlantal articulations with all the danger of nerve
compression and/or irritation that we know is possible in this highly
vulnerable area of the spine.
The spine is always subject to the trauma of daily living (stumbles, jars,
falls, blows, strains, chronic biomechanical microtrauma, psychic tension,
etc), and it is disturbing to see the spine of a patient in which the mechanisms of adaptation are continually being overtaxed and overthrown by
fixation-subluxations. These deficiencies add to the noxious process and
introduce new causes of imbalance that force adaptive reserves to start new
efforts at several stages. It is this poorly adaptable spine that we see so
frequently within our respective practices. But let us not forget that even a
perfectly rebalanced spine can and will, sooner or later, become functionally
inadequate as mechanisms of rebalancing lose their ideal properties.
Adding the Factor of Fixation. We should not insist that all the compensations described are seen only in the standing position and disappear in positions that eliminate the basic factor of imbalance such as the influence of an
anatomical short leg. Ideally, they should not exist in the sitting and recumbent postures. However, such adaptive forces necessary in the erect position
will, little by little, tend to become fixed and remain in the state of compensation regardless of the position assumed, whether it serves a beneficial
purpose or not. In the situation of adaptation to a short leg, such fixation
is especially true in an individual whose occupation requires prolonged hours
of standing, for it is in the standing position that the involved muscles,
ligaments, and cartilages have been forced to change their architecture. The
ligaments especially on the concave side of a spinal curve tend to shorten and
those on the convex side of the curve stretch to conform to the demands upon
them. Then, and only then, will the lumbar curve, the sacral adaptation, the
iliac rotation, the thoracic counterrotation, the trochanter phenomenon, and
the flattened longitudinal arch become static, fixated. As such, they must not
be "replaced" but mobilized. Thereafter, the role of the doctor of chiropractic changes from therapeutic to preventive. And unless the reason for the
focal imbalance is found and corrected (eg, a short leg), all the fixations
associated will recur.
Testing a Patient's Spinopelvic Adaptability. The following test will
demonstrate to the student of dynamic chiropractic a patient's ability to
adjust to imbalancing factors: First, position the patient in front of a plumb
line and dot the back with a skin pencil where the vertical line falls.
Second, place a piece of wood or a book about 2-cm thick under a patient's
foot. Observe the changes of the plumb line relative to the patient's spine
and pelvis, and mark with a different color the points at which the line
crosses the patient's cervicals, thoracics, lumbars, and sacrum or buttocks.
Then place the block or book under the other foot of the patient and mark the
patient again with a different color. If this test is first conducted with
many supple spines, the examiner is likely to be astonished to see how much
imbalancing a normal spine can withstand. Sometimes, it does not appear to
react with any difficulty to even a 3 cm foot raise. Then compare this to the
reactions viewed with typical adult patients. Some spines will not be able to
adapt to even 1 cm of change, and some changes witnessed will be abnormal.
Although this test will not be of benefit in localizing the specific sites of
fixations, it will show the diverse changes that can take place within an
individual's spine that are due to imbalancing influences.
The Mechanisms of Irritation
Gillet's studies continually verified several major characteristics of
fixations, one being that the pathogenicity of a fixation varies inversely to
the degree of fixation existing. In a unilateral nontotal fixation, for
example, signs of irritation will be found on the movable (contralateral) side
of the vertebra and not on the side of fixation. In a partial bilateral fixation in which some movement occurs on the A-P plane, the signs of irritation
will be bilateral and often of the same degree on both sides. In a total fixation, there are rarely any signs of irritation at the level of the involved
segments with one notable exception: the occipitoatlantal articulation.
Another finding of Gillet was that if the area of the spine in fixation
was actively or passively flexed or rotated several times, skin temperature
readings tend to immediately increase and then decrease upon rest. This supports the hypothesis that the site of fixation, especially if degeneration has
occurred, will exhibit signs and symptoms of hypofunction (eg, anesthesia,
paresthesia, vasodilation, stasis). This would explain why a total fixation
(eg, an ankylosed articulation) is not painful but important clinically
because of the extraordinary motion it forces on adjacent mobile articulations
in the kinematic chain and by the secondary fixations it produces.
When a unilateral fixation exists that allows some contralateral movement,
that motion will occur around an abnormal axis which, if forced, causes a
distinct pivoting-type of aberrant joint separation rather than the normal
translatory gliding or sliding of the articulating surfaces. Oblique x-ray
films of the spine, for example, will reveal reduced facet mobility on the
side of fixation and separation of the facets contralaterally which will
widen further when the patient's spine is forced into flexion or rotation.
Although there is a tendency of many within chiropractic to narrow their
practices to the treatment of musculoskeletal disorders, Gillet strongly
believes that a subluxation complex is involved in many functional disorders
of the viscera. He also proposes that many of these disorders are due more to
faults in autonomic innervation than to irritation or compression of the
cerebrospinal nerves. The question then arises why a subluxation should affect
the smaller sympathetic and parasympathetic nerves without seemingly producing
greater harm to the extremely larger motor and sensory nerves. He answers this
by calling attention to the position of the vertebra in fixation, whose motion
may be blocked either within or beyond the normal range of motion. The latter
occurs when an articulation is forced into a compensatory movement that it
would not normally take.
This type of subluxation was frequently described in pioneer chiropractic
literature. In has been absent in more recent years because it has not conformed to the data about normal vertebral motion. Gillet contends, however,
that when such abnormal motion is forced to occur, the facets are displaced,
the intervertebral foramen is abnormally closed, the IVF contents are
impinged, and processes leading to neurologic, circulatory, and osseous degeneration in this area are formed that involve the most vulnerable tissues
first. If occurring in the thoracic spine, for example, we could have visceral
symptoms but no intercostal neuralgia associated. This could be called a
pathologic subluxation in contrast to the physiologic subluxation in which
motion is restricted within the normal range of motion. In the latter, we
would expect to find minimal compression on or stretching of the involved IVF
contents. Fixations producing sympathetic abnormalities appear to produce far
less secondary contractions in the long spinal muscles and, therefore, far
less postural distortion.
Potential Effects of the Summation of Irritation
It has been perplexing to many chiropractors of a narrow school of thought
why doctors of chiropractic using widely divergent techniques, medical
doctors, doctors of osteopathy, physiotherapists, Christian Science practitioners, etc, frequently obtain comparable results on seemingly the same types
of cases. Typical rationalizations either deny the allegations of others or
attribute the benefits achieved to suggestion or a placebo effect. Our
competitors have done the same when the benefits to our form of chiropractic
are described. Obviously, there are several factors at work during a healing
process that can be activated either directly or indirectly through a wide
variety of approaches.
Individual Responses to Adverse Conditions
Every practitioner who has been in practice for several years has seen
patients with frightful compensations that exhibit little handicap and few
symptoms. There are also those patients in whom only minor, recently acquired
fixation-subluxations produce grotesque manifestations. In each situation, the
fixation-subluxations found may be either a cause or an effect of some other
disturbing focus.
We have previously described how an articular correction made in any part
of the spine (or anywhere in the skeletal system) has an influence on the
neuromusculoskeletal system as a whole. This is especially true with partial
muscular-type fixations. Thus, the correction of an atlas fixation will have
an affect on the sacrum and possibly as distal as the feet, and the correction
of a metatarsal or sacral fixation will have an affect on the atlas. This fact
does not mean that one fixation is necessarily the cause of the remote effect;
it just means that it can be one factor within the causal picture.
There is, however, far more to consider in the analysis of the cause of
disease than articular fixations and their correction. The effects of pathogenic microbes, parasites, toxins, poisons, excessive heat or cold, malnutrition, poor habits, physical and psychologic stress, etc, should not be
overlooked. Any one of these factors can produce illness in itself, but more
frequently each plays a variable contributing share or predisposing role in
the health status of the patient at hand. See Table 1.2.
Table 1.2. Assaults of Daily Living
Type of
Stress Examples
Mental Anger Divorce
Anxiety Emotional overexertion
Changes in lifestyle Frustration
Changes in sex life Loss of a job
Constant tension Loss of social status
Death of a loved one Mental exhaustion
Depression Phobias
Physical Biomechanical microtrauma Insufficient rest or sleep
Changes in environmen Obesity
Dislocation Overexertion, prolonged
Fixation-subluxations Postural imbalance
Fracture Sprain
Homeostatic malfunction Strain
Inadequate exercise Structural distortion
Inherited impairments Surgery
Thermal Abrupt temperature changes Frostbite
Burns Heatstroke
Dehydration Temperature extremes
Chemical Caustic chemical contact Food additives
Chemical depressants Herbicides
Chemical stimulants Malnutrition
Denourished foods Pesticides
Drugs Poisoning
Endotoxins Pollution
Environmental anoxia Radiation
Exhaust fumes Toxicosis
Neural Stimulation vs Irritation
The physiologists of Europe make a subtle differentiation between biologic
stimulation and irritation. They consider stimulation to be any circumstance
that sets up a normal action or response in a tissue or function. Thus, the
sight and smell of tempting food to a hungry person does not irritate the
optic and olfactory nerves, higher CNS centers, or the salivary glands;
rather, the visual image and odor just stimulate certain tissues to act in a
normal manner that is beneficial to an individual's health and well being. It
is usually a subtle yet precise reaction, adapted to the needs of the moment.
In contrast, any situation that is dangerous to the life or integrity of a
body is considered to be irritative to the tissues responding. It is usually a
more violent reaction such as when drawing the hand away from a hot or otherwise dangerous object, but it may be subtle such as during the development of
antibodies to fight an invasion. Unfortunately, this differentiation between
stimulation and irritation is not made in North America: here biologic stimulation and irritation are considered to be synonymous.
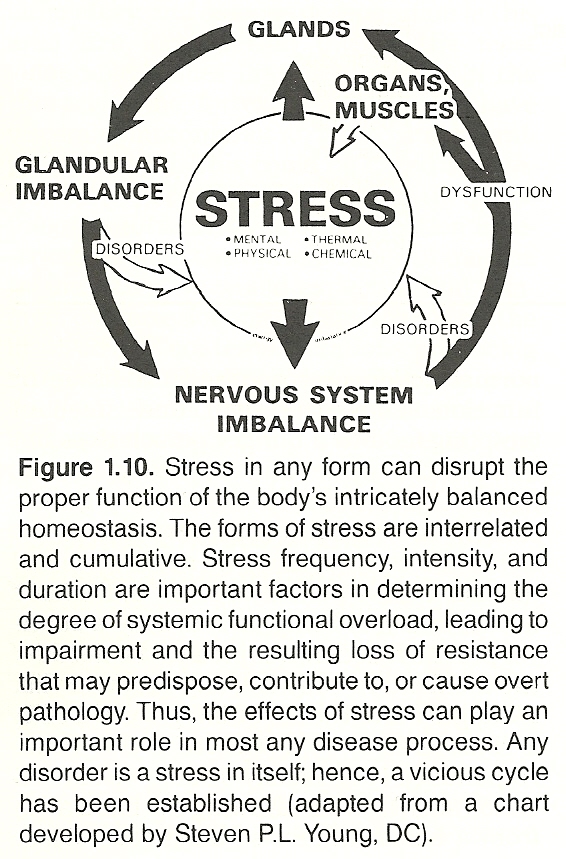
We are indebted to Hans Selye for his descriptions of the nonspecific
mechanisms that the body initiates to defend itself against danger and stress
(Fig. 1.10). Unfortunately, he did not differentiate between normal and abnormal defensive reactions in time or degree. We can, however, divide diseases
into two categories for study in which:
(2) the
manifestations reflect degeneration of diseased tissues.
In this context, we can consider a subluxation complex as being one possible effect of an excessive normal defensive mechanism. Gillet hypothesizes
that the deep short muscles of the spine were the slowest to adapt to the
upright biped posture, therefore in a constant state of alert readiness or
preparedness for danger. In this functional state, he believes that an overreaction to a threat of danger is likely and that, once the danger has passed,
a noxious self-perpetuating nerve-muscle cycle manifesting as contraction can
be established.
From another viewpoint, Gillet believes that subclinical subluxations may
so pre-irritate spinal nerves and lower their firing threshold that a minor
peripheral irritation will produce reactions far out of proportion to the
extent or severity of the lesion. In such a case, either peripheral or spinal
therapy would likely be beneficial at least temporarily until the summation
factor of circumstances detrimental to neurologic, musculoskeletal, circulatory, glandular, or psychic health arise again.
Let us suppose that an individual has a health index that is capable of
withstanding a moderate degree of debilitating factors before dysfunction
appears in the most vulnerable tissues. If smoking, drinking too much, infrequently exercising, chronic worry, having poor nutritional habits, and the
irritation from subclinical subluxations deplete his or her reserves to just
below the threshold of dysfunction, it would not require much additional
stress (in whatever manner) to so overtax his systems reserves that one or
more vital organs fail. A chill, unaccustomed exertion, a fright, loss of a
job, or a mild infection may be all that is necessary for functional collapse
to occur. Conversely, correcting existing subluxations and offering logical
counsel regarding rest, diet, and exercise, even if wise counsel is followed
only partially, may be all that is necessary to have the patient become symptom free and feeling well.
The same principles can be applied strictly from a spinal-health viewpoint. If a patient's health index is being depleted from cervical, pelvic,
and some extraspinal fixation-subluxations and manifesting as neuromusculoskeletal complaints in tissues with a low threshold to stress, correction of any
one or more of these factors may be enough to make the patient symptom free
and feeling well.
In discussing this concept with students, Gillet admonishes that "truth is
always complex; all generalizations are false, including this one."
The Hereditary Factor
Patients who are born into families whose members have lived long lives
for generations often appear to come into this world with an intrinsic genetic
makeup for longevity in spite of some adversities that would lead to the early
death of another. Many extremely heavy drinkers and smokers who overeat and
avoid exercise long outlive their doctors who neither drink or smoke, are
careful in their diet, and exercise frequently. Population statistics are useless in predicting the actions and reactions of an individual. We must learn
to deal with the patient and circumstances at hand not on our subjective
expectations, regardless of how valid they might be when related to humanity
as a whole.
The Psychic Factor
When a patient enters a doctor's office, he or she does so for two
reasons: the disorder existing and the disorder feared. Both must be treated
and treated with skill, compassion, thoroughness, and confidence. Also, it
should not be forgotten that:
(2) psychotherapeutic suggestion designed to enhance the
patient's hope in achieving rational goals are two therapeutic components in
every act of healing, whether it be chiropractic, medical, or whatever.
DIFFERENTIATING JOINT DYSFUNCTION FROM JOINT DISEASE
Primary joint dysfunction is usually the product of intrinsic joint stress
that occurs at an unguarded moment when the joint is active within its normal
range of motion. Another cause is that of extrinsic joint stress following a
definite but minor trauma and often classified as sprain and/or strain.
Secondary joint dysfunction is often overlooked in traditional medicine.
Yet joint dysfunction is, according to Mennell, "the most common cause of
residual symptoms after severe bone and joint injury and after almost every
joint disease when the primary pathological condition has been eradicated, has
healed, or is quiescent." Immobilization after surgery, immobilization from a
fracture cast even if the fracture is far from a joint, and immobilization
from a taped sprain all cause residual symptoms of joint dysfunction. Such
symptoms also follow joint inflammation or resolution of systemic joint
disease with or without internal adhesions. When joint dysfunction causes
residual symptoms after so-called joint disease recovery, the symptoms change
from those of joint disease to those of joint dysfunction; ie, during the
active process, rest increases joint pain and stiffness. During the residual
dysfunction, rest relieves and action aggravates the pain. These points should
be brought out during the case history.
Specific features elicited in the history can point directly to certain
diseases. For instance, migrating joint pain following systemic illness
suggests rheumatic fever. A tubercular joint is often a single joint offering
mild complaints yet associated with marked muscle atrophy. An acute gonococcal
joint presents a single acutely painful joint that is protected by the patient
as if it were a boil. Hemarthrosis has a history of trauma and is characterized by slight but rapid swelling from the blood pool; the joint is hot and
acutely painful. Synovitis may also have a history of trauma, but the swelling
due to excess synovial fluid may not occur for many hours. The joint may feel
warm rather than hot, aching rather than acutely painful.
In the hand(s), the location of joint involvement offers a general rule
that aids the diagnostic process:
(2) rheumatoid arthritis involves the proximal interphalangeal joints, and
(3) osteoarthritis affects the distal interphalangeal joints.
Mennell
feels that osteoarthritis by itself does not cause joint pain; rather, he pro-
jects that the pain is from the associated joint dysfunction rather than the
disease process itself.
The key history points of primary joint dysfunction are:
(2) it usually follows stress at some unguarded
joint motion,
(3) the pain is limited to one or adjacent joints,
(4) the pain
is aggravated by movement and usually is at some particular area of motion,
(5) rest relieves the pain and doesn't produce stiffness, and
(6) marked
swelling or warmth is not associated.
Keep in mind that while the major problem may be of joint dysfunction,
persistent pain following normally adequate treatment may show the presence of
a secondary low-grade asymptomatic infection or irritation in spite of blood
reports to the contrary. In such cases, suspicion should be directed toward a
distant focus of infection such as the gastrointestinal or genitourinary
tracts, the teeth, sinuses, or tonsils. In food preparation, adequate cooking
heat will kill pathogenic bacteria, but it has little affect on toxins and
spores.
In summary,
(2) usually one joint is involved in the major complaint,
(3) joint swelling is not associated,
(4) the onset is sudden,
(5) the pain occurs when doing the same action the same way, and
(6) the pain is not relieved by aspirin.
PRACTICING THE MODERN SUBLUXATION COMPLEX PARADIGM
In the modern context, there are two categories of significance in the
rationale of joint manipulation:
(2) the hypomobile
(restricted, fixated) state, which requires mobilization to return the joint
to normal function.
The objective of studying motion palpation and the related concepts of
dynamic chiropractic is to know with confidence
(2) when
to adjust,
(3) why adjust,
(4) how to adjust, and
(5) how often to adjust.
If a fixation palpates as being completely cleared on one visit and is
found to recur on the subsequent visit, it should not be readjusted. Rather,
its cause (a primary fixation elsewhere) should be sought. If, however, the
fixation does not clear completely during the office visit, it should be
adjusted on the next and subsequent visits until full mobility is achieved.
[See Clinical Comment 1.6]
DR. FAYE'S CLINICAL COMMENT #1.6
PERTINENT BIOMECHANICAL TERMINOLOGY
Movement Terms
Degrees of Freedom.
Vertebrae have six degrees of freedom (ranges of
motions); ie, translation along and rotation about each of three orthogonal
axes. Any motion in which an object may translate to and fro along a straight
course or rotate one way or another about a particular axis equals one degree
of freedom. For example, joints with one axis have one degree of freedom to
move in one plane (eg, pivot and hinge joints). Joints with two axes have two
degrees of freedom to move in different planes, and joints with three axes
have three degrees of freedom to move in all planes (eg, ball-and-socket
joints).
Range of Motion (ROM). ROM refers to the difference between two points of
physiologic extremes of motion. Rotation is measured in degrees. A vertebra
has six degrees of freedom as it moves in three-dimensional space; eg, translations along and rotations about each of the three cardinal axes (x, y, and
z). If passive distraction is considered a motion, seven degrees of freedom
exist.
Translation.
Linear motion that occurs when all parts of an object at a
given time have the same direction of motion about a fixed point is called
translation. This commonly occurs in a train moving along a track, the body
moving as a whole during gait, or a facet that glides or slips across a relatively fixed surface. Translation is measured in millimeters.
Coupling.
Coupling is a motion of translation or rotation occurring along
or about an axis as an object (eg, a vertebra) moves about another axis.
Instantaneous Axis of Rotation (IAR).
The IAR is that fixed point which
does not move but about which rotation occurs. It can exist inside or outside
the object moving and is subject to change at any given instant.
Kinetics.
Kinetics is the study of the rate of change of a specific factor
in the body that disregards the cause of the motion; ie, the study of the
relationship between a force acting on a body or body segment and the changes
produced in body motion. Kinetic actions are expressed in amounts per units of
time.
Kinematics.
Kinematics is the complex study of motions of body parts and
forces causing motion (with emphasis on displacement, acceleration, and velocity) that is mainly the result of muscle activity.
Closed Kinematic System.
This phrase refers to a series of body links or a
chain of joints in which segments are interdependent on each other for certain
movements in order that each joint can function properly in a coordinated
movement; eg, the movement of the first costotransverse joint necessary for
the cervical spine to extend and laterally flex.
Orthogonal Coordinates.
These coordinates are points of position described
around three axes (x, y, and z). Typical vertebral motions and their coordinates are shown in Table 1.3.
Table 1.3. Vertebral Movements and Their Coordinates
Motion Coordinate
Flexion + X
Extension X
Right rotation Y
Left rotation + Y
Right lateral flexion + Z
Left lateral flexion Z
Flexion and Extension.
Generally, when the joint angle becomes smaller
than when in the anatomical position, it is in flexion. For example, when the
elbow is bent, it is flexed. The opposite of flexion is extension. Thus, when
the elbow is straight, it is extended. Most joints are able to flex and
extend. When motion exceeds the normal range, it is called hyperflexion or
hyperextension; eg, as in instability of the elbow or knee.
Abduction and Adduction.
When a part is farther away from the midline than
it is in the anatomical (zero) position, it is in abduction. The opposite of
abduction is adduction. Abduction and adduction occur at the shoulder, metacarpophalangeal, hip, and metatarsophalangeal joints.
Elevation and Depression.
Raising a part from its normal (zero) position
is called elevation. Depression means to lower a part from its normal position. Good examples of both can be seen in the shoulder.
Circumduction.
Movement of a bone circumscribing a cone such as at the
shoulder or hip is called circumduction. Such motions usually comprise at
least flexion, extension, abduction, and adduction.
Rotation.
If a bone of a joint is capable of angular motion or turning on
its longitudinal axis (spinning), the motion is called rotation. The motion of
turning an anterior surface of a part toward the midline of the body is called
inward or internal rotation. The motion of turning out is called outward or
external rotation. The axis may be located outside or inside the rotating
body. The classic example of internal-external rotation is at the shoulder.
Pronation.
The word pronation refers to the act of assuming the prone
position or the state or condition of being prone. When applied to the hand,
it refers to the act of turning the hand backward, posteriorly, or downward by
medial rotation of the forearm. When applied to the ankle or foot, it refers
to a combination of eversion and abduction movements taking place in the tarsal and metatarsal joints that result in lowering the medial margin of the
foot and thus the longitudinal arch.
Supination.
Supination is the opposite of pronation. It is the act of
turning the palm forward or upward or of raising the medial margin or longitudinal arch of the foot. Pronation and supination movements are seen at the
forearm (rotation of forearm between the wrist and elbow, palm turning up or
down, respectively) and in the foot. However, inversion and eversion are
better terms to use for actions of the foot than pronation and supination.
Dorsiflexion and Plantar Flexion.
Backward flexion or bending such as of
the hand or foot is called dorsiflexion; movement toward the dorsal surface.
Plantar flexion or palmar flexion is the opposite of dorsiflexion: movement
toward the plantar surface or palm. In the hand or foot, the midline is an
arbitrary line drawn through the middle finger or toe. Dorsiflexion movements
are seen at the ankle and wrist, toes and fingers.
Inversion and Eversion.
A turning inward, inside out, or other reversal of
the normal relation of a part is called inversion. Inversion is a type of
adduction of the foot where the plantar surface is turned inward relative to
the leg. Eversion is the opposite of inversion, referring to a turning outward
of a part. Eversion of the foot means to turn the plantar surface outward in
relation to the leg.
Arthrokinematic Terms
Roll.
The term roll refers to movement in which points at intervals on a
moving joint surface contact points at the same intervals on an apposing surface.
Slide.
When one bone slides over another with little rotation or angular
movement, the action is referred to as a sliding motion; eg, carpal motion. It
is motion in which a single contact point on a moving articular surface contacts various points on the apposing surface.
Spin.
Any rotational, sliding movement in which a bone moves but its
mechanical axis remains stationary is called a spin. In the shoulder, for
example, spin is accomplished by flexion combined with some abduction because
the glenoid cavity faces slightly forward. With spin, one half of the articular surface slides in one direction, while the other half slides in the
opposite direction; ie, the moving joint surface rotates about some point on
the apposing articular surface.
Impure Swing.
This is a type of motion in which the mechanical axis
follows the path of an arc about an appositioned ovoid surface of a joint.
Pure (Chordate) Swing. The term pure swing refers to movement of a bone in
which an end of the mechanical axis traces the path of a chord about the ovoid
formed by an appositioned joint surface.
Conjunct Rotation.
This motion refers to the element of spin that accompanies impure swing or the rotation that may occur with a succession of
swings.
Compression.
The approximation of joint surfaces is called compression;
eg, motion occurring when joint surfaces are moving toward a packed or jammed
position.
Distraction.
This term refers to separation of joint surfaces, usually by
traction.
Accessory Movements.
These are secondary movements that are necessary for
a primary motion to occur. They occur with most all joint movements. Secondary
movements may include such actions as rolls, slides, spins, distractions,
and/or compressions. They usually occur to prevent undue articular cartilage
jamming or capsule stress. Lateral rotation of the tibia during extension of
the knee is a typical example.
Notation Symbols Used in Motion Palpation
See Figure 1.11.
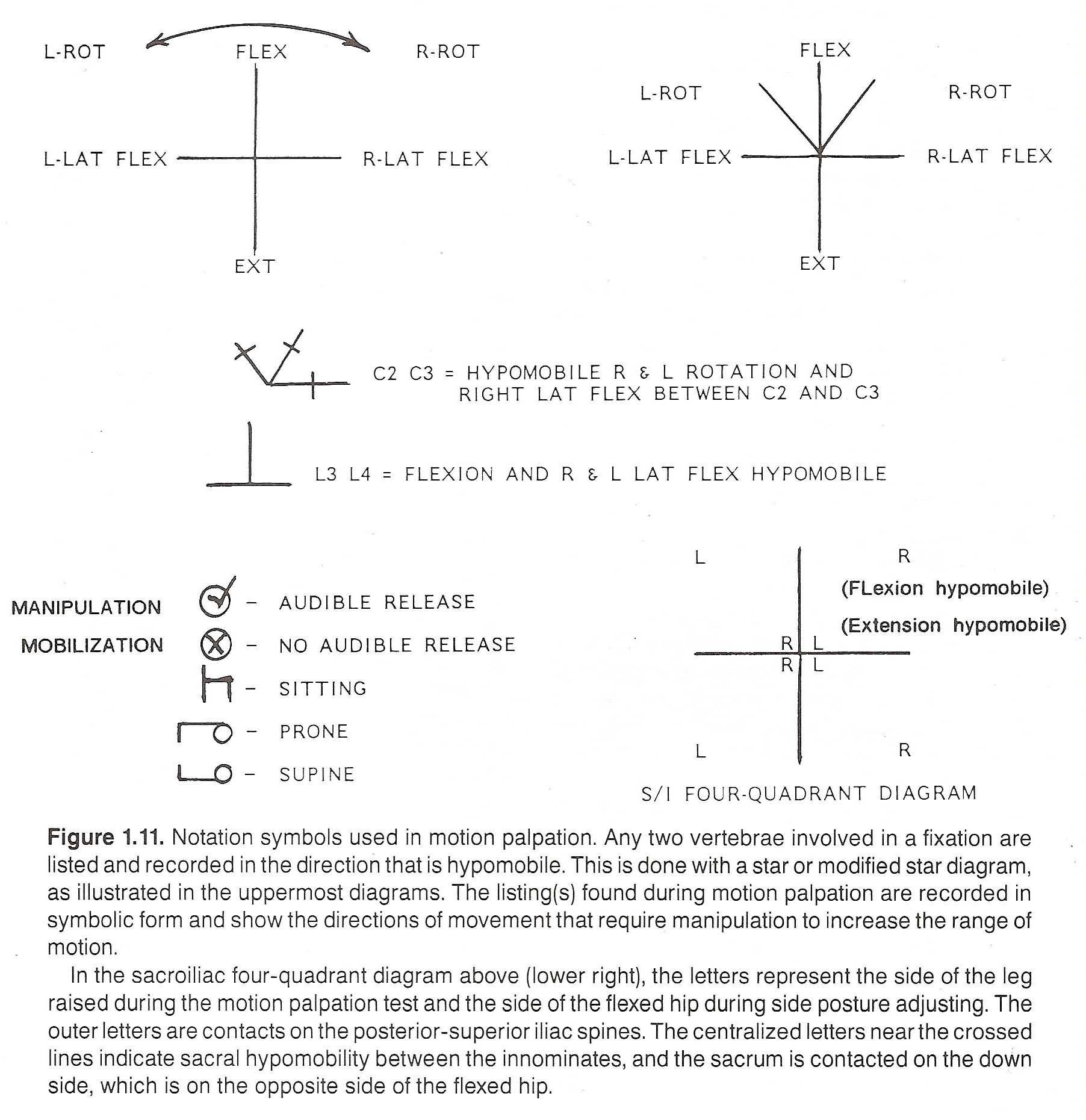
FUNDAMENTALS OF CHIROPRACTIC ADJUSTMENT TECHNICS
This section will attempt to briefly define certain general underlying
principles that underlie most all chiropractic adjustive technics, yet few
apply in all instances. These principles must be amended to the situation at
hand and the individual making the application. For example, technics must be
adapted to the size, strength, and skill of the doctor; the age, sex, health
status, and pain tolerance of the patient; and the type of adjusting table
used. Obviously, a doctor of relatively short height treating a senior citizen
on a high table may find difficulty in applying the same contact or technic
that might be applied by a tall doctor treating a lean young adult on a low
table. The variables that can arise are too numerous to list, and each must be
adapted to when encountered as conditions and personal skill permit.
A technic is only a method, one method of many, that must be adapted to
the situation at hand, clinical judgment, and personal preference. This is
true for those technics described in this text or within any other book or
seminar.
Background
The goal of any therapy must be based upon a rational hypothesis. Accord-
ing to its founder, the primary objective of chiropractic therapy is to
restore normal "tone" to the nervous system. This goal has not varied over the
years, but the primary and secondary methods (technics and techniques) used to
achieve this goal have undergone and will continue to undergo constant refinement. This is true for the therapeutic procedures used within all health-care professions. Although some practitioners achieve this by "nonthrust" means
(eg, the application of somatosomatic reflexes), objectives are generally
achieved by dynamic manual articular mobilization unless such a technic is
contraindicated in a specific situation.
Terminology
The terms technique and technic are generally considered to be synonymous
outside the profession of chiropractic. In chiropractic, however, the term
technic has been historically restricted to the application of a manually
applied adjustive force, while the term technique is used in reference to the
application of any other procedure (therapeutic or diagnostic).
Chiropractic treatment or therapy should be differentiated from chiropractic technic, which is one form of treatment. Case management includes the
application of a primary method plus all ancillary procedures incorporated to
achieve the clinical objective. These ancillary procedures often include such
procedures as physiotherapeutic modalities, heat, cold, nutritional supplementation, diet control, therapeutic exercise, meridian therapy, biofeedback,
psychotherapy or other counseling, or other forms of justifiable therapy in
the most efficient manner.
Bergmann has stated that the most specialized and significant therapy
employed by the chiropractor involves the adjustment of the articulations of
the human body, especially of the spinal column, manually or mechanically,
actively or passively, for the purpose of restoring normal articular relationship and function, restoring neurologic integrity, and influencing physiologic
processes.
Although the "adjustment" has always been the foundation of chiropractic
therapeutics, few have tried to define it and most who have were met with
severe criticism.
Sandoz states that an "adjustment" is a passive manual maneuver during
which the three-joint complex (IVD and apophyseal joints) is suddenly carried
beyond the normal physiologic range of movement without exceeding the boundaries of anatomical integrity. Swezey, an allopath, refers to a dynamic
chiropractic adjustment as the high-velocity short-arc-inducing passive movement of one articulating surface over another. Few would strongly object to
either of these attempts to define the purely structural effect induced; ie,
if the objective is solely to mobilize a fixation or realign a subluxation.
Unfortunately, such purely mechanical concepts are limited; eg, they fail to
consider the induced neurologic stimulation upon the cord, root, axoplasmic
flow, and mechanoreceptors of the area and the local and remote "spillover"
effects of such stimuli.
A recent trend by some authors and editors is to lump what a chiropractor
does during an "adjustment" under the general category of spinal manipulative
therapy (SMT). This appears to be a term originated by the allied health professions for it was rarely seen in chiropractic literature before the late
1970s. Schafer is uncomfortable with such a generalization because he believes
that what a chiropractor attempts to do is far removed from the general
"mobilization" and gross "manipulation" procedures commonly conducted by
physiotherapists and many osteopaths, which typically are passive attempts to
increase a restricted gross range of movement of a joint by stretching
contractures. While the term SMT may be appropriate for a large variety of
low-velocity extraspinal adjustive techniques or the application of a
stretching maneuver to improve a joint's gross range of motion, it can be
argued that its use is a clear misnomer in most instances when applied to the
application of scientific chiropractic during spinal therapy.
The function of a robot can be explained in electrical and mechanical
terms. This is not true for the human organism. Purely biomechanical explanations will not suffice for every situation. More than 20 years ago, Levine had
the foresight to warn those who defined the chiropractic adjustment solely in
structural terms without considering the neurologic overtones involved:
"What differentiates chiropractic adjusting from orthopedic manipulations,
osteopathic maneuvers, massage, zone therapy, etc? In one sentence, it is
the dynamic thrust! The use of the dynamic thrust is singularly chiropractic. And it is the identifying feature of chiropractic techniques.
"However, chiropractic's rationale is hardly based on the fact that its
adjustive techniques are applied with a sudden impulse of force. It is the
reasons why these techniques are applied, and why they are applied in a
certain manner, that distinguish chiropractic from other healing disciplines, manipulative or not. In fact, some chiropractic techniques of
recent vintage are not characterized by sudden application. We are think-
ing of those techniques which have been named 'non-force,' though strictly
speaking, the term is a misnomer. What makes them also part of chiroprac tic is that they are designed to serve the same purpose as the dynamic
thrust, though whether they are equally efficient is a moot question."
The Articular Snap
Skilled spinal adjustments often involve the breaking of the synovial seal
of the apophyseal joints, which results in an audible "snap." While some feel
this is of little significance, most authorities feel that breaking the joint
seal permits an increase in mobility (particularly that not under voluntary
control) from 15–20 minutes allowing the segment to normalize its position
and functional relationships. Unsuccessful manipulations that result in
increased pain rarely produce an audible joint release, while successful
adjustments usually produce an immediate sense of relief (even though some
pain and spasm remain), a reduction in palpable hypertonicity, and an improvement in joint motion, and are typically followed by a gradual reduction in
symptoms.
The General Oval Posture
The original adjusting table was primarily designed to position the
patient's spine in an "oval posture" (mild flexion). In general terms, it can
be said that without an abdominal support that can be arched, it is difficult
to open the thoracolumbar foramina and facets. It also avoids postural
compression of the discs, permits free movement at the posterior articular
processes, reduces muscular tension, and enhances the corrective forces of a
properly applied adjustment. Without an abdominal support that can be lowered
and released of tension, it would be contraindicated to adjust a pregnant
woman in the prone position. Today, this primary objective of achieving an
"oval posture" has been sustained and a large number of other optional mechanical adjustments and automatic mobilization devices can be incorporated that
enhance the application of chiropractic technics. The two most important
instruments for a chiropractic adjuster are his or her hands and adjusting
table.
Contact Points and Their Options
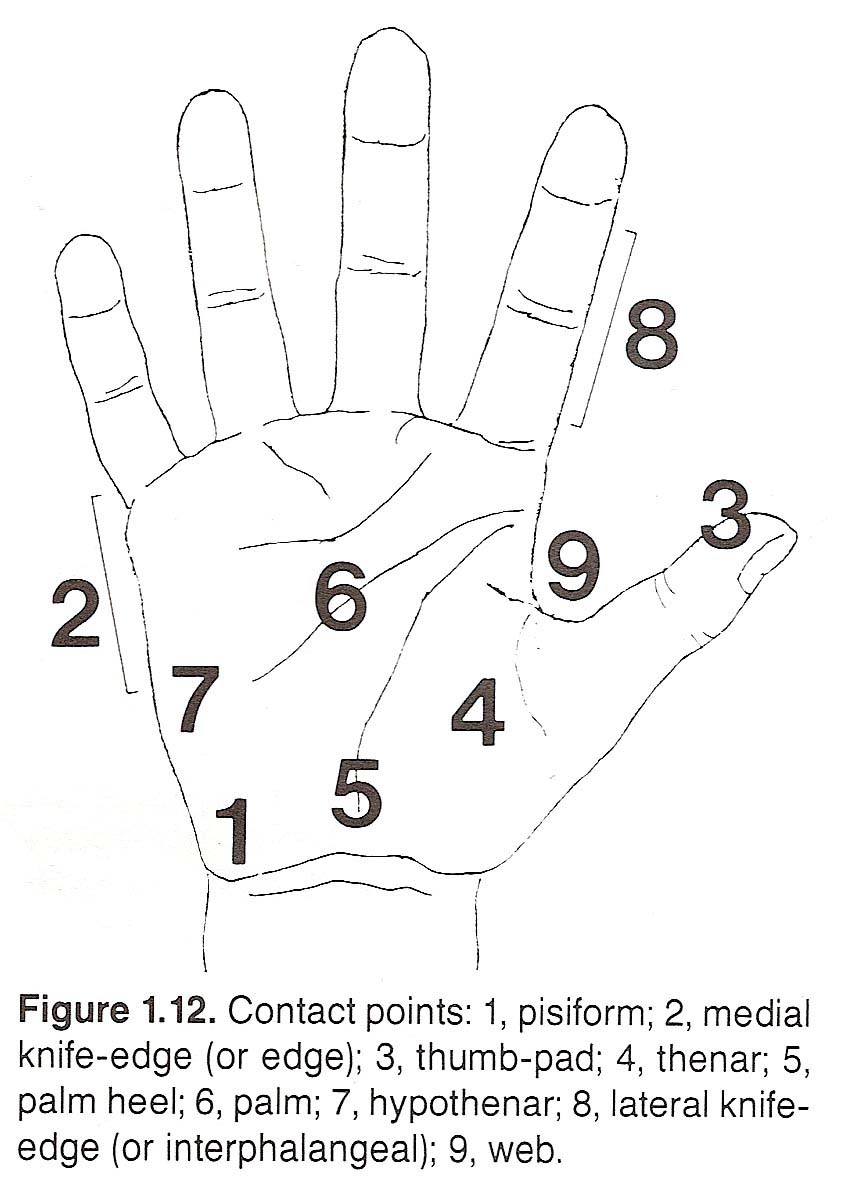
All contact points are optional at some time. For example, if the site of
contact is to be upon a thoracic transverse process, the use of a pisiform,
thenar, palm heel, or thumb contact could all meet the same objective, essentially depending on doctor-patient positions and the segmental position of
fixation.
Stance and Spinal Zones
The principles of stance and spinal zones were originally developed in
pioneer chiropractic when a recoil thrust was almost the sole type of
adjustive thrust used in chiropractic. At that time, stance and its relationship to the spinal zones were religiously adhered to. This is no longer true in
modern chiropractic, but the principles of proper stance still are applicable
in the delivery of recoil and other types of adjustive thrusts. Proper stance
allows the line of drive to be delivered in the most efficient direction.
The term spinal zones refers to four zones of the spine: Zone One, T2–L3;
Zone Two, C6–T1 and L4–L5; Zone Three, C2–C5; and Zone Four, the atlas.
Some classic stances for Zone One are shown in Figure 1.13.
Table Height
It has often been stated that the ideal adjusting table height is 18
inches for an adjuster of average stature. Of course, other variables would be
the thickness of the patient and the type of adjustment to be given. If the
table is too high, a mechanical disadvantage occurs. If too low, overstress on
the adjuster's spine results when several patients must be treated.
Securing the Contact (Active, Nail) Hand
Precautions should always be taken when applying an adjustment to avoid
slipping and pounding, as both can bruise the patient, induce unnecessary
pain, and result in an inefficient correction attempt. Slipping results from
not having the contact point properly anchored. Pounding is generally produced
by administering an adjustment when the contact is lifted from the patient's
skin just prior to applying the adjustive force or delivering a recoil adjustment when the elbows are not completely relaxed.
As an example of proper contact, the following describes anchoring the
pisiform to deliver a recoil thrust: Once the vertebra to be adjusted has been
located, the index finger of the palpating (nonactive) hand comes to rest on
the exact point where the contact will be taken. The patient's skin is then
drawn taut in the direction of drive. Next, all fingers except the palpating
finger are withdrawn and the wrist of the palpating hand is dropped or
lowered. In applying contact with the active hand, the wrist of the nail hand
is extended and the fingers are flexed to form an arch. The fingers of the
nail hand should contact the patient's skin first, drawing the skin further
taut to insure a secure (anchored) contact. The pisiform contact (nail point)
is then slid into the exact position previously occupied by the palpating
(pointing) finger, while simultaneously withdrawing the palpating finger. The
higher the arch of the active hand, the smaller the contact point at which the
force of the adjustment will be concentrated. This may or may not be an advan-
tage.
The palpating hand is then used to reinforce and further stabilize the
active hand. This supporting hammer hand is placed over the contact hand (nail
hand) during recoil thrusts. The fingers of the hammer hand grasp the wrist
and lower forearm of the contact hand so that the pisiform of the hammer hand
is directly over the pisiform of the nail hand.
Direction of Drive
The direction of drive should be against (through) the fixation, in the
direction of blocked mobility, and in line with the articular plane. As in any
generality, there are a few exceptions to this rule that will be described in
subsequent chapters.
Movement of the segment being adjusted is determined by the direction of
drive and the plane of articulation. To understand this, let us take as an
example a midthoracic vertebra whose apophyseal joints have a plane of articulation almost at a 45° angle. A P-A force directed against both transverse
processes will move the segment anteriorly and superiorly. A P-A force
directed against the right transverse process will rotate the vertebra in a
counterclockwise direction (anterosuperiorly on the right, posteroinferiorly
on the left) while a P-A force applied against the left transverse process
will rotate the segment in a clockwise direction (anterosuperiorly on the
left, posteroinferiorly on the right).
If the contact is taken on the left side of the spinous process and a
force is delivered toward 2 o'clock, the vertebra will rotate in a coun-
terclockwise direction, and vice versa if the contact is applied against the
contralateral side of the spinous process.
A spinous process contact taken in the midline or a double transverse contact will flex the vertebra if a P-A force is delivered and the subjacent
segment is stabilized. However, if the superior segment is stabilized and the
inferior segment is forced to extend, the same intersegmental motion is
achieved. Once the mechanical principles behind this concept are grasped,
there need be little argument in the effectiveness of one technic over
another. Likewise, a P-A thrust against a right transverse process or a thrust
against the left side of the spinous process will both rotate the vertebra in
a counterclockwise direction. The choice of contact is solely a matter of
clinical judgment and personal preference. The direction of drive, however, is
not optional if the best mechanical advantage is to be assured. The direction
of drive is determined by the site of fixation.
Different Types of Adjustive Technics
Thrust technics applied to an articulation can be divided into two categories: low-velocity technics (LVTs) and high-velocity technics (HVTs), and
each has various subdivisions depending upon the joint being treated, its
structural-functional state, and the primary and secondary objectives to be
obtained. The term adjustment velocity refers to the speed at which the
adjustive force is delivered.
In either low-velocity or high-velocity technics:
Low-Velocity Technics (LVTs)
In the category of low-velocity adjustments fall the many applications
that apply slow stretching, pulling, compression, or pushing forces. Sustained
or rhythmic manual traction or compression and procedures to obtain proprioceptive neuromuscular facilitation (PNF) are typical examples. Many of the
leverage techniques advocated by Spears, Cox, Markey-Steffensmeier, and others
to reduce IVD protrusions and functional spondylolisthesis can be placed in
this category.
High-Velocity Technics (HVTs)
Within the category of high-velocity adjustments fall the many applications of classic dynamic-thrust (direct, rotary, or leverage) chiropractic
adjustment technics that are applied to a vertebra's transverse or spinous
process or a lamina, with various degrees of counterleverage and/or contralateral stabilization. Contact pressure is usually firm, if the underlying
tissues are not acutely painful, when the contact is to be maintained at a
specific point and the thrust delivered in a precise direction.
The objective of almost all HVTs is to release the fixated articulation
(increase joint mobility). How this is achieved has not been specifically
determined because more is involved than the application of a mechanical force
against a resistance. The most common theories are briefly described below:
(2) are
stimulative to the neurons involved, resulting in increased short-term neural
and related endocrine activity; and
(3) set up postural and muscle-tone-normalizing cerebellar influences via the long ascending and descending tracts.
Indirect (Functional) Approches
Manual mobilization and thrust techniques are direct approaches to
relieving articular fixations. Indirect functional approaches are often used
when the cause for fixation has been determined to be essentially muscular in
origin or when any form of manipulation would be contraindicated. Within this
category fall many manual light-touch cutaneous reflex techniques, triggerpoint therapy, electrotherapy, transverse massage, traction, therapeutic
vibration, isometric and isotonic contraction, etc. It is theorized that these
procedures produce much of their effects because of their influence on the
gamma-loop system and/or by the superiority of mechanoreceptor input upon
nociceptive input.
Different Types of Adjustive Thrusts
Impulse Thrusts
Faye describes an impulse thrust as coming from the diaphragm, like
coughing or spitting. The hands adopt a preset tension in the direction of the
impulse, and the impulse is characterized by a high-velocity low-depth thrust.
Recoil Thrusts
A thoracolumbar recoil adjustment delivered to a patient in the prone
position should not be applied on a firm table. Injury to the patient's chest
or abdomen may result because of the velocity and force associated with this
type of thrust. The table should have a spring support in which the tension is
released, yet there must be resistance under the thighs and upper thorax of
the patient.
The classic recoil thrust, stated Firth, is applied against a spinous process in Zone One. After the contact has been accurately taken and secured, the
correct stance must be assured and the elbows must be completely relaxed. At
the instant of maximum patient exhalation, the adjuster's extensor muscles of
the arms and pectorals are suddenly and simultaneously contracted. As the
elbows are in line with each other and in the same plane, this spasmodic-like
contraction will adduct the elbows and produce the thrust. So that the force
of the adjustment will not go in the opposite direction (ie, toward the
ceiling), the adjuster must contract the abdominal, thoracic, and neck muscles
at the same time the adjustment is delivered. This will maintain a rigid trunk
and the adjuster's body weight will concentrate the force upon the spinous
process being adjusted.
The force of the adjustment should be applied equally with both arms at
the same instant after the adjuster positions the trunk so that the force of
the adjustment will be applied in a straight line from the episternal notch to
the point of contact. The proper position, therefore, is to have the episternal notch directly over the point of contact. Another factor of importance is
for the adjuster to position the elbows at right angles to the line of drive
and bent only to the extent that allows the entire force of the adjustment to
be delivered in a short, swift manner. Immediately after the adjustment is
delivered, the adjuster's hands should "recoil" away from the patient's spine.
Body Drop Thrusts
A body-drop thrust is usually associated with Carver's technic, as described by Beatty. The adjuster centers trunk weight over the contact hand(s)
and raises the body between the shoulders using straight arms. The adjuster's
trunk is then allowed to drop to apply a short sharp impulse, and the force is
delivered through the straight arms. This method is not to be confused with
that of dropping the body by bending the knees as is occasionally used in lumbar side-posture adjusting. The Carver body drop must be used cautiously with
children, the elderly, osteoporotics, etc.
Leverage Moves
The term leverage move refers to the use of counterpressure or contralateral stabilization. It is applied to prevent the loss of applied force,
secure the most work with the least amount of energy expenditure, and concentrate the movement or force at the directed point of contact. Only enough
counterpressure is used to balance the force of the adjustive thrust.
Multiple Thrusts
The objective of multiple thrusts is to permit a gradual increase in
force, prolong the relief on compressed discs and articular cartilage, allow
time to compensate for the applied force, and permit the application of a
force that can be equal to or greater than that used in a single thrust, thus
reducing patient discomfort.
A specific example of a multiple-thrust technic would be the application
of Spears' double-transverse contact, which is applied to the spine with thenar contacts in a deep, low-velocity, alternating, rhythmic fashion to obtain
patient relaxation and to stretch perispinal and intersegmental adhesions and
other tightened tissues prior to more specific spinal therapy. It has been
described as a "down light, down heavy, and down deeper" multiple thrust in
which each nonjerky thrust (without retraction) applies progressive pressure
after tissue adaptation.
Extension Thrusts
The term extension thrust should not be confused with that for an extension fixation. An extension (distraction) or separation of joint surfaces and
elongation of shortened soft tissues, states Beatty, should be a component of
every thrust so that articular pressure is reduced to a minimum at the moment
of joint movement. In this manner, articular friction with its accompanying
trauma and pain will be reduced and taut tissues contributing to the fixation
will be stretched. Instruction in adding intersegmental traction to all adjustive procedures was a fundamental principle in pioneer chiropractic.
Rotatory Trusts and Rotatory Breaks
A rotatory thrust, with accompanying joint distraction, is administered
for the purpose of correcting either local or area rotatory fixations. A rotatory break, commonly applied in the cervical area, is the addition of a
lateral force on the contralateral side of an accompanying lateral flexion
fixation (eg, as in unilateral disc wedging along the concavity of a scoliosis).
Test Thrusts
Test thrusts are mild preliminary thrusts applied before the actual corrective thrust is delivered. They have a twofold purpose: first, to acquaint
the adjuster with the structural resistance present and patient response to
the pressure applied; second, to acquaint the patient with what to expect.
Different Approaches to Adjusting
Most all chiropractic adjustive technics have the common objectives of
freeing restricted mobility and releasing impinged or stretched nerves. Added
factors are the expansion or compression of abnormal IVFs and IVDs, the
elongation of shortened tendons and ligaments, and the release of adhesions.
General Adjusting
General adjusting means nonspecific adjustments applied in different
general areas of the spine. Such general adjustment are usually applied in
postural distortions (eg, scoliosis, lordosis, kyphosis) to affect groups of
vertebrae, muscles, and ligaments rather than specific segments. Many practitioners apply a general adjustment to relax the patient before adminstering
specific adjustments.
Specific Adjusting
Specific adjusting means to deliver an adjustment to a specific vertebrae
to alter specific symptomatology.
The biomechanical objective in specific chiropractic adjustments is to
restore motion throughout the active, passive, and paraphysiologic range of
motion (refer to Fig. 1.5). Because of the dynamic forces involved, such techniques must carefully consider the exact geometric plane of articulation
(normal or abnormal), asymmetry, the force magnitude to be applied, the direction of force, torque, coupling mechanisms, the state of the holding elements
(eg, spastic muscles, articular fixations, stiffness and damping factors), the
integrity of the check ligaments (eg, stretched, shortened), and any underlying pathologic processes (eg, infectious, neoplastic, sclerotic, arthrotic,
osteoporotic) of the structures directly or indirectly involved. As local
tissue temperature, trabeculae arrangement, density, elasticity, flexibility,
plasticity, nutrition, etc, are variables that affect the material properties
of tissues, these factors must also be considered. The application of any
clinical procedure without consideration of the cause-and-effect forces anticipated is not within the confines of scientific chiropractic.
It can generally be stated that joints and nerves become painful only when
nociceptors are stretched, compressed, or chemically irritated. In adjusting
acute lesions, proper analysis consists of the localization of fixations as
well as the determination of which of these conditions exist to produce the
nociceptive input experienced by the patient in pain.
Major Adjusting
Major adjusting refers to the correction of a priority motion unit to
relieve a presenting complaint. Once this major (primary) consideration has
been corrected, the next motion unit in importance to the patient's condition
becomes the major.
Bibliography
Baltzell LG, Mackey RH (eds): Firth's Technic Notes. Publishing data not shown,
1967, pp 7-11, 34-40. Distributed by National College of Chiropractic.
Beatty HG: Anatomical Adjustive Technic, ed 2. Denver, published by author,
1939, pp 25-39, 133-186.
Bergmann T: Integrated chiropractic methods. Compilation of notes presented to
the convention of the Oklahoma Chiropractic Association; April 23, 1983; in
cooperation with Northwestern College of Chiropractic.
Burns L, Chandler LC, Rice RW: Pathogenesis of Visceral Disease Following Vertebral Lesions. Chicago, American Osteopathic Association, 1948, pp 11-27.
Cassidy JD, Kirkaldy-Willis WH, McGregor M: Spinal manipulation for the treatment of chronic low back and leg pain: an observational study. In Buerger AA,
Greenman PE (eds): Empirical Approaches to the Validation of Spinal Manipulation. Springfield, MO, Charles C. Thomas, 1985.
Chicoine EP: The place of chiropractic in sports. MPI's Dynamic Chiropractic,
6(10):14-16, May 15, 1988.
Cox JM: Low Back Pain: Mechanism, Diagnosis and Treatment. Baltimore, Williams
and Wilkins, 1985.
Dishmann R: Review of the literature supporting a scientific basis for the
subluxation complex. Journal of Manipulative and Physiological Therapeutics,
8(3):163-172, September 1985.
Elftman H: Biomechanics of muscle. Journal of Bone and Joint Surgery, 48A:363-377, 1966.
Elftman H: The action of muscles in the body. Biological Symposium, 3:191-209,
1941.
Faye LJ: Before the Consultation (Patient Education Film) [Videotape]. Dynaspine, Inc, 10780 Santa Monica Blvd, Suite 400, s Angeles, CA 90025.
Faye LJ: Before the Report of Findings (Patient Education Film) [Videotape].
Dynaspine, Inc, 10780 Santa Monica Blvd, Suite 400, Los Angeles, CA 90025.
Faye LJ: Chiropractic Subluxation Complex [Cassette tapes]. Huntington Beach
CA, Motion Palpation Institute, 1986, tapes 1 and 2.
Faye LJ, et al: Spine II: Motion Palpation and Clinical Considerations of the
Cervical and Thoracic Spine. Huntington Beach, CA, Motion Palpation Institute, 1986, p 3.
Faye LJ: Introduction, Rationale, Review of Clinical Examination; Causes,
Treatment, and Management of Joint Dysfunction [Videotape]. Dynaspine, Inc,
10780 Santa Monica Blvd, Suite 400, Los Angeles, CA 90025.
Faye LJ: Motion Palpation and Clinical Considerations of the Lower Extremities.
Huntington Beach, CA, Motion Palpation Institute, 1986, p 2.
Faye LJ: Patient Education [Cassette tape]. Huntington Beach, CA, Motion Palpation Institute, date not shown.
Faye LJ: Spine I: Motion Palpation and Clinical Considerations of the Lumbar
Spine and Pelvis. Huntington Beach, CA, Motion Palpation Institute, 1987, pp
2-4.
Faye LJ, Weary B, Hooper P: Motion Palpation and Clinical Considerations of
the Upper Extremities. Huntington Beach, CA, Motion Palpation Institute,
1986, p 2.
Giles LG: Leg length inequalities associated with low back pain. Journal of the
Canadian Chiropractic Association, 20(1):25-32, 1976.
Giles LG: Lumbosacral facetal joint angles associated with leg length inequality. Rheumatology and Rehabilitation, 20:233-238, 1981.
Giles LG, Taylor JR: Lumbar spine structural changes associated with leg length
inequality. Spine, 7(2):159-162, 1982.
Giles LG, Taylor JR: Low back pain associated with leg length inequality.
Spine, 6(5):510-21, 1981.
Gillet H: A definition of the subluxation. The Texas Chiropractor, February
1974.
Gillet H: Gillet of Belgium: a definition of the subluxation. Digest of Chiropractic Economics, 15(6):14-17, 1973.
Gillet H: The history of motion palpation. European Journal of Chiropractic,
31(4):196-201, 1983.
Gillet H, Liekens M: Belgian Chiropractic Research Notes. Huntington Beach, CA,
Motion Palpation Institute, 1984, pp ii-iv, 1-4, 11-35, 65-70, 78-81,
123-125; 165.
Gillet H, Liekens M: A further study of spinal fixations. Annals of the Swiss
Chiropractors Association, 4:41-46, 1969.
Gillet H: Spinal and related fixations. Digest of Chiropractic Economics,
14(3):22-24, 1971.
Glasgow EF, Twomey LT, Scull ER, Kleynhans AM, Idczak RM: Aspects of Manipulative Therapy, ed 2. New York, Churchill Livingstone, 1985, pp 109-115.
Goodman CE: Pathophysiology of pain. Archives of Internal Medicine, 143:527,
1983.
Gowitzke BA, Gowitzke MM: Understanding the Scientific Bases of Human Movement,
ed 2. Baltimore, Williams & Wilkins, 1980, pp 3-10.
Grecco MA: Chiropractic Technic Illustrated. Jarl, New York, 1953, pp 9-24, 51.
Grice AS: A biomechanical approach to cervical and dorsal adjusting. In Haldeman S (ed): Modern Developments in the Principles and Practice of Chiropractic. New York, Appleton-Century-Crofts, 1980, pp 338-339.
Homewood AE: The Neurodynamics of the Vertebral Subluxation, ed 3. Place of
publication not shown, published by author, 1981, pp 51, 71.
Illi FW: The Vertebral Column: Life-Line of the Body. Chicago, National College
of Chiropractic, 1951, pp 19-21, 25-40.
Janse J: History of the development of chiropractic concepts: Chiropractic Terminology. In Goldstein M (ed): The Research Status of Spinal Manipulative
Therapy; NINCDS Monograph No. 15, US Dept of HEW. Washington, DC, U.S. Printing Office, 1975, pp 25-32.
Kellgren JH, Samuel EP: The sensitivity and innervation of the articular capsule. Journal of Bone & Joint Surgery, 32(B):84-92, 1950.
Kendall HO, Kendall FP, Wadsworth GE: Muscles Testing and Function, ed 2. Baltimore, Williams & Wilkins, 1971, pp 18-22, 28.
Kern DP: Preface. In Gillet H, Liekens M: Belgian Chiropractic Research Notes.
Huntington Beach, CA, Motion Palpation Institute, 1984, p iv.
Kessler RM, Hertling D (eds): Management of Common Musculoskeletal Disorders.
Philadelphia, Harper & Row, 1983, pp 18-19, 75-104, 107-109, 178-181.
Kirkaldy-Willis WH: Manipulation. In Kirkaldy-Willis WH (ed): Managing Low Back
Pain. New York, Churchill Livingstone, 1983, pp 175-177.
Korr IM (ed): The Neurobiologic Mechanisms in Manipulative Therapy. New York,
Plenum Press, 1978, pp 5-6, 44-45.
Levine M: The Structural Approach to Chiropractic. New York, Comet Press,
1964, p 85.
Lieb MM: Oral orthopedics. In Gelb H (ed): Clinical Management of Head, Neck,
and TMJ Pain and Dysfunction. Philadelphia, W.B. Saunders, 1977, pp 32-71.
McCole GM: An Analysis of the Osteopathic Lesion. Great Falls, MT, published by
author, 1935, pp 10-11, 23-30.
Mennell JMcM: Joint Pain. Boston, Little, Brown, 1964, pp 1-10, 12-31, 134-136,
156-157, 167.
Palmer DD: Textbook of the Science, Art and Philosophy of Chiropractic. Portland, OR, Portland Printing House, 1910, pp 69, 77.
Rosse C, Simkin PA: Joints. In Rosse C, Clawson DK: The Musculoskeletal System
in Health & Disease. Hagerstown, PA, Harper & Row, 1980, pp 77-80.
Salter RB: Textbook of Disorders and Injuries of the Musculoskeletal System.
Baltimore, Williams & Wilkins, 1970, pp 22-26.
Sandoz R: Some physical mechanisms and effects of spinal adjustments. Annals
of the Swiss Chiropractors' Association, 6:91, 1976.
Schafer RC: Chiropractic Health Care, ed 3. Des Moines, IA, The Foundation for
Chiropractic Education and Research, 1979, pp 35, 41-44.
Schafer RC: Clinical Biomechanics: Musculoskeletal Actions and Reactions.
Baltimore, Williams & Wilkins, 1983, pp 44-46, 57-59, 74-81, 136-137,
246-247, 468.
Schafer RC (ed): Basic Chiropractic Procedural Manual, ed 4. Arlington, VA,
American Chiropractic Association, 1984, pp 5-8.
Schafer RC (ed): Chiropractic State of the Art. Des Moines, IA, American Chiropractic Association, June 1979, pp 9-13.
States AZ: Spinal and Pelvic Technics, rev ed 2. Lombard, IL, National College
of Chiropractic, 1968, pp foreword, 1-7.
Stephenson RW: Chiropractic Textbook. Davenport, IA, published by author, 1927,
pp 308, 322-325.
Swezey RL: The modern thrust of manipulation and traction therapy. Seminars in
Arthritis and Rheumatism, 12(3):326, 1983.
Tehan PJ: Functional technique: A different perspective in manipulative
therapy. In Glasgow EF, Twomey LT, Scull ER, Kleynhans AM, Idczak RM:
Aspects of Manipulative Therapy, ed 2. New York, Churchill Livingstone,
1985, pp 94-96.
Travell JG, Simons DG: Myofascial Pain and Dysfunction: The Trigger Point
Manual. Baltimore, Williams & Wilkins, 1983, pp 18-19, 21-24.
Vladef T, Hardy M: The theory of fixation points, National Chiropractic Journal, June 1945.
Watkins RJ: Subluxation terminology since 1964. ACA Journal of Chiropractic,
2(9):S65-70, 1968.
White AA, Hirsch C: The significance of the vertebral posterior elements in
the mechanics of the thoracic spine. Clinical Orthopaedics, 81:2-41, 1971.
Will TE: The biochemical basis of manipulative therapeutics: hypothetical considerations. Journal of Manipulative and Physiological Therapeutics, 1(3):
153-156, September 1978.
Wyke BD: Articular neurology and manipulative therapy. In Aspects of Manipula tive Therapy. Proceedings of Multidisciplinary International Conference on
Manipulative Therapy. Melbourne, Lincoln Institute of Health Sciences,
Carlton, Victoria, Australia, August 1979, pp 67-72.