

A Theoretical Basis For Maintenance
Spinal Manipulative Therapy For The
Chiropractic ProfessionThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Chiropractic Humanities 2011 (Dec); 18 (1): 74–85 ~ FULL TEXT
OPEN ACCESS David N. Taylor
Director, Multimed Center, Inc.,
Greenfield, MA.
A Chiro.Org Editorial
The World Health Organization defines health as being "a state of complete physical, mental, and social well-being, and not merely the absence of disease or infirmity". [ 1 ]
Given this broad definition of health, epistemological constructs borrowed from the social sciences may demonstrate health benefits not disclosed by randomized controlled trials.
Health benefits, such as improvement in self-reported quality-of-life (QOL), behaviors associated with decreased morbidity, patient satisfaction, and decreased health care costs, are reported in the following articles, and they make a compelling statement about the effects of chiropractic on general health.
This study is supported by Descarreaux's 2004 JMPT study, which concluded that:“This experiment suggests that maintenance spinal manipulations after intensive manipulative care may be beneficial to patients to maintain subjective post-intensive treatment disability levels”.
It also confirms the findings of Dr. Ron L. Rupert, in his ground-breaking 2000 JMPT article, titled:
Maintenance Care: Health Promotion Services Administered to
US Chiropractic Patients Aged 65 and Older, Part II
which found that:“The cost of health care for patients receiving MC in this study was far less than that for patients of similar age in the general population, despite the doubling of physician visits (medical plus chiropractic). The greatest difference in health care costs with patients receiving MC was in the areas of nursing care and, especially, hospital care. This reduced need for hospital and nursing home services has recently been corroborated by the research of Coulter et al.”
Coulter et al (Topics In Clinical Chiropractic 1996) performed an analysis of an insurance database, comparing persons receiving chiropractic care with nonchiropractic patients. The study consisted of senior citizens >75 years of age. Recipients of chiropractic care reported better overall health, spent fewer days in hospitals and nursing homes, used fewer prescription drugs, and were more active than the nonchiropractic patients.As part of a comprehensive geriatric assessment program, the RAND Corporation studied a subpopulation of patients who were under chiropractic care compared to those who were not and found that the individuals under continuing chiropractic care were:
- Free from the use of a nursing home [95.7% vs 80.8%];
- Free from hospitalizations for the past 23 years [73.9% vs 52.4%];
- More likely to report a better health status;
- More likely to exercise vigorously;
- More likely to be mobile in the community [69.6% vs 46.8%].
Although it is impossible to clearly establish causality, it is clear that continuing chiropractic care is among the attributes of the cohort of patients experiencing substantially fewer costly healthcare interventions.
You may enjoy other Blog postings on this topic:
Newly Published Study Confirms That “Maintenance Care” Delivers!
In Support of Chiropractic (and Maintenance) Care
General Health, Wellness, and Chiropractic Care
OBJECT: The purpose of this article is to discuss a theoretical basis for wellness chiropractic manipulative care and to develop a hypothesis for further investigation.
METHODS: A SEARCH OF PUBMED AND OF THE MANUAL, ALTERNATIVE, AND NATURAL THERAPY INDEX SYSTEM WAS PERFORMED WITH A COMBINATION OF KEY WORDS: chiropractic, maintenance and wellness care, maintenance manipulative care, preventive spinal manipulation, hypomobility, immobility, adhesions, joint degeneration, and neuronal degeneration. Articles were collected, and trends were identified.
RESULTS: The search revealed surveys of doctors and patients, an initial clinical pilot study, randomized control trials, and laboratory studies that provided correlative information to provide a framework for development of a hypothesis for the basis of maintenance spinal manipulative therapy. Maintenance care optimizes the levels of function and provides a process of achieving the best possible health. It is proposed that this may be accomplished by including chiropractic manipulative therapy in addition to exercise therapy, diet and nutritional counseling, and lifestyle coaching.
CONCLUSIONS: It is hypothesized that because spinal manipulative therapy brings a joint to the end of the paraphysiological joint space to encourage normal range of motion, routine manipulation of asymptomatic patients may retard the progression of joint degeneration, neuronal changes, changes in muscular strength, and recruitment patterns, which may result in improved function, decreased episodes of injuries, and improved sense of well-being.
From the Full-Text Article:
Introduction
The chiropractic profession continues to grow in collective thinking and progress in defining care rendered. In so doing, the profession participates in the investigation of the types of care rendered and in the translation of research into practice. Different types of care are developed from theories, clinical practice, and clinical observations and, ultimately, based on scientific evidence. However, certain types of chiropractic care are the subject of debate. This article considers the scientific basis of the commonly practiced procedure of chiropractic maintenance care and whether a hypothesis of a physiological basis can be generated to explain findings and practice.
Recent publications by the Council of Chiropractic Guidelines and Practice Parameters have summarized clinical best practices for chiropractic care and identified some of the changes that chiropractic clinicians need to make to improve care for their patient population. [1] Two articles [2, 3] give us insight into the types of care rendered. Dehen et al [2] defined the stages of chiropractic care into care for acute and chronic/recurrent conditions, and wellness care. A distinction is made between the chronic/recurrent care and wellness or maintenance care. Care for chronic/recurrent conditions is defined as medically necessary care for conditions that are not expected to completely resolve, but in which one can provide documented improvement. According to Dehen et al, wellness or maintenance care may not be defined as being “medically necessary” for a current condition. However, this type of care optimizes the levels of function and provides a process of achieving the best possible function and health.
This care includes chiropractic manipulative therapy in addition to exercise therapy, diet and nutritional counseling, and lifestyle coaching. [2] This concurred with surveys made by Danish and Swedish chiropractors who defined the purpose of chiropractic maintenance care as optimizing spinal function and decreasing the frequency of future episodes of back pain. [4] Various definitions have been provided for maintenance care:(1) “Appropriate treatment directed toward maintaining optimal body function. This is treatment of the symptomatic patient who has reached pre-clinical status or maximum medical improvement, where condition is resolved or stable”;
(2) “a regimen designed to provide for the patient's continued well-being or for maintaining the optimum state of health while minimizing recurrences of the clinical status”; and
(3) “maintenance care was offered to patients that did not improve.” [5]The current health care system more often focuses upon the doctors to fix problems that have developed over a number of years, instead of modifying patient behaviors to promote good health and prevent chronic illness. [6] Musculoskeletal conditions may be prevented by years of appropriate diet and physical activities as wellness activities. [5] Wellness is defined differently in the allopathic profession and in the retail industry. The allopathic profession defines wellness as the provision of diagnostic testing for early detection of disease processes. The retail industry often uses the term in marketing to sell products that may make the person feel better, look better, and function better, or prevent onset of aging or disease. Wellness has been defined as both a process and an outcome. [7]
Because of the multiple uses of the terms in the literature, for the purpose of this investigation, maintenance care and wellness care are used synonymously to represent the process of spinal manipulative therapy for an asymptomatic patient or a patient that has reached maximum therapeutic improvement after treatment of an acute condition, an acute exacerbation of a chronic condition, or an initial treatment regimen for a chronic condition. Some insurers have independently defined maintenance care as care provided for a stable condition without any functional improvement of the patient net health outcome over a 4-week period and further determine it as not being medically necessary. [8] Jamison [9] did a random survey of Australian and American doctors of chiropractic to obtain a global definition of maintenance care. She found that more than 90% opined that the purpose of maintenance care was to minimize recurrences or exacerbations, whereas greater than 80% responded that it would optimize the patients' health. This indicates some agreement of the opinions of the rationale for such care.
Ninety-seven percent of the American and 85% of the Australian chiropractors report using manipulative therapy as a component of the maintenance care. A combined greater than 93% also used exercise as part of the maintenance care, whereas a great majority also used patient education in eating habits and other lifestyle choices. There was a greater than 91% agreement that the musculoskeletal system was most amenable to maintenance care, whereas many also felt that maintenance care was beneficial for stress; respiratory system; gastrointestinal system; and, to a lesser degree, cardiovascular system. This was all apparently based on clinical observation, personal philosophies, and experience because only 40% of the Americans and 22% of the Australians opined that the care was supported by adequate research. [9] Rupert [10] performed a similar study of US chiropractors in 2000 and had similar results showing that 95% of chiropractors recommended maintenance care to minimize recurrences or exacerbations of conditions and 90% recommended the care to optimize the health of the patient. Again, this was in the absence of known scientific support. A study that interviewed patients and doctors regarding maintenance care noted that 96% of elderly patients who received such care believed that it was either considerably or extremely valuable. [11] The prevalence of the rendering of this type of care is again noted by Rupert [10] as contributing an average of 23% of the chiropractors' income. It is interesting to note that Sarnat and Winterstein [12] found substantial cost savings in an Independent Practice Association that used chiropractors as primary care providers despite the fact that 28% of the patients presented for wellness care and it was not uncommon for the patients to present twice a month for such care. Despite this, the US Preventive Task Force, which has been evaluating preventive health care measures for 27 years, fails to list this type of care as a preventive measure. [13]
If the chiropractic profession feels that maintenance care is important to our patients, then we need further evidence of a scientific basis of the physiological responses to this care. It has been reported that 79% of patients in chiropractic offices are recommended maintenance care and nearly half of those patients elect to receive these services. [10] The lack of third-party payment for such services in the US health care system may be a factor in how many patients elect to participate.
There are many questions surrounding maintenance care, and previous research has investigated some of these questions, [14, 15] The object of this article is to look at the available evidence for a possible physiological basis that might allow development of a theory of the reported clinical benefits of such care. Given the positive clinical reports and the current state of knowledge of manipulative therapy, it is hypothesized that a theoretical physiological framework could be developed for future research. The purpose of this article is to provide the initial bridge from the clinical observations and theories to proposed hypotheses for further investigation into the clinical meaningfulness of maintenance care.
Methods
Referencing STARLITE search strategy approach, [16] the following is outlined. The sampling strategy was purposeful to include chiropractic as the primary discipline for the defining of wellness or maintenance care. However, other disciplines were included to obtain the research regarding the physiology or pathology relative to spinal manipulation. The type of studies included were surveys of clinical practice to assess common practice and provide definitions. Laboratory studies were included to assess the known physiology and pathology. The search approach was mainly by Internet/electronic means. When open access to full text was not available through current subscriptions, further search was conducted through the local hospital subscription service. Search was conducted by subject and included titles and abstracts. Hand search was conducted regarding personally known work by various authors or to follow up on references from reviewed articles. Because this subject is one that was only recently researched, the range of years of the search was from 1970 through 2011. The search was limited to those in the English language. Because this was an interpretive narrative review, articles were reviewed for a common understanding of wellness care and maintenance care within chiropractic.
Once this was established, the search strategy inclusion criteria were used to further narrow down the search to target spinal manipulative therapy while excluding other common chiropractic therapies. The remaining literature was then reviewed for common themes of dosage and duration of care. An additional search was then conducted with the commonly established findings of spinal manipulation effectiveness. These were then reviewed for dosage and duration for onset of pathology and reversal or retardation of the pathology. Cross-referencing was then conducted between the common dosage and duration of chiropractic maintenance spinal manipulative therapy and the onset of pathologies. Reviews of abstracts were conducted; and when articles met the inclusion criteria, full-text articles were obtained whenever possible. The search and exclusion/inclusion decision making were all conducted by the sole author.
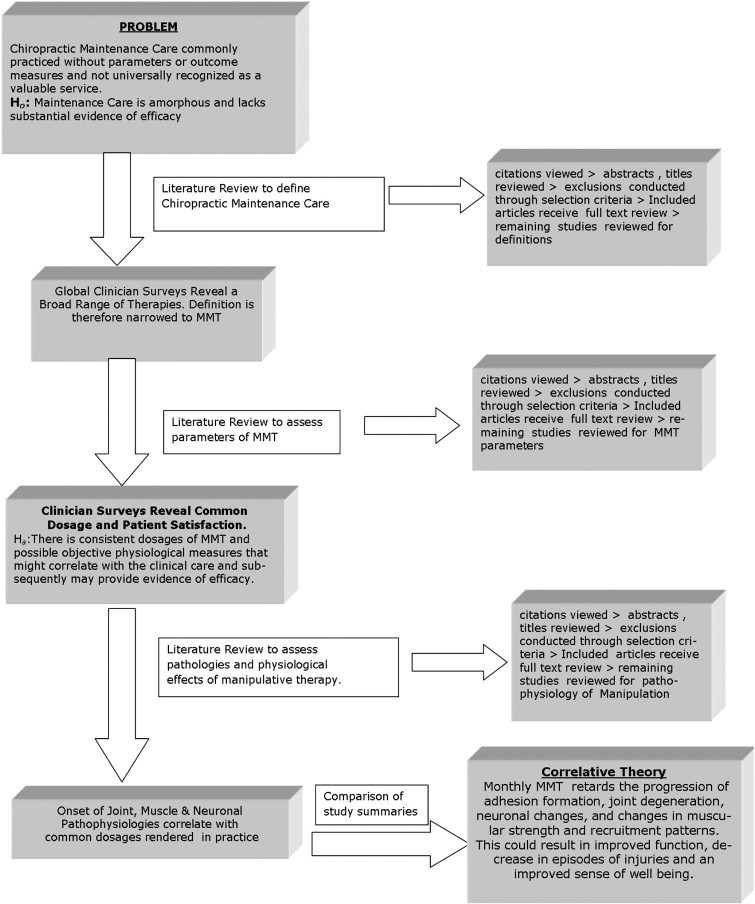
Figure 1 A search of the Electronic Medline Database was conducted through Pubmed Central; and the Manual, Alternative, and Natural Therapy Index System search was conducted through ChiroAccess. The key words and terms Chiropractic Maintenance Care, Maintenance Manipulative Care, Maintenance Manipulation, Preventive Spinal Manipulation, Spinal Manipulation Effectiveness, Maintenance, and Wellness were used in various combinations. An additional search of the same databases was performed with known related topics such as hypomobility OR immobility and adhesions, hypomobility OR immobility and joint degeneration, neuronal AND hypomobility, and neurology of hypomobility OR immobility. Boolean operators were used to narrow down the search. Further manual search from related citations and bibliographic references was conducted.
Reviews were conducted to narrow the definition of Maintenance Care in Chiropractic Practice, to assess the dosage and duration of care, and to look at physiological parameters that would relate to this care (Figure 1).
Results
Subjective clinical observations
The search terms of Spinal Manipulation AND Maintenance revealed conflicting results, with some studies published that demonstrated a lack of benefit and other studies in which benefits were noted. A 2011 study by Senna and Machaly [17] was one of the few studies on spinal manipulation for maintenance care of the chronic nonspecific low back pain patient. This was a randomized clinical trial in which 60 patients with this condition were randomized to

Table 1 (1) 12 sham treatments over 1 month,
(2) 12 spinal manipulative treatments (SMTs) over 1 month without follow-up, and
(3) 12 SMT over 1 month followed by “Maintenance Manipulative Therapy (MMT)” at a frequency of every 2 weeks for the following 9 months (Table 1).The results demonstrated that only the maintenance care group showed more improvement in pain and disability from the 1-month period to a 10-month follow-up. In fact, the group that did not receive maintenance care returned to the pretreatment levels of pain and disability. The authors concluded that long-term benefits may be derived from MMT. Hawk et al [18] performed a pilot study to look at this type of care with outcomes measured by the degree of pain, dizziness, and balance via their respective outcome measures. This was a small group of 34 total patients, which limits the statistical application to the general population. However, the randomized groups were similar to those in the study of Senna and Machaly. One group received treatment for 8 weeks, a second group received treatment for 8 weeks followed by monthly treatments for 10 months, and the third group received no treatment except for an exercise booklet. The outcomes were monitored at 1, 2, 6, and 12 months. Although there was no difference noted in balance, there was a difference in pain and dizziness. Pain was improved to a greater degree in the maintenance care group, whereas dizziness improved in both spinal manipulation groups and remained so at 1 year. They concluded that further investigation of maintenance chiropractic therapy was warranted. Unfortunately, the chiropractic care consisted of more than just spinal manipulation; so one could not draw conclusions about MMT as an isolated procedure.
Subjective clinical observationsObjective clinical findings Using the search terms of hypomobility/immobility, adhesions and degeneration revealed possible physiological abnormalities present in low back patients.
Burton et al [19] studied joint mobility in adults. This study revealed that mean mobility values of lumbar joints in younger patients were reduced by both previous and current low back trouble when compared with nonsufferers. This did not correlate with the findings in middle-aged adults with low back pain histories but did with the patients in this age group with sciatica history. The authors suggested that it was possible that aspects of increased mobility in the middle-aged adults, such as localized segmental instability or abnormal coupled motions, may be associated with an increased frequency of recurrent low back trouble. [19, 20] It is hypothesized that regular wellness/maintenance chiropractic care may correlatively be treating these abnormalities in the early stages. Subsequently, this may be preventing their progression and development of later-stage acute and chronic injuries and disease.
Objective Laboratory Findings
Changes in joint mobility
Further search of mobility changes revealed additional correlations. Cramer et al [21] used an established small animal model of spinal fixation of 3 contiguous lumbar segments (L4, L5, L6) of rats to assess fixated zygapophyseal joints at 1, 4, and 8 weeks of fixation. A total of 584 zygapophyseal joints (left and right L3/L4, L4/L5, L5/L6, L6/S1) and 1168 articular surfaces were evaluated macroscopically. They found that the longer the animals were fixed, the greater the number of osteophytes that developed. Differences found between control animals and spinal fixation animals at 1, 4, and 8 weeks were statistically significant (P < .05) both for the total number of degenerated articular surfaces per animal and for average severity of articular surface degeneration. They concluded that there appeared to be a threshold of time when osteophyte formation and articular surface degeneration become so severe that very little return to normal occurs even after a considerable length of time. Degenerative articular surface changes preceded osteophyte formation. This study demonstrated that zygapophyseal joint changes occurred following spinal fixation and that the amount and severity of degeneration are time dependent with a threshold of between 4 and 8 weeks for osteophytes and less than 1 week for articular surface degeneration. [21] These findings may provide an explanation to the anecdotal findings reported in clinical practice in which patients report increased well-being and decreased incidence of spinal complaints with once per month preventive wellness manipulation. The timing of common clinical treatment frequency at every 4 weeks correlates with the findings of the threshold of 4 weeks for irreversible degenerative osteophyte formation. In addition, he had findings that facet articular degeneration began after only 1 week of fixation. This finding correlates with the common practice pattern of progressive decreasing of the frequency of manipulation as the patients progress in recovery from an acute incident. It also indicates that even when patients present for once per month asymptomatic preventive manipulation, the process of degeneration of the articular surfaces may have already begun.
Another study by Cramer et al [22] looked at the time dependence of adhesion formation. This study monitored the onset of fibrotic adhesions over a similar period of 4, 8, and 12 weeks after joint fixation. Micrographs manifested initial synovial folds that progressed to mild adhesions in 4 weeks, moderate adhesions in 8 weeks, and severe adhesions after 12 weeks. Additional studies compared the fixated segments to nonfixated segments and noted a statistical difference in occurrence, therefore ruling out any natural process. [23] This has not been correlated with onset of symptoms in the human subjects, but it can be hypothesized that there is a period where the adhesions are forming without clinical symptoms. If this is true, then this would again support the common once per month clinical spinal examination. It has also been demonstrated that lumbar spinal manipulation gaps the facet joints. [24, 25] Although much has been written about manipulation breaking up adhesions, the correlation of this gapping to the breaking of adhesions has not yet been fully investigated. If this were to be demonstrated, then this would lend additional support for the once per month clinically recommended spinal manipulative therapy. The process of joint immobility, adhesions, degeneration, and onset of back pain would also explain the surveyed clinical opinions of the doctors in the study of Hansen et al. [14] The Nordic survey opined that the indications for maintenance care consisted of a prior history of low back pain along with a positive response to previous care.
Neurological effects
Using the search terms neuronal, immobilization, and joint manipulation also revealed possible neurological abnormalities that regular wellness/maintenance chiropractic care may be treating in the early stages and preventing their progression and development of later-stage acute and chronic injuries and disease states.
This search revealed an interesting study on the a-motor neuronal activity. Immobility was induced in a guinea pig knee joints, and a-motor neuron activity was monitored by light microscope. This revealed a progressive time-dependent shrinkage of the nuclear envelope and loss of DNA. This demonstrated progressive degeneration and loss of neuronal activity. [26] In addition, electron microscopic evaluation showed demyelination of the nerves at the level of the primary motor neuron. [26] This time dependency showed loss of neurons after only 4 weeks of immobilization and got progressively worse thereafter. Surprisingly, there was an increase in neurons following release of fixation after the 4 weeks of immobilization. This needs to be further investigated in regard to the physiological spinal joint fixation in human subjects, but does present an interesting hypothesis to resultant weakness in the related innervated muscles. Such weakness with resultant atrophy and fatty deposition of the multifidi muscles was demonstrated by Kader et al [27] when they looked at the magnetic resonance imaging (MRI) changes in these muscles and the correlation to leg pain. They also noted a time-dependent factor from normal muscles to mild, moderate, and severe muscular atrophy.
Fahim [28] took it one step further and noted in his electron microscopic analysis of extremity soleus changes in neuromuscular end plates. He found that, with only 5 days of immobilization of the knee and ankle, there was degeneration of the soleus motor end plates, in addition to the muscle atrophy. The neuromuscular junction changes consisted of nerve terminal disruption, exposed junctional folds, and postsynaptic areas that contained little or no postjunctional folds. This was a preliminary laboratory study, but then Lundby-Jensen and Nielsen [29] looked at 12 human subjects' H-reflexes of the soleus muscles with 2 weeks of immobilization of the foot and ankle. They observed that there were an increase in the amplitude and a decrease in the long latency depression of the H-reflex. This suggested that, with only 2 weeks of immobilization and disuse in humans, there were plastic changes in spinal interneuronal circuitries responsible for presynaptic control of Ia afferent sensory input to the spinal cord and affecting the a-motor neuron through decreased inhibition. [29] They were also able to reproduce this result in an upper extremity study with some further indications that it was happening at the cord level. [30]
The question then arises whether the maintenance/wellness manipulative care in clinical practice would prevent neuronal degeneration and onset of muscle weakness, or change muscular recruitment patterns and predispose the patient to injuries. It is suggested that if He's findings in guinea pigs could be found to correlate in humans, then there may also be a possibility of reversal of the neuronal degeneration and muscular weakness through manipulation and remobilization of the joint.
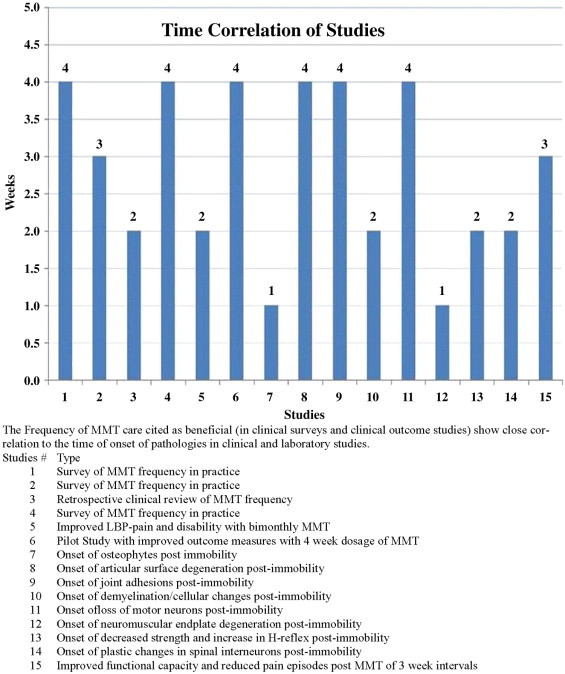
Figure 2 In summary, this narrative literature review manifested progressive physiological consequences as a result of joint immobility. When this is correlated with the biomechanical and neurological research finding of manipulative therapy, a line of reasoning arises that generates a theoretical framework for a physiological hypothesis of the basis of MMT. There appears to be a correlation of time intervals of immobility and the onset of joint adhesions, spinal joint degeneration, aberrant Ia neurological input, degeneration of the a-motor neuronal pool, motor end plate degenerative changes, and onset of muscular weakness and atrophy. This correlates with the usual clinical dosage of MMT as shown in clinician surveys in numerous countries and patient satisfaction (Figure 2). The graphic depiction clearly demonstrates that the clinical consensus of dosage of MMT has been found to be most beneficial at an average of once every 2 to 4 weeks. We also see here that it closely correlates with the studies that show onset of facet joint degeneration, neural degeneration, neuroplastic changes, and muscular atrophy and weakness at an average of 2 to 4 weeks.
It is known that manipulative care mobilizes the joint to the end of the paraphysiological joint space and theorized that this breaks up adhesions. [31] Case reports have also suggested that there is an effect on multifidus muscle strength. [32] This review has revealed evidence of the progression of the neuromusculoskeletal changes with immobility. Taking into account the neurological and biomechanical consequences of manipulative therapy, [33] it is plausible to hypothesize that monthly manipulative therapy retards the progression of adhesion formation, joint degeneration, neuronal changes, and changes in muscular strength and recruitment patterns. This could result in improved function, decreased episodes of injuries, and improved sense of well-being. This review represents a narrative of the literature that provides evidence to support the theoretical framework of the value of maintenance chiropractic manipulation and provides the basis to generate such a theory. However, the literature was not qualitatively or quantitatively evaluated. Therefore, collective evidence needs to be further evaluated. Finally, it should be noted that the conclusions represent a theory and that this theory needs further higher evidence testing to support or refute it.
Discussion
There is still ambiguity in the literature regarding the clinical benefits of maintenance or wellness manipulative care. A previous report by LeBoeuf-Yde and Hestabek [5] concluded that there was no evidence base for the indications or the nature of the use of maintenance care based on a 2008 literature review. They also point out the lack of an objective measure of the benefits. In addition, Aker and Martel [34] in their qualitative literature review concurred that there was no scientific evidence to support the claim that maintenance care improves one's health status, although anecdotal evidence from both doctors and patients is strong. A recent randomized controlled trial of monthly preventive spinal manipulation of more than 10 months' duration showed no difference in functional measures, range of motion, or visual analogue pain scales when compared with a control group of bimonthly reassurance or a combination of manipulation and home exercise. This author concluded that the premise of stating that regular treatments, designed to preserve optimum health and minimize the recurrence of clinical problems, was more likely due to interventions of reassurance, patient education, help with self-management, and active care strategies. [35] In contrast, a different study looked at the pain levels and functional Oswestry disability measures of 2 chronic low back pain groups. [36] Both received an initial 12 spinal treatments over 4 weeks. Then the maintenance care was provided to one group at a frequency of every 3 weeks for a 9-month follow-up, but not to the second group. This study found that disability remained at the lowered post 4-week level for the maintenance group but returned to the previous levels for the control group. They concluded that there were positive effects of preventive maintenance chiropractic spinal manipulation in maintaining functional capacities and reducing the number and intensity of pain episodes after the acute phase of treatment of low back pain patients. [36] This seemed to concur with the Swedish surveys of chiropractors who found consensus on providing such care to prevent relapses. [37]
There is a common thread of the time dependency noted in all the laboratory and clinical studies. The periods of onset of the anatomical and physiological changes ranged from 2 to 4 weeks. The clinical studies also provided MMT every 4 weeks and noted positive changes in the pain and disability measures. This time interval also correlates with the common recommendations found in the surveys of chiropractic physicians. Although there have been physiological measures to assess the results of manipulative therapy, studies of these measures applied to preventive manipulation have not been conducted; nor has there been any testing of physiological vs psychological contributions to the reported clinical benefits. Further investigatory studies in these areas would be able to tie together some of the laboratory and clinical findings.
In the first conference on spinal manipulation in 1977 sponsored by the National Institute of Neurological and Communicative Disorders and Stroke, Haldeman [38] presented the criteria for investigating the clinical basis of the mechanisms of manipulative therapy. These still apply today and can be paraphrased to apply to MMT.
That the application of MMT must demonstrate consistent clinical results under controlled conditions in the treatment of a specific pathologic process, organ dysfunction, or symptom complex.
That MMT demonstrates a specific effect on the musculoskeletal system to which it is applied.
That the musculoskeletal effect caused by MMT must be shown to have a specific influence on the nervous system.
That the influence on the nervous system brought about by the manipulation must demonstrate a beneficial influence on abnormal function of an organ, tissue pathology, or symptom complex. But we must be careful about presenting theory as fact. [38]
As science starts with a theory, the theory must then be investigated for validity. Currently, the theories involving MMT are evolving; and there are initial investigations that may apply to this care. In response to the beliefs, positive anecdotal findings, patient satisfaction, and historical clinical reports, the following is a response to those directives.
One cannot attribute MMT as a preventive cure-all. We must therefore look at specific conditions in which MMT may effect. It appears that the clinical opinions and the research to date have looked at the effect on low back conditions. This would be a good starting point to research the efficacy of MMT in reducing the incidence of low back injuries or the severity of the episodes. It has been theorized that there is a neurological response to the manipulation. This has included the increase in population of proprioception, stimulation of a-motor neuronal pool, and reflexogenic responses through the stretch reflex. There is now increasing research available that is confirming much of this; but further research is still warranted, especially in regard to these effects under MMT. There is initial evidence of the effect of immobility on the Ia afferent nerves, the a-motor neuronal pool, the motor end plates, and the muscular end organs. Further research should be aimed at confirming these findings in human subjects and the reversal of these effects with the application of MMT procedures. The influence on the nervous system from the manipulative therapy has been shown in the studies outlined in our literature search. Future research should look at the beneficial influence of MMT on patients with chronic musculoskeletal conditions before looking at healthy individuals. Population studies similar to those performed by Senna and Machaly [16] and by Hawk et al [17] with larger populations should give us further insight into the clinical value of MMT. In vivo assessment of neurological and musculoskeletal changes would be beneficial in providing further physiological evidence to support the recommendations of MMT.
Limitations
This study is limited in scope because it is not a quantitative analysis of the literature, nor does it qualitatively evaluate the literature reviewed. This was a narrative review to provoke thought, further debate and discussion on the topic, generate theories, and challenge future research directions.
Conclusion
The value of maintenance care must be demonstrated to substantiate use of this service and for it to be a covered service on par with other preventive care services such as annual physical examinations, colonoscopic examinations, prostate examinations in men, and mammograms in women. The purpose of this discussion was to address MMT, its clinical care, and the body of evidence and to generate theories that might further investigate evidence on the same basis as other common preventive services. Therefore, a theoretical framework was developed based on the grounded theory of the common clinical practice of MMT and its common dosage. This review suggests that there may be a correlation between clinical dosages with the time of onset of pathologies. This article aimed to enlighten the debate between the clinical theories and the scientific evidence, and between the philosophy and science of MMT, while providing a physiological hypothesis of the benefits of and direction for future MMT research.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
References:
Triano, JJ.
What Constitutes Evidence For Best Practice?
J Manipulative Physiol Ther. 2008 (Nov); 31 (9): 637–643Dehen MD, Whalen WM, Farabaugh RJ, Hawk C.
Consensus Terminology for Stages of Care: Acute, Chronic, Recurrent, and Wellness
J Manipulative Physiol Ther. 2010 (Jul); 33 (6): 458–463Farabaugh RJ, Dehen MD, Hawk C.
Management of Chronic Spine-Related Conditions:
Consensus Recommendations of a Multidisciplinary Panel
J Manipulative Physiol Ther 2010 (Sep); 33 (7): 484–492Top Moller L, Hansen M, Leboeuf-Yde C:
The Nordic Maintenance Care Program – An Interview Study on the Use
of Maintenance Care in a Selected Group of Danish Chiropractors
Chiropractic & Osteopathy 2009 (Jun 17); 17: 5Leboeuf-Yde C, Hestbaek L.
Maintenance Care In Chiropractic –
What Do We Know?
Chiropractic & Osteopathy 2008 (May 8); 16: 3Johnson C., Green B.N.
Public Health, Wellness, Prevention, and Health Promotion:
Considering the Role of Chiropractic
and Determinants of Health
J Manipulative Physiol Ther. 2009 (Jul); 32 (6): 405–412Eric G. Russell, DC
Process Versus Outcome: Challenges of the Chiropractic Wellness Paradigm
J Chiropractic Humanities 2009 (Dec); 16 (1): 50–53Blue Cross Blue Shield of Massachusetts.
Reimbursement policy and billing guidelines for chiropractic services, 2007.
Available from:
https://www.bluecrossma.com/staticcontent/review_guidelines/ Revised_BCBSMA_Chiropractic_Billing_Guidelines.pdfJamison JR, Rupert RL:
A Survey of Practice Patterns and the Health Promotion and Prevention
Attitudes of US Chiropractors Maintenance Care: Part I
J Canadian Chiropractic Association 2001 (Jun); 45 (2): 100–105Rupert RL:
A Survey of Practice Patterns and the Health Promotion and Prevention
Attitudes of US Chiropractors Maintenance Care: Part I
J Manipulative Physiol Ther 2000 (Jan); 23 (1): 1–9Rupert RL, Manello D, Sandefur R:
Maintenance Care: Health Promotion Services Administered to US Chiropractic
Patients Aged 65 and Older, Part II
J Manipulative Physiol Ther 2000 (Jan); 23 (1): 10–19Sarnat, RL and Winterstein, J.
Clinical and Cost Outcomes of an Integrative Medicine IPA
J Manipulative Physiol Ther 2004 (Jun); 27 (5): 336–347U.S. Preventive Services Task Force.
Available from: http://www.uspreventiveservicestaskforce.org/. Accessed March 2011Hansen SF, Laursen ALS, Jensen TS, Leboeuf-Yde C, Hestbaek L:
The Nordic Maintenance Care Program: What Are The Indications For
Maintenance Care In Patients With Low Back Pain? A Survey
of the Members of the Danish Chiropractors' Association
Chiropractic & Osteopathy 2010 (Sep 1); 18: 25Sandnes KF, Bjornstad C, Leboeuf-Yde C, Hestbaek L:
The Nordic Maintenance Care Program - Time Intervals Between Treatments
of Patients With Low Back Pain: How Close and Who Decides?
Chiropractic & Osteopathy 2010 (Mar 8); 18: 5Booth A.
“Brimful of STARLITE”: toward standards for reporting literature searches.
J Med Libr Assoc. 2006;94(4):421–429. e205Senna M.K., Machaly S.A.
Does Maintained Spinal Manipulation Therapy for Chronic Non-specific
Low Back Pain Result in Better Long Term Outcome?
Spine (Phila Pa 1976) 2011 (Aug 15); 36 (18): 1427–1437Hawk C, Cambron JA, Pfefer MT.
Pilot Study of the Effect of a Limited and Extended Course of Chiropractic
Care on Balance, Chronic Pain, and Dizziness in Older Adults.
J Manipulative Physiol Ther. 2009 (Jul); 32(6): 438–447Burton A.K., Tillotson K.M.
Is recurrent low back trouble associated with increased lumbar sagittal mobility?
J Biomed Eng. 1989;11(3):245–248Burton A.K., Tillotson K.M., Troup J.D.
Variation in lumbar sagittal mobility with low-back trouble.
Spine (Phila Pa 1976) 1989;14(6):584–590Cramer G.D., Fournier J., Henderson C.
Degenerative changes of the articular processes following spinal fixation.
J Chiro Educ. 2002;1:7–8Cramer G.D., Henderson C.N., Little J.W., Daley C., Grieve T.J.
Zygapophyseal Joint Adhesions After Induced Hypomobility
J Manipulative Physiol Ther. 2010 (Sep); 33 (7): 508–518Cramer G.D., Fournier J.T., Henderson C.N., Wolcott C.C.
Degenerative Changes Following Spinal Fixation in a Small Animal Model
J Manipulative Physiol Ther 2004 (Mar); 27 (3): 141–154Cramer G.D., Gregerson D.M., Knudsen J.T., Hubbard B.B., Ustas L.M., Cantu J.A.
The effects of side-posture positioning and spinal adjusting on the lumbar Z joints:
a randomized controlled trial with sixty-four subjects.
Spine (Phila Pa 1976) 2002;27(22):2459–2466Cramer G.D., Tuck N.R., Jr, Knudsen J.T., Fonda S.D., Schliesser J.S., Fournier J.T., Patel P.
Effects of side-posture positioning and side-posture adjusting on the lumbar zygapophysial joints
as evaluated by magnetic resonance imaging: a before and after study with randomization.
J Manipulative Physiol Ther. 2000;23(6):380–394He X, Dishman V.
Spinal Motor Neuronal Degeneration After Knee
Joint Immobilization in the Guinea Pig
J Manipulative Physiol Ther. 2010 (Jun); 33 (5): 328–337Kader D.F., Wardlaw D., Smith F.W.
Correlation between the MRI changes in the lumbar multifidus muscles and leg pain.
Clin Radiol. 2000;55(2):145–149Fahim M.A.
Rapid neuromuscular remodeling following limb immobilization.
Anat Rec. 1989;224(1):102–109Lundbye-Jensen J., Nielsen J.B.
Immobilization Induces Changes in Presynaptic Control of
Group Ia Afferents in Healthy Humans
J Physiol. 2008 (Sep 1); 586 (Pt 17): 4121–4135Lundbye-Jensen J., Nielsen J.B.
Central nervous adaptations following 1 wk of wrist and hand immobilization.
J Appl Physiol. 2008;105(1):139–151Haldeman S., editor.
Modern developments in the principles and practice of chiropractic.
Prentice-Hall; NJ: 1980. p. 339Brenner A.K., Gill N.W., Buscema C.J., Kiesel K.
Improved activation of lumbar multifidus following spinal manipulation:
a case report applying rehabilitative ultrasound imaging.
J Orthop Sports Phys Ther. 2007;37(10):613–619Pickar JG.
Neurophysiological Effects of Spinal Manipulation
Spine J (N American Spine Society) 2002 (Sep); 2 (5): 357–371Aker P.D., Martell J.
Maintenance Care
Topics In Clinical Chiropractic 1996; 3 (4): 32–35Martel J, Dugas C, Dubois JD, Descarreaux M.
A Randomised Controlled Trial of Preventive Spinal Manipulation With and Without
a Home Exercise Program for Patients With Chronic Neck Pain
BMC Musculoskelet Disord. 2011 (Feb 8); 12: 41Descarreaux M, Blouin JS, Drolet M, Papadimitriou S, Teasdale N:
Efficacy of Preventive Spinal Manipulation for Chronic Low-Back Pain
and Related Disabilities: A Preliminary Study
J Manipulative Physiol Ther 2004 (Oct); 27 (8): 509–514Axen I, Jensen IB, Eklund A, Halasz L, Jorgensen K, Lange F, Lovgren PW, Rosenbaum A, Leboeuf-Yde C:
The Nordic Maintenance Care Program: When Do Chiropractors Recommend
Secondary and Tertiary Preventive Care For Low Back Pain?
Chiropractic & Osteopathy 2009 (Jan 22); 17: 1Haldeman S.
Neurological effects of the adjustment.
J Manipulative Physiol Ther. 2000;23(2):112–114
Return to MAINTENANCE CARE
Since 3-10-2013


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |