

Clinical and Cost Outcomes of an
Integrative Medicine IPAThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2004 (Jun); 27 (5): 336–347 ~ FULL TEXT
Richard L Sarnat, MD, James Winterstein, DC
Alternative Medicine Integration Group, LP,
Highland Park, IL 60035, USA.
rsarnat@amibestmed.com
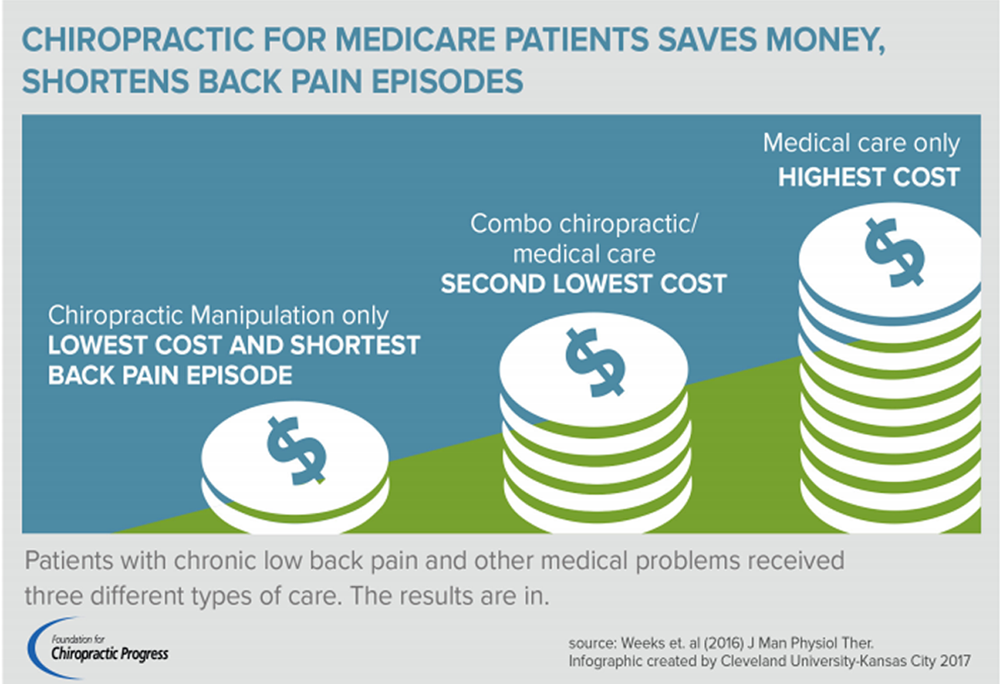
FROM: Weeks ~ JMPT 2016 (Feb) Hurwitz ~ JMPT 2016 (May)
In 1999, a large Chicago HMO began to utilize doctors of chiropractic (DCs) in a primary care provider role. The DCs focused on assessment and evaluation of risk factors and practiced with a non-pharmaceutical/non-surgical approach. Insurance claims and patient surveys were analyzed to compare clinical outcomes, costs and member satisfaction with a normative control group.
During the 4–year study, this integrative medical approach, emphasizing a variety of complimentary and alternative medical (CAM) therapies, resulted in lower patient costs and improved clinical outcomes for patients. The patients who went to DCs as their primary care providers had 43 percent decreases in hospital admissions, 52 percent reductions in pharmaceutical costs and 43 percent fewer outpatient surgeries and procedures.
If you like these results, you will absolutely LOVE the 7–Year Follow-Up!OBJECTIVE: We hypothesized that primary care physicians (PCPs) specializing in a nonpharmaceutical/nonsurgical approach as their primary modality and utilizing a variety of complementary/alternative medicine (CAM) techniques integrated with allopathic medicine would have superior clinical and cost outcomes compared with PCPs utilizing conventional medicine alone.
DESIGN: Incurred claims and stratified randomized patient surveys were analyzed for clinical outcomes, cost offsets, and member satisfaction compared with normative values. Comparative blinded data, using nonrandomized matched comparison groups, was analyzed for age/sex demographics and disease profiles to examine sample bias.
SETTING: An integrative medicine independent provider association (IPA) contracted with a National Committee for Quality Assurance (NCQA)-accredited health maintenance organization (HMO) in metropolitan Chicago.
SUBJECTS: All members enrolled with the integrative medicine IPA from January 1, 1999 through December 31, 2002.
RESULTS: Analysis of clinical and cost outcomes on 21,743 member months over a 4–year period demonstrated decreases of 43.0% in hospital admissions per 1000, 58.4% hospital days per 1000, 43.2% outpatient surgeries and procedures per 1000, and 51.8% pharmaceutical cost reductions when compared with normative conventional medicine IPA performance for the same HMO product in the same geography over the same time frame.
CONCLUSIONS: In the limited population studied, PCPs utilizing an integrative medical approach emphasizing a variety of CAM therapies had substantially improved clinical outcomes and cost offsets compared with PCPs utilizing conventional medicine alone. While certainly promising, these initial results may not be consistent on a larger and more diverse population.
The Full-Text Article:
INTRODUCTION:
The escalation of medical expenditures is an urgent problem. Although various types of managed care, once thought by some to be part of the solution to increasing medical expenditures, have been used for decades, little evidence exists that this or any other cost-containment strategy has significantly influenced a 50–year trend of increasing medical expenses on a long-term basis. [1–5] Managed care rates are now posting double-digit annual increases, [6] with pharmaceuticals estimated to account for 50% of the cost increases over the past 3 years. [7]
While the health care system excels in acute care and crisis disease state management, this accounts for only a small percentage of the total medical care in both cost and volume rendered daily. [8] The greater health care burden is the prevention and treatment of the multiple chronic disorders in the general population that now account for the majority of health care expenditures. [9]
Chronic diseases are a major public problem in the United States. Currently, about 40% of the US population (approximately 100 million Americans) suffer from at least 1 chronic disorder. [9] This high level of prevalence within the United States raises concerns about the efficacy and limitations of our conventional health care system. [10] Such concerns appear to contribute to public and professional interest in alternatives to conventional modern medicine.
Studies now suggest that 50% of the deaths [11] and 70% of the diseases [12] in the United States are caused by unhealthy lifestyle habits such as smoking, alcohol abuse, and improper diet. Unlike the preantibiotic era when mortality was primarily because of infectious diseases, our nation now faces a behavior-induced epidemic of chronic illness. Managed care and government policy makers are faced with the dilemma of trying to decrease medical costs caused mainly by lifestyle choices while continuing to maintain personal freedom of choice.
Iatrogenic illness (an adverse condition arising from the treatment of a physician) is estimated as the etiology of 15% of our hospital days, and pharmaceuticals are estimated to cause between 100,000 to 250,000 deaths per year, [13,14] as well as nonquantifiable morbidity. Prescription drug addiction, administering the wrong drug, and prescription overdoses are a large percentage [15,16] of reported deaths by medical mistake. The National Conference of State Legislatures, November/December 2000, estimates the cost of lost income, disability, and health care resulting from medical mistakes is as much as $29 billion per year. [17]
Given these facts, it may be time to rethink this country's current medical model with its overall reliance on pharmaceuticals as a first line option. Complementary/alternative medicine is one viable approach that should be considered because it addresses the privacy, quality, and expense considerations facing health care delivery systems.
Unlike conventional medical education and care, which relies heavily on high technology and pharmaceuticals, complementary/alternative medicine exists in a “low-tech arena.” “Low-tech” therapeutic modalities such as chiropractic manipulation, homeopathy, stress management, massage, and use of herbal medicines are perceived by the public as more gentle, less morbid, and less costly than conventional modern medicine. [18]
Many previous studies on various complementary/alternative medicine (CAM) modalities have illustrated improved clinical outcomes and substantially decreased costs compared with standard conventional medical practice protocols. [19–44] However, while individual diagnostic categories have been analyzed, a study of the clinical outcomes and cost effectiveness of primary care physicians (PCPs) specializing in CAM, and more particularly chiropractic care, within the context of a classical gatekeeper health maintenance organization (HMO) has never previously been attempted.
METHODS:
Data reported in this study were drawn from incurred claims data, originating from both the integrative medicine independent provider association (IPA) and the HMO. The IPA data included all inpatient and outpatient encounters for both cost and diagnosis, including the professional fees associated with patient referrals, outpatient diagnostics (encounters and costs), and outpatient laboratories (encounters and costs). The HMO data included the encounters and costs of all pharmaceutical usage, inpatient admissions, and outpatient surgery and procedures. This information was collected prospectively over a 4–year period.
The HMO actuarial department prepared an annual financial projection for the IPA membership as an age/sex risk-adjusted population. On a cost basis, the discrepancies between the projected costs versus the actual costs were analyzed annually.
Standard managed care benchmarks, including hospital days per 1000, hospital admissions per 1000, outpatient surgeries and procedures per 1000, and pharmaceutical utilization were reported annually by the HMO (normative network values) and then compared with the actual utilization of the integrative medicine IPA.
Randomized patient surveys were conducted annually by the HMO to assess member satisfaction, quality of care benchmarks, and member behavior patterns (eg, tobacco usage).
Integrative Medicine IPA-Development and Implementation
In 1996, a large HMO accredited by the National Committee for Quality Assurance (NCQA) servicing the metropolitan Chicago area was initially contacted to test the feasibility of gathering data on a CAM-oriented health care delivery system. This HMO was a classical gatekeeper HMO with over 600,000 members enrolled in the greater Chicago area.
The project's objective was to build an integrated medicine system in the Chicago metropolitan area that would use primary care physicians who specialize in a nonpharmaceutical/nonsurgical approach as their primary modality. These nonpharmaceutically oriented PCPs, notably chiropractic physicians, were organized into a well-defined structure along with their more conventional allopathic counterparts to create a truly integrated health care system encompassing both CAM therapies and conventional modern medicine within a single comprehensive insurance benefit structure. The project was designed for a gatekeeper HMO format because its structure simplified data collection and made mandatory reporting a contractual obligation.
To test this new model, an “alternative medicine” IPA, legally incorporated in 1997 as Alternative Medicine, Inc. (AMI), was formed to function within the classical gatekeeper HMO format under the same rules and regulations as any other contracted conventional allopathic IPA. The data reported herein refer to the contractual relationship between AMI as an integrative medicine IPA and the specific HMO (unless otherwise noted).
The formation of an IPA under contract with the HMO required specific contractual elements to be met according to the National Committee for Quality Assurance. The minimum requirements for PCP network support included:
Contracted availability of all allopathic specialists
Contractual relationships with regional hospitals to provide inpatient access
A minimum roster of both pediatricians and obstetricians/gynecologists exclusive to the IPA
HMO Peer Review Committee approval of the IPA's utilization management (UM) and utilization review (UR) plan policy and procedures
As reported later in section IV, “Medical Management,” each of these prerequisites was successfully addressed prior to PCP impanelment.
All primary care physicians had to pass credentialing by the Credentialing Peer Review Committee of the HMO, which was composed of medical doctors (MDs) exclusively. For a new IPA to be impaneled, every PCP needed to successfully pass the credentialing criteria. A single failure would have prohibited the project from initiation. Initial analysis identified 4 separate and independent but related processes that needed to occur to provide the foundation for successful execution:
Physician Recruitment: Targeting that subset of physicians who would be appropriate PCPs to function in a nonpharmaceutical/nonsurgical model. In this study, only chiropractic physicians agreed to participate as PCPs.
Credentialing Process: Developing a credentialing process exceeding the existing NCQA requirements for CAM providers, a standardized process to quantify the performance of this subset of prospective primary care physicians according to accepted industry standards.
Member Recruitment: Addressing the ability to recruit potential members or patients to test the hypothesis that primary care chiropractic physicians specializing in nonpharmaceutical/nonsurgical approaches as their primary modality and using CAM techniques integrated with allopathic medicine would have superior clinical and cost outcomes compared with PCPs utilizing conventional medicine alone. [4]
Medical Management: Formalizing the medical management to provide integrated care between the CAM therapies delivered by the chiropractic physicians and other conventional medical specialists throughout the inpatient/outpatient cycle.
The following sections address the mechanics of how each element was defined and executed to successfully achieve the outcomes reported herein.
Physician recruitment
Nonpharmaceutical/nonsurgical physicians were defined to include those physicians who use as their primary diagnostic/treatment modalities such disciplines as chiropractic manipulation, osteopathic manipulation, naturopathy, homeopathy, Traditional Chinese Medicine (TCM), acupuncture, Ayurvedic medicine, herbal medicine preference over pharmaceuticals, massage, and energy healing techniques.
Under the Medical Practice Act and Managed Care Act, the State of Illinois only licenses medical doctors, Doctors of Osteopathy (DO), and Doctors of Chiropractic (DC) as primary care physicians. Therefore, Doctors of Naturopathy (ND) and Doctors of Oriental Medicine (OMD), although licensed in other states, were automatically excluded from the IPA physician network. At the project's inception, personal interviews were conducted with all categories of physicians, including MDs/DOs and DCs whose style of medical practice qualified them as potential CAM-oriented PCPs. For a variety of professional, personal, political, and economic reasons, only the Doctors of Chiropractic were willing to undertake the project.
All CAM-oriented MDs/DOs interviewed rejected participation for reasons including too restrictive a reimbursement model, philosophical or political issues with managed care in general, inability to meet credentialing requirements because of lack of board certification, or independent (“lone ranger”) personality, not comfortable with third-party oversight and review.
Credentialing process
Since, to our knowledge, Doctors of Chiropractic had previously never served as PCPs in a classical gatekeeper HMO model, this presented an immediate credentialing challenge. A unique credentialing process was developed to identify that subset of Doctors of Chiropractic who could successfully function as PCPs.
Each prospective PCP underwent a personal interview to review his or her treatment modalities, criterion for referrals, and comfort in dealing with a primary care role. Preference was given for such qualities as broad scope of practice patterns, history of appropriate interactions with other medical specialists, and demonstrated understanding of the pathophysiologic basis of disease as currently understood by evidence-based Western medicine. This process has now been formalized into a standardized test and is currently offered as provisional credentialing to students at the National University of Health Sciences in Lombard, Illinois, as well as endorsed by the American Academy of Chiropractic Physicians (AACP).
The credentialing process also involved an educational component, including seminars given by AMI MD medical directors to review conventional medicine diagnostic and referral decision trees. Registered nurses provided the onsite component where prospective physicians and their office staff received training in Health Employer Data and Information Set (HEDIS) compliance, Occupational Safety & Health Administration (OSHA) compliance, and instruction in proper charting requirements. Time spent in the onsite component varied between 4 hours and 20 hours to achieve successful completion. All primary care chiropractic physicians were held accountable to the same criteria as their MD/DO counterparts under NCQA regulations.
It is important to note the educational training of the chiropractic physician. While similar in many regards to medical training, there is no training in surgical procedures or in the use of drugs in the management of human illness. The standard course of training is in excess of 4800 hours, with approximately one quarter spent in the clinical setting. Course work encompasses programs in standard diagnosis (ie, cardiovascular diagnosis, neurological diagnosis, gastrointestinal diagnosis, genitourinary diagnosis, etc.), as well as more specifically chiropractic programs (ie, manipulation of the spine and extremities, physiotherapeutic modalities) and other forms of CAM (ie, homeopathy, herbal therapy, botanical medicine, etc.). [45, 46]
The HMO Peer Review Committee formally approved all of AMI's primary care chiropractic physicians in the fall of 1998. AMI began patient encounters on January 1, 1999 with 16 fully credentialed primary care chiropractic physicians. As of December 31, 2002, AMI had 30 primary care chiropractic physicians in the HMO model.
Member recruitment
The HMO under contract had an enrollment of over 600,000 members and was available only to companies with a minimum employee base of 100 enrollees. AMI's prospective members originated from open enrollment offered to the total population of the HMO. Most members obtained information about AMI from the HMO's standard primary care and specialist physician directories or their company's human resource (HR) personnel. The HMO used no marketing incentives to attract potential patient enrollees to the alternative medicine IPA. Like all classical HMOs, there was no exclusion of patients having preexisting illnesses.
In the first month of operation, January 1, 1999, AMI's HMO had an enrollment of 37 members. Enrollment as of December 31, 2002 was 649 members. Because marketing had been by “word of mouth,” growth in IPA enrollment was steady but slow. IPA enrollment measured in member months (mm) per calendar year grew from 1726 mm (calendar year 1999) to 4987 mm (calendar year 2000), to 6932 mm (calendar year 2001), and to 8098 mm (calendar year 2002). In total, 21,743 mm of data were analyzed. This standard managed care unit is calculated by multiplying each unique member by the number of months enrolled within the IPA during a calendar year.
The HMO calculates the ratio of new member “transfer in” versus “transfer out” for each IPA on a monthly basis. AMI's range for “transfer in” lies between 3.43% and 5.53%, and “transfer out” is between 2.83% and 3.50%. The higher ratio of transfer in versus out correlates with the observed growth in member enrollment.
Medical management
The intention was to provide members with the best treatment that both chiropractic, using a variety of CAM techniques, and conventional modern medicine had to offer. All of the AMI primary care chiropractic physicians focused primarily on the assessment and evaluation of all risk factors whether they were related to diet/nutrition, exercise, postural/structural problems, behavioral/emotional problems, physiological disease, or the need for improved stress management. Similar to the role allopathic PCPs assume in a conventional medical IPA, all examinations, treatments, and procedures that occurred within the offices of the primary care chiropractic physicians were at the discretion of the PCP. The number of recommended visits, the choice of appropriate treatments, and ancillary modalities utilized did not require approval from the IPA MD medical directors. All ancillary testing and treatment outside the personal office of the primary care chiropractic physician was subject to MD medical director approval to benefit from the enhanced experience of allopathic physicians in dealing with more complex and varied disease states.
One inpatient-oriented and 2 outpatient-oriented MD medical directors were available 24 hours a day, 7 days per week to provide consultation and comanagement by phone or facsimile, as required, according to the complexity of the patient's presentation. Over 3000 medical specialists and 18 hospitals (including university based) were under contract by AMI as part of the IPA to provide integrated care as appropriate to medical necessity. Ongoing telephonic and/or facsimile consultation and comanagement between the PCPs and the MD medical directors occurred daily.
In general, primary care chiropractic physicians practiced what they do best: nonpharmaceutical/nonsurgical prevention. When and if acute life threatening disease or advanced disease management required inpatient status or conventional modern medicine, the PCP delegated his/her authority to the attending medical physician consulted. A registered nurse specializing in utilization management and utilization review coordinated continuity of care between the inpatient and outpatient cycle.
By design, AMI's PCPs had a higher number of encounters initially to correct structural dysfunctions and provide re-education in lifestyle choices that left unchanged may have manifested into more serious disease states. It was not atypical for new AMI members to have PCP encounters at an average of twice per month. This is in contrast to conventional medical IPAs, wherein the majority of members have PCP encounters on a “crisis-only” basis.
AMI's “New Member Welcome” letter informed the patient that it was IPA policy to have a mandatory initial visit with their PCP within the first 3 months of enrollment. These frequent education-oriented encounters combined with hands-on healing were believed to forge a strong doctor/patient relationship. The PCP then became the “trusted guide” and assisted the patient with the required lifestyle changes or gave professional advice on the many and varied uses of CAM. Many modalities of CAM remain unregulated and are most safely and effectively utilized when supervised by a licensed physician truly knowledgeable from extended training in CAM.
The chiropractic PCPs also utilized nonphysician (CAM) providers. These providers were licensed and/or credentialed in various CAM therapies, such as massage, acupuncture, cranial sacral therapy, and stress management techniques, including meditation, yoga, and energy balancing, as well as more traditional cognitive therapy. It is important to note that the chiropractic physicians included in this study utilized all the modalities noted above and not just the chiropractic adjustment as a sole therapeutic intervention.
It was anticipated that this increased intensity in prevention-oriented encounters and concomitant comanagement with AMI's MD medical directors would reduce the utilization of high-cost, high-technology conventional medicine downstream.
Member Populations: AMI Versus Nonrandomized Matched Comparison Groups
In this section, Tables 1 through 3 compare various aspects of the AMI membership versus 2 nonrandomized matched comparison groups. Both comparison groups represent separate conventional IPA enrollment within the same commercial HMO product, in the same geographic region, and during the same time frame as AMI's data.
Table 1. Diagnostic profile of AMI's HMO population year 2000
Diagnoses Diagnoses by percentage Diagnoses by members Wellness 28.5% 149 Orthopedic 23.5% 123 Other medical 11.7% 61 Mental health* 8.1% 43 Gynecological 6.7% 35 Sinus/allergy 6.0% 31 Cardiac/hypertension 4.6% 24 Headaches (all variations) 2.7% 14 Neoplastic 1.5% 8 URI 1.5% 8 Asthma 1.4% 7 Gastrointestinal 1.3% 7 Thyroid disease 1.2% 6 Diabetes 1.2% 6 522 522 members with diagnoses includes 31 severely ill patients (multiple ICD-9 comorbidities).
AMI, Alternative Medicine, Inc; HMO, health maintenance organization; URI, upper respiratory infection.
*Mental health defined as those patients requiring a referral to a mental health specialist.
Table 2. Comparison of “well” members AMI versus comparison groups I and II
IPA Members enrolled Members with no or non-ICD-9 encounters Percentage of members coded as “wellness” Percentage of members coded for active disease AMI 522 149 28.5% 71.5% Control group I 7549 2618 34.7% 65.3% Control group II 7723 3206 42.0% 58.0% AMI, Alternative Medicine, Inc.; IPA, independent provider association.
Table 3. Comparison of ICD-9 diagnostic profile by percentage of member enrollment AMI versus comparison group I
Diagnosis AMI % Comparison group I Wellness 28.5% 34.7% Orthopedic 23.5% 8.0% Other medical 11.7% 17.0% Mental health 8.1% 1.3% Gyne (non-OB) 6.7% 9.4% Sinus/chronic allergy 6.0% 2.8% Cardiac/hypertension 4.6% 9.4% Headache (all variants) 2.7% 0.7% Neoplastic (all) 1.5% 1.1% URI 1.5% 10.4% Asthma 1.4% 1.3% GI 1.3 0.9% Diabetes 1.2% 3.4% Thyroid disease (all) 1.2% 1.4% AMI, Alternative Medicine, Inc.; GYN, gynecology; OB, obstetrics; URI, upper respiratory infection; GI, gastrointestinal.
AMI patient population demographics versus comparisons
While the comparison groups' demographics have been matched as much as possible to remove any underlying bias, certain dissimilarities exist. “Children,” defined as member enrollment under the age of 20, represents a smaller population percentage in the AMI program compared with the comparison groups: 11.9% (AMI) versus 32.8% (comparison group I) and 19.0% (comparison group II). The smaller percentage of children enrolled is not accidental. Chiropractic physicians are unable to legally administer childhood immunizations because of limitations in the scope of practice of their licensure. While AMI does not prohibit enrollment for children under 10, it is not encouraged.
Statistical analysis also reveals a slightly decreased average age of adult members in the AMI population (39.5 years) compared with comparison groups I (41.3 years) and II (40.3 years). While this slight average age discrepancy certainly favors increased cost expenditures in the comparison groups, this may be offset by the fact that AMI has a greater percentage enrollment of female members compared with male members. The actuarial department of the HMO predicts more than a 50% greater utilization within the IPA by female members versus male members. The sex distribution of AMI membership is 61.6% female members and 38.4% male memers. By contrast, comparison group I had 58.9% female members and 41.1% male members; comparison group II had 59.1% female members and 40.9% male members.
The HMO forwarded age/sex distribution data to AMI in the form of monthly eligibility lists. Comparison group data were forwarded to the authors from the conventional IPAs after receiving their individualized data from the HMO.
AMI patient population disease profile
AMI's HMO membership, as reported herein, represented a unique population dissimilar from previously published literature of disease states commonly seen by chiropractors. [47] Chiropractors primarily care for patients with complaints of musculoskeletal origin or headaches. As AMI was the first managed care program to utilize chiropractors in a PCP role, it was not surprising that membership included a wide range of disease states not seen in the typical chiropractic office, as illustrated in Table 1.
When analyzing IPA data, diagnostic classification was assigned to individual patients based on PCP encounter data, specialist encounter data, referral activity, and pharmaceutical usage. When multiple International Classification of Diseases, Ninth Revision (ICD-9) codes were listed on encounter data, the diagnosis requiring the higher expenditure for workup or treatment was chosen as the primary classification. If the presence of prominent severe comorbidity such as hypertensive cardiac disease, diabetes mellitus, and bipolar disorder were all prominent in a patient's encounter data, then the patient received 3 separate and distinct classifications. This explains why 491 unique patients in the year 2000 received 522 disease classifications (Table 1).
The diagnostic category “wellness” referenced in Tables 1 through 3 was defined as:(1) members having patient encounters but not receiving ICD-9 codes (these patients may have been symptomatic but received chiropractic codes for subluxation/dysfunction by their PCPs)
(2) members having encounters for nonsymptomatic screening test only, or
(3) members having no encounters within a given calendar year.The category “other medical” listed in Table 1 (11.7% of AMI's population) encompassed a wide range of diseases affecting 61 patients. These diseases included (listed in order of frequency) but were not limited to the following: neurologic disorders, abdominal pain, dermatologic disorders, prostate disease, adrenal cortical insufficiency, chronic fatigue syndrome, cystitis, esophageal reflux, multiple sclerosis, tinnitus, temporomandibular joint (TMJ), and human immunodeficiency virus (HIV).
As Doctors of Chiropractic had not previously functioned as PCPs, the congruence of their diagnoses when compared with conventional PCPs when reporting on a Health Care Financing Administration (HCFA) 1500 encounter form was unknown. When PCP diagnostic coding data were cross-correlated with both specialist referral data and pharmaceutical usage, agreement was found between the conventional medical specialist and the chiropractic PCP 93.1 % of the time. When the diagnosis necessitated a treatment that required the use of pharmaceuticals or surgery, then an appropriate referral was made to a conventional medical specialist.
ICD-9 Profile of Nonrandomized Matched Medical Comparison Groups I and II
In this section, Tables 2 and 3 reflect membership breakdown by ICD-9 diagnostic coding percentage comparing AMI's membership with the membership of comparison groups I and II. Both comparison groups represent conventional IPA enrollment for the same commercial HMO product in the same geographic region during the same time frame as AMI's data. A blinded independent contractor with previous employment in the medical records department of a local hospital analyzed ICD-9 coding data, compiling the disease profiles between AMI's membership and comparison group I membership.
Previously published literature indicates that users of CAM modalities are not necessarily the “worried well” and may actually represent an adverse selection of patients who are “medical failures” in the traditional medical system. [48,49] The prevalence of active disease in the AMI population as shown in Tables 2 and 3 is consistent with earlier reports of this phenomena.
The fact that potentially life-threatening disease states, such as cardiac disease, hypertension, and diabetes had higher enrollment in conventional medicine IPAs was not surprising. The similar percentage enrollment of patients with asthma and neoplastic disease between conventional and integrative medicine IPAs was somewhat surprising. The large enrollment disparity among patients with upper respiratory infections (URI), as previously mentioned, reflects the small percentage of AMI's enrollment under 10 years of age.
A comparison of smoker prevalence among the AMI population, the HMO population, and the general state population further demonstrates possible adverse selection in the AMI population. Member satisfaction surveys, randomly distributed by stratified random selection to between 35,000 and 45,000 HMO members, annually elicited a response rate that varied between 25% and 30%. These surveys revealed a variance in the AMI population when measuring for smoker prevalence rate.
In calendar year 2001, the AMI membership showed its highest rate of smoker prevalence: 34.9% versus the HMO population rate of 18.0% versus the Illinois general population of 22.3%. [50]
In calendar year 2003, by contrast, AMI membership had its lowest smoker prevalence rate of 13.3% versus the HMO population rate of 16.3%. We assume the large variance from year to year was secondary to the relatively low membership response rates elicited by the survey.
Data Analysis
AMI's outcomes data are based on claims incurred. Data were collected in parallel by the HMO and Independent Health Resources (IHR), which functions as AMI's third-party administrator (TPA). The HMO specifically analyzed all inpatient costs, outpatient facility costs, and pharmaceutical usage. AMI, via its TPA, analyzed all inpatient and outpatient professional encounters and utilization, as well as outpatient laboratory. The HMO reported all utilization back to AMI on a 6–month delay to allow for the reporting of all claims during the experience period. This reporting method produced actual claims, removing the potential inaccuracies of claims incurred but not reported (IBNR).
Data Reporting
The HMO prepared quarterly reports to AMI on such managed care benchmarks as:
Hospital admissions per 1000 members
Total hospital days per 1000 members
Outpatient surgical cases and procedures per 1000 members
Average length of stay
Pharmaceutical utilization and cost per member/per month
These statistical benchmarks were reported as a comparison between the performance of AMI as an IPA and the HMO network as a whole. Because of the HMO's proprietary concerns regarding their network's unique data points, AMI's outcomes are reported as percentage comparisons with HMO outcomes.
RESULTS:
Outcomes: Clinical
The se data points are based on the HMO's corroborated data for the 4 calendar years 1999, 2000, 2001, and 2002. AMI's encounter data represent 21,743 member months over this 4–year period. The traditional managed care benchmarks depicted in Table 4 illustrate AMI's apparent superior clinical outcomes compared with conventional IPA performance over the same time frame.
Table 4. AMI outcomes comparison with HMO network data (1999–2002)*
AMI percentage utilization vs HMO AMI percentage reduction vs HMO Hospital-based data Hospital admissions/1000 57.0% 43.0% Hospital days/1000 41.6% 58.4% Average length of stay 76.2% 23.8% Outpatient-based data Outpatient surgical cases/1000 56.8% 43.2% Pharmaceutical usage (cost) 48.2% 51.8% AMI, Alternative Medicine, Inc.; HMO, health maintenance organization.
*Obstetrics admissions excluded from comparison percentages.
AMI's outcomes are reported as “percentage utilization” and “percentage reduction” versus the HMO network as a whole. Percentage utilization is based on actual claims data after a 6–month runoff comparing AMI's utilization of key benchmarks versus the HMO network as a whole. Percentage reduction reflects the mathematical complement of AMI's utilization percentages using the HMO network outcomes as the normative value of 100%.
Traditional P values of statistical significance could not be reported. Insurance actuaries do not currently have data points for variance and mean on groups of similar size and demographics. Only aggregate data (the HMO normative network performance) representing groups of all sizes and demographics were available.
Calendar year 2000 data on hospital admission days (Table 5) obtained from the Illinois Department of Insurance similarly reflect improved AMI outcomes compared with all the major HMOs in the Chicago metropolitan area.
Table 5. Calendar year 2000 hospital days incurred among major Illinois Managed Care Organizations (MCO) versus AMI
Managed care entity Total member months Total hospital days incurred per 1000 member months AMI percentage utilization AMI percentage reductions HMO Illinois 7,537,362 344.85 33.3% 66.7% Personal Care Insurance Company of Illinois 787,853 320.02 35.9% 64.1% Prudential Health Care Plan 269,268 285.38 40.3% 59.7% United Healthcare of the Midwest 361,437 236.75 48.6% 51.4% CIGNA Healthcare of IL 143,236 201.00 57.2% 42.8% Aetna US Healthcare of IL 1,664,525 177.64 64.7% 35.3% Humana Health Plan, Inc. 3,536,085 170.94 67.3% 32.7% AMI 3-year cumulative 13,645 115.0 AMI, Alternative Medicine, Inc; HMO, health maintenance organization.
The referral pattern of AMI's PCPs compares favorably with historical referral patterns generated by traditional allopathic IPAs utilizing internists, pediatricians, or OB/GYNs as PCPs. As shown in Table 6 , the strategy of comanagement resulted in only 40% of the AMI membership requiring an allopathic specialist referral in the calendar year 2000. In other words, during the year 2000, 60% of the patients were managed solely by their primary care chiropractic physicians.
Table 6. Analysis of referral patterns on AMI HMO population, calendar year 2000
1.Average number of members during 2000 (4987 member months / 12) 416 2.Total number of referrals 330 3.Total number of unique patients requiring a referral 167 4.Percentage of population requiring referral to allopathic specialist (167/416) 40% 5.Percentage of population managed by chiropractic primary care physicians (PCPs) without allopathic referral (100% – 4) 60% AMI, Alternative Medicine, Inc; HMO, health maintenance organization.
Referral data analysis annualized for the year 2001 shows AMI primary care chiropractic physicians generated 1 referral per 33 patient encounters (1:33 ratio). This is in contrast to data generated from comparison group II illustrating that conventional medicine PCPs generate 1 referral per 3 patient encounters (1:3 ratio). This referral pattern was consistent with our prediction that an increase in CAM-oriented PCP encounters initially would result in less utilization of conventional medicine downstream.
In addition to the clinical outcomes referenced in Table 6, measures of Quality Care were benchmarked by randomized patient satisfaction surveys and an annual audit of all UM/UR Committee documents by the HMO nursing administrators. Annually, the HMO independently surveyed by “stratified random selection” over 45,000 patients. Response rates were between 25% and 30% annually. The HMO required a minimum score for patient satisfaction to be between 80% and 90%, depending on the calendar year. AMI member satisfaction scores for the first 4 years were 100%, 89%, 91%, and 90%, respectively. Analysis of HMO member satisfaction surveys demonstrates the AMI members consistently rated their experience with AMI above the HMO network normative average.
Annual audit scores measuring IPA compliance with Utilization Management Adherence/Utilization Review Activity written policy and procedures conducted by HMO onsite nurse auditors also were above the HMO network normative values. AMI's annual audit scores for medical administration and medical management were between 97% and 100% in each category. The HMO minimum required score for IPA performance is 90%.
Outcomes: Cost
AMI also received an annual age/sex adjusted risk pool analysis of its members by the HMO's actuarial department. Derived from this risk pool analysis was a hypothetical budget of predicted expenditures excluding pharmaceuticals for AMI's actual membership defined as the utilization management fund (UM fund). This budget was calculated in “target usage units” that have an assigned dollar equivalency. IPA actual performance was then calculated against IPA-predicted performance. AMI's utilization management fund cost savings (below predicted budget) were 66.7%, 88.1%, 57.1%, and 69.3% for the calendar years 1999, 2000, 2001, and 2002, respectively.
It is believed that the improvement in cost effectiveness between year 1 (1999) and year 2 (2000) occurred primarily due to an innovative mental health initiative. In calendar year 1999 (AMI's first year), 33% of the hospital days were categorized as “mental health.” Beginning in calendar year 2000 (AMI's second year), a quality initiative targeting stress management techniques was introduced to impact the high percentage of mental health admissions.
In the subsequent 3 years following this initiative, mental health admissions have accounted for less than 2% of all hospital days utilized. This protocol relied heavily on “mind/body” techniques such as cranial sacral therapy and energy balancing, as well as more traditional cognitive therapy.
DISCUSSION:
Certainly, we now appreciate the importance of lifestyle and environmental factors in the optimization of health and subsequent prevention of disease. Reliance on the conventional medical model, in which pharmaceuticals and surgical interventions represent first-line treatment, may not provide the best therapeutic index to our patients. The AMI model seems to demonstrate the potential superiority of an integrated health system in which chiropractic and CAM therapies play a significant primary care role.
Traditional PCPs, be they MDs or DOs, have little formal training in the various evidence-based techniques within the CAM arena. Doctors of Chiropractic, however, receive extensive formal training in the arts of spinal manipulation, herbal medicine, and nutrition, as well as conventional modern physical diagnosis. Most of the AMI PCPs electively received additional postgraduate training in homeopathy, TCM, and other CAM modalities. Students of chiropractic learn to auscultate heart and lungs, draw blood, and read electrocardiograms (EKGs), as well as perform pelvic and rectal exams. However, the educational focus and scope of practice laws vary among chiropractic colleges and states, respectively.
It is incumbent on the primary care physician, of whatever licensure, to look at all evidence-based risk factors and seek to coordinate their reduction. Most of the time this will involve the re-education of patients regarding lifestyle choices such as diet, exercise, nutrition, supplementation, correction of posture, and stress management issues. Lifestyle re-education emphasizing prevention and wellness may be best addressed by PCPs with an unconventional medical orientation, as opposed to conventional medical physicians who have been educated and focus primarily on disease management. The AMI experience seems to indicate that a nonpharmaceutical/nonsurgical orientation can reduce overall health care costs significantly and yet deliver high-quality care. These results have been achieved not by decreasing or denying access to care but, rather, by increasing the frequency of PCP prevention-oriented encounters.
The chiropractic profession is the largest stakeholder in the ongoing evolution of integrating CAM therapies into mainstream conventional medicine. Doctors of Chiropractic are licensed in all states, compared with Doctors of Naturopathy licensed in 11 states and Doctors of Oriental Medicine licensed in only 5 states. Acupuncturists and massage therapists are licensed in 40 and 30 states, respectively. Chiropractic is the most commonly utilized CAM therapy, as published in many previous surveys. Yet, paradoxically, core coverage by insurance benefit design rarely includes unrestricted access to chiropractic. Instead, a myriad of excuses both by the private insurance industry and by the federal government currently reduce one's personal freedom by restricting access to choose unconventional medicine, even when practiced by licensed physicians in good standing. Various authors believe the restrictions on covered benefits for CAM therapies and unconventional physicians are indefensible, given the growing evidence base on these therapies. [51]
“Discount affinity programs” promoted as a “value added” service are currently the most common insurance format by which CAM therapies are available. In reality, these programs are not covered insurance benefits at all. They do not place the mainstream insurance underwriter at financial risk. Rather, they provide the insured with a discount off market fee-for-service rates for severely restricted pseudo benefits. [52] The American Chiropractic Association (ACA), the largest professional association representing the largest stakeholder to the delivery of CAM therapies, has formally rejected discount affinity programs as an insurance sham. [53]
While the availability of discount affinity programs gives the public the illusion that CAM therapies are a covered service on par with conventional medicine, that is not the case. The AMI Wellness Model, by contrast, has been formally recognized by both the ACA and the American Academy of Chiropractic Physicians as a future template of an integrated medical model, which is “front-end loaded” to address prevention and wellness. An increase in initial PCP services is required by the patient to re-educate and emphasize the modification of inappropriate lifestyle choices, thereby re-empowering the patient toward improved self-determination. The good news is that within a 3– to 4–month time period, much of the behavior responsible for the etiology of new or chronic disease has been modified. The initial investment of time, energy, and financial resources for CAM therapies has been successful, apparently much more successful than a quick pharmaceutical prescription and a hasty visit with a conventional PCP (typical of the way managed care is practiced today).
Recently published literature also suggests patient preference and increased satisfaction with integrative therapies for chronic disease states. In the articles by Eisenberg et al [54–56] comparing patients' subjective perceptions as to the relative value of conventional care versus CAM therapies, in only 3 of 10 therapies was conventional medicine perceived as superior to CAM therapies. The 3 disease states scoring higher for conventional medicine were high blood pressure, lung conditions, and digestive conditions. By contrast, back conditions, allergies, fatigue, arthritis, headaches, neck conditions, and strains and sprains were perceived better treated by CAM therapies. [54–56] AMI's higher percentage of members with ICD-9 codes for orthopedics, mental health, chronic sinus, allergy, gastrointestinal problems, and headaches versus the comparison group enrollment is consistent with this pattern.
Limitations
This article's methodology is a nonrandomized longitudinal population study comparing and contrasting both clinical and cost outcomes among similar populations enrolled in the same insurance product for the same time frame and geography.
The strengths of this article's methodology are numerous:(1) study length of approximately 4 years;
(2) cost and clinical data reported “at arms length” by the actuarial department of the HMO to the IPA;
(3) availability of matched comparison groups for blinded analysis of membership population for ICD-9 comparisons;
(4) availability of randomized patient surveys generated by the HMO to analyze both membership satisfaction with ongoing treatment and preexisting risk factors, such as lifestyle behaviors (tobacco usage);
(5) availability of corroborating data, such as pharmaceutical usage and specialist consultations, to cross-check the accuracy of membership ICD-9 population profiles; and
(6) patient-oriented medical management, whereby a variety of CAM therapies were individualized for each patient in the “real life” setting of a metropolitan wide IPA doing business as a “clinic without walls.”
Of course, this article's methodology also suffers from inherent weaknesses:(1) the relatively limited enrollment of AMI's membership population versus the matched comparison groups;
(2) the inability to determine the exact effect of membership transfer in and transfer out on the cost and clinical outcomes;
(3) lack of uniformity in disease-specific treatment protocols utilized among all AMI's physicians;
(4) no randomization of comparative IPA memberships; and
(5) inability to perform standardized statistical probability analysis due to industry nonavailability of required actuarial data.So, at the end of the day, where does this leave us? Have we derived valid and credible knowledge that is useful? At the very least, this article, for the first time, has demonstrated that a select group of chiropractic physicians successfully functioned in both a safe and effective manner as PCPs in a classical gatekeeper HMO model. Second, it has demonstrated that these same chiropractic physicians were capable of initiating and coordinating care for patients with a broad spectrum of disease states, representing a wider variety of diagnostic presentations than is commonly seen in most chiropractic offices. Third, the magnitude of improvement in both clinical and cost outcomes compared with normative values is so large that it is difficult to dismiss as purely coincidental to population bias and nothing more.
While admittedly the data are not definitive because of all of the methodological concerns enumerated, this article seems to demonstrate, for the first time, the potential superiority of integrating a nonpharmaceutical/nonsurgical-oriented gatekeeper or entry point with our already existing conventional health care system. Why should this change in PCP orientation make seemingly such a profound impact on outcomes?
CONCLUSION
AMI's integrative medicine IPA represents a new model in the delivery of managed care. This unique model has demonstrated promising clinical and cost outcomes by the integration of complementary alternative medicine with conventional medicine in a defined program encompassing physician selection, medical management, and scientific accountability. AMI believes this model to be replicable on a much larger scale and is currently implementing different programs, such as preferred provider organization (PPO), point-of-service (POS), and Workers' Compensation to new geographies. AMI's HMO outcomes reported herein were the results of an initial prototype still in evolution. The performance of physicians with other licensures, such as Doctors of Naturopathy and Doctors of Oriental Medicine, as well as MDs and DOs who are nonpharmaceutically oriented needs to be studied in this context as well.
The traditional argument against coverage for prevention-oriented medicine is that it will not reap immediate financial benefits and that employee or insurance turnover is too high to wait for an extended turnaround time. The AMI experience suggests that cost savings may occur in the first calendar year of operations.
The magnitude of improvement in both clinical outcomes and cost savings documented herein may not remain constant when the AMI model is utilized on larger and more diverse populations. However, even a small percentage of the AMI outcomes would still have significant implications, given a $1.3 trillion national health care budget. At such a high price, AMI's initial results should warrant additional funding for a larger and better controlled replication of these findings.

Return to COST-EFFECTIVENESS
Return to SPINAL PAIN MANAGEMENT
Return to INTEGRATED HEALTH CARE
Return to COST EFFECTIVENESS JOINT STATEMENT
Since 9-08-2004


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |