

Cost of Chiropractic Versus Medical Management of
Adults with Spine-related Musculoskeletal Pain:
A Systematic ReviewThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Chiropractic & Manual Therapies 2024 (Mar 6); 32: 8 ~ FULL TEXT
OPEN ACCESS Ronald Farabaugh • Cheryl Hawk • Dave Taylor • Clinton Daniels
Claire Noll • Mike Schneider • John McGowan • Wayne Whalen
Ron Wilcox • Richard Sarnat, Leonard Suiter • James Whedon
American Chiropractic Association,
2008 St. Johns Avenue,
Highland Park, Illiois. 60035
Arlington, VA, USA.
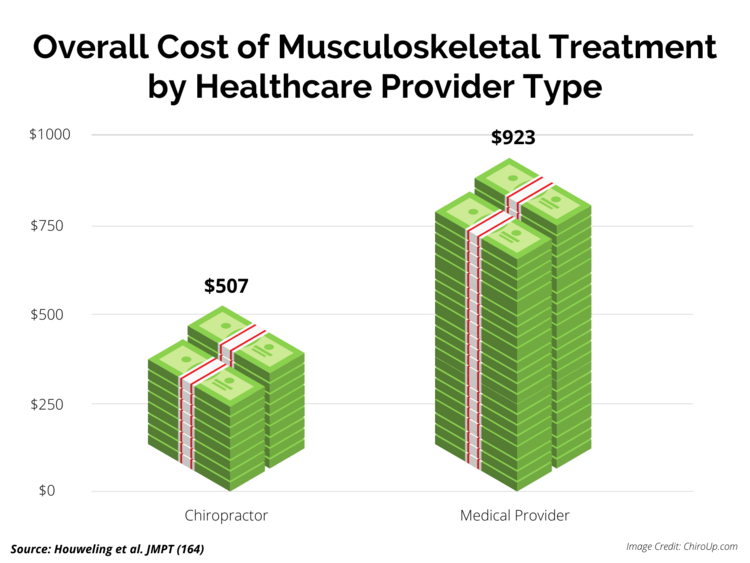
FROM: Houweling, JMPT 2015Background: The cost of spine-related pain in the United States is estimated at $134.5 billion. Spinal pain patients have multiple options when choosing healthcare providers, resulting in variable costs. Escalation of costs occurs when downstream costs are added to episode costs of care. The purpose of this review was to compare costs of chiropractic and medical management of patients with spine-related pain.
Methods: A Medline search was conducted from inception through October 31, 2022, for cost data on U.S. adults treated for spine-related pain. The search included economic studies, randomized controlled trials and observational studies. All studies were independently evaluated for quality and risk of bias by 3 investigators and data extraction was performed by 3 investigators.
Results: The literature search found 2256 citations, of which 93 full-text articles were screened for eligibility. Forty-four studies were included in the review, including 26 cohort studies, 17 cost studies and 1 randomized controlled trial. All included studies were rated as high or acceptable quality. Spinal pain patients who consulted chiropractors as first providers needed fewer opioid prescriptions, surgeries, hospitalizations, emergency department visits, specialist referrals and injection procedures.
Conclusion: Patients with spine-related musculoskeletal pain who consulted a chiropractor as their initial provider incurred substantially decreased downstream healthcare services and associated costs, resulting in lower overall healthcare costs compared with medical management. The included studies were limited to mostly retrospective cohorts of large databases. Given the consistency of outcomes reported, further investigation with higher-level designs is warranted.
Keywords: Chiropractic; Conservative care; Healthcare costs; Healthcare utilization; Low back pain; Manipulation; Opioids; Spinal.
From the FULL TEXT Article:
Introduction
Spine-related musculoskeletal pain is the leading cause of disability worldwide and one of the most common reasons for missed work. [1] In the United States (U.S.), healthcare costs for low back and neck pain are rising and as of 2016 were the highest for any condition, with an estimated $134.5 billion for care related to spinal pain. [2]
There are many options for treatment of acute or chronic spine-related pain. These range from conservative therapies, such as manual or behavioral therapies, to medications, injection procedures and surgery. [3, 4] Approaches to management of spine-related musculoskeletal pain differ by type of provider, such as chiropractors, physical therapists, primary care medical physicians and medical specialists such as orthopedists and neurologists. [5] In the U.S., chiropractic care is one of the most commonly utilized approaches to treatment of spine-related musculoskeletal pain. [6] Chiropractic care guidelines are concordant with the American College of Physicians’ recommendations for initial management of low back pain (LBP) using non-pharmaceutical treatment. [7, 8]
In the midst of rising healthcare costs, it is important to examine not only clinical outcomes but also the cost of intervention strategies for spine-related pain. Although most cases of spine-related musculoskeletal pain can be effectively managed with conservative guideline-concordant non-pharmacological and non-invasive approaches, frequently a patient’s course of care is unnecessarily escalated by use of more invasive, hazardous, and/or costly procedures. [9] The escalation of care for spine-related musculoskeletal pain may include emergency department visits, medical specialist visits, diagnostic imaging, hospitalization, surgery, interventional pain medicine techniques, prescription of drugs with high risk for addiction or abuse, and encounters for complications of spine care (e.g., adverse drug events). [9] The escalation of spine-related musculoskeletal pain management is closely associated with increased downstream costs.
Gold et al. defined “downstream” costs as those that “may have changed, intentionally or unintentionally, as a result of the implementation strategy and intervention.” [10]p.3 Downstream costs may include those associated with healthcare utilization, patient and caregiver costs, productivity costs and costs to other sectors. For spine-related musculoskeletal pain, most often LBP, an emerging body of evidence suggests that downstream costs are significantly affected by the specialty of the initiating care provider. [5] Such costs typically include diagnostic tests, particularly advanced imaging [11], surgery, specialist care and medication use. [12]
The opioid epidemic. For patients with spine-related musculoskeletal disorders, among the most important escalations of care associated with downstream human and societal costs that are receiving recent attention are opioid use, abuse and overdose. In 2017, the U.S. government declared the opioid epidemic to be a Public Health Emergency. [13] This epidemic is still on the rise, with drug overdose deaths increased by 31% in a single year, 2019–2020. [14]
It is not certain which combination of provider and/or therapy offers the most cost-effective approach to managing spine-related musculoskeletal pain. A 2015 systematic review compared the costs of chiropractic care to those of other types of health care. [15] The costs were generally lower when musculoskeletal spine care was managed by chiropractors, though the included studies contained methodological limitations. [15] The purpose of this review was to update, summarize, and evaluate the evidence for the cost of chiropractic care compared to conventional medical care for management of spine-related musculoskeletal pain. [15]
Methods
Our team followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol to conduct the review and registered it with PROSPERO in December 2022 prior to data abstraction (CRD42022383145). We elected a priori not to pursue meta-analysis due to heterogeneity of the included studies. Most of the included studies are cohort studies which by their nature can only show associations, cannot prove causation, and are of a lower level of evidence than RCTs, which are the study design usually included in meta-analyses. We conducted the searches and quality assessments from July through December 2022 and data abstraction from January through March 2023.
The primary aim of our systematic review was to address the research question:Is chiropractic management of spine-related musculoskeletal pain in U.S. adults
associated with lower overall healthcare costs as compared to medical care?To answer the research question, we formulated PICO elements (Population, Intervention, Comparison, Outcome) as follows:
P: U.S. adults with spine-related musculoskeletal pain
I: Chiropractic management
C: Medical care
O: Healthcare costs and use of procedures estimated to increase downstream costs involved in escalation of careCosts in a controlled setting are not often comparable to usual and customary costs in a clinical setting. [16] Therefore, in addition to randomized controlled trials, we also included economic and cohort studies that collected data specifically on cost, whether or not treatment outcomes were considered.
Eligibility criteriaInclusion criteria
Published in peer-reviewed journal and available in Medline from inception through 10/31/2022
English language
Study population comprised of US adults treated for spine-related musculoskeletal pain
Compared chiropractic management to medical care
Cost data for treatment of spine-related musculoskeletal pain were provided
Designs were randomized controlled trial, cohort study or economic evaluation.
Exclusion criteria
Reviews, commentaries, abstracts from conference proceedings, theses, cross-sectional descriptive surveys and gray literature.
Systematic reviews were not used as part of quality assessment or data abstraction. They were retrieved only to identify eligible studies which were not found in the literature search.
Studies with clinical effectiveness outcomes only and no inclusion of cost or utilization data
Literature search
We developed a search strategy based on the PICO terms, with a health sciences librarian working with the other investigators. We made several “trial runs” to refine the strategy to be sure it was as inclusive as possible while screening out obviously non-relevant citations. Our search was conducted exclusively in Medline, as relevant high-quality articles were more likely to be found in journals indexed there. We developed a search strategy with keyword clusters based on our PICO. Most publications about spine-related pain study adults (our P) and “adult” was not helpful as a limiter. Intervention (I) cluster terms were selected from a previously published search string of complementary and alternative medicine terms. [17] The Outcome (O) cluster started with terms used in a prior cost-effectiveness study [18], with the subsequent addition of indexing terms found during early search trial runs. The MeSH heading Cost-Effectiveness Analysis was not yet available at the time of our search. The complete search strategy is shown in Additional File 1.
Retrieved citations were downloaded into an EndNote library (v. 20). Using Rayyan https://rayyan.ai/, [19] online systematic review software, at least two investigators screened titles and abstracts for eligibility and resolved disagreements by discussion. At least two investigators checked the references included in all relevant systematic reviews found in the literature search and added any eligible citations not identified in our literature search to the library. At least two investigators did full-text screening of the titles remaining after title/abstract screening was completed, and disagreements were again resolved by discussion. All authors contributed during the process in review of eligible citations.
Evaluation of risk of bias
We evaluated randomized controlled trials (RCTs) using a checklist modeled after those of the Scottish Intercollegiate Guideline Network (SIGN) [20], which we have used elsewhere. [3] An article was rated as “high quality, low risk of bias,” “acceptable quality, moderate risk of bias,” “low quality, high risk of bias,” or “unacceptable” quality. For studies analyzing treatment costs (e.g., economic studies), we developed a checklist with similar format to those of SIGN checklists. [20]
For cohort studies, it was difficult to identify a single appropriate checklist because most seemed designed to be more appropriate to assess prospective cohort studies, and the most recent relevant studies related to our topic are retrospective cohort studies using large datasets. We therefore developed a checklist for prospective cohort studies after reviewing other existing checklists. [20] For retrospective or cross-sectional cohort studies, we developed a checklist combining some features of the SIGN checklist for cohort studies [20] and the NIH tool for observational cohort and cross-sectional studies. [21] These checklists included items assessing comparability of the included cohort groups, as part of the risk of bias assessment. Three investigators (RF, CH and JW), one of whom is an author of a number of cohort studies, piloted and then refined this form with a sample of studies.
Two or more investigators rated each article. Disagreements were resolved by including additional reviewers and discussing differences in ratings until they reached agreement.
Because of the large number of cohort studies, which are considered to have an inherent risk of bias due to their design, we only included studies which the investigators agreed were at minimum “acceptable quality, moderate risk of bias” using the SIGN quality criteria. We excluded any studies that the investigators found to be “low quality, high risk of bias” or “unacceptable quality.”
Data extraction
Because it has been found that data extraction errors are frequent in systematic reviews, we followed the recommendations on data extraction in a review of data extraction guidelines and methods. [22] Before starting the process, we listed all the items we thought were necessary for answering our research question. Then we drafted a data extraction form with these items and two investigators (RF and CH) piloted it on a sample of studies. We then provided brief, online training on use of the forms with the 3 investigators who did the data extraction (RF, CH, DT). This included instructions on how disagreements would be resolved, which was to recheck the source paper and provide it to the other reviewer(s). Two investigators (RF and CH) did independent parallel extraction for all studies, and DT then reviewed the drafted tables; thus the data extraction was triple-checked. We did not attempt to subcategorize patient populations from the included studies.
Results

Figure 1

Table 5

Table 1

Table 2

Table 3

Table 4 We concluded the search in November 2022 and retrieved 2247 citations. Figure 1 shows the PRISMA flow chart, showing reasons for exclusions. Nine articles were identified by reference tracking and expert consultation to make the total number of articles for screening 2,256. Title and abstract screening of these resulted in 93 articles for full-text screening, with 49 excluded (see Additional File 2 for citations) and 44 remaining for quality assessment and data extraction. Please refer to Table 5 for a summary of findings including a quick-view color coded identification format related to each accepted paper. For ease of viewing, we divided the papers using two headings: (1) types of costs and (2) factors affecting costs.
Final inclusions and quality assessment
Table 1 lists the study design and quality rating for the 44 included studies.
All were rated high or acceptable quality (see Additional File 3 for details for the quality assessment). [20]
There were 4 prospective cohort studies [23–26],
22 retrospective or cross-sectional cohort studies [9, 12, 27–46],
17 cost studies [5, 47–62] and one randomized controlled trial [63],
although 2 of the cost studies used data from RCTs.
Data extraction and summary
Because of the large number of studies, we separated the data extraction into two tables, using 2017, the year the U.S. declared the opioid epidemic [13], as the dividing line. Table 2 displays data extracted from each included study published between 2018 and 2022. Table 3 displays data extracted from each included study published between 1991 and 2017.
There were 17 included articles published in the 5 years from 2018 to 2022 (approximately 3 articles per year). There were 27 included articles published in the 26 years from 1991 to 2017 (approximately 1 article per year). From 2018 to 2022, most [15] were retrospective/cross-sectional cohort studies, with 1 prospective cohort study and 1 economic/cost study. From 1991 to 2017, most [16] were economic/cost studies, with 7 retrospective/cross-sectional cohort studies, 3 prospective cohort studies and 1 randomized controlled trial.
Summary of cost factors
Table 4 summarizes the findings of all included studies, by year of publication. Below we have grouped these by type of cost and factors affecting cost. Table 5 depicts chiropractic services versus comparisons in terms of higher, lower or no difference in association for each of the identified types of costs and downstream utilization of factors affecting costs. All of the included studies newer than 2009 demonstrated associations that favored chiropractic services in regard to lower costs and lower utilization of services.
Type of costsFactors affecting costs
Total costs Ten studies found that Doctor of Chiropractic (DC) care had lower overall costs.
[5, 12, 38, 41, 42, 51, 52, 55, 58, 62]
No studies found that DC care had higher overall costs.Costs per episode of care Six studies found that DC care had lower costs per episode
[35, 38, 41, 49, 59, 62],
and two found that it had higher cost per episode. [23, 56]Insurance/compensation costs Four studies found DC care had lower insurance and compensation payment costs
[49, 53, 55, 57].
No studies found higher costs.Long-term healthcare costs Two studies found lower long-term healthcare costs associated with DC care.
[36, 42]
No studies found higher costs.Office visit costs One study found reduced costs for DC office visits [12];
four studies found that DC care had higher costs for office visits [47–49, 61].
Two of these studies noted that chiropractic office costs were higher only when referral costs were not included in the calculation.
When referral costs were included, chiropractic office visit costs did not differ significantly from medical care costs. [48, 61]
Diagnostic imaging Fifteen studies found that diagnostic imaging, particularly advanced imaging like MRI,
was used less with DC care; six studies were published 2018–2022 [5, 9, 27–29, 31]
and nine studies from 1991 to 2017 [25, 32, 33, 47, 51–54, 61].Opioids Eleven studies found that fewer opioid prescriptions were dispensed or filled with DC care.
Ten of these were published 2018–2022 [5, 12, 29, 36, 37, 39, 43–46],
and only one between 1991 and 2017. [40]Surgery Eight studies found fewer surgeries with DC care; four published 2018–2022 [27–30]
and 4 published 1991–2017 [26, 51, 54, 61].Hospitalization Seven studies found fewer hospitalizations with DC care;
two studies were published from 2018 through 2022 [9, 29]
and five from 1991 through 2017 [51, 54, 55, 59, 60].DC as 1st provider Six studies analyzed cost factors related to having a DC as the 1.st care provider.
Generally, this was associated with lower downstream costs.
Four studies were published 2018–2022 [5, 27, 36, 37]
and two published from 1991 through 2017. [26, 38]Injection procedures Five studies found decreased use of injection procedures with DC care;
all were published from 2018 through 2022. [9, 27–29, 36]Specialist visits (including surgeon referral visits) Five studies found fewer referrals for specialist visits with DC care;
three were published from 2018 through 2022 [9, 29, 31]
and two published 1991–2017 [32, 33].
Three studies in the 1991–2017 group stated that their analyses had excluded all referral costs. [47, 48, 61]Emergency department (ED) visits Two studies, both published from 2018 through 2022,
found that fewer ED visits were associated with DC care. [9, 28]
Discussion
The purpose of this systematic review was to address our primary research question: Is chiropractic management of spine-related musculoskeletal pain in U.S. adults associated with lower overall healthcare costs as compared to medical care? This is the first systematic review of this type performed since 2015. In that review, Dagenais et al. found that health care costs were generally lower among patients whose spine pain was managed with chiropractic care. Due to the heterogeneity of patient populations and sample sizes each paper was evaluated by three separate reviewers using the checklists previously described in the Methods Sect. [15] As the literature review progressed, we found that in studies published within the past few years, an important aspect of cost began to emerge that went beyond the immediate per episode cost: the type of initial provider was strongly associated with lower downstream costs.
Downstream costs are often incurred after the initial provider has completed the episode of care. Downstream financial costs include expensive and invasive procedures such as hospitalization, surgery, injection procedures and advanced imaging. There are additional financial and non-financial downstream costs associated with the long-term consequences of addiction to opioid analgesics, including work absenteeism, decreased quality of life, psychological distress, and death due to drug overdose.
Bise et al. continued pursuing this concept in a 2023 cohort study, finding an association between the first choice of provider and future healthcare utilization. [64] His team concluded that both chiropractors and physical therapists provide nonpharmacologic and nonsurgical interventions, and that their early use appears to be associated with a decrease in immediate and long-term utilization of healthcare resources. This study adds further confidence in the emerging body of evidence on provider-related cost differentials and provides a compelling case for the influence of conservative care providers as the first provider managing for spine-related musculoskeletal pain. It follows logically that if downstream interventions are reduced, lower healthcare system costs will follow.
nonpharmacologic and nonsurgical interventions, and that their early use appears to be associated with a decrease in immediate and long-term utilization of healthcare resources. This study adds further confidence in the emerging body of evidence on provider-related cost differentials and provides a compelling case for the influence of conservative care providers as the first provider managing for spine-related musculoskeletal pain. It follows logically that if downstream interventions are reduced, lower healthcare system costs will follow.
The potential human and societal cost savings of avoiding overuse of opioid analgesics, with the possibility of overdoses and addiction, is another important emerging concept in the literature. We found that 10 studies published since the U.S. government declared the opioid epidemic in 2017 found reduced dispensing of opioid prescriptions when DCs were the first provider. [5, 12, 29, 36, 37, 39, 43–46] Only one study published in the earlier time period (1991–2017) included opioid prescribing as a comparison. [41]
Overall, as summarized in Table 4, diagnostic imaging, opioid utilization, surgery, hospitalizations, injection procedures, specialist visits and emergency department visits were all reduced where chiropractors were involved early in the case. We did not subcategorize the patient populations (e.g., general population, Medicare, insurance claims) within any of tables.
Limitations of the study
First, most of the included studies were retrospective cohort studies using large databases. Observational studies can only show associations, not prove causation, so definitive conclusions cannot be made about costs. However, their findings were so consistent that they warrant further scrutiny using higher-level study designs. Second, most of the included studies were retrospective cohort studies and therefore not the highest level of evidence. Third, we did not use any single validated checklist to assess study quality. We evaluated several checklists (e.g., SIGN, CHESS, MMAT) before determining that modification of validated checklists was necessary. Existing checklists seemed better-suited to prospective cohort designs and not as well-suited to the included retrospective cohort designs. The included studies were so variable in design and patient populations that it was not possible to pool the results for meta-analysis. Fourth, some large established datasets contained limited cost outcome variables. This made important factors such as pharmaceutical use and costs unavailable if they were not included in the dataset. Fifth, some observational studies using claims data and electronic health records do not provide enough detailed clinical information to determine whether opioid prescriptions were filled, or if filled, were actually used by the patient. Lastly, we searched only the MEDLINE database, and it is possible we missed other relevant articles not indexed there.
Strengths
Although there are few randomized controlled trials available on this topic, there were many well-conducted cohort studies that provided analyses of large datasets with cost and care data identified by provider type.
While there are certainly other factors affecting cost of care, this paper included the most common cost escalators associated with typical care for LBP, including opioids, injection procedures, surgery, specialist visits and emergency department visits.
Based on the substantial body of evidence published since 1991, a trend is developing in US healthcare systems to include chiropractors as an integral part of the medical/healthcare team, as exemplified by the Veterans Administration (VA) chiropractic clinics across the country. [65, 66]
Recommendations. When considering this evidence, it may be in society’s best interest for U.S. healthcare organizations and governmental agencies to consider modifying benefit designs to reduce barriers to access to chiropractic providers. Modifying or eliminating pre-authorization requirements, medical doctor gatekeepers, arbitrary visit limits, co-pays and deductibles may all be considered. Eliminating these barriers would allow easier access to chiropractic services, which based on currently available evidence consistently demonstrate reduced downstream services and associated costs.
Conclusion
Patients with spine-related musculoskeletal pain who consulted a chiropractor as their initial provider incurred substantially decreased downstream healthcare services and associated costs, resulting in lower overall healthcare costs compared with medical management. A primary limitation was related to the heterogeneity and sample sizes of the populations and retrospective data sets. While observational studies cannot prove causation, the recurrent theme of the data seems to support the utilization of chiropractors as the initial provider for an episode of spine-related musculoskeletal pain. Future studies using randomized designs will be helpful in clarifying and validating this trend.
Supplementary Material
Additional File 1 Search Strategy (14K, docx)
Additional File 2 Articles excluded after full-text screening (20K, docx)
Additional File 3 Quality assessment details (32K, docx)Author contributions
Conception/design: RF, CH, DT, CD, JW, MS.
Acquisition of data: CN, CH, RF, CD, JW, MS.
Analysis/interpretation of data: RF, CH, DT, CD, CN, MS, JM, WW, RW, RS, LS, JW.
Drafting and revising manuscript: RF, CH, DT, CD, CN, MS, JM, WW, RW, RS, LS, JW.
Approved the submitted version of manuscript: RF, CH, DT, CD, CN, MS, JM, WW, RW, RS, LS, JW.
All authors agreed both to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work are resolved and documented: RF, CH, DT, CD, CN, MS, JM, WW, RW, RS, LS, JW.
All authors’ initials: RF, CH, DT, CD, CN, MS, JM, WW, RW, RS, LS, JW.
Funding
This project was supported in part by the Clinical Compass and the NCMIC Foundation.
Competing interests
The authors declare that they have no competing interests.
References
Global Burden of Disease 2019 Diseases and Injuries Collaborators.
Global burden of 369 diseases and injuries in 204 countries and territories,
1990–2019: a systematic analysis for the Global Burden of Disease Study 2019.
Lancet (London, England). 2020;396(10258):1204–22.Dieleman JL, Cao J, Chapin A, Chen C, Li Z, Liu A, et al.
US Health Care Spending by Payer and Health Condition, 1996-2016
JAMA 2020 (Mar 3); 323 (9): 863–884Hawk C, Whalen W, Farabaugh RJ, et al.
Best Practices for Chiropractic Management of Patients with
Chronic Musculoskeletal Pain: A Clinical Practice Guideline
J Altern Complement Med 2020 (Oct); 26 (10): 884–901Whalen W, Farabaugh RJ, Hawk C, Minkalis AL, Lauretti W, Crivelli LS, et al.
Best-Practice Recommendations for Chiropractic
Management of Patients With Neck Pain
J Manipulative Physiol Ther. 2019 (Nov); 42 (9): 635–650Harwood KJ , Pines JM , Andrilla CHA , et al .
Where to Start? A Two Stage Residual Inclusion Approach to
Estimating Influence of the Initial Provider on Health Care
Utilization and Costs for Low Back Pain in the US
BMC Health Serv Res 2022 (May 23); 22 (1): 694Clarke TC, Barnes PM, Black LI, Stussman BJ, Nahin RL.
Use of yoga, meditation, and chiropractors among U.S. adults aged 18 and over.
NCHS Data Brief. 2018;325:1–8.Qaseem A , Wilt TJ , McLean RM , et al .
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Murphy DR, Justice B, Bise CG, Timko M, Stevans JM, Schneider MJ.
The primary spine practitioner as a new role in healthcare systems in North America.
Chiropr Man Therap. 2022;30(1):6.
doi: 10.1186/s12998-022-00414-8.Whedon JM, Kizhakkeveettil A, Toler AW, Bezdjian S, Rossi D, Uptmor S, et al.
Initial Choice of Spinal Manipulation Reduces Escalation of Care for
Chronic Low Back Pain Among Older Medicare Beneficiaries
Spine (Phila Pa 1976) 2022 (Feb 15); 47 (4): E142–E148Gold HT, McDermott C, Hoomans T, Wagner TH.
Cost data in implementation science:
categories and approaches to costing.
Implement Sci. 2022;17(1):11.
doi: 10.1186/s13012-021-01172-6.Sajid IM, Parkunan A, Frost K.
Unintended consequences: quantifying the benefits, iatrogenic harms
and downstream cascade costs of musculoskeletal MRI in UK primary care.
BMJ Open Qual. 2021;10(3):e001287.
doi: 10.1136/bmjoq-2020-001287.Rhon DI, Greenlee TA, Fritz JM.
The influence of a guideline-concordant stepped care approach on downstream
health care utilization in patients with spine and shoulder pain.
Pain Med. 2019;20(3):476–485.
doi: 10.1093/pm/pny212.Haffajee RL, Frank RG.
Making the opioid public health emergency effective.
JAMA Psychiat. 2018;75(8):767–768.
doi: 10.1001/jamapsychiatry.2018.0611.Hedegaard H, Miniño AM, Spencer MR, Warner M.
Drug overdose deaths in the United States, 1999–2020.
NCHS Data Brief. 2021;426:1–8.Dagenais S, Brady O, Haldeman S, Manga P.
A Systematic Review Comparing the Costs of Chiropractic Care
to other Interventions for Spine Pain in the United States
BMC Health Serv Res. 2015 (Oct 19); 15: 474Reeves BCDJ, Higgins JPT, Shea B, Tugwell P, Wells GA,
Chapter 24: Including non-randomized studies on intervention effects.
In: Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, eds, , editor.
Cochrane Handbook for Systematic Reviews of Interventions version 63 Cochrane; 2022.Ng JY, Dhawan T, Dogadova E, Taghi-Zada Z, Vacca A, Fajardo RG, et al.
A comprehensive search string informed by an operational definition
of complementary, alternative, and integrative medicine for systematic
bibliographic database search strategies.
BMC Complement Med Ther. 2022;22(1):200.
doi: 10.1186/s12906-022-03683-1.Andronis L, Kinghorn P, Qiao S, Whitehurst DG, Durrell S, McLeod H.
Cost-Effectiveness of Non-Invasive and Non-Pharmacological Interventions
for Low Back Pain: A Systematic Literature Review
Applied Health Econ and Health Policy 2017 (Apr); 15 (2): 173–201Kellermeyer LHB, Knight S.
Covidence and rayyan.
J Med Libr Assoc. 2018;106(4):580–583.
doi: 10.5195/jmla.2018.513.Miller J.
The scottish intercollegiate guidelines network (SIGN)
Br J Diabetes Vasc Dis. 2002;2(1):47–49.
doi: 10.1177/14746514020020010401.National Heart LaBI.
Study quality assessment tools. 2021.Buchter RB, Weise A, Pieper D.
Development, testing and use of data extraction forms in
systematic reviews: a review of methodological guidance.
BMC Med Res Methodol. 2020;20(1):259.
doi: 10.1186/s12874-020-01143-3.Carey TS, Garrett J, Jackman A, McLaughlin C, Fryer J, Smucker DR.
The Outcomes and Costs of Care for Acute Low Back Pain Among Patients
Seen by Primary Care Practitioners, Chiropractors, and Orthopedic
Surgeons The North Carolina Back Pain Project
New England J Medicine 1995 (Oct 5); 333 (14): 913–917Elder C, DeBar L, Ritenbaugh C, Dickerson J, Vollmer WM, Deyo RA, et al.
Comparative Effectiveness of Usual Care With or Without Chiropractic
Care in Patients with Recurrent Musculoskeletal Back and Neck Pain
J Gen Intern Med. 2018 (Sep); 33 (9): 1469–1477Graves JM, Fulton-Kehoe D, Martin DP, Jarvik JG, Franklin GM.
Factors associated with early magnetic resonance imaging utilization
for acute occupational low back pain: a population-based
study from Washington State workers' compensation.
Spine. 2012;37(19):1708–1718.
doi: 10.1097/BRS.0b013e31823a03cc.Keeney BJ, Fulton-Kehoe D, Turner JA, Wickizer TM, Chan KC, Franklin GM.
Early Predictors of Lumbar Spine Surgery After Occupational Back
Injury: Results From a Prospective Study of Workers in Washington State
Spine (Phila Pa 1976). 2013 (May 15); 38 (11): 953–964Anderson BR, McClellan SW.
Three Patterns of Spinal Manipulative Therapy for Back Pain and
Their Association With Imaging Studies, Injection Procedures, and
Surgery: A Cohort Study of Insurance Claims
J Manipulative Physiol Ther 2021 (Nov); 44 (9): 683–689Anderson BR, McClellan WS, Long CR.
Risk of treatment escalation in recipients vs nonrecipients of spinal manipulation
for musculoskeletal cervical spine disorders: an analysis of insurance claims.
J Manipulative Physiol Ther. 2021;44(5):372–377.
doi: 10.1016/j.jmpt.2021.03.001.Bezdjian S, Whedon JM, Russell R, Goehl JM, Kazal LA., Jr
Efficiency of Primary Spine Care as Compared to Conventional
Primary Care: A Retrospective Observational Study at
an Academic Medical Center
Chiropractic & Manual Therapies 2022 (Jan 6); 30: 1Davis M, Yakusheva O, Liu H, Anderson B, Bynum J.
The Effect of Reduced Access to Chiropractic Care
on Medical Service Use for Spine Conditions
J Manipulative Physiol Ther 2021 (Jun); 44 (5): 353–362Davis MA, Yakusheva O, Liu H, Tootoo J, Titler MG, Bynum JPW.
Access to Chiropractic Care and the Cost
of Spine Conditions Among Older Adults
American J Managed Care 2019 (Aug); 25 (8): e230–e236Fritz JM, Kim J, Dorius J.
Importance of the Type of Provider Seen to Begin Health Care for a New
Episode Low Back Pain: Associations with Future Utilization and Costs
J Eval Clin Pract. 2016 (Apr); 22 (2): 247–252Hong AS, Ross-Degnan D, Zhang F, Wharam JF.
Clinician-level predictors for ordering low-value imaging.
JAMA Intern Med. 2017;177(11):1577–1585.
doi: 10.1001/jamainternmed.2017.4888.Hurwitz EL, Li D, Guillen J, Schneider MJ, Stevans JM, Phillips RB, et al.
Variations in Patterns of Utilization and Charges for the Care of Neck
Pain in North Carolina, 2000 to 2009: A Statewide Claims' Data Analysis
J Manipulative Physiol Ther. 2016 (May); 39 (4): 240–251
This is one of the 3 of Hurwitz's Cost-Effectiveness Triumvirate articlesHurwitz EL, Li D, Guillen J, Schneider MJ, Stevans JM, Phillips RB, et al.
Variations in Patterns of Utilization and Charges for the Care of Low Back Pain
in North Carolina, 2000 to 2009: A Statewide Claims' Data Analysis
J Manipulative Physiol Ther. 2016 (May); 39 (4): 252-262Jin MC, Jensen M, Zhou Z, Rodrigues A, Ren A, Barros Guinle MI, et al.
Health care resource utilization in management of opioid-naive patients
with newly diagnosed neck pain.
JAMA Netw Open. 2022;5(7):e2222062.
doi: 10.1001/jamanetworkopen.2022.22062.Kazis LE, Ameli O, Rothendler J, Garrity B, Cabral H, McDonough C, et al.
Observational Retrospective Study of the Association of Initial Healthcare
Provider for New-onset Low Back Pain with Early and Long-term Opioid Use
BMJ Open. 2019 (Sep 20); 9 (9): e028633Liliedahl RL, Finch MD, Axene DV, Goertz CM.
Cost of Care for Common Back Pain Conditions Initiated with Chiropractic
Doctor vs Medical Doctor/Doctor of Osteopathy as First Physician: Experience
of One Tennessee-Based General Health Insurer
J Manipulative Physiol Ther 2010 (Nov); 33 (9): 640–643Louis CJ, Herrera CS, Garrity BM, McDonough CM, Cabral H, Saper RB, et al.
Association of Initial Provider Type on Opioid Fills
for Individuals With Neck Pain
Archives of Phys Med and Rehab 2020 (Aug); 101 (8): 1407–1413Weeks WB, Goertz CM.
Cross-Sectional Analysis of Per Capita Supply of Doctors of Chiropractic
and Opioid Use in Younger Medicare Beneficiaries
J Manipulative Physiol Ther. 2016 (May); 39 (4): 263–266Weeks WB, Leininger B, Whedon JM, Lurie JD, Tosteson TD, Swenson R, et al.
The Association Between Use of Chiropractic Care and Costs of Care
Among Older Medicare Patients With Chronic Low Back Pain
and Multiple Comorbidities
J Manipulative Physiol Ther. 2016 (Feb); 39 (2): 63–75Whedon JM, Kizhakkeveettil A, Toler A, MacKenzie TA, Lurie JD, Bezdjian S, et al.
Long-Term Medicare Costs Associated with Opioid Analgesic Therapy vs
Spinal Manipulative Therapy for Chronic Low Back Pain
in a Cohort of Older Adults
J Manipulative Physiol Ther 2021 (Sep); 44 (7): 519-526Whedon JM, Kizhakkeveettil A, Toler AW, MacKenzie TA, Lurie JD, Hurwitz EL, et al.
Initial Choice of Spinal Manipulation Reduces Escalation of Care for
Chronic Low Back Pain Among Older Medicare Beneficiaries
Spine (Phila Pa 1976) 2022 (Feb 15); 47 (4): E142–E148Whedon JM, Toler AWJ, Goehl JM, Kazal LA.
Association Between Utilization of Chiropractic Services for
Treatment of Low-Back Pain and Use of Prescription Opioids
J Altern Complement Med. 2018 (Jun); 24 (6): 552–556Whedon JM, Toler AWJ, Kazal LA, Bezdjian S, Goehl JM, Greenstein J.
Impact of Chiropractic Care on Use of Prescription Opioids
in Patients with Spinal Pain
Pain Medicine 2020 (Dec 25); 21 (12): 3567–3573Whedon JM, Uptmor S, Toler AWJ, Bezdjian S, MacKenzie TA, Kazal LA., Jr
Association Between Chiropractic Care and Use of Prescription Opioids
Among Older Medicare Beneficiaries with Spinal Pain:
A Retrospective Observational Study
Chiropractic & Manual Therapies 2022 (Jan 31); 30: 5Grieves B, Menke JM, Pursel KJ.
Cost minimization analysis of low back pain claims data for
chiropractic vs medicine in a managed care organization.
J Manipulative Physiol Ther. 2009;32(9):734–739.
doi: 10.1016/j.jmpt.2009.10.001.Haas M, Sharma R, Stano M.
Cost-effectiveness of Medical and Chiropractic Care for
Acute and Chronic Low Back Pain
J Manipulative Physiol Ther 2005 (Oct); 28 (8): 555–563Jarvis KB, Phillips RB, Morris EK.
Cost Per Case Comparison of Back Injury Claims of Chiropractic Versus
Medical Management for Conditions With Identical Diagnostic Codes
J Occupational and Environmental Med 1991 (Aug); 33 (8): 847–852Kominski GF, Heslin KC, Morgenstern H, Hurwitz EL, Harber PI.
Economic evaluation of four treatments for low-back pain:
results from a randomized controlled trial.
Med Care. 2005;43(5):428–435.
doi: 10.1097/01.mlr.0000160379.12806.08.Legorreta AP, Metz RD, Nelson CF, Ray S, Chernicoff HO, Dinubile NA.
Comparative analysis of individuals with and without chiropractic coverage:
patient characteristics, utilization, and costs.
Arch Intern Med. 2004;164(18):1985–1992.
doi: 10.1001/archinte.164.18.1985.Leininger B, McDonough C, Evans R, Tosteson T, Tosteson AN, Bronfort G.
Cost-effectiveness of Spinal Manipulative Therapy, Supervised Exercise,
and Home Exercise for Older Adults with Chronic Neck Pain
Spine J. 2016 (Nov); 16 (11): 1292–1304Mosley CDCI, Arnold AM.
Cost-effectiveness of chiropractic care in a managed care setting.
Am J Man Care. 1996;2(3):280–282. [Google Scholar]Nelson CF, Metz RD, LaBrot T.
Effects of a Managed Chiropractic Benefit on the Use of Specific Diagnostic
and Therapeutic Procedures in the Treatment of Low Back and Neck Pain
J Manipulative Physiol Ther 2005 (Oct); 28 (8): 564–569Phelan SP, Armstrong RC, Knox DG, Hubka MJ, Ainbinder DA.
An Evaluation of Medical and Chiropractic Provider Utilization and Costs:
Treating Injured Workers in North Carolina
J Manipulative Physiol Ther 2004 (Sep); 27 (7): 442–448Shekelle PG, Markovich M, Louie R.
Comparing the Costs Between Provider Types of Episodes of Back Pain Care
Spine (Phila Pa 1976) 1995 (Jan 15); 20 (2): 221–227Smith M, Stano M.
Costs and Recurrences of Chiropractic and Medical Episodes of Low-back Care
J Manipulative Physiol Ther 1997 (Jan); 20 (1): 5–12Stano M.
A Comparison of Health Care Costs for Chiropractic and Medical Patients
J Manipulative Physiol Ther 1993 (Jun); 16 (5): 291–299Stano M.
The economic role of chiropractic: an episode analysis of relative insurance costs for low back care.
J Neuromusculoskeletal Sys. 1993;1(2):64–68Stano M.
Further Analysis of Health Care Costs for Chiropractic and Medical Patients
J Manipulative Physiol Ther 1994 (Sep); 17 (7): 442–446Stano M, Haas M, Goldberg B, Traub PM, Nyiendo J.
Chiropractic and Medical Care Costs of Low Back Care:
Results From a Practice-Based Observational Study
Am J Manag Care 2002 (Sep); 8 (9): 802-809Stano M, Smith M.
Chiropractic and Medical Costs of Low Back Care
Medical Care 1996 (Mar); 34 (3): 191–204 Cherkin DC, Deyo RA, Battié M, Street J, Barlow W.
Cherkin DC, Deyo RA, Battié M, Street J, Barlow W.
A Comparison of Physical Therapy, Chiropractic Manipulation, and Provision
of an Educational Booklet for the Treatment of Patients with Low Back Pain
New England Journal of Medicine 1998 (Oct 8); 339 (15): 1021-1029Bise CG, Schneider M, Freburger J, Fitzgerald GK, Switzer G, Smyda G, et al.
First Provider Seen for an Acute Episode of Low Back Pain
Influences Subsequent Health Care Utilization
Physical Therapy 2023 (Jun 28); 103 (9): pzad067Corcoran KL, Peterson DR, Jr, Zhao X, Moran EA, Lisi AJ.
Characteristics and Productivity of the Chiropractic
Workforce of the Veterans Health Administration
Chiropractic & Manual Therapies 2022 (Apr 11); 30: 18Lisi AJ, Brandt CA.
Trends in the Use and Characteristics of Chiropractic Services
in the Department of Veterans Affairs
J Manipulative Physiol Ther. 2016 (Jun); 39 (5): 381–386

Return to COST-EFFECTIVENESS
Return to SPINAL PAIN MANAGEMENT
Return to INITIAL PROVIDER/FIRST CONTACT
Since 5-05-2024

| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |