

Health Maintenance Care in Work-Related
Low Back Pain and Its Association
With Disability RecurrenceThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Occupat Enviro Med 2011 (Apr); 53 (4): 396–404 ~ FULL TEXT
OPEN ACCESS Manuel Cifuentes, MD, PhD, Joanna Willetts, MS, and Radoslaw Wasiak, PhD, MA, MSc
From the Center for Disability Research at the Liberty Mutual Research Institute for Safety
(Dr Cifuentes and Ms Willetts) and
University of Massachusetts Lowell
(Dr Cifuentes), Hopkinton, Mass; and
Center for Health Economics & Science Policy at United BioSource Corporation,
London, United Kingdom (Dr Wasiak).

FROM: Keeney ~ Spine 2013 (May 15)
This study is unique in that it was conducted by the Center for Disability Research at the Liberty Mutual Research Institute for Safety AND the University of Massachusetts Lowell, Hopkinton, Mass
Their objective was to compare the occurrences of repeated disability episodes between types of health care providers, who treat claimants with new episodes of work-related low back pain (LBP). They followed 894 patients over 1-year, using workers’ compensation claims data.
By controlling for demographics and severity, they determined the hazard ratio (HR) for disability recurrence between 3 types of providers:Physical Therapists (PT),
Physicians (MD), or
Chiropractors (DC).The results are quite interesting:
- For PTs: HR = 2.0
- For MDs: HR = 1.6
- For DCs: HR = 1.0
Statistically, this means you are twice as likely to end up disabled if you got your care
from a Physical Therapists (PT), rather than from a chiropractor.
You’re also 60% more likely to be disabled if you choose a Physicians (MD)
to manage your care, rather than a chiropractor.
The authors concluded:“In work-related nonspecific LBP, the use of health maintenance care provided by physical therapist or physician services was associated with a higher disability recurrence than with chiropractic services.”
OBJECTIVES: To compare occurrence of repeated disability episodes across types of health care providers who treat claimants with new episodes of work-related low back pain (LBP).
METHOD: A total of 894 cases followed 1 year using workers' compensation claims data. Provider types were defined for the initial episode of disability and subsequent episode of health maintenance care.
RESULTS: Controlling for demographics and severity, the hazard ratio [HR] of disability recurrence for patients of physical therapists (HR = 2.0; 95% confidence interval [CI] = 1.0 to 3.9) or physicians (HR = 1.6; 95% CI = 0.9 to 6.2) was higher than that of chiropractor (referent, HR = 1.0), which was similar to that of the patients non-treated after return to work (HR = 1.2; 95% CI = 0.4 to 3.8).
CONCLUSIONS: In work-related nonspecific LBP, the use of health maintenance care provided by physical therapist or physician services was associated with a higher disability recurrence than in chiropractic services or no treatment.
From the Full-Text Article:
Introduction
Low back pain (LBP) continues to be one of the costliest work-related injuries in the United States in terms of disability and treatment costs. [1, 2] An additional, important component of the human and economic costs is the recurrence of LBP. [3] Recurrences of LBP are complex to study because of the difficulty in predicting recurrence and the varying definitions and measurements of recurrence. [4–9] So far, there has been little success in preventing recurrent LBP with few studies to investigate this topic. More evidence is needed to understand recurrent LBP and justify interventions to prevent recurrence.
Health maintenance care is a clinical intervention approach thought to prevent recurrent episodes of LBP. It conceptually refers to the utilization of health care services with the aim of improving health status and preventing recurrences of a previous health condition. Breen’s original definition of health maintenance care [10, 11] refers to “treatment after optimum recorded benefit was reached.” The definition of optimum is subject to interpretation, making it difficult to clearly distinguish curative treatment from health maintenance; it blends the public health concepts of secondary prevention (treatment and prevention of recurrences) with tertiary prevention (obtaining the best health condition while having an incurable disease). [10] Health maintenance care can include providing advice, information, counseling, and specific physical procedures. [10–12] Health maintenance care is predominantly and explicitly recommended by chiropractors, although some physical therapists also advocate health maintenance procedures to prevent recurrences. [12] Physicians do not use this terminology when assisting a patient that has reached an optimum level.
There have been few scientific studies to evaluate the effectiveness of health maintenance care. A 2008 review found only 13 eligible citations and did not arrive at any conclusion about its effectiveness, and the operational definitions of health maintenance care were vague at best. [10] None of these citations referred to work-related LBP.
In the occupational health field, sustained return-to-work is considered an important goal during injury recovery. Given the patient’s condition and context, going back out of work is considered an appropriate measurement of a recurrent condition because it reflects the non-sustainability of working and implies a failure of the return-to-work process. However, it is possible that different providers focus more on return to work (eg, chiropractors) than others (eg, physicians that could focus more on pain control). An association between specific type(s) of treatment or providers and significant recurrence of a condition (measured as recurrent work disability) could imply an important advancement in the treatment of work-related back injuries.
Work-related LBP is often treated by a combination of providers, including chiropractors, physical therapists, and physicians. Given that chiropractors are proponents of health maintenance care, we hypothesize that patients with work-related LBP who are treated by chiropractors would have a lower risk of recurrent disability because that specific approach would be used. Conversely, similar patients treated by other providers would have higher recurrence rates because the general approach did not include maintaining health, which is a key concept to prevent recurrence. Unfortunately, there is no available data that could allow direct characterization of which procedures were specifically product of the health maintenance care approach. Therefore, the present study aims to study the association between provider type during the initial period of return to work and risk of recurrence of disability due to work-related LBP.
METHODS
Study Population
After institutional review board approval, data were extracted from the administrative records of a large insurance company that represents approximately 10% of the US workers’ compensation with coverage to a broad array of states, industries, and company sizes. Claims filed in Illinois, Massachusetts, Maryland, New Hampshire, New York, Texas, and Wisconsin between January 1, 2006, and December 31, 2006, were reviewed because claimants in these states can choose the provider they prefer to see for a work-related injury. [13] A total of 11,420 nonspecific LBP cases were identified by body part (lower back, sacrum, coccyx, or multiple trunk) and nature of injury (sprain or strain) codes. All claimants were followed from the date of injury until 12 months after the first episode of disability. Claimants who did not receive any paid disability were excluded (n = 7552). To capture new episodes of LBP cases, claimants who filed a workers’ compensation claim in the prior year were identified by using the same LBP identification criteria and excluded (n = 227). [14, 15]
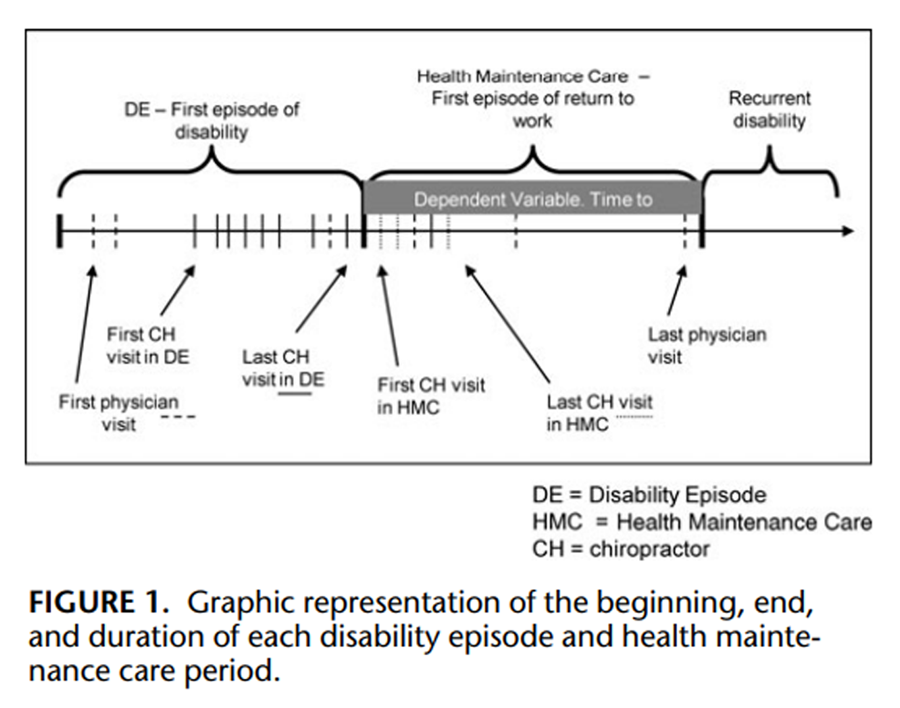
Figure 1 Temporary total disability compensation information, defined as the worker completely unable to work on a temporary basis due to health related impairment, for each claimant was used to determine the beginning, end, and duration of each disability episode and health maintenance care period (Figure 1). The health maintenance care period of interest was defined as the period after the initial disability episode had ended and the person had returned to work for more than 14 days. Temporary partial disability periods, defined as the worker returning to work but on an alternate duty job, usually part time with lower wages, were defined as periods where the claimant was working and were included in the health maintenance care periods.
Recurrent disability was defined as a resumption of temporary total disability compensation after an episode of health maintenance care. If the first disability episode was 7 days or less, the claimant was excluded from the data set (n = 755) because there is a waiting period for disability compensation of up to 7 days that varies by state. Including these claimants with 7 days or less of disability would have introduced misclassification in the measure of disability duration. If the health maintenance care period was 7 days or less, it was assumed that the person was not truly ready to be back at work, and this period was included in the initial disability episode that bounded it. Claimants with a health maintenance care period between 8 and 14 days were excluded from the study cohort under the assumptions that it is not likely that the actual pattern of service utilization during this period could have been properly determined in such short time period (n = 69).
To obtain a homogeneous study population, additional cases were excluded according to the following criteria:(1) More than one injury date was reported for the same claim (19 excluded);
(2) The first disability episode began more than 7 days after the injury occurred, which ensured that all cases shared similar severity/complexity with respect to requirements for work disability within the first week after the injury (652 excluded);
(3) The claimant had fewer than four physical therapy or chiropractic visits during the disability episode period, which could have resulted in improper characterization of disability episode period treatment because of unstable numbers (1182 excluded);
(4) The claimant was younger than 17 or older than 65 years old (13 excluded);
(5) The first medical visit occurred more than 14 days after the injury occurred, which implies a retroactive evaluation of work causality where cases could have received some type of treatment not included in claim bills, causing misclassification of received health care (33 excluded);
(6) During first medical visit, none of the diagnoses was related to LBP (18 excluded);
(7) The follow-up of the health maintenance care period was less than 1 year when censored at July 31, 2008 (73 excluded).
(8) Incomplete data (two excluded). The final study cohort was composed of 894 cases.
Measurements
Exposure Variable: Provider Type During Health Maintenance Care Period

Table 1 An algorithm, based on standard medical procedure (current procedural terminology), provider, and other company-specific provider codes, was designed and implemented to designate each visit as physical therapy, chiropractic, or physician services. Given that each patient could utilize any combination of physical therapy, chiropractic, and/or physician visit(s), the provider for which the patient sought care for more than 50% of visits defined the provider type. Cases who did not receive health care during the health maintenance care period or who could not be properly classified were also included as separate groups (Table 1).
Provider type during disability episode period was used as a sensitivity analysis. With the same purpose, we defined separate groups for preferred provider type during both periods to account for potential changes in the provider type between disability episode and health maintenance care (Table 1).
For Tables 2-4, please refer to the FULL TEXT Article
Outcome Variable
Time-to-disability-recurrence was the outcome variable. This was defined as the number of days between the first day of returning to work for at least 15 consecutive days after the initial disability episode until the day before recurrence of disability. Recurrent disability was defined as the resumption of at least 15 consecutive days of temporary total disability payments following the health maintenance care period.
Covariates
Demographic variables were age, gender, and job tenure. Severity was measured using a modified classification system developed by Krause et al. [16] Cases were assigned to the high severity group, if they received any medical service with an International Classification of Diseases, 9th Edition, diagnostic code compatible with radiculopathy, spinal stenosis, instability, or sequelae of prior back surgery within the first 2 weeks after injury, and to the low severity group in the absence of any of these codes. [15] The following variables were also included as proxies of initial severity:Comorbidity was defined as the presence or absence of any non-LBP diagnosis reported during the first 15 days after the onset of the claim (previously described as a confounder of the association between provider type and LBP recurrence [17]);
surgery during disability episode or health maintenance care periods (two cases had surgery during health maintenance care period); and
opioid use (yes/no), average weekly treatment cost for disability episode and health maintenance care periods, and duration of the initial episode of disability.Because worker’s compensation in the United States is regulated at the state level, state of jurisdiction was also included. Using claim information to describe job title, occupation was manually coded using the O * NET 13 database, which allowed job-level working conditions to be attributed to each case using exposure algorithms designed and validated in previous studies. [18–21]
Job-level physical and psychosocial indicators of exposure were obtained for most job titles in the sample (92 cases [10.3%] could not be coded). In addition, occupations were grouped into O * NET job families according to O * NET Web page at:
http://online.onetcenter.org/find/
Analysis
Descriptive statistics for severity indicators were compared for each type of exposure measure. Exposure measures and categorical covariates were also compared for presence of recurrent disability. Cox regression models were used to estimate the association between exposure (referent group: those identified as only or mostly visiting a chiropractor) with time-to-disability recurrence after controlling for potential confounders. To be considered a confounder, a covariate had to change the exposure coefficient by at least 15% of its value after its inclusion in the original hazard regression model. A series of three nested multivariate models was created in a step-wise forward manner. First, the exposure variable was included as the only predictor in the model; then, demographic indicators were added; and finally, severity indicators were included. Only those variables that were significant or identified as confounders for the next step were kept in the nested model that followed. To prevent bias due to improper case-mix adjustment, the association between the covariate and the outcome was checked to ensure that it did not vary across the exposure categories. [22] Those variables with varying association levels across exposure categories were excluded from the final model. SAS 9.2 (SAS, Inc, Cary, NC) was used to analyze the data.
RESULTS
Our cohort consisted of 894 cases with a median age of 41 years (interquartile range [IQR] = 33 to 49), among whom 32% were women. The median job tenure was 2 years (IQR = 0.0 to 7.0). The most frequent O * NET job families weretransportation and material moving (29.1%),
production (12.8%),
office and administrative support (9.6%), and
building and ground cleaning (6.0%).New York (27.0%), Texas (20.4%), and Illinois (18.1%) were the states with the largest contribution to the sample.
Table 1 describes the frequency and proportion of the study cohort for the operational definitions of health care utilization during disability episode, the health maintenance care period, and both combined. During disability episode, the largest group was only or mostly visits to a physical therapist (48%), followed by only or mostly visits to a chiropractor (27%). During the health maintenance care period, the largest group was only or mostly visits to physician (31%) followed by only or mostly visits to physical therapist (24%) and only or mostly visits to chiropractor (21%). Sixteen percent received no medical care during the health maintenance care period.
Provider Type and Severity Indicators
Table 2 shows the frequency and proportion of each exposure category that were positively classified for each of the severity indicators. In general, except for the severity based on International Classification of Diseases, 9th Edition , those cases treated by chiropractors consistently tended to have a lower proportion in each of the categories for severity proxy compared to the other groups; fewer used opioids and had surgery. In addition, people who were mostly treated by chiropractor had, on average, less expensive medical services and shorter initial periods of disability than cases treated by other providers.
Covariates, Exposure Measures, and Disability Recurrence
Almost a tenth (11%) of the cohort experienced recurrent disability because of work-related LBP (n = 98). Among the continuous covariates, job tenure was higher in the group with no disability recurrence (5.5 vs 3.6 years). The average weekly treatment costs during disability episode was $122 higher for those who had recurrent disability in comparison to those who did not ($565 vs $444, P = 0.0019) and $318 higher during health maintenance care ($371 vs $53, P <0.0001). Duration of initial length of disability and all O * NET continuous covariates were not significantly associated with recurrent disability.
Among the categorical covariates (Table 3), the proportion of those with recurrent disability was significantly different between states of jurisdiction (P = 0.0013). Having received at least one opioid prescription during disability episode was not associated with having recurrent disability (10.1% among non–opioid users vs 14.1% among opioid users, P = 0.1227), but having received opioids during the health maintenance care period was significantly associated with recurrent disability (9.5% vs 21.6%, P = 0.0001).
Provider type during the health maintenance care period was significantly associated with recurrent disability (P = 0.0053) with the only or mostly physical therapy group having the highest proportion of recurrent disability (16.9%) and the only or mostly chiropractor and the no health maintenance care groups having the lowest proportion of recurrent disability (6.5% and 5.5%, respectively).
In sensitivity analyses, provider type during the disability episode was not significantly associated with recurrent disability (P = 0.0650). The provider type of both periods combined is also significantly associated with recurrent disability (P = 0.0056), with physician loyalists having the highest proportion of recurrent disability (16.7%) and those receiving no health maintenance care or being chiropractor loyalist having the lowest proportion of disability recurrence (5.5% and 5.7%, respectively).
Crude estimates for mean duration at work after the initial period of disability and before the recurrence were 345 (95% confidence interval [CI] = 334 to 356) days for only or mostly chiropractor during health maintenance care period, 316 (95% CI = 301 to 331) days for only or mostly physical therapy patients, and 316 (301, 331) days for only or mostly physician cases.
MULTIVARIATE SURVIVAL MODELS
Provider Type During Health Maintenance Care Period
During the health maintenance care period using unadjusted and adjusted Cox regression analysis (Table 4), a trend is seen where the hazard ratios [HRs] of disability recurrence are generally higher for the only or mostly physical therapy and only or mostly physician groups than for the only or mostly chiropractor group (referent). However, after controlling for demographics and severity indicators just the only or mostly physical therapy group remains with a higher HR (models 3 and 4). The no health maintenance care group does not have any statistically significant difference with the only or mostly chiropractor group.
EVALUATING ALTERNATIVE CATEGORIZATIONS OF EXPOSURE
Provider Type During Disability Episode
Provider type during disability episode was associated with the hazard of disability recurrence after returning to work. Compared with the only or mostly chiropractor (referent), the groups of only or mostly physical therapy and only or mostly physician had significantly higher HRs (2.0 and 2.7 respectively, model 1). After controlling for significant demographic variables (model 2), there was a slight attenuation in some HRs. After adding severity indicators (models 3), the HRs were slightly higher than the unadjusted model.
Preferred Provider Type
After controlling for demographics and severity, compared with the “chiropractor loyalist” group (referent), the “physical therapist loyalist” group had a significantly higher HR (model 3). The no health maintenance care group does not have any statistically significant difference with the chiropractor loyalist group.
The only covariate that had varying association with the outcome variable across the exposure measurements was state of jurisdiction. Therefore, a series of fully controlled models that excluded state of jurisdiction was run (model 4). Model 4 tended to have a similar or better fit than the full model that included state (model 3) and the differential effect of provider type over recurrent disability increased in the same direction as the previous models.
DISCUSSION
A cohort of 894 patients suffering work-related LBP was followed from their first episode of disability through their subsequent return-to-work (health maintenance care period). A tenth of them had recurrent disability due to LBP. After controlling for demographic and severity factors, compared with receiving treatment only or mostly by chiropractors during the health maintenance care period, receiving treatment by physical therapists, physicians, or a combination of both tended to result in significantly higher HRs of recurrent disability. Similarly, when compared to patients treated only or mostly by chiropractors during the disability episode or patients who were “chiropractor loyalists” during transition from the disability episode to the health maintenance care period, patients treated by other care providers tended to have a higher hazard of recurrent disability.
In our study, after controlling for demographics and severity indicators, the likelihood of recurrent disability due to LBP for recipients of services during the health maintenance care period by all other provider groups was consistently worse when compared with recipients of health maintenance care by chiropractors. Care from chiropractors during the disability episode (“curative”), during the health maintenance care period (main exposure variable, “preventive”), and the combination of both (curative and preventive) was associated with lower disability recurrence HRs.
This clear trend deserves some attention considering that chiropractors are the only group of providers who explicitly state that they have an effective treatment approach to maintain health.
Our findings should be viewed in the context of prior research. Few studies have addressed evaluating the effectiveness of health maintenance care. [10] Most of the reviewed studies found no clear advantage of any health maintenance approach or reported small benefits for the chiropractor maintenance care. A clinical trial found better disability indicators for patients exposed to spinal manipulation, [23] but no study compared work-related LBP recurrence rate across different providers. In 1999, Carey [17] found that in ambulatory general practice, the rate of recurrent disabling LBP was not significantly different at 6 months for chiropractors (8%), primary care physicians (9%), orthopedic surgeons (10%), and physicians and mid-level practitioners working as health maintenance organization staff (14%). The same nonsignificant results were observed at 22 months of follow-up. However, Carey’s study did not consider time to recurrence and did not utilize a multivariate model, which might have provided different results.
SUGGESTED MECHANISM OF THE CHIROPRACTOR ADVANTAGE
Our results, which seem to suggest a benefit of chiropractic treatment to reduce disability recurrence, imply that if the benefit is truly coming from the chiropractic treatment, there is a mechanism through which care provided by chiropractors improves the outcome. It is always possible that unknown patient differences, which we were not able to control for, could be acting as unadjusted confounders and eventually explain the findings. With those caveats, we dare to speculate that for the purpose of preventing disability recurrence in cases of work-related LBP, the main advantage of chiropractors could be based on the dual nature of their practice. On one hand, it is the do-nothing approach: by visiting only or mostly a chiropractor or becoming a chiropractor loyalist, the patients do not receive other traditional medical approaches. In fact, there is a continuous struggle between chiropractors and orthopedic providers regarding the most basic principles that sustain each others’ clinical practice. [24] There is a growing evidence that health-care-as-usual does not necessarily improve health outcomes in nonspecific LBP. [25, 26] This hypothesis is supported by our finding that, after controlling for severity and demographics, no health maintenance care is generally as good as chiropractor care. Therefore, not as a conclusion but a hypothesis, chiropractors might be preventing some of their patients from receiving procedures of unproven cost utility value [27] or dubious efficacy. [25, 26]
This argument has to be tempered by the fact that the most numerous group for a continued relationship with the provider (disability episode and health maintenance care) are the switchers (55 of them) and the any other combination (163 of them) groups, which together compose approximately 24% of the study group. The reasons why a small group of patients chose to switch or to combine providers during the health care maintenance period might be related to their good outcome, which is indistinguishable from the reference group. In others words, it may be possible that those switchers and any other combination groups for some reason knew what the best health care path was for them.
On the other hand, chiropractors argue that their aim is to provide care while being centered on the whole patient. It is possible that this approach provides more opportunities for a provider–patient relationship that improves communication, and likely emphasizes the importance of return to work over symptom control, and focuses on psychosocial issues that have been demonstrated to be important in the evolution of LBP disability. [28] Some of the important weakness of this hypothesis is the fact that we are attributing to a whole job title attributes that vary among individual providers. Do chiropractors truly emphasize in their practice relationship quality and communication? Do patients of non-chiropractor providers who focus on personal relationship and good communication have better health outcomes than those patients whose providers do not do so? Some studies seem to point in that direction. [29] In addition, it is important to state that this considered mechanism is not at all a chiropractor exclusivity and other care providers may similarly think along these lines. Naturalistic studies that focus on the actual experiences of the provider–patient relationships could help to test our proposed mechanisms.
Study Limitations
As shown in Table 2, the only or mostly chiropractor group during the disability episode and health maintenance care periods and “chiropractor loyalists” during both periods combined had fewer surgeries, used fewer opioids, and had lower costs for medical care than the other provider groups. Therefore, it is important to consider that the claim of more effective prevention of recurrent disability by chiropractors might be attributed to what has been called “casemix” bias, [22, 30] which may be caused by the differences between the patients that visit each provider type. Any provider treating less severe patients should have a lower risk for recurrent disability for its patients. After controlling for demographic and severity factors, only a small component of the lowest risk of recurrent disability for chiropractic patients was removed, and this group consistently had a significantly lower HR for recurrent disability than physical therapist–treated patients.
Prior research has not found a strong association between measures of LBP clinical severity and return-to-work outcomes. [31–34] Some LBP severity scores are not strongly associated with disability, and although we controlled for some clinical indicators of severity, our study did not include other important variables; for example, characteristics of previous LBP episodes; patterns of pain and impairments within the current LBP episode; health care system characteristics that divert more severely injured patients away from chiropractors (could result in better recurrence rates to that provider group); self-selection that places fully or almost fully recovered patients into health maintenance care (ie, chiropractors), while other patients seek care from providers focused on curative goals (ie, physical therapists and physicians). Therefore, the complexity of controlling for “casemix” bias with this type of condition is a problematic link in all observational studies of this type, even among those studies that include biomedical data. In addition, we did not evaluate work-related psychosocial variables at the individual level (only at the job level with O?NET), which have been established as confounders or effect modifiers for the relationship between pain and disability. [33, 35, 36]
In workers’ compensation, health maintenance care has a distinctive relevance because full health recovery is not considered a requirement for return to work. [37, 38] Therefore, a person can return to work while still symptomatic. As a consequence, what is considered to be health maintenance care by some in the occupational health field, because it occurs after the patient has returned to work, can just as easily be seen as the completion of curative treatment by others who considered that the worker was recovered just enough to return to work but not fully recovered to an optimum level as the traditional definition of health maintenance care requires. However, this operational definition of health maintenance care has the distinct advantage of having a precise temporal boundary of onset (the moment of return-to-work) and at least one clear outcome (presence or absence of disability recurrence). It is possible that health maintenance care for work-related injuries needs an updated definition. Exposure misclassification might have played a role in wrongly identifying patients to the only or mostly physician group into the only or mostly physical therapy group as physical therapy visits (2 to 3 per week) typically occur more frequently than physician visit (1 to 2 every 2 weeks). The impact of this misclassification should not have affected the risk of disability recurrence in those who typically utilized chiropractic services might have averaged out the risk of recurrent disability for those who typically utilized physical therapy/physician services.
CONCLUSION
After controlling for demographic factors and multiple severity indicators, patients suffering nonspecific work-related LBP who received health services mostly or only from a chiropractor had a lower risk of recurrent disability than the risk of any other provider type. Even without an improvement in days until recurrent disability, our findings seem to support the use of chiropractor services, as chiropractor services generally cost less than services from other providers. If a lower rate of disability recurrence in work-related LBP cases for chiropractors holds as true, it is important to identify the mechanism of action.
References:
Murphy PL, Volinn E.
Is occupational low back pain on the rise?
Spine (Phila Pa 1976). 1999;24:691–697.Dagenais S, Caro J, Haldeman S.
A Systematic Review of Low Back Pain Cost of Illness Studies
in the United States and Internationally
Spine J 2008 (Jan); 8 (1): 8–20Wasiak R, Kim J, Pransky G.
Work disability and costs caused by recurrence of low back pain:
longer and more costly than in first episodes.
Spine (Phila Pa 1976). 2006;31:219–225.Wasiak R, Pransky G, Verma S, Webster B.
Recurrence of low back pain: definition-sensitivity analysis using administrative data.
Spine (Phila Pa 1976). 2003;28:2283–2291.Wasiak R, Pransky GS, Webster BS.
Methodological challenges in studying recurrence of low back pain.
J Occup Rehabil. 2003;13:21–31.Wasiak R, Verma S, Pransky G, Webster B.
Risk factors for recurrent episodes of care and work disability: case of low back pain.
J Occup Environ Med. 2004;46:68–76.Wasiak R, Young AE, Dunn KM, et al.
Back pain recurrence: an evaluation of existing indicators and direction for future research.
Spine (Phila Pa 1976). 2009;34:970–977.Marras WS, Ferguson SA, Burr D, Schabo P, Maronitis A.
Low back pain recurrence in occupational environments.
Spine (Phila Pa 1976). 2007;32:2387–2397.Stanton TR, Latimer J, Maher CG, Hancock M.
Definitions of recurrence of an episode of low back pain: a systematic review.
Spine (Phila Pa 1976). 2009;34:E316–E322.Leboeuf-Yde C, Hestbaek L.
Maintenance Care In Chiropractic – What Do We Know?
Chiropractic & Osteopathy 2008 (May 8); 16: 3Axen I, Rosenbaum A, Eklund A, et al.
The Nordic Maintenance Care Program – Case Management of Chiropractic Patients
With Low Back Pain: A Survey of Swedish Chiropractors
Chiropractic & Osteopathy 2008 (Jun 18); 16: 6Pincus T, Vogel S, Breen A, Foster N, Underwood M.
Persistent back pain—why do physical therapy clinicians continue treatment? A mixed methods study of chiropractors, osteopaths and physiotherapists.
Eur J Pain. 2006;10:67–76.Tanabe RP, Murray SM.
Managed Care and Medical Cost Containment in Workers’ Compensation.
A National Inventory, 2001–2002.
Cambridge, MA: Workers Compensation Research Institute; 2004:328.Webster BS, Cifuentes M, Verma S, Pransky G.
Geographic variation in opioid prescribing for acute, work-related, low back pain and associated factors: a multilevel analysis.
Am J Ind Med. 2009;52:162–171.Webster BS, Verma SK, Gatchel RJ.
Relationship between early opioid prescribing for acute occupational low back pain and disability duration, medical costs, subsequent surgery and late opioid use.
Spine. 2007;32:2127–2132.Krause N, Rugulies R, Ragland DR, Syme SL.
Physical workload, ergonomic problems, and incidence of low back injury: a 7.5-year prospective study of San Francisco transit operators.
Am J Ind Med. 2004;46:570–585.Carey TS, Garrett JM, Jackman A, Hadler N.
Recurrence and care seeking after acute back pain: results of a long-term follow-up study. North Carolina Back Pain Project.
Med Care. 1999;37:157–164.Boyer J, Galizzi M, Cifuentes M, et al.
Ergonomic and socioeconomic risk factors for hospital workers’ compensation injury claims.
Am J Ind Med. 2009;52;551–562.Cifuentes M, Boyer J, Gore R, et al.
Job strain predicts survey response in healthcare industry workers.
Am J Ind Med. 2008;51:281–289.Cifuentes M, Boyer J, Gore R, et al.
Inter-method agreement between O?NET and survey measures of psychosocial exposure among healthcare industry employees.
Am J Ind Med. 2007;50:545–553.d’Errico A, Punnett L, Cifuentes M, et al.
Hospital injury rates in relation to socioeconomic status and working conditions.
Occup Environ Med. 2007;64:325–333.Nicholl J.
Case-mix adjustment in non-randomised observational evaluations: the constant risk fallacy.
J Epidemiol Community Health. 2007;61:1010–1013.Descarreaux M, Blouin JS, Drolet M, Papadimitriou S, Teasdale N:
Efficacy of Preventive Spinal Manipulation for Chronic Low-Back Pain and Related Disabilities:
A Preliminary Study
J Manipulative Physiol Ther 2004 (Oct); 27 (8): 509–514Fitzcharles MA.
Is it time for rheumatologists to rethink the use of manual therapies?
J Rheumatol. 2002;29:1117–1120.Haldeman S, Dagenais S.
What Have We Learned About the Evidence-informed
Management of Chronic Low Back Pain?
Spine J. 2008 (Jan); 8 (1): 266–277Haldeman S, Dagenais S.
A Supermarket Approach to the Evidence-informed Management of Chronic Low Back Pain
Spine Journal 2008 (Jan); 8 (1): 1–7Dagenais S, Roffey DM, Wai EK, Haldeman S, Caro J.
Can cost utility evaluations inform decision making about interventions for low back pain?
Spine J. 2009;9:944–957.Shaw WS, Pransky G, Fitzgerald TE.
Early prognosis for low back disability: intervention strategies for health care providers.
Disabil Rehabil. 2001;23:815–828.Dasinger LK, Krause N, Thompson PJ, Brand RJ, Rudolph L.
Doctor proactive communication, return-to-work recommendation, and duration of disability
after a workers’ compensation low back injury.
J Occup Environ Med. 2001;43:515–525.Bjorkgren MA, Fries BE, Hakkinen U, Brommels M.
Case-mix adjustment and efficiency measurement.
Scand J Public Health. 2004;32:464–471.Waddell G, Newton M, Henderson I, Somerville D, Main CJ.
A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability.
Pain. 1993;52:157–168.Thelander U, Fagerlund M, Friberg S, Larsson S.
Describing the size of lumbar disc herniations using computed tomography. A comparison of different size index calculations and their relation to sciatica.
Spine (Phila Pa 1976). 1994;19:1979–1984.Takahashi N, Kikuchi S, Konno S, et al.
Discrepancy between disability and the severity of low back pain: demographic, psychologic, and employmentrelated factors.
Spine (Phila Pa 1976). 2006;31:931–939; discussion 940.Michel A, Kohlmann T, Raspe H.
The association between clinical findings on physical examination and self-reported severity in back pain. Results of a population-based study.
Spine (Phila Pa 1976). 1997;22:296–303; discussion 303–304.Hoogendoorn WE, Bongers PM, de Vet HC, et al.
Psychosocial work characteristics and psychological strain in relation to low-back pain.
Scand J Work Environ Health. 2001;27:258–267.Ghaffari M, Alipour A, Farshad AA, Jensen I, Josephson M, Vingard E.
Effect of psychosocial factors on low back pain in industrial workers.
Occup Med (Lond). 2008;58:341–347.Lotters F, Hogg-Johnson S, Burdorf AE.
Health status, its perceptions, and effect on return to work and recurrent sick leave.
Spine (Phila Pa 1976). 2005;30:1086–1092Young AE.
Employment maintenance and the factors that impact it after vocational rehabilitation and return to work.
Disabil Rehabil. 2010;32: 1621–1632
Return to LOW BACK PAIN
Return to COST-EFFECTIVENESS
Return to WORKERS' COMPENSATION
Return to MAINTENANCE CARE, WELLNESS AND CHIROPRACTIC
Since 3-17-2011


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |