

Pain Location Matters: The Impact of Leg Pain on
Health Care Use, Work Disability and Quality
of Life in Patients with Low Back PainThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: European Spine Journal 2015 (Mar); 24 (3): 444–451 ~ FULL TEXT
OPEN ACCESS Samantha L. Hider, David G. T. Whitehurst, Elaine Thomas, Nadine E. Foster
Arthritis Research UK Primary Care Centre,
Keele University, Keele,
Staffordshire, ST5 5BG, UK.
s.hider@keele.ac.uk
PURPOSE: In low back pain (LBP) patients, those with radiating leg pain or sciatica have poorer pain and disability outcomes. Few studies have assessed the effect of leg pain on health care use and quality of life.
METHODS: Prospective cohort study of 1,581 UK LBP primary care consulters. Back pain, employment, health care utilisation, and quality of life (EQ-5D) data were collected at baseline, 6 and 12 months. At baseline, patients were classified as reporting(1) LBP only
(2) LBP and leg pain above the knee only (LBP + AK) or
(3) LBP and leg pain extending below the knee (LBP + BK).RESULTS: Self-reported leg pain was common; at baseline 645 (41%) reported LBP only, 392 (25%) reported LBP + AK and 544 (34%) reported LBP + BK. Patients with LBP + BK, compared to those with LBP only, were significantly more likely to be unemployed, take time off work, consult their family doctor, receive physical therapy, or be referred to other health care practitioners. There were statistically significant decrements in EQ-5D scores for LBP + AK compared to LBP only, and for LBP + BK compared to LBP + AK (p ≤ 0.05 for all comparisons).
CONCLUSIONS: Patients with self-reported leg pain below the knee utilise more health care are more likely to be unemployed and have poorer quality of life than those with LBP only 12 months following primary care consultation. The presence of leg pain warrants early identification in primary care to explore if targeted interventions can reduce the impact and consequences of leg pain.
Keywords Low back pain Sciatica Work Health care use Quality of life EQ-5D
From the FULL TEXT Article:
Introduction
Low back pain (LBP) is a common musculoskeletal problem. Estimates suggest that LBP affects one-third of the UK population annually; of these individuals, around 20% (1 in 15 of the population) will consult their family doctor (GP) [1]. LBP-related leg pain is also common, although prevalence rates vary widely between studies, ranging from 1 to 43% of LBP patients [2], reflecting the different populations studied and different definitions used. Radiculopathy, nerve root pain or sciatica is defined as pain radiating to the leg, normally below the knee and into the foot with variable neurological findings [2]. Although radiating leg pain is common, clearly not all leg pain is caused by nerve root involvement and may be caused by referred pain or other joint disease.
Studies have shown that the presence of radiating leg pain is a poor prognostic feature in LBP patients and may represent an obstacle to recovery [2, 3]. Although the majority of LBP patients improve within the first 6 weeks, those with radiating leg pain have higher levels of pain and disability [4], take longer to recover [3, 5], are more likely to develop chronic symptoms [6] and also more likely to undergo surgery for their symptoms [7].
Although several systematic reviews have explored the prognosis of non-specific LBP [8–10] and sciatica [7], one of the major issues with considering leg pain as a prognostic factor is in the definition of leg pain and/or sciatica. Indeed, in a review by Kent and Keating [8], the authors highlight that some studies fail to provide a definition of ‘sciatica’ and, often, the term is used to describe any LBP-related leg pain. In a review by Hayden and colleagues [9], sciatica (or “nerve root examination findings”) was considered to be a poor prognostic factor for low back pain, and similar findings were reported by Chou and Shekelle [10] with respect to presence of radiculopathy or leg pain. In a systematic review of prognostic factors predicting outcome in non-surgically treated sciatica patients, Verwoerd and colleagues [7] concluded that leg pain intensity at baseline was the only factor with a strong positive association with outcome.
In terms of impact on employment, it has been observed that sciatica is associated with slower return to work for individuals with temporary work disability due to musculoskeletal disorders [11], while other research suggest that individuals with LBP and radiating leg pain below the knee are more likely to have time off work or undergo surgery compared to those with LBP only [12]. In contrast, some studies suggest that sciatica has a good prognosis, with more than 50% of patients included in placebo-control groups in randomised trials of non-surgical interventions showing improvement [13]. However, these studies have either been conducted within secondary care, which may include more severe cases, or have included discrete subpopulations such as males only [12] or older patients [14]. Fewer studies have been conducted specifically within primary care, the setting in which most patients with LBP and radiating leg pain are managed; of the primary care studies, some have specifically excluded patients with any radiating pain [15] or radiculopathy [16].
The poor prognostic impact of radiating leg pain is reflected in a number of diagnostic and management guidelines for LBP [17–19], which encourage differentiation between non-specific LBP, nerve root pain and serious spinal pathology. Nevertheless, current clinical guidelines suggest that with the exception of those with progressive neurological deficit, those with radiating leg pain should be managed in the same way as those with non-specific LBP only [17–19]. Due to the paucity of information regarding the impact of radiating leg pain in primary care, we sought to determine the prevalence of leg pain within a primary care population of LBP consulters and explore the impact of baseline leg pain status on self-reported work disability, health care resource use and quality of life over a 12-month period.
Methods
Study design and participants
Briefly, this was a prospective observational cohort study of consecutive patients consulting with LBP in eight general practices in North Staffordshire and Cheshire, two counties in England, UK (full details of the study design are reported elsewhere [20, 21]). Ethical approval for the study was obtained from the North Staffordshire and Central Cheshire Research Ethics Committees and permission was given by each general practice. Contact information for all patients aged 18–60 years consulting their family doctor with LBP from September 2004 to April 2006 was downloaded weekly from practice databases and these lists were checked by the lead family doctor. Patients were sent postal questionnaires at baseline, 6 and 12 months.
Measurements
The questionnaires collected data on a number of demographic variables and clinical outcomes including patients’ self-reported LBP and leg pain status. From the baseline questionnaires, responses to two questions were used to generate three patient subgroups.
The first question asked,
‘Has the pain from your back spread down one or both of your legs in the last 2 weeks?’
If the patient responded ‘yes’ to this, the second question asked,
‘Have you felt pain or numbness or pins and needles below your knee in the last 2 weeks?’
The derived subgroups were(1) LBP only (negative response to the first question)
2) LBP and pain above the knee (LBP + AK) (indicated ‘yes’ to the first question and ‘no’ to the second) or
(3) LBP and pain below the knee (LBP + BK) (indicated ‘yes’ to both questions).Further data included socio-demographics such as age, gender, socioeconomic status, and work-related factors [employment status (employed yes/no), workplace activity (doing their usual job, on light duties, on paid or sick leave, or on unpaid leave) and LBP-related work absence (number of days off work due to LBP in the preceding 6 months)]. Patients were also asked to complete a checklist of health care practitioners seen within the previous 6 months (family doctor, nurse, hospital doctor, physical therapist, osteopath, chiropractor and a ‘free text’ response option).
At each time point –– baseline, 6 and 12 months –– patients completed the EQ-5D [22], a generic preference-based measure of health-related quality of life that covers five dimensions of health (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). Each dimension contains three levels, which defines 243 (i.e. 35) distinct health states. Health state valuations (also known as utility scores) for each response permutation have been elicited from a representative sample of the UK adult population [23]. The scoring algorithm provides utility scores within a range of –0.594 (state 33333, the lowest level on each dimension) to 1.000 (state 11111, the highest level on each dimension). Negative values reflect that some health states are considered to be worse than being dead.
Statistical analyses
Analyses were performed using STATA version 10 and SPSS version 15. Participants were grouped according to their baseline leg pain status (as described above). For the work and health care resource use variables, categorical data were presented as frequencies and percentages. The associations between baseline pain leg status and work-related factors and health care resource use at baseline, 6 and 12 months were estimated as odds ratios and 95% confidence intervals using logistic regression. Both unadjusted and adjusted (for age, gender and baseline pain duration) were performed, using those with LBP only as the referent group.
As part of the quality of life analysis, quality-adjusted life year (QALY) estimates were generated using area-under-the-curve analysis [24] for those patients providing EQ-5D responses at each time point (baseline, 6 and 12 months). The distributions of mean baseline EQ-5D scores within the three patient subgroups were explored using box-plots. The associations between baseline leg pain status and EQ-5D scores at each time point, and for the 12-month QALY estimates, were explored using analysis of covariance (ANCOVA), controlling for age and gender. An omnibus ANCOVA was used to identify whether there are any differences or not in EQ-5D scores and/or QALY estimates across the subgroups.
To explore specific differences in EQ-5D scores and QALYs between subgroups, the following planned pairwise comparisons were performed if, and only if, the omnibus test was statistically significant at the 5% level:(1) LBP only versus LBP + BK
(2) LBP only versus LBP + AK and
(3) LBP + AK versus LBP + BK.
Results
Response rates and patient characteristics
Of the 1,591 baseline study participants (adjusted response 52.7% of the 3,019 eligible adults mailed [21]), 10 did not provide data on leg pain and were excluded from the analysis. Of the remaining 1,581, 1,289 (82.0%) gave permission for further follow-up contact. At 6 months, 1,254 patients were eligible to receive the questionnaire (29 people declined to participate and 6 people stated ill-health as the reason for their non-response). Of the 1,254 eligible recipients at 6 months, 803 responses were received (64% of those eligible, or 50% of the baseline responders), although only 746 (59%) completed the health care utilisation and EQ-5D questions (57 patients completed a minimum data questionnaire, sent as the final reminder, which did not include these measures). At 12 months, 529 were eligible to receive the questionnaire and 473 (89% of those eligible or 29.7% of the baseline responders) were returned.

Table 1 At baseline, study participants had a mean (standard deviation) age of 43.9 (10.3) years and 59% were women. In total, 63% of patients reported LBP of an acute duration (<3 months), while 11% reported that the current episode had lasted for more than 3 years. Table 1 summarises baseline demographics for the three patient subgroups. Self-reported leg pain was common; at baseline 645 (41%) reported LBP only, 392 (25%) reported leg pain above the knee (LBP + AK) and 544 (34%) reported leg pain below the knee (LBP + BK). The prevalence of leg pain was similar at each of the three time points (see Table 1).
Work-related factors (see Table 2)

Table 2 At baseline, the LBP + BK subgroup were significantly more likely to be unemployed than those with LBP only [adjusted OR = 1.97 (95% CI 1.48, 2.62)]. For patients in employment at baseline, those with LBP + BK compared to those with LBP only were three times more likely not to be doing their usual job because of their back problem [2.97 (2.17, 4.07)], and more than twice as likely to have taken time off work because of their symptoms at both 6-month [2.35 (1.59, 3.49)] and 12-month follow-up [2.53 (1.38, 4.65)]. Similar associations, although of smaller magnitude, were seen when comparing the LBP + AK subgroup to those with LBP only. The impact of any leg pain on these work-related factors persisted at 6 and 12 month follow-up.
Health care use (see Table 3)

Table 3 Patients with LBP + BK were more likely to report consulting their family doctor in the previous 6 months at each follow-up time point compared to those with LBP only; for example, at 6-month follow up, 67% of LBP + BK patients had re-consulted their GP compared to 46% of those with LBP only. In addition, LBP + BK patients were more likely to be referred for other health care services, including physical therapy, at all time points compared to those with LBP only. No difference was seen in the rates of consultation with either chiropractors or osteopaths between the subgroups, although the rates of consultation for both these groups of practitioners were small (<3% of the cohort, data not shown), reflecting a UK health care system where such practitioners work predominately within the private sector. In terms of hospital referral, those with LBP + BK were three times more likely to be referred to a hospital doctor for their symptoms in the previous 6 months compared to those with LBP only at each time point. Findings were similar, although of smaller magnitude, for the comparison of the LBP + AK and LBP only subgroups.
Quality of life (see Table 4)

Table 4 Figure 1 reports a box-plot of baseline EQ-5D scores across each patient subgroup. All three subgroups show a non-symmetric distribution, with a negative skew. It is also evident that the EQ-5D scores relating to the LBP + BK subgroup have a broader spread across the scoring range, indicating greater variation in quality of life. Patients reporting health states worse than death (i.e. index scores below zero) were present in each subgroup, although such patients in the LBP + BK group were not considered outliers in the distribution.
Table 4 indicates the mean EQ-5D scores at each time point, and QALY estimates over the 12-month period. The number of EQ-5D responders relates to the number of returned questionnaires that provide sufficient data to generate an EQ-5D index score. QALY scores refer only to participants who provided complete data at each time point.
The planned comparisons were(1) LBP only versus LBP + BK
(2) LBP only versus LBP + AK and
(3) LBP + AK versus LBP + BK.
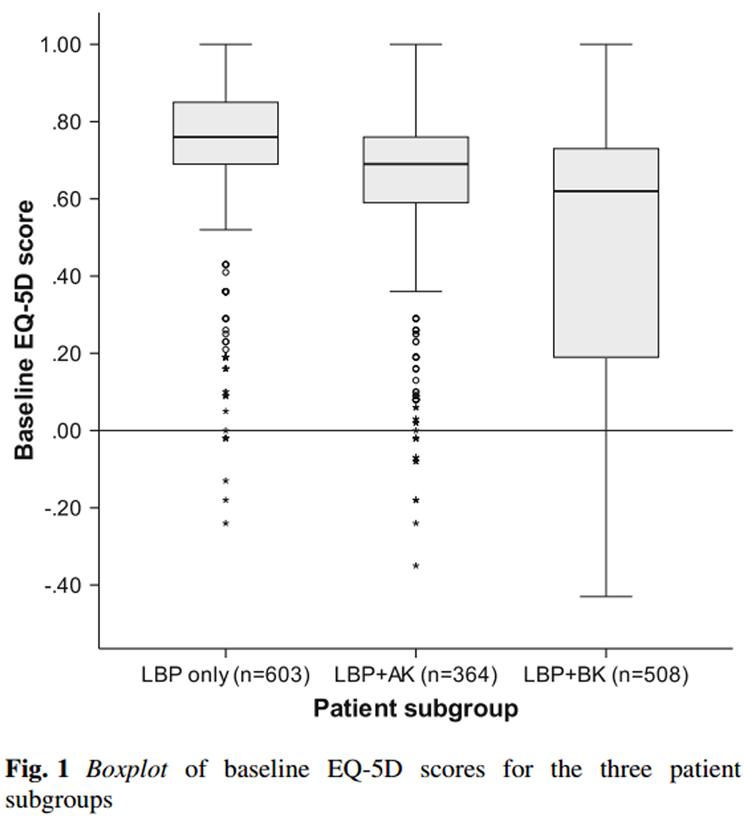
Figure 1 Reported p values do not assume equal variances across the patient subgroups (evident in Fig. 1). All analyses are conducted while controlling for age and gender
Differences were observed across the three subgroups in EQ-5D scores at each time point, and QALYs over the 12-month follow-up period. Those with LBP only reported the highest utility scores (indicating higher self-rated quality of life), and those with LBP + BK reported the lowest.
Results of the omnibus ANCOVA analysis confirm that mean EQ-5D scores were significantly different across the three subgroups at each time point (p < 0.001). Complete EQ-5D scores at all three time points were provided by 366 patients; mean QALY scores across the three subgroups showed the same statistically significant difference (p < 0.001). For the planned pairwise comparisons, differences in mean EQ-5D utility scores at baseline, 6 and 12 months, and mean QALYs over the 12-month follow-up period, were all statistically significant but to varying levels; 8 of 12 planned comparisons were significant at a 0.1% level, 3 at the 1% level and 1 at the 5% level, indicating that the LBP + BK group had the lowest and the LBP only group the highest quality of life.
Discussion
This study suggests that self-reported radiating leg pain is common in patients consulting their family doctor with LBP, with 34% indicating leg pain radiating below the knee at baseline. Those with leg pain below the knee, our proxy for sciatica, were significantly less likely to be employed than the other two subgroups; and even amongst employed patients, those with leg pain below the knee were more likely not to be doing their usual job and to have taken time off work because of their symptoms. Patients with leg pain below the knee also utilise significantly more health care than those with LBP only: at 6-month follow-up, 67% of patients with leg pain below the knee had re-consulted their family doctor, 39% had consulted a physical therapist and 23% had been referred to hospital (all within the preceding 6 month period). Despite this, those with radiating leg pain reported significantly poorer quality of life.
Our results are in keeping with other studies, suggesting that patients with sciatica have greater levels of work absence and a slower return to work than patients with LBP alone [11, 25]. Our data show higher levels of work disability than in the primary care study by Grotle et al. [5], in which 55% of their cohort had no work loss. These different results could be partly explained by the differences in symptom duration; in Grotle’s study, the cohort comprised acute LBP patients, whereas the present study included a wide range of symptom duration.
In terms of health care resource use, previous studies suggest that patients with radiating leg pain are more likely to undergo investigations and surgery than those with LBP only [7, 12]. Our study suggests that within a population of primary care consulters, the presence of radiating leg pain is associated with more consultations with both primary and secondary care practitioners.
Our data on quality of life support the results of other studies, which have suggested that patients with sciatica have a poor perception of their general health and quality of life [12, 14, 26]. However, these studies have either been cross-sectional in design or have been limited to defined population subgroups such as males only [12] or older age groups [14]. We have demonstrated in a large and unselected cohort of adults consulting their family doctor about LBP that those who report the presence of radiating leg pain suffer significantly worse quality of life than those with LBP only, and, importantly, this effect remains 12 months after the initial consultation, despite the increased use of health care resources. In comparison with UK population norms for similar age groups, all three patient subgroups had low quality of life scores at baseline and remained lower than UK norm values during the 12-month follow-up period [27].
Current LBP guidelines either exclude radiculopathy or encourage similar initial management strategies (in terms of advice, exercise and medication in the first 4 weeks) for patients with both LBP alone and radiculopathy [17]. However, our data suggest that the presence of radiating leg pain may provide a useful clinical indicator for patients requiring early and more systematic identification, with targeted interventions to reduce the impact and consequences of leg pain on work status, health care resource use and quality of life.
An important strength of our paper is that this was a large study, recruiting consecutive primary care consulters with LBP across eight general practices, meaning that our results are likely to be highly generalisable. In addition, the study incorporated longitudinal data over 12 months and included validated instruments to measure quality of life [22]. However, there are significant potential limitations. First, not all patients who consulted took part in the study and so there is the potential for bias. There was a significant loss to follow-up at both 6 and 12 months; those not completing the baseline questionnaire and those lost to follow-up at 6 months were younger and more likely to be male [21]. However, the likely effect of this would have been to underestimate the effect on work since those lost to follow-up were more likely to be of working age. It is possible that those more severely affected were more likely to remain in the study, which may have affected the quality of life data; however, the proportions of each pain category were similar at baseline and 12 months. The loss to follow-up can be explained, in part, by the research ethics constraints of the study. Participants had to “opt in” and agree to receive further questionnaires and, therefore, those not responding at 6 months were excluded from 12-month follow-up.
A further limitation is that our definition of leg pain was made by self-report data rather than by clinical examination or imaging. Only a proportion of the leg pain subgroups may have had true nerve root compression. However, the likely effect of this would be that our findings present an underestimate of the impact of leg pain (by including those with non-nerve root pain), meaning that the associations seen would have been even stronger in patients with clinically determined nerve root compression. It is important to acknowledge that consensus studies support the use of “pain below the knee” as a reasonable proxy for sciatica [28].
The resource use data collection process may also be regarded as a limitation of the study, i.e. reliance on patients to recall their health care use. This can introduce two types of bias: recall bias (the failure to remember a particular event) and telescoping (the tendency to remember distant events as occurring more recently). Although criticisms of self-report resource use data are well established, the method provides an efficient approach to data collection in the absence of accessible routine data sources and has been used in previous musculoskeletal economic evaluations [29, 30] which have included small sample validation tests to verify the accuracy of self-report data compared to primary care records [30].
In summary, self-reported leg pain is common in LBP patients in primary care. Patients consulting their family doctor with leg pain below the knee have higher levels of work disability, utilise significantly more health care over a prolonged period of time and report significantly worse quality of life over 12 months than those with LBP only. This suggests that patients with radiating leg pain warrant early intervention to reduce the negative impact of their leg pain.
Acknowledgments
This study is supported financially by a Programme Grant from Arthritis Research UK (13413) and by the North Staffordshire Primary Care Consortium. Nadine Foster is supported through an NIHR Research Professorship. This report is independent research supported by the National Institute for Health Research NIHR Research Professorship NIHR-RP-011-015. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health. The authors would like to thank GPs, staff and patients of the eight GP practices who participated in the study. Thanks also to the administrative and health informatics staff at the Arthritis Research UK Primary Care Centre, Keele University.
Conflict of interest
None.
References:
Macfarlane GJ, Jones GT, Hannaford PC (2006)
Managing low back pain presenting to primary care: where do we go from here?
Pain 122(3):219–222Konstantinou K, Dunn KM (2008)
Sciatica: review of epidemiological studies and prevalence estimates.
Spine (Phila Pa 1976) 33(22):2464–2472Tubach F, Beaute J, Leclerc A (2004)
Natural history and prognostic indicators of sciatica.
J Clin Epidemiol 57(2):174–179Dunn KM, Croft PR (2004)
Epidemiology and natural history of low back pain.
Eura Medicophys 40(1):9–13Grotle M, Brox JI, Veierød MB, Glomsrød B, Lønn JH, Vøllestad NK (2005)
Clinical course and prognostic factors in acute low back pain: patients consulting primary care for the first time.
Spine (Phila Pa 1976) 30(8):976–982Mehling WE, Gopisetty V, Bartmess E, Acree M, Pressman A, Goldberg H (2012)
The prognosis of acute low back pain in primary care in the United States: a 2-year prospective cohort study.
Spine (Phila Pa 1976) 37(8):678–684Verwoerd AJ, Luijsterburg PA, Lin CW, Jacobs WC, Koes BW, Verhagen AP (2013)
Systematic review of prognostic factors predicting outcome in non-surgically treated patients with sciatica.
Eur J Pain 17(8):1126–1137Kent PM, Keating JL (2008)
Can we predict poor recovery from recent-onset nonspecific low back pain? A systematic review.
Man Ther 13(1):12–28Hayden JA, Chou R, Hogg-Johnson S, Bombardier C (2009)
Systematic reviews of low back pain prognosis had variable methods and results: guidance for future prognosis reviews.
J Clin Epidemiol 62(8):781–796Chou R, Shekelle P (2010)
Will this patient develop persistent disabling low back pain?
JAMA 303(13):1295–1302Abásolo L, Carmona L, Lajas C, Candelas G, Blanco M, Loza E (2008)
Prognostic factors in short-term disability due to musculoskeletal disorders.
Arthritis Rheum 59(4):489–496Selim AJ, Ren XS, Fincke G, Deyo RA, Rogers W, Miller D, Linzer M, Kazis L (1998)
The importance of radiating leg pain in assessing health outcomes among patients with low back pain. Results from the Veterans Health Study.
Spine (Phila Pa 1976) 23(4):470–474Vroomen PC, de Krom MC, Knottnerus JA (2002)
Predicting the outcome of sciatica at short-term follow-up.
Br J Gen Pract 52(475):119–123Hicks GE, Gaines JM, Shardell M, Simonsick EM (2008)
Associations of back and leg pain with health status and functional capacity of older adults: findings from the retirement community back pain study.
Arthritis Rheum 59(9):1306–1313Coste J, Delecoeuillerie G, Cohen de Lara A, Le Parc JM, Paolaggi JB (1994)
Clinical course and prognostic factors in acute low back pain: an inception cohort study in primary care practice.
BMJ 308(6928):577–580Henschke N, Maher CG, Refshauge KM et al.
Prognosis in Patients with Recent Onset Low Back Pain in Australian Primary Care:
Inception Cohort Study
British Medical Journal 2008 (Jul 7); 337: a171Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr., Shekelle P, Owens DK:
Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline
from the American College of Physicians and the American Pain Society
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 478–491Royal College of General Practitioners.
Clinical Guidelines for the Management of Acute Low Back Pain
London: Royal College of General Practitioners; (1999). [UK]van Tulder M, Becker A, Bekkering T, et al; On behalf of the COST B13 Working Group on Guidelines for the Management of Acute Low Back Pain in Primary Care.
Chapter 3. European Guidelines for the Management of Acute Nonspecific Low Back Pain in Primary Care
European Spine Journal 2006 (Mar); 15 Suppl 2: S169–191Foster NE, Bishop A, Thomas E, Main C, Horne R, Weinman J, Hay E (2008)
Illness perceptions of low back pain patients in primary care: what are they, do they change and are they associated with outcome?
Pain 136(1–2):177–187Foster NE, Thomas E, Bishop A, Dunn KM, Main CJ (2010)
Distinctiveness of psychological obstacles to recovery in low back pain patients in primary care.
Pain 148(3):398–406Rabin R, de Charro F (2001)
EQ-5D: a measure of health status from the EuroQol group.
Ann Med 33(5):337–343Dolan P, Gudex C, Kind P, Williams A (1995)
A social tariff for the EuroQol: results from a UK General Population Survey.
Discussion Paper 138. Centre for Health Economics, University of YorkRäsänen P, Roine E, Sintonen H, Semberg-Konttinen V, Ryynänen OP, Roine R (2006)
Use of quality-adjusted life years for the estimation of effectiveness of health care: a systematic literature review.
Int J Technol Assess Health Care 22(2):235–241Andersson GB, Svensson HO, Oden A (1983)
The intensity of work recovery in low back pain.
Spine (Phila Pa 1976) 8(8):880–884Lyons RA, Lo SV, Littlepage BN (1994)
Comparative health status of patients with 11 common illnesses in Wales.
J Epidemiol Community Health 48(4):388–390Kind P, Hardman G, Macran S (1999)
UK population norms for EQ-5D. Discussion Paper 172.
Centre for Health Economics, University of YorkDionne CE, Dunn KM, Croft PR, Nachemson AL, Buchbinder R, Walker BF, Wyatt M, Cassidy JD, Rossignol M, Leboeuf-Yde C, Hartvigsen J, Leino-Arjas P, Latza U, Reis S, Gil Del Real MT, Kovacs FM, Oberg B, Cedraschi C, Bouter LM, Koes BW, Picavet HS, van Tulder MW, Burton K, Foster NE, Macfarlane GJ, Thomas E, Underwood M, Waddell G, Shekelle P, Volinn E, Von Korff M (2008)
A consensus approach toward the standardization of back pain definitions for use in prevalence studies.
Spine (Phila Pa 1976) 33(1):95–103Ratcliffe J, Thomas KJ, MacPherson H, Brazier J (626)
A randomised controlled trial of acupuncture care for persistent low back pain: cost effectiveness analysis.
BMJ 333(7569):626Whitehurst DG, Lewis M, Yao GL, Bryan S, Raftery JP, Mullis R, Hay EM (2007)
A brief pain management program compared with physical therapy for low back pain: results from an economic analysis alongside a randomized clinical trial.
Arthritis Rheum 57(3):466–473
Return to LOW BACK PAIN
Return to RADICULOPATHY
Return to CHIROPRACTIC AND SCIATICA
Since 4–05–2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |