Galactooligosaccharide Supplementation Reduces Stress-induced
Gastrointestinal Dysfunction and Days of Cold or Flu:
A Randomized, Double-blind, Controlled Trial
In Healthy University Students
Gastrointestinal Dysfunction and Days of Cold or Flu:
A Randomized, Double-blind, Controlled Trial
In Healthy University Students
Send all comments or additions to: Frankp@chiro.org




FROM: Am J Clin Nutr. 2011 (Jun); 93 (6): 1305–1311 ~ FULL TEXT
Christine Hughes, Yalda Davoodi-Semiromi, James C Colee, Tyler Culpepper,
Wendy J Dahl, Volker Mai, Mary C Christman, and Bobbi Langkamp-Henken
Departments of Food Science and Human Nutrition,
University of Florida,
Gainesville, FL 32611-0370, USA.
Gastrointestinal dysfunction is common – occurring due to various conditions – and can result in the failure of the intestine to digest food and absorb the fluids, electrolytes, and nutrients essential for life. At some point in any patient's life, the chances that he or she will develop a GI tract problem, be it peptic ulcer disease, gallstones, irritable bowel syndrome, food poisoning, or some other malady, are extremely high. Common complaints may include dysphagia, early satiety, reflux, constipation, abdominal pain, nausea, vomiting, and diarrhea.
Prebiotics are non-digestible food ingredients that stimulate the growth and/or activity of bacteria in the digestive system which are beneficial to the health of the body. Typically, prebiotics are carbohydrates (such as oligosaccharides), but the definition may include non-carbohydrates. The most prevalent forms of prebiotics are nutritionally classed as soluble fiber. To some extent, many forms of dietary fiber exhibit some level of prebiotic effect. A prebiotic should increase the number and/or activity of bifidobacteria and lactobacillus. The importance of bifidobacteria and lactobacillus is that these groups of bacteria have several beneficial effects on the host, especially in terms of improving digestion (including enhancing mineral absorption) and the effectiveness and intrinsic strength of the immune system.
Current research suggests that daily supplementation with prebiotics may boost immune function and gastrointestinal health during times of heightened stress. The following randomized, double-blind study included 419 college students who were randomized to receive 0, 2.5 or 5.0 grams of a galactooligosaccharide prebiotic supplement for eight weeks before, during and after final exams. The results revealed that the study participants showed fewer symptoms of gastrointestinal problems, including diarrhea, constipation, indigestion and abdominal pain following prebiotics supplementation.
It was also found that normal-weight individuals receiving the 5.0 gram prebiotic supplement experienced a 40 percent reduction in days with cold or flu, although no effect was observed in overweight or obese participants. These findings suggest that galactooligosaccharide prebiotics may provide beneficial protection during times of increased stress.
BACKGROUND: Acute psychological stress induced by academic exams is associated with dysregulated gastrointestinal and immune function.
OBJECTIVE: We examined whether supplementation with galactooligosaccharides reduced gastrointestinal dysfunction and the percentage of days with cold or flu in academically stressed undergraduate students.
DESIGN: In a randomized, double-blind study, subjects (n = 427) received 0, 2.5, or 5.0 g galactooligosaccharides for 8 wk around the time of fall final exams. Levels of stress and cold or flu symptom intensity (SI; 0 = not experiencing to 3 = severe) were recorded daily. The SI from 9 cold or flu symptoms was summed with 1 d of cold or flu defined as a sum >6. The Gastrointestinal Symptom Response Scale was completed weekly.
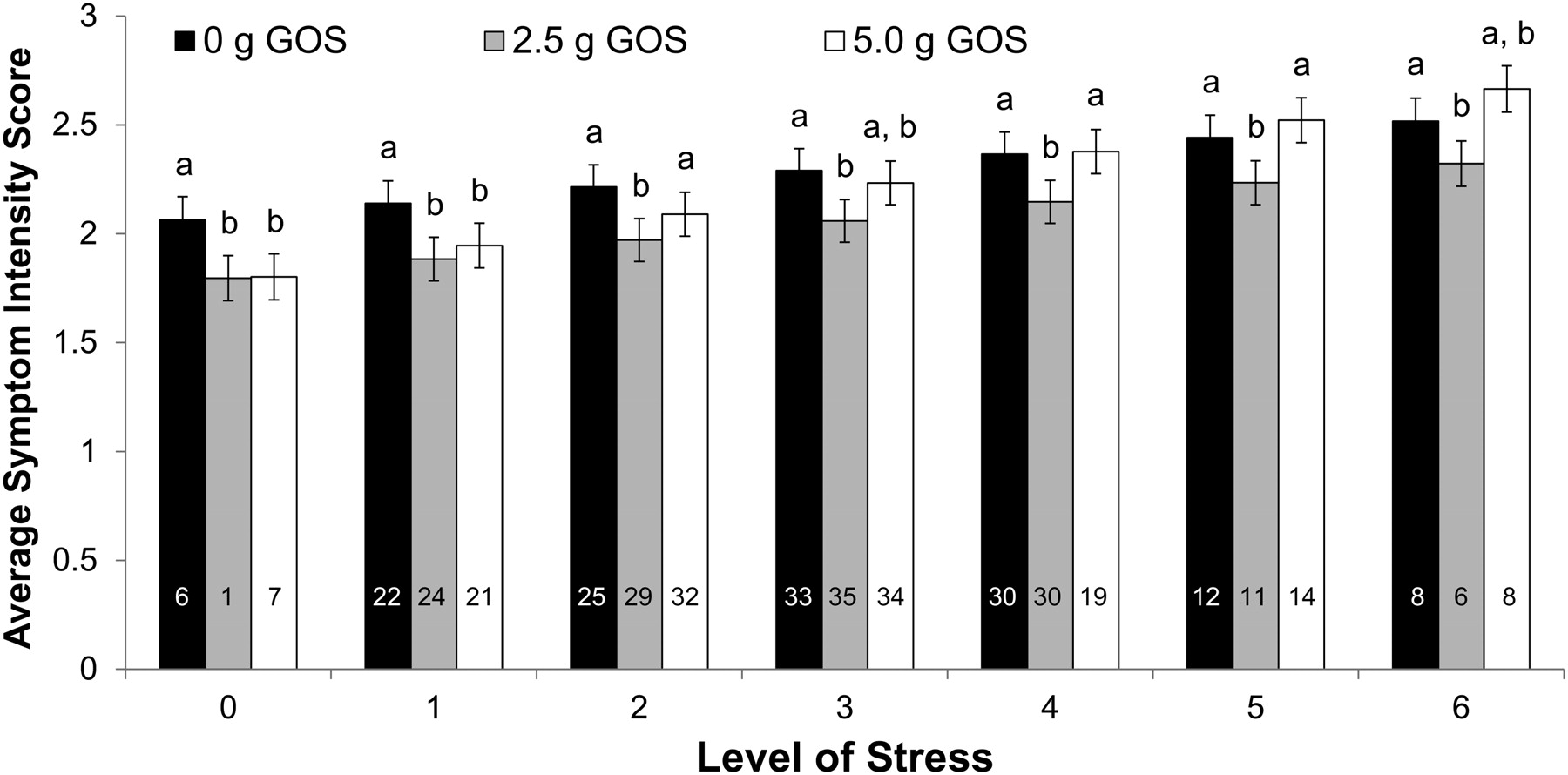
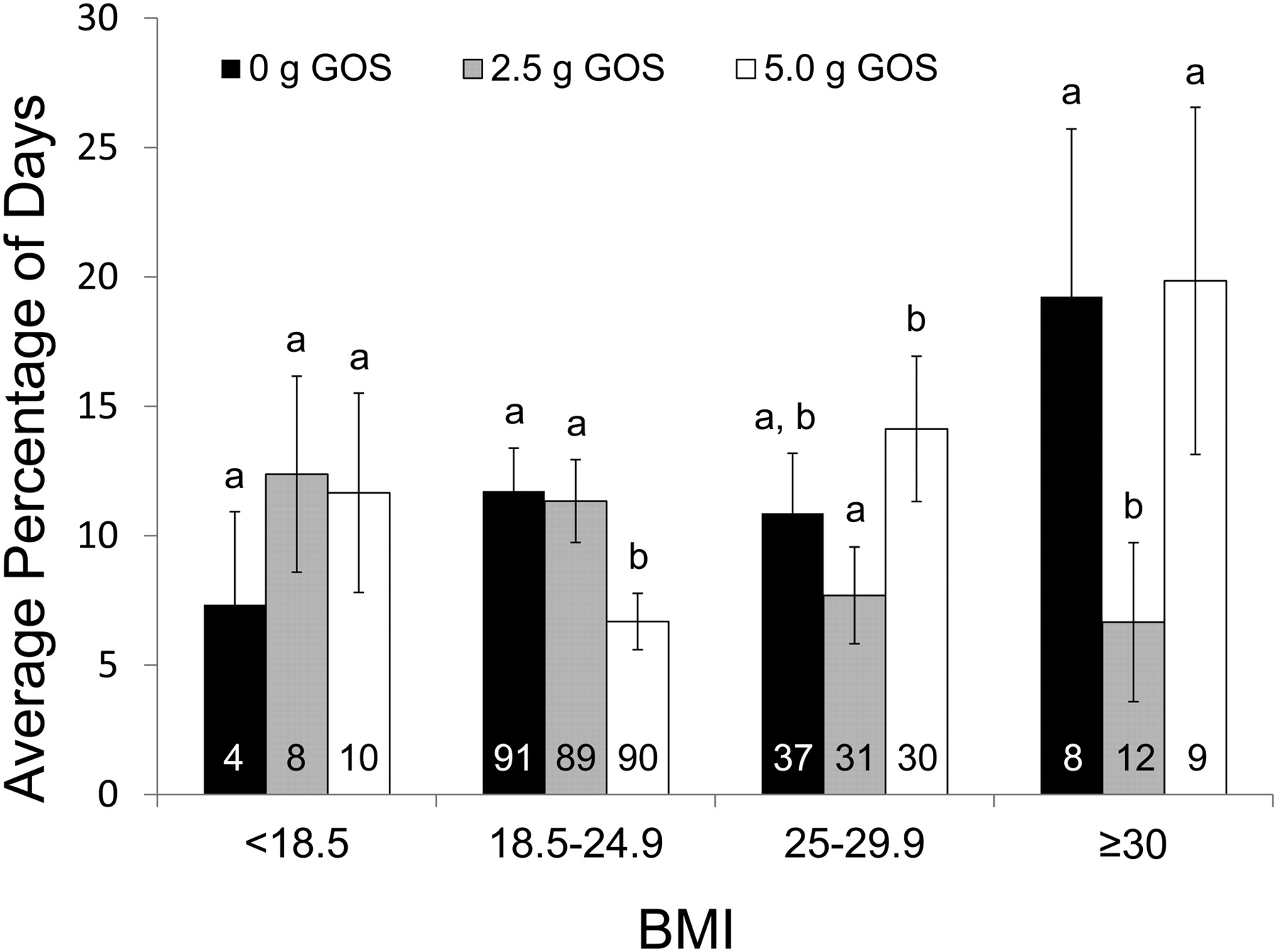
RESULTS: Stress was positively related to diarrhea, indigestion, and reflux syndromes and with abdominal pain, average daily cold or flu SI score, and the percentage of days with cold or flu. Gastrointestinal symptom scores for diarrhea (P = 0.0298), constipation (P = 0.0342), abdominal pain (P = 0.0058), and indigestion (P = 0.0003) syndromes were lower after galactooligosaccharide supplementation. The cold or flu SI score was affected by galactooligosaccharides and stress (P < 0.0001); 2.5 g was associated with a lower SI score across all levels of stress, but 5.0 g was protective only at lower levels of stress. The percentage of days with cold or flu was associated with galactooligosaccharides within different body mass index categories (P = 0.0002), wherein a 40% reduction in the percentage of days with cold or flu was observed in normal-weight individuals with 5.0 g galactooligosaccharides. This effect was not observed in overweight or obese individuals.
CONCLUSIONS: Acute psychological stress was directly related to symptoms of gastrointestinal dysfunction and cold or flu. Galactooligosaccharide supplementation reduced these symptoms and the number of days with cold or flu.
From the Full-Text Article:
INTRODUCTION
Acute upper respiratory illnesses are common in college students. Over a 6-mo period including the winter months, 80–90% of students recorded =1 d of cold/flu symptoms, 22% reported at least one health care visit, 41% missed =1 d of class, and 28% self-reported that they did poorly on an exam because of an upper respiratory illnesses [1, 2]. In another study, students followed for 8 wk around the time of fall final exams were more likely to report a cold (ie, =2 cold symptoms on =2 d) when they had higher average stress levels in the prior 3 d [3].
Acute psychological stress, such as that induced by academic exams, is associated with dysregulated immune and gastrointestinal function [4–6]. Classic studies showed a reduction in cellular immunity in first-year medical students undergoing academic exams [7, 8]. Activity of natural killer cells, one of the front-line defenses against viral infections, was reduced during exams, and those students who scored higher for stressful life events had lower natural killer cell activity [7]. Cytokine production was also associated with acute psychological stress, ie, increased interleukin (IL)-6 and IL-10 and decreased interferon-γ with increased stress [4]. In addition to the changes in immune function, academic stress is associated with increased cortisol production, abdominal pain, and a disruption of the intestinal microbiota, which result in lower viable lactic acid bacteria counts [5, 6].
Psychological stress can modulate the gastrointestinal and immune systems through the hypothalamus-pituitary-adrenal (HPA) axis. Glucocorticoids (eg, cortisol), which play a key role in the HPA, are likely responsible for the observed changes in natural killer cell function, dysfunction of the gastrointestinal tract, and altered microbiota [6, 9]. Recently, the concept of the brain-gut-enteric microbiota axis was introduced, which suggests bidirectional communication between the gastrointestinal tract and brain with input from the enteric microbiota [10]. Another model in which cortisol may be driving changes in immune function and enteric microbiota is that of immunosenescence [11]. Vulevic et al [12] supplemented the diets of older adults with a prebiotic, galactooligosaccharides, and observed increased numbers of beneficial bacteria (ie, bifidobacteria), decreased production of IL-6, and increased natural killer cell activity. With these concepts in mind, we were interested in determining whether galactooligosaccharide supplementation would reduce gastrointestinal dysfunction and the percentage of days of cold/flu in university students undergoing academic stress. If successful, such an intervention may help reduce personal, academic, and financial costs associated with cold or flu viruses.
SUBJECTS AND METHODS
Subjects
Participants from the University of Florida were recruited via listservs, flyers, posters, and announcements in early fall of 2009. Participants were healthy full-time students aged ≥18 y who experienced at least one cold in the past year. Potential subjects were excluded if they 1) had chronic allergies involving the upper respiratory tract (defined as taking allergy medicine daily), milk allergy, or immunosuppressive illnesses or treatments in the past year; 2) would not have Internet access for the duration of the protocol; 3) did not have at least one scheduled final exam; 4) were current smokers; 5) received antibiotic therapy during the 2 mo before the start of the study; 6) were unwilling to discontinue any fiber or potentially immune-enhancing dietary supplements [eg, prebiotics, probiotics, echinacea, fish oil, vitamin E (>100% of the Recommended Dietary Allowance or >15 mg/d)]; or 7) had a cold on the day of enrollment. Each subject gave written informed consent, and all study procedures were in accordance with the ethical standards of the University of Florida Institutional Review Board.
Experimental design
Subjects (n = 427) were randomly assigned to a supplement group during the first week in November of 2009 and were followed for 8 wk, including the time of fall final exams. Exams were held over the span of 1 wk during the sixth week of the intervention. The number and scheduled time of exams varied with each subject's academic course schedule. Once students completed their last exam, subjects were on semester break through the remainder of the study.
The study was a prospective, randomized, parallel, double-blind, placebo-controlled trial. Subjects were proportionally stratified based on sex (50/50) and randomly assigned over a 5-d period via sealed envelopes to receive 0, 2.5, or 5.0 g galactooligosaccharides (Purimmune GTC Nutrition, Golden, CO). The stratification and randomization schemes were generated by the study statistician (MCC) who did not have direct contact with any subjects. On the basis of the number of upper respiratory tract infections in galactooligosaccharide-supplemented infants and the number of colds in academically stressed undergraduate students [3, 13], a sample size of 140 subjects in each group was calculated to observe a 50% reduction in the proportion of colds in the treatment groups with 80% power, α = 0.05, and a 10% attrition rate.
Fiber administration protocol
The galactooligosaccharide supplements were provided in coded packets that were similar in size and shape to commercially available single-serving drink mixes. Bakers’ sugar (sucrose) was added to the 0-g and 2.5-g packets so that all packets were the same weight and looked similar. A flow agent (silicon dioxide) was added to all packets to improve emptying of the package contents. The fiber supplement contained 86% galactooligosaccharides with 21% DP2 and 65% DP3 and above; therefore, the final weights of the packets were adjusted to provide 0, 2.5, and 5.0 g galactooligosaccharides. The subjects were instructed to pour the contents of the packet into any beverage, mix well, and consume the beverage in its entirety each day for 8 wk. Both the galactooligosaccharides and sucrose had a slightly sweet taste. The subjects were unable to distinguish the galactooligosaccharide packets from the placebo. Regardless of the actual treatment group, the proportions of subjects who thought they were receiving 0, 2.5, and 5.0 g galactooligosaccharides were 44%, 42%, and 14%, respectively. No differences were found between groups, which suggested successful blinding.
Online study questionnaires
On the day of random assignment, subjects met with investigators to have their height and weight measured, be instructed on study procedures, and obtain the supplement packets. Each subject was assigned a study number to use as their login user name for online questionnaires. The subjects provided their own password. User names were not linked to university records; however, paper records retained by the study coordinators linked subject number to the subjects’ identification and contact information. The subjects were instructed on how to complete online baseline, daily, weekly, and final questionnaires. The questionnaires used throughout the 8-wk protocol were administered through the University of Florida–hosted E-Learning System (Blackboard Learning System, Washington, DC). Questions regarding demographic information were contained on a short questionnaire at baseline. Daily online questionnaires asked about level of stress on a scale from 0 (no stress) to 10 (extremely stressed), consumption of the supplement to the nearest quarter packet, cold and flu symptoms, number and consistency of stools, hours of sleep, and antibiotic use. Subjects were asked to rate symptom intensity (0 = none, 1 = mild, 2 = moderate, and 3 = severe) for running/congested nose, stiffness or chills, headache, cough, fatigue, fever, sore throat, achiness, and ear discomfort. The cold/flu symptom intensity (SI) score was calculated as the sum of the individual symptom intensities. [14] The subjects were asked to score their stool consistency using the Bristol stool score. [15] The stool scale, which ranged from 1 (hard-to-pass stools) to 7 (entirely liquid stools), was shown graphically on the questionnaire. The baseline and weekly questionnaires inquired about gastrointestinal symptoms by using the Gastrointestinal Symptom Scale Score. [16] On the final questionnaire, the subjects were asked whether they received an annual influenza vaccination (2008–2009 and 2009–2010 flu seasons) or the 2009 H1N1 vaccination and to guess the amount of galactooligosaccharides (0, 2.5, or 5.0 g) that they received in their daily packets. Each daily questionnaire was to be completed by noon the following day; weekly and final questionnaires were to be completed within 3 d of online release. Study coordinators monitored subject compliance online on a daily basis and contacted subjects via E-mail or phone if they missed these time limits. The subjects were discouraged from completing questionnaires that were 3 d overdue. The questionnaires were no longer available to subjects once completed.
Statistical analyses
Compliance was assessed by summing the daily reported percentage of the supplement packet consumed and dividing by 56 d. Missing daily questionnaires were considered as an intake of 0% of the supplement packet. We assumed that there would be a lag time between the start of the supplement and effects on study outcomes; therefore, data from the first 7 d were not used in the analyses of supplement modulated outcomes in the cold/flu symptoms. Differences in demographic data and in the average number of days with cold/flu symptoms between groups were analyzed by using a one-factor analysis of variance or the Kruskal-Wallis one-factor analysis of variance on ranks. Tests of treatment effects were done by using Bonferroni or Dunn's adjustments for multiple comparisons. Categorical data were compared by using the chi-square statistic.
Variables included in all models for daily cold/flu symptoms and SI were stress; lag stress with a 1-, 2-, and 3-d lag; sex; day of randomization; ethnicity; antibiotic use; vaccination against seasonal influenza for the 2009–2010 and 2008–2009 flu seasons; vaccination against H1N1; number of final exams; body mass index (BMI); age; and hours of sleep. The 2-factor interactions were also included. Variables and variable interactions that were not significant were eliminated from the model.
To adjust for personal differences in scoring cold/flu SI, the subjects were categorized on the basis of the average sum of their SI score from the first week of supplementation. Symptom intensity score categories were an average sum of <1 (60% of subjects), 1–3 (29% of subjects), and >3 (11% of subjects) over the first week of supplementation. The average SI sum for the remaining weeks of supplementation was significantly different between categories (<1, 1.2 ± 0.01; 1–3, 2.0 ± 0.1; and >3, 3.4 ± 0.1; P < 0.0001), which suggested that the personal differences in scoring SI continued throughout the study. The daily average SI score from study weeks 2 through 8 was compared between the 3 groups by using a general linear mixed model with an autoregressive correlation structure to account for correlation of daily observation.
Before the data were analyzed and while the investigators were still blinded to treatment, individual daily cold/flu SI scores were reviewed to identify a cutoff above which a subject was likely to have a cold/flu (ie, be sick). The cutoff was to differentiate cold/flu symptoms from symptoms associated with stress. An SI score >6, which would represent a minimum of 3 symptoms (≥2 of moderate and 1 of severe intensity), was selected as the SI that reflected a sick day. An indicator variable of being “sick” was compared between groups by using a generalized linear mixed model on the response variable with an autoregressive correlation structure to account for the correlation of daily observations. A binomial error distribution was used because the response variable was either “yes” (the individual had a cold/flu) or “no” (he or she did not).
Fifteen gastrointestinal symptoms divided among 5 categories (diarrhea syndrome, constipation syndrome, abdominal pain, indigestion syndrome, and reflux syndrome) were each rated from 1 = no discomfort to 7 = very severe discomfort. Scores within each category were summed, and weekly gastrointestinal symptoms were adjusted for baseline responses. The baseline response was an individual's response for the week before randomization. A generalized linear mixed model was then used to model gastrointestinal symptom categories. Because the data were not normally distributed, an exponential distribution was specified and an autoregressive correlation structure was used to correct for the correction over time that was caused by individuals being measured repeatedly over the course of the study. The df values were corrected by using the Kenward-Roger method to control the family-wise error rate. For the weekly gastrointestinal symptoms model, the daily covariates were replaced with their average value for the week. For example, daily stress levels were replaced with average weekly stress. The same process was repeated for hours of sleep. The lag daily stress variables were not used. Unless stated otherwise, data represent least-squares means ± SEMs. Analyses were completed by using SigmaPlot (version 11.0, 2008; Systat Software Inc, San Jose, CA) and the generalized linear mixed models were fitted by using SAS version 9.2 (SAS Institute, Cary, NC).
RESULTS
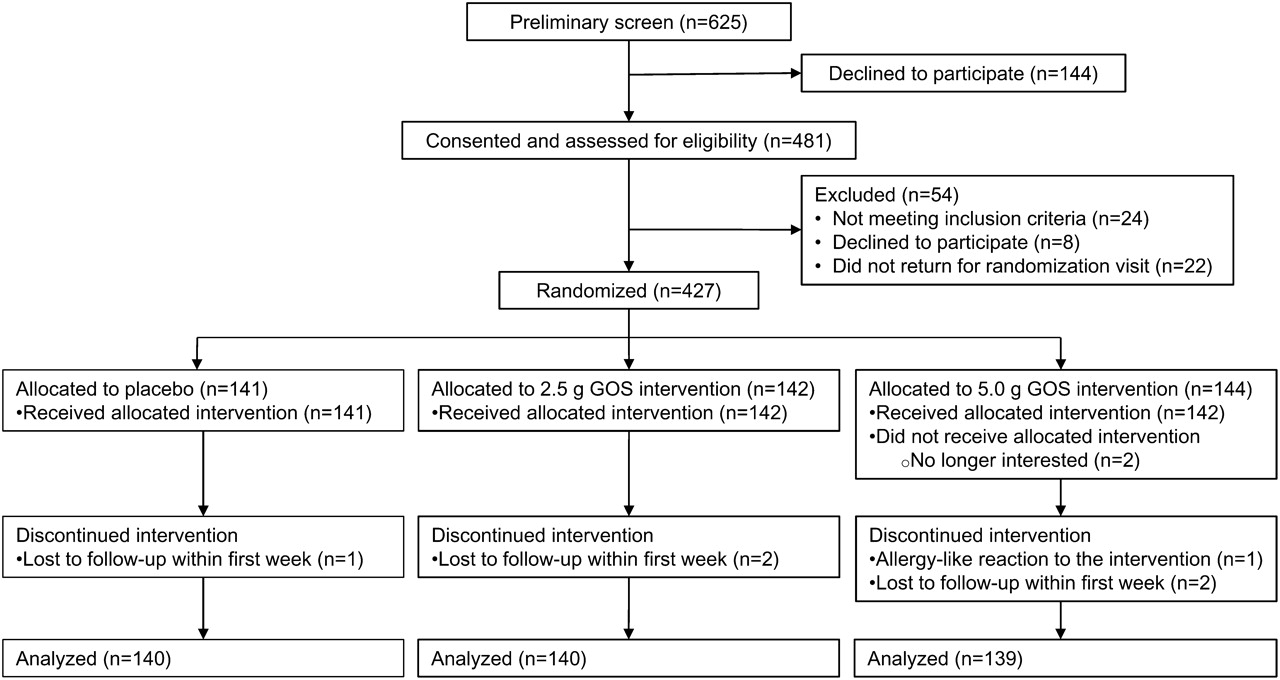
Figure 1 A total of 481 subjects provided consent and were assessed for eligibility (Figure 1). Of this group, 24 did not meet the inclusion criteria, 8 declined to participate, and 22 did not return for the randomization visit. Of the 427 remaining subjects, 141, 142, and 144 subjects were randomly assigned to receive 0, 2.5, or 5.0 g galactooligosaccharides, respectively. Two subjects dropped out before beginning the supplement. One subject (5.0 g galactooligosaccharides) dropped out on the first day of the intervention with allergy-like symptoms. No other harms were reported. Five subjects completed ≤7 d of records and were therefore not included in any of the analyses. Data were analyzed on an intent-to-treat basis from 419 subjects who completed on average 55 of 56 daily records and consumed an average of >93% of the supplement packets each day (Table 1).

Table 1 No significant differences between groups were found in the number of final exams, vaccinations against H1N1 in 2009 or seasonal influenza in 2008–2009, antibiotic use, or subject characteristics; significant differences in age and in the number vaccinated against the 2009–2010 influenza were found between the groups (Table 1). Subjects who consumed 5.0 g galactooligosaccharides each day were on average 6 mo younger than those subjects who received the placebo. On average, the subjects reported cold/flu symptoms on 56 d (ie, one symptom/d), with fatigue on 12 d; running/congested nose on 10 d; headache on 7 d; cough on 7 d; sore throat on 6 d; achiness, stiffness or chills on 5 d; ear discomfort on 2 d; and fever on 1 d over the 8-wk study period. No differences in the average number of cold/flu symptoms reported by subjects were found between groups (data not shown).
Average daily stress was not different between groups (Table 1). Peak average stress occurred during the week of final exams (5.0 ± 0.2), and the lowest level of stress (1.3 ± 0.2) was reported during the semester break (ie, the final weeks of the study). The average cold/flu SI score was significantly associated with stress and galactooligosaccharide supplementation (P < 0.0001). Stress was positively related to SI score, and a lower SI score was associated with 2.5 g galactooligosaccharide supplementation across all levels of stress (Figure 2). At lower levels of daily stress, 5.0 g galactooligosaccharides was also associated with a lower average SI score. The protective effect of 5.0 g galactooligosaccharides was not detected at higher levels of stress.
The probability of having a sick day was positively related to the level of stress (P < 0.0001) and was significantly associated with galactooligosaccharide supplementation for different categories of BMI (interaction of BMI and galactooligosaccharides: P = 0.0002; Figure 3). In individuals with a healthy weight (64% of the study population), those receiving 5.0 g galactooligosaccharides reported a 40% reduction (adjusted difference = 5.0%; 95% CI: 2.9, 7.2) in the probability of having a sick day compared with those receiving 0 and 2.5 g galactooligosaccharides. This protective effect was not seen in overweight and obese individuals (30% of the study population); however, in these individuals, a lower percentage of sick days was reported in those receiving 2.5 g galactooligosaccharides than in those receiving 0 or 5.0 g.

Table 2 Across all treatment groups, stress was positively related to the 5 gastrointestinal symptom score categories and was highly significant (P < 0.01) for all but constipation syndrome (P = 0.1017; data not shown). Across all levels of stress, gastrointestinal symptom scores were significantly lower with galactooligosaccharide supplementation for all symptom categories [diarrhea syndrome (treatment group effect: P = 0.0298), constipation syndrome (P = 0.0342), abdominal pain (P = 0.0058), and indigestion syndrome (P = 0.0003)] except reflux syndrome (P = 0.2073; Table 2). No differences in the number of stools per day were observed; however, daily stool consistency was softer with 2.5 g galactooligosaccharides (Table 2).
DISCUSSION
This study provides new information on the benefit of galactooligosaccharides on gastrointestinal and immune health outcomes in apparently healthy young adults undergoing an academic stress. As anticipated, in the 8 wk before, during, and after fall final exams, university undergraduates self-reported daily stress that was positively related to gastrointestinal symptoms, cold/flu symptom intensity, and the percentage of days with cold/flu. Galactooligosaccharide supplementation modulated all of these symptoms. The dose of 2.5-g galactooligosaccharides was more effective than the 5.0-g dose at reducing symptoms associated with abdominal pain (ie, abdominal pain, hunger pains, and nausea) and indigestion syndrome (ie, rumbling, bloating, burping, and gas). This is of interest to note considering that galactooligosaccharides are fermented by the intestinal microbiota, which results in gas production [17]. The higher dose of galactooligosaccharides (5.0 g) yielded a lower indigestion syndrome score than did the placebo (0 g) (Table 2). Although 2.5 g galactooligosaccharides was associated with slightly improved stool consistency, 5.0 g galactooligosaccharides was associated with the decreased likelihood of constipation syndrome.
To our knowledge this was the first study to show a benefit of galactooligosaccharides, a prebiotic, on modulating stress-induced gastrointestinal dysfunction in adults. Previously, Diop et al [18] showed a protective effect of a probiotic mix containing Lactobacillus acidophilus and Bifodobacterium longum on stress-induced gastrointestinal symptoms. In that 3-mo study, adults aged 18–60 y who were affected daily by symptoms of stress reported significantly less nausea and vomiting and abdominal pain with the probiotic than with the placebo. The authors suggested that the effects on the residual intestinal microbiota, intestinal barrier, and immune system may have modulated these symptoms [18]. In our study, galactooligosaccharides may have worked through similar mechanisms or through the HPA axis [6, 9, 10]. Galactooligosaccharide intake was previously shown to increase the numbers of bifidobacteria and lactobacilli [12, 19] as well as fecal short-chain fatty acids, which have been associated with decreased epithelial permeability [17, 20].
It is possible that gastrointestinal symptoms actually contributed to the reported level of stress. If this were the case, it may help to explain why 5.0 g galactooligosaccharides lost effectiveness at increased levels of stress (Figure 2). At lower levels of stress 5.0 g galactooligosaccharides was associated with lower average cold/flu SI, but this protective effect was lost at higher levels of stress. The 5.0-g dose of galactooligosaccharides was not as effective as the 2.5-g dose at reducing abdominal pain (Table 2). It could be that abdominal pain contributed to overall stress and ultimately to the risk of cold/flu symptoms.
In healthy-weight individuals, supplementation with 5.0 g galactooligosaccharides reduced the average percentage of days of cold/flu (Figure 3). This protective effect was not seen in underweight, overweight, and obese individuals. It should be noted that because 64% of the subjects fell within the healthy-weight category, we are most certain about these data. Additionally, emerging evidence points to differences in microbiota, including fewer bifidobacteria in obese than in lean individuals [21–23]. If galactooligosaccharides improved gastrointestinal and immune function by changing the microbiota, then it is possible that we would observe different effects in individuals within different BMI categories.
This study is one of the first to show a protective effect of galactooligosaccharides in relation to the percentage of days with cold/flu; however, many limitations need to be addressed. Academic stress was used as a model of acute psychological stress; although students only reported an average daily stress of 3 on the 10-point scale, with a high of 5 during exam week. Populations with higher levels of stress may experience more severe gastrointestinal and immune dysregulation. With a greater degree of daily stress, the galactooligosaccharide-associated health benefits may have been observed with a smaller sample size or, alternatively, may not have been observed to the same degree. Another limitation is in how we defined a day of cold/flu (ie, SI sum of >6 or a minimum of 3 different symptoms of more than minimal intensity). Although this is a fairly conservative definition compared with that used in other studies [1, 24, 25], we did not confirm the presence of cold/flu-associated pathogens. It was advantageous to report the percentage of days with cold/flu rather than the incidence and duration, because it is difficult to determine when one cold ends and a new cold begins. Another potential limitation is the use of Internet-based questionnaires in place of traditional paper questionnaires. Although student responses to the Internet version of the questionnaires were not compared with those to the traditional paper version, these comparisons were made with other questionnaires. Ritter et al [26] compared the distribution of responses from 16 different health-related instruments administered online with traditional mailed paper questionnaires. In every case, the Internet-based instrument appeared to be reliable, and Internet participation in the study was as good if not better than that of the traditional method [26]. For the undergraduate students in our study, the convenience of completing questionnaires online and the ability of the investigators to follow subject compliance in real time likely contributed to the high compliance rate.
In summary, acute psychological stress, such as that associated with academic exams, was directly related to symptoms of gastrointestinal dysfunction and cold/flu. Galactooligosaccharide supplementation attenuated these symptoms. Future studies should determine the mechanisms by which galactooligosaccharides improve health outcomes within the brain-gut-enteric microbiota axis, because these findings may have wide applicability beyond academic stress.
Acknowledgments
We thank Stephanie-Anne Girard, Amanda Shore, Carmelo Nieves Jr, Christina Nguyen, Allyson Radford, and all of the University of Florida undergraduates who helped with and participated in this study.
The authors’ responsibilities were as follows—BL-H, MCC, WJD, and VM: designed the research; CH, TC, YD-S, and BL-H: conducted the research; JCC and MCC: analyzed the data; CH, BL-H, JCC, WJD, MCC, and VM: wrote and edited the manuscript; and BL-H: had primary responsibility for final content. All authors read and approved the final manuscript. The study sponsor did not contribute to the design, implementation, analyses, or interpretation of the data. None of the authors had a personal or financial conflict of interest.
Return to ACIDOPHILUS
Since 9-29-2013


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |