

Combination of Acupuncture and Spinal
Manipulative Therapy: Management of a
32-year-old Patient With Chronic
Tension-type Headache and MigraineThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Chiropractic Medicine 2012 (Sep); 11 (3): 192–201 ~ FULL TEXT
OPEN ACCESS Bahia A. Ohlsen
Chiropractic Physician,
Chiropractic, Acupuncture and Yoga Center,
Buffalo Grove, IL.OBJECTIVE: The purpose of this case study is to describe the treatment using acupuncture and spinal manipulation for a patient with a chronic tension-type headache and episodic migraines.
CLINICAL FEATURES: A 32–year-old woman presented with headaches of 5 months' duration. She had a history of episodic migraine that began in her teens and had been controlled with medication. She had stopped taking the prescription medications because of gastrointestinal symptoms. A neurologist diagnosed her with mixed headaches, some migrainous and some tension type. Her headaches were chronic, were daily, and fit the International Classification of Headache Disorders criteria of a chronic tension-type headache superimposed with migraine.
INTERVENTION AND OUTCOME: After 5 treatments over a 2–week period (the first using acupuncture only, the next 3 using acupuncture and chiropractic spinal manipulative therapy), her headaches resolved. The patient had no recurrences of headaches in her 1–year follow-up.
CONCLUSION: The combination of acupuncture with chiropractic spinal manipulative therapy was a reasonable alternative in treating this patient's chronic tension-type headaches superimposed with migraine.
KEYWORDS: Acupuncture, Acupuncture analgesia, Headache disorders, Migraine headaches, Tension-type headaches
From the FULL TEXT Article:
Introduction
Migraines are common primary headaches, affecting 30% of women and 17% of men aged 21 to 34 years.1 These headaches can evolve and become chronic, exacting considerable personal and social economic cost2; they are the most likely headache to lead to analgesic drug overuse. [1, 2]
Acupuncture has been found to be clinically beneficial for patients with chronic headaches, particularly migraines [3–6] and tension-type headaches (TTHs). [7, 8] Acupuncture has also been suggested to be an effective first-line complementary alternative medicine modality to treat migraines. [9] Chiropractic care has also demonstrated evidence to manage adults with headaches. [10] However, at present, there have been no reported cases of management of migraine headaches with a combination of these 2 management strategies. The purpose of this case report is to describe treatment of chronic TTHs (CTTHs) with superimposed migraine using acupuncture and chiropractic spinal manipulative therapy.
Case report
A 32–year-old woman, 5'4” in height, 63.6 kg, presented in April 2010 with daily headaches that began in 2002. There was no precipitating incident leading up to the headaches other than she stated that she was “stressed” because of working full-time while in graduate school. She saw a neurologist who performed a brain magnetic resonance imaging, the result of which was negative. The patient was diagnosed with mixed headaches. Less than 8 days per month, the headaches were migrainous in nature; and the remaining chronic daily headaches (CDHs) were TTHs. She was given verapamil, a calcium channel blocker, and Tylenol (Johnson and Johnson, New Brunswick, NJ); and this combination of medications relieved the headaches.
In November 2009, the patient developed acute gastrointestinal symptoms: vomiting, nausea, and stomach cramping. She had no history of gastrointestinal disorders. Her blood laboratory values were unremarkable. She had normal results on upper and lower gastrointestinal scope studies. No specific diagnosis was given for her gastrointestinal symptoms.
Her doctor recommended that she consume a bland diet and stop all medications to control the gastrointestinal issues. She stopped eating fruits and vegetables. Her diet consisted primarily of bland carbohydrates: bread, cereal, and pasta. The patient felt that, as a result of stopping the medications, her headaches returned. Another brain magnetic resonance imaging was performed, and the result was similarly unremarkable. She was trying unsuccessfully to use over-the-counter analgesic drugs to control the headaches, taking 1 to 2 extrastrength Tylenol tablets per week.
The patient described the daily headaches as a tight band around her head, constant, and present over both temples and midbrow; they were not worsened by physical or mental exertion, differentiating them from both medication overuse headaches (MOHs) and migraines. She stated that nothing made them either better or worse. The superimposed migraines, which occurred less than 8 times a month, were pulsatile, throbbing, and stabbing over her right temple; were accompanied by vertigo, ptosis, photophobia, and nausea; and worsened with exertion. She experienced an aura before the migraine, consisting of scintillating scotomas, flashing lights in her visual field. On a Visual Analog Scale pain scale of 1 to 10 (1 being the least intense and 10 being the most intense), she stated that the headaches ranged in intensity between a level 2 and a level 8. The CTTHs were always present, regardless of the time of day or night. When her stress levels increased, the headaches became very intense and migrainous in nature. Her medical history was unremarkable, except for episodic migraine headaches that began in her late teens. Her mother and sister also experienced migraines.
The patient reported that she tried getting a massage, and this exacerbated the headaches and made her feel ill. She had never received acupuncture or spinal manipulative therapy.
Palpation of her neck revealed tenderness and tightness over the suboccipital area on the right side. Deep palpation of the right upper cervical spine elicited a painful localized response. Active right rotation of her cervical spine was reduced compared to active left rotation of her cervical spine. Passive right rotation and right lateral bending of her neck were decreased compared to passive left rotation and left lateral bending. Motion palpation examination of her cervical spine revealed segmental dysfunction of the right upper cervical spine.
On the day she first presented to the office, she had a migraine headache. She had ptosis of her right eyelid, although her vision was not altered and results of cranial nerve and fundoscopic examinations were normal. Her right and left temples and scalp above her ears were tender to light touch. Notable in her history was a high level of fatigue. Her prior activities included kickboxing, running, and working out twice a week with a personal trainer; and now she experienced fatigue with walking. She stated that she was unable to concentrate effectively. In addition, she experienced dizziness when changing positions, such as standing up after being seated. She also experienced dizzy spells even without changing positions.
A Traditional Chinese Medicine history and examination concluded that she had a blood deficiency, liver qi stagnation and gall bladder channel obstruction. The reasons for this diagnosis were as follows: she had headaches and cold hands and feet; her periods were very scanty, although regular; she had menstrual cramping in the middle of the night during her period; her tongue was pale and had a very thin white coat; and her pulses were weak, wiry, and deep in all positions. In addition, she got dizzy and lightheaded when changing positions, her energy was low, she had dry eczematous patches of skin, and her complexion was dull white. And finally, she had multiple tender points on her head, neck, and shoulders following the gall bladder channel.
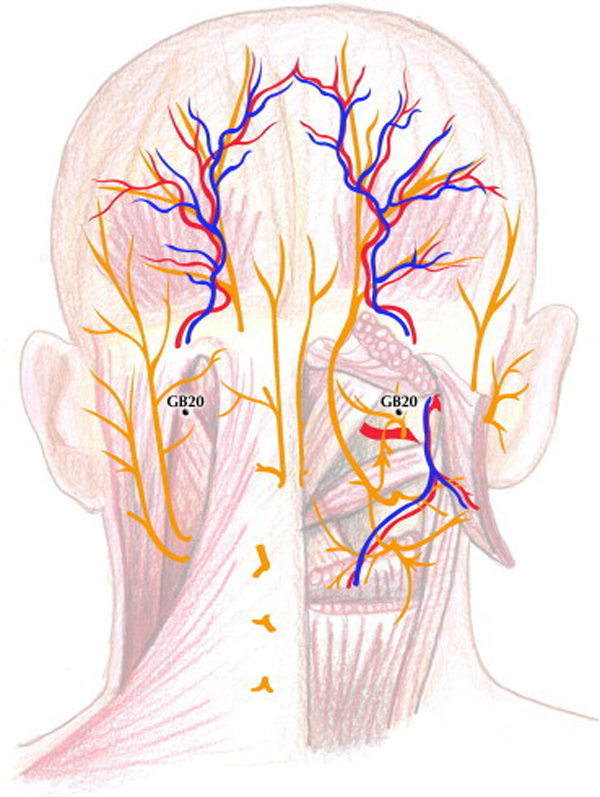
In Traditional Chinese Medicine, if pressure and massage over an area exacerbate the condition, it most likely indicates an excess condition or a blockage. The location of the most intense migraine headaches was over the outer canthus of her right eye, the location of the beginning of the gallbladder meridian (BL), GB 1, the meeting point of the small intestine and triple warmer meridians (Figure 1). This area was very sensitive to light touch, as were GB 20, at the base of the skull on the right side, and GB 8 above her ears (Figure 2).
Figure 1. Location of gallbladder (GB) meridian 1 and 8.
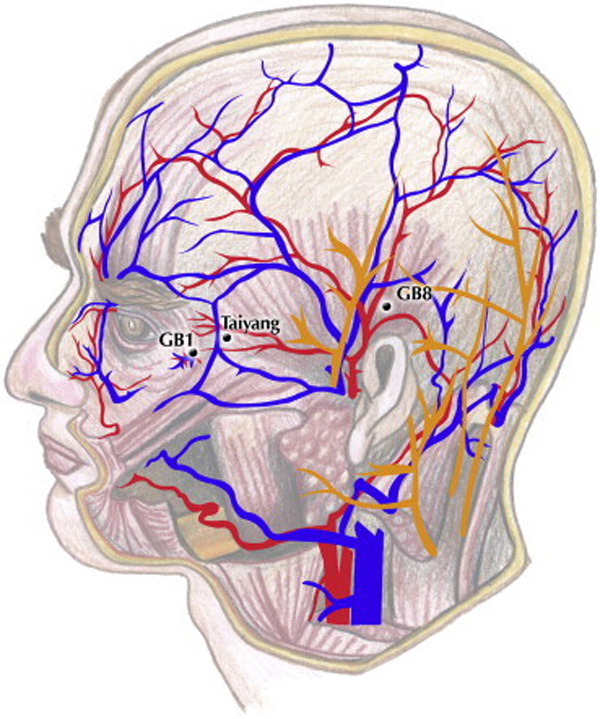
Figure 2. Location of gallbladder (GB) meridian 20.
The patient was diagnosed with and treated for CTTH with superimposed migraines, using the Traditional Chinese Medicine protocols for blood deficiency, liver qi stagnation, and gall bladder channel obstruction described above. She was also diagnosed with cervical spine segmental joint dysfunction. The right eyelid ptosis due to parasympathetic activation of the sphenopalatine ganglion, [11] the vertigo, and the throbbing unilateral nature of the most intense frontotemporal and ocular pain, including unilateral neck pain, were characteristic of migraines. [12]
The goals of the acupuncture therapy were to relieve the headaches and address the blood deficiency, liver qi stagnation, and gall bladder channel obstruction. The goal of the chiropractic spinal manipulative therapy was to restore active and passive cervical spine range of motion. The supine lateral cervical break technique was administered to the upper cervical spine to address the segmental dysfunction. No other areas were manipulated, and no physical therapy or modalities were used at this time.

Table 1 Table 1 lists points that were used on the first, third, and fifth visits to relieve the headaches and harmonize the paired liver and BL. The patient was lying supine for these points. She was seated for the insertion of BL 18 (1.5 cun lateral to T9) and BL 19 (1.5 cun lateral to T10), bilaterally, with a Tai-Chi Power 80, 0.25 × 50 mm, sterile single-use acupuncture needle, which was then twirled clockwise, pressed in a caudal direction against the skin, and taped so that she could lie back down. The choice of GB 1, GB 8, and GB 20 was made because these points were very tender to palpation and because GB 1 was the location of her most intense headaches. GB 20 was also needled with the patient in a seated position. She then reclined supine on the treatment table with the headpiece wide enough to accommodate the GB 20 needle, and GB 1 was needled during the same session.

Table 2 Table 2 lists points that were used on the second, fourth, sixth, and 3 subsequent follow-up visits after her headaches resolved. The goal was to address the blood deficiency. Patient was lying prone for these points. The reason that treatment of the gallbladder channel obstruction and liver qi stagnation and treatment of the blood deficiency were done on different days was because it was felt that there would be too many points used if these were done all on the same treatment session.
The needle type used was Tai-Chi Power 80, 0.18 × 15 mm, over face points, Tai-Chi Power 80, 0.25 × 30 mm, on arms and legs, single-use, sterile needles; and on BL 18 and BL 19, when patient was lying supine, Tai-Chi Power 80, 0.25 × 50 mm, single-use needles were used. The needles remained in place for 35 minutes after the arrival of “deqi” (a heavy pressure, achy, dull, or pulling sensation) was obtained; needles were twirled clockwise slowly at desired points for tonification effect, namely, ST 36, K 3, K 7, BL 18, and BL 19. At GB 1, needle insertion was 0.5 cun obliquely toward GB 8. This method of needling can simultaneously stimulate one of the extra acupuncture points, Tai Yang (M-HN-9).
Dietary treatment was designed to reintroduce fruits, vegetables, and proteins to her daily regimen. The reason for the diet change is that it was suspected that her recent diet was high in refined simple carbohydrates and low in protein, and may have contributed to the elevated liver enzymes.13 No supplements were given to the patient.

Table 3 The first treatment was acupuncture only, after which the patient reported she had no headache for 2 hours (Table 3). When the headache returned to the original location over her right eye, GB 1, and temple, it was less intense than that in the prior day. The second treatment was acupuncture only, after which the patient reported a 90% reduction in headache intensity over the same area for the remainder of the day. The third treatment was acupuncture and spinal manipulative treatment, after which the patient reported that her headache was now no longer over her right eye and temple, but localized over her right suboccipital area, over GB 20. The fourth treatment was acupuncture and spinal manipulative treatment, after which the patient reported that the headache was still reduced by 90% from its original intensity and localized on the right side of her neck. The fifth treatment was acupuncture and chiropractic spinal manipulative treatment (high-velocity, low-amplitude, manual technique), after which the patient reported that her headache over her right temple, eye, and neck was completely gone.

Table 4 The patient received 5 treatment sessions in a 2 week period, after which she reported no further headaches. Four follow-up treatments of acupuncture and chiropractic spinal manipulation were continued over an 11–week period to monitor the headaches, her response to the reintroduction of varied foods into diet, and her liver enzyme levels (Table 4). At the time of her last treatment session, she continued to be headache-free; her diet was varied and normal; and her liver enzymes had returned to normal healthy levels. One year later, the patient was contacted; and she reported no recurrences of headaches. The patient gave permission for publication of this case study.
Discussion
This case study supports the literature that recommends acupuncture as first-line therapy for migraines. [9] Spinal manipulative therapy has been reported to be an effective prophylactic therapy for migraines [14] and treatment of CTTHs. [10, 15]
Observational and population-based studies describe progressive migraine headaches that become CDHs, a condition that affects 3% to 5% of the population with episodic headaches. [16–21] Chronic daily headaches are defined as primary headaches that occur at least 15 days per month, [22–26] although they are not described in the International Classification of Headache Disorders (ICHD)–2 criteria.
Two of the most common primary headaches are TTHs and migraine headaches. [9, 22] Most CDHs are also either chronic migraines or CTTHs. [23] According to the ICHD-2, CTTHs are characterized as TTHs for at least 15 days per month, lasting at least 3 months, with less than 8 days per month meeting the criteria for migraine. [27]
Tension-type headaches are described as being bilateral, nonpulsating, tightening, or squeezing sensation around the head and not aggravated by activity. Tension-type headaches are not accompanied by moderate or severe nausea and vomiting, and only one of the following: photophobia, phonophobia, or mild nausea. [22, 27]
When CTTHs are accompanied by less than 8 migraines per month, the ICHD-2 classifies these patients as having CTTH with migraine. [21, 27] The term chronic migraine has been suggested as being more appropriate to describe migraine attacks superimposed on a background of daily TTH. [22, 23] The ICHD-2 criteria use the term chronic migraine specifically when patients experience more than 8 migraines per month for more than 3 consecutive months. [27]
According to the ICHD-2 criteria, migraine headaches are characterized by unilateral, moderate-to-severe pulsating pain that is aggravated by activity. Migraines are accompanied by either nausea and vomiting or light and sound sensitivity, and at least one of the following: visual changes such as scintillating scotomas, fortification spectra or photopsia, sensory changes (either paresthesia or numbness), unilateral weakness, or aphasia. [27]
Headaches can evolve and become chronic, which may lead to analgesic drug overuse [1, 2] and can result in concurrent secondary headaches called medication overuse headaches or rebound headaches. [2, 16, 27] Medication overuse headaches are described as headaches that are present on more than 15 days per month, with regular use for more than 3 months of either (1) ergotamine, triptans, opioids, or combination analgesic medication on more than 10 days per month or (2) simple analgesics or any combination of ergotamine, triptans, and analgesic opioids on more than 15 days per month. [26] Most notably, the headache worsens during the period of medication overuse. [18, 19, 21, 23] What differentiates the quality of MOHs from CTTHs most clearly is that MOHs worsen significantly with mental or physical exertion, whereas CTTHs do not. Medication overuse headaches occur in approximately 1% of the population [28] and can be a major contributing factor in the transformation of episodic headaches to CDHs. [29] According to the ICHD-2, the diagnosis of MOH is made when medication is withdrawn for 2 months and the headache either resolves or reverts to its previous episodic pattern.27 Thirty percent of all CDH patients are estimated to have MOH. [20]
The term transformed migraines is used to describe a progressive evolution from episodic migraine headaches to chronic migraine headaches, formerly called mixed headaches, [19] 80% of the time against a background of MOH,20–25 although this evolution can also occur without medication overuse. [25, 26, 30–32] Some authors state that 14% of patients will transform from episodic to chronic migraine headaches. [21] Transformed migraines are not addressed in the ICHD-2. [19, 21–23] Migraines can be chronic, more than 8 migraines per month for 3 months according to ICHD-2 criteria, [27, 30] without being transformed. Transformed migraines, which are daily or near-daily “mixed” TTH and migraine in nature, [19, 28] occur predominantly in women, starting as strictly simple episodic migraines associated with or (more commonly) without auras in the teens and early 20s. [25, 28] They then change (hence “transform”), becoming more frequent and less severe, losing their episodic nature, [19, 25, 28] and becoming associated with allodynia or reduced pain thresholds [33, 34] and changes in the periaqueductal gray matter. [24]
Patients who have migraines are the most likely to overuse medications.35 Approximately 65% of patients with chronic daily MOHs had migraines, 27% had TTHs, and 8% had mixed or other types of primary headaches. [36–39] Treatment of transformed migraines usually involves discontinuing the medication that is creating the MOH and preventatively managing the episodic migraines with pharmaceuticals. [20, 24–26]
Chronic migraines are described in the ICDH-2 as primary headaches occurring more than 15 d/mo for more than 3 months, with at least 8 days meeting the criteria for migraine. When the migraine headaches occur less than 8 days per month, against a backdrop of CTTH, without medication overuse, the description of CTTH with superimposed migraine is most accurate. [19, 27, 31] It is estimated that 2.5% of patients with either high-frequency (10–14 headaches per month) or low-frequency (< 10 headaches per month) migraine will transition to chronic migraines (? 15 headaches per month). [24, 25]
The reason this headache case is not described as a transformed migraine is because the medication use did not meet or exceed that required to describe a migraine headache superimposed on a MOH; however, it is possible that this patient developed a transformed migraine without medication overuse, as there are proposed classification criteria for transformed migraines both with and without medication overuse. [19] When episodic migraines become progressively more chronic in nature, differentiating a transformed migraine without medication overuse from a chronic migraine becomes a difficult and debatable subject. [37–39] For the sake of conforming to the current ICHD-2 criteria in this case, the term transformed migraine is not used, although it could be an accurate description; and because of the low frequency of migraine headaches (< 8 migraines per month), the term chronic migraine is not used.
In Traditional Chinese Medicine, GB 1, GB 8, and GB 20 points together with K 3 and ST 36 (specifically nourishing kidney yin, tonifying qi, and calming shen) are thought to resolve the liver qi stagnation and gall bladder channel obstruction, tonifying the qi and blood. In Western medicine, stimulating GB 1, GB 8, and GB 20 is thought to lead to changes in the nervous system and blood circulation.GB 1: Located beneath this point are the zygomaticoorbital artery and vein, the zygomaticofacial nerve (V2), and the zygomatic and temporal branch of the facial nerve. The insertion technique needling obliquely toward GB 8 also stimulates Tai Yang by transverse insertion, beneath which is the zygomaticotemporal nerve (V2).
GB 8: Located beneath this point are the parietal branches of the superficial temporal artery and vein and the anastomotic branches of the auriculotemporal nerve and the great occipital nerve.\
GB 20: Located beneath this point are the branches of the occipital artery and vein and a branch of the lesser occipital nerve.Migraine attacks are thought to begin with disinhibition of the trigeminal ganglion, by activation of the contralateral thalamus and dorsal rostral brainstem, [40, 41] which results in the release of vasoactive peptides at the vascular ends of the trigeminal nerve fibers. [42] The end result of the release of these vasoactive peptides, such as substance P, is a state of neurogenic inflammation [43] and stimulation of the trigeminal nucleus [44] by nociceptive unmyelinated C fibers. The trigeminal nerve and upper cervical nerve root innervate the structures in the brain with nociceptive unmyelinated C fibers: the large cerebral vessels, meningeal blood vessels, venous sinus, and pia and dura mater. [44] The mechanism by which acupuncture modulates pain is by the activation of large fibers, specifically A-Beta and A-Delta fibers, which stimulate both wide dynamic range neurons and inhibitory neurons in layers III, IV, and V of the dorsal horn. These touch, pressure, and proprioceptive fibers are inhibitory or antinociceptive; they modulate the pain sensation by stimulating GABA and glycine release via interneurons at the spinal cord level. Wide dynamic range neurons receive highly convergent input from joints and muscles and via the paleospinothalamic tract, and continue on to nonspecific inhibitory thalamic nuclei. Because migraines are believed to begin through disinhibition of the trigeminal nucleus via activation of the thalamus, this mechanism explains how acupuncture can modulate pain.
Activating large-diameter fibers by acupuncture can suppress the pain signal by increasing the release of norepinephrine and serotonin,45–48 enkephalins, and opioids, [49, 50] which inhibit neurotransmission in the dorsal horn. [51–54]
One study showed that acupuncture-induced analgesia is created by both central and peripheral mechanisms; the peripheral endorphin release plays a role in downregulating the neurogenic inflammation. [55] Central mechanisms include initiating descending pain control through the insular and frontal cortex activation of the periaqueductal gray, the strongest center to suppress pain, via the spinoreticulothalamic tract.
Spinal manipulative therapy also activates large-diameter A-Beta touch, pressure and proprioceptive fibers, deep afferents, in muscles, ligaments and joints. Creating normal movement through exercise, mobilization, or spinal manipulative therapy within a joint stimulates normal proprioceptive receptors that activate GABAergic receptors; this is antinociceptive and can block pain from spinal tissues. Spinal manipulative therapy has been shown to increase cutaneous pain tolerance levels, [56, 57] decrease local electromyographic activity in painful joint segments, [57] as well as potentially activate the descending inhibitory pathways of the periaqueductal gray [58] through the administration of appropriate mechanical input.
GB 1, GB 8, GB 20, and Tai Yang represent local “Ashi points” or tender points in Traditional Chinese Medicine. Needling these tender points for migraine headaches, noted Melzack in 1977, may create relief by “hyperstimulation analgesia,” similar in nature to trigger point therapy, increasing input to the inhibitory mechanisms of pain as explained by the gate theory. [59, 60] More recent studies that support acupuncture for migraine prevention and relief suggest that the pain relief is indeed achieved by the needling process and subsequent neurological changes, but that the results are not as dependent on point specificity or the arrival of “deqi.” [3, 4]
Headache pain relief has been obtained from needling both acupuncture points and sham points. [3–9] It is interesting to question, however, whether the sham acupuncture points used were actual acupuncture points in acupuncture traditions other than Traditional Chinese Medicine and whether the neurological input that occurred during the sham acupuncture treatment was sufficient to trigger the central and peripheral changes associated with acupuncture analgesia.
The liver-gallbladder system in Oriental medicine bears no correlation to the liver and gallbladder in Western medicine. The patient's unusual diet of highly refined carbohydrates and low protein and her level of fatigue led to the comprehensive metabolic panel order and the discovery of the elevated liver enzymes. The most likely reason for the elevated liver enzyme levels was the unusual high-carbohydrate, low-protein nature of her diet13 and perhaps, but less likely, the prolonged nonsteroidal anti-inflammatory use. The reason a patient may develop liver qi stagnation and gallbladder channel obstruction is from prolonged emotional stress and/or liver blood deficiency. The patient's prolonged inappropriate diet likely contributed to deficiencies in the spleen's transformation and transportation functions, eventually causing the blood deficiency, which in turn led to the liver qi stagnation. As the kidneys are the mother of the liver, the kidneys' deficiency may induce secondary liver qi stagnation as well.
Limitations
As this is a study of one patient, it cannot be certain that the treatment was responsible for the response in the patient, as there are other uncontrolled factors. As well, it is not quantifiable how much of the headache could be attributed to the patient's unusual 5–month diet and how much relief could be attributed to the gradual balancing of the food groups. However, it is suspected that the diet was not a precipitating factor because the onset of migraines started in her teens. It is also not known what relationship the headache that began in 2009 had to the headaches that were diagnosed and treated pharmacologically in 2002, although she described them as being similar in nature (chronic daily TTHs with migraines a couple of times a month). It is also possible that an improvement in the daily headaches was due to cessation of analgesic use. This would have meant that the chronic daily TTHs were MOHs and that the migraines were being maintained by analgesic overuse. Additional limitations of this case report are that this study was of one patient and that the results may not be generalizable to the broader population with headache disorders. Furthermore, there remains the possibility that the treatment had a placebo effect resulting in the patient improving. Larger studies are needed to determine if the combination of acupuncture with spinal manipulation is more effective than either proven therapy alone for populations with CTTH and superimposed migraines.
Conclusions
A patient presented with CTTH with superimposed migraine headaches of 5 months' duration. She had not been headache-free without pharmaceutical therapy since she was a teenager. Her headaches resolved after the first 5 sessions, and she reported that she was headache-free 1 year later. The combination of acupuncture with chiropractic spinal manipulative therapy seemed to be a reasonable alternative management strategy in managing this patient's headaches.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
Acknowledgment
The author thanks Yihyun Kwon, DC, MSOM, PhD, faculty advisor, and Jerrilyn Cambron DC, PhD, for their guidance in writing this case report and Robert Hansen, Graphic Designer, for his original illustrations of GB 1, GB 8, and GB 20.
References:
Lipton R.B., Bigal M.E., Diamond M., Freitag F., Reed M.L., Stewart W.F. AMPP Advisory Group. Migraine prevalence, disease burden, and the need for preventative therapy. Neurology. 2007;68:343
Bigal M.E., Serrano D., Reed M., Lipton R.B. Chronic migraine in the population: burden, diagnosis, and satisfaction with treatment. Neurology. 2008;71:559–566
Endres H.G., Diener H.C., Molsberger A. Role of acupuncture in the treatment of migraine. Expert Rev Neurother. 2007;7:1121–1134
Linde K., Allais G., Brinkhaus B., Manheimer E., Vickers A., White A.R. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009;(1):CD001218
Vickers A.J., Rees R.W., Zollman C.E., McCarney R., Smith C.M., Ellis N. Acupuncture for chronic headache in primary care: large, pragmatic, randomised trial. BMJ. 2004;328:744
Birch S., Hesselink J.K., Jonkman F.A., Hekker T.A., Bos A. Clinical research on acupuncture. Part 1. What have reviews of the efficacy and safety of acupuncture told us so far? J Altern Complement Med. 2004;10:468–480
Linde K., Allais G., Brinkhaus B., Manheimer E., Vickers A., White A.R. Acupuncture for tension-type headache. Cochrane Database Syst Rev. 2009;(1):CD007587
Granato A., Chiodo Grandi F., Stokelj D., Musho S., Pizzolato G. Acupuncture in tension-type headache. Neuroepidemiology. 2010;35:160–162
Nicholson R.A., Buse D.C., Andrasik F., Lipton R.B. Nonpharmacologic treatments for migraine and tension-type headache: how to choose and when to use. Curr Treat Options Neurol. 2011;13:28–40
Bryans R, Descarreaux M, Duranleau M, Marcoux H, Potter B, Ruegg R.
Evidence-Based Guidelines for the Chiropractic Treatment
of Adults With Headache
J Manipulative Physiol Ther. 2011 (Jun); 34 (5): 274–289Barbanti P., Fabbrini G., Pesare M. Neurovascular symptoms during migraine attacks. Cephalgia. 2001;21:295.
Evans R.W. Migraine: a question and answer review. Med Clin NA. 2009;93:245–262
Simek J., Shkurupy V.A., Shorina G.N., Bgatova N.P., Cervinková Z., Holecek M. Effect of long-term administration of a high protein or low protein diet on rat liver. Morphological and biochemical findings. Physiol Bohemoslov. 1986;35:127–133
Nelson C.F., Bronfort G., Evans R., Boline P., Goldsmith C., Anderson A.V. The efficacy of spinal manipulation, amitriptyline and the combination of both therapies for the prophylaxis of migraine headache. J Manipulative Physiol Ther. 1998;21:511–519
Boline PD, Kassak K, Bronfort G, Nelson C, Anderson AV.
Spinal Manipulation vs. Amitriptyline for the Treatment of Chronic Tension-type Headaches:
A Randomized Clinical Trial
J Manipulative Physiol Ther 1995 (Mar); 18 (3): 148–154Lipton R.B., Pan J. Is migraine a progressive brain disease? JAMA. 2004;291:493–494
Kavuk I., Yavuz A., Cetindere U., Agelink M.W., Diener H.C. Epidemiology of chronic daily headache. Eur J Med Res. 2003;8:236–240
Wiendels N.J., Knuistingh Neven A., Rosendaal F.R., Spinhoven P., Zitman F.G., Assendelft W.J. Chronic frequent headache in the general population: prevalence and associated factors. Cephalgia. 2006;26:1434–1442
Silberstein S.D., Lipton R.B., Sliwinski M. Classification of daily and near-daily headaches: field trial of revised IHS criteria. Neurology. 1996;47:871–875
Scher A.I., Lidgette L.A., Lipton R.B. Risk factors for headache chronification. Headache. 2008;48:16–25
Couch J.R. Update on chronic daily headaches. Curr Treat Options Neurol. 2011;13:41–55
Bigal M.E., Lipton R.B. Tension-type headache: classification and diagnosis. Curr Pain Headache Rep. 2005;9:423–429
Garza I., Schwedt T.J. Diagnosis and management of chronic daily headache. Semin Neurol. 2010;30:154–166
Lipton R.B. Tracing transformation: chronic migration classification, progression, and epidemiology. Neurology. 2009;92(5 Suppl):S3–S7
Silberstein S.D. Chronic daily headache. J Am Osteopath Assoc. 2005;105:23S–29S
Dodick D.W. Clinical practice. Chronic daily headache. N Engl J Med. 2006;354:158–165
Headache Classification Subcommittee of the International Headache Society The international classification of headache disorders, 2nd edn. Cephalgia. 2004;24(Suppl. 1):9–160
Munakata J., Hazard E., Serrano D., Klingman D., Rupnow M.F., Tierce J. Economic burden of transformed migraine: results from the American Migraine Prevalence and Prevention (AMPP) Study. Headache. 2009;49:498–508
Kavuk I., Katsarva Z., Selekler M., Sayar K., Agelink M.W., Limmroth V. Clinical features and therapy of medication overuse headache. Eur J Med Res. 2004;9:565–569
Silberstein S.D., Burstein R., Dodick D.W., Lipton R.B. Understanding the clinical features, biology, and management of transformed migraine: the evidence base. Continuing Education. Annual Scientific Meeting of the American Headaches Society. Boston; 2005.
Allais G., De Lorenzo C., Quirico P.E., Lupi G., Airola G., Mana O. Non-pharmacological approaches to chronic headaches: transcutaneous electrical nerve stimulation, laser therapy and acupuncture in transformed migraine treatment. Neurol Sci. 2003;24(Suppl 2):S138–S142
Dodick D., Freitag F. Evidence-based understanding of medication-overuse headache: clinical implications. Headache. 2006;46(Suppl. 4):S202–S211
Cooke L., Eliasziw M., Becker W.J. Cutaneous allodynia in transformed migraine patients. Headache. 2007;47:531–539
Kitaj M.B., Klink M. Pain thresholds in daily transformed migraine versus episodic migraine headache patients. Headache. 2005;45:992–998
Diener H.C., Limmroth V. Medication-overuse headache: a worldwide problem. Lancet Neurol. 2004;3:475–483
Scher A.I., Stewart W.F., Ricci J.A., Lipton R.B. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003;106:81–89
Headache Classification Committee. Olesen J., Bousser M.G., Diener H.C., Dodick D., First M., Goadsby P.J. New appendix criteria open for a broader concept of chronic migraine. Cephalgia. 2006;26:742–746
da Silva A., Jr, Costa E.C., Gomes J.B., Leite F.M., Gomez R.S., Vasconcelos L.P. Chronic headache and comorbidities: a two-phase population-based, cross-sectional study. Headache. 2010;50:1306–1312
Seshia S.S., Woeber-Bingoel C., Guidetti V. The classification of chronic headache: room for further improvement? Cephalgia. 2010;30:1268–1270
Bahra A., Matharu M.A., Buchel C., Frackowiak R.S.J., Goadsby P.J. Brainstem activation specific to migraine headache. Lancet. 2001;357:1016–1017
Weiller C., May A., Limmroth V., Jüptner M., Kaube H., Schayck R.V. Brain stem activation in spontaneous human migraine attacks. Nat Med. 1995;1:658–660
Limmroth V., Katsarava Z., Liedert B., Guehring H., Schmitz K., Diener H.C. An in vivo rat model to study calcitonin gene related peptide release following activation of the trigeminal vascular system. Pain. 2001;92:101–106
Hanko J., Hardebo J.E., Kåhrström J., Owman C., Sundler F. Calcitonin gene-related peptide is present in mammalian cerebrovascular nerve fibers and dilates pial and peripheral arteries. Neurosci Lett. 1985;57:91–95
Moskowitz M.A., Moskowitz R. Neurovascular and molecular mechanisms in migraine headaches. Cerebrovasc Brain Metab Rev. 1993;5:159–177
McLennan H., Gilfillan K., Heap Y. Some pharmacological observations on the analgesia induced by acupuncture in rabbits. Pain. 1977;3:229–238
Shen E., Ma W.H., Lan C. Involvement of descending inhibition in the effect of acupuncture on the splanchnically evoked potential in the orbital cortex of cat. Sci Sin. 1978;21:677–685
Cheng R.S., Pomeranz B. Monoaminergic mechanism of electroacupuncture analgesia. Brain Res. 1981;215:77–92
Han C.S., Chou P.H., Lu C.C., Lu L.H., Yang T.H., Jen M.F. The role of central 5-hydroxytryptamine in acupuncture analgesia. Sci Sin. 1979;22:91–104
Mayer D.J., Rafii A. Antagonism of acupuncture analgesia in man by the narcotic antagonist naloxone. Brain Res. 1977;121:368–372
Pomeranz B., Chiu D. Naloxone blockage of acupuncture analgesia: endorphin implicated. Life Sci. 1976;19:1757–1762
Chen X.H., Han J.S. All three types of opioid receptors in the spinal cord are important for 2/15 Hz electroacupuncture analgesia. Eur J Pharmacol. 1992;211:203–210
Han J.S., Xie G.X., Shou Z.F. Acupuncture mechanisms in rabbits studied with microinjection of antibodies against beta-endorphin, enkephalin and substance P. Neuropharmacology. 1984;23:1–5
Han J.S., Xie G.X. Dynorphin: important mediator for electroacupuncture analgesia in the spinal cord of the rabbit. Pain. 1984;18:367–376
Tsai H.Y., Lin J.G., Inoki R. Further evidence for possible analgesic mechanism of electroacupuncture: effects on neuropeptides and serotonergic neurons in rat spinal cord. Jpn J Pharmacol. 1989;49:181–185
Ceccherelli F., Gagliardi G., Ruzzante L., Giron G. Acupuncture modulation of capsaicin-induced inflammation: effect of intraperitoneal and local administration of naloxone in rats. A blinded controlled study. J Altern Complement Med. 2002;8:341–349
Terrett A.C., Vernon H. Manipulation and pain tolerance. A controlled study of the effect of spinal manipulation on paraspinal cutaneous pain tolerance levels. Am J Phys Med. 1984;63:217–225
Lehman G.J., Vernon H., McGill S.M. Effects of a mechanical pain stimulus on erector spinae activity before and after a spinal manipulation in patients with back pain: a preliminary investigation. J Manipulative Physiol Ther. 2001;24:402–406
Sterling M., Full G., Wright A. Cervical mobilization: current effects on pain, sympathetic nervous system activity and motor activity. Man Ther. 2001;6:72–81
Melzack R., Stillwell D.M., Fox E. Trigger points and acupuncture points for pain: correlations and implications. Pain. 1977;3:3–23
Melzack R. Basic Books; New York: 1973. The puzzle of pain.

Return to HEADACHE
Return to ACUPUNCTURE
Since 3-06-2013


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |