

Effectiveness of Manual Therapy for Chronic Tension-type Headache:
A Pragmatic, Randomised, Clinical TrialThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Cephalalgia. 2011 (Jan); 31 (2): 133–143 ~ FULL TEXT
Rene F Castien, Danielle AWM van der Windt, Anneke Grooten and Joost Dekker
Healthcare Centre Haarlemmermeer,
The Netherlands.
r.castien@vumc.nl
OBJECTIVE: To evaluate the effectiveness of manual therapy (MT) in participants with chronic tension-type headache (CTTH).
SUBJECTS AND METHODS: We conducted a multicentre, pragmatic, randomised, clinical trial with partly blinded outcome assessment. Eighty-two participants with CTTH were randomly assigned to MT or to usual care by the general practitioner (GP). Primary outcome measures were frequency of headache and use of medication. Secondary outcome measures were severity of headache, disability and cervical function.
RESULTS: After 8 weeks (n = 80) and 26 weeks (n = 75), a significantly larger reduction of headache frequency was found for the MT group (mean difference at 8 weeks, -6.4 days; 95% CI -8.3 to -4.5; effect size, 1.6). Disability and cervical function showed significant differences in favour of the MT group at 8 weeks but were not significantly different at 26 weeks.
CONCLUSIONS: Manual therapy is more effective than usual GP care in the short- and longer term in reducing symptoms of CTTH. Dutch Trial Registration no. TR 1074.
From the FULL TEXT Article:
Introduction
The point prevalence of chronic tension-type headache (CTTH) in adults has been estimated at 3%. [1] In half of the CTTH cases, headache-related impairment in work performance and participation is reported. In addition to considerable impact on daily functioning and work participation, CTTH is a risk factor for overuse of analgesic medication. [2–4] Only about 20% of the CTTH patients seek medical care for their headache. This low consultation rate may be explained by insufficient information on the effectiveness of treatments or by negative experiences with healthcare. [2, 5, 6]
Several treatments are used in primary care, including pharmacology, physical therapy, stress management, and acupuncture. There is no substantial evidence to support any of these treatments. [7] In primary care, treatment for patients with CTTH is often provided by the general practitioner (GP). The Dutch national general practice guideline for the management of headache describes diagnostic and therapeutic algorithms, consisting mainly of re-assurance, life-style advice and medication. [8] The effectiveness of this guideline for patients with CTTH has not been investigated.
The pathogenesis of CTTH remains unclear. Pathophysiological theories considering central (sensitisation and inadequate endogenous pain control) and peripheral (myofascial nociception) pain mechanisms have been described and discussed in the literature. [7, 9] The relationship between CTTH and impairment of the craniocervical musculoskeletal function (forward head position, trigger points trapezius muscle, neck mobility) has been reported in recent literature. [10–13] This leads to the hypothesis that improvement of the craniocervical musculoskeletal function by manual therapy, an intervention targeted at mobilisation, active stabilisation of the cervical spine and postural correction, may be an effective intervention to reduce pain in CTTH.
Until now, evidence has been lacking to draw definite conclusions regarding the use of a manual therapy intervention in the treatment of CTTH. Previous studies show methodological shortcomings, including heterogeneity of mobilisation techniques and small sample sizes. [14] Well-designed clinical trials have been recommended to provide more substantial evidence for the effectiveness of manual therapy. [14, 15] The objective of our trial was to evaluate the effectiveness of manual therapy on frequency of headache, use of pain medication, impact of headache and cervical physical function in patients with chronic tension-type headache, compared to usual care by the GP.
Patients and methods
The study was a pragmatic, multicentre, randomised, clinical trial with unblinded treatment, self-reported primary outcome and partly blinded secondary outcome assessment. Participants were randomised to receive either manual therapy (MT) or usual care (UC) by the general practitioner (GP). Assessments were performed at baseline, directly after the treatment period of 8 weeks and after 26 weeks. The procedures and design of this study were approved by the Medical Ethics Committee of the VU University Medical Centre in Amsterdam, The Netherlands. The design of this study has been published [16] and is registered with the Dutch Trial Register (no. TR 1074). The design conforms to the guidelines of the International Headache Society (IHS) for the design of randomised clinical trials. [17]
Study population
Thirty-eight GPs working in primary healthcare centres and private settings in an urban area in The Netherlands provided eligible participants with headache with written information about the trial. For participants interested in participation, a researcher screened eligibility by telephone and made an appointment for the baseline assessment at a research clinic. During this appointment, written consent was obtained and, subsequently, a baseline assessment was carried out by a research assistant which included a standardised history and a 2-week headache diary that was kept by the participant prior to the baseline assessment. Participants were enrolled in the study if they were between 18–65 years old and fulfilled the CTTH criteria according to the classification of headaches of the IHS: [18] headache occurring on at least 15 days on average per month for a period of more than 3 months and headache lasting for hours, or was continuous.
The headache has at least one of the following characteristics:(i) bilateral location;
(ii) pressing/tightening (nonpulsating) quality:
(iii) mild or moderate intensity, not aggravated by normal physical activity such as walking or climbing stairs – and both of the following:
(iv) no more than one of photophobia, phonophobia or mild nausea; and
(v) neither moderate or severe nausea nor vomiting.Participants were excluded if they had rheumatoid arthritis, suspected malignancy, pregnancy, intake of either triptans, ergotamines or opioids on ≥10 days/month or simple analgesics on ≥15 days/month on a regular basis for ≥3 months, if they had received manual therapy treatment in the 2 months before enrolment into the study, and if they were not able to read and write Dutch.
Participants with a strong preference for manual therapy intervention who did not want to be randomised were asked to participate in a parallel cohort study, which will be reported elsewhere.
Treatment allocation and blinding
After the baseline measurement, allocation was carried out by an independent administrative assistant who was not informed about the random sequence. The participants received a numbered and sealed envelope and opened the envelope in the presence of the administrative assistant. This assistant subsequently made an appointment for the first treatment session either with the participant’s GP or one of the participating manual therapists. Data entry and administration was carried out by an independent assistant.
InterventionsUsual care (UC) intervention. Participants were treated by their GP according to the Dutch general practice guideline for the management of headache. [8] According to this guideline, the GP provided information, re-assurance and advice, and discussed the benefits of life-style changes. If necessary, the GP prescribed analgesics or non-steroidal anti-inflammatory drugs (NSAIDs) or changed current pain medication. Twenty GPs provided this treatment on average in 2 or 3 visits.
Manual therapy (MT) intervention. MT treatment consisted of a combination of mobilisations of the cervical and thoracic spine, exercises and postural correction specifically chosen for the management of cervicogenic headache. [19]
In two meetings, four participating manual therapists were trained in the treatment protocol and received a treatment manual and booklets for the participants with home exercises. All four manual therapists were registered members of the national association of manual therapists. They had, on average, 10 years’ experience as manual therapist and completed an additional course on the mechanical diagnosis and management of disorders of the cervical spine provided by the McKenzie Institute.
The duration of each treatment session was 30 min with a maximum of nine treatments and included all three approaches: mobilisations, craniocervical muscle exercises and posture correction. At each session, the manual therapist decided, depending on the patient’s condition and outcomes, which type of techniques and exercises were selected from the protocol (Appendix).
Outcome assessment
At baseline, immediately after the treatment period (at 8 weeks), and at 26 weeks after randomisation, outcome assessments were carried out at the research clinic by an independent research assistant.Primary outcome measures. The frequency of days with headache in the past 2 weeks, and pain medication (number of doses of NSAIDs or simple analgesics) was registered by the participant in a headache diary. A 2-week registration period for tension-type headache was considered to be sufficient. [20] A 50% reduction in frequency of headache days was used to define a clinically relevant change. [17]
Secondary outcome measures
Headache pain intensity over the past 24 h was scored by the participant on an 11-point numerical rating scale (0 = no pain, 10 = most worse), which has been described as a valid, reliable and responsive instrument to measure pain. [21]
For the impact of headache on daily life, the Headache Disability Inventory (HDI) and the Headache Impact Test-6 (HIT-6) were used and completed by the participant. The HDI includes 25 questions on physical and emotional functioning with three possible response options: no = 0 points; sometimes = 2 points; yes = 4 points. A total score is computed by summating all scores, resulting in an individual HDI score ranging from 0 (no disability) to 100 (severe disability). A decrease in the total HDI of ≥16 points is considered to be a clinically significant improvement. The test–retest reliability of the total score has been shown to be adequate. [22]
The Headache Impact Test (HIT-6) consists of six items (pain intensity, social functioning, role functioning, vitality, cognitive functioning and psychological distress) each with five response options: never, 6 points; rarely, 8 points; sometimes, 10 points; very often, 11 points; always, 13 points, with a total score ranging from 36 to 78 points. Internal consistency (Cronbach alpha 0.89) and test–retest reliability (ICC ranging from 0.78 to 0.90) have been demonstrated to be good. [23] A decrease in HIT-6 change score of 2.3 points among patients with chronic daily headache reflects improvement in headache that is considered to be clinically significant. [24]
The active range of movement in flexion, extension, right and left rotation and right and left lateroflexion of the cervical spine with the participant in a seated position was measured by the research assistant with the CROM-device. The intra- and intertester reliability have been shown to be good (ICC >0.80). [25, 26]
Algometry on the trapezius descendens and the suboccipital muscle was performed by the research assistant with a Wagner FDK algometer with a 3.0 kg/cm pressure at four points at the left and right side: two points on the upper trapezius muscle and two points on the suboccipital muscle. Participants rated the severity of pain on a 0–10 point NRS scale (0 = no pain, 10 most severe pain). Scores for each pressure point were summated into a total score ranging between 0 and 80 points. Mechanical pressure algometry has been described by several authors as a valid and reliable measurement for pain pressure threshold for the trapezius muscle. [27–29]
Endurance of the neck flexor muscles was scored by the research assistant as the number of seconds the participant can raise his head from the table when lying on his/her back. This test has good to excellent intratester reliability (ICC 0.82–0.91) and moderate intertester reliability (ICC 0.67–0.78). [30]
Participants’ perceived improvement was reported on a 7-point scale. (0 = very much worse to 6 = very much better) at 8 and 26 weeks. A priori, a cut-off of 5 and 6 points (much better, very much better) was used to define recovery.
Sick leave (number of days) and additional use of healthcare resources (including consultation of a GP, psychologist, physiotherapist, or acupuncture) as reported by the participant were registered at 26 weeks follow-up. The registration of sick leave (number of days) was planned but not stated in the study-design article. [16]
As described in the study protocol, we aimed to detect a difference in reduction of headache frequency of at least 3 days (SD 5) between both groups. [16] To detect this difference with a one-sided significance level of 0.05, and power of 0.80 we had to include at least 35 participants in each treatment group. With a calculated loss to follow-up of participants in the trial of 15%, we aimed to enrol 42 participants with CTTH in each treatment group.
Statistical analysis
Baseline comparability was investigated by descriptive statistics to examine whether randomisation had been successful. Next, for each participant, the change between baseline and follow-up was calculated for all primary and secondary outcome measures. Between-group differences in improvement including 95% confidence intervals were calculated, and statistical significance of differences was tested using the Student t-test for continuous outcomes, and the χ2 -test for dichotomous outcomes (e.g. perceived recovery) using a two-sided significance level of 0.05. Non-parametric tests (Mann–Whitney) were conducted in case of non-normal distribution of outcome measures. The statistical analysis was performed according to the intention-to-treat principle and a complete case analysis was used without imputation of missing values given the low attrition rate.
In addition, a per-protocol analysis was performed, analysing only those participants with no serious protocol deviations (other treatment). Multivariable regression analysis was conducted to examine the potential influence of differences in baseline characteristics on outcome. Effect sizes were computed as the mean difference between groups over the pooled standard deviation. Effect sizes were rated as follows: small (0.2–0.5), medium (0.5–0.8) or large (>0.8). [31] For the primary outcome measure (headache frequency), we also calculated the difference in the proportion of participants reporting a 50% reduction in headache frequency, and the accompanying relative risk (RR) and number needed to treat (NNT) including 95% confidence intervals.
Finally, an exploratory subgroup analysis was carried out to explore differences in effects on primary outcome measures in participants with and without additional migraine.
Results
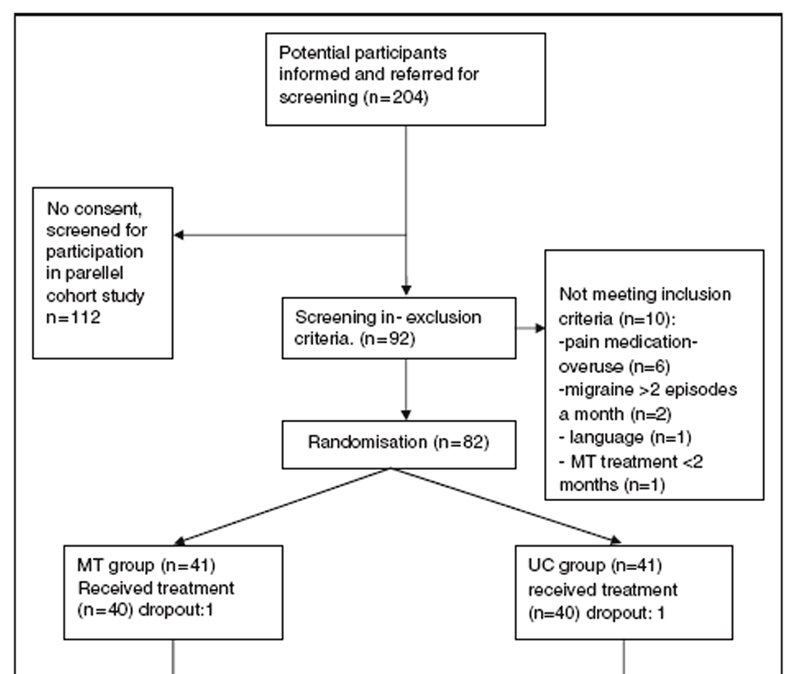
Figure 1

Table 1

Table 2 In the period between June 2007 and December 2008, 82 participants were enrolled and randomised; all follow-up measurements were completed in June 2009. In each group, 40 participants received treatment and seven participants (8.5%; 3 in the MT and 4 in the UC group) were lost to follow-up. Figure 1 summarises recruitment and retention of participants throughout the trial. Participants who were lost to follow-up showed similar baseline characteristics as those who completed the trial.
Baseline characteristics showed no large differences between intervention groups, although the UC group reported using a slightly higher number of doses of analgesics, had slightly higher HDI scores, lower cervical range of motion and higher algometry scores at baseline (Table 1). No adverse events were reported in both intervention groups.
Results at 8 weeksPrimary outcomes. Within and between group mean differences after the treatment period of 8 weeks are summarised in Table 2. There were significant differences in favour of the MT group for change in headache frequency (–6.4 days; 95%CI –8.3 to –4.6), duration of headache (–5.3 h, 95%CI –9.5 to –1.2) and headache intensity (–1.8, 95%CI –3.1 to –0.7). At 8 weeks, a 50% reduction of headache frequency was found in 87.5% (35/40) of the participants in the MT group and in 27.5% (11/40) in the UC group resulting in a RR of 3.2 (95%CI 1.9–5.3) and a NNT of 2 (CI 95% 1.3–2.2). The calculated effect size for the frequency of headache days was large at 1.6. Use of medication for NSAIDs and analgesics was categorised in three groups: decreased, no change or increased intake of tablets. Differences in use of medication were not significantly different between groups (chi squared test, P=0.22).
Secondary outcomes. Changes in results of disability measured by the HIT-6 (P<0.001) and HDI (P = 0.001) showed significant differences in favour of the MT group and effect sizes were large: 1.0 (HIT-6) and 0.8 (HDI). The same significant differences applied for physical tests including cervical range of motion (P = 0.023), algometry (P = 0.001) and endurance of the neck flexors (P = 0.011). The calculated effect sizes were rated as medium: 0.5 (cervical range of motion), 0.6 (algometry) and 0.6 (endurance neck flexors). In order to verify statistical testing in case of nonnormal distribution of the data, the independent Mann–Whitney test was used for the HDI and neck flexor endurance, but this did not result in different conclusions regarding statistical significance of findings. The mean number of manual therapy sessions was 6.6 (SD 1.7; range, 4–9).

Table 3 Results at 26 weeks
Primary outcomes. Within and between group mean differences at 26 weeks follow-up are summarised in Table 3. Between group differences were statistically significant for changes in headache frequency (–4.9 days, 95%CI –6.95 to –2.98) and pain intensity (–1.4, 95%CI –2.7 to –0.2) in favour of the MT group. The proportion of participants showing a 50% reduction in headache frequency was 81.6% (31/38) in the MT group and 40.5% (15/37) in the UC group at 26 weeks, resulting in a RR of 2.0 (95%CI 1.3–3.0) and a NNT of 3 (95%CI 1.6–4.8). The calculated effect size for headache frequency was large at 1.2.
Use of medication (decreased, no change, increased) showed no significant difference (P = 0.92) in intake of medication for analgesics and NSAIDs.
Secondary outcomes. The impact of headache on disability still showed differences in favour of the MT group at 26 weeks (see Table 3). Mean changes on the HIT-6 (–5.5, 95% CI –9.0 to –1.2) and HDI (–9.9, 95% CI –19.5 to –0.6) were significantly different, although the difference in the HDI was not significant (P=0.116) when using a non-parametric test. Effect sizes were of medium size: 0.6 (HIT-6) and 0.5 (HDI). For all physical tests, differences between groups at 26 weeks were smaller compared to those at 8 weeks and no longer statistically significant.

Table 4 Sick leave was registered at 26 weeks and showed a significant difference (P = 0.027) with 7.9% of the participants (n = 3) in the MT group and 32.4% (n = 12) in the UC group reporting at least one day of sick leave in the previous 6 months. The use of additional healthcare is specified in Table 4, showing that, in total, 13.2% (n = 5) of the participants in the MT group compared to 59.4% (n = 22) in the UC group reported use of additional care (P<0.001).
Additional analyses
Multivariable regression analyses showed only very small effects of differences in baseline values of the HDI, cervical range of motion and algometry on outcome. Therefore, we presented crude estimates in Tables 2 and 3. A subgroup analysis for CTTH participants with co-morbid migraine showed similar results for the primary outcome measures. The difference between intervention groups in change in headache frequency was –5.1 days (95% CI –9.2 to –1.1) for the subgroup with migraine, and –6.3 days (95%CI –8.5 to –4.2) for those without migraine. There was also no difference in the use of pain medication (data not shown). A per-protocol analysis was performed excluding two participants who received alternative treatment in the first 8 weeks but this revealed no differences compared with the intention to treat analysis.
Discussion
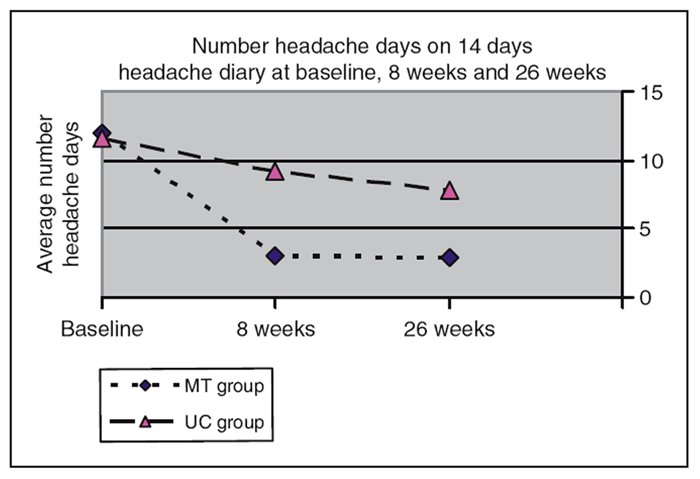
Figure 2 The results of this trial showed that manual therapy was effective for CTTH in reducing frequency (see Figure 2), intensity and impact of headache, both at short-term and long-term follow up. For frequency of headache, the effect size was large and the number needed to treat low. The use of medication did not show a significant difference between the groups. Differences between intervention groups for scores on cervical function (range of motion of the cervical spine, endurance of neck flexor muscle, algometry) were large and statistically significant in the short term, but the differences were smaller at 26 weeks and no longer significant.
While the large improvement at 8 weeks in scores on physical tests in the MT group was maintained at 26 weeks follow-up, the UC group showed additional improvement at 26 weeks. An explanation might be the (self-)referral for physiotherapy by 40% (15/37) of the participants in the UC group after the intervention period of whom seven received the same MT treatment as offered to the participants randomised to MT described for this trial. This group of participants showed larger improvements in frequency of headache days at 26 weeks than participants who did not received additional treatment (data not shown).
Use of medication did not significantly decrease in both groups, which may be explained by the large number of patients who did not use medication at baseline (see Table 1). This resulted in a large proportion of participants with no change in analgesic use during the trial (>40% in both groups at both time points) or in the use of NSAIDs (more than 60%). Additional medication (amiltryptiline) was prescribed for two patients and this restricted prescription of prophylactic medication reflects the recommendation of the Dutch GP guideline.
The impact of headache as measured by psychosocial and functional disability scores on the HIT-6 showed a significant difference in mean change scores at 8 weeks and 26 weeks in favour of the MT group. The between-group score on the HDI was significantly different at 8 weeks although non-parametric testing did not show a significant difference at 26 weeks. CTTH may be associated with considerable limitations in psychosocial functioning. Therefore, questionnaires on headache impact or disability are strongly encouraged to monitor progress in research and clinical settings. [17] However, additional research is necessary to produce explicit criteria for a minimal important change on the HIT-6 and HDI that are suitable for CTTH patients in primary care. We used criteria that have been defined based on secondary care populations, and these may not hold in patients encountered in primary care.
The substantial economic burden associated with the direct and indirect costs of tension type headache demands a cost-effective treatment. [32] Because of the reduced use of additional healthcare and sick leave, the manual therapy intervention in this trial offers a promising intervention to be tested in future cost-effectiveness studies.
Overestimation of symptom burden upon entering the trial may be a possible explanation for the beneficial outcomes for headache frequency. The large improvement may also be partly explained by regression to the mean of symptoms in the MT group and the UC group.Participants go to the doctor at a time of severe symptoms; thus, reduction in the first weeks could partly reflect natural recovery of the problem. Regression to the mean may also have played a role since we selected participants with a minimal frequency of headache of at least 15 days per month. These factors will explain part of the within-group changes, but do not explain the difference between groups.
The manual therapy intervention used in this trial was based on the theory that improvement of craniocervical musculoskeletal function with mobilisation, active stabilisation of the cervical spine and postural correction would have a positive effect on the inhibitory systems at various levels in the spinal cord and would modulate pain perception and decrease sensitisation. Further analysis of the data is necessary to clarify the relations between changes on physical functioning, headache frequency and pain intensity.
Our trial supports the earlier favourable results of a similar approach for tension-type headache by van Ettekoven et al. [33] In that trial, a standardised physical therapy intervention was compared to an intervention including the same physical therapy accompanied by a craniocervical training programme. Subgroup analysis of a group of 42 patients with CTTH showed a significant reduction in headache frequency and intensity in favour of the additional craniocervical programme after treatment and at 26-week follow-up. To what extent the individual elements of the MT treatment protocol, particularly manipulation (high-velocity techniques) in our trial contributed to the beneficial outcomes remains unclear and could be studied in an experimental design in which exercises are compared to exercises in combination with manipulation.
Our trial was only of moderate sample size. Replications of this trial with larger sample sizes are needed to confirm the promising and beneficial results of mobilisation, training and posture correction of the cervical spine for CTTH and explore their generalisability to other settings and other populations.
The strengths of our trial include a successful blinding of the research assistant to treatment allocation and a limited loss to follow-up of 8.5% (n = 7). Critical comments can be made on the procedures used to include participants with CTTH, the absence of blinding of treatment and the time spent on treatment in our trial. All participants were screened by the GP and not by a neurologist, which may have weakened the validity of the diagnosis of CTTH. This approach, however, increases the external validity of this trial, as in primary care in The Netherlands as well as in several other countries the diagnosis of tension-type headache is made by a primary care physician, in most cases without referral for a specialist opinion.
As we have argued before, it is not possible to blind participants, manual therapists and GP for treatment in a pragmatic trial. [16] Preferences and expectations of participants and practitioners may affect adherence to treatment and may influence participants’ reported outcomes. To verify the influence of expectations and adherence to treatment, all participants rated their expectations for treatment before randomisation and we included questions regarding adherence to treatment after 26 weeks. Although there were no significant differences of these ratings between both groups we still cannot exclude an effect of treatment preference on the outcome of this trial.
Conclusions
We performed a pragmatic, randomised clinical trial to evaluate the effect of manual therapy compared to usual care by the general practitioner. Based on this trial, we conclude that manual therapy provides an effective intervention for patients with chronic tension-type headache (CTTH) and, thereby, an effective option for referral for the general practitioner.
AppendixThe first goal of treatment was mobilisation of the cervical spine in flexion, extension, retraction and left and right rotation. Spinal mobilisation consisted of low and/or high-velocity cervical and upper-thoracic joint mobilisation and manipulation techniques. The treatment protocol described the therapeutic procedures and home exercises for mobilisation of the cervical and upper thoracic spine. In this protocol, all mobilisations started with active mobilisation (hands-off techniques) and, if necessary, the manual therapist proceeded with passive mobilisations (hands-on techniques). In addition to mobilisation techniques, soft tissue techniques (muscle stretching, deep muscle frictions) could be used to reduce cervical muscular tension and pain.
Second goal of treatment was training of the endurance of the craniocervical muscles and this training consisted of low-load craniocervical muscle endurance exercises as described by G. Jull with a stabiliser (19). In case a stabiliser could not be used, the participants were instructed, while lying on their back in a horizontal position, to pull their chin in (atlanto-occipital cervical flexion) and hold this position (isometric contraction) for 10–20 s. In combination with retraction of the cervical spine, this exercise was also instructed in a sitting position and participants were asked to perform these exercises at least two times a day.
Third goal of treatment was postural correction of the cervical and thoracic spine. Instructions were given to correct the position of the thoracic and cervical spine and the manual therapists underlined the importance of this posture correction. The participant was placed in a sitting position with correction or support of the lumbar spine (upright sitting position). In this position, the manual therapist instructed the participant to straighten the thoracic spine with a simultaneously retraction of the cervical spine. The craniocervical muscle endurance exercises were incorporated in exercises of postural correction in sitting and standing position. Besides these posture correction, all participants were given advice about their work place, especially to those who performed sedentary work several hours a day.
All participants received a booklet with home exercises, which included a full description of all exercises, and written instructions by the manual therapist on type, frequency and duration of the exercises. After the treatment period, participants were encouraged to continue their exercises focusing on retraction of the cervical spine and posture correction.
References:
Stovner LJ, Hagen K, Jensen R, et al.
The global burden of headache: a documentation of headache prevalence, disability worldwide.
Cephalalgia 2007; 27: 193–210.Rasmussen BK.
Epidemiology of headache.
Cephalalgia 2001; 21: 774–777.Jensen R.
Diagnosis, epidemiology and impact of tension-type headache.
Curr Pain Headache Rep 2003; 7: 455–459.Zwart AJ, Dyb G, Hagen K, Svebak S, Stovner LJ and Holmen J.
Analgesic overuse among subjects with headache, neck, and low-back pain.
Neurology 2004; 62: 1540–1544.Coeytaux R and Linville J.
Chronic daily headache in a primary care population: prevalence and headache impact test scores.
Headache 2007; 47: 7–12.Vinding GR, Zeeberg P, Lyngberg A, Nielsen RT and Jensen R.
The burden of headache in a patient population from a specialized headache centre.
Cephalalgia 2007; 27: 263–270.Fernandez-de-las Penas C and Schoenen J.
Chronic tension-type headache: what is new?
Curr Opin Neurol 2009; 22: 254–261.Knuistingh Neven A, Bartelink MEL, de Jungh TOH, et al.
NHG standaard Hoofdpijn.
Huisarts en Wetenschap 2004; 46: 411–422
http://nhg.artsennet.nl/ upload/104/standaarden/M19/start.htmFumal A and Schoenen J.
Tension-type headache: current research and clinical management.
Lancet Neurol 2008; 7: 70–83.Fernandez-de-las-Penas C, Alonso-Blanco C, Luz Cuadrado M.
Trigger points in the suboccipital muscles and forward head posture in tension-type headache.
Headache 2006; 46: 454–460.Fernandez-de-las-Penas C, Luz Cuadrado M, Gerwin RD and Pareja JA.
Myofascial trigger points and headache clinical parameters in chronic tension-type headache.
Headache 2006; 46: 1264–1272.Fernandez-de-las-Penas C, Luz Cuadrado M, Arendt-Nielsen L.
Increased pericranial tenderness, decreased pressure pain threshold, and headache clinical parameters in chronic tension-type headache patients.
Clin J Pain 2007; 23: 346–352.Ferna´ ndez-de-las-Pen˜ as C, Alonso-Blanco C, Cuadrado ML and Pareja JA.
Forward head posture and neck mobility in chronic tension-type headache: a blinded, controlled study.
Cephalalgia 2006; 26: 314–319.Fernandez-de-las-Penas C, Alonso-Blanco C, Luz Cuadrado M, Miangolarra JC.
Are manual therapies effective in reducing pain from tension-type headache? A systematic review.
Clin J Pain 2006; 22: 278–285.Lenssinck M, Damen L, Verhagen AP, Berger M, Passchier J and Koes B.
The effectiveness of physiotherapy and manipulation in patients with tension-type headache: a systematic review.
Pain 2004; 112: 381–388.Castien RF, van der Windt DAWM, Dekker J, Mutsaers B and Grooten A.
Effectiveness of manual therapy compared to usual care by the general practitioner for chronic tension-type headache: design of a randomised clinical trial.
BMC Musculoskel Disord 2009; 10: 21.Andrasik F, Lipchik GL, McCrory DC and Wittrock DA.
Outcome measurement in behavioral headache research: headache parameters and psychosocial outcomes.
Headache 2005; 45: 429–437.International Headache Society.
The International Classification of Headache Disorders, 2nd edition.
Cephalalgia 2004; 24(Suppl 1): 9–160.Jull GA.
Management of cervical headache.
Man Ther 1997; 2: 182–190.Blanchard EB, Hillhouse J, Appelbaum KA and Jaccard J.
What is an adequate length of baseline in research and clinical practice with chronic headache?
Biofeedback Self Regul 1987; 12: 323–329.Williamson A and Hoggart B.
Pain: a review of three commonly used pain rating scales.
J Clin Nurs 2005; 14: 798–804.Jacobson GP, Ramadan NM, Norris L and Newman CW.
Headache Disability Inventory (HDI): short-term test–retest reliability and spouse perceptions.
Headache 1995; 35: 534–539.Kosinski M, Bayliss MS, Bjorner JB, et al.
A Six-item Short-form Survey for
Measuring Headache Impact:
The HIT-6
Quality of Life Research 2003 (Dec); 12 (8): 963–794Coeytaux R, Kaufman J, Chao R, Mann J and DeVellis R.
Four methods of estimating the minimal important difference score were compared to establish a clinically significant change in Headache Impact Test.
J Clin Epidemiol 2006; 59: 374–380.Tousignant M, Smeesters C, Breton AM, Breton E and Corriveau H.
Criterion validity study of the cervical range of motion (CROM) device for rotational range of motion on healthy adults.
J Orthop Sports Phys Ther 2006; 36: 242–248.de Koning C, van den Heuvel S, Staal B, Smits-Engelsman B and Hendriks E.
Clinimetric evaluation of active range of motion measures in patients with nonspecific neck pain: a systematic review.
Eur Spine J 2008; 17: 905–921.Fischer AA.
Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold.
Pain 1987; 30: 115–126.Nussbaum E and Downes L.
Reliability of clinical pressure pain algometric measurements obtained on consecutive days.
Phys Ther 1998; 78: 160–169.Antonaci F, Sand T and Lucas GA.
Pressure algometry in healthy subjects: interexaminer variability.
Scand J Rehabil Med 1998; 30: 3–8.Harris KD, Heer DM, Roy TC, et al.
Reliability of a measurement of neck flexor muscle endurance.
Phys Ther 2005; 85: 1349–1355.Cohen J.
Statistical power analysis for the behavioral sciences, 2nd edition.
Hillsdale, NJ: Lawrence Erlbaum, 1988.Jensen R and Stovner LJ.
Epidemiology and comorbidity of headache.
Lancet Neurol 2008; 7: 354–361.van Ettekoven H and Lucas C.
Efficacy of physiotherapy including a craniocervical training programme for tension-type headache; a randomized clinical trial.
Cephalalgia 2006; 26: 983–991.
Return to CHRONIC TENSION HEADACHE
Return to INITIAL PROVIDER/FIRST CONTACT
Since 8–09–2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |