

Prevalence of Headache and Migraine in Children
and Adolescents: A Systematic Review
of Population-based StudiesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Dev Med Child Neurol 2010 (Dec); 52 (12): 10881097 ~ FULL TEXT
OPEN ACCESS Ishaq Abu-Arafeh Sheik Razak Baskaran Sivaraman Catriona Graham
Fraser of Allander Neurosciences Unit,
Royal Hospital for Sick Children,
Glasgow, UK.
Aim: The aim of this study was to review systematically the prevalence of headache and migraine in children and adolescents and to study the influence of sex, age, and region of residence on the epidemiology.
Method: we systematically searched the literature in electronic databases to cover the period between 1 January 1990 and 31 December 2007. We assessed and included population-based studies on epidemiology of headache and migraine in children and adolescents if they fulfilled the following criteria: (1) reporting on unselected childhood population; (2) reliable methods of data collection using a questionnaire or face-to-face interviews; (3) using the International Headache Society's (IHS) criteria (1988 or 2004) for the diagnosis of migraine; and (4) provision of sufficient and explicit data for analysis. We used Excel, Stata, and Confidence Interval Analysis software.
Results: we identified and analysed 50 population-based studies reporting the prevalence of headache and/or migraine in children and adolescents (<20y). The estimated prevalence of headache over periods between 1 month and lifetime in children and adolescents is 58.4% (95% confidence interval [CI] 58.158.8). Females are more likely to have headache than males (odds ratio [OR] 1.53, 95% CI 1.481.6). The prevalence of migraine over periods between 6 months and lifetime is 7.7% (95% CI 7.67.8). Females are more likely than males to have migraine (OR 1.67, 95% CI 1.601.75). Regional differences in prevalence of migraine, though statistically significant, may not be of clinical significance. The change in the IHS's criteria for the diagnosis of migraine was not associated with any significant change in the prevalence of migraine.
Interpretation: this study confirms the global high prevalence of headache and migraine in children and adolescents. Sex, age, and regional differences are evident.
What this paper adds
It allows better understanding of the epidemiology of headache and migraine in children and adolescents.
It quantifies the effects of sex, age, and regional influences on the prevalence of headache in children over variable periods of time.
It assesses the influence of different diagnostic criteria on the prevalence of migraine.
To our knowledge, no similar study has been published.
From the FULL TEXT Article:
Background
Childhood headache has an important adverse impact on the child and the family, as shown in many studies, including a recent review. [1] Therefore an accurate estimate of the true prevalence derived from all published world literature will help in assessing the magnitude of the problem, streamlining resources in improvement of diagnosis and treatment, and reducing its burden.
The prevalence of childhood headache and migraine has been reported from across the world with widely variable estimates of prevalence. Since the publication of the International Headache Societys (IHS) Classification and Diagnosis of Headache Disorders [2] in 1988 and the second edition of the International Classification of Headache Disorders [3] in 2004 (ICHD-II), there have been several published studies that share common methods and criteria for the diagnosis of migraine. These allow a systematic review of the world literature, despite some inevitable minor variations in methods such as the use of a questionnaire, face-to-face interviews, or both in collecting data, point-in-time prevalence, and reporting on different age groups within the childhood population. A degree of heterogeneity is, therefore, an inherent feature of such analysis and is addressed in this study by maintaining its focus on a few questions relating to prevalence. The large number of children and adolescents in the studies is likely to minimize the effects of such minor differences.
Method
A protocol for this study was developed by paediatricians with interest in headache epidemiology and supported by a statistician. A quantitative summary of published data as described by Blattner et al. [4] is considered an appropriate method for analysing the epidemiology of headache and migraine in children. We based our data collection, analysis, and reporting on the methods and style of Cochrane databases, and in keeping with the preferred reporting items for systemic reviews and meta-analysis: the PRISMA statement. [5]
Literature search
We searched the literature on the epidemiology of headache and migraine in children using PubMed. We used the search command (prevalence or epidemiology) and (headache or migraine) and (children or adolescents) for publications between 1 January 1990 and 31 December 2007. We also searched Cochrane databases, Embase, and Google Scholar, and cross-referenced recent review articles on childhood headache and migraine.
Quality assessment and inclusion criteria
We assessed each paper to eliminate any selection bias. A strict adherence to the inclusion criteria with the focus on the research methods, but not the results, was followed. The first three authors agreed after reading all the papers, independently, on their validity for inclusion. Studies were included if they fulfilled the following criteria. (1) Population-based studies of randomly selected participants published between 1 January 1990 and 31 December 2007. The starting date was based on the fact that no population-based studies were published before this date that used the 1988 IHSs criteria for the diagnosis of migraine. The year 2007 was the last full year before the beginning of our work on this project. (2) Reporting on a population of children and adolescents. Studies reporting on populations under 20 years of age were included to maximize the inclusion of relevant studies. (3) Descriptive data were available or easily reproducible from the original article. (4) The diagnosis of migraine was based on the IHS criteria and classification of 1988 or 2004. (5) Clear description of the methods of data collection such as the use of a questionnaire, face-to-face interview, and examination were provided. (6) Appropriate statistical methods were used for analysis. Corresponding authors were contacted for clarifications if an ambiguity was detected but could not be resolved.
Collection of data
From each study we collected data on the year of publication, sample size, number of participants with effects and the prevalence of headache and/or migraine, the geographical origin of the study, the methods of assessment of headache and migraine, age range of the participants, and prevalence by sex. The data were tabulated for ease of comparison, analysis and to show similarities as well as differences (heterogeneity). Analysis of the prevalence of migraine with and without aura was not possible in these studies and is not presented here.
Publication bias
We tested for publication bias by using the informal funnel graph as recommended by Begg and Berlin. [6]
Assessment of heterogeneity and subgroup analysis
Differences between studies were explored to identify heterogeneity.
These included the following areas.(1) The reported prevalence of headache and migraine over different periods of time, ranging from 1 month to lifetime, was investigated. It is feasible that these variables may constitute major differences and may provide heterogeneous data. Therefore we comparatively assessed the prevalence of headache and migraine in studies reporting over a short period (<6mo) with prevalence in those reporting over a long period (at least 6mo).
(2) Differences in prevalence between age groups were explored. We assessed the prevalence of migraine in young children (<14y) compared with that in all children and adolescents up to the age of 20 years.
(3) The role of the diagnostic criteria on the prevalence of migraine was also explored. We separately analysed the prevalence of migraine in studies using the IHS criteria for the diagnosis of migraine (1988) and in those using the ICHD-II.
(4) We also investigated and compared the possible influences of racial or geographical origin.Statistical analysis
We show the raw data in tables and our assessments in figures. Heterogeneity between studies for point-in-time prevalence, method of data collection, and age range of childhood populations are included. We used Confidence Interval Analysis software (published by the British Medical Journal Publishing Group [7]) and analysed the differences between the percentages by a χ2 test. We also used Excel and Stata for the odds ratio (OR) with 95% confidence intervals (CIs) where appropriate. Analysis included graphic data summary and Forest Plot. [8, 9]
Results
The search of PubMed, Google Scholar, Cochrane databases, and Embase produced 258 articles. PubMed produced most of the papers except for five articles identified by Google Scholar. It was possible to exclude 213 articles: 40 were review articles, 21 clinic series, 28 prevalence studies on adult populations, 38 on headache diagnosis or the prevalence of headache among specific patients groups, 21 on headache treatment, nine on genetics of headache, nine on chronic daily headache, 12 on the prognosis of headache, one case report, and 34 on headache comorbidities. Only 50 articles were found to fulfil the search criteria for population-based studies of headache and/or migraine in childhood.

Table 1+2
page 2
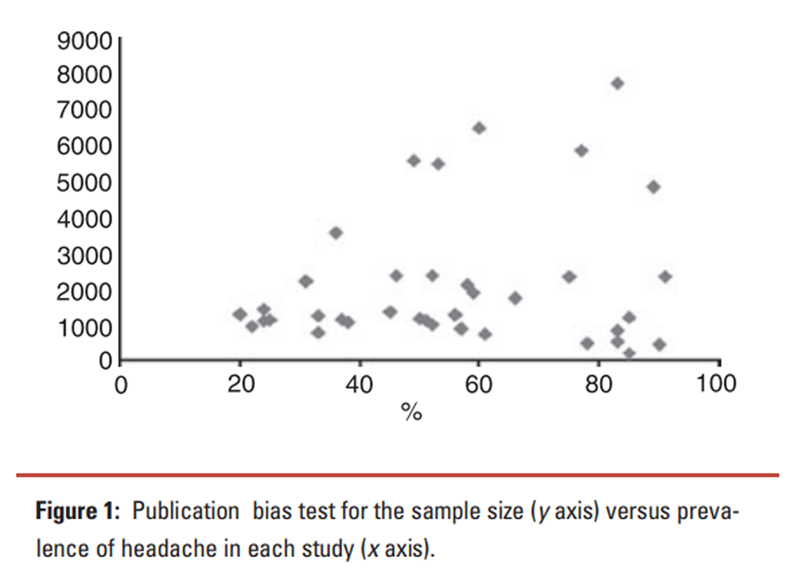
Figure 1
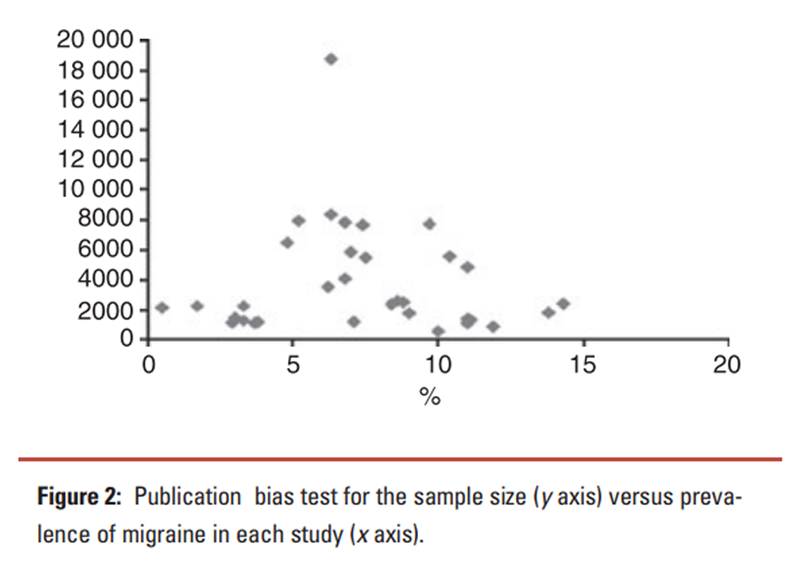
Figure 2

Figure 36
page 5

Table 3

Table 4

Table 5 We summarize the findings of each study in Tables I and II, showing year of publication, country of origin, number of participants in the study population, number of cases, methods of data collection, diagnostic criteria of migraine, prevalence, and sex differences if applicable.
Publication bias
The informal funnel graph, as recommended by Begg and Berlin,6 shows the typical pyramid-shaped graph with tapering for prevalence of headache (Figure 1) and migraine (Figure 2).
Prevalence of headache
Thirty-seven population-based studies (Table I) provided 38 sets of data and reported on the prevalence of headache in children under the age of 20 years. [1012, 1459] All studies collected information from unselected childhood populations using a questionnaire with or without an interview and examination. Prevalence of headache was reported for children complaining of headache occurring over lifetime or the past 12, 6, 3, or 1 month; however, in nine studies no reference was made to the period of time. The reported prevalence of headache and the calculated 95% CIs in all studies are shown in Figure 3 and demonstrate the variability in prevalence among studies. The overall calculated prevalence of headache (at any point in time) in a total population of 80 876 children is 58.4% with a narrower 95% CI (58.158.8%).
Twenty-two studies provided the sex-specific prevalence of headache. Meta-analysis of the sex differences in prevalence of headache using Stata to calculate OR and the 95% CI is shown in Figure 4. The OR for prevalence of headache in females compared with males is 1.53 (1.481.60).
Prevalence of migraine
Thirty-five studies (Table II) provided 37 sets of data of the prevalence of migraine in people under the age of 20 years. The diagnosis of migraine was made on the application of the IHSs criteria of 1988 or the ICHD-II. [2, 3] Two studies used revised criteria. The reported prevalence figures of migraine over a minimum period of 3 months (and 95% CIs) are shown in Figure 5. The cumulative analysis showed the overall prevalence of migraine in children and adolescents is 7.7% (95% CI 7.67.8).
Subgroup analysisRole of sex on prevalence of migraine Twenty-eight population-based studies provided data on the prevalence of migraine among males. Twenty-nine studies provided data on the prevalence of migraine in females (one study reported on females only). The overall prevalence of migraine in female children and adolescents is 9.7% (95% CI 9.49.9) and in males 6.0% (95% CI 5.86.2); the difference is 3.7% (95% CI 3.43.9, p<0.001). Meta-analysis of the OR for prevalence of migraine in females, as shown in Figure 6, gives a value of 1.67 (95% CI 1.601.75).
Role of age on prevalence of migraine Table III shows the population studies reporting prevalence of migraine in children (≤14y). The prevalence of migraine among females is 7.0% (95% CI 6.77.4), which is significantly lower than the prevalence of migraine in all females under the age of 20 years, which is 9.7%; the difference is 2.7% (95% CI for difference 2.52.9, p<0.001). Similarly the prevalence of migraine in males of 14 years of age or under is 4.7% compared with 6.0% in males of all ages under 20 years (95% CI 5.86.2); the difference is 2.3% (p<0.01).
Role of diagnostic criteria on the prevalence of migraine Twenty-one studies used the 1988 IHS criteria, giving a total number of children of 68 954 and a prevalence of 7.5% (95% CI 7.37.7). Eleven studies used the ICHD-II of 2004, giving a total number of children of 64 985 and a prevalence of 7.8% (95% CI 7.68.0). The difference in prevalence between the two sets of criteria is not statistically significant, although it may be of clinical value for individual patients.
Role of geographical background on prevalence of migraine The prevalence of migraine by geographical region is illustrated in Table IV. There is evidence of a statistically significant difference ( χ2=173.12, degrees of freedom=3, p<0.001). It is not possible to assess the role of any possible racial influences on the prevalence of migraine from the information given in the studies.
Point-in-time prevalence of migraine No evidence of a significant difference was noted between studies that reported on prevalence of migraine or headache over long periods of time (at least 6mo or no report on the time period) compared with the overall prevalence (Table V).
Discussion
Study methods
The use of published literature is unlikely to carry any selection bias as most papers presented at meetings and conferences were subsequently published in full and are included. It is not possible to assess the quality of methods and data in studies that were neither published nor presented.
We realize the difficulties that are inherent with systemic reviews and meta-analyses of published literature, especially when some or all of the epidemiological studies are observational in nature and may have disparate results, as described by Greenland. [9] We therefore identified and managed the differences between studies as appropriate and performed subgroup analysis, capturing as much homogeneity among the subgroups as possible by assessing one variable at a time.
The prevalence figures in the pooled data, though, produced narrow 95% CIs that should be read with caution as they should not hide the differences in the individual studies. Despite these limitations of our data, it is still possible to make reasonable conclusions about the appropriateness of the methods we used, particularly the inclusion of the whole age spectrum of children and adolescents up to 20 years.
Also, the heterogeneity of the studies in reporting prevalence against different points in time may seem a significant difference. However, the high frequency of headache and migraine, as shown in several population-based studies, has minimized any such differences and proved of little consequence in the overall analysis.
Similarly, the use of the first or second editions of the IHS criteria for the diagnosis of migraine are shown in our analysis to be of some effect, but probably of no clinical significance on the prevalence of migraine, for which subgroup analysis has proved a very useful tool.
Pooled grouping has also provided data on specific population characteristics. The validity of our study and the analysis of the data were assessed against the checklist of items as suggested by a recent publication on research methods and reporting. [5] Analysis for publication bias using the informal graphic method was reassuring and conforms to accepted recommendations. [6]
Prevalence of headache
Despite the wide differences in the reported prevalence of headache in different studies in children and adolescents, a clear and reliable estimate of the magnitude of the problem has emerged. This analysis shows that around 60% of children are prone to headache, over periods varying from 3 months to lifetime, and may have attacks of variable frequency. It does not mean that 60% of children have headache at any given point in time. Such a high prevalence may not surprise many researchers and clinicians, but it confirms the high prevalence of headache in children. This result will help public health planners and doctors treating children to understand better the extent of the condition. Our review also shows that headache is significantly more common in females (67%) than in males (58%), and that headache is common across the age range and across the world.
Prevalence of migraine
Similarly, we confirm that migraine is a common disorder: approximately 8% of children and adolescents are prone to it over at least a 3month period. We have also shown that migraine is more common in older children over the age of 14 years. The prevalence of migraine in our systematic review should be viewed as a minimum estimate as it was not possible to adjust for non-responders to questionnaires in some studies and those who did not attend interviews. Experience from one study that adjusted for these variables showed an increase from the actual to the estimated prevalence by a factor of 1.17 (Abu-Arafeh and Russell [13]).
The only difference between the IHSs diagnostic criteria of migraine of 1988 and those of ICHD-II of 2004 is the reduction in the duration of migraine attacks from a minimum of 2 to 1 hour. This change is clinically important in making the diagnosis of migraine in individual patients, but it does not seem to have made a significant difference in the calculation of migraine prevalence in children and adolescents.
This review shows clear and statistically significant differences in the prevalence of migraine between Europe and the Middle East on the one hand and the USA and the Far East on the other. The differences are probably a combination of genetic predisposition as well as environmental factors. Despite the clear differences in migraine prevalence in different regions of the world, it is not possible to assume that the differences are due to racial background as most studies did not provide data on the racial makeup of their populations.
Conclusion
Headache is common across the world, with about 60% of children and adolescents being prone to it over at least a 3month period. Migraine is also common, and despite small variations in reporting across the world it is safe to state that around 8% of children and adolescents suffer from it over periods ranging from 3?months to lifetime. This analysis confirms the frequently reported observation of a significantly lower prevalence of migraine in children under the age of 14?years than in the general childhood population. Small regional and possibly interracial differences in its prevalence are also evident. Migraine affects males and females equally at a young age (<14y), and more females than males in adolescence and young adulthood.
Abbreviations
IHS = International Headache Society
CI = Confidence Interval
ICHD-II = International Classification of Headache Disorders, second edition
OR = Odds Ratio
References:
Kernick D, Campbell J.
Measuring the impact of headache in children:
a critical review of the literature.
Cephalalgia 2008; 29: 316.Classification Committee of the International Headache Society.
Classification and diagnostic criteria for headache disorders,
cranial neuralgias and facial pain.
Cephalalgia 1988; 8(Suppl. 7): 196.Headache Classification Subcommittee of the International Headache Society.
The International classification of headache disorders. 2nd edn.
Cephalalgia 2004; 24(Suppl. 1): 152.Blattner M, Sauerbrei W, Schlehofer B, Scheuchenpflug T, Friedenreich C.
Traditional reviews, meta-analysis and pooled analysis in epidemiology.
Int J Epidemiol 1999; 28: 19.Moher D, Liberati A, Tetzlaff J, Altman DG.
Preferred reporting items for systemic reviews and meta-analysis:
the PRISMA statement.
BMJ 2009; 339: 3326.Begg CB, Berlin JA.
Publication bias: a problem in interpreting medical data.
J R Stat Soc 1988; 151: 41963.Gardner MJ, Altman DG.
Confidence Interval Analysis v 1.0,
Statistics with Confidence.
London: British Medical Journal Publishing Group, 1989.Greenland S.
Invited commentary: a critical look at some popular meta-analysis methods.
Am J Epidemiol 1994; 140: 2906.Greenland S.
Can meta-analysis be salvaged?
Am J Epidemiol 1994; 140: 7837.King NJ, Sharpley CF.
Headache activity in children and adolescents.
J Paediatr Child Health 1990; 26: 504.Mortimer MJ, Kay J, Jaron A.
Epidemiology of headache and childhood migraine in an urban
general practice using ad hoc, Vahlquist and IHS criteria.
Dev Med Child Neurol 1992; 34: 1095101.Kristja΄nsdo΄ttir G, Wahlberg V.
Sociodemographic differences in the prevalence of
self-reported headache in Icelandic school-children.
Headache 1993; 33: 37680.Abu-Arafeh I, Russell G.
Prevalence of headache and migraine in schoolchildren.
BMJ 1994; 309: 7659.Pothmann R, Frankenberg SV, Muller B, Sartory G, Hellmeier W.
Epidemiology of headache in children and adolescents:
evidence of high prevalence of migraine among girls under 10 years.
Int J Behav Med 1994; 1: 7689.Raieli V, Raimondo D, Cammalleri R, Camarda R.
Migraine headaches in adolescents:
a student population-based study in Monreale.
Cephalalgia 1995; 15: 512.Barea LM, Tannhauser M, Rotta NT.
An epidemiological study of headache among children
and adolescents of southern Brazil.
Cephalalgia 1996; 16: 5459.Carlsson J.
Prevalence of headache in schoolchildren: relation to family and school factors.
Acta Paediatr 1996; 85: 6926.Antoniuk S, Kozak MF, Michelon L, Montemor NettoMR.
Prevalence of headache in children of a school from Curitiba,
Brazil, comparing data obtained from children and parents.
Arq Neuropsiquiatr 1998; 56: 72633.Aromaa M, Sillanpaa ML, Rautava P, Helenius H.
Childhood headache at school entry: a clinical study.
Neurology 1998; 50: 172936.Bener A, Swadi H, Qassimi EM, Uduman S.
Prevalence of headache and migraine in schoolchildren
in the United Arab Emirates.
Ann Saudi Med 1998; 18: 5224.Metsahonkala L, Sillanpa¨a¨ M, Tuominen J.
Social environment and headache in 8- to 9-year-old children:
a follow-up study.
Headache 1998; 38: 2228.Anttila P, Metsahonkala L, Sillanpaa M.
School start and occurrence of headache.
Pediatrics 1999; 103: e80.Krasnik A.
Headache in the population of school children in Poznan.
Neurol Neurochir Pol 1999; 33 (Suppl. 5): 1115.Bendell-Hockstra IE, Abu-Saad HH, Passchier J, Frederiks CM.
Prevalence and characteristics of headache in Dutch schoolchildren.
Eur J Pain 2001; 5: 14553.Al Jumah M, Awada A, Al Azzam S.
Headache syndromes amongst schoolchildren in Riyadh, Saudi Arabia.
Headache 2002; 42: 2816.Fichtel A, Larsson B.
Psychological impact of headache and co-morbidity with
other pains among Swedish school adolescents.
Headache 2002; 42: 76675.Ho K-H, Ong BK-C.
A community-based study of headache diagnosis and prevalence in Singapore.
Cephalalgia 2003; 23: 613.Shivpuri D, Rajesh MS, Jain D.
Prevalence and characteristics of migraine among adolescents:
a questionnaire survey.
Indian Pediatr 2003; 7: 6659.Laurell K, Larsson B, Eeg-Olofsson O.
Prevalence of headache in Swedish schoolchildren,
with a focus on tension-type headache.
Cephalalgia 2004; 24: 3808.Zwart JA, Dyb G, Holmen TL, Stovner LJ, Sand T.
The prevalence of migraine and tension headaches among adolescents
in Norway. The Nord-Trondlag Health Study (HeadHUNT-Youth),
a large population-based epidemiological study.
Cephalalgia 2004; 14: 3739.Bessisso MS, Bener A, Elsaid MF, Al-Khalaf FA, Huzaima KA.
Pattern of headache in school children in the State of Qatar.
Saudi Med J 2005; 26: 56670.Bugdayci R, Ozge A, Sasmaz T, et al.
Prevalence and factors affecting headache in Turkish schoolchildren.
Pediatr Int 2005; 47: 31622.Roth-Isigkeit A, Thyen U, Stoven H, Schwarzenberger J, Schmucker P.
Pain among children and adolescents in daily living and triggering factors.
Pediatrics 2005; 115: e15262.Alawneh HF, Bataineh HA.
Prevalence of headache and migraine among school children in Jordan.
Sudan J Public Health 2006; 1: 28991.Ayatollahi SM, Khorsavi A.
Prevalence of migraine and tension-type headache
in primary-school children in Shiraz.
East Mediterr Health J 2006; 17: 80917.Karli N, Aki N, Zarifoglu M, et al.
Headache prevalence in adolescents aged 12 to 17:
a student-based epidemiological study in Bursa.
Headache 2006; 46: 64955.Lundqvist C, Clench-Aas J, Hofoss D, Bartonova A.
Self-reported headache in schoolchildren:
parents underestimate their childrens headaches.
Acta Paediatr 2006; 95: 9406.Siddiqui SJ, Shamin SMS, Hashemi AM.
Prevalence and patterns of headache in school children in Karachi.
J Pak Med Assoc 2006; 56: 2157.van Dijk A, McGrath PA, Pickett W, VanDenKerkhof EG.
Pain prevalence in nine- to 13-year-old schoolchildren.
Pain Res Manag 2006; 11: 23440.Akyol A, Kiylioglu N, Aydin I, et al.
Epidemiology and clinical characteristics of migraine
among school children in the Menderes region.
Cephalalgia 2007; 27: 7817.Brun Sundblad GM, Saartok T, Engstrom LM.
Prevalence and co-occurrence of self-rated pain and perceived
health in school-children: age and gender differences.
Eur J Pain 2007; 11: 17180.Kroner-Herwig B, Heinrich M, Morris L.
Headache in German children and adolescents:
a population-based epidemiological study.
Cephalalgia 2007; 27: 51927.Isik U, Ersu RH, Ay P, et al.
Prevalence of headache and its association with sleep disorders in children.
Pediatr Neurol 2007; 36: 14651.Milovanovic M, Jarebinski M, Martinovic Z.
Prevalence of primary headaches in children from Belgrade, Serbia.
Eur J Paediatr Neurol 2007; 11: 13641.Unalp A, Dirik E, Kurul S.
Prevalence and clinical findings of migraine and
tension-type headache in adolescents.
Pediatr Int 2007; 49: 9439.Ando N, Fujimoto S, Ishikawa T, et al.
Prevalence and features of migraine in Japanese
junior high school students ages 1215 years.
Brain Dev 2007; 29: 4825.Lee LH, Olness KN.
Clinical and demographic characteristics of migraine in urban children.
Headache 1997; 37: 26976.Mavromichalis I, Anagnostopoulos D, Metaxas N, Papanastassiou E.
Prevalence of migraine in schoolchildren and some
clinical comparisons between migraine with and without aura.
Headache 1999; 39: 72836.Split W, Neuman W.
Epidemiology of migraine among students from
randomly selected secondary schools in Lodz.
Headache 1999; 39: 494501.Lu SR, Fuh JL, Juang KD, Wang SJ.
Migraine prevalence in adolescents aged 1315:
a student population-based study in Taiwan.
Cephalalgia 2000; 20: 47985.Kong CK, Cheng WW, Wong LY.
Epidemiology of headache in Hong Kong primary-level schoolchildren:
questionnaire study.
Hong Kong Med J 2001; 7: 2933.Ayatollahi SM, Moradi F, Ayatollahi SA.
Prevalences of migraine and tension-type headache in
adolescent girls of Shiraz (southern Iran).
Headache 2002; 42: 28790.Fuh JL, Wang SJ, Lu SR, Juang KD.
Ice-cream headache a large survey of 8359 adolescents.
Cephalalgia 2003; 23: 97781.Ozge A, Bugdayci R, Sasmaz T, et al.
The sensitivity and specificity of the case definition criteria in
diagnosis of headache: a school-based epidemiological study
of 5562 children in Mersin.
Cephalalgia 2003; 23: 13845.Zencir M, Ergin H, Sahiner T, et al.
Epidemiology and symptomatology of migraine among
school children: Denizli urban area in Turkey.
Headache 2004; 44: 7805.Wang SJ, Fuh JL, Juang KD, Lu SR.
Rising prevalence of migraine in Taiwanese adolescents
aged 1315 years.
Cephalalgia 2005; 25: 4338.Anttila P, Metsahonkala L, Sillanpaa M.
Long-term trends in the incidence of headache
in Finnish schoolchildren.
Pediatrics 2006; 117: e1197201.Bigal ME, Lipton RB, Winner P, Reed ML, Diamond S, Stewart WF.
Migraine in adolescents association with
socioeconomic status and family history.
Neurology 2007; 69: 1625.Visudtibhan A, Siripornpanich V, Khongkhatithum C, et al.
Migraine in Thai children: prevalence in junior high school students.
J Child Neurol 2007; 22: 111720.
Return to HEADACHE
Return to PEDIATRICS
Since 10-14-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |