Plausible Impact of Forward Head Posture
on Upper Cervical Spine StabilityThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Family Med Prim Care 2020 (May 31); 9 (5): 2517–2520 ~ FULL TEXT
OPEN ACCESS Eric C. P. Chu, Fa Sain Lo, and Amiya Bhaumik
New York Chiropractic and Physiotherapy Centre,
New York Medical Group,
Hong Kong, China.The cervical spine is responsible for allowing mobility and stability to the head and neck. Any deviation to the center of gravity of the head results in an increase in cantilever loads, which can be particularly damaging to the upper cervical joints. Excessive neck bending also exaggerates stretching through the cervical spine and all of the spinal structures below. It has been reported that forward head posture (FHP) can cause a multitude of disorders including cervical radiculopathy, cervicogenic headaches and cervicogenic dizziness. Most of these conditions manifest with clusters of painful symptoms and spine dysfunctions. The purpose of this case study is to describe the radiographic imaging considerations and to illustrate the potential impacts in symptomatic adults with FHP. We randomly selected radiographs of three individuals with FHP who had undergone cervical adjustment for cervical pain. The occipito-axial (C0-C2) and atlanto-axial (C1-C2) joints were assessed via the C0-2 distance from the C2 base to the McGregor line (Redlund-Johnell criterion) and the Ranawat C1-2 index, in addition to subjective radiographic parameters. By comparing the radiographs of before-and-after intervention of each patient, a regressive joint spacing was observed from both indices. Such a long-lasting stretching concordant with FHP was assumed to be hazardous to joint stability. A definite conclusion, however, cannot be drawn due to the small sample size and a lack of convincing measurements.
Keywords: Atlantoaxial joint; cervical adjustment; forward head posture; instability; occipito-axial joint.
From the FULL TEXT Article:
Introduction
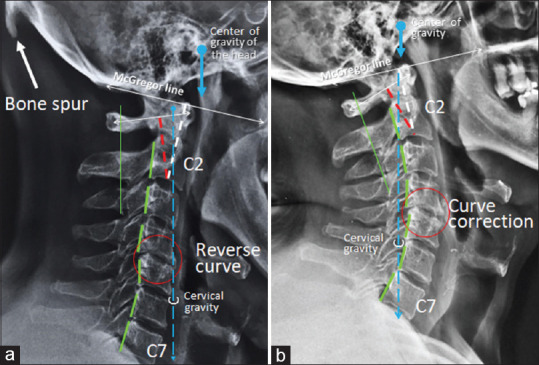
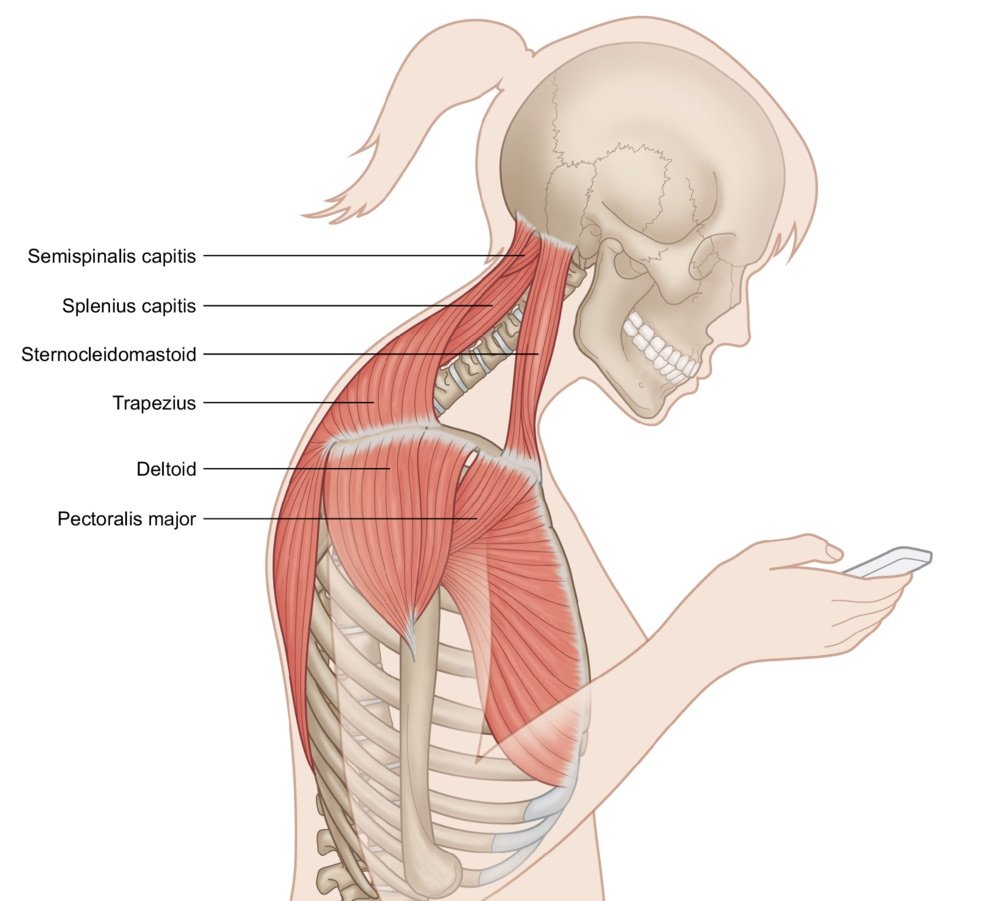
Figure 1 It has been reported that forward head posture (FHP) can cause a multitude of disorders including cervical radiculopathy, [1] cervicogenic headaches, [2] and cervicogenic dizziness. [3] The purpose of this report is to shed light on the potential impacts of FHP on upper cervical stability in symptomatic adults. Radiographic parameters used in this report included the following: The center of gravity of the head was approximated by using the anterior portion of the external auditory canal as the initial point for the plumb line, [4] cervical gravity line is a plumb line drawn through the apex of the dens. Both gravity lines allow a gross assessment of the gravitational stresses. McGregor's line is the line drawn between the hard palate and the most caudal occipital point, and is used to assess a vertical displacement of the C2 relative to insert proper parameter. Redlund-Johnell criterion is the distance from the base of C2 to the McGregor's line (males >34 mm and females >29 mm). Ranawat's line is the perpendicular distance between the midpoint of the base of C2 and a line drawn along the axis of the C1 vertebra, (males >23.7 mm, females >24.2 mm). [5] Swischuk's line is the line drawn between the laminae of C1 and C3 on a lateral X-ray. C2 should be within 1.5–2 mm of this line. There are several radiographic parameters commonly used to assess the cervical alignment including lordotic angle, cranio-vertebral angle, neck tilt, etc., However, a gross angle measurement may be obliterated by the effect of segmental deformities, as those with the S-shaped cervical curvature [Figure 1a]. The regional vertebral anomaly must be taken into consideration when dealing with a gross curve assessment.
Case Reports
This retrospective chart review was exempted from the ethics committee/IRB approval.
Case 1
A 55-year-old male, office worker, presented with a history of progressively worsening nuchal pain and paresthesias radiating into the right shoulder and arm of 6 months duration. The symptoms were worse in the latter part of the day. On clinical examination, the patient exhibited forward head posture (FHP), joint restrictions in upper and mid cervical regions, limited cervical extension, and sensory deficit consistent with C5 dermatomal distribution. The cervical radiography [Figure 1a] showed a loss of cervical lordosis, backward subluxation of the C4 on C5 (red circle), and an occipital enthesophyte (white arrow). A right C5 radiculopathy was diagnosed, and subsequently cervical adjustment was commenced. After 12 sessions of chiropractic treatment, the patient experienced complete alleviation from nuchal pain and radicular symptoms. At 9 month follow-up radiographs revealed a restoration of the cervical curvature [Figure 1b].
Case 2
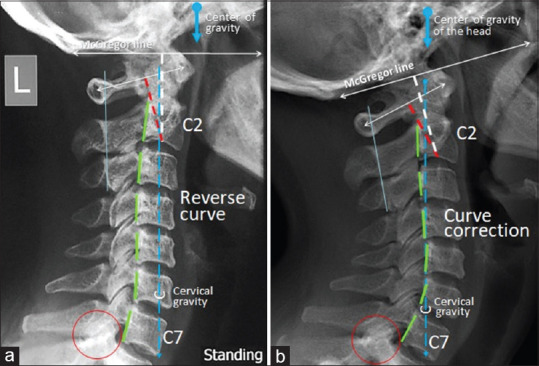
Figure 2
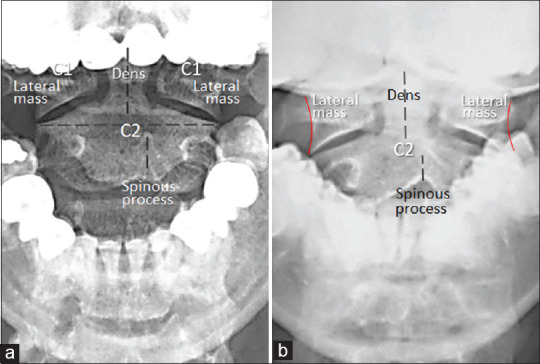
Figure 3 A 49-year-old female, accounting manager, presented with neck pain and radicular pain travelling down the right shoulder and back of the arm and forearm, going into the 4th and 5th digits. The symptoms were sometimes exacerbated after working on a computer for long periods. Her primary care physician suggested that she was suffering from a spinal degeneration and cervical radiculopathy. The patient underwent physiotherapy and was prescribed pain medications and herbal remedies over 9 months duration with only minimal relief. Upon presentation to our clinic, the patient exhibited FHP. The cervical range of motion (ROM) was limited to 50° right rotation (normal > 90°) and 30° extension (normal > 70°). The intersegmental restrictions were found at C4/5, C5/6, and C7/T1 levels. The cervical radiography [Figure 2a] displayed reverse cervical lordosis and degenerative spondylosis with ankylosis of the C7/T1 facet joints (red circle). In addition, some rotatory displacement of the C2 was suspected on open mouth view [Figure 3a]. The patient underwent chiropractic treatment consisting of thermal ultrasound therapy, spinal mobilization, cervical adjustment, and cervical extension-compression traction. The symptoms started to get better and were resolved at 2 months. The X-ray indicated a satisfactory restoration of the cervical lordosis at 9 months follow-up [Figure 2b].
Case 3
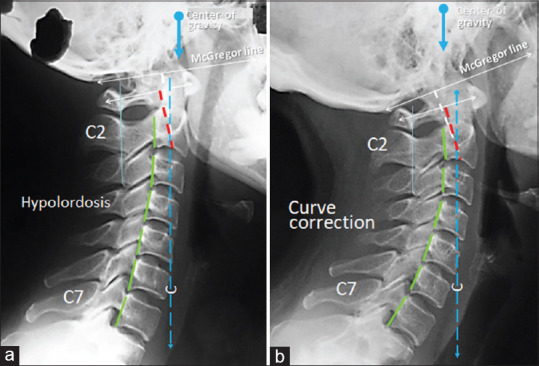
Figure 4 A 43-year-old female, fitness trainer, complained of chronic nuchal pain and bilateral upper arm pain. Her symptoms began 2 years prior and had intermittent, insidious symptom exacerbation. She described the pain as starting from her neck and extending down to her right shoulder and then to the lateral forearm. In the absence of identifiable pathology on cervical magnetic resonance imaging (MRI), she initiated non steroidal anti-inflammatory drugs (NSAID) treatment and did not attain any significant improvement. The regular massage therapy offered some temporary symptomatic relief but no long lasting results. Approximately one week prior to presenting to our clinic, the patient had experienced severe, acute flare-up of the nuchal symptoms with shoulder numbness. She sought chiropractic care and rated the pain at 4/10 on a numeric pain score. The cervical ROM was limited to 70° bilateral rotation (normal >90°) and 40° extension (normal >70°). The spinal palpation revealed intersegmental restriction at the cervicothoracic junction. The cervical radiography [Figure 4a] revealed a loss of cervical lordosis, narrowing of the C7/T1 interspace, and facetitis of the right C5/C6 and C7/T1 facet joints. In addition, some rotatory displacement of the C2 was suspected on open mouth view [Figure 3b]. She was diagnosed with degenerative spondylosis with possible right C6 radiculopathy. The treatment included thermal ultrasound, cervical extension-compression traction, and spinal manipulation. Within 3 months of initiating the treatment, the patient had significant improvement of her symptoms and continued to receive maintenance chiropractic treatment. The radiographs obtained 2 years since the beginning of treatment revealed complete restoration of the cervical curve [Figure 4b].
Discussion
The upper cervical spine (C0-C2) is responsible for 50% of total neck flexion and extensionas as well as 50% of overall cervical rotation. The FHP involves increased extensions of the upper cervical vertebrae, extension of the occiput on C1, and increased flexion of the lower cervical vertebrae and the upper thoracic regions. While the ligaments act as sensory organs involved in ligamento-muscular reflexes, joint displacement (s) produce pain and muscle spasms. The reflex is emanated from the ligamentous mechanoreceptors (i.e. pacinian corpuscles, golgi tendon organs, and ruffini endings) and transmitted to the muscles. [6] In the upper cervical spine, joint instability can cause a number of biomechanical symptoms including, but not limited to, vertebrobasilar insufficiency, cervicogenic dizziness, head and facial pain, nerve irritation, and cervical radiculopathy [6] Therefore, it is reasonable to assume that in some cases of FHP, the root cause of complaints may be underlying biomechanical effects due to joint instability.
A bony spur (enthesophyte) projecting from the external occipital protuberance [Figure 1a] is a vestigial trait as evidence for previous enthesitis (insertional tendinitis). The enthesis is the insertional site of where a tendon or ligament attaches to the bone. Repetitive biomechanical strain and micro damage can induce cytokines to trigger an inflammatory response in the adjacent synovial tissue leading to synovitis. [7] Substantial immune response contributes to abnormal induction of fibrous tissue/fibro cartilage-bone interactions resulting in radiographically detectable enthesopathy (insertional tendinopathy). [7, 8] In cases of FHP, long lasting pull on the nuchal ligament and nuchal muscle created by abnormal postures can cause insertional tendinitis and bony spur in the nuchal ligament, which extends from the external occipital protuberance to the spinous process of the 7th cervical vertebra.
The scientific literature indicates that posture, radiographic positioning, and radiographic line drawing are all very reliable/repeatable. [9] There are some limitations for the measurement of distance and cervical angle. Firstly, most radiographic films were obtained retrospectively from clinicians’ referral. There were technical problems to measure the length of line segments from hard-copy films. Secondly, the patients were positioned to be routinely desired while taking radiography. The lordosis angle measurement may be independent of a resting posture. In addition to the effect of segmental spine deformity, just measuring C2-C7 lordosis angle did not reflect a gross curvature. The S-shaped cervical spine may obliterate the angle measurement by a compensatory backward tilting at the lower neck [Figure 1a]. However, the afore mentioned biases would be avoided because the radiographic parameters in this report were analyzed by comparing the differences between the before-and-after images. Both Redlund-Johnell (white dotted line) and Ranawat (red dotted line) indices regressed, with average approximation of 8% and 11% respectively. The symptomatic improvement is the supporting evidence for radiographic changes. Any pre-to-post alignment changes in patients are a result of the treatment procedures applied. [9]
The most common postural abnormality is the FHP arising from modern lifestyle. An observational assessment by a general practitioner will detect significant faults in the posture, e.g. presence of head tilt, forward head posture, uneven shoulders, spinal misalignment, and spinal curvature deformities. It will give an overview of the patient's problems in clinical settings. Analysis of a patient's posture offers information about the muscle endurance and the muscle capability to cope with physical stressors. Several reports have established the FHP as a real clinical entity with significant musculoskeletal consequences. [10] The FHP can get worse over time, causing spinal degeneration, muscle weakness and tightness, entrapment neuropathies, and the loss of vital lung capacity. The general practitioner provides immediate medical assistance for the FHP patient with a broad range of complains. The practitioner can become an effective facilitator for alleviating pain and preventing damage where abnormal posture is found to be a main contributing factor.
Conclusion
By comparing the radiographs before-and-after correction of the FHP in three symptomatic patients, a regressive joint spacing was observed from both Redlund-Johnell criterion ((C0-C2)) and the Ranawat C1-2 index. The radiographic parameters illustrated the potential impacts on upper cervical stability in symptomatic cases.
Declaration of patient consent
A copy of the written consent is available for review by the Editor-in Chief of this journal.
Conflicts of interest
The authors have no conflicts of interest to declare.
References:
Chu RCP, Lim T, Mak KC.
Cervical radiculopathy alleviating by manipulative correction of cervical hypolordosis.
J Med Cases. 2018;9:139–41.Chu ECP, Chu VKY, Lin AFC.
Cervicogenic headache alleviating by spinal adjustment in combination with extension-compression traction.
Arch Clin Med Case Rep. 2019;3:269–73.Chu RCP, Chin WL, Bhaumik A.
Cervicogenic dizziness.
Oxf Med Case Reports. 2019;11:476–8.Scheer JK, Tang JA, Smith JS, Acosta FL, Jr, Protopsaltis TS, Blondel B, et al.
Cervical spine alignment, sagittal deformity, and clinical implications: A review.
J Neurosurg Spine. 2013;19:141–59.Kwong Y, Rao N, Latief K.
Craniometric measurements in the assessment of craniovertebral settling: Are they still relevant in the age of cross-sectional imaging?
AJR Am J Roentgenol. 2011;196:W421–5.Steilen D, Hauser R, Woldin B, Sawyer S.
Chronic neck pain: Making the connection between capsular ligament laxity and cervical instability.
Open Orthop J. 2014;8:326–45.Kehl AS, Corr M, Weisman MH.
Review: Enthesitis: New insights into pathogenesis, diagnostic modalities, and treatment.
Arthritis Rheumatol. 2016;68:312–22.Voudouris KP, Sidiropoulos P, Vounotrypidis P, Arvanitakis M.
Ethesial fibrocartilage-bone interaction: A radiographic study of selected sites of nonsynovial peripheral enthesopathy.
J Musculoskel Neuron Interact. 2003;3:89–100.Harrison DD, Colloca CJ, Betz J, Janik TJ, Holland B.
Repeatability over time of posture, radiograph positioning, and radiograph line drawing: An analysis of six control groups.
J Manipulative Physiol Ther. 2003;26:87–98.Sheikhhoseini R, Shahrbanian S, Sayyadi P, O’Sullivan K.
Effectiveness of therapeutic exercise on forward head posture: A systematic review and meta-analysis.
J Manip Physiol Ther. 2018;41:530–9.
Return to FORWARD HEAD POSTURE
Since 7-28-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |