

Comparison of Spinal Manipulation Methods and
Usual Medical Care for Acute and Subacute
Low Back Pain: A Randomized Clinical TrialThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Spine (Phila Pa 1976). 2015 (Feb 15); 40 (4): 209–217 ~ FULL TEXT
OPEN ACCESS Schneider, Michael DC, PhD; Haas, Mitchell DC, MA; Glick, Ronald MD;
Stevans, Joel DC; Landsittel, Doug PhD
School of Health and Rehabilitation Sciences,
Clinical and Translational Science Institute,
University of Pittsburgh,
Pittsburgh, PA
FROM: Schneider ~ Spine (Phila Pa 1976) 2015 (Feb 15)STUDY DESIGN: Randomized controlled trial with follow-up to 6 months.
OBJECTIVE: This was a comparative effectiveness trial of manual-thrust manipulation (MTM) versus mechanical-assisted manipulation (MAM); and manipulation versus usual medical care (UMC).
SUMMARY OF BACKGROUND DATA: Low back pain (LBP) is one of the most common conditions seen in primary care and physical medicine practice. MTM is a common treatment for LBP. Claims that MAM is an effective alternative to MTM have yet to be substantiated. There is also question about the effectiveness of manipulation in acute and subacute LBP compared with UMC.
METHODS: A total of 107 adults with onset of LBP within the past 12 weeks were randomized to 1 of 3 treatment groups: MTM, MAM, or UMC. Outcome measures included the Oswestry LBP Disability Index (0-100 scale) and numeric pain rating (0-10 scale). Participants in the manipulation groups were treated twice weekly during 4 weeks; subjects in UMC were seen for 3 visits during this time. Outcome measures were captured at baseline, 4 weeks, 3 months, and 6 months.
RESULTS: Linear regression showed a statistically significant advantage of MTM at 4 weeks compared with MAM (disability = –8.1, P = 0.009; pain = –1.4, P = 0.002) and UMC (disability = –6.5, P = 0.032; pain = –1.7, P < 0.001). Responder analysis, defined as 30% and 50% reductions in Oswestry LBP Disability Index scores revealed a significantly greater proportion of responders at 4 weeks in MTM (76%; 50%) compared with MAM (50%; 16%) and UMC (48%; 39%). Similar between-group results were found for pain: MTM (94%; 76%); MAM (69%; 47%); and UMC (56%; 41%). No statistically significant group differences were found between MAM and UMC, and for any comparison at 3 or 6 months.
CONCLUSION: Manual-Thrust Manipulation (MTM) provides greater short-term reductions in self-reported disability and pain scores compared with Usual Medical Care (UMC) or Mechanical-Assisted Manipulation (MAM).
Keywords: Low back pain, spinal, manipulation, usual medical care, chiropractic, mechanical assisted manipulation, manual thrust manipulation, pain, disability
From the FULL TEXT Article:
Introduction
Low back pain (LBP) is amongst the most common medical ailments and an important public health issue. Approximately 50% of U.S. working-age adults experience LBP each year [1] with a quarter of U.S. adults reporting an episode of back pain in the previous 3 months. [2] Back pain is the most common cause of disability for persons under the age of 45 and 1 of the most common reasons for office visits to primary care physicians in the U.S. [3, 4] as well as Europe and Australia. [5–7]
Spinal manipulative therapy (SMT) is used by chiropractors, physical therapists, and osteopathic physicians for the treatment of acute LBP. The most recent Cochrane Review concluded that SMT was no more effective than inert interventions, sham SMT, or usual medical interventions. [8] A recent meta-analysis using Bayesian methods concluded that the effectiveness of SMT is equivocal. [9] However other guidelines and systematic reviews have shown moderate effectiveness of manual SMT for the care of acute LBP. [10–13]
Systematic reviews have focused on manual-thrust manipulation (MTM) and are not generalizable to mechanical-assisted manipulation (MAM) methods. MTM is still the most common type of manipulation used by chiropractors. However, surveys of the chiropractic profession over the past decade have shown a trend toward increased utilization of mechanical manipulation devices. These devices are now the second most common type of manipulation used by American chiropractors. [14–16] The most popular mechanical device used by chiropractors is the Activator® Instrument (Activator Methods, Phoenix, AZ).
Mechanical devices are promoted as safe and effective alternatives to manual manipulation, yet there is a lack of high quality trials to support this claim. A few clinical studies [17–21] compared Activator to MTM with equivocal results, but none of these trials compared Activator with usual medical care (UMC). The purpose of this study was to compare the effectiveness of MTM and MAM, and to compare both types of manipulation with UMC for the treatment of acute and sub-acute LBP.
MATERIALS AND METHODS
Design Overview
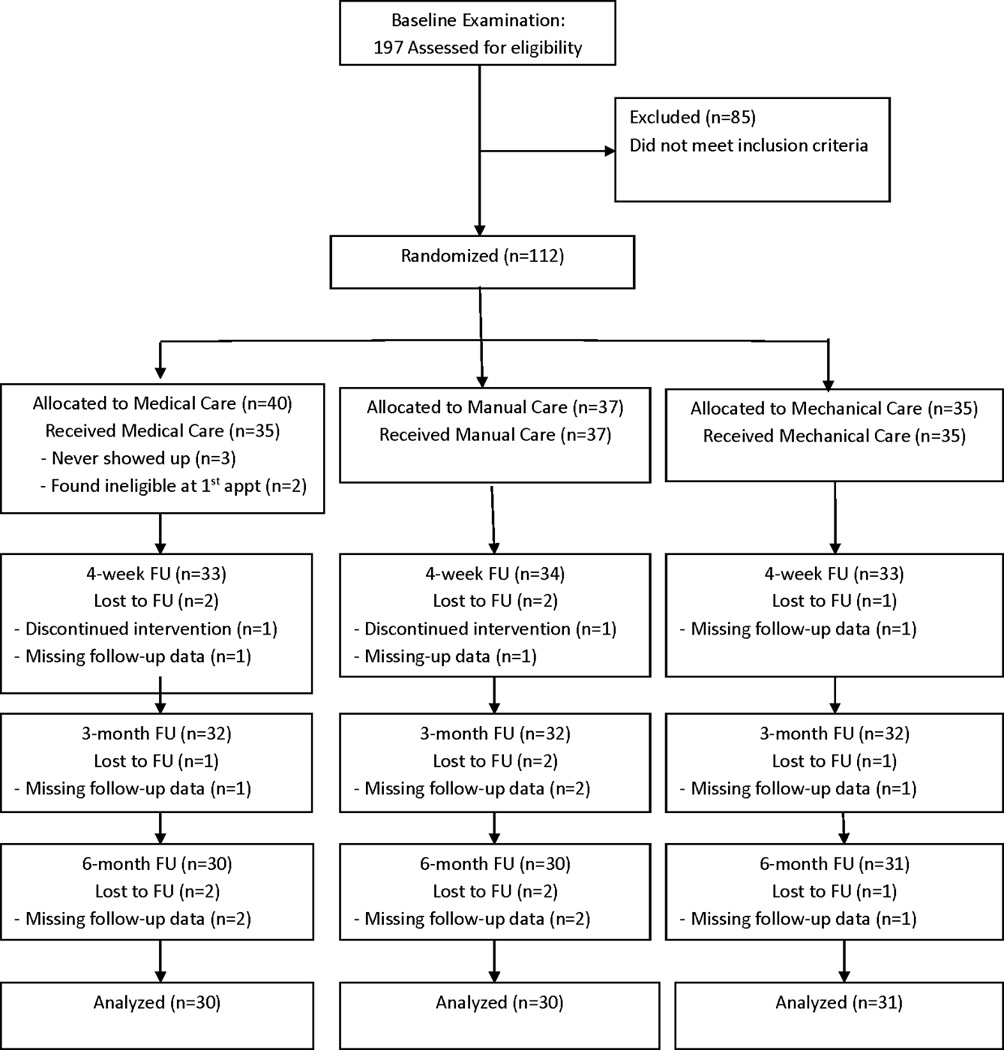
Figure 1 This was a prospective, randomized clinical trial evaluating the comparative effectiveness of manual and mechanical types of spinal manipulation and UMC for treatment of acute and sub-acute LBP. This study was approved by the University of Pittsburgh Institutional Review Board (PRO10040327); written informed consent was obtained from all study participants. We followed the CONSORT guidelines for reporting randomized trials (http://www.consort-statement.org/) and provided a CONSORT flow diagram (Figure 1).
Setting and Participants
The study was conducted between November 2010 and March 2013 at the UPMC Center for Integrative Medicine in Pittsburgh. Participants were required to have a new LBP episode within the previous 3 months, be at least 18 years of age, and speak/understand English. To prevent floor effects, minimum levels of self-reported pain (3 on 0–10 scale) and disability (20 on 0–100 scale) were also required. Participants also agreed to be randomized, attend 2 office visits per week for 4 weeks, and cooperate with follow-up data collection.
Exclusion criteria included:1) chronic LBP (> 3 months duration)
2) previous chiropractic, medical, or physical therapy treatment for the current LBP episode
3) radicular features including leg pain distal to the knee, numbness/weakness of the lower leg, or positive nerve root tension/neurological signs
4) contraindications to spinal manipulation, including: previous history of metastatic cancer, severe osteoporosis, fracture or instability, or prolonged anticoagulant or oral steroid use, or
5) current use of prescription pain medications. Participants were permitted to take over-the-counter medications for back pain.Randomization and Blinding
Randomization was conducted using a rank-based adaptive allocation design [22] to balance groups on baseline pain, disability, and treatment expectation. Randomization was computer generated remotely via a data center website following baseline examination so that allocation was concealed until the moment of randomization. It was not possible to blind participants or treating clinicians to treatment assignment.
Informed consent and baseline examinations to determine eligibility were performed by a chiropractor with 10 years of clinical experience; he did not provide treatment. A research coordinator with 20 years of clinical trials experience was responsible for overseeing randomization and data collection procedures. She maintained a secure randomization master file that linked personal identifying information with a unique research ID. The principal investigator (PI) was blinded and had no interaction with research participants. The PI was also blinded during the tasks of data collection and the primary data analysis. These tasks were conducted by the research coordinator (collection) and biostatistician (analysis), who were not blinded to group allocation.
Study Interventions1. Manual-Thrust Manipulation (MTM) Participants were given high-velocity low-amplitude thrust manipulation in the side posture position by a licensed chiropractor. Segmental levels where manipulation was applied were determined using standard chiropractic methods of static and motion palpation. [23]
2. Mechanical-Assisted Manipulation (MAM) Participants were given mechanical-assisted manipulation in the prone position by a certified Activator Methods chiropractor using the Activator IV Instrument (FDA approval # K003185, Manufacturer: Activator Methods International Ltd., Phoenix, AZ). Segmental levels where the manipulation was applied was determined by using palpation and the Activator method of leg length analysis. [24]
3. Usual Medical Care (UMC) Participants were seen by a medical physician, board certified in physical medicine and rehabilitation. These participants were told that most new episodes of back pain are typically self-limiting, were prescribed over-the-counter analgesic and NSAID medications, given advice to stay physically active and avoid prolonged bed-rest. This protocol is consistent with current clinical guidelines for the management of non-specific LBP in primary care practice. [25]All participants were treated over the course of 4 weeks. The 2 manipulation groups attended 8 office visits (~15 mins each), twice per week for 4 weeks, a typical chiropractic treatment schedule. Chiropractors typically consider the lower thoracic, lumbar, and sacroiliac joints as one kinetic chain, and therefore we permitted them to perform manipulation in any of these regions as they deemed necessary. No manipulation of other spinal or peripheral joints was permitted. If manipulation was not indicated on any particular visit, the patient was given reassurance and dismissed without treatment that day. The UMC group attended a total of 3 office visits; an initial visit (~30 mins) with follow-up visits (~15 mins each) at 2 and 4 weeks. After the 4-week assessment, participants were free to pursue rehabilitation or manipulative treatment.
The same clinician provided all care within each treatment group: a single PM&R physician provided all UMC; a single chiropractor provided all MTM, and a single chiropractor provided all MAM. Each of the treating clinicians had over 15 years of clinical experience and provided strong enthusiasm for his respective treatment approach. Participants in all 3 treatment arms received a copy of the same educational booklet [26] from their clinician, providing information about proper posture and movements during activities of daily living.
Outcomes and Follow-up
The primary outcome measure was the Oswestry LBP Disability Index. It has been widely used in LBP research and is considered to be a valid/reliable measure of functional impairment. [27] The Oswestry score ranges from 0 to 100, with higher numbers representing higher levels of self-reported disability. The secondary outcome was a self-reported pain-intensity scale, computed as the mean of 3 numeric pain rating scales: current pain, worst pain in the past 24 hours, and average pain over the past week. [28] The 3 individual 0 to 10 scales were anchored by 0 indicating “no pain” and 10 indicating “unbearable pain”. Outcomes were assessed at baseline, 4 weeks, 3 months, and 6 months. Additional baseline variables included demographics, physical examination findings, fear avoidance beliefs questionnaire [29], and treatment credibility-expectation questionnaire. [30]
Statistical Analysis
The primary analysis was linear regression [31] with Oswestry score as the dependent variable, treatment group as the independent variable, and forced covariate adjustments for baseline Oswestry, pain, and treatment expectation (used in the randomization algorithm). Comparison of MTM to MAM was specified a-priori as the single primary comparison; therefore, no adjustments were made for multiple comparisons. Secondary associations included comparisons of MTM to UMC and MAM to UMC. The analysis was repeated using pain as the dependent variable.
Longitudinal trends were evaluated using a mixed model [32] with a random intercept to account for within-patient correlations, and using separate linear models fit to the 3-month and the 6-month outcomes. The same covariates were included in the models.
Participants who achieved at least 30% or 50% decreases in an outcome were considered to be responders with “moderate” or “substantial” improvement, respectively. [33, 34] The proportions of responders in each treatment group were compared using logistic regression with the previously-described covariate adjustments.
All analyses were conducted as intention-to-treat with participants in their originally assigned group. For missing follow-up data, the outcome measure was imputed using the prediction from a participant-specific regression of available outcomes at baseline and later time points. Sensitivity analyses were run without imputed data. Stata version 12 (Stata Corp., College Station, TX) was used for all statistical analyses.
Sample size was determined a priori by power analysis that indicated the need for 105 participants (n=35 per group) to achieve 80% power for detecting a 10-point difference between groups in Oswestry score (primary outcome) at an alpha level of 0.05. This was based upon a conservative estimate of the minimal clinically important difference for Oswestry score and using a standard deviation of 14 points. [35, 36]
RESULTS

Table 1 After telephone screening, 197 potentially eligible people received a baseline examination, 112 were randomized, and 107 received treatment (Figure 1). Of the 40 participants allocated to medical care, 2 were subsequently found ineligible and 3 never began treatment. Baseline variables were successfully balanced across the 3 groups (Table 1). Mean participant disability (39.9) and pain (5.7) were moderate in intensity. No adverse events were reported.
Primary and Secondary Analysis

Table 2 Outcomes, within-group changes and between-groups comparisons with SDs and/or 95% confidence intervals are found in Table 2. The primary comparison at 4 weeks showed significantly reduced disability for MTM versus MAM, with an adjusted mean difference (Δ) of –8.1, p=0.009. Comparison of MTM to UMC showed a similar result (Δ = –6.5, p=0.032). Comparison of MAM to UMC showed a non-significant difference (Δ = 1.5, p=0.609). Excluding missing data led to very similar results.
For pain scores, the adjusted mean difference between MTM and MAM was –1.4 (p=0.002). MTM again showed a significant reduction in pain versus UMC (Δ = –1.7, p<0.001). However, there was no significant difference between MAM in comparison to UMC (Δ = –0.3, p=0.480). All results were similar after excluding all missing data.
Longitudinal Analysis
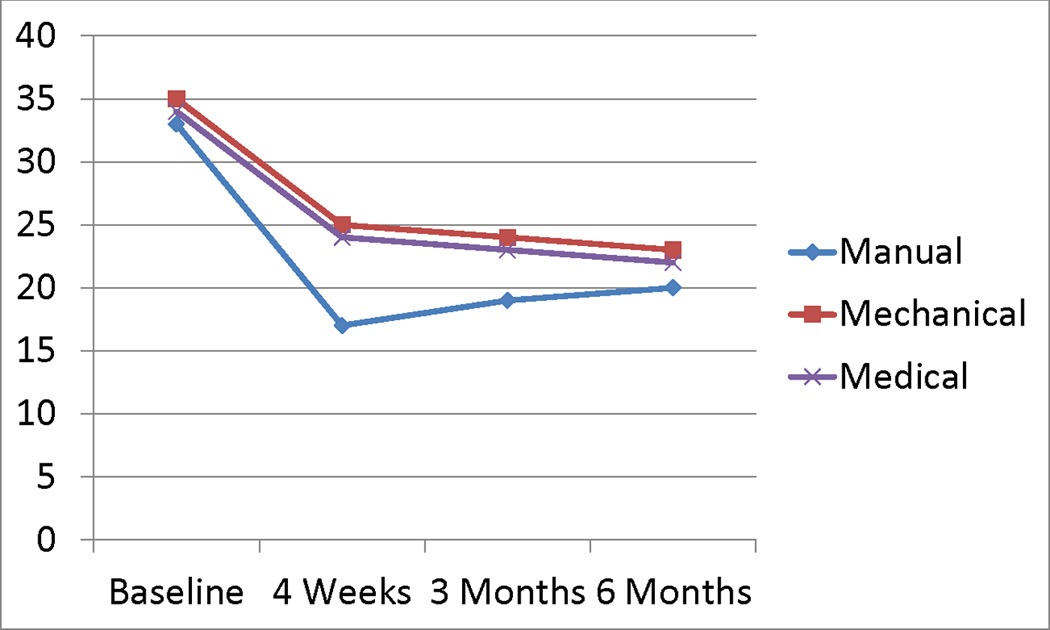
Figure 2
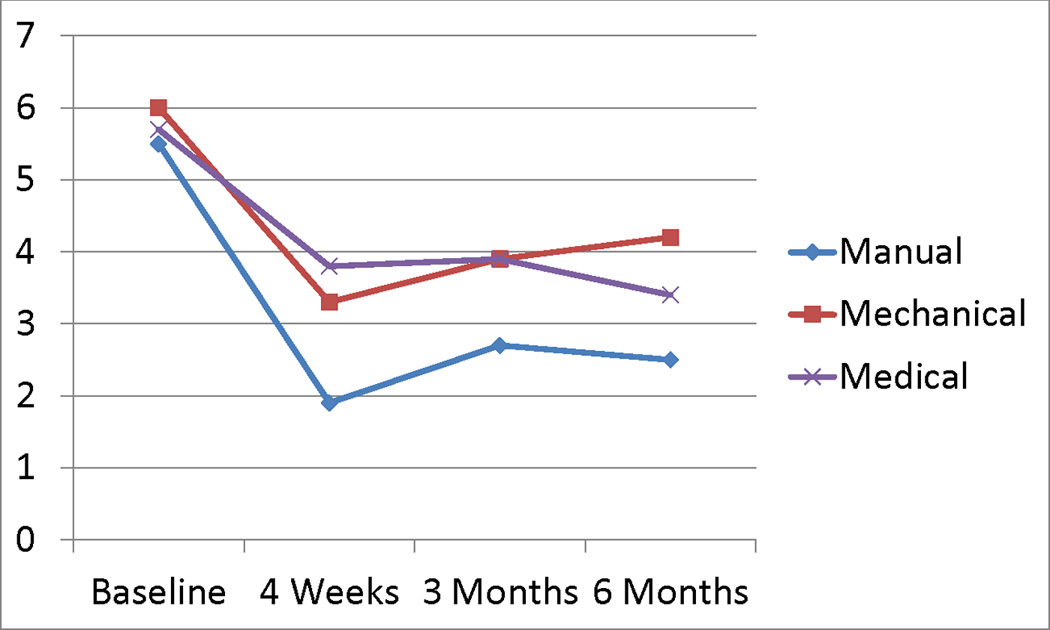
Figure 3

Table 3
Figure 4

Figure 5 The longitudinal profiles portraying group differences in disability and pain over time are plotted in Figures 2 and 3. For disability, there were no statistically significant differences between groups in the repeated measures model: the adjusted mean differences were 3.5 (p=0.308) for MTM versus MAM; –2.5 (p=0.461) for MTM versus UMC; and 1.0 (p=0.778) for MAM versus UMC. None of the tests at the 3 or 6-month time points were statistically significant (Table 2).
For pain, the adjusted mean differences were: –1.1 (p=0.0.047) for MTM versus MAM; –1.2 (p=0.039) for MTM versus UMC; and 0.04 (p=0.940) for MAM versus UMC. Although the repeated-measures model demonstrated statistically significant differences in the 2 comparisons with MTM, the individual regressions at the 3-month and 6-month time points showed no significant results (Table 2). Sensitivity analysis showed that exclusion of missing data led to similar adjusted mean differences between groups for the longitudinal analysis of both disability and pain. There were no statistically significant group differences for disability as above. For pain, the repeated-measures analysis was also statistically significant for MTM versus UMC. However, the 6-month analysis was significant for MTM versus MAM in contrast to the analysis with imputed data.
Responder Analysis
Table 3 and Figure 4 display the disability responder analysis at 4 weeks. Seventy-six percent of the MTM group achieved at least a 30% reduction in disability compared with approximately 50% of the MAM (p = 0.013) or UMC (p = 0.024) groups; MAM was not significantly different from UMC (p=0.804). Fifty percent of the manual group achieved at least a 50% reduction compared with 16% of the MAM (p = 0.001) and 39% of the UMC (p = 0.267) groups; MAM was significantly worse than UMC (p= 0.015) for this outcome.
Table 3 and Figure 5 show that 94% of the MTM group achieved greater than 30% reduction in pain compared to 69% of MAM (p=0.009) and 56% of UMC (p=0.002). Seventy-six percent of the MTM group attained more than 50% reduction in pain compared to 47% of MAM (p=0.008) and 41% of UMC (p=0.006). The comparisons between MAM and UMC were not significant.
DISCUSSION
Treatment for acute and sub-acute LBP is a classic example of preference-sensitive care [37], where several effective treatment options exist for a specific condition and all should be offered to the patient. Guidelines from the American College of Physicians and the American Pain Society recommend that patients with nonspecific LBP should be provided with NSAIDS and “watchful waiting” which emphasizes spontaneous recovery and prompt return to normal activity. [38, 39] Although this approach is reasonable and the general prognosis for acute back pain is favorable, some patients may actually have preference for non-pharmacological therapies including spinal manipulation.
Our primary analysis showed that the MTM group achieved a statistically significant short-term reduction in disability compared with the UMC group (and MAM). The magnitude of the treatment effect size and clinical significance are relatively modest, but still relevant to patients with back pain. Manipulation should be offered as an effective therapeutic option to patients within the context of preference-sensitive care, allowing the patient to make an informed choice which reflects their individual values and preferences. It has been found that treatment options which align with patient preferences lead to enhanced patient satisfaction. [40]
One reason for the observed advantage of MTM may be the characteristics of our study population; we only included patients with recent onset of LBP that had localized lumbar/buttock pain provoked by palpation, and did not have pain distal to the knee. This was by design, because previous research has found that these characteristics represent key clinical findings in a subgroup of LBP patients that are likely to respond well to spinal manipulation and can be helpful in guiding shared decision making. [41–44]
An important finding from our study was the significant advantage of MTM over MAM on reductions in both disability and pain scores (Table 2). Also, the MTM group had at least 25% more responders for both outcomes and levels of improvement compared to the MAM group (Table 3). These findings contradict the assumption of therapeutic equivalence between these 2 methods of manipulation. This is another important factor to consider when advising patients on the manipulation treatment options available for LBP.
There were several limitations to our study. We could not determine what portion of the healing response was attributable to natural history, direct treatment effect, and/or non-specific factors, because there was no natural-history control. This was a single-center study with a modest sample size. It was not possible to blind participants and providers to treatment group. Each type of treatment was delivered by a single clinician, and it is possible that part of the treatment response was due to indirect contextual factors related to participant-provider interaction, rather than the direct effect of the treatment alone. This has been noted in a randomized trial of care provided by chiropractors for chronic LBP. [45]
Participants had 8 treatments with the chiropractors but only 3 with the medical doctor, creating a differential in clinical time/attention between participants and their providers. However, this difference is generalizable to the “real world” setting; a recently analysis of the Medicare Expenditure Panel Survey data revealed that the average number of chiropractic and medical visits were 8 and 2, respectively. [46] Also, the doctor-patient encounter was found to be a poor mediator between number of assigned visits to a chiropractor and clinical outcomes. [45]
CONCLUSION
Manual-Thrust Manipulation (MTM) led to greater short-term reductions in self-reported pain and disability than Mechanical-Assisted Manipulation (MAM) or Usual Medical Care (UMC). These changes were both statistically significant and clinically meaningful. The benefit seen at end-of-intervention was no longer statistically significant at 3 or 6 months. No adverse outcomes were reported. MTM should be considered an effective short-term treatment option for patients with acute and sub-acute LBP. MAM and UMC appear similar in effect; both lead to decreased pain and disability, but their value compared to natural history was not evaluated in this study.
Acknowledgments
The device(s)/drug(s) is/are FDA-approved or approved by corresponding national agency for this indication. The National Institutes of Health, National Center for Complementary and Alternative Medicine (NIH/NCCAM) Grant # R00 AT004196 funds were received in support of this work. Relevant financial activities outside the submitted work: consultancy, expert testimony, grants, payment for lecture, royalties, payment for development of educational presentations.
ABBREVIATIONS
LBP = Low Back Pain
MTM = Manual Thrust Manipulation
MAM = Mechanical Assisted Manipulation
SMT = Spinal Manipulative Therapy
UMC = Usual Medical Care
Contributor Information
Michael Schneider, Associate Professor, School of Health and Rehabilitation Sciences, Associate Professor, Clinical and Translational Science Institute, University of Pittsburgh, Bridgeside Point 1, 100 Technology Drive, Suite 210, University of Pittsburgh, Pittsburgh, PA 15219 USA, (Tel) 412.383.6640(Fax) 412.648.5970 ; Email: ude.ttip@5sjm
Mitchell Haas, Associate Vice President of Research, University of Western States, 2900 NE 132nd Avenue, Portland, OR 97230, Email: ude.swu@saahm
Ronald Glick, Assistant Professor of Psychiatry and Physical Medicine and Rehabilitation; University of Pittsburgh School of Medicine, Medical Director; Center for Integrative Medicine at UPMC Shadyside, 580 South Aiken Avenue, Suite 310, Pittsburgh, PA 15232, Email: ude.cmpu@mrkcilg
Joel Stevans, Assistant Professor and PhD Candidate, School of Health and Rehabilitation Sciences, Bridgeside Point 1, 100 Technology Drive, Suite 210, University of Pittsburgh, Pittsburgh, PA 15219, Email: ude.ttip@363smj
Doug Landsittel, Professor, Department of Medicine and Department of Biostatistics, Professor, Clinical & Translational Science Institute, Biostatistician, Center for Research on Health Care Data Center University of Pittsburgh, 200 Meyran Avenue, Suite 300, Pittsburgh, PA 15213, Email: ude.cmpu@pdlettisdnal
References:
Andersson GBJ.
Epidemiological features of chronic low-back pain.
Lancet. 1999;354:581–585Hart LG, Deyo R, Cherkin D.
Physician office visits for low back pain. Frequency, clinical evaluation, and
treatment patterns from a U.S. national survey.
Spine. 1995;20:11–19Deyo RA, Tsui-Wu YJ.
Descriptive epidemiology of low-back pain and its related medical care
in the United States.1987.
Spine. 1987;12:264–268Cunningham LS, Kelsey JL.
Epidemiology of musculoskeletal impairments and associated disability.
Am J Public Health. 1984;74:574–579Palmer KT, Walsh K, Bendall H, Cooper C, Coggon D.
Back pain in Britain: comparison of two prevalence surveys at an interval of 10 years.
BMJ. 2000;320:1577–1578Santos-Eggimann B, Wietlisbach V, Rickenbach M,
Paccaud F, Gutzwiller F.
One-year prevalence of low back pain in two Swiss regions: estimates from the
population participating in the 1992–1993 MONICA project.
Spine. 2000;25:2473–2479Walker BF, Muller R, Grant WO.
Low back pain in Australian adults: prevalence and associated disability.
J Manipulative Physiol Ther. 2004;27:238–244Rubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW.
Spinal manipulative therapy for acute low back pain: an update of the Cochrane review.
Spine. 2013;38:E158–E177Menke JM.
Do Manual Therapies Help Low Back Pain?: A Comparative Effectiveness Meta-Analysis.
Spine. 2014;39:E463–E472Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr., Shekelle P, Owens DK:
Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline
from the American College of Physicians and the American Pain Society
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 478–491Chou R, Huffman LH; American Pain Society.
Nonpharmacologic Therapies for Acute and Chronic Low Back Pain:
A Review of the Evidence for an American Pain Society/
American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 492–504Bronfort, G, Haas, M, Evans, R, Kawchuk, G, and Dagenais, S.
Evidence-informed Management of Chronic Low Back Pain
with Spinal Manipulation and Mobilization
Spine J. 2008 (Jan); 8 (1): 213–225Lawrence DJ, Meeker W, Branson R, Bronfort G, Cates JR, Haas M, Haneline M et al.
Chiropractic Management of Low Back Pain and Low Back-Related
Leg Complaints: A Literature Synthesis
J Manipulative Physiol Ther 2008 (Nov); 31 (9): 659–674Christensen MG, Kerkhoff D, Kollasch MW.
Job Analysis of Chiropractic 1993
Greeley (CO): National Board of Chiropractic Examiners, 1993Christensen MG, Kerkhoff D, Kollash MW.
Job Analysis of Chiropractic. Greeley, CO:
National Board of Chiropractic Examiners; 2000Christensen MG, Kollash M, Ward R, Webb K, Day M, zum Brunnen J.
Job Analysis of Chiropractic. 2005
Greeley, CO: National Board of Chiropractic Examiners; 2005Yurkiw D, Mior S.
Comparison of two chiropractic techniques on pain and lateral flexion in
neck pain subjects: a pilot study.
Chiropractic Technique. 1996;8:155–162Wood TG, Colloca CJ, Mathews R.
A Pilot Randomized Clinical Trial on the Relative Effect of Instrumental
(MFMA) Versus Manual (HVLA) Manipulation in the Treatment
of Cervical Spine Dysfunction
J Manipulative Physiol Ther 2001 (May); 24 (4): 260–271Gemmell HA, Jacobson BH.
The immediate effect of Activator vs. Meric adjustment on acute low back pain:
A randomized controlled trial.
J Manipulative Physiol Ther. 1995;18:453–456Shearer KA, Colloca C, White H.
A Randomized Clinical Trial of Manual Versus Mechanical Force
Manipulation in the Treatment of Sacroiliac Joint Syndrome
J Manipulative Physiol Ther 2005 (Sep);28 (7): 493–501Schneider MJ, Brach J, Irrgang J, Verdolini K,
Wisniewski S, Delitto A.
Mechanical versus manual manipulation for low back pain: An observational cohort study.
J Manipulative Physiol Ther. 2010;33:193–200Stigsby B, Taves DR.
Rank-Minimization for balanced assignment of subjects in clinical trials.
Contemp Clin Trials. 2010;31:147–150Bergmann TF, Peterson DH.
Chiropractic Technique: Principles and Procedures. 3rd ed.
St. Louis, MO: Mosby; 2011Fuhr AW, Green JR, Colloca CJ, Kellern T.
Activator Methods Chiropractic Technique. St. Louis, MO:
Mosby Year Book; 1997Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C.
An Updated Overview of Clinical Guidelines for the Management of
Non-specific Low Back Pain in Primary Care
European Spine Journal 2010 (Dec); 19 (12): 2075–2094Schneider MJ, Farrell P.
Preventing Low Back Pain and Injury.
Minneapolis, MN: OPTP Inc; 2003Fairbank JC, Pynsent PB.
The Oswestry Disability Index
Spine (Phila Pa 1976) 2000 (Nov 15); 25 (22): 2940–2952Von Korff M, Deyo RA.
Back pain in primary care: Outcomes at 1 year.
Spine. 1993;18:855–862Waddell G, Newton M.
A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs
in chronic low back pain and disability.
Pain. 1993;52:157–168Smeets RJ, Beelen S, Goossens ME, Schouten EG, Knottnerus A, Vlaeyen JW.
Treatment expectancy and credibility are associated with the outcome of both physical
and cognitive behavioral treatment in chronic low back pain.
Clin J Pain. 2008;24:305–315Rosner B.
Fundamentals of Biostatistics. 7th Edition.
Boston MA: Brooks/Cole, Cengage Learning; 2011Rabe-Hesketh S, Skrondal A.
Multilevel and Longitudinal Modeling Using Stat. 1st Edition.
College Station TX: Stata Press; 2005Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS,
Farrar JT, Haythornthwaite JA, Jensen MP, Kerns RD, Ader DN, et al.
Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials:
IMMPACT Recommendations.
J Pain. 2008;9:105–121Dworkin RH, Turk DC, McDermott MP, Peirce-Sandner S,
Burke LB, Cowan P, Farrar JT, Hertz S, Raja SN, Rappaport BA, et al.
Interpreting the clinical importance of group differences in chronic pain clinical trials:
IMMPACT recommendations.
Pain. 2009;146:238–244Fritz JM, Irrgang JJ.
A comparison of a Modified Oswestry Disability Questionnaire and the
Quebec Back Pain Disability Scale.
Phys Ther. 2001;81:776–788Hagg O, Fritzell P, Nordwall A.
The clinical importance of changes in outcome scores after treatment
for chronic low back pain.
Eur Spine J. 2003;12:12–20Wennberg JE.
Tracking Medicine. New York, NY:
Oxford University Press; 2010Stanley J. Bigos, MD, Rev. O. Richard Bowyer, G. Richard Braen, MD, et al.
Acute Lower Back Problems in Adults. Clinical Practice Guideline No. 14.
Rockville, MD: Agency for Health Care Policy and Research,
Public Health Service, U.S. Department of Health and Human Services; 1994Chou R, Qaseem A, Snow V, Casey 0, Cross J, Shekelle PG, Owens 0.
Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline
from the American College of Physicians and the
American Pain Society
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 478–491Eisenberg DM, Post DE, Davis RB, et al.
Addition of choice of complementary therapies to usual care for acute low back pain:
a randomized controlled trial.
Spine. 2007;32:151–158Flynn T, Fritz J, Whitman J, Wainner R, Magel J, Rendeiro D. et al.
A Clinical Prediction Rule for Classifying Patients with Low Back Pain
who Demonstrate Short-term Improvement with Spinal Manipulation
Spine (Phila Pa 1976). 2002 (Dec 15); 27 (24): 2835–2843Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, Majkowski GR, et al.
A Clinical Prediction Rule To Identify Patients With Low Back Pain Most Likely To Benefit
from Spinal Manipulation: A Validation Study
Annals of Internal Medicine 2004 (Dec 21); 141 (12): 920–928Cleland JA, Fritz J, Kulig K, et al.
Comparison of the effectiveness of three manual physical therapy techniques in a
subgroup of patients with low back pain who satisfy a clinical prediction rule:
a randomized clinical trial.
Spine. 2009;34:2720–2729Brennan GP, Fritz J, Hunter S, et al.
Identifying subgroups of patients with acute/subacute "nonspecific" low back pain:
results of a randomized clinical trial.
Spine. 2006;31:623–631Haas M, Vavrek D, Neradilek MB, Polissar N.
A Path Analysis of the Effects of the Doctor-patient Encounter and Expectancy in an Open-label
Randomized Trial of Spinal Manipulation for the Care of Low Back Pain
BMC Complement Altern Med. 2014 (Jan 13); 14: 16Davis, MA, Sirovich, BE, and Weeks, WB.
Utilization and Expenditures on Chiropractic Care
in the United States from 1997 to 2006
Health Serv Res. 2010 (Jun); 45 (3): 748-761
Return to LOW BACK PAIN
Return to WHAT IS USUAL CARE?
Since 4–06–2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |