

Dose-response and Efficacy of Spinal Manipulation
for Care of Chronic Low Back Pain:
A Randomized Controlled TrialThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Spine J. 2014 (Jul 1); 14 (7): 1106–1116 ~ FULL TEXT
OPEN ACCESS Mitchell Haas, DC, Darcy Vavrek, ND, David Peterson, DC,
Nayak Polissar, PhD, Moni B. Neradilek, MS
Center for Outcomes Studies,
University of Western States,
2700 NE 132nd Ave.,
Portland, OR 97230, USA.
haasmitch@comcast.net.
BACKGROUND CONTEXT: There have been no full-scale trials of the optimal number of visits for the care of any condition with spinal manipulation.
PURPOSE: To identify the dose-response relationship between visits to a chiropractor for spinal manipulation and chronic low back pain (cLBP) outcomes and to determine the efficacy of manipulation by comparison with a light massage control.
STUDY DESIGN/SETTING: Practice-based randomized controlled trial.
PATIENT SAMPLE: Four hundred participants with cLBP.
OUTCOME MEASURES: The primary cLBP outcomes were the 100-point modified Von Korff pain intensity and functional disability scales evaluated at the 12- and 24-week primary end points. Secondary outcomes included days with pain and functional disability, pain unpleasantness, global perceived improvement, medication use, and general health status.
METHODS: One hundred participants with cLBP were randomized to each of four dose levels of care: 0, 6, 12, or 18 sessions of spinal manipulation from a chiropractor. Participants were treated three times per week for 6 weeks. At sessions when manipulation was not assigned, they received a focused light massage control. Covariate-adjusted linear dose effects and comparisons with the no-manipulation control group were evaluated at 6, 12, 18, 24, 39, and 52 weeks.
RESULTS: For the primary outcomes, mean pain and disability improvement in the manipulation groups were 20 points by 12 weeks and sustainable to 52 weeks. Linear dose-response effects were small, reaching about two points per six manipulation sessions at 12 and 52 weeks for both variables (p<.025). At 12 weeks, the greatest differences from the no-manipulation control were found for 12 sessions (8.6 pain and 7.6 disability points, p<.025); at 24 weeks, differences were negligible; and at 52 weeks, the greatest group differences were seen for 18 visits (5.9 pain and 8.8 disability points, p<.025).
CONCLUSIONS: The number of spinal manipulation visits had modest effects on cLBP outcomes above those of 18 hands-on visits to a chiropractor. Overall, 12 visits yielded the most favorable results but was not well distinguished from other dose levels.
TRIAL REGISTRATION: ClinicalTrials.gov NCT00376350
KEYWORDS: Chiropractic; Chronic low back pain; Dose-response; Randomized controlled trial; Spinal manipulation
From the FULL TEXT Article:
Introduction
It has long been known that low back pain is a prevalent and costly condition [1, 2], and that chiropractors provide the vast majority of spinal manipulation [3] and treat a large proportion of low back pain in the US. [4] It is therefore important to determine the optimal quantity of spinal manipulative therapy (SMT), particularly for chronic low back pain (cLBP). [5]
Recommendations for duration and frequency of SMT/chiropractic care for cLBP have varied widely and have long been based on clinical experience and opinion. [6] In the early 1990's, a multidisciplinary RAND panel found that opinion was too varied to come to a formal evidence-based consensus (2 to 24 weeks of care, 1 to 5 visits per week), but on average members expected the typical patient to improve in 4 to 6 weeks with 3 visits per week. [7] In contrast, an all-chiropractic RAND expert panel recommended 30 visits over 14 weeks. [8] Shekelle et al [3] noted a range of 1 to 19 visits in published studies of chiropractic care. Later, Nyiendo et al [9] found a mean of 6.7 visits (SD = 7.5, range = 1 to 56) in a practice-based cohort of 526 nonspecific cLBP patients.
To this day, there is no consensus on the efficacy of SMT and its role in the care of cLBP. Some systematic reviews have reported quality evidence in support of SMT [10, 11], while others including the latest Cochrane review found SMT to be no better than other interventions. [12] Results of systematic reviews, whether meta-analysis or best-evidence synthesis, may depend on the quantity of care used in the trials included in the reviews. Investigators have had virtually no evidence from dose-response trials to inform the number of SMT sessions provided.
Because of the dearth of evidence for duration and frequency of care, we conducted the first pilot randomized trial evaluating dose-response of SMT (n=72). [5] We found a clinically important association between number of visits to a chiropractor (1 to 4 weekly visits for 3 weeks) and short-term pain and disability relief showing that a higher number of visits yielded more favorable results. We have subsequently conducted the current 5–year study, the first full-scale dose-response trial with the aim of identifying optimal care of cLBP with SMT and informing the design of comparative effectiveness studies. We also evaluated the efficacy of the SMT dose levels by testing the hypothesis of no difference between SMT and a hands-on control. The trial evaluated the unique contribution of SMT to outcomes beyond the effects of a light massage to control attention (quantity of visits) and touching the patient, as well as history and context. [13]
Methods
Design
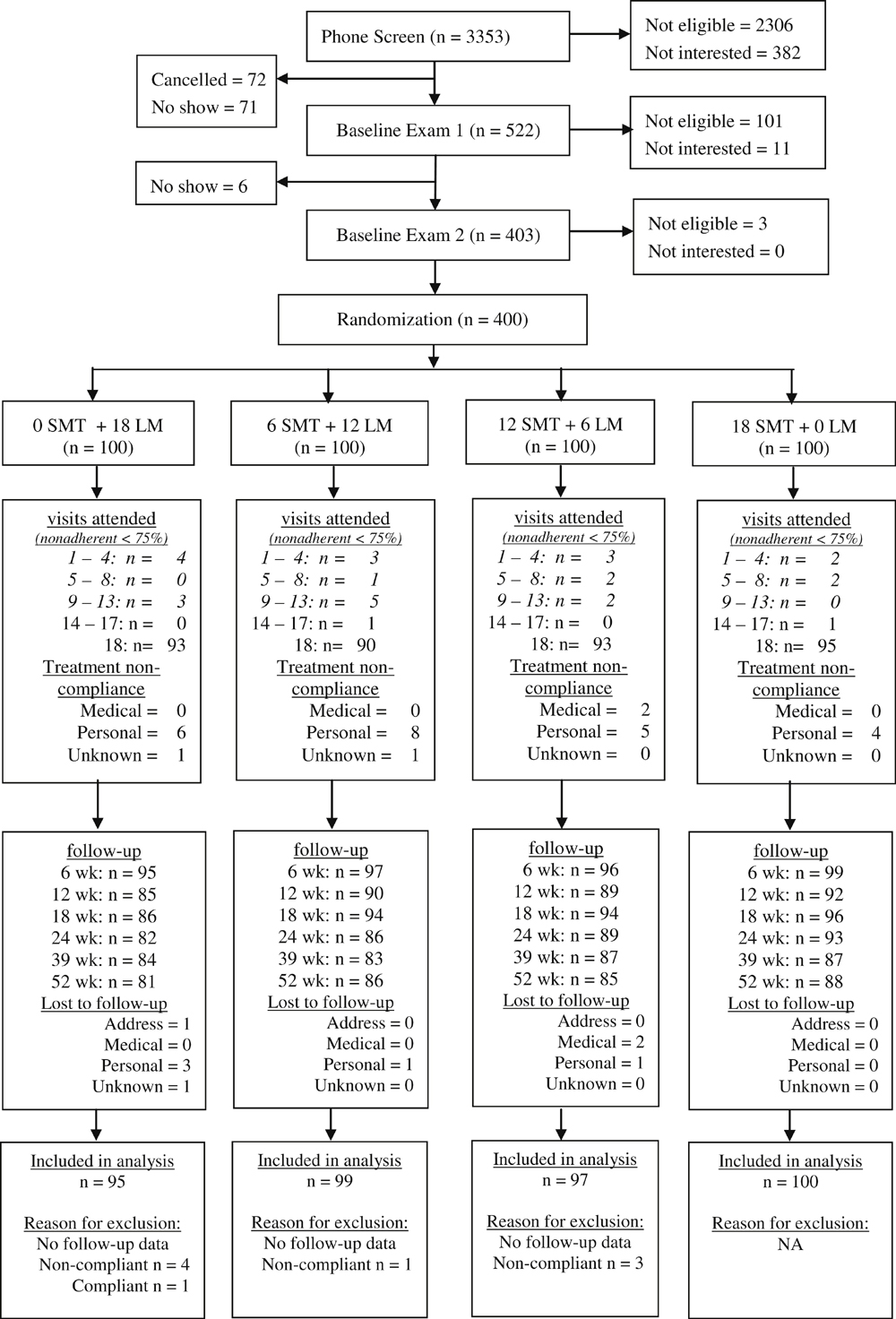
Figure 1 In a prospective open-label, randomized controlled trial, 400 participants with nonspecific cLBP were randomized to receive a dose of 0, 6, 12, or 18 SMT sessions from a chiropractor. All participants were assigned 18 treatment visits, three per week for six weeks. SMT was performed at the assigned number of visits, and a brief light massage control was performed at non-SMT visits to control provider attention and touching the participants. [14] For example, those receiving 12 visits for SMT received 6 visits for light massage from the chiropractor (Figure 1). Follow-up evaluation was by mailed questionnaire or blinded phone interview at 6, 12, 18, 24, 39, and 52 weeks after randomization. The primary outcomes were prespecified as self-reported pain intensity and functional disability at the 12 and 24–week endpoints. The primary endpoints were chosen to emphasize a short-term and a long-term post treatment time point.
Randomization was conducted using computer-generated design adaptive allocation [15, 16] to balance six baseline variables across groups: pain and disability scores, age, gender, relative confidence in SMT and massage, and any previous SMT or massage care. Allocation to study groups was hence concealed from all study personnel and participants by requiring entry of data into the computer program collected immediately before randomization (pain, disability, and confidence in treatment success). Patient coordinators called in the allocation variables over the phone to research staff that entered the data into the allocation computer program. The patient coordinator then assigned the participant to group by placing an unmarked sealed envelope identifying care in the patient's clinic file. Participants and treating clinicians were not blinded to intervention after randomization. However, patient coordinators, who collected some outcomes by phone interview, remained blinded to group assignment throughout the study.
Protocol overview
Participants were recruited through craigslist, mailers, and local newspapers. They were informed the study was investigating 18 visits for different combinations of two manual therapies for cLBP. Preliminary screening was conducted through telephone interview by study staff. At the first baseline visit, participants signed an informed consent form and filled out a baseline survey. Eligibility screening examinations were then conducted at a central university clinic by one of two licensed chiropractors (faculty with more than 20 years of experience) using history, physical exam, and lumbar x-rays. [17]
Eligible participants selected a convenient clinic for study care. Care was provided by one of 12 licensed chiropractors with four to 24 years of experience in nine Portland-area clinics. The treating chiropractors were selected because their abilities were known to the authors and some had previous experience on our trials. Following a second baseline survey at the clinic, participants were given a brief, confirmatory screening examination by the treating clinician. They were then randomized and received their first treatment. Participants were compensated for each treatment visit, mailed questionnaires, and phone interviews ($10 to $20). Participants signed an informed consent form.
Participants
Participants were required to be at least 18 years old and have a current episode of cLBP [18] of mechanical origin [19] of at least three months duration. [3] They were further required to have had some LBP on 30 days in the prior six weeks and a minimum LBP index of 25 on a 100–point scale to prevent floor effects. Participants were excluded if they received manual therapy within the previous 90 days, or for contraindications to study interventions [17, 20] and complicating conditions such as active cancer, spine pathology, inflammatory arthropathies, autoimmune disorders, anti-coagulant conditions, neurodegenerative diseases, pain radiating below the knee, organic referred pain, pregnancy, and disability compensation.
Intervention
Each visit was 15 minutes long with a treating chiropractor, consistent with chiropractic practice. [21] Participants received a hot pack for five minutes to relax spinal muscles followed by five minutes for the SMT or control intervention. The visit was completed with five minutes of very low dose pulsed ultrasound (20% duty cycle with 0.5 watts/cm2). This was used as a quasi-sham to enhance treatment credibility and adherence to care. [13]
SMT consisted of manual thrust (high velocity low amplitude) spinal manipulation in the lumbar and transition thoracic regions, predominantly in the side-posture position. [22] Specific manipulations to be performed were determined at each visit by the chiropractor through ongoing evaluation of the participants including patient progress, self-reported and provocative pain, spinal range of motion, and palpation of the spine and paraspinal soft tissue. [17, 22] Manipulation was not performed at a visit, if the treating chiropractor failed to find any indication. Lighter thrust manipulation including use of mechanical assistance of a spring-loaded table and segmental, low velocity mobilization were permitted in the case of acute exacerbation of the lumbar spine pain. [22]
The light massage control consisted of five minutes of gentle effleurage and petrissage of the low back (lumbar and lower thoracic) paraspinal muscles [22, 23], focused on the symptomatic areas. The massage used was gentler and of shorter duration than recommended for therapeutic massage practice. [21, 24] As such, it was a minimalist intervention to control touching the patient; it was not a formal sham. The treating chiropractors were also asked to render SMT and control intervention with equal enthusiasm to help balance expectations of treatment success imparted by the practitioner. Protocol standardization and provider equipoise across treatment groups were maintained through quarterly training and monitored by office observation and patient phone interview. [14, 25]
Outcomes and Baseline Variables
This report emphasizes the pre-specified primary outcomes, the self-reported Modified Von Korff pain and disability scales validated by Underwood et al. [26] The pain score is the average of three 11–point numeric rating scales converted to a 100–point scale: back pain today, worst back pain in the last four weeks, and average back pain in the last four weeks. The disability score is also the average of three scales: interference with daily activities, social and recreational activities, and the ability to work (outside or around the house).
Secondary outcomes included pain unpleasantness [27], Physical and Mental Component Summary Scales of the SF-12 [28], Health State visual analog scale from EuroQol [29], perceived pain and disability improvement, and the number of the following in the prior four weeks: days with pain and disability, and medication use. Additional baseline variables included demographics, Fear-Avoidance Beliefs Questionnaire, [30] confidence in treatment success [14], and any from a list of comorbid conditions (arthritis, asthma or allergies, gastrointestinal problems, gynecological problems, hypertension, or other chronic condition). [31]
Statistical analysis
An intention-to-treat analysis was conducted with each participant included in the original allocation group and missing data imputed using linear interpolation then last datum carried forward. Nine participants were omitted from the analysis because they had no follow-up data. A sensitivity analysis with all missing data excluded was conducted for the two primary outcomes.
The prespecified primary analysis consisted of regression models to 1) identify the linear effect of SMT dose (slope = outcome increment / 6 SMT sessions) and 2) compare each SMT group to the no-SMT control group (adjusted mean differences). Zellner's seemingly unrelated (simultaneous) regression was used to model outcomes for the individual time points. [32, 33] In addition, for the primary outcomes only, longitudinal effects across all follow-ups were modeled with generalized estimating equations utilizing unstructured correlation to account for within-person correlation between time points [33]. Slopes and group comparisons were adjusted for the six baseline balancing variables used to randomize the participants [15, 16]: pain and disability scores, age, gender, relative confidence in SMT and massage, and any previous SMT or massage care. The baseline value of the outcome measure was added as a covariate if not already included among the six balancing variables.
In a prespecified secondary “responder” analysis, the two primary outcomes were dichotomized to show the proportion of participants with 50% improvement. The analysis above was then repeated using binomial regression to identify slopes and group differences in proportion of responders. [33]
The sample size was determined a priori to have at least 80% power to detect a between-groups effect of 10 of 100 points in the two primary outcomes using a two-tailed test. It took into consideration a 10% dropout rate. The .025 level of significance was used to adjust for having two primary outcomes. Detection of a 10 point between-group difference was chosen to be consistent with our past studies. [31, 34] All analyses were conducted with Stata 11.2 (StataCorp, College Station, TX).
Administration
The study was approved by the University of Western States Institutional Review Board (FWA 851). The trial was registered at ClinicalTrials.gov NCT00376350. This study was funded by the National Center for Complementary and Alternative Medicine (NCCAM), National Institutes of Health (U01 AT001908). The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the official views of NCCAM. The authors declare no conflicts of interest.
Results
Participants were enrolled from March 2007 to May 2010 and followed for one year with the last follow-up ending May 2011. Allocation was equally spread out across clinics and providers with group assignments averaging 25% (SD = 6%) per group per clinic and 25% (SD = 12%) per group per treating physician.
The study flowchart in Fig. 1 shows strong adherence to care with 90% to 95% of participants attending all 18 study visits. Four participants, allocated to 18 SMT sessions and who attended all 18 visits, collectively had five treatment visits where SMT was deemed inappropriate and withheld per protocol. Three had SMT withheld at one visit because it was not indicated and two received mobilization at one visit because of acute exacerbation. There was one violation of protocol where a patient accidentally received 13 SMT visits instead of 12. Compliance with data collection was greater than 80% for all follow-up time points. Nine participants were completely lost to follow-up.
Medication use and care from a non-study provider for cLBP were balanced across groups at each time point. During the treatment phase, 93% to 97% of participants in each treatment arm refrained from professional care outside the study and 94% to 95% abstained from prescription medication. Thereafter, approximately three-fourths reported no outside professional care at each follow-up; the maximum difference between groups ranged from 4% to 11% of participants. Also, 90% refrained from prescription medication at each follow-up with maximum group differences ranging from 1% to 8%. Nonprescription analgesics were balanced across groups. Confidence in the success of the two interventions was approximately equal and balanced across groups.

Table 1

Table 2
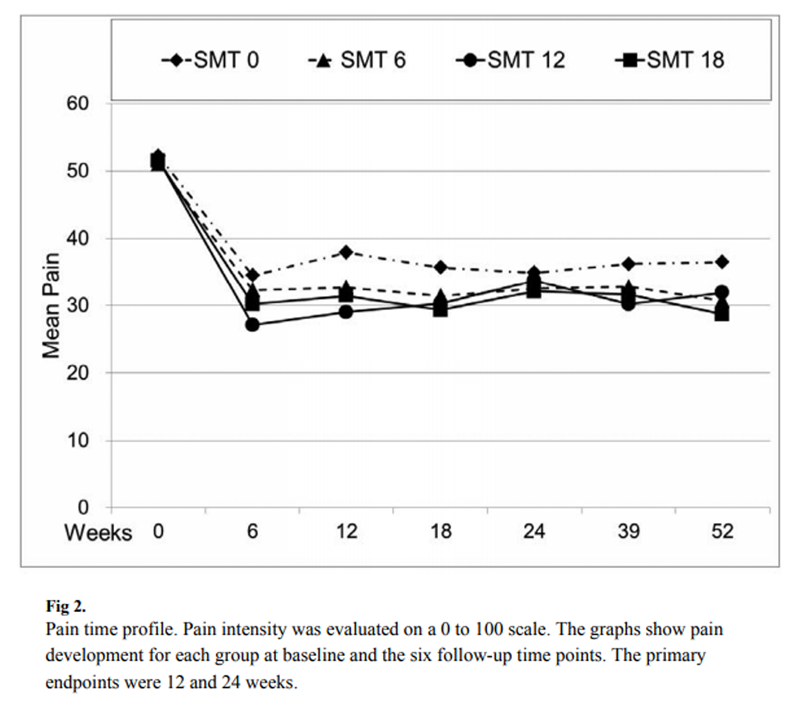
Figure 2
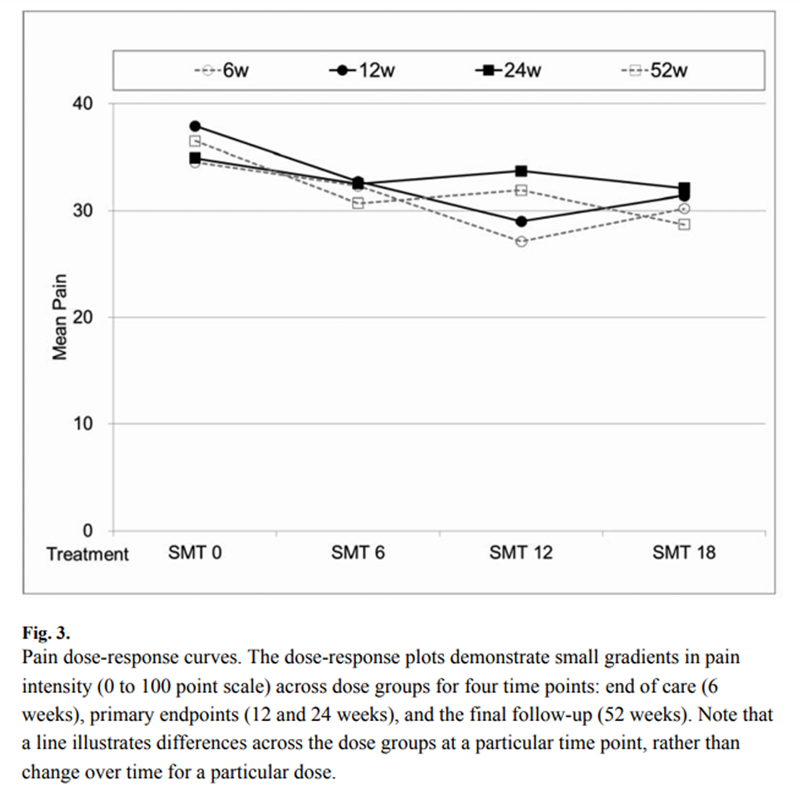
Figure 3
Baseline characteristics (Table 1) were balanced across groups with the exception of smoking; inclusion of smoking in the analysis produced no substantive changes in effect sizes. The mean age was 41.3 years and most participants were white non-Hispanic. Half of the participants reported the following characteristics: female, college degree, comorbidity, and experience with a study intervention. The mean duration of LBP was 11.8 years. The average participant experience LBP 6 days per week and took medication for it twice per week.
Pain
Pain improved by the end of treatment and was durable up to 52 weeks after randomization for all groups (Table 2 and Figure 2). Mean pain reduction within groups reached over 20 points for SMT treatment arms.
Adjusted slopes and mean differences (AMD) with confidence intervals are presented in Table 2 for the primary analysis. A small statistically significant linear dose-response effect in pain intensity across the treatment levels was observed at the 12–week primary endpoint (2.2 points per 6 visits, P = .007) but not the 24–week primary endpoint (0.6 points per 6 visits). Slopes were small at the other time points as well (1.6 to 2.0). Overall, there were minimal differences between adjacent dose groups at all time points (Figure 3).
At 12 weeks, the maximum pain difference between treatment and no-SMT control was observed for 12 SMT visits (AMD = 8.6, P =.002); at 24 weeks, there were no meaningful differences from the control (AMD < 2.5). For the secondary time points, a notable effect was observed at 52 weeks; here, 18 SMT visits showed the greatest advantage over the control (AMD = 7.6, P = .011). Analyses of the three pain score components gave similar results and are available from the authors.
Repeated-measures analysis of the full 6 to 52–week pain profile demonstrated a small advantage of treatment over control. The largest effect was observed for 12 SMT visits versus control (AMD = 5.3, P = .011).
Functional disability
Mean functional disability reduction reached 20 points. Trends in slopes and group comparisons were similar to those for pain, but smaller in magnitude with fewer statistically significant results (Table 2). At the 12–week primary endpoint, the greatest advantage for SMT over control was also found for 12 SMT visits (AMD = 7.5, P = .011) and at the 24–week primary endpoint, there were no clinically meaningful effects (AMD < 3.4). At 52 weeks, 18 SMT visits was observed to have the greatest effect (AMD = 8.8, P = .002). As for pain, there were no clinically meaningful differences in disability profiles between 12 and 18 SMT visits.
Sensitivity analysis
There were no material changes in the results for pain and disability outcomes when imputed data were excluded from the analysis. For the primary endpoints, changes were ? 0.3 in slope and ? 1.4/100 points in group differences. The changes at other time points were similarly negligible. Clustering by care provider or clinic produced no substantive changes in effect sizes.
Responder Analysis
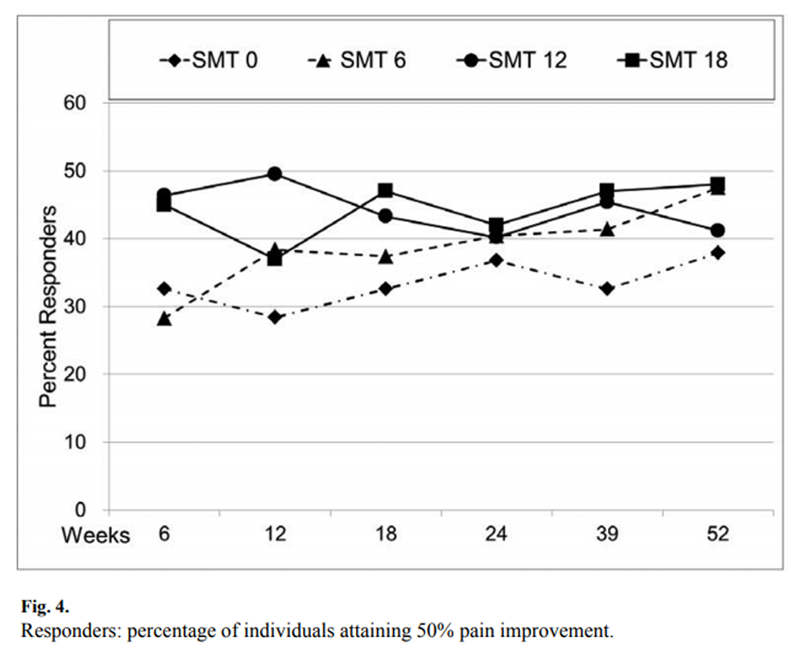
Figure 4

Table 3

Table 4 The responder profile in Figure 4 and Table 3 shows about 30% to 50% of individuals in each group achieved 50% pain improvement at each time point. Only one statistically significant difference between treatment and control was found. At 12–weeks, a substantial proportion of response to care was attributable to manipulation for 12 SMT visits (21.1%, P = .002). This difference corresponds to a number needed to treat = 5. For functional disability, about 40% to 60% of individuals were responders for all groups and time points. However, there were no statistically significant group differences.
Secondary outcomes
Generally, there was within-group improvement in secondary outcomes recorded at the end of care showing the same durability for these outcomes as for pain outcomes. However, the improvement in the no-SMT control group was of such magnitude that there were few sizable, statistically significant differences between treatment and control groups (Table 4).
Days with pain and disability were reduced from baseline by one to two days per week. Perceived pain and disability improvement was typically rated as “better.” The standardized SF-12 physical health component improved about 7 to 10 points (up to one standard deviation), returning to U.S. population norms in 3 to 6 months. The mental health component deviated little from population norms at baseline. EuroQol's Health State visual analog scale showed little change from baseline. There was a small decrease in medication use following end of care. The mean reductions in pain unpleasantness scores were similar to pain score reduction, about 20 points.
Adverse events
There were no notable adverse events. Three persons reported seeking care for symptomatic relief of low back pain exacerbation related to the study. One ineligible person subsequently reported increase of pain following the screening examination. One participant in the 12-SMT group lost several days of work followed by complete resolution or the episode during the treatment phase. One participant in the 12-SMT group dropped out after an exacerbation associated with lifting a child.
Discussion
This first full-scale dose-response study of SMT had several notable findings. Based on the pain and functional disability primary outcomes, 12 sessions of SMT yielded the overall best, albeit modest, treatment effects (group differences). This was particularly noted in the short term at the 12–week primary endpoint. Group differences were negligible at the 24–week primary endpoint and favored 18 SMT sessions to a small degree in the long term, at 52 weeks. In general, the data were consistent with a dose-response relationship being saturated at 12 sessions with little or no additional benefit attributable to additional SMT visits, even at 52 weeks. Analysis of the full time profile supported no additional benefit overall of 18 over 12 sessions. In addition, responder analysis gave additional support for some advantage of 12 visits, but only in the short term.
The linear dose-response gradients for the primary outcomes were small in general, reaching approximately 2/100 scale points per six sessions of SMT at 12 and 52 weeks. Even excluding the highest dose group for short-term results, the gradient would only double to about 4/100 scale points per six SMT sessions. The fact that there was little difference between adjacent dose groups makes it difficult to recommend one treatment dose over another. However, two considerations come into play. First, the effects across dose accumulate to modest benefit of SMT above the hands-on control. Second, an aim of the study was to find a saturation dose level for use in future studies. The time profiles, dose-response gradients, and comparisons to the control group suggest in aggregate that 12 visits would the best choice, particularly for short-term improvement.
Interpretation of the dose-response effects requires consideration of several factors. This was a fastidious randomized trial designed to isolate the effects of SMT. We controlled number of visits, time with the participant, effects of touching the patient, patient-provider interaction, and intervention credibility. This was accomplished with 18 visits of hands-on therapy and electronic modality (minimal ultrasound) for all groups. The specific and contextual effects of light massage at non-SMT visits, ultrasound, or simply 18 visits to a healthcare provider potentially obfuscated a larger dose-response gradient that might be found in clinical practice. For example, such larger effects were seen in our pilot study where participants attended only visits for the active intervention. [5]
In terms of efficacy, the light massage control is technically a comparison intervention rather than a true sham. Many sessions with even a minimal massage may have more effect than one might expect. As such, the differences between SMT and the control may be somewhat smaller than for a comparison with a sham manipulation. We did not attempt to use a sham for two reasons. First, it would be virtually impossible to blind participants because half received visits for both treatment and control and could compare interventions. Second, we wanted to avoid some disappointment that can arise when participants think they may be receiving sham intervention.v All participants were scheduled to receive their assigned dose of SMT. There were no treatment stoppage rules based on improvement during the care period. The effects of care stoppage are unknown, and could be either beneficial or detrimental to outcomes in the short and long term.
Another issue is the threshold of a clinically important difference between groups for the continuous-variable primary outcomes. Studies on patient-rated minimal important change have lead some authors to conclude that 30% improvement (about 15 to 20/100 points) can be considered a robust indicator of within-person minimal clinically important change for these outcomes. [35] A 50% improvement has been recommended as a success threshold for the individual. [36] However, Dworkin et al [37] point out that these numbers do not apply to between-groups effects, and identifying meaningful group differences is a multi-factorial process that is far from straightforward. The between-group differences of 8.6 in pain and 7.5 in disability scores at a primary endpoint are certainly marginal, but it is not clear yet whether effects of this magnitude constitute a degree of clinical relevance. The associated number needed to treat for pain (= 5) may actually indicate a meaningful effect. [12, 38]
Conclusion
Overall, 12 sessions of spinal manipulation in six weeks from a chiropractor yielded the most favorable pain and functional disability improvement for chronic, non-specific low back pain. Mean participant improvement for this group was substantial at the end of care and sustainable to 52 weeks. Approximately half of patients would be expected to achieve 50% improvement in pain/disability. Therefore, 12 sessions of SMT is the current best estimate for use in comparative effectiveness trials. However, the recommendation is made with caution because the gradient of treatment effects across dose groups was too small to clearly distinguish 12 visits from adjacent dose levels. Even with 12 visits, the contribution of SMT to outcomes beyond that of a focused light massage delivered by a chiropractor (hands-on control) was at best modest at the 12–week primary endpoint and negligible at the 24–week primary endpoint.
Supplementary Material
Acknowledgments
This study was funded by the National Center for Complementary and Alternative Medicine (NCCAM), National Institutes of Health (U01 AT001908).
The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the official views of NCCAM. The authors declare no conflicts of interest.
References:
Andersson, G.B.J.
Epidemiological features of chronic low-back pain.
Lancet. 1999; 354: 581–585Leigh, J.P., Markowitz, S.B., Fahs, M. et al.
Occupational injury and illness in the United States.
Arch Intern Med. 1997; 157: 1557–1568Shekelle, P., Adams, A., Chassin, M. et al.
Spinal manipulation for low-back pain.
Ann Intern Med. 1992; 117: 590–598Waddell, G.
Low back pain: a twentieth century health care enigma.
Spine. 1996; 21: 2820–2825Haas, M., Groupp, E., and Kraemer, D.F.
Dose-response for Chiropractic Care of Chronic Low Back Pain
Spine J 2004 (Sep); 4 (5): 574–583Shekelle, P.G., Adams, A.H., Chassin, M.R. et al.
The Appropriateness of Spinal Manipulation for Low-Back Pain.
Project Overview and Literature Review
RAND Corp., Santa Monica, CA; 1991Shekelle, P.G., Adams, A.H., Chassin, M.R. et al.
The Appropriateness of Spinal Manipulation for Low-back Pain:
Indications and Ratings by a Multidisciplinary Expert Panel
RAND, Santa Monica, CA; 1991Shekelle, P.G., Adams, A.H., Chassin, M.R. et al.
The appropriateness of spinal manipulation for low-back pain:
indications and ratings by an all-chiropractic expert panel
RAND, Santa Monica, CA; 1992Nyiendo J, Haas M, Goldberg B, Sexton G.
Patient Characteristics and Physicians' Practice Activities for
Patients with Chronic Low Back Pain: A Practice-based Study
of Primary Care and Chiropractic Physicians
J Manipulative Physiol Ther 2001 (Feb); 24 (2): 92–100Bronfort, G, Haas, M, Evans, R, Kawchuk, G, and Dagenais, S.
Evidence-informed Management of Chronic Low Back Pain
with Spinal Manipulation and Mobilization
Spine J. 2008 (Jan); 8 (1): 213–225Chou R, Huffman LH; American Pain Society.
Nonpharmacologic Therapies for Acute and Chronic Low Back Pain:
A Review of the Evidence for an American Pain Society/
American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 492–504Rubinstein, S.M., van Middelkoop, M., Assendelft, W.J. et al.
Spinal manipulative therapy for chronic low-back pain: an update of a Cochrane review.
Spine. 2011; 36: E825–E846Kaptchuk TJ.
The Placebo Effect in Alternative Medicine:
Can the Performance of a Healing Ritual Have Clinical Significance?
Annals of Internal Medicine 2002 (Jun 4); 136 (11): 817–825Haas M, Spegman A et al. (2010)
Dose Response and Efficacy of Spinal Manipulation for Chronic Cervicogenic Headache:
A Pilot Randomized Controlled Trial
Spine J. 2010 (Feb); 10 (2): 117–128Begg, C.B. and Iglewicz, B.
A treatment allocation procedure for sequential clinical trials.
Biometrics. 1980; 36: 81–90Aickin, M.
Randomization, balance, and the validity and efficiency of design—adaptive allocation methods.
J Stat Plan Inference. 2001; 94: 97–119Gatterman, M.I. and Panzer, D.M.
Disorders of the lumbar spine.
in: M.I. Gatterman (Ed.) Chiropractic management of spine related disorders.
Williams & Wilkins, Baltimore, MD; 1990: 129–175Anderson, J.A.D.
Problems of classification of low-back pain.
Rheumatol Rehabil. 1977; 16: 34–36DiFabio, R.P., Mackey, G., and Holte, J.B.
Physical therapy outcomes for patients receiving workers' compensation following treatment for herniated lumbar disc and mechanical low back pain syndrome.
J Orthop Sports Phys Ther. 1996; 23: 180–187Belanger, A.
Ultrasound.
in: A. Belanger (Ed.) Evidence-based guide to therapeutic physical agents.
Lippincott Williams & Wilkins, Philadelphia, PA; 2002: 223–261Cherkin, D.C., Deyo, R.A., Sherman, K.J. et al.
Characteristics of licensed acupuncturists, chiropractors, massage therapists and naturopathic physicians.
J Am Board Fam Pract. 2002; 15: 463–472Peterson, D.H. and Bergmann, T.F.
Chiropractic technique: principles and practice. 2nd ed.
Mosby, St Louis, MO; 2002Nicholson, G.G. and Clendaniel, R.A.
Manual techniques.
in: R.M. Scully, M.R. Barnes (Eds.)
Physical therapy. J.B. Lippincott Company, Philadelphia, PA; 1989: 926–985Furlan, A.D., Brosseau, L., Imamura, M., and Irvin, E.
Massage for low back pain: a systematic review within the framework of the Cochrane collaboration back review group.
Spine. 2002; 27: 1896–1910Haas, M., Aickin, M., and Vavrek, D.
A path analysis of expectancy and patient-provider encounter in an open-label randomized controlled trial of spinal manipulation for cervicogenic headache.
J Manipulative Physiol Ther. 2010; 33: 5–13Underwood, M.R., Barnett, A.G., and Vickers, M.R.
Evaluation of two time-specific back pain outcome measures.
Spine. 1999; 24: 1104–1112Price, D.D.
Psychological mechanisms of pain and analgesia.
IASP Press, Seattle, WA; 1999Ware, J.E., Kosinski, M., and Keller, S.D.
A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity.
Med Care. 1996; 34: 220–233Luo, N., Johnson, J.A., Shaw, J.W. et al.
Self-reported health status of the general adult U.S. population as assessed by the EQ-5D and Health Utilities Index.
Med Care. 2005; 43: 1078–1086Waddell, G., Newton, M., Henderson, I. et al.
A fear-avoidance beliefs questionnaire (FABQ) and the role of fear avoidance beliefs in chronic low back pain and disability.
Pain. 1993; 52: 157–168Nyiendo, J., Haas, M., Goldberg, B., and Sexton, G.
Pain, disability and satisfaction outcomes and predictors of outcomes: a practice-based study of chronic low back pain patients attending primary care and chiropractic physicians.
J Manipulative Physiol Ther. 2001; 24: 433–439Zellner, A.
An efficient method of estimating seeming unrelated regressions and tests for aggregation bias.
J Am Stat Assoc. 1962; 57: 348–368StataCorp.
Stata: release 11.2 statistical software.
Stata Corporation, College Station, TX; 2009Haas M, Groupp E, Panzer D, Partna L, Lumsden S, Aickin M
Efficacy of Cervical Endplay Assessment
as an Indicator for Spinal Manipulation
Spine (Phila Pa 1976) 2003 (Jun 1); 28 (11): 1091–1096Ostelo, R.W., Deyo, R.A., Stratford, P. et al.
Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change.
Spine. 2008; 33: 90–94Fritz, J.M., Hebert, J., Koppenhaver, S., and Parent, E.
Beyond minimally important change: defining a successful outcome of physical therapy for patients with low back pain.
Spine. 2009; 34: 2803–2809Dworkin, R.H., Turk, D.C., McDermott, M.P. et al.
Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations.
Pain. 2009; 146: 238–244Froud, R., Eldridge, S., Lall, R., and Underwood, M.
Estimating the number needed to treat from continuous outcomes in randomised controlled trials: methodological challenges and worked example using data from the UK Back Pain Exercise and Manipulation (BEAM) trial.
BMC Med Res Methodol. 2009; 9: 35
Return to LOW BACK PAIN
Since 5-27-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |