Adding Chiropractic Manipulative Therapy to Standard Medical
Care for Patients with Acute Low Back Pain: Results of a
Pragmatic Randomized Comparative Effectiveness StudyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Spine (Phila Pa 1976). 2013 (Apr 15); 38 (8): 627–634 ~ FULL TEXT
Christine M. Goertz, DC, PhD; Cynthia R. Long, PhD; Maria A. Hondras, DC, MPH;
Richard Petri, MD; Roxana Delgado, MS; Dana J. Lawrence, DC, MMedEd, MA;
Edward F. Owens, MS, DC; William C. Meeker, DC, MPH
Palmer Center for Chiropractic Research,
Davenport, IA 52803, USA.
christine.goertz@palmer.edu
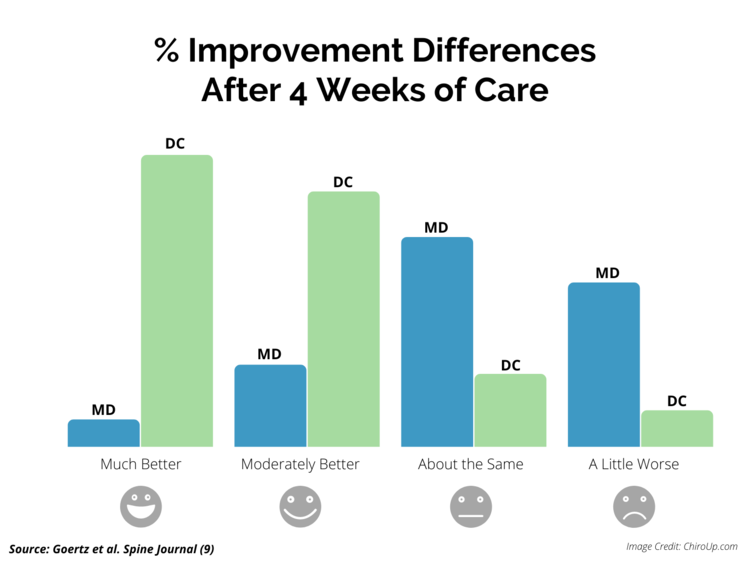
FROM: ChiroUP 2021, Goertz et. al, Spine J 2013STUDY DESIGN: Randomized controlled trial.
OBJECTIVE: To assess changes in pain levels and physical functioning in response to standard medical care (SMC) versus SMC plus chiropractic manipulative therapy (CMT) for the treatment of low back pain (LBP) among 18 to 35–year-old active-duty military personnel.
SUMMARY OF BACKGROUND DATA: LBP is common, costly, and a significant cause of long-term sick leave and work loss. Many different interventions are available, but there exists no consensus on the best approach. One intervention often used is manipulative therapy. Current evidence from randomized controlled trials demonstrates that manipulative therapy may be as effective as other conservative treatments of LBP, but its appropriate role in the healthcare delivery system has not been established.
METHODS: Prospective, 2–arm randomized controlled trial pilot study comparing SMC plus CMT with only SMC. The primary outcome measures were changes in back-related pain on the numerical rating scale and physical functioning at 4 weeks on the Roland-Morris Disability Questionnaire and back pain functional scale (BPFS).
RESULTS: Mean Roland-Morris Disability Questionnaire scores decreased in both groups during the course of the study, but adjusted mean scores were significantly better in the SMC plus CMT group than in the SMC group at both week 2 (P < 0.001) and week 4 (P = 0.004). Mean numerical rating scale pain scores were also significantly better in the group that received CMT. Adjusted mean back pain functional scale scores were significantly higher (improved) in the SMC plus CMT group than in the SMC group at both week 2 (P < 0.001) and week 4 (P = 0.004).
CONCLUSION: The results of this trial suggest that CMT in conjunction with SMC offers a significant advantage for decreasing pain and improving physical functioning when compared with only standard care, for men and women between 18 and 35 years of age with acute LBP.
TRIAL REGISTRATION: is at: ClinicalTrials.gov NCT00632060
Key words: low back pain, chiropractic manipulation, military medicine, physical functioning.
Commentary from Spine-health
When acute low back pain strikes, your goal is fast, lasting relief. One recently published study suggests that spinal manipulation is more effective than pain medication for low back pain relief.
The question remains: should a person suffering from acute low back pain seek standard medical care from a general practitioner in addition to chiropractic manipulation from a chiropractor?
Until recently, there had been no clear consensus on whether standard medical care alone, or standard medical care in conjunction with chiropractic manipulation works best to relieve low back pain. To help answer this question, researchers recently studied active-duty military men and women (ages 18–35) suffering from acute low back pain. The study group had all been experiencing pain for four weeks or less.
The study enrolled a total of 91 patients. One randomly selected group of 46 patients received standard medical care alone.Standard Care Group:
- Focused history and physical examination
- Diagnostic imaging as indicated
- Education about self-management, including maintaining activity levels as tolerated
- Parmacological management with the use of analgesics and anti-inflammatory agents
- Physical therapy and modalities, such as heat/ice
- Pain clinic referral
The remaining 45 patients received a combination of standard medical care plus chiropractic manipulation.
Combination Care Group: The Combination Care Group Received:
- Same standard medical care outlined above from a medical doctor
- High-velocity low-amplitude (HVLA) manipulative therapy from a chiropractor
- Complementary treatments as needed: brief massage, stretching instruction, McKenzie exercises
Investigators measured the results of the two different treatment regiments using the Roland-Morris Disability Questionnaire (RMQ), which rates physical functioning, and the numerical rating scale (NRS), which measures self- reported pain on a scale from 1–11.
Study results indicate that at the end of four weeks:
- Reported pain and disability decreased significantly in both groups.
- Reported pain and disability decreased significantly more in the combination (standard medical care plus chiropractic manipulative therapy) group than in the standard medical care only group.
The results of this study suggest that a combination of both standard medical care and chiropractic manipulation may be a more effective choice for relief of acute lower back pain than standard medical care alone.
An interesting future study would compare a combination of standard medical care plus chiropractic manipulation to chiropractic manipulation therapy alone.
From the FULL TEXT Article:
Background
Low back pain (LBP) is exceedingly common, costly, and a significant cause of long-term sick leave and work loss. [1–4] Lifetime prevalence has been estimated to be as high as 84%, with a median cost per quality-adjusted life year of $13,015. [5, 6]
Manipulative therapy delivered by doctors of chiropractic is commonly used to treat patients with LBP. At least 7.5% of US adults seek care from chiropractors annually, representing approximately 190 million patient visits. [7, 8]
The majority of systematic reviews find that chiropractic manipulative therapy (CMT) seems to reduce pain and disability at least moderately for many patients with LBP. [9–16] Thus, current evidence from randomized trials within controlled settings indicates CMT's potential effectiveness for LBP, but the appropriate role of CMT in treating LBP within the healthcare delivery system has not been delineated. Although more than 200 studies exist evaluating the effects of manipulative therapy for LBP, there are few studies focusing on high-velocity low-amplitude (HVLA) for patients with acute LBP delivered by chiropractors that include a standard medical care (SMC) intervention in both treatment groups, include diverse racial and ethnic populations, and focus on younger adults. [17] Thus, we know very little about the impact of CMT on diverse populations in real-world settings.
The primary aim of this pragmatic, patient-centered comparative effectiveness study was to assess whether the addition of CMT to SMC reduces pain and increases physical functioning compared with only SMC for the treatment of acute LBP.
MATERIALS AND METHODS
Study Design and Setting
This was a prospective, 2–arm randomized controlled trial pilot study comparing CMT plus SMC with only SMC in US active-duty military personnel. The study took place from February 2008 to June 2009 at William Beaumont Army Medical Center (WBAMC), Fort Bliss, El Paso, TX. According to the 2010 Census report, the racial make-up of the area was approximately 72% white, 15% black, 2% Asian, 2% American Indian and Alaska Native, less than 1% Pacific Islander, 9% other races, and 18% Hispanic or Latino. [18]
Participants
Eligibility criteria included male and female US active-duty military personnel between 18 and 35 years of age with acute LBP, defined as LBP of less than 4 weeks duration. Soldiers were excluded if they were relocating or leaving the post within 6 weeks from the day of the screening, had LBP for more than 4 weeks, were pregnant, or had a condition in which CMT was contraindicated.
Interventions
Standard Medical Care The study did not restrict access to SMC or prescribe a SMC delivery protocol. Thus, both groups had normal access to the SMC typically provided to patients with LBP at WBAMC. Standard care included any or all of the following: a focused history and physical examination, diagnostic imaging as indicated, education about self-management including maintaining activity levels as tolerated, pharmacological management with the use of analgesics and anti-inflammatory agents, and physical therapy and modalities such as heat/ice and referral to a pain clinic.
Chiropractic Manipulative Therapy Participants in the group receiving CMT in addition to SMC were scheduled for up to 2 visits weekly with a doctor of chiropractic (DC) for a period of 4 weeks. The initial visit with the DC included a focused history and physical examination and diagnostic imaging as indicated. Treatments consisted of HVLA manipulation as the primary approach in all cases, with ancillary treatments at the doctor's discretion, including brief massage, the use of ice or heat in the lumbar area, stretching exercises, McKenzie exercises, advice on activities of daily living, postural/ergonomic advice; and mobilization. HVLA manipulation involves a single load or impulse "thrust" to body tissues. Patients were placed in a lateral recumbent or side-lying position with the superior or free hip and knee flexed and adducted across the midline. The chiropractor Stabilized the patient's free leg with his own leg while holding the patient's superior shoulder. The manipulative load was applied by using a pisiform contact on the patient's lumbar spine or sacroiliac joint while preventing motion of the patient through stabilizing holds on the shoulder and hip. The single impulse load, or thrust, was delivered by a quick, short controlled movement of the shoulder, arm, and hand combined with a slight body drop.
Outcome Measures
The prespecified primary outcomes for this study were backrelated pain and physical functioning at 4 weeks. Pain was measured using the numerical rating scale (NRS) and physical functioning was measured using the Roland-Morris Disability Questionnaire (RMQ) and the Back Pain Functional Scale. [19] The NRS asks participants to rate their level of pain during the past 24 hours on an ordinal 11–point scale (0 = no LBP; 10 = worst possible pain). The minimal clinically important difference is a change of 2.5 points. [20] The modified RMQ assesses LBP-related disability and the minimal clinically important difference is estimated at 2 to 3.5 points. [21, 22]
Secondary outcomes included patient satisfaction and global improvement. Satisfaction was measured with an 11–point NRS, by asking "How satisfied are you with the overall results of your care?" Responses were anchored with 0 equal to "not at all satisfied" and 10 equal to "extremely satisfied." Patients also were asked to rate improvement on a 7–point Likert scale by rating "Compared with your first visit, your back pain is:" with responses in the range of 1, that indicates "completely gone" to 7, that indicates "much worse." Outcome assessments occurred at baseline, 2 weeks and 4 weeks.
Treatment Allocation
Randomization was achieved via a web-based minimization algorithm that balanced participant age, sex, and prescreen NRS between groups. Treatment allocation was conducted by the project manager through a web interface to the minimization algorithm. All future assignments were concealed. It was not possible to blind the participant or treating clinician to participant group assignment. However, the principal investigator and data analysts were blinded to treatment allocation.
Statistical Methods
Our estimates of the standard deviations for RMQ and NRS were derived from several of our other trials of CMT for LBP. On the basis of this information, a sample size of 50 participants per group was determined for this pilot study. We estimated that this sample size would give us more than 80% power to detect group differences of 3 points on the RMQ. We had more than 70% power to detect differences of 1 point on the NRS and more than 90% to detect differences of 2 points.
Descriptive statistics were used to summarize participant characteristics at baseline for each treatment group. All analyses used an intention-to-treat approach. Linear mixed-effects models were fit for each of the 3 outcome variables over the week 2 and 4 endpoints. Ceneral covariance structures were used in each model to account for within-participant correlation over time. Those who did not provide follow-up data at both 2 and 4 weeks were not included in the analyses. The models were adjusted for age, sex, prescreen NRS, and the baseline value of the respective outcome variable. Adjusted mean differences between the 2 treatment groups and 95% confidence intervals were reported for each final model.
RESULTS
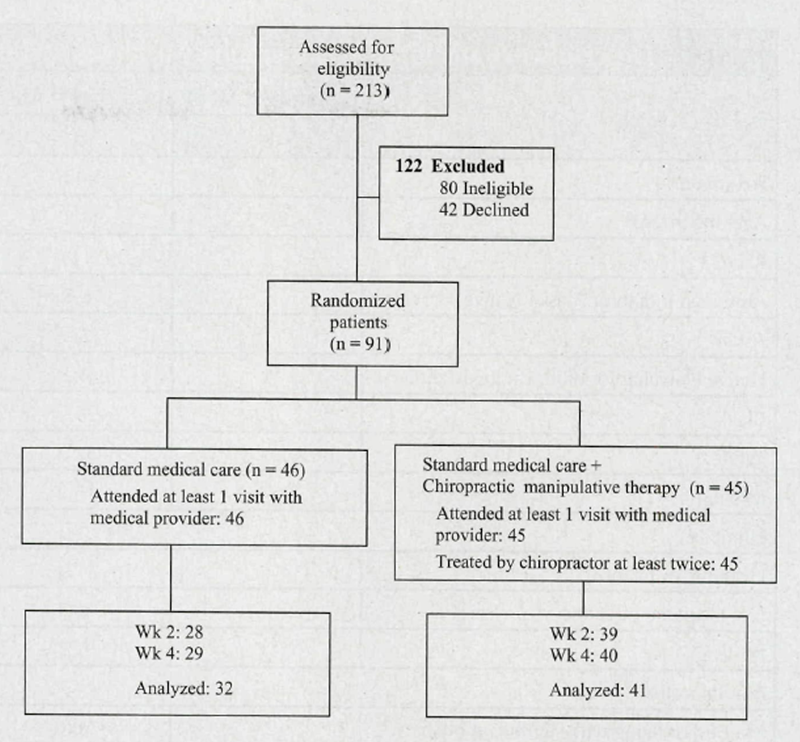
Figure 1

Table 1

Table 2
Screening, Enrollment, and Follow-up Participants were recruited from the Soldier and Family Medical Clinic at WBAMC and throughout Fort Bliss. The recruitment efforts included dissemination of flyers and posters at throughout the clinics, dining facilities, and Army Community Services. We also asked the medical providers for referrals of patients who met eligibility criteria. A total of 213 potential participants were screened for this study and 91 were enrolled (Figure 1). We extended the recruitment period by 3 months in attempt to meet our projected sample size of 100, but concluded recruitment at 91 participants when the grant period ended. Of those excluded, 80 did not meet eligibility criteria and 42 declined participation. A total of 46 participants were randomized to the SMC group and 45 were randomized to the SMC plus CMT group. Follow-up rates were 85% at both endpoints for the SMC plus CMT group and 61% and 63% for the SMC group at weeks 2 and 4, respectively.
Baseline Characteristics
>NR? Study participants had a mean age of 26 years; 86% were male, and 63% were white. The median duration of participant current LBP episode at the time of enrollment was 9 days and 43% had radicular signs. Most participants (71%) reported taking some medication for their back pain during the past week. Participants had a higher expectation of helpfulness for SMC plus CMT compared with only SMC (Tables 1 and 2).
Study Treatments
The number of visits in the SMC group was in the range of 0 to 8, with a mean of 1.4 visits. The majority of participants (n = 24) in this group had only 1 visit. Medications were prescribed for 37% of the participants and included nonsteroidal anti-inflammatory drugs, muscle relaxants, benzodiazepines, analgesic creams, and narcotics. Thirty-three percent were placed on a treatment plan (exercise program, range of motion, stretching and modalities including heat and electrical stimulation) delivered primarily by a physical therapist. Fifty percent were given referrals, with a majority for physical therapy (38%) followed by radiographical evaluation (31%). The SMC group providers were physician assistants (28%), family practice physicians (18%), physical therapists (16%) or aides (12%), nurse practitioners (9%), or specialty providers (physical medicine [3%], athletic trainer [3%], and chiropractor [3%]).
Those assigned to SMC plus CMT had a mean of 1 visit for SMC (range, 0–4) and a median of 7 visits for CMT (range, 2–8). All patients received HVLA. In addition, patients may have received 1 or more of the following services provided by the DC: mobilization, brief massage, use of ice in the lumbar area, stretching exercises, McKenzie exercises, advice for activities of daily living, postural/ergonomic advice. Medications, including nonsteroidal anti-inflammatory drugs, muscle relaxants and narcotics, were prescribed to 18% of the participants in the SMC plus CMT group. Exercises, trigger point therapy, and modalities including heat and electrical stimulation were delivered hy physical therapists to 6 participants.
Rain and Functional Status

Table 3
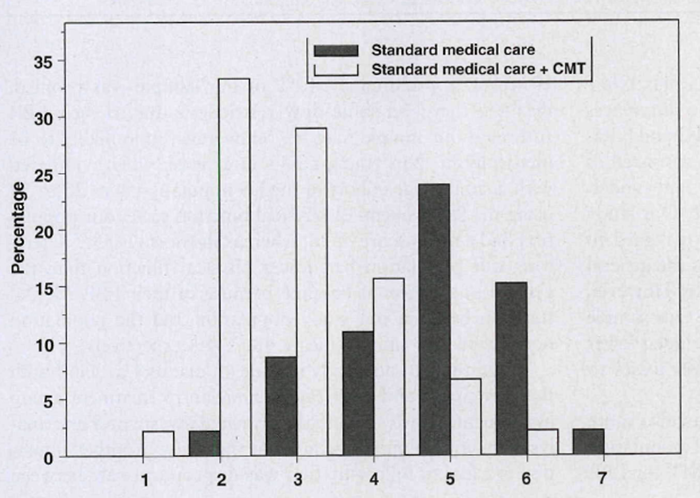
Figure 2

Table 4
Mean RMQ scores decreased in both groups during the course of the study, but adjusted mean scores were significantly better in the SMC plus CMT group than in the SMC group at both week 2 (P < 0.001) and week 4 (P = 0.004) (Table 3). Mean NRS pain scores were also significantly better in the group that received CMT (Table 3). Adjusted mean Back Pain Functional Scale scores were significantly higher (improved) in the SMC plus CMT group than in the SMC group at both week 2 (P < 0.001) and week 4 (P = 0.01) (Table 3).
Secondary Outcomes
Seventy-three percent of participants in the SMC plus CMT group rated their global improvement as pain completely gone, much better, or moderately better, compared with 17% in the SMC group (Figure 2). The mean satisfaction with care score on a 0 to 10 scale for the SMC plus CMT group was 8.9 at both weeks 2 and 4; the mean for the SMC group was 4.5 at week 2 and 5.4 at week 4 (Table 4).
Because of the disproportional loss to follow-up, we did a post hoc evaluation of the possible effects of this on the primary outcomes. We performed 15 imputations for missing values of the outcome variables from baseline demographic characteristics and pain and function scores. We combined the results to obtain estimates of regression coefficients, standard errors and P values and compared those with the results of the original analyses. The results of the multiple imputation analyses were similar to and consistent with the original analyses for all outcomes.
RESULTS
Screening, Enrollment, and Follow-up Participants were recruited from the Soldier and Family Medical Clinic at WBAMC and throughout Fort Bliss. The recruitment efforts included dissemination of flyers and posters at throughout the clinics, dining facilities, and Army Community Services. We also asked the medical providers for referrals of patients who met eligibility criteria. A total of 213 potential participants were screened for this study and 91 were enrolled (Figure 1). We extended the recruitment period by 3 months in attempt to meet our projected sample size of 100, but concluded recruitment at 91 participants when the grant period ended. Of those excluded, 80 did not meet eligibility criteria and 42 declined participation. A total of 46 participants were randomized to the SMC group and 45 were randomized to the SMC plus CMT group. Follow-up rates were 85% at both endpoints for the SMC plus CMT group and 61% and 63% for the SMC group at weeks 2 and 4, respectively.
Baseline Characteristics
Study participants had a mean age of 26 years; 86% were male, and 63% were white. The median duration of participant current LBP episode at the time of enrollment was 9 days and 43% had radicular signs. Most participants (71%) reported taking some medication for their back pain during the past week. Participants had a higher expectation of helpfulness for SMC plus CMT compared with only SMC (Tables 1 and 2).
Adverse Events
There were no serious adverse events (AEs). Two AEs graded as mild, expected events were reported by participants from the SMC plus CMT treatment arm. One AE was reported as sharp pain in the right buttocks that resolved within 24 hours; this AE was graded unrelated to trial interventions. The other AE was graded possibly related to the CMT when the participant reported sharp pain in the lower back that prompted a visit to the physician assistant for pain medication; this AE resolved within 48 hours.
DISCUSSION
The results of our pragmatic pilot study indicate a statistically and clinically significant benefit to those receiving CMT in addition to SMC. Juni et al [23] conducted the only other study we found that compared only SMC with SMC plus CMT using the same outcome measures. They found no differences between the groups at 2 weeks using both the RMQ and NRS. CMT primarily included HVLA, whereas SMC consisted of medication and general home care advice. Participants underwent a single medical visit and 5 visits for CMT. Our study is similar to that conducted by Juni et al [23] with regard to the number of visits to DC and SMC, as well as the general treatment approaches provided within each group. However, there are differences in the populations studied. Our sample was younger and more ethnically diverse and included fewer women. Also, Juni et al [23] had substantially fewer losses to follow-up.
It is possible that our military population was also more physically fit at baseline than either the general population or previous study populations that evaluated CMT for LBP. However, approximately 40% of our sample was profiled, meaning they had some duty restrictions due to their LBP. Although our sample may be, on average, more likely to be physically fit than young adults in general, when compared with a similar age cohort of the US population ages 25 to 34 using the Short Form-12 physical function scale, our population had a mean score of 36, whereas the norm is 53. [24] Therefore, our population had lower physical function than the general population at baseline because of their LBP. Mental function between our study population and the population norm were very similar (mean, 48 vs. 49 respectively).
Limitations to our study include an inability to blind both the participant and the treating clinician to treatment group assignment. However, both the principal investigator and analyst remained blinded throughout the study. Another limitation is a loss to follow-up that was disproportionate between groups. Although our loss to follow-up in the SMC plus CMT group was only 15%, we were unable to obtain follow-up assessments in more than 35% of the SMC group. This may have been because of the scheduling differences between the 2 groups. All CMT visits were scheduled at the first visit and coincided with the outcome assessments. However, followup visits in the SMC group were scheduled independently from treatment visits. Although the analyses of the imputed data did not differ from the analyses that included only the observed data, the possibility of attrition bias cannot be ruled out. Finally, while we tracked the prescription of medications at the outset of care, we did not gather detailed data regarding actual medication use during the trial. Thus, it is possible that differences may have influenced study results. It is important to note that participants in the SMC group were twice as likely to have received medication as those in the SMC plus CMT group. It is difficult to attribute improvement to any 1 component of the care provided. Both treatment groups combined medication with physical modalities and medication was prescribed in less than half of the patients. However, our results suggest that the somewhat increased medication use in the SMC group did not confer a significant benefit.
This study answers some questions, while raising others. It will be important to attempt to replicate our findings using a larger sample size, with significant resources committed to follow-up strategies.
CONCLUSION
The results of this trial suggest that chiropractic manipulative therapy (CMT) in conjunction with standard medical care (SMC) offers a significant advantage for decreasing pain and improving physical functioning compared with only SMC for active-duty men and women between 18 and 35 years of age with acute LBP when delivered in a pragmatic treatment setting. These findings are clinically significant and in contrast to Juni et al [23] Differences could be largely because of the populations studied but may also reflect limitations in our study itself, including loss to follow-up. It is clear that additional high quality randomized controlled trials are required to establish the appropriate role definitively for CMT in diverse populations within pragmatic health care settings.
Key Points
Mean low back function scores improved in both groups during the course
of the study but adjusted mean scores were significantly better in the
group that received chiropractic manipulative therapy when compared
with only standard medical care (SMC) at both weeks 2 and 4.Adjusted pain scores were significantly improved in the group that received
chiropractic manipulative therapy when compared with only SMC at both
weeks 2 and 4.There was a statistically and clinically significant benefit to those patients
receiving chiropractic manipulative therapy (CMT) in addition to SMC
for patients aged 18 to 35 years, with acute LBP.
Acknowledgments
The authors thank the soldiers who participated in this study. Dr. Mikel Anderson who provided chiropractic care to participants, and all the physicians, therapists, and staff who provided standard medical care and adjusted their schedules to accommodate the logistics of the project.
The views expressed in this document are those of the authors and do not reflect the official policy of William Beaumont Army Medical Center, The Department of the Army, the United States Government or the funding agency.
This study was approved for human subjects' research by the Institutional Review Boards of Palmer College of Chiropractic and William Beaumont Army Medical Center.
ClinicalTrials.gov Identifier: NCT00632060
References:
Hart LG, Deyo RA, Cherkin DC, et al.
Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey.
Spine (Phila Pa 1976) 1995; 20: 11-9.Andersson GB.
Epidemiology of low back pain.
Acta Orthop Scand Suppl 1998; 281: 28-31.Maniadakis N, Gray A.
The economic burden of back pain in the UK.
Pain 2000; 84: 95-103.Macfarlane GJ, Beasley M, Jones EA, et al.
The prevalence and management of low back pain across adulthood: results from a population-based cross-sectional study (the MUSICIAN study).
Pain 2012; 153: 27-32.Dagenais S, Caro J, Haldeman S.
A Systematic Review of Low Back Pain Cost of Illness Studies
in the United States and Internationally
Spine J 2008 (Jan); 8 (1): 8–20Walker BF.
The prevalence of low back pain: a systematic review of the literature from 1966 to 1998.
J Spinal Disord 2000; 13: 205-217.Barnes PM , Powell-Griner E , McFann K , Nahin RL:
Complementary and Alternative Medicine Use Among Adults:
United States, 2002
Advance Data 2004 (May 27); 343: 1–19Barnes PM , Bloom B , Nahin RL:
Complementary and Alternative Medicine Use Among Adults and Children:
United States, 2007
US Department of Health and Human Services,
Centers for Disease Control and Prevention,
National Center for Health Statistics, Hyattsville, MD, 2008.Assendelft WJ, Morton SC, Yu El, et al.
Spinal manipulative therapy for low back pain. A meta-analysis of effectiveness relative to other therapies.
Ann Intern Med 2003; 138: 871-81.Lawrence DJ, Meeker W, Branson R, Bronfort G, Cates JR, Haas M, Haneline M et al.
Chiropractic Management of Low Back Pain and Low Back-Related Leg Complaints:
A Literature Synthesis
J Manipulative Physiol Ther 2008 (Nov); 31 (9): 659–674Bronfort, G, Haas, M, Evans, R, Kawchuk, G, and Dagenais, S.
Evidence-informed Management of Chronic Low Back Pain
with Spinal Manipulation and Mobilization
Spine J. 2008 (Jan); 8 (1): 213–225Bronfort G, Haas M, Evans R, Leiniger B, Triano J.
Effectiveness of Manual Therapies: The UK Evidence Report
Chiropractic & Osteopathy 2010 (Feb 25); 18 (1): 3Furlan, AD, Yazdi, F, Tsertsvadze, A et al.
Complementary and Alternative Therapies for Back Pain II
Evidence/Technology Report Number 194
AHRQ Publication No. 10(11)-E007 (October 2010),
U.S. Department of Health and Human Services, Rockville, MDKoes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C.
An Updated Overview of Clinical Guidelines for the Management of
Non-specific Low Back Pain in Primary Care
European Spine Journal 2010 (Dec); 19 (12): 2075–2094Walker BF, French SD, Grant W, et al.
Combined chiropractic interventions for low-back pain.
Cochrane Database Syst Rev 2010; CD005427.Rubinstein SM, van MM, Assendelft WJ, et al.
Spinal manipulative therapy for chronic low-back pain: an update of a Cochrane review.
Spine (Phila Pa 1976) 2011; 36: E825-46Goertz GM, Pohlman KA, Vining RV, et al.
Patient-centered Outcomes of High-velocity, Low-amplitude Spinal Manipulation
for Low Back Pain: A Systematic Review
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 670-691US Gensus Bureau 2010. Available at
http://quickfacts.census.gov/qfd/states/48/4826664.html
Accessed January 24, 2012.Stratford PW, Binkley JM, Riddle DL.
Development and initial validation of the back pain functional scale.
Spine 2000; 25: 2095-102.van der Roer N, Ostelo RW, Bekkering GE, et al.
Minimal clinically important change for pain intensity, functional status, and general health status in patients with nonspecific low back pain.
Spine (Phila Pa 1976) 2006; 31: 578-82.Bombardier C, Hayden J, Beaton DE.
Minimal clinically important difference. Low back pain: outcome measures.
J Rheumatol 2001; 28: 431-38Ostelo RW, de Vet HC.
Clinically important outcomes in low back pain.
Best Pract Res Clin Rheumatol 2005; 19: 593-607.Juni P, Battaglia M, Nuesch E, et al.
A randomised controlled trial of spinal manipulative therapy in acute low back pain.
Ann Rheum Dis 2009; 68: 1420-27.Ware JE, KosinskiM,Turner-Bowker DM, et al.
User's Manual for the SF-12v2 Health Survey (with a Supplement Documenting SF-12 Health Survey).
Lincoln, RI: Quality Metric Incorporated; 2002
Return to LOW BACK PAIN
Return to McKENZIE METHOD
Return to CHIROPRACTIC CARE FOR VETERANS
Since 1-28-2015


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |