

Changes in the Use of Telehealth and Face-To-Face
Chiropractic Care in the Department of Veterans
Affairs Before and After the COVID-19 PandemicThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2021 (Sep); 44 (7): 584–590 ~ FULL TEXT
Thanks to JMPT for permission to reproduce this Open Access article! Gregory R. Roytman, DC, Brian C. Coleman, DC, Kelsey L. Corcoran, DC,
Christine M. Goertz, DC, PhD, Cynthia R. Long, PhD, PStat, Anthony J. Lisi, DC
Yale Center for Medical Informatics,
Yale University,
New Haven, and VA Connecticut Healthcare System,
Connecticut.

Objective: The purpose of this study was to describe the use of face-to-face and telehealth chiropractic care in the U.S. Veterans Health Administration (VHA) before and after the declaration of the COVID-19 pandemic.
Methods: A cross-sectional study was performed of VHA administrative data, including monthly numbers of unique patients and visits for face-to-face and telehealth (synchronous video or telephone) chiropractic care from October 1, 2019, to March 31, 2021.
Results: During the pre-pandemic phase (October 2019 to February 2020), a mean of 28,930 (SD 289) total monthly visits were conducted face-to-face (99.9%). In March 2020, total monthly visits decreased to 17.0% of the pre-pandemic average, 25.0% being face-to-face, with over a 200–fold increase in telehealth visits (rising to 1,331 visits) compared to the pre-pandemic average. April showed the lowest number of face-to-face visits at (4,094). May-October 2020 showed that face-to-face visits increase on average by 70.7% per month, while telehealth visits averaged 17.3% per month. October-February 2020 had total monthly visits plateau at a mean of 22,250 (76.9% of the pre-pandemic average). Telehealth visits reduced to a mean of 1,245 monthly visits over this 5–month period, a drop of –5.6% of the average of monthly visits. In March 2021, total monthly visits (31,221) exceeded the pre-pandemic average for the first time since January 2020; 4.0% remained in telehealth.
Conclusion: Face-to-face visits decreased early in the pandemic but increased after May 2020. Chiropractic telehealth use rapidly increased during the early stage of the COVID-19 pandemic, and decreased later, but remained slightly higher than pre-pandemic levels.
Keywords: COVID-19; Chiropractic; Pandemic; Remote Consultation; Telemedicine; Telephone.
From the FULL TEXT Article:
Introduction
In recent years, the Veterans Health Administration (VHA) has expanded the use of telehealth services to increase veterans’ access to care. [1–4] VHA telehealth policies and practice have helped many veterans, including geriatric, disabled, and rural veterans who cannot easily visit VHA facilities for care. [1–4] These policies were introduced after decades of study, indicating satisfactory healthcare delivery via telehealth. [5, 6] These studies of telehealth include analyses in the context of chronic disease management, [7, 8] musculoskeletal care, [9] and cost effectiveness. [10] In fiscal year 2019, (October 1, 2018, to September 30, 2019) the VHA provided 2.6 million telehealth visits to nearly 1 million veterans. [11]
With the onset of the COVID-19 pandemic in the United States in March 2020, necessary restrictions on in-person, face-to-face (F2F) health care visits developed. [12–14] Federal mandates, VHA policy, and procedural changes led to the rapid expansion of VHA telehealth resources across the nation. [15–17] For example, following the U.S. Department of Health and Human Services's relaxation of the types of platforms that could be used for telehealth services, [18] VHA concurrently enabled its providers to use external platforms such as Zoom and FaceTime to facilitate delivery of remote visits. [19] Overall, the number of F2F visits to all clinics in the VHA dropped by nearly 11 million across a 10–week period beginning in mid-March 2020. [20] This was concurrent with a 2–fold increase in the number of telehealth visits. [20]
Consistent with all VHA healthcare services, VHA chiropractic clinics faced the need to expand their use of telehealth. At that time, little was known about the delivery of chiropractic care via telehealth in the VHA or broader U.S. health care system. In the following year, works describing chiropractor perceptions [21, 22] and institutional and regulatory policy [23, 24] have provided some insight into aspects of chiropractic care during the early stage of the COVID-19 pandemic, yet to date there are no published data on service use. This growing trend toward telehealth in the wake of the pandemic requires description of the extent to which chiropractic care could be delivered in a telehealth environment. The VHA system is an opportune environment in which to study widescale national deployment of chiropractic telehealth. Therefore, the purpose of this study was to describe trends in the use of telehealth and F2F chiropractic care during the 6 months preceding and 12 months following the onset of the COVID-19 pandemic in the VHA system.
Methods
We performed a cross-sectional study of VHA administrative data on national chiropractic clinic use during October 1, 2019, to March 31, 2021. We categorized time by calendar month and defined the onset of the COVID-19 pandemic as March 1, 2020. The World Health Organization (WHO) declaration of COVID-19 as a pandemic in March 2020 [13] was used to segment the study period into pre-pandemic and continuing phases by month. Thus, we assessed 6–months pre-pandemic WHO declaration and 12–months post-pandemic declaration. We identified a cohort of all patients nationally receiving VHA chiropractic visits onsite at any VHA facilities or via telehealth from VHA providers during the study period. We did not include patients receiving any form of community-based chiropractic care exclusively.
Demographic data were obtained for each patient including age at first chiropractic visit, sex, race/ethnicity, and marital status. All clinic visits were identified and categorized into mutually exclusive groups as “F2F” (in-person visits at the VHA facility), “video” (synchronous virtual visits using any VHA-approved video platform), or “telephone” (synchronous telephone call between patient and provider). Video and telephone visits were limited to those including 1–to–1 patient care (ie, did not include telephone calls for administrative items like scheduling, nor video group presentations or classes) and collapsed into a single “telehealth” visit category. Telephone visits were identified by the presence of telephone Current Procedural Terminology codes. F2F and video visits were identified by VHA administrative clinic identifiers known as stop codes.
All data were extracted from the VHA Corporate Data Warehouse and analyzed with descriptive statistics in Microsoft Excel (Microsoft, Redmond, Washington). The Reporting of Observational Studies in Epidemiology Guidelines for cross-sectional study was used to inform this report. [25] This project was a program analysis of operational data, and consistent with VA Connecticut Research and Development Office and VHA Office of Research and Development Program Guide 120021, and it did not require institutional review board approval.
Results

Table 1

Table 2
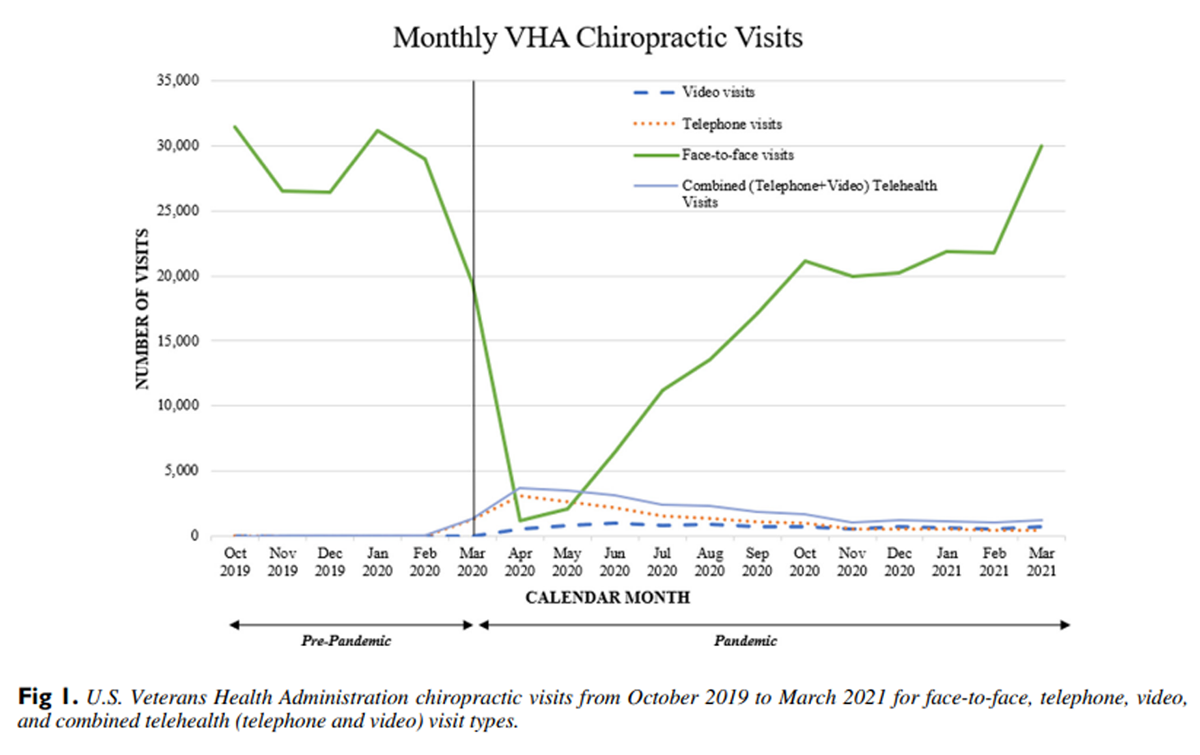
Figure 1 During the 18–month study period, we identified 90,485 patients receiving VHA chiropractic care at 184 VHA medical facilities. The mean age was 52.4 years (range, 19–102 years), 82.9% were male and 65.8% were white. Demographics are presented in Table 1. The monthly distribution of patients and visits are shown in Table 2, and a graphical representation of visits is shown in Figure 1.
In the pre-pandemic period, the mean number of unique chiropractic patients per month was 20,294 (SD 1,208). Over the next 2 months, the number of patients seen decreased sharply, reaching a low of 3,887 patients (19.2% of the pre-pandemic monthly average) in April 2020. In the late Spring and Summer of 2020, the number of patients seen steadily rose each month. From October 2020 to February 2021, the mean monthly number of patients remained relatively constant at approximately 81.3% of the pre-pandemic overall average, and in March 2021 reached 21,340, which surpassed the pre-pandemic average.
The types of chiropractic visits delivered to patients changed during this study period. During the pre-pandemic phase from October 2019 through February 2020, there was a mean of 28,930 (SD 2,389) total visits per month, almost all exclusively F2F care (99.9%). Starting in March 2020, monthly visits decreased to a low of 4,904 (17.0% of the pre-pandemic average) in April 2020. In that month the proportion of F2F visits dropped to 25.0% of the total number of visits while telehealth increased to 75.0%. From May 2020 to October 2020, F2F visits increased at an average rate of 70.7% per month. Meanwhile during this same period, there was a mean of 2,501 telehealth visits each month, which represented 17.3% of the average of all monthly visits, both telehealth and F2F. From October to February 2020, monthly visits of all types plateaued at a mean of 22,250 (76.9% of the pre-pandemic average). Concurrently, telehealth visits reduced to a mean of 1,245 visits per month over this 5–month period and represented 5.5% of the average of all monthly visits. In March 2021, the total number of monthly visits (31,221) exceeded the pre-pandemic average for the first time since January 2020. Of the visits in March 2021, 4.0% were telehealth.
Discussion
We present the first health services data on the use of chiropractic care via F2F and telehealth mechanisms around the start of the COVID-19 pandemic. During February to April 2020, the early months of the COVID-19 pandemic in the United States, uncertainty and concerns about transmission, infection severity, and infection mortality of COVID-19 called into question the necessity of any U.S. health care visits that were not of an urgent or life-threatening nature. VHA took steps to decrease F2F visits when the overall risk–reward assessment favored doing so, and replaced them with virtual services when appropriate. [26] VHA's regional Veterans Integrated Service Network and individual facility leadership determined when and to what degree to restrict (and subsequently return) to F2F visits for all health care services.
As would be expected, we saw a dramatic decrease in the number of patients receiving either type of VHA chiropractic care in those months. Although greatly diminished, nationally chiropractic visits (including F2F visits) never reached 0 in any given month. However, as with other health care services, F2F chiropractic care at particular facilities could have been fully suspended at various points in time based on local considerations including infection rates, inpatient censuses, and infection control capacity.
Although F2F visits decreased, there was a substantial increase in the number of telehealth visits during the early months. In the pre-pandemic period, VHA provided telehealth chiropractic care at a low rate. The steep increase in telehealth visits that occurred in the early months showed VHA's capacity to modulate its delivery of chiropractic care by telehealth. Yet, telehealth visits did not completely compensate for the concurrent reduction in F2F visits, suggesting possible barriers to adopting telehealth.
When considering barriers, we offer these suggestions. First, patients and clinicians may have been hesitant to engage in virtual care because of unfavorable perceptions or barriers to technology. [27–31] Systemic factors, such as privacy policies and video platform bandwidth, also might have limited the uptake of virtual care. Because telehealth was rare in VHA chiropractic care before the pandemic, many VHA chiropractors might not have had the experience, familiarity, or training to adopt telehealth. Others have described barriers and facilitators of implementing chiropractic telehealth primarily outside the VHA system during the early pandemic days. [21–24] Further work is needed to determine whether similar themes apply to the VHA. However, the data here describe low utilization of telehealth in the pre-pandemic period and, nonetheless, institutional inertia might have had an effect in dampening the subsequent adoption of telehealth. [27, 32, 33]
Another potential barrier to telehealth includes the perception among chiropractors and other manual therapists that telehealth services are of limited utility, given the emphasis of these professions on providing touch-based care. [34] However, guidelines on spinal disorders [35, 36] promote diagnosis and triage, active exercise, and education modalities [35] that are within the scope and expected practice of chiropractic care [37] and are conducive to delivery via telehealth. [22] A recent international, interprofessional expert team developed patient and clinical guides to help triage cases and to inform the use of telehealth in management of spinal disorders. [38] As a result, chiropractors have an opportunity to facilitate continuity of care through the use of telephone or video methods. [39, 40]
In our study of chiropractic use of telehealth in the VHA, with the increased use of telehealth services, telephone visits were more frequently seen than video visits. Chiropractors might have been more familiar with telephone encounters compared with video encounters. Reasons for this could include the requirement of additional procedures, equipment, privacy and security requirements, and technological literacy, which are well known [41–44] and nonnegligible barriers in a video visit. These factors could be a deterrent to both patients and chiropractors; however, this could have been overcome during the study period, with federal policies allowing an expanded range of commercial video platforms to be used for clinical encounters. [18]
Future Studies
The results of our study are purely descriptive of the trends of use of telehealth services and do not describe in any detail the nature of the chiropractic care delivered. Nonetheless, it is necessary to describe such trends, which will frame subsequent inquiries into their causes and effects. The efficacy and effectiveness of chiropractic telehealth services has yet to be determined. Yet several ongoing studies assessing the treatment of chronic pain by non-pharmacologic methods, including chiropractic care, have adopted virtual care delivery. [45, 46] Future work in the VHA should assess clinical and sociodemographic characteristics of patients receiving chiropractic care via telehealth, as well as the services delivered in such visits. In addition, studies are needed to examine virtual chiropractic care under non-pandemic conditions, to explore potential blending and sequencing of telehealth and F2F visits in treatment plans, the most effective types of services to be used during telehealth visits, and the effects on provider workload and productivity. Clinical research studies assessing the use of telehealth during the management of patients receiving chiropractic care or aiming to provide recommendations for telehealth use in usual practice, should consider individualization of clinically appropriate care, patient preferences (including acceptability), and involvement in shared decision making. The VHA system provides an excellent setting in which to conduct such work, and we believe that future studies providing more granular detail on patients and providers could be relevant for chiropractic care in the broader U.S. health care system.
Limitations
A characteristic limitation of cross-sectional studies is that the exposure and outcome occur simultaneously. In this study, however, we can be reasonably confident that necessary social distancing guidelines stemming from the COVID-19 pandemic led to the rapid drop in F2F visits in March 2020 and resulting expansion of telehealth. The location where providers were based when delivering telehealth care might have varied from onsite at the VHA facility to remotely from their own home as appropriate. National data presented here do not depict detail on individual facilities, so we were unable to identify locations that telehealth was provided. We did not assess variation in state-level mandates or facility COVID-19 case numbers. Lastly, our sample of VHA chiropractors might not be representative of the population of chiropractors in other settings.
Conclusion
This study described the trends in VHA chiropractic use during an 18–month period around the start of the COVID-19 pandemic. Unique patients and total visits decreased dramatically in March and April 2020 but slowly rose thereafter, returning to pre-pandemic levels by March 2021. A dramatic increase in the use of telehealth visits occurred early on, which remained elevated at study end, compared with the beginning of the study.
Funding Sources and Conflicts of Interest
This work was supported through cooperative agreement UH3AT009761 from the National Center for Complementary and Integrative Health and the Office of Research on Women's Health. This work was also supported with resources and the use of facilities at the VA Connecticut Healthcare System, West Haven, Conneticut. The authors have no additional conflicts of interest, financial or otherwise, to disclose. The contents of this manuscript represent the view of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs, the National Institutes of Health, or the United States Government.
Contributorship Information
Concept development (provided idea for the research): A.J.L.
Design (planned the methods to generate the results): G.R.R., A.J.L., B.C.C.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): A.J.L., B.C.C., G.R.R., K.L.C., C.M.G., C.R.L.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): B.C.C., G.R.R.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): A.J.L., B.C.C., G.R.R.
Literature search (performed the literature search): G.R.R.
Writing (responsible for writing a substantive part of the manuscript): G.R.R., A.J.L., B.C.C., K.L.C.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): A.J.L., B.C.C., G.R.R., K.L.C., C.M.G., C.R.L.
References:
Lum H Nearing K Pimentel C Levy C Hung W
Anywhere to anywhere: Use of telehealth to increase health care
access for older, rural veterans.
Gerontol Soc Am. 2020; : 12-18Elliott V.
Delivery of VA Telehealth Services During COVID-19.
In: Service CR, editor. Online:
Congressional Research Service; 2020.What Is Telehealth? VA Telehealth.
U.S. Department of Veterans Affairs, Online 2021Veazie S Bourne D Peterson K Anderson J
Evidence brief: Video telehealth for primary care and mental health services.
US Department of Veterans Affairs Evidence Synthesis Program, Washington, DC 2019Dorsey ER Topol EJ
State of telehealth.
N Engl J Med. 2016; 375: 154-161Flodgren G Rachas A Farmer AJ Inzitari M Shepperd S
Interactive telemedicine: Effects on professional practice and health care outcomes.
Cochrane Database Syst Rev. 2015; CD002098Kitsiou S Pare G Jaana M
Systematic reviews and meta-analyses of home telemonitoring interventions
for patients with chronic diseases: A critical assessment
of their methodological quality.
J Med Internet Res. 2013; 15: e150Pare G Jaana M Sicotte C
Systematic review of home telemonitoring for chronic diseases: the evidence base.
J Am Med Inform Assoc. 2007; 14: 269-277Kroenke K Krebs EE Wu J Yu Z Chumbler NR Bair MJ
Telecare collaborative management of chronic pain
in primary care: A randomized clinical trial.
JAMA. 2014; 312: 240-248Polisena J Coyle D Coyle K McGill S
Home telehealth for chronic disease management: A systematic review
and an analysis of economic evaluations.
Int J Technol Assess Health Care. 2009; 25: 339-349Delivery of VA Telehealth Services During COVID-19.
Elliott V, editor. In Focus.
Congressional Research Service; 2020.Schuchat A
Public health response to the initiation and spread of pandemic COVID-19
in the United States, February 24–April 21, 2020.
MMWR Morbid Mortal Wkly Rep. 2020; 69: 551-556Ghebreyesus T
WHO Director-General's opening remarks at the media briefing on COVID-19.
World Health Organization, Geneva2020COVID-19 Response Plan.
Veterans Health Administration -
Office of Emergency Management; 2020.Gupta S Federman DG
Hospital preparedness for COVID-19 pandemic: Experience from department
of medicine at Veterans Affairs Connecticut Healthcare System.
Postgrad Med. 2020; 132: 489-494Etingen B Amante DJ Martinez RN et al.
Supporting the implementation of connected care technologies in the
Veterans Health Administration: Cross-sectional survey findings from
the Veterans Engagement with Technology Collaborative (VET-C) Cohort.
J Particip Med. 2020; 12 (e21214.is§)CARES Act, §1, Mar. 27, 2020, 134 Stat. 281. Pub L No 116-136.
Office of Civil Rights (OCR).
Notification of Enforcement Discretion for Telehealth Remote Communications
During the COVID-19 Nationwide Public Health Emergency.
Emergency Preparedness. Washington, DC:
U.S. Department of Health and Human Services.Clancy C
Use of Video Communication Technology for VHA Research
and Development Activities Under COVID-19.
Department of Veterans Affairs, Washington, DC2020Baum A Kaboli PJ Schwartz MD
Reduced in-person and increased telehealth outpatient
visits during the COVID-19 pandemic.
Ann Intern Med. 2021; 174: 129-131Green BN Pence TV Kwan L Rokicki-Parashar J
Rapid deployment of chiropractic telehealth at 2 worksite health centers
in response to the COVID-19 pandemic: Observations from the field.
J Manipulative Physiol Ther. 2020; 43 (404.e1-e10)Johnson CD Green BN Konarski-Hart KK et al.
Response of practicing chiropractors during the early phase
of the COVID-19 pandemic: A descriptive report.
J Manipulative Physiol Ther. 2020; 43: 403.e1-403.e21Neff SM Roecker CB Okamoto CS et al.
Guidance concerning chiropractic practice in response to COVID-19
in the U.S.: A summary of state regulators’ web-based information.
Chiropr Man Therap. 2020; 28: 44Johnson CD Little CS Sterling TA Gojkovich S Boghosian K Ciolfi MA
Response of chiropractic organizations to the COVID-19 pandemic:
A descriptive report.
J Manipulative Physiol Ther. 2020; 43: 405.e1-405.e7von Elm E Altman DG Egger M et al.
The Strengthening the Reporting of Observational Studies in Epidemiology
(STROBE) statement: Guidelines for reporting observational studies.
Int J Surg. 2014; 12: 1495-1499Veterans Health Administration.
Moving Forward Guidebook: Safe Care Is Our Mission. 2020.
Available at:
https://www.va.gov/covidtraining/docs/20200611MovingForward/VHA_Moving_Forward_Guidebook.pdfGomez T Anaya YB Shih KJ Tarn DM
A qualitative study of primary care physicians’ experiences
with telemedicine during COVID-19.
J Am Board Fam Med. 2021; 34: S61-S70Hawley CE Genovese N Owsiany MT et al.
Rapid integration of home telehealth visits amidst COVID-19:
What do older adults need to succeed?
J Am Geriatr Soc. 2020; 68: 2431-2439Padala KP Wilson KB Gauss CH Stovall JD Padala PR
VA video connect for clinical care in older adults in a rural
state during the COVID-19 pandemic: Cross-sectional study.
J Med Internet Res. 2020; 22: e21561Ackerman SL Gleason N Shipman SA
Comparing patients’ experiences with electronic and
traditional consultation: Results from a multisite survey.
J Gen Intern Med. 2020; 35: 1135-1142Polinski JM Barker T Gagliano N Sussman A Brennan TA Shrank WH
Patients’ satisfaction with and preference for telehealth visits.
J Gen Intern Med. 2016; 31: 269-275Cowan KE McKean AJ Gentry MT Hilty DM
Barriers to use of telepsychiatry: Clinicians as gatekeepers.
Mayo Clin Proc. 2019; 94: 2510-2523Shachar C Engel J Elwyn G
Implications for telehealth in a postpandemic future: Regulatory and privacy issues.
JAMA. 2020; 323: 2375-2376Malliaras P Merolli M Williams CM Caneiro JP Haines T Barton C
‘It's not hands-on therapy, so it's very limited’:
Telehealth use and views among allied health clinicians
during the coronavirus pandemic.
Musculoskelet Sci Pract. 2021; 52102340Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Guzman J, Haldeman S, Carroll LJ, et al.
Clinical Practice Implications of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders:
From Concepts and Findings to Recommendations
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S199–S212Vining RD, Shannon ZK, Salsbury SA, Corber L, Minkalis AL, Goertz CM.
Development of a Clinical Decision Aid for Chiropractic Management
of Common Conditions Causing Low Back Pain in Veterans:
Results of a Consensus Process
J Manipulative Physiol Ther. 2019 (Nov); 42 (9): 677–693Haldeman S Nordin M Tavares P et al.
Distance management of spinal disorders during the COVID-19 pandemic
and beyond: Evidence-based patient and clinician guides
from the Global Spine Care Initiative.
JMIR Public Health Surveill. 2021; 7: e25484Chaet D Clearfield R Sabin JE Skimming K
Council on Ethical and Judicial Affairs American Medical Association.
Ethical practice in telehealth and telemedicine.
J Gen Intern Med. 2017; 32: 1136-1140Khera A Baum SJ Gluckman TJ et al.
Continuity of care and outpatient management for patients with and at
high risk for cardiovascular disease during the COVID-19 pandemic:
A scientific statement from the American Society for Preventive Cardiology.
Am J Prev Cardiol. 2020; 1100009Clay-Williams R Baysari M Taylor N et al.
Service provider perceptions of transitioning from audio to video
capability in a telehealth system: A qualitative evaluation.
BMC Health Serv Res. 2017; 17: 558Banbury A Nancarrow S Dart J et al.
Adding value to remote monitoring: Co-design of a health literacy
intervention for older people with chronic disease delivered by telehealth -
The telehealth literacy project.
Patient Educ Couns. 2020; 103: 597-606Sezgin E Huang Y Lin D Ramtekkar U Pauline L Lin S
Documented reasons of cancellation and rescheduling
of telehealth appointments during the pandemic.
Telemed J E Health. 2021; 27: 1143-1150Fernandes L, Devan H, Fioratti I, Kamper S, Williams C, Saragiotto B.
At my own space, pace and place: A systematic review of qualitative
studies of enablers and barriers to telehealth interventions
for people with chronic pain [e-pub ahead of print].
Pain. doi:10.1097/j.pain.0000000000002364.Fritz JM Davis AF Burgess DJ et al.
Pivoting to virtual delivery for managing chronic pain with
nonpharmacological treatments: Implications for pragmatic research.
Pain. 2021; 162: 1591-1596Coleman BC Kean J Brandt CA Peduzzi P Kerns RD
Adapting to disruption of research during the COVID-19 pandemic while
testing nonpharmacological approaches to pain management.
Transl Behav Med. 2020; 10: 827-834
Return to CHIROPRACTIC CARE FOR VETERANS
Since 5-12-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |