A New Conceptual Model Of Neck Pain:
Linking Onset, Course, And CareResults of the Bone and Joint Decade 2000–2010 Task Force
on Neck Pain and Its Associated DisordersThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther. 2009 (Feb); 32 (2 Suppl): S17–28 ~ FULL TEXT
Republished from: Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S14–23
OPEN ACCESS Jaime Guzman, MD, MSc, FRCP(C), Eric L. Hurwitz, DC, PhD,
Linda J. Carroll, PhD, Scott Haldeman, DC, MD, PhD, Pierre Côté, DC, PhD,
Eugene J. Carragee, MD, FACS, Paul M. Peloso, MD, MSc, FRCP(C),
Gabrielle van der Velde, DC, Lena W. Holm, DrMedSc, Sheilah Hogg-Johnson, PhD,
Margareta Nordin, PT, DrMedSci, J. David Cassidy, DC, PhD, DrMedSc
Department of Medicine,
University of British Columbia, Canada.STUDY DESIGN: Iterative discussion and consensus by a multidisciplinary task force scientific secretariat reviewing scientific evidence on neck pain and its associated disorders.
OBJECTIVE: To provide an integrated model for linking the epidemiology of neck pain with its management and consequences, and to help organize and interpret existing knowledge, and to highlight gaps in the current literature.
SUMMARY OF BACKGROUND DATA: The wide variability of scientific and clinical approaches to neck pain described in the literature requires a unified conceptual model for appropriate interpretation of the research evidence.
METHODS: The 12-member Scientific Secretariat of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders critically reviewed and eventually accepted as scientifically admissible a total of 552 scientific papers. The group met face-to-face on 18 occasions and had frequent additional telephone conference meetings over a 6-year period to discuss and interpret this literature and to agree on a conceptual model, which would accommodate findings. Models and definitions published in the scientific literature were discussed and repeatedly modified until the model and case definitions presented here were finally approved by the group.
RESULTS: Our new conceptual model is centered on the person with neck pain or who is at risk for neck pain. Neck pain is viewed as an episodic occurrence over a lifetime with variable recovery between episodes. The model outlines the options available to individuals who are dealing with neck pain, along with factors that determine options, choices, and consequences. The short- and long-term impacts of neck pain are also considered. Finally, the model includes a 5-axis classification of neck pain studies based on how subjects were recruited into each study.
CONCLUSION: The Scientific Secretariat found the conceptual model helpful in interpreting the available scientific evidence. We believe it can assist people with neck pain, researchers, clinicians, and policy makers in framing their questions and decisions.
KEYWORDS: neck pain, conceptual model, course, health care, impacts, management
From the Full-Text Article:
Background
This article describes the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders (Neck Pain Task Force) conceptual model for the onset, course, and care of neck pain. We start with the scope and rationale for proposing a new conceptual model, followed by its purposes and premises. After describing the model's components and associated case definitions, we conclude with a discussion on implications of the model.
One of the first issues faced by the Neck Pain Task Force was to define its scope given the time and resources available. Neck pain may be a feature of virtually every disorder and disease that occurs above the shoulder blades, [1] although it is only rarely a symptom of tumors, infections, and other space-occupying lesions of the head and neck. Neck pain can also be a component of headaches, temporomandibular joint syndrome, disturbances of vision, certain types of stroke, disorders affecting the upper extremities, inflammatory arthropathies, and fibromyalgia. [2]
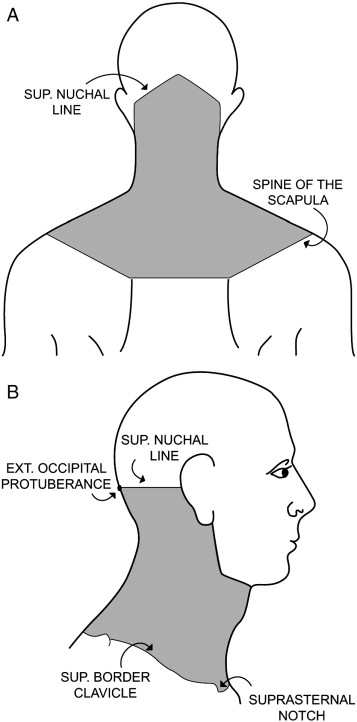
The Neck Pain Task Force mandate was to study what is frequently referred to as “nonspecific,” “soft tissue,” or “mechanical neck pain.” Specifically, we excluded from our considerations neck pain associated with serious local pathology or systemic disease, and there was no attempt to review the literature on neck pain because of skin lesions, throat disorders, tumors, infections, fractures and dislocations (except where such literature informed screening practices or differential diagnosis), myelopathy, rheumatoid arthritis, or other inflammatory joint diseases. [3, 4] The Neck Pain Task Force mandate was specific to pain located in the anatomic region of the neck as outlined in Figure 1, with or without radiation to the head, trunk, and upper limbs.
Pain has been described as “an unpleasant sensory and emotional experience” — a subjective experience. [5] As such, pain can usually best be ascertained by what the person reports about his or her pain, although we acknowledge that this way of assessing pain has its limitations. For example, self-reporting of the presence and severity of pain is not possible in some cases (e.g., preverbal children or persons with limited communication capacity), and the accuracy of reports cannot be confirmed against external criteria. Although the conceptualization of pain as a personal, subjective experience is widely accepted, great variation exists in how neck pain is described and considered in the published literature. This variability makes it difficult to compare the results of different studies and to be confident that participant populations were similar.
Many authors approach the study of neck pain in a way which suggests a view that all neck pain has a local pathologic cause, and that this cause can be identified and treated. Other authors seem to consider neck pain as a primarily nonorganic problem with psychological and social roots. There is also a tendency to separate neck pain into categories based on their linkage to particular events or precipitating factors such as whiplash-associated disorders (WAD), [6] occupational neck pain, [7] sports-related neck pain, [8] and neck pain of unknown origin (often called “non-specific neck pain”). [9] These varied approaches often imply different etiological models for neck pain.
It was necessary that the Neck Pain Task Force consider these models and approaches in the light of available scientific evidence, to develop an overarching conceptual model and meaningful subgroups of people with neck pain (case definitions). Having such a model allowed us to organize and properly interpret the available information and also to identify significant knowledge gaps.
This chapter presents the conceptual model for the onset, course, and care of neck pain used by the Neck Pain Task Force to inform our work, and includes a proposed classification system. The proposed model integrates concepts derived from the scientific literature relating to the impact of musculoskeletal symptoms and diseases, most notably from:
the conceptual framework of the International Classification of Functioning Disability and Health (ICF). [10]
von Korff et al's classification of musculoskeletal pain according to intensity and impact. [11]
the model proposed by the Québec Task Force to categorize WAD. [6]
the model proposed by Côté et al to categorize prognosis literature in WAD. [12]
the concepts underpinning decision analysis. [13]
the conceptualization of musculoskeletal soft tissue symptoms as lifelong, episodic occurrences. [14, 15]
the differentiation between patients and claimants proposed by Hadler. [16]
the conceptual dimensions of recovery proposed by Beaton et al. [17]
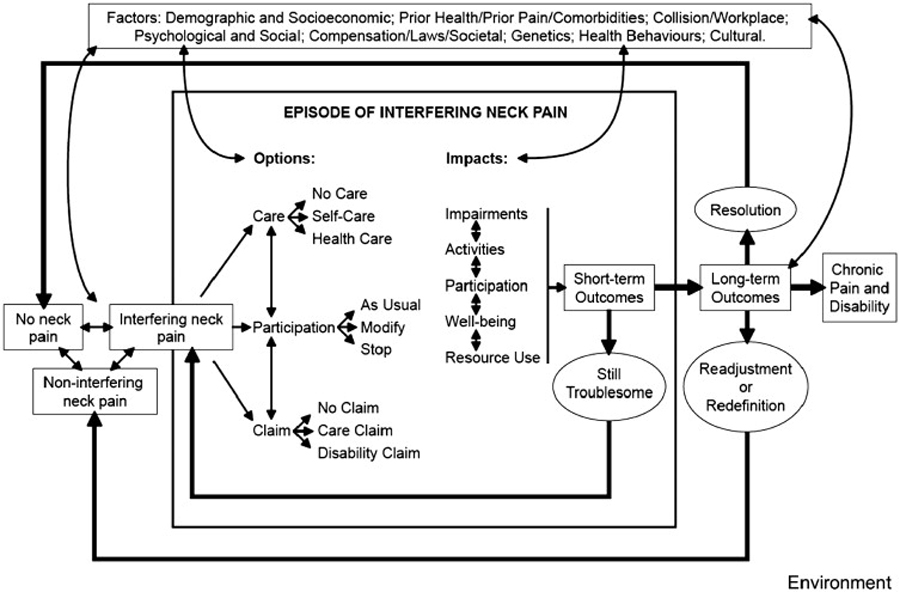
The simplified graphical representation of the model is depicted in Figure 2. The conceptual model was built on 6 explicit premises (see below). It was then refined through an iterative process, as the Scientific Secretariat summarized more and more evidence during the 6-year existence of the Neck Pain Task Force. The model has 5 components. Each component is described in turn in the following sections accompanied by examples.
Purposes and Premises
The purpose of the Neck Pain Task Force conceptual model for the onset, course and care of neck pain is 2-fold:(1) to provide an integrated model for linking the epidemiology of neck pain (incidence, prevalence, course, prognosis) with its management (assessment, diagnosis, treatment, self-management); and
(2) to help organize and interpret existing knowledge and to highlight gaps in the current literature.We hope the model will also prove helpful for other purposes, but these are the 2 purposes that guided its development. The model is built on 6 premises:
Premise 1: The Primary Perspective of Interest is That of Persons With Neck Pain
or Who are at Risk of Developing Neck Pain
The overarching goal of the Neck Pain Task Force is to help reduce the personal and societal burden of neck pain and to empower persons with neck pain to make their own decisions. [3] For this reason the model focuses on the transitions in neck pain experienced by the person over a lifetime and the options available for dealing with neck pain. Because conceptual models are explicitly derived to inform the thinking and work of many people, a common tension in their development is the compromise between specificity and detail (geared to a particular discipline or perspective) and generalizability (applicable across disciplines and perspectives). Because neck pain is by definition a subjective, personal experience, we believed that most disciplines could interpret and use the model if it was centered on the person experiencing neck pain or at risk of developing neck pain.
Premise 2: The Course of Neck Pain is Best Described as Episodes Occurring
Over a Lifetime With Variable Degrees of Recovery in Between Episodes
This premise is consistent with the mounting evidence about the episodic course of other musculoskeletal symptoms (such as back pain). This premise is more supportable than previously held views, which viewed neck pain as a single event with permanent resolution. [14, 15]
Premise 3: The Onset and Course of Neck Pain are Affected by Multiple Factors
This premise is consistent with both the biopsychosocial model of health and disease, and the conceptual framework of the ICF. [10] This premise states that, as a general rule, many environmental and personal factors combine to cause neck pain and to influence its course. This premise best accommodates published evidence on the multiple factors associated with the development, course, and consequences of neck pain. [12, 18, 19]
Premise 4: The Management and Subsequent Course of Neck Pain Depend on the
Options Available at the Time and on How These Options are Appraised
The options available to people with neck pain are primarily determined by prevailing personal, cultural, and societal factors. In some instances, the options are so restricted that the person really has few choices. For example, in some jurisdictions, access to health care is limited, and for some people with neck pain, the cost of certain treatments is prohibitive. Similarly, the individual may have no choice in whether or not to submit an insurance claim. For example in Ontario, Canada in 2005, a visit to a family physician (for neck pain or any other health concern) automatically generated a claim by the physician for payment, through the provincial universal health insurance plan. Once the patient consulted a physician, he or she had no choice on whether to submit a claim.
Premise 5: The Impact of Neck Pain on the Person can be Described Within Various Domains
In the model, these domains include changes to body structures and functions (impairments), tasks the person can accomplish (activities), involvement in life situations (participation), subjective well-being, and resource utilization (health care and nonhealth care resources). This premise is based on the ICF's conceptual framework for impairments, activities, and participation, [10] but also incorporates subjective well-being and resource utilization as important domains.
Premise 6: Linkages Between Factors and Impacts can Occur in Multiple Directions
Conceptually any element in the model could influence another. Thus, any given factor could (in theory) impact the onset, course, or outcomes of neck pain, and a short-term outcome could impact subsequent factors and long-term outcomes. Empirical evidence is needed to demonstrate which of those interactions are most relevant to a particular situation.
Components of the Conceptual Model
The model is comprised of 5 major components:(1) factors affecting the onset and course of neck pain
(2) the “care” complex
(3) the “participation” complex
(4) the “claim” complex, and
(5) the impact and outcomes of neck pain (Figure 2).All these major components are situated in and influenced by a particular physical, cultural, attitudinal, and social environment (the outer frame in Fig 2). Thus, we suggest that the onset, course, and consequences of neck pain for a person cannot be understood without implicit or explicit knowledge of the person's environment.
Neck pain is as ubiquitous a symptom as headaches, abdominal pain, or back pain. From a life-course perspective, most people will have their first experience with neck pain early in life. This statement is supported by many studies which have demonstrated the occurrence of neck pain in childhood and adolescence. [20-22] As with back pain, even intense neck pain may be perceived as ultimately noninterfering and not recalled on later questioning. [23]
The model deals first with onset of pain and the transition from noninterfering neck pain to interfering neck pain. Interfering neck pain is defined as a condition which prompts the person to consider action; usually because of neck pain severity, duration, or because it interferes with the ability to function. Factors which may affect the onset of neck pain or the transition from non-interfering to interfering neck pain are listed at the top of Figure 2.
Once the individual experiences neck pain, he or she is likely to face 3 questions:“How should I care for this pain?
Should I change the things I do (participation)?
Should I (can I) file a claim to access financial benefits?”The options available for the person to answer these questions depend on the particular environment and circumstances; these are further elaborated on below.
1. Factors Affecting the Onset and Course of Neck Pain
The Neck Pain Task Force uses the term “factor” to refer to any attribute of the person or his/her environment that can affect the onset, course, or care of neck pain and its consequences. This includes the full spectrum of attributes, from a person's genetic endowment and their circumstances at the time of neck pain onset, to cultural expectations and the policies that govern the provision of health care and insurance services (listed at the top of Fig 2).
Depending on where an individual with neck pain is positioned in the conceptual model, and based on his or her personal circumstances, a particular set of factors will likely make the greatest contribution to subsequent events and impacts. In other words, the probability of transition from one point in the neck pain experience to another point will often be determined by a subset of factors relevant to the specific situation. A single factor could act as a determinant at different points in the model: for example it may well be that younger age decreases not only the risk for developing neck pain, but also its relative severity and the chance of a poor outcome. [15, 20] Other factors might have limited influence and act as a determinant at just a single point in the model.
There are multiple ways of classifying these factors. Factors can be classified according to the point in the conceptual model where they are believed to have primary influence. So, one could speak of risk factors (i.e., those which increase or decrease the probability of developing neck pain), and prognostic factors (i.e., those which increase or decrease the probability of recovery in people with neck pain).
The Neck Pain Task Force proposes a simplified classification of both risk and prognostic factors by their origin as follows: demographic and socioeconomic factors, prior health/prior pain/comorbidities, collision/ workplace factors, psychological and social factors, compensation/laws/societal factors, genetics, health behaviors, cultural factors. If a more detailed classification of these factors is desired, the extended classification of environmental factors in the ICF is a possible resource. [10]
Clinical care of neck pain (including clinical diagnosis and treatment) and societal interventions can also be conceptualized as factors affecting the course of neck pain. For purposes of clarity, however, the Neck Pain Task Force has chosen to discuss these interventions as separate components.
Independently of its origin, a factor should be classified as either modifiable or not modifiable, depending of the feasibility of changing that factor. This is important for identifying interventions that are likely to have an impact on the onset, course, and care of neck pain. Of particular importance are modifiable factors that could have a large positive impact on the prevention and recovery of neck pain (e.g., increasing well-being and minimizing symptoms, impairments, activity limitations, participation restrictions, and resource utilization). Thus, according to our conceptual model for the onset, course, and care of neck pain, interventions can be defined as purposeful changes in one or more factors. But we must acknowledge that such interventions may also have undesirable effects.
In conducting our best evidence synthesis, the Neck Pain Task Force also classified factors according to the degree of scientific certainty that specific factors had an independent effect. Based on work published in the area of breast cancer, we linked the degree of certainty to the design and methodologic quality of available studies. [24] Details on this classification are provided elsewhere. [15, 20, 25, 26]
2. The “Care” Complex
The majority of people with neck pain do not seek health care for neck pain. Decisions about care are influenced by environmental and personal factors, especially by local health policy factors that affect the care options available to the person. Consider the person who develops neck pain shortly after a car crash in a remote location of a developing nation. In this situation, urgent health care may not be an option. If another person develops neck pain which is similar to a previous episode that resolved spontaneously, he or she might choose not to seek care.
The main options available in most circumstances are no care, self-care (e.g., self massage, over-the-counter medication, hot compresses), and professional health care (conventional or alternative health care, e.g., attending the walk-in clinic nearby) (Fig 2).
Once the person with neck pain seeks health care, a chain of events — including assessment, diagnosis and management — begins to unfold. The particulars of assessment, diagnosis, and management will vary according to the setting, the chosen (or available) health care provider, and personal preferences. Persons with neck pain may have preferences for self-care versus health care, as well as preferences for specific care providers or management strategies. These preferences are influenced by both personal and environmental factors. Similar sets of factors, along with prior experience with the health care system, potentially influence the person's decision to (a) seek recurrent care, and (b) choose a certain type of care for subsequent episodes of neck pain.
The care complex encompasses the patient-provider nexus. This includes factors which affect — and are affected by — patient-provider interaction, including patient expectations, adverse events, compliance, patient satisfaction, and possible iatrogenesis. The patient-provider nexus is influenced by social, cultural, and environmental factors, as well as by more specific health policy factors.
Different health care disciplines have different standards for assessing, diagnosing and managing neck pain. Later in this document, we propose a 4-grade classification system of neck pain severity that we hope will be useful for all health care disciplines, and for neck pain of various types (traumatic and nontraumatic).
3. The “Participation” Complex
A person experiencing an episode of interfering neck pain would need to consider whether to modify his/her participation (defined in the ICF model as involvement in life situations, such as paid employment, leisure, or household responsibilities). [10] The options available to the individual vary greatly across settings and personal circumstances, for example, if stopping work means cutting off the only source of income, and the person has no savings, this would not be an option. If the person is a single parent caring for young children on his or her own, stopping the care of children because of neck pain may be very problematic.
In most other situations, the main options would be to continue participation as usual, to modify or adjust one or more areas of participation (e.g., avoid taking on extra work or going out with friends after work), or to stop participating in one or more sets of daily activities (e.g., stop working because neck pain interferes with an essential part of the job and modified duties are not available) (Fig 2).
By its nature, involvement in life situations implies interactions with other people. Thus the option to adapt one's involvement in life situations depends on negotiating one's own needs and motivation (in the context of neck pain and associated comorbidities) with the needs and demands of others. At work, demands are often defined as required job tasks which can be divided into essential and nonessential. As the required job tasks vary from job to job, neck pain of similar severity can prevent some people from working, and not others. Among other factors, this depends on the nature of their jobs, the degree of control they have over their job tasks, the available incentives to maintain participation, whether they can negotiate accommodations with supervisor and coworkers, and personal factors. [18, 19]
Similar situations apply to household responsibilities, except that the negotiation involves the other members of the household and their needs and demands. Neck pain may become particularly disabling if a person lives on his or her own, with no one else to help with or assume household responsibilities. If the person with neck pain plays a central supporting role in the household, the other household members may have to develop alternative skills or allow some of their needs to go unfulfilled until the person with neck pain recovers.
4. The “Claim” Complex
Filing a claim to access financial benefits is relevant only if a person has insurance. The exception is personal injury claims, as these are allowed by legislation in most countries irrespective of insurance availability.
The variation in claims allowance/availability across settings is broad. In some instances, simply filing a claim requires careful consideration (e.g., filing an auto insurance claim often requires paying a large deductible and may result in increased premiums). In other cases, this is not a problem (e.g., in some settings with universal health care coverage, the claim is automatically submitted by the health care provider with no requirement for direct payment). Options available in most developed countries include claims to pay for the cost of health care, disability claims to replace lost income or to hire assistance (e.g., worker's compensation claims), and personal injury claims for pain and suffering and/or punitive damages (Fig 2).
Where more than one option exists, the decision to file a claim will depend on how the person perceives his or her options. Three important elements are the insurance coverage contracted by the person before developing neck pain, the size of any copayment or deductible, and the amount of payable benefits, along with the perceived consequences of making a claim (future insurability, future premiums).
People might have little awareness of the existence and nature of insurance coverage. It is likely that the person with neck pain will have to spend time negotiating the insurance system, usually while he or she is in pain and feeling unwell. The existence and nature of insurance coverage often depend on society's attitudes and perceptions about illness and injury in general, and about neck pain in particular. For example, in some states or countries auto insurance is mandatory, in others is not; some countries have universal health care insurance, others do not; some countries have separate compensation systems for workers injured at work, others do not. Insurance policies can, in turn, influence attitudes and perceptions about neck pain and the filing of a claim when one develops neck pain. [27]
The care, participation, and claim complexes described above are interdependent. The linkage between them can vary — from being quite obvious to being quite subtle. For example, if a person decides not to seek care, it is obvious no claim will be made to reimburse health care expenses; likewise, if participation is not significantly curtailed, no disability claim will be generated.
But a clinician may impact participation in a more subtle way, for example, by recommending follow-up visits and tests that will interfere with work schedules. This might cause the patient to miss work or simply worry to the point that he or she decides it is better to stop working until the situation is clarified. Another example of “subtle effects” is when insurance policies require that clinicians with a specific background be involved in assessing someone with neck pain in order for disability claims to be accepted, as this will result in certain treatments be provided more often than others. The interdependence between the care, participation, and claim complexes is represented by double-headed arrows in Figure 2.
5. The Impacts and Outcomes of Neck Pain
The Neck Pain Task Force found it helpful to describe the impacts of neck pain in 5 domains:impact on body structures and functions (symptoms, signs, and other detectable changes to the body, also referred to in ICF as impairments),
impact on the person's ability to accomplish tasks (activities),
impact on the person's involvement in life situations (participation),
impact on the person's subjective wellbeing, and
impact on resource utilization. This is an extension of the ICF domains. [10]
The status in each domain can be described (on average) for groups of people at any point in the course of neck pain, and (more precisely) for a single person with neck pain. The impact of neck pain in each of these domains is modified by environmental and personal factors.
Short-term outcomes of neck pain are changes in the described domains over a relatively short period of time (e.g., before and after care is provided, or before and after a particular option to deal with neck pain is selected). Thus pain and related symptoms could disappear, persist, decrease or increase; and restrictions in activities and participation could also disappear, persist, decrease or increase. Often changes in the different domains will move in parallel (e.g., symptoms, activities, and participation all improve), but sometimes they will not (e.g., a rehabilitation program might produce some increase in pain, yet allow the person to return to work). When the short-term outcomes are unsatisfactory, and neck pain is still troublesome, the person will reconsider the original decisions about care, participation and claim one or more times within a given episode of interfering neck pain (Fig 2).
The long-term outcomes in the model are defined, following Beaton et al, as global personal appraisals of the impacts of neck pain over a long period of time (months to years). [17] Thus persons with neck pain might eventually regain a sense of “balance” and consider themselves recovered. This occurs not necessarily because all the symptoms and impacts of neck pain have disappeared (referred to by Beaton et al as “resolution”), but because activities and participation have been readjusted to a new status which the person deems acceptable (referred to by Beaton et al as “readjustment”), or because the person has been able to redefine personhood and his or her life goals (referred to by Beaton et al as “redefinition”). In some instances, interfering neck pain will persist, and the person will experience major ongoing unsatisfactory deficits in their activities and participation (i.e., long-term disability). [17]
Classification of Neck Pain and its Associated Disorders
A fundamental issue in interpreting scientific studies on neck pain and its associated disorders is agreeing on a parsimonious, meaningful set of case definitions. This is vital to the task of grouping studies and making sensible comparisons.
The conceptual model for the onset, course, and care of neck pain discussed in this chapter sets the 3 broad categories of no neck pain, noninterfering neck pain, and interfering neck pain as defined below (Fig 2):
The classification of no neck pain is made when the person answers negatively to any and all questions concerning the presence of neck pain or disorders associated with neck pain.
The classification of noninterfering neck pain is made when the presence of neck pain and/or an associated disorder is elicited from individuals, but the person does not seek care for this pain, does not file a claim, and he or she states that the pain does not result in restriction or change in activities or “participation.”
The classification of interfering neck pain is made when the presence of neck pain or an associated disorder is elicited from individuals, and when it causes the person to seek health care for this pain, file a claim for neck pain or when the person states that the pain results in activity/participation restrictions.
Table 1 These 3 broad categories are a good beginning, but they are insufficient to meaningfully interpret the scientific literature on neck pain and its associated disorders. In fact, more than 300 case definitions were used in the admissible studies considered by the Neck Pain Task Force. So the Neck Pain Task Force proposes the use of a 5-axis classification system to group published studies (Table 1).
The 5 axes are(1) the source of subjects and data,
(2) the setting or sampling frame,
(3) the severity of neck pain and its consequences,
(4) the duration of neck pain, and
(5) its pattern over time.We recommend that a full case definition in a neck pain study should define the corresponding category in each of these axes.
The fit between the Neck Pain Task Force conceptual model and the case definitions proposed above is not perfect at the present time. This is because case definitions reflect, in good part, what has been done rather than what the model suggests should be done. Future adherence to a common limited set of case definitions that fit better within our conceptual model of neck pain will greatly accelerate knowledge in the field of neck pain and its associated disorders. [28]
Sources of Subjects and Data
The first classification axis is relevant to research (or users of research) and relates to the source of subjects and data included in the study. It includes “neck pain in surveys,” “neck pain with health care,” and “neck pain with claim.” Although neck pain in surveys might be most relevant to epidemiologists, neck pain with health care to clinicians, and neck pain with claim to insurers; all of them will benefit from a global view that outlines similarities and differences.
Of course, at a personal level these are not exclusive categories, but most available studies can be classified into these 3 groups because authors often chose one of these sources for their study subjects. It follows from our conceptual model that choosing subjects in this way results in subsets that may not be comparable. Surveys can include both noninterfering and interfering neck pain, but neck pain with health care and neck pain with claim include (by definition) only interfering neck pain. Also, people can receive extensive health care but not file a claim if they have no insurance.
Our conceptual model also drives home the point that “neck pain with health care” and “neck pain with claim” cannot be fully understood in the absence of information about the health care and insurance systems in place at the time and location of the study.
Setting or Sampling Frame
The second axis of classification (again, relevant for research purposes) refers to the setting or sampling frame for study subjects.
In neck pain surveys, this can be divided into 4 categories: general population, employed populations, specific occupations, and injury surveillance during sporting events.
For studies of neck pain with health care, this can include one or more of the following settings: hospital emergency room, primary ambulatory care, secondary care, and tertiary care.
For neck pain with claim, this can include health insurance, auto insurance, workers' compensation insurance, and personal injury claims.
Severity of Neck Pain and Its Consequences
The third level of classification deals with the severity of neck pain and its consequences, and this level of classification is potentially useful to clinicians and policy makers, as well as researchers (and research users). The Neck Pain Task Force felt that a 4-grade categorization was manageable and sufficient. To develop such a categorization, we were guided by the classification system proposed by the Quebec Task Force on Whiplash Associated Disorders and by a classification system developed by von Korff et al. [11]
The Québec Task Force on WAD proposed a wellknown classification system which categorized neck pain which occurs after a traffic collision into grades 0 to 4.6 Briefly, this classification system is as follows:grade 0 WAD is “no complaint about the neck, no physical sign(s)”;
grade 1 WAD is “neck pain, stiffness, or tenderness, with no physical sign(s)”;
grade 2 WAD is “neck pain, stiffness, or tenderness with musculoskeletal sign(s)”;
grade 3 WAD is “neck pain, stiffness, or tenderness with neurologic signs”; and
grade 4 WAD is “neck fracture or dislocation.”The Neck Pain Task Force proposes to expand and adapt this WAD classification by integrating it with the pain classification system proposed by von Korff et al [11] Briefly, that classification is as follows:
grade I — pain of low intensity, and related to low levels of disability and interference with activities of daily living;
grade II — pain of high intensity, but associated with low levels of disability and interference with activities of daily living;
grade III — pain that is associated with high levels of disability and moderate limitations in activities of daily living; and
grade IV — pain that is associated with high levels of disability and severe limitations in activities of daily living.For neck pain in surveys, we recommend adopting the classification proposed by von Korff et al, [11] because it has known psychometric properties and prognostic implications. Surveys cannot generally capture detailed clinical information such as signs or symptoms.
The Neck Pain Task Force proposes a similar, but more detailed categorization system for neck pain with health care. Our goal in this endeavor was to produce a severity classification system that encompasses all neck pain syndromes, and that is relevant irrespective of the professional background of the health care provider and the circumstances surrounding the onset of pain (traffic collisions, sports, nontrauma, etc.). Thus, we propose that the assessment of a person with neck pain and associated disorders should distinguish 4 situations which have major management implications.
These are:
Grade I neck pain: Neck pain and associated disorders with no signs or symptoms suggestive of major structural pathology and no or minor interference with activities of daily living. Major structural pathologies include (but are not limited to) fracture, vertebral dislocation, injury to the spinal cord, infection, neoplasm, or systemic disease including the inflammatory arthropathies.
Grade II neck pain: No signs or symptoms of major structural pathology, but major interference with activities of daily living. [11]
Grade III neck pain: No signs or symptoms of major structural pathology, but presence of neurologic signs such as decreased deep tendon reflexes, weakness, or sensory deficits.
Grade IV neck pain: Signs or symptoms of major structural pathology.
The most significant differences from the original classification for WAD are:
There is no grade 0 (which, in the original WAD classification referred to “no neck pain”).
Grade II is distinguished from grade I by the presence of major interference with activities of daily living, rather than localized tenderness or restricted range of motion. Interference with daily living has larger prognostic and management implications than these relatively unreliable physical signs. [11, 29, 30]
Grade IV includes all major structural pathology, not only fractures.
The classification is applicable to all neck pain and associated disorders, not only WAD.
For neck pain with claim the Neck Pain Task Force recommends:
Grade I neck pain with claim for reimbursement of primary health care or car and equipment repair only
Grade II neck pain with claim for reimbursement of secondary/tertiary care or temporary wage replacement.
Grade III neck pain with claim for long-term disability.
Grade IV neck pain with claim for permanent disability or punitive damages for pain and suffering.
Duration of Neck Pain
The fourth axis of classification deals with the duration of neck pain. Homogeneous categories for neck pain in surveys, neck pain with care, and neck pain with claim are desirable, but might not be feasible at this stage because of the studies/data available. The following categories are proposed:1) transitory neck pain which lasted less than 7 days;
2) short-duration neck pain that lasted 7 days or more, but less than 3 months;
3) long-duration neck pain that lasted 3 months or more.
Pattern of Neck Pain
The fifth axis of classification deals with the pattern of neck pain over time. The following categories are proposed:(1) single episode, no neck pain before, full recovery afterwards (recovery preferably defined by self-report);
(2) Recurrent, 2 or more episodes of neck pain with full recovery in-between;
(3) Persistent, no periods of full recovery.The minimum period of full recovery required to distinguish recurrent from persistent neck pain might vary across studies, but it should be explicitly defined and ascertained.
The first 3 axes of the classification can be assigned shortly after onset, but axes fourth and fifth can only be assigned after a reasonable period of follow-up. For research purposes, the degree of confidence in comparing studies increases when their case definitions correspond in more axes. In other words, studies with case definitions which correspond in all 5 axes can be confidently interpreted together; however, confidence declines when studies only correspond in 3 or 2 axes. If studies are found to correspond at just one or in no axis, we believe comparisons should be avoided.
Implications of the Conceptual Model
The Neck Pain Task Force conceptual model of the onset, course, and care of neck pain presented in this chapter is the result of an iterative process spanning 6 years. It was generated through ongoing discussions by a multidisciplinary Scientific Secretariat reviewing the international literature on neck pain and its associated disorders.
The model describes neck pain as an episodic occurrence over a lifetime with variable degrees of recovery in between episodes. The model outlines options available to the person who is dealing with neck pain, the factors that determine available options, choices and consequences, and the short- and long-term impacts of neck pain.
The simplified graphical representation of the overall model is presented in Figure 2; the associated case definitions for neck pain studies are listed in Table 1. But we must emphasize that the most important part of the model is not the graphical representation (which is necessarily a simplified version of our conceptual model); rather, the important foundation of our proposed model is the underlying agreement on clear definitions when discussing important concepts and linkages. Thus the definitions and classifications for meaningful subgroups (case definitions), for factors related to course and management of neck pain, and the consequences and effect of neck pain on the individual are essential and integral to the model.
At its core, our conceptual model can be seen as a tool for appraising the status of a person with neck pain. It requires that we distinguish interfering from noninterfering neck pain, distinguish the various grades of neck pain from one another, and appraise both short- and long-term outcomes.
It is important to add that the results of such appraisals are highly dependent on the person doing the appraisal; they also depend on circumstances that delimit the options and ways of conducting the appraisal. This is explicitly discussed in the model for the person with neck pain, but similar contextual issues should also be considered when the appraiser is a health care provider, a supervisor or family member, or a claim adjudicator.
Besides its potential in helping categorize and interpret the available evidence about neck pain, we believe our conceptual model will have other uses:
It might be used to describe the overall burden of neck pain in a given population. We could say for example (fictional data), that “During the year 2025 in the Province of Ontario, Canada, for every one thousand adults in the population 200 experienced a new episode of neck pain, which was interfering for 60. Among these 60, 30 people sought health care during that year, and 6 filed a disability claim; 2 people became permanently disabled with neck pain.” [15, 20]
The model could also be used to inform decisions of a person experiencing neck pain, by helping him/her pinpoint the available options, the factors that determine those options, and the possible consequences associated with those options. [13, 31]
The model and case definitions of neck pain with health care can help inform clinician's decisions about assessment and management. [13, 31-34]
The model could also be used for group advocacy at the societal level to increase and improve available options for managing neck pain and to help define appropriate health care and insurance policies.
This chapter has introduced and described a new conceptual model for the onset, course, and care of neck pain. This model was developed and used by the Neck Pain Task Force to link the epidemiology of neck pain with its management, to organize, and interpret existing knowledge and to highlight knowledge gaps.
Besides being used for these explicit purposes, the Neck Pain Task Force hopes the new conceptual model will assist persons experiencing neck pain on making informed decisions, assist researchers in choosing their research questions, provide clinicians with an overall picture of neck pain which places their advice and treatment in perspective, and help policy makers realize how their decisions actually influence the onset, course, and care of neck pain in society.
The iterative process used for developing the model does not end with its publication. We expect that the model and case definitions will be revised periodically as more and better scientific evidence becomes available.
The Neck Pain Task Force hopes that our new conceptual model for the onset, course, and care of neck pain will signal a shift in our thinking about this widespread problem, and that it will open a constructive dialogue on how to best decrease the personal and societal burden of neck pain and its associated disorders.
Key Points
The international and multidisciplinary Decade of the Bone and Joint 2000–2010
Task Force on Neck Pain and its Associated Disorders proposes a new
conceptual model for the onset, course, care, and consequences
of neck pain, which was used to interpret available
scientific evidence.The model is centered on the person with neck pain or who is at risk for neck pain;
it describes neck pain as an episodic occurrence over a lifetime with
variable recovery between episodes.The model outlines the options which may be available to the person in dealing
with neck pain; the factors that determine available options, choices,
and consequences; and the short- and long-term impacts of neck pain.The model is multifactorial, reflecting the multiple environmental and personal
factors which affect the onset, course, and consequences of neck pain.The model includes a 5-axis classification of neck pain studies based on how
subjects were recruited into each study.Besides helping in the interpretation of scientific evidence, the model may
assist people with neck pain, researchers, clinicians, and policy makers
in framing their questions and decisions.
Acknowledgment
The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders was supported by grants from the following: National Chiropractic Mutual Insurance Company (USA); Canadian Chiropractic Protective Association (Canada); State Farm Insurance Company (USA); Insurance Bureau of Canada; Länsförsäkringar (Sweden); The Swedish Whiplash Commission; Jalan Pacific Inc. (Brazil); Amgen (USA). All funds received were unrestricted grants. Funders had no control in planning, research activities, analysis or results. The report was not released to grantors prior to publication and no approval was required from funders regarding the final report. Dr. Côté is supported by the Canadian Institutes of Health Research through a New Investigator Award and by the Institute for Work & Health through the Workplace Safety and Insurance Board of Ontario. Dr. van der Velde is supported by the Canadian Institutes of Health Research through a Fellowship Award. Dr. Carroll is supported by a Health Scholar Award from the Alberta Heritage Foundation for Medical Research. Dr. Cassidy is supported by an endowed research chair from the University Health Network.
References:
Bliss, SJ, Flanders, SA, and Saint, S.
Clinical problem-solving. A pain in the neck.
N Engl J Med. 2004; 350: 1037–1042Harris, ED, Budd, R, Firestein, GS et al.
Neck Pain. Kelley's Textbook of Rheumatology.
7 ed. Elsevier, ; 2006Haldeman, S, Carroll, LJ, and Cassidy, JD.
Introduction/mandate: the empowerment of people with neck pain.
The Bone and Joint Decade 2000–2010 Task Force on Neck Pain
and Its Associated Disorders.
Spine. 2007;Carroll, LJ, Cassidy, JD, Peloso, PM et al.
Methods for the Best Evidence Synthesis on Neck Pain and its Associated Disorders:
Results of the Bone Joint Decade 2000–2010 Task Force on
Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S33–38International Association for the Study of Pain (IASP).
IASP Task Force for Taxonomy.
Pain Terminology. IASP, Seattle; 2004Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Bongers, PM, Ijmker, S, van den, HS et al.
Epidemiology of work related neck and upper limb problems:
psychosocial and personal risk factors (part I) and effective interventions
from a bio behavioural perspective (part II).
J Occup Rehabil. 2006; 16: 279–302Dorshimer, GW and Kelly, M.
Cervical pain in the athlete: common conditions and treatment.
Prim Care. 2005; 32: 231–243Borghouts, JA, Koes, BW, and Bouter, LM.
The clinical course and prognostic factors of non-specific neck pain:
a systematic review.
Pain. 1998; 77: 1–13World Health Organization.
International Classification of Function, Disability and Health:
ICF. WHO, Geneva; 2001Von Korff, M, Ormel, J, Keefe, FJ et al.
Grading the severity of chronic pain.
Pain. 1992; 50: 133–149Côté, P, Cassidy, JD, Carroll, L et al.
A systematic review of the prognosis of acute whiplash and a new
conceptual framework to synthesize the literature.
Spine. 2001; 26: E445–E458van der Velde, G, Hogg-Johnson, S, Bayoumi, A et al.
Identifying the best treatment among common non-invasive
neck pain treatments: a decision analysis.
Spine. 2008; 33: S184–S191Bot, SD, van der Waal, JM, Terwee, CB et al
Predictors of outcome in neck and shoulder symptoms:
a cohort study in general practice.
Spine. 2005; 30: E459–E470Carroll, LJ, Hogg-Johnson, S, van der Velde, G et al.
Course and Prognostic Factors for Neck Pain in the General Population:
Results of the Bone and Joint Decade 2000–2010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S75–82Hadler, NM.
in: Occupational Musculoskeletal Disorders. 3 ed.
Lippincott Williams & Wilkins, Philadelphia; 2005: 1–339Beaton, DE, Tarasuk, V, Katz, JN et al
Are you better? A qualitative study of the meaning of recovery.
Arthritis Rheum. 2001; 45: 270–279Ariens, GA, van Mechelen, W, Bongers, PM et al.
Physical risk factors for neck pain.
Scand J Work Environ Health. 2000; 26: 7–19Ariens, GA, van Mechelen, W, Bongers, PM et al.
Psychosocial risk factors for neck pain: a systematic review.
Am J Ind Med. 2001; 39: 180–193Hogg-Johnson, S., van der Velde, G., Carroll, L. J. et al (2008).
The Burden and Determinants of Neck Pain in the General Population:
Results of the Bone and Joint Decade 2000–2010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S39–51Stahl, M, Mikkelsson, M, Kautiainen, H et al.
Neck pain in adolescence. A 4-year follow-up of pain-free preadolescents.
Pain. 2004; 110: 427–431van Gent, C, Dols, J, de Rover, C et al.
The weight of schoolbags and the occurrence of neck, shoulder,
and back pain in young adolescents.
Spine. 2003; 9: 916–921Carragee, EJ, Hurwitz, EL, and Haldeman, S.
The Pyrite standard: the Midas touch in the diagnosis of axial pain syndromes.
Spine. 2007; 7: 27–31Hartling, L, Brison, RJ, Ardern, C et al.
Prognostic value of the Quebec classification of Whiplash-associated disorders.
Spine. 2001; 26: 36–41Cote P, van der Velde G, Cassidy JD, Carroll LJ, Hogg-Johnson S, Holm LW, et al.
The Burden and Determinants of Neck Pain in Workers:
Results of the Bone and Joint Decade 2000–2010 Task Force on
Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S60-74Holm, LW, Carroll, LJ, Cassidy, JD et al.
The Burden and Determinants of Neck Pain in Whiplash-associated Disorders
after Traffic Collisions: Results of the Bone and Joint Decade 2000–2010
Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S52-59Cassidy, JD, Carroll, LJ, Côté, P et al.
Effect of eliminating compensation for pain and suffering on the outcome
of insurance claims for whiplash injury.
N Engl J Med. 2000; 342: 1179–1186Carroll LJ, Hurwitz EL, Côté P, Hogg-Johnson S, Carragee EJ.
Research Priorities and Methodological Implications: The Bone and Joint Decade
2000-2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S214–S220Suissa, S, Harder, S, and Veilleux, M.
The relation between initial symptoms and signs and the prognosis of whiplash.
Eur Spine J. 2001; 10: 44–49Altman, DG and Bland, JM.
Diagnostic tests. 1: Sensitivity and specificity.
BMJ. 1994; 308: 1552Guzman J, Haldeman S, Carroll LJ, et al.
Clinical Practice Implications of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders:
From Concepts and Findings to Recommendations
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S199–S212Nordin M, Carragee EJ, Hogg-Johnson S, Weiner SS, Hurwitz EL, Peloso PM, et al.
Assessment of Neck Pain and Its Associated Disorders: Results of the Bone and Joint Decade
2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S101–S122Hurwitz, EL, Carragee, EJ, van der Velde, G et al.
Treatment of Neck Pain: Noninvasive Interventions: Results of the
Bone and Joint Decade 2000–2010 Task Force on Neck Pain
and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123–152Carragee EJ, Hurwitz EL, Cheng I, Carroll LJ, Nordin M, Guzman J, et al.
Treatment of Neck Pain: Injections and Surgical Interventions: Results of the Bone and Joint Decade
2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S153–169
Return to WHIPLASH
Return to CHRONIC NECK PAIN
Return to INTEGRATED HEALTH CARE
Since 9-25-2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |