A Systematic Review of Chiropractic Management of Adults
with Whiplash-Associated Disorders: Recommendations for
Advancing Evidence-based Practice and ResearchThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Work. 2010; 35 (3): 369–394 ~ FULL TEXT
Lynn Shaw, Martin Descarreaux, Roland Bryans, Mireille Duranleau,
Henri Marcoux, Brock Potter, Rick Ruegg, Robert Watkin, Eleanor White
The literature relevant to the treatment of Whiplash Associated Disorders (WAD) is extensive and heterogeneous.
Methods: A Participatory Action Research (PAR) approach was used to engage a chiropractic community of practice and stakeholders in a systematic Review to address a general question: ‘Does chiropractic management of WAD clients have an effect on improving health status?’ A systematic review of the empirical studies relevant to WAD interventions was conducted followed by a review of the evidence.
Results: The initial search identified 1155 articles. Ninety-two of the articles were retrieved, and 27 articles consistent with specific criteria of WAD intervention were analyzed in-depth. The best evidence supporting the chiropractic management of clients with WAD is reported. For the review identified ways to overcome gaps needed to inform clinical practice and culminated in the development of a proposed care model: The WAD-Plus Model.
Conclusions: There is a baseline of evidence that suggests chiropractic care improves the cervical range of motion (cROM) and pain in the management of WAD. However, the level of this evidence relevant to clinical practice remains low or draws on clinical consensus at this time. The WAD-Plus Model has implications for use by chiropractors and interdisciplinary professionals in the assessment and management of acute, sub-acute and chronic pain due to WAD. Furthermore, the WAD-Plus Model can be used in the future study of interventions and outcomes to advanced evidenced-based care in the management of WAD.
Background
Whiplash Associated Disorder (WAD) is a clinical condition that occurs with acceleration or deceleration of the head and neck in relation to other parts of the body. This typically occurs during motor vehicle collisions or other mishaps.
There are major health concerns that have a disruptive effect on the daily lives of many people around the world [1]. The chiropractic community has provided leadership with respect to interventions that support the clinical management of those suffering from WAD injuries [2, 3]. Over the past several years, there has been a paradigm shift in the body of knowledge that is used to guide management of WAD injuries. Evidence-based knowledge is being used more vehemently to guide treatment management and decision-making practices in the profession.
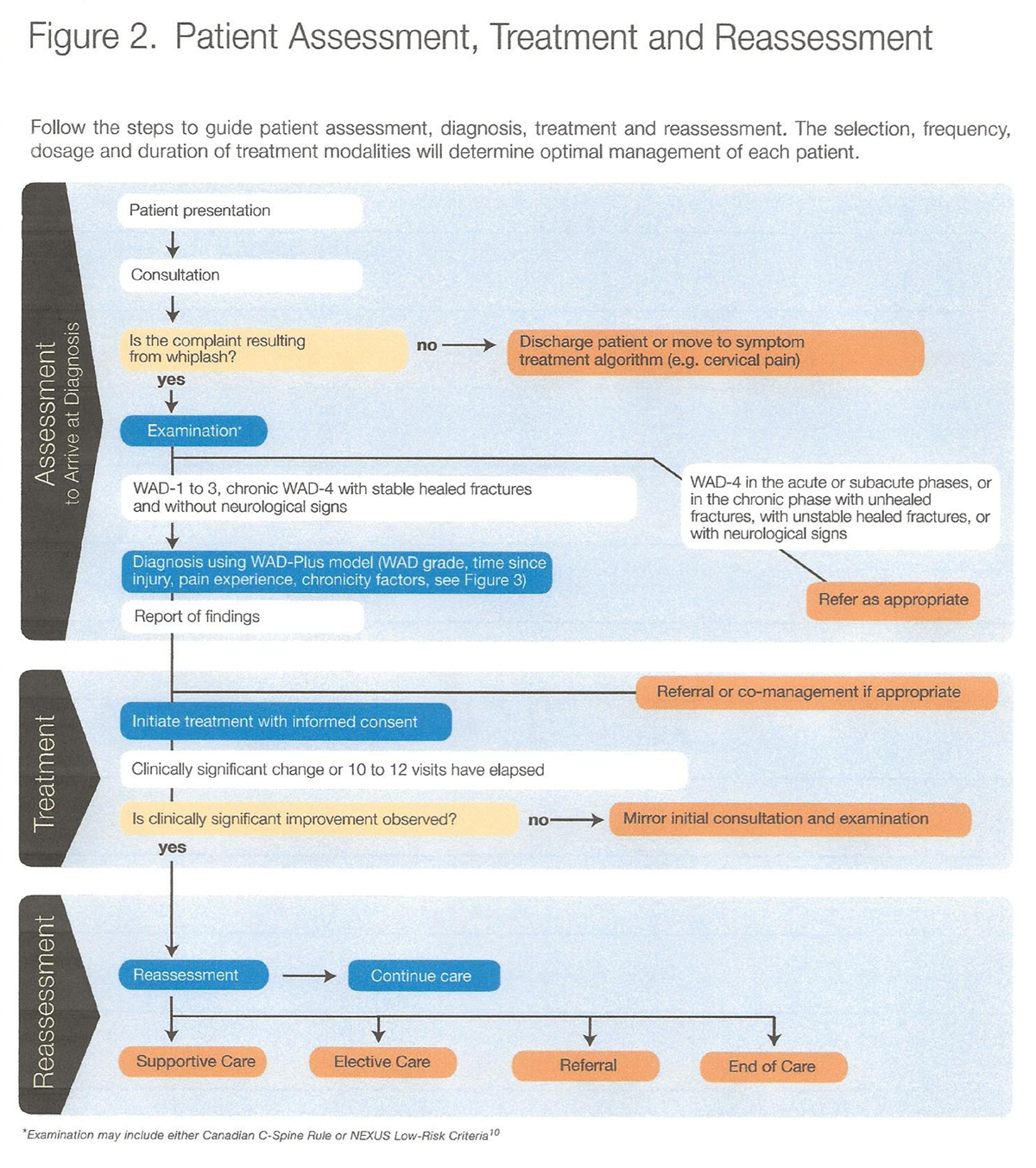
The Clinical Practice Guidelines Task Force (CPGTF) and the Guidelines Development Committee (GDC) reviewed various evidence-based management and knowledge models to development protocols for treating Whiplash Associated Disorders. They also provided recommendations with respect to the management of WAD injuries in the acute, sub-acute and chronic phases, and the development of the WAD-Plus model guideline.
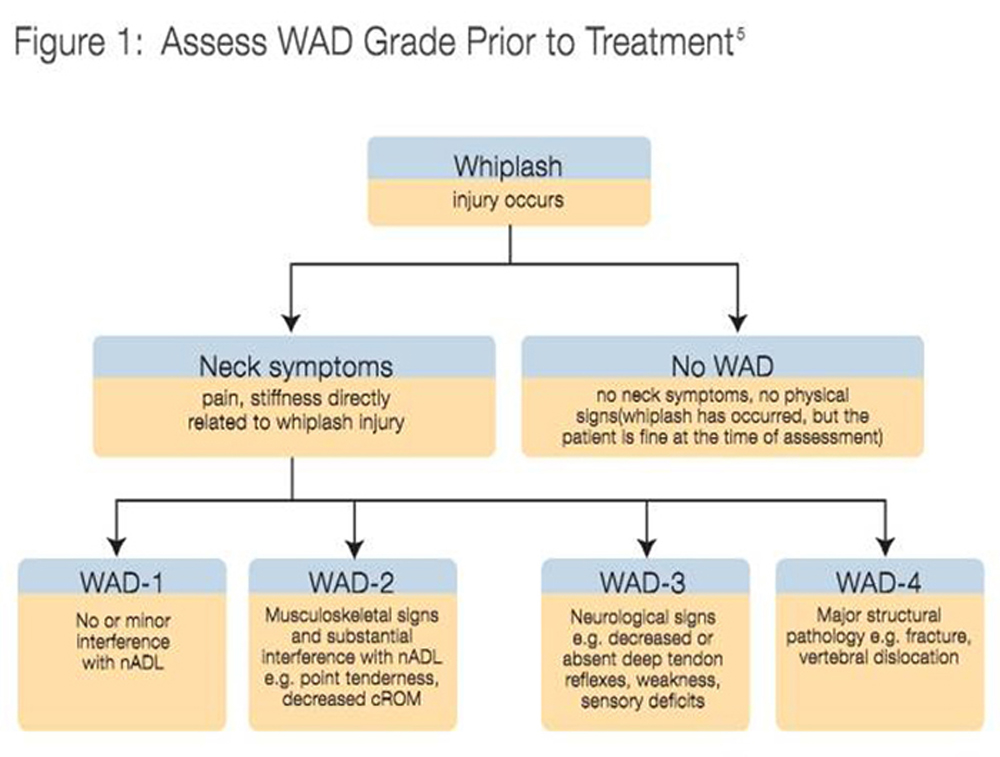
This paper reviews the clinical definition of WAD and their grades. The definitions include – but are not limited to – the prevalence and/or severity of the following factors: neck pain, musculoskeletal signs (i.e., hyperalgesia, movement loss, stiffness, kinesthetic deficits, balance loss), deafness, dizziness, tinnitus, headache, memory loss, dysphasia, temporomandibular (TMJ) pain, radiating symptoms, neurological and orthopaedic sequelae [2, 4]. The most common intervention reviewed and discussed in the chiropractic community is the adjustment [5].
Results
Chiropractic care has been shown to improve cervical range-of-motion (cROM) and pain management in WAD cases.
Methods were identified to overcome deficiencies in the research and the current (traditional) WAD model
Clinical practice guidelines and the development of a proposed care model (the WAD-plus Model)
Development of the WAD-Plus Model to advance evidence-based care and the management of whiplash injuries that embodies critical contributory factors to recovery such as the ‘pain experience’ and the chronicity of injuries.
GDC (Guidelines Development Committee) Findings & Recommendations
Acute Phase WAD Cases: The literature provided sufficient evidence to establish that acute WAD patients may benefit from a combination of the following modalities: early mobilization, education/instruction, unsupervised and supervised cervical ROM exercises with multimodal treatment regimens [6–9]. The GDC recommends a balanced passive and active care as well encouraging the patient to resume normal daily activities at the earliest interval. Evidence does not support the use of collars or immobilizing devices to improve health outcomes in this (or any) phase of the WAD injury.
Sub-acute Phase WAD Cases: Literature suggests in this stage the patient may benefit from multiple modalities including: posture instruction, mobilization, massage and cervical ROM exercise. Treatment that is less complex and less costly is recommended as well as the treatment that is least likely to contribute toward a propensity for chronic WAD. The exercise protocols varied greatly in the literature and should be prescribed based on clinical experience and the patient's own specific situation [10, 11]. GDC stated that further investigation is required to evaluate the effects of treatment in sub-acute WAD cases. The GDC additionally advised that the practitioner should use a balanced approach of active and passive therapy, but should become increasingly more active during this phase of care.
Chronic Phase WAD Cases: Health outcomes in this phase were expanded to include not only pain perception and cervical ROM improvement, but additionally: posture, perceived disability, coping resources and life satisfaction [12–16]. Best evidence suggests that in this stage a combination of unsupervised and supervised exercise, and cognitive behavioral therapy should be incorporated. Active intervention and independence is encouraged in this phase. The evidence suggests that health outcomes of chronic WAD is more likely to improve if the patient is actively involved in the care – characterized by active involvement and responsibility by both the practitioner and patient (i.e., independent exercise, self-directed applications of cryotherapy, portable TENS/IFC units, etc.) can maximize health outcomes. The GDC consensus is to balance active and passive care (as discussed in the earlier phases) in relation to the patient's clinical presentation.
GDC Recommendations for Improving the Literature: In general the GDC advocates that efforts are required to improve the rigor and quality of studies evaluating the effect of chiropractic treatment in WAD cases. It was suggested that the WAD-Plus Model might enhance the comparison of studies relevant to advancing chiropractic management of WAD. Gaps in current evidence on WAD intervention acknowledge that their review does not provide a comprehensive review of all chiropractic treatment modalities and techniques. Future WAD research should also utilize “active comparators,” non-treatment and/or placebo groups to enhance evidence-based research on WAD outcomes and patient management [17, 18]
The WAD-Plus model
The GDC put forth the WAD-Plus Model to advance the management of whiplash associated disorders and improving consistency and clinical management. The model refers to the assessment and defining of a WAD injury using conventional methods (i.e., Standard WAD 1, WAD 2, WAD 3, and WAD 4 definitions). Plus, three additional important dimensions relevant for client care:
1. The Time Since Injury: generally accepted stages of soft tissue injury are classified into the inflammation, repair and remodeling stages [19]. The GDC consensus is that the practitioner should identify the individual’s phase of healing prior to starting care – as treatment intervention may vary depending on what stage of healing they are in.
2. The Pain Experience: This embodies psychosocial features of injury and pain experience. Individual's perception of pain, self-perceived disability, the meaning of their symptoms and how to best manage them are pertinent factors in the recovery process [20]. Pain perception can vary depending on: gender, belief in the effectiveness of treatment, strong emotional states, cultural, family and work factors [20–23]. The GDC deemed the following evaluative measures were helpful in quantifying psychosocial pain and the need for multidisciplinary care: Bournemouth Questionnaire, McGill Pain Questionnaire, Self-Efficacy Scale and Pain Catastrophizing Scale. The GDC recommends if the individual has a high degree of psychosocial pain, the focus should be on multidisciplinary management or behavioral components outside of chiropractic care.
3. Chronicity Factors: The GDC recommended that the practitioner should carefully consider the following criteria for potential chronicity factors: socioeconomic factors; psychosocial factors, prior health status, symptom severity, compensation and legal factors, health behaviors, attitudes and interventions contemplated. [1]
The GDC recommends that all four dimensions of the WAD-Plus Model should be considered as part of WAD care.
Conclusions / Clinical Applications
The development of guidelines to improve the assessment of WAD grades prior to beginning treatment. This guide is available to all practitioners through the Canadian Chiropractic Association's website (see additional readings).
The WAD-Plus Model was developed to identify clinical musculoskeletal signs & symptoms described in the original WAD model. However, the WAD-Plus Model takes further steps to consider the elapsed time since the accident, the pain experience and potential chronicity factors.
The WAD-plus model is an expanded model of care that includes the conventional dimensions of patient care plus three other important dimensions discussed earlier: time since injury, pain experience and chronicity factors. The practitioner should incorporate into his/her clinical management model the time since injury (i.e., acute, sub-acute and chronic), the pain experience (psychosocial factors, etc.); and potential chronicity factors (demographic, socioeconomics prior health status, symptom severity, compensation and legal factors, and health behaviors). The GDC advises that all of these factors have a bearing on the frequency, duration and scope of chiropractic intervention.
Study Strengths/Weaknesses
Systematic review including literature search, review of evidence, selection for relevance, quality assessment, evidence synthesis, quantity/consistency of evidence and interpretation of knowledge for advancing the management of WAD. Systematic reviews are inherently weak in terms of study design. However it should be noted that for discussion of such a topic such as the creation of guidelines, this method would be considered appropriate.
In my opinion the authors presented a balanced summary of the existing literature and integrated it quite well into a model for advancing the management of Whiplash Associated Disorders and further research in this area.
This study method is generally used in guiding healthcare decision-making processes and considered a reasonable approach in developing best-evidence practice guidelines [24].
The participatory action research (PAR) method used in this study embodied the process of systematic review and its application in general practice [25]. This incorporates the process of:
Defining the Problem – in this case the need to establish baseline evidence on chiropractic care in the management of WAD injuries
Planning – the process for review and analysis of information using source evidence review and best evidence synthesis (including literature search, selection for relevance, quality assessment and synthesis) [26]
Data Generation – by way of systematic review, data extraction and analysis
Analysis and Interpretation – best evidence synthesis relevant to chiropractic treatment
Action – GDC recommendations and the WAD-plus model, and
Evaluation – feedback from stakeholders and practitioners
References:
1. Carroll, LJ, Hogg-Johnson, S, van der Velde, G et al.
Course and Prognostic Factors for Neck Pain in the General Population:
Results of the Bone and Joint Decade 2000–2010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S75–82
2. Spitzer, W., Skovorn, M., et al.
Scientific Monograph of the Québec Task Force on Whiplash-Associated Disorders:
Redefining Whiplash and Its Management.
Spine 1995, 20 (8S), S1-73.
3. Bryans, R.
Whiplash - A Practitioner's Guide to Understanding Whiplash Associated Disorders (WAD).
Canadian Chiropractic Association, 1999.
4. Sterling, M. & Kennedy, J.
Physical and Psychological Aspects of Whiplash:
Important Considerations for Primary Care Assessment.
Manual Therapy 2008 (May); 13 (2): 93–102
5. Coulter, I., Shekelle, P.
Chiropractic in North America: a Descriptive Analysis.
J Manipulative Physio Ther, 28(2) 2005, 83-89.
6. Bonk, A., Ferrari, R., Giebel, G., et al.
Prospective, Randomized, Controlled Study of Activity Versus Collar and the Natural History for Whiplash Injury in Germany.
J Musculoskeletal Pain 8(1-2) 2000, 123-132.
7. Crawford, J., Khan, R., and Varley, G.
Gurley Management and Outcome Following Soft Tissue Injuries of the Neck - A Randomized Controlled Trial.
Injury (35), 2004, 891-895.
8. McKinney, L.
Early Mobilization and Outcome in Acute Sprains of the Neck.
BMJ 299(6706), 1989, 1006-1008.
9. Mealy, K. Brennan, H. & Fenelon, G.
Early Mobilization of the Key Whiplash Injuries.
BMJ (Clin Res Ed) 292(6521) 1986, 656-657.
10. Provinciali, L., Baroni, M, et al.
Multimodal Treatment to Prevent the Late Whiplash Syndrome.
Scand J Rehabil Med 28(2) 1996, 105-111.
11. Soderlund, A., Olerud, C., and Lindberg, P.
Acute Whiplash Associated Disorder (WAD): The Effects of Early Mobilization and Prognostic Factors in Long-Term Symptomatology.
Clin Rehabil, 14(5) 2000, 457-467.
12. Fitz-Rison, D.
Phasic Exercises for Cervical Rehabilitation after Whiplash Trauma.
J Manipulative Physiol Ther, 18(1) 1995, 21-24.
13. Heikkila, H., Heikkila, E., Eisemann.
Predictive Factors for the Outcome of a Multidisciplinary Pain Rehabilitation Program on Sick Leave and Life Satisfaction in Patients with Whiplash, and Other Myofascial Pain: a Follow-Up Study.
Clin Rehabil, 12(6) 1998, 487-496.
14. Soderlun, A. and Lindberg, P.
Cognitive Behavioral Components and Physiotherapy Management of Chronic Whiplash Associated Disorders (WAD) - A Randomized Group Study.
Physiotherapy Theory and Practice, 17(4) 2001, 229-239.
15. Sterner, Y., Lofgren, M., et al.
Early Interdisciplinary Rehabilitation Program for Whiplash Associated Disorders.
Disabil Rehabil, 23(10) 2001, 422-429.
16. Vendrig, A., van Akkerveeken, P, et al.
Results of a Multimodal Treatment Program for Patients with Chronic Symptoms after a Whiplash Injury of the Neck.
Spine, 25(2) 2000, 238-244.
17. Altman, D., Schulz, K., et al.
The Revised Consort Statement for Reporting Randomized Trials: Explanation and Elaboration.
Ann Intern Med, 134(8) 2001, 663-694.
18. Des Jarlais, D. Lyles, C., et al.
Improving the Reporting Quality of Nonrandomized Evaluations of Behavioral and Public Health Interventions: The Trend Statement.
Am J Public Health, 94(3) 2004, 361-366.
19. Kumar, V., Abbas, A., et al.
Tissue Renewal and Repair: Regeneration, Healing and Fibrosis in Pathological Basis of Disease (Volume 7).
Robbins & Cotran, 2004, 87-118.
20. Merskey, H. and Bogduk, N.
IASP Task Force on Taxonomy, Classification of Chronic Pain: Descriptions of Chronic Pain Symptoms and Definition of Pain Terms (Vol. 2).
IASP Press, Seattle: 1994, 209-214.
21. Jordan, A. and Ostergaard, K.
Rehabilitation of Neck/Shoulder Patience in Primary Health Care Clinics.
J Manipulative Physiol Ther, 19(1) 1996, 32-35.
22. Liebenson, C.
Functional Reactivation for Neck Pain Patients.
J Bodywork Movement Ther, 2002, 6(1): 59-66.
23. Rodriquez, A., Barr, K., Burns, S.
Whiplash: Pathophysiology, Diagnosis, Treatment and Prognosis.
Muscle Nerve 29(6) 2004, 768-781.
24. Skinner, K.,
Developing a Tool to Measure and Knowledge Exchange Outcomes.
Canadian Journal of Program Evaluation (2007) 22, 49-73.
25. Speziale, H., Carpenter, D.
Qualitative Research in Nursing: Advancing the Humanistic Imperative (Volume 3).
Lippincott, Williams and Wilkins, Philadelphia, 2003.
26. Slavin, R.
Best Evidence Synthesis: An Intelligent Alternative to Meta-Analysis.
J Clin Epidemiol, 48(1) 1995, 9-18.
Additional Readings:
Canadian Chiropractic Association (June 2010)
Practice Guide for the Management of Whiplash-Associated Disorders in Adults .

Return to WHIPLASH
Since 6-01-2011


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |