

Mechanism of Whiplash Injury This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Clinical Biomechanics 1998 (Jun); 13 (4-5): 239-249 ~ FULL TEXT
OPEN ACCESS Manohar M. Panjabi • Jacek Cholewicki • Kimio Nibu • Jonathan N. Grauer • Lawrence B. Babat • Jiri Dvorakd
Biomechanics Laboratory,
Department of Orthopaedics and Rehabilitation,
Yale University School of Medicine,
New Haven, CT, USA.
OBJECTIVE: To propose a different hypothesis of whiplash injury mechanism based on a series of experimental studies summarized in this communication.
DESIGN: A series of biomechanical studies simulating whiplash trauma using isolated human cadaveric spine specimens.
BACKGROUND: Whiplash injuries are on the rise as reported in several recent studies, due primarily to the increased traffic density. Although the symptoms associated with whiplash have been described, our understanding of the injury mechanism remains poor. The prevailing view of neck hyper-extension causing the injury has not been supported by recent experimental studies.
METHODS: Eight fresh human cadaveric cervical spine specimens were prepared and traumatized to varying degrees under controlled conditions using a bench-top model of whiplash trauma. Before and after each trauma, the specimen was studied by functional radiography and flexibility test to document changes in the anatomic alignment and biomechanical properties at each level indicating injuries sustained. At the end of all testing, CT-scans, MRI and cryomicrotome images were obtained. During each trauma, relative motions of all intervertebral joints were recorded with a high speed movie camera. Elongations of the vertebral artery and several capsular ligaments were also monitored during the trauma using specially designed transducers.
RESULTS: The hyper-extension hypothesis of injury mechanism was not supported by these studies. We found a distinct bi-phasic kinematic response of the cervical spine to whiplash trauma. In the first phase, the spine formed an S-shaped curve with flexion at the upper levels and hyper-extension at the lower levels. In the second phase, all levels of the cervical spine were extended, and the head reached its maximum extension. The occurrence of anterior injuries in the lower levels in the first phase was confirmed by functional radiography, flexibility tests and imaging modalities. The largest dynamic elongation of the capsular ligaments was observed at C6–C7 level during the initial S-shaped phase of whiplash. Similarly, the maximum elongation of the vertebral artery occurred during the S-shape phase of whiplash.
CONCLUSION: We propose, based upon our experimental findings, that the lower cervical spine is injured in hyperextension when the spine forms an S-shaped curve. Further, this occurs in the first whiplash phase before the neck is fully extended. At higher trauma accelerations, there is a tendency for the injuries to occur at the upper levels of the cervical spine. Our findings provide truer understanding of whiplash trauma and may help in improving the diagnosis, treatment, and prevention of these injuries.
RELEVANCE: Although the symptoms associated with whiplash have been described, our understanding of the injury mechanism remains poor. Understanding the mechanism of injury is important. Knowing the correct injury mechanism will indicate where the potential injury sites are, and which anatomic elements are more likely to be injured. Additionally, it may also help in developing more effective injury prevention strategies.
From the FULL TEXT Article:
Introduction
Fifty percent of car to car traffic accidents in Japan result in neck injuries. [1] Reports from several European countries indicate an alarming increase in the annual number of neck injuries in recent years owing to the increased traffic density. [2] The National Highway Traffic Safety Administration in the USA estimates that 84% of all neck injuries are classified as AISI, i.e. soft tissue injuries. [3] Such injuries are most commonly sub-failure injuries; there are no complete failures of soft tissues. Although, the presently available imaging methods, such as MRI, often do not have sufficient resolution to identify these injuries, the decreased function and long-term pain associated with whiplash trauma may be explained by these sub-failure injuries.
Whiplash has been loosely defined as an acceleration injury and most commonly involves an unaware victim in a stationary vehicle being struck from behind. Resulting symptoms, including neck pain, dizziness, and headaches, are non-specific and are reported up to months or years after accidents. [4–6] Whiplash investigations have ranged from reviews of clinical data to a number of different laboratory approaches. Nevertheless, a solid understanding of whiplash injuries requires knowledge of intervertebral kinematics, and a clear definition of what constitutes a soft tissue injury. The relatively recent Quebec Task Force on WhiplashAssociated Disorders found the need for further biomechanical information about whiplash. [7]
Several attempts have been made to define the mechanism of whiplash injuries. Macnab, realizing the difficulties of clinical studies, turned to experimental trauma of anesthetized monkeys. [8–10] He found a predominance of anterior element injuries. He hypothesized that it is the hyper-extension of the cervical spine that caused the injuries.
Penning postulated that the primary mechanism of whiplash injury is hyper-translation of the head as opposed to the more conventional view of hyper-extension. [11, 12] He studied lateral radiographs of “chin-in and chin-out” subjects as representative of posterior and anterior head translations. He then compared associated intervertebral sagittal plane rotations with those of actively flexed and extended functional radiographs. He found that the rotations of the cranio-vertebra1 junction (CO–C2) were greater with simple head translations than with head flexion and extension. This was not the case for the lower cervical intervertebral joints. He thus concluded that upper level injuries should predominate in whiplash trauma.
Understanding the mechanism of injury is important. Knowing the correct injury mechanism will indicate where the potential injury sites are, and which anatomic elements are more likely to be injured. Additionally, it may also help in developing more effective injury prevention strategies. Based upon the Macnab theory of hyperextension as the injury mechanism in whiplash, the head-restraint was designed to prevent neck injuries in rear-end collisions by blocking the hyper-extension of the neck. Although the head-restraint has decreased the injuries, it did not eliminate them. In a study in Sweden, Nygren and co-workers found only a 20% decrease in neck injuries after the introduction of the head-restraint. [13] This would suggest that the hyper-extension injury mechanism, first proposed by Macnab more than thirty years ago and currently the most prevalent view, needs to be re-examined. [9]
The purpose of this communication was to consolidate and present our findings from a set of previously published studies on whiplash biomechanics. The goals of these studies were several: to document quantitatively the intervertebral rotations during experimental whiplash trauma; to quantify the functional injuries to each level of the cervical spine; to measure dynamic elongations of vertebral artery and capsular ligaments; to image the actual injuries that occurred; and, based upon the experimental findings, to propose an injury mechanism for whiplash trauma. These studies utilized a fresh cadaveric human spine specimen and a newly developed bench-top whiplash minisled. We have studied the human cervical spines in a highly controlled and instrumented system. Intervertebral rotations were tracked with high speed cinematography. Head and sled kinematics and soft tissue elongations were recorded by specially developed instrumentation. Injuries to the cervical spine were quantified by a multi-directional flexibility test and various imaging modalities.
Methods
Overview
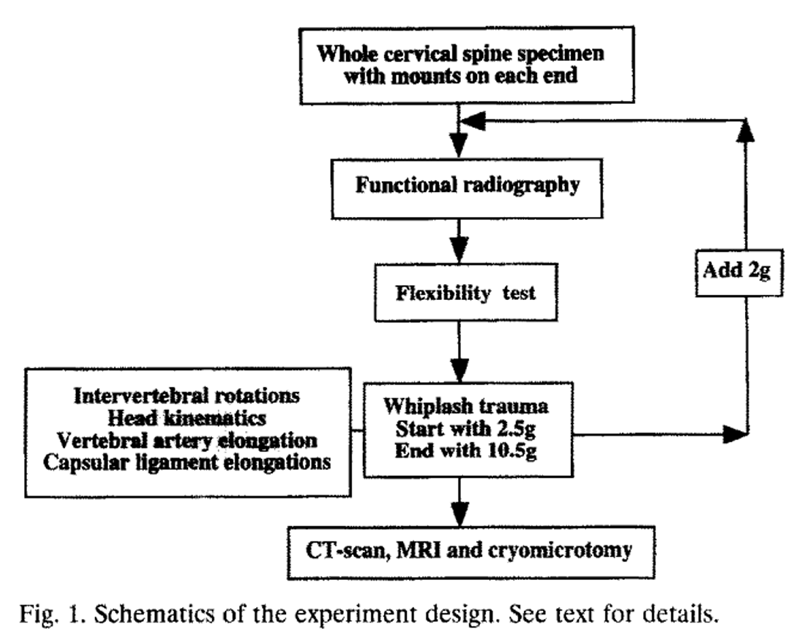
Figure 1 The methodological scheme is given in Figure 1. A fresh cadaveric cervical spine specimen including the occiput was prepared and provided with mounts on each end. Functional radiographs and multidirectional flexibility test documented and quantified the physical and mechanical properties of the specimen. The specimen was provided with appropriate head surrogate and was subjected to simulated whiplash trauma, starting with 2.5 g sled acceleration and ending with 10.5 g, in 2 g increments. During the trauma the specimen intervertebral rotations were filmed by a high speed movie camera. Head motion (rotation, translations and accelerations) was recorded by attached potentiometers and accelerometers. Dynamic elongations of the vertebral artery and capsular ligaments were monitored with specially designed transducers. The functional radiographs and flexibility test were repeated after each trauma to quantify the injury. Finaliy, the injury was visualized by CT-scan, MRI and cryomicrotomy.
Specimens and their preparation
Eight fresh cadaveric whole human cervical spine specimens (4 occiput to C7 and 4 occiput to Tl) were radiographed, to ensure only the normal degenerative changes were present. They were then cleaned of musculature, with care to preserve the discs and ligaments. The occiput and C7 or Tl vertebrae were mounted in quick setting epoxy mounts white the specimen was held in neutral posture. The specimens, sealed in double-plastic bags, were stored at –20°C and thawed before the testing.
Simulated Whiplash Trauma
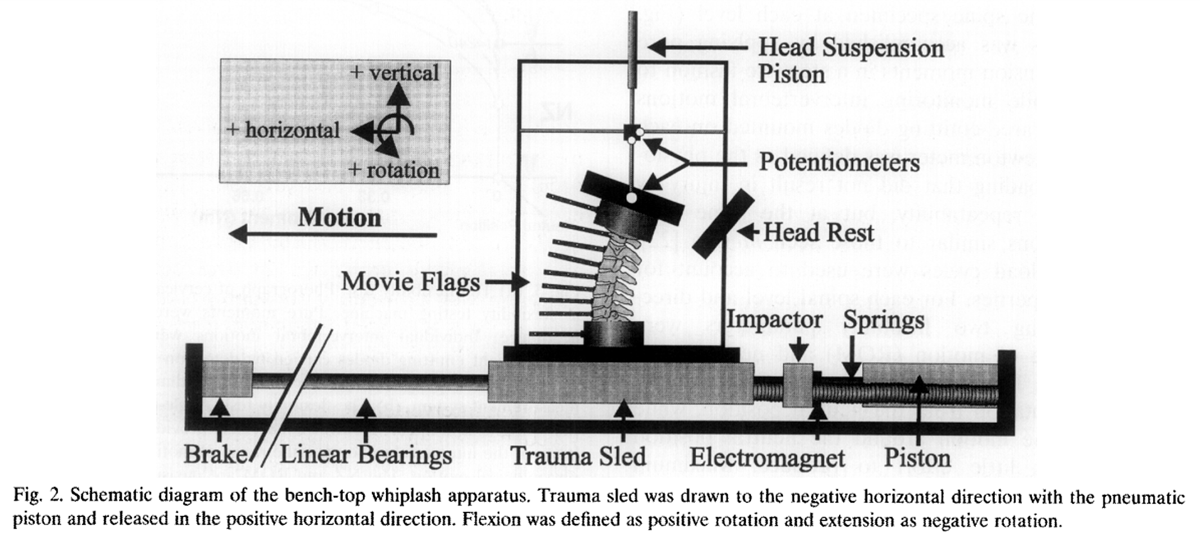
Figure 2 The whiplash trauma was produced with a specially developed trauma apparatus (Figure 2). [14] A trauma sled was mounted on horizontal linear bearings and was accelerated by a pneumatic piston, power springs, and an electromagnet release. The lower end of each spine specimen was attached to the sled while the upper end carried a steel head surrogate (5.5 kg mass and 0.035 kg m2 moment of inertia) designed to represent a 50th percentile human head. [15] The head surrogate was rigidly attached to the occiput mount with the center of gravity located analogous to that of a real head. The head weight was suspended from its center of gravity and balanced by a pneumatic suspension system, but the inertial components of the head remained effective. The suspension of the head was such that the head was completely free to move within its three degrees of freedom in the sagittal plane. Three potentiometers were attached between the head surrogate and the sled frame. A head stop was empirically set at a 45° angle so that the natural extension of the head lead to a perpendicular contact of the head and head stop. To record the intervertebral motions during the trauma, each vertebra was fitted with a motion monitoring flag completely visible from a lateral view to be recorded with a high speed movie camera (NAC Inc., Tokyo, Japan). Specially designed spinal ligament transducers were attached across capsular ligaments from C2–C3 to CO–C7 alternating the two sides. [16]
These transducers were affixed to two K-wires drilled into the bone at the approximated points of ligament origin and insertion. The resolution of the transducers was 5 µm with average accuracy of 0.025 mm. [17] Elongation of the vertebral artery was measured with a transducer of a similar principle. For that purpose, a thin nylon-coated flexible cable was inserted into the right vertebral artery. The cable was ixed at one end to the occipital bone and at the other end to a displacement transducer. [18]
Once a specimen was mounted on the sled, the springs were compressed with the piston to the extent needed to impart a desired sled acceleration. At time zero magnets were released, the sled was struck from the rear, accelerated forward, reached its maximum velocity, decelerated as it hit breaks, and finally came to rest. The whiplash trauma was filmed at 500 frames per second. Images of the movie flags were later digitized and the data converted to intervertebral rotations. [19] The head motion was quantified by recording the three potentiometer signals via an analog to a digital converter and a personal computer. [20] Each specimen was sequentially traumatized at 2.5, 4.5, 6.5, 8.5 and 10.5 g sled acceleration.
Functional radiographs
Lateral radiographs of the specimen were taken in neutral posture, and when flexed and extended respectively by a 5 N anterior or posterior shear force applied to the occiput. The radiographs were analyzed, qualitatively and quantitatively, to document injuries after each trauma.
Flexibility test

Figure 3
page 4The mechanical properties of the intact and traumatized cervical spines were determined with a flexibility test that characterized the flexion/extension mechanical properties of the spine specimen at each level (Figure 3(a)). [21] This was accomplished by applying pure flexion and extension moments in a stepwise fashion to the occiput while monitoring intervertebral motions with sets of infrared-emitting diodes mounted on each vertebra. One newton meter was defined as the physiologic limit of loading that did not result in injury by experiments of repeatability, but at the same time produced motions similar to those seen in viva. [22] Three load-unload cycles were used to account for viscoelastic properties. For each spinal level and direction of loading two flexibility parameters were obtained: range of motion (ROM) and neutral zone (NZ), Fig. 3(b). The former is defined as the maximum physiological rotation from the neutral position, while the latter is the motion around the neutral position which requires little effort to produce. Maximum elongation of the capsular ligaments and vertebral artery were recorded during the flexibility tests. The elongations served as the physiological limits against which the trauma elongations were evaluated.
Imaging modalities
CT-scan and MRI were performed at the end of all experimental testing. Further, to visualize directly the injuries, especially those to the soft tissue, the specimens were shaved while frozen at –70°C and photographed using the cryomicrotomy technique of Rauschning. [23]
Results
What is the spine posture during whiplash?

Figure 4
page 6Analysis of the high speed films revealed a distinctive bi-phasic kinematic response of the cervical spine to whiplash trauma. [19] Digitized intervertebral rotation data from one specimen (#460) during 8.5 g whiplash trauma is shown in Figure 4(a). The 50–75 ms time period illustrates the first kinematics phase, i.e. the S-shaped curvature of the cervical spine with upper levels flexed and the lower ones extended. At the beginning of this time period, i.e. at about 50 ms, the head had translated posteriorly about 6 cm but with practically no head rotation (Fig. 4(b)). [20] The l00–125 ms time period represents the start of a second phase during which the entire cervical spine bends into extension. The head reaches its maximum extension at about 100 ms. The maximum intervertebral extension of the lower levels of the cervical spine occurred during the first phase (S-shaped curvature of the spine), 25 ms before the full neck extension.
Where does the injuly occur?

Figure 5
page 7Functional radiographs, before and after each trauma, provided a qualitative picture of the injuries. This is exemplified by specimen #460, Figure 5. The left X-ray is the lateral view of the specimen in full extension before the trauma. The middle X-ray shows the specimen under similar loading condition, but after a 2.5 g trauma. Normal alignment of the vertebrae is observed in both these views. The X-ray to the right shows the specimen after 4.5 g trauma. Notice the closeness of the C5 and C6 spinous processes and disruption of the C5–C6 disc. This indicates an anterior injury at this level. No injuries are seen at other levels
A flexibility test is an excellent tool to document incomplete soft tissue injuries. [24] By monitoring the intervertebral motions in response to 1 N m of moment, before and after each trauma, we obtained a quantified and precise evaluation of the injuries to the cervical spine.

Figure 6
page 8Flexibility testing revealed a varied pattern of injury at different spinal levels. To visualize complete set of changes in the ROM and NZ due both to different traumas and spinal levels, average percentage increases from the intact values were computed. [25] The analysis demonstrated significant increases (p < 0.05) in the extension ROM at the C5–C6 level after 4.5 g, and higher traumas (Figure 6(a)). The analysis also demonstrated a significant increase in extension NZ at the C5–C6 level after 4.5 g and greater traumas. Extension NZ also tended to increase (p ~0.1) at CO–Cl and C6–C7 after 6.5 g trauma (Fig. 6(b)).
What kind of injury is this?
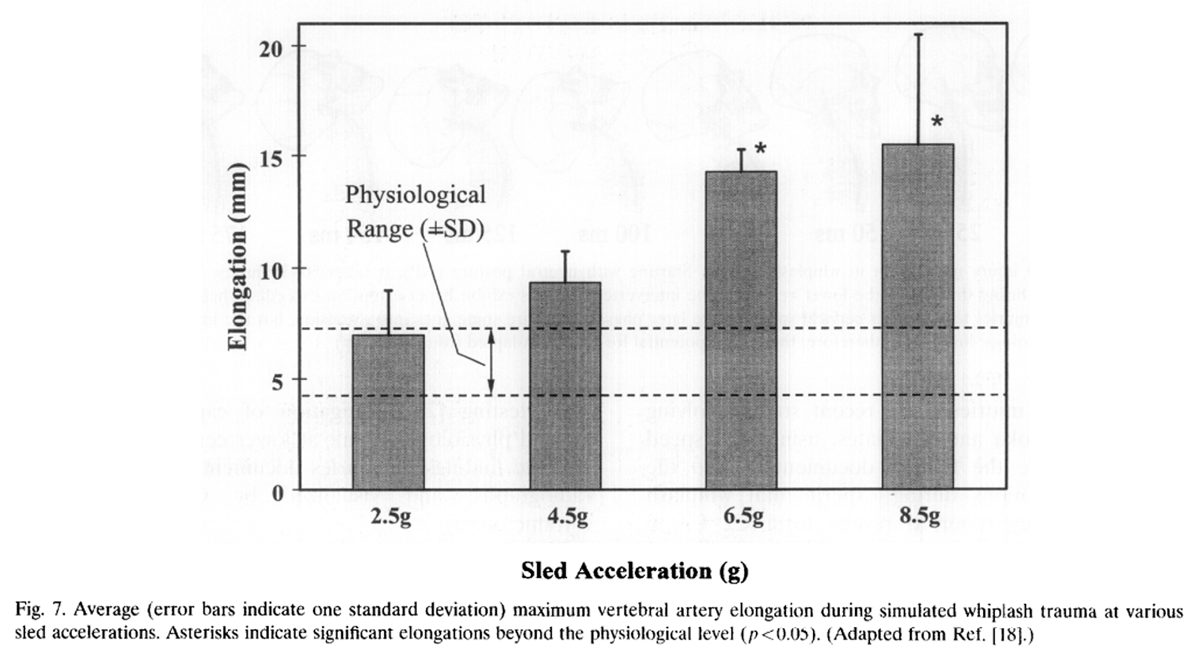
Figure 7 Vertebral artery lesions initiated by its stretch, have been suggested to explain some of the complicated symptoms related to whiplash trauma. [10] The maximum VA elongation measured during the whiplash simulation was significantly correlated with the horizontal acceleration of the sled (R2 =0.7, p ~0.05). The VA elongation exceeded the physiological limit on average (SD) by: l.0(2.1), 3.1(2.6), 8.9(1.6) and 9.0(5.9) mm respectively in the 2.5, 4.5, 6.5, and 8.5 g trauma classes respectively (Figure 7). Furthermore, the maximum dynamic elongations occurred during the initial, S-shape phase of whiplash.

Figure 8
page 9Similarly, the capsular ligaments elongated most in the initial phase of trauma and reached their peak values between 50 and 150 ms after the impact. The largest percentage elongations above the physiological limit were 23.6% and 14.8%, seen at C6–C7 during the 6.5 g and 8.5 g sled acceleration trials.
CT, MRI, and cryomicrotome images provided further evidence for injuries located at the lower cervical levels. The anterior disc injury, seen in Specimen #460 at C5–C6 in all three images, is consistent with the other findings from the flexibility testing, and dynamic ligament elongations (Figure 8). Functional radiographic studies (Fig. 5) not only confirm the anterior disc injury at C5–C6, but also show the nearing of the spinous processes. Thus, there may also be an injury of the facet joims.
Discussion
The mechanism of whiplash has remained unclear over the past seventy years since the term was first coined in 1928 by Crowe. [26] Our laboratory has approached the question of what mechanism produces such trauma by a comprehensive method. We developed a bench-top whiplash model, using fresh cadaveric human spine, that allowed us to observe the trauma directly. We studied the intervertebral rotations of the cervical spine during the trauma with high speed cinematography. Whiplash injuries are partial soft tissue injuries. These are dif~cult to visualize, let alone quantify. For this purpose, we studied the changes in mechanical properties of the cervical spine at each intervertebral level, before and after the trauma, using well-proven and accurate flexibility testing. Several ligaments and vertebral artery dynamic elongations were monitored directly during the trauma. Functional radiographs, CT-scans, MRI, and cryomicrotomy collectively helped visualize the injuries to the soft tissues.
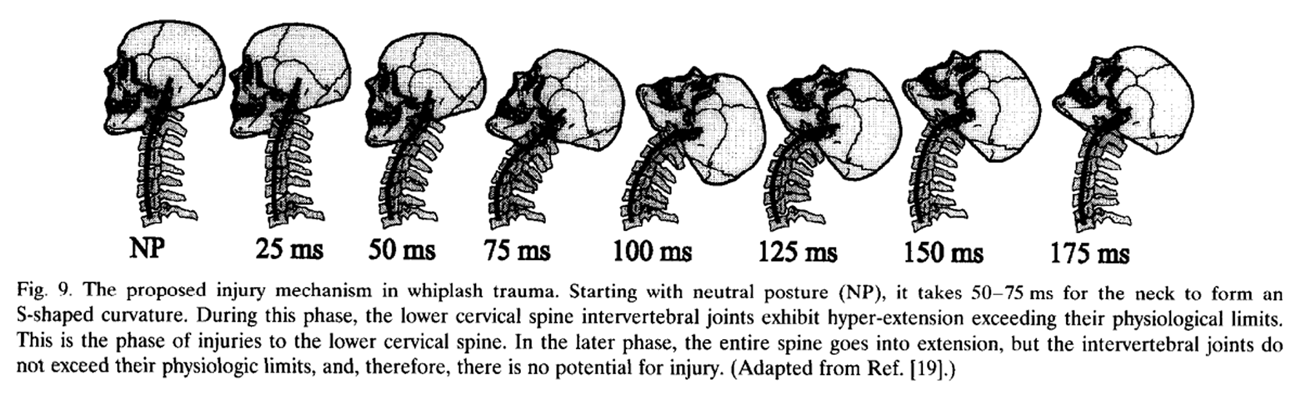
The prevailing view of whiplash injury mechanism, i.e. hyper-extension of the neck as a result of rear-end car impact, was not supported by our experimental findings. Instead, we found a more complex injury mechanism. The main features of the injury mechanism were the foIlowing.For the first 50 ms, the head translated posteriorly, with practically no head rotation. In the first phase between 50 and 75 ms, the spine formed an S-shaped curve resulting in local extension of the lower cervical spine concurrent with upper cervical spine flexion. Maximum extension at the lower levels was seen at 75 ms. Maximum head extension occurred at 100 ms in the second phase.
The intervertebral extensions in the lower levels of the cervical spine in the first phase exceeded their corresponding physiological ranges, but this did not happen in the second phase. This potential for injury was verified by the multidirectional flexibility tests that indeed found the lower levels to exhibit increased both extension neutral zones and extension ranges of motion at 4.5 g or higher whiplash trauma. Furthermore, capsular ligaments and vertebral artery elongated maximally in the initial phase of whiplash. Finally, the injuries that occurred were clearly visualized by the imaging techniques of functional radiographs, CT-scan, MRI and cryomicrotomy.
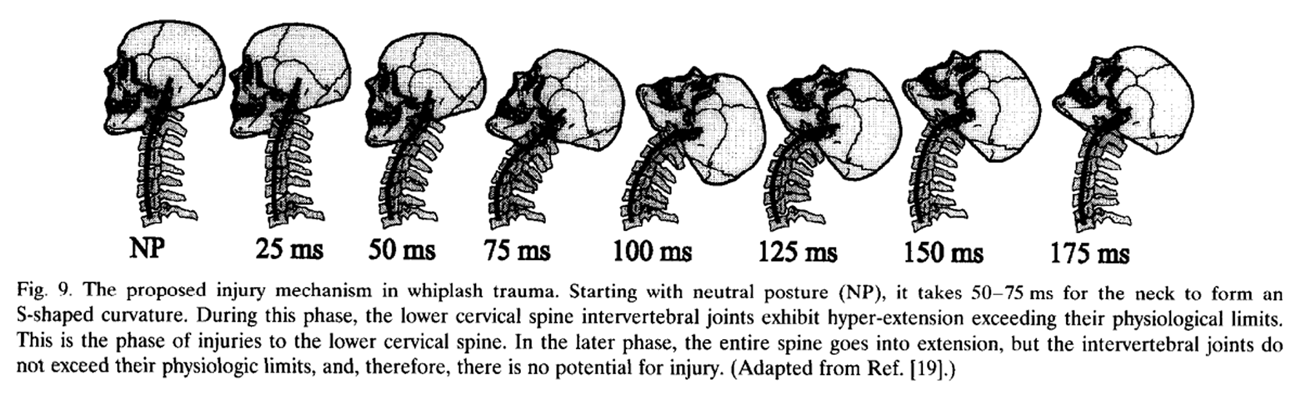
Figure 9 We conclude that the mechanism of whiplash injury is the formation of the S-shaped curvature of the cervical spine in the early phase of trauma, which primarily produces hyper-extension at lower levels and flexion at the upper levels (Figure 9). This implies the stretching of the anterior and compression of the posterior elements of the lower cervical spine beyond their normal physiological limits, resulting in incomplete or subfailure soft tissue injuries consistent with AIS1 type.
The head rest in cars was designed to prevent rearend collision injuries, but the decrease in whiplash injuries after the introduction of the head rest is relatively small, about 20%. [13] The basic injury mechanism hypothesis on which the concept of the head rest is based was first proposed by Macnab more than thirty years ago. [8] Macnab hypothesized that the anterior injuries of the lower cervical spine he saw in animal experiments were due to hyper-extension of the neck. The head rest was designed to prevent the neck hyper-extension by blocking the head motion. Our findings suggest that the lower cervical spine injuries occur before the neck is hyper-extended. In other words, the head rest is ineffective in preventing the formation of the S-shaped curvature of the cervical spine in the first phase of trauma where we saw the neck injuries to occur. If our findings could be projected onto real life whiplash trauma, then we could explain, to a certain extent, the lack of success in significantly reducing the whiplash injuries by the introduction of the head rest.
The S-shaped cervical spine curvature in the first phase of trauma was also noted by Svensson in a dummy preparation, but he did not relate it to spinal column injury. [27] Geigl and associates also measured, in whiplash trauma of a whole cadaver, rotations with in the cervical spine. They found CO–C4 flexion with simultaneous C4–C7 extension, i.e. S-shaped curve, which peaked at 120 ms, while the head rotation peaked much later at 160 ms. [28] However, they did not relate this phenomenon to injury mechanism as they did not have the means to document the incomplete soft tissue injuries. In a recent study involving volunteers, Kaneoka and associates, using high speed radiography, were the first to document in vivo the intervertebral motions during experimental whiplash trauma. [29] They reported results from C2–C3 to C5–C6 levels. They found all the intervertebral motions to be first flexions, which converted into extensions starting at the lowest level, as the trauma progressed. At about 110 ms, they observed an S-shaped spinal curvature, similar to our results.
The S-shaped curvature was also an assumption on which Penning’s theory of injury mechanism is based. [11, 12] However, Penning hypothesized that the crania-vertebral junction is the principle site of cervical injuries in whiplash. In contrast, our experimental findings show that the lower cervical levels more consistently exceed their physiologic motion limits while the upper cervical levels did not. It is of further note that our simulated whiplash did not produce head extension beyond the physiologic limits. This is supported by in vivo findings of two recent studies in which whiplash experiments were conducted with volunteers. [30, 31] This means that injury could not be caused by simple bending of the neck in extension during whiplash. This directly contradicts one of the most popular and prevailing concepts first put forth by Macnab. [8, 9]
The basic assumption underlying our whiplash model, and the interpretation of our findings, is that the intervertebral motion at any spinal level beyond the physiologic limit has the potential to cause soft tissue injury at that level. Furthermore, we define the physiologic limit as the rotation that is reproducible under the application, in this case, of 1 N m pure moment. These assumptions are not arbitrary, but have been established by prior experiments and by the studies presented here. There was internal consistency between three independent measures of injury in the three studies: i.e. abnormal intervertebral extensions in the lower cervical spine observed during the trauma by high speed movie [19]; increased ROM and NZ at the same levels after the trauma as determined by flexibility testing [25]; elongation of capsular ligaments beyond physiological limit at lower cervical levels [16]; and the findings of injuries documented by functional radiographs, and visualized by CT, MRI and cryomicrotomy.
There are some limitations to our studies. Being an in vitro study, there are no muscles which may serve several roles in accident victims. Firstly, muscles stabilize the neck and thus help carry the weight of the head. This function was simulated in our model by suspending the head from its center of gravity with a well-developed suspension system which negated the gravitational force without compromising the inertial effects of the head mass. Secondly, muscles can act, given a warning, in response to trauma, to produce forces to limit the head and neck motions. However, the time for an un-warned victim to develop sufficient muscle force to brace the spine is approximately 200 ms. [28, 32] This is more than twice as long as the time to peak trauma event, i.e. the formation of the S-shaped curvature, as we observed in our experiments. Thus, in an un-warned victim, there is little chance that the muscles can effectively prevent or minimize neck injury. Another limitation of our isolated cervical spine model is that the Tl vertebra is rigidly fixed to the sled. The volunteer studies have measured upward movements of the lower cervical vertebrae [29] and the shoulders. [31] This constraint in our model may be relieved to a certain extent by allowing the Tl vertebra some freedom of motion. But how much freedom to allow, is presently unknown. We hypothesize that the in vivo motions of Tl vertebra are functions not only of the spine characteristics and the trauma acceleration, but also of the seat design, especially the front-back seat stiffness.
The understanding of the whiplash injury mechanism which has resulted from our studies will, we hope, help in the interpretation of ongoing biomechanical and clinical studies. As the understanding of whiplash continues to improve, the associated injury prevention, clinical diagnosis and treatments will be made more effective.
Acknowledgements
This study was funded in part by the National Institute of Health Grant AR42211 and NSERC-Canada.
References:
K Ono, M Kanno
Influences of the physical parameters on the risk to neck injuries
in low impact speed rear-end collisions
International Conference on the Biomechanics of Impacts,
IRCOBI, Eindhoven (8–10 Sept. 1993)LTB van Kampen
Availability and proper adjustment of head restraints in The Netherlands
International Conference on the Biomechanics of Impacts,
IRCOBI, Eindhoven (8–10 Sept. 1993), pp. 367-378C Compton
The use of public crash data in biomechanics research
A Nahum, J Melvin (Eds.), Accident injury biomechanics and prevention,
Springer, New York (1993), pp. 49-66JI Balla
The last whiplash syndrome
Aust N Z J Surg, 50 (1980), p. 610MM Braaf, S Rosner
Trauma of the cervical spine as cause of chronic headache
J Trauma, 15 (1975), p. 441J Dvorak, L Valach, ST Schmid
Cervical spine injuries in Switzerland
J Manual Med, 16 (1989), pp. 7-16Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73I Macnab
Acceleration injuries of the cervical spine
J Bone Joint Surg, 46A (1964), pp. 1797-1799I Macnab
Whiplash injuries of the neck
Manitoba Med Rev, March (1966), pp. 172-174I Macnab
Acceleration extension injuries of the cervical spine
RH Rothman, FA Simeone (Eds.), The spine,
WB Saunders, Philadelphia, PA (1982), pp. 647-660L Penning
Acceleration injury of the cervical spine by hypertranslation of the head:
Part 1. Effect of normal translation of the head on the cervical spine motion:
a radiological study
Eur Spine J, 1 (1992), pp. 7-12L Penning
Acceleration injury of the cervical spine by hypertranslation of the head:
Part 2. Effect of hypertranslation of the head on the cervical spine motion:
discussion of literature data
Eur Spine J, 1 (1992), pp. 13-19A Nygren, H Gustafsson, C Tingvall
Effects of different types of headrests in rear-end collisions
10th International Conference on Experimental Safety Vehicles,
NHTSA, USA (1985), pp. 85-90MM Panjabi, J Cholewicki, L Babat, K Nibu, J Dvorak
Simulation of whiplash trauma using whole cervical spine specimens
Spine, 23 (1998), pp. 17-24HJ Mertz, LM Patrick
Strength and response of the human neck
Proceedings of the 15th Stapp Car Crash Conference (3rd edn), Paper # 710855,
Society of Automotive Engineers, Warrendale, PA (1971)Panjabi MM, Cholewicki J, Nibu K, et al.
Capsular ligament stretches during in vitro whiplash
simulations. J Spinal Disorders, in press.J Cholewicki, MM Panjabi, K Nibu, ME Macias
Spinal ligament transducer based on a Hall effect sensor (a technical note)
J Biomechanics, 30 (1997), pp. 291-293K Nibu, J Cholewicki, MM Panjabi, et al.
Dynamic elongation of the vertebral artery during an in vitro whiplash simulation
Eur Spine J, 6 (1997), pp. 286-289JN Grauer, MM Panjabi, J Cholewicki, K Nibu, J Dvorak
Whiplash produces S-shaped curvature of the neck
with hyperextension at lower levels
Spine, 22 (1997), pp. 2489-2494Cholewicki J, Panjabi MM, Nibu K, Grauer JN, Dvorak J.
Head kinematics during in vitro whiplash simulation.
Accident Anal. Prevention, in press.MM Panjabi, K Abumi, J Duranceau, JJ Crisco
Biomechanical evaluation of spinal fixation devices: II.
Stability provided by eight internal fixation devices
Spine, 13 (1988), pp. 1135-1140J Dvorak, MM Panjabi, JE Novotny, JA Antinnes
In Vivo Flexion/Extension of the Normal Cervical Spine
J Orthop Res, 9 (1991), pp. 828-834W Rauschning
Computed tomography and cryomicrotomy of lumbar spine specimens:
a new technique for multiplanar anatomic correlation
Spine, 8 (1983), pp. 170-180TR Oxland, MM Panjabi
The onset and progression of spinal injury.
A demonstration of neutral zone sensitivity
J Biomechanics, 25 (10) (1992), pp. 1165-1172Panjabi MM, Nibu K, Cholewicki J.
Whiplash injuries and potential for mechanical instability.
A biomechanical investigation.
Eur Spine J, submitted.Crowe HE.
Injuries of the cervical spine.
Paper presented at the meeting of Western Orthopaedic Association.
San Francisco, CA.MY Svensson, Y Haland, S Larsson
Rear-end collisions — a study of the influence of backrest properties
on head-neck motion using a new dummy neck
Proceedings of the 37th Stapp Car Crash Conference (3rd edn),
Paper # 930343, Society of Automotive Engineers,
Warrendale, PA (1993)BC Geigl, H Steffen, P Leinzinger, M Roll Muhlbauer, G Bauer
The movement of head and cervical spine during rear-end impact
IRCOBL, Lyon (1994), pp. 127-137K Kaneoka, K Ono, K Hayashi
Motion analysis of cervical vertebrae in low-impact, rear-end collisions
Poster, AAOS 64th Annual Meeting,
San Francisco, CA (13–17, February 1997)T Matsushita, TB Sato, K Hirabayashi, S Fujimura, T Asazuma, T Takatori
X-ray study of the human neck motion due to head inertia loading
Proceedings of the 38th Stapp Car Crash Conference (3rd edn),
Paper #942208, Society of Automotive Engineers,
Warrendale, PA (1994)WE McConnell, RP Howard, HM Guzman, et al.
Analysis of human test subject responses to low velocity rear end impacts
Proceedings of the 37th Stapp Car Crash Conference (3rd edn),
Paper #930889, Society of Automotive Engineers,
Warrendale, PA (1993)SA Tennyson, NK Mital, AI King
Electromyographic signals of the spinal musculature during +Gz impact acceleration
Orthop Clin North Am, 8 (1977), pp. 97-119
Return to WHIPLASH
Since 9-13-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |