

Use of Complementary Health Approaches at Military
Treatment Facilities, Active Component,
U.S. Armed Forces, 2010-2015This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Medical Surveillance Monthly Report (MSMR) 2016 (Jul); 23 (7): 9–22 ~ FULL TEXT
OPEN ACCESS Valerie F. Williams, MA, MS; Leslie L. Clark, PhD, MS; Mark G. McNellis, PhD
Department of Defense Center for Deployment Health
Research at the Naval Health Research Center,
San Diego, CA, USA.
Survey-based research has demonstrated the increasing use and acceptance of complementary and alternative medicine (CAM) in general and military populations. This report summarizes the use of three CAM procedures (chiropractic/osteopathic manipulation, acupuncture, and biofeedback) among active component service members from 2010 through 2015. Findings document a marked increase in the use of chiropractic/osteopathic manipulation and acupuncture procedures since 2010.
The majority of the 240 military installations in this analysis provided chiropractic/osteopathic manipulation; more than three-quarters provided acupuncture; and approximately one-third provided biofeedback procedures. "Other and unspecified disorders of the back" was the most frequent condition for which chiropractic/osteopathic manipulation and acupuncture were used. "Non-allopathic lesions not elsewhere classified" was the second most frequent diagnosis during chiropractic/osteopathic manipulation-related visits. The second and third most frequent diagnoses during acupuncture-related visits were "acute and chronic pain" and "adjustment reaction," respectively. "Adjustment reaction" was the second most frequent diagnosis associated with biofeedback. Continued research is needed to gain a better understanding of why military personnel are using CAM and the role these procedures play in their health care.
From the FULL TEXT Article:
Background
C0mplementary health approaches, also known as complementary and alternative medicine (CAM), are terms used to describe a diverse group of practices and products with a history of use or origins outside of conventional Western medicine. [1] The use of CAM procedures has been increasing among the general adult population. In 2002, 2007, and 2012, estimates of the percentage of U.S. adults aged 18 years and older who used any complementary health approach in the previous 12 months were 32.3%, 35.5%, and 33.2%, respectively. [1, 2] Trends in the U.S. military mirror those reported in the general population. A survey-based study of U.S. Navy and Marine Corps personnel using data from December 2000 through July 2002 reported that more than one-third (37.2%) of the respondents had used at least one CAM procedure in the preceding year. [3] The 2005 Department of Defense (DoD) Survey of Health Related Behaviors Among Active Duty Military Personnel yielded a prevalence estimate of 44.5% for any CAM (without prayer) use. [3, 4]
In September 2008, the MSMR summarized the number and nature of CAM procedures during ambulatory visits of U.S. military members in 2006 and 2007. [5] Since that time, survey-based research has further demonstrated the increasing use and acceptance of these approaches in the general and military populations. [6–8] For example, results of a 2012 survey of military personnel and family members presenting to an Emergency Department in a tertiary military treatment facility (MTF) indicate that 45% of respondents described previous or current CAM use. [9] Furthermore, in the past decade, the DoD has funded additional research into the use of CAM approaches such as acupuncture and chiropractic manipulation in the treatment of an array of conditions common to the military population, including post-traumatic stress disorder, traumatic brain injury, and chronic pain syndromes in a wide range of settings including while deployed. [10–13] Despite this increased research focus, few studies have used medical administrative data to assess the use of complementary health approaches in the U.S. military.
This report describes trends in the use of three complementary health approaches by active service members during healthcare encounters over a 6–year surveillance period, from 2010 through 2015. The modalities of interest include chiropractic/osteopathic manipulation, acupuncture, and biofeedback. These modalities were selected because they are three of the most commonly used approaches in both the U.S. general and military populations and are documented with a discrete set of standardized procedure (CPT) codes. In addition, this report characterizes patterns of use with regards to treatment location (military installation), key demographic characteristics (age, gender, race/ethnicity, education level, service, military status, and occupation) of CAM recipients, and treated conditions.
Methods

Table 1 The surveillance period was 1 January 2010 through 31 December 2015. The surveillance population included all individuals who served in the active component of the U.S. Army, Navy, Air Force, or Marine Corps anytime during the surveillance period. Records of all healthcare encounters (hospitalizations and ambulatory visits) maintained in the Defense Medical Surveillance System (DMSS) that included CPT codes that documented CAM procedures of interest (acupuncture, chiropractic/osteopathic manipulation, and biofeedback) were identified (Table 1). The analysis was restricted to direct care encounters at U.S. military medical facilities; as such, it did not include encounters at civilian facilities (e.g., purchased/outsourced care).
For all healthcare encounters of interest, relevant CPT codes in all procedure positions of the electronic records of the encounters (i.e., outpatient CPT 1–4; in-patient PCS 1–20) were identified. To ascertain CAM use during combat-related deployments, records of medical encounters maintained in the Theater Medical Data Store (TMDS) were searched; no CAM procedures of interest were documented in the TMDS during the surveillance period.
The illnesses and injuries that were treated with CAM procedures were characterized using three-digit groupings for ICD-9 and four-character groupings for ICD-10. CAM use was summarized as the proportion of active component members who had at least one healthcare encounter that included a CAM procedure of interest and as the number of CAM procedure-related visits per 100 service members per year.
Results
NOTE: For Tables 2–6, please refer to the Full Text article During the 6–year surveillance period, 14.9% (n = 358,394) of active component service members had at least one healthcare encounter that included a CAM procedure of interest (chiropractic/osteopathic manipulation, acupuncture, or biofeedback) (data not shown). Among all active component members during this period, slightly more than one-eighth (12.8%; n = 307,897) had at least one ambulatory visit that included a chiropractic/osteopathic manipulation procedure; approximately 2% (n = 46,950) had at least one visit that included acupuncture; and nearly 1% (0.9%; n = 22,209) had a visit that included biofeedback (Table 2). Very few (0.04%) of all healthcare encounters that included acupuncture procedures were associated with inpatient care (data not shown).
In general, members of the Air Force and Army, women, senior enlisted members and officers, service members aged 30 years or older, those with an education level of some college or more, and those in healthcare and pilot/air crew occupations were more likely than their respective counterparts to have had outpatient visits with chiropractic/osteopathic manipulations (Table 2). Overall, active members of the Army, women, senior enlisted members and senior officers, those aged 30 years or older, and those in healthcare occupations were more likely than their respective counterparts to have had acupuncture procedure-related visits (Table 2). The most pronounced differences in the proportions of service members with outpatient visits that included biofeedback procedures were by service; active members of the Army were approximately 10.5, 5.9, and 3.7 times more likely to have biofeedback procedures during medical encounters than Navy, Air Force, and Marine Corps members, respectively (Table 2).
Chiropractic/osteopathic manipulation (n = 1,768,621 visits) accounted for 88.0% of all encounters for which CAM procedure codes were listed; such encounters were 10 and 26 times more frequent than encounters coded for acupuncture (8.7%; n = 175,679) and biofeedback (3.3%; n = 66,149) visits, respectively (data not shown). Numbers of CAM procedure-related visits per 100 service members per year (per 100/yr) for chiropractic/osteopathic manipulation procedures more than doubled from 2010 (10.3 per 100/yr) to 2015 (24.5 per 100/yr) (Table 3). Annual utilization rates of such visits were consistently nearly twice as high among females than males, and they generally increased with age and with formal educational attainment (Table 3). Also, rates were consistently higher among service members who were white, non-Hispanic; in the Air Force or Army; senior enlisted or officers; and in healthcare and pilot/air crew occupations, compared to their respective counterparts (Table 3).
Annual rates of visits that included acupuncture procedures were more than four times higher in 2015 (2.8 per 100/yr) than in 2010 (0.7 per 100/yr) (Table 4). In general, rates of acupuncture-related encounters increased with age, military grade, and formal educational attainment. Also, rates were generally higher among Army members, women, and those in healthcare occupations compared to their respective counterparts.
Annual rates of encounters that included biofeedback procedures more than doubled from 2010 (0.3 per 100/yr) to 2015 (0.8 per 100/yr). In general, annual rates increased each year through 2014 but then decreased by approximately one-fourth in 2015. In contrast to the experiences with other CAM procedures, rates of biofeedback-related visits generally decreased in 2015—overall and in every demographic and military subgroup except Air Force members and the oldest (≥55 years) (Table 5).
During the surveillance period, most active component members (85.9%) who had at least one CAM-related visit received at least one chiropractic/osteopathic manipulation procedure. Of service members with any CAM-related visits, 13.1% had at least one acupuncture-focused visit and 6.2% had at least one biofeedback-associated visit. Approximately two-thirds (66.1%) of all service members with any CAM procedure-related visits had two or more such visits. Among service members with two or more CAM visits, 10.9% were treated with both chiropractic/osteopathic manipulation and acupuncture and 4.2% with both chiropractic/osteopathic manipulation and biofeedback. Only 1.2% of service members with multiple CAM visits were treated with all three of the modalities assessed for this report (data not shown). A total of 240 installations had at least one CAM-related visit of any of the three types. The vast majority (97.5%) of these installations provided at least one chiropractic/osteopathic manipulation procedure during the period. More than three-quarters (78.8%) of the installations provided acupuncture procedures and a little more than one-third (35.8%) provided biofeedback procedures (data not shown).
The top 20 installations with the most encounters that included chiropractic/osteopathic manipulations accounted for nearly half (45.9%) of all such encounters. The 20 installations with the most acupuncture-related encounters accounted for more than three-quarters (76.7%) of all such encounters; and the 20 installations with the most biofeedback procedure-related encounters accounted for 88.5% of all such encounters (Table 6).
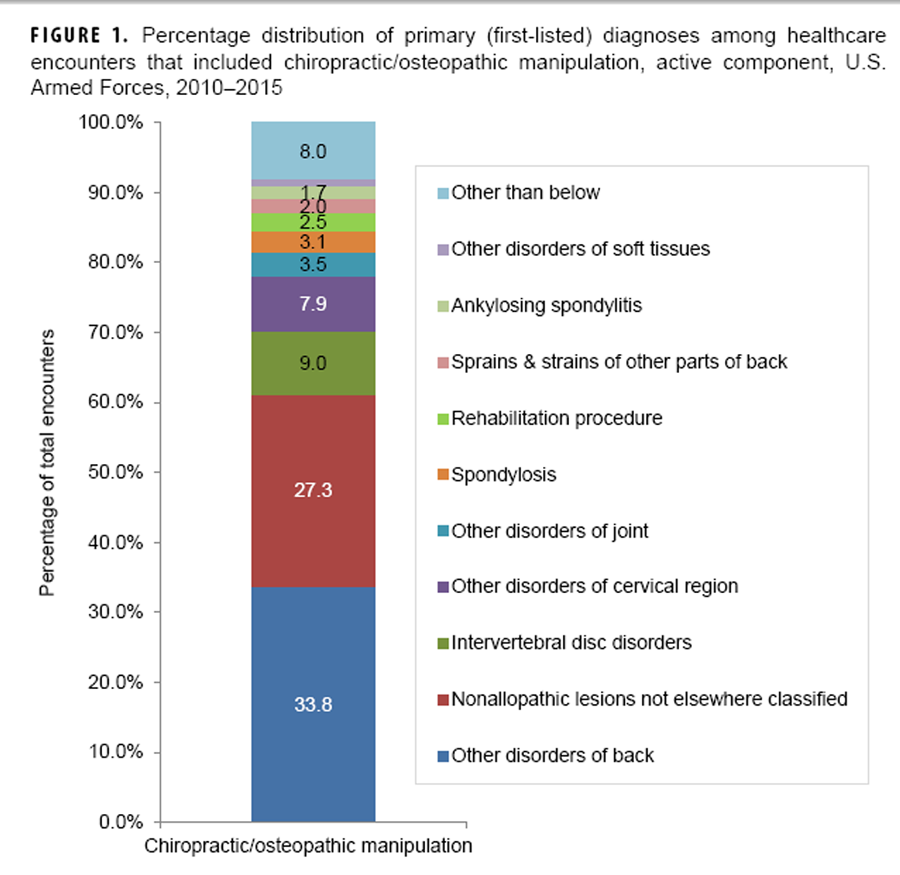
Figure 1
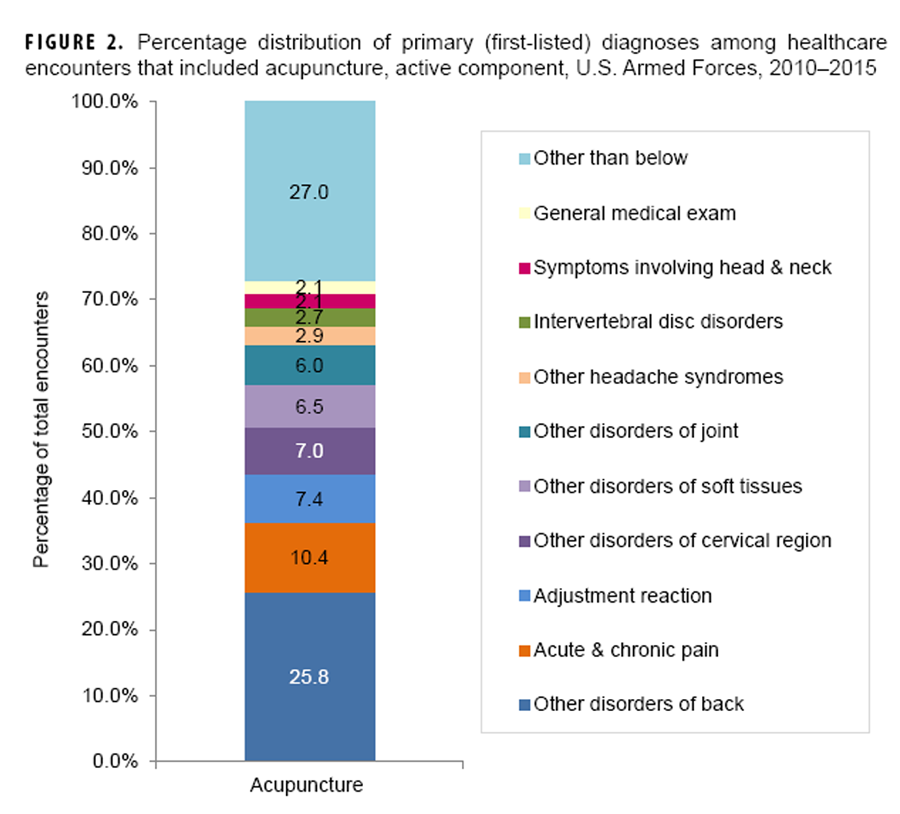
Figure 2
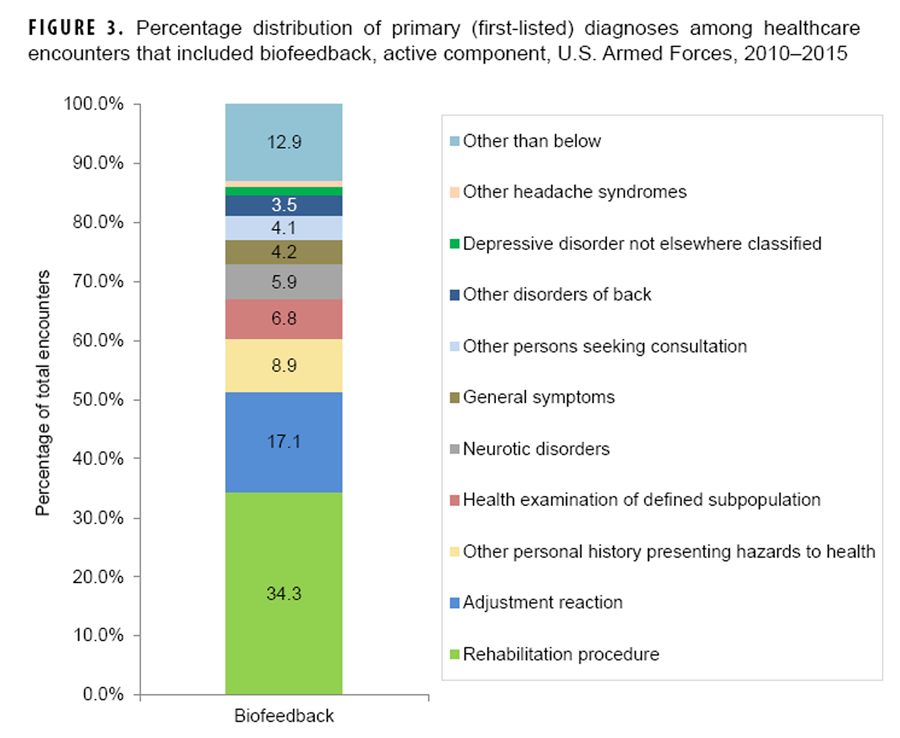
Figure 3 Army installations accounted for majorities of the 20 installations with the most visits for each CAM modality (14 chiropractic/osteopathic manipulation; 11 acupuncture [includes one multi-service]; 16 biofeedback [includes one multi-service]) (Table 6). Nine installations were among the top 20 installations in regard to visits for all three CAM modalities; and Fort Hood, TX, and Camp Pendleton, CA, were among the top 10 installations in regard to visits for all three modalities. Fort Hood and Camp Pendleton accounted for 3.8% and 3.1% of all CAM visits, respectively, while Joint Base Lewis-McChord, WA, and Joint Base San Antonio, TX, each accounted for 3.6% of all CAM encounters (Table 6).
During the period overall, more than half (56.2%) of all CAM-related visits had primary (first-listed) diagnoses of “other and unspecified disorders of the back” (32.1%) or “nonallopathic lesions [of the musculoskeletal system] not elsewhere classified” (24.1%) (data not shown). The former diagnosis was the most frequent during visits that included chiropractic/osteopathic manipulation (33.8%) or acupuncture procedures (25.8%) and the eighth (3.5%) most frequent during biofeedback-related visits (Figures 1–3). The majority of these back disorders had specific diagnostic codes for lumbago (data not shown).
The diagnosis of “non-allopathic lesions not elsewhere classified” was the second most frequent during chiropractic/osteopathic manipulation-related visits (27.3%) and the 16th most frequent during visits that included acupuncture procedures (1.2%) (Figure 1 data not shown). Most of these diagnoses had specific codes for “somatic dysfunction” of either the lumbar or thoracic region (data not shown). The second most frequent (10.4%) primary diagnosis during acupuncture-related visits was “acute and chronic pain” (Figure 2). “Adjustment reaction” was the third most frequent (7.4%) primary diagnosis during acupuncture-related visits and the second most frequent diagnosis during encounters that included biofeedback procedures (17.1%) (Figures 2 and 3).
Editorial Comment
This report provides an overview of CAM procedures used during healthcare encounters among active component service members from 2010 to 2015. Overall, about one of every seven (14.9%) individuals who served in the active component during the surveillance period had at least one healthcare encounter that included one of the CAM procedures of interest for this report.
Chiropractic/osteopathic manipulation procedures represented the majority (88.0%) of visits that included any of the CAM procedures of interest. During the surveillance period, 12.8% of all active component members had at least one ambulatory visit that included a chiropractic/osteopathic manipulation procedure. Survey-based prevalence estimates for use of chiropractic procedures using military samples range from 6.2% to 8.6%. [2, 4, 14] The age-adjusted prevalence estimate for use of chiropractic/osteopathic manipulation among U.S. adults from the 2012 National Health Interview Survey (NHIS) was 8.4%. [1]
In the current study, approximately 2% of all active component members had at least one medical visit that included acupuncture. This estimate falls within the range of survey-based prevalence estimates (1.5% to 2.4%) [2, 4, 14] for use of acupuncture procedures among military samples. The NHIS 2012 survey yielded an age-adjusted prevalence estimate of 1.5% for use of acupuncture. [1]
In this analysis, 0.9% of all active component service members had at least one biofeedback procedure-related visit during the surveillance period. The estimate is slightly higher than those from survey-based studies using military service member samples which range from 0.6% to 0.7%. [2, 4, 14] The age-adjusted prevalence estimate for use of biofeedback procedures from the NHIS 2012 survey was 0.1%. [1]
Many of the demographic characteristics associated with chiropractic/osteopathic manipulation-related visits in this analysis correspond to those previously identified as correlates of higher use of chiropractic procedures among military personnel, including female sex, white non-Hispanic race/ethnicity, older age, and higher formal educational attainment. [4] Other studies of CAM use, among the general and military populations, have not assessed the uses of acupuncture and biofeedback separately in relation to demographic characteristics.
The vast majority (97.5%) of military installations included in this analysis provided chiropractic/osteopathic manipulation procedures; more than three-quarters (78.8%) of the installations provided acupuncture procedures; and, a little more than one-third (35.8%) provided biofeedback procedures. This distribution of CAM modalities is roughly similar to that reported for the 120 MTFs offering CAM programs in 2012. [15]
The most frequent medical condition for which chiropractic/osteopathic manipulation and acupuncture were used was “other and unspecified disorders of the back.” Back disorders are consistently leading causes of medical encounters, lost duty time, and medical disability discharges among U.S. military members. [16, 17] In 2015, this category (which includes diagnoses such as lumbago and unspecified backache) was the primary diagnosis in more than a million medical encounters, affecting 222,787 service members. [16] Conditions of the musculoskeletal system and connective tissue accounted for the vast majority (90.1%) of chiropractic/osteopathic manipulation-associated diagnoses. To clarify the observation about the frequency of diagnoses of “somatic dysfunction,” the following detail is provided. Somatic dysfunction is an osteopathic concept that is defined as “impaired or altered function of related components of the somatic (body framework) system: skeletal, arthrodial, and myofascial structures, and related vascular, lymphatic, and neural elements.” [18] Diagnostic criteria for this condition include asymmetry, restriction of motion, tissue texture abnormality, and tenderness—any of which are required for the diagnosis. [18] The second and third most frequent primary diagnoses during acupuncture-related visits were “acute and chronic pain” and “adjustment reaction,” respectively. Musculoskeletal and connective tissue conditions accounted for approximately half (53.9%) of all primary diagnoses during acupuncture-related visits.
“Adjustment reaction” was the second most frequent diagnosis during encounters that included biofeedback procedures. In 2015, adjustment reaction (which includes post-traumatic stress disorder) was among the 10 most frequently reported illness-specific diagnoses during ambulatory encounters for both men and women.16 Other frequent diagnoses associated with biofeedback-related visits included a mix of rehabilitation procedures, some mental health conditions (e.g., neurotic disorders, depressive disorders not elsewhere classified, specific nonpsychotic mental disorders following organic brain damage), and supplemental classification codes/factors not indicative of a current illness or injury but associated with health status and contact with health services.
There are significant limitations that should be considered when interpreting the results of this analysis. The results presented here are likely to underestimate utilization of the CAM approaches of interest for several reasons. First, because of the reliance on CPT codes, the analysis was restricted to direct care encounters at U.S. military medical facilities. Records of purchased (outsourced) care that entailed the use of CAM procedures were not available for this analysis.
Another limitation of this report’s findings applies specifically to the biofeedback results. Biofeedback procedures can be self-administered or accessed outside of conventional medical treatment facilities. Under those circumstances, such practices are not documented in medical records and thus could not be included in the analysis. Also, there are two biofeedback codes for mental health providers, 90875 and 90876, that refer to sessions that combine biofeedback with a form of talk therapy or counseling. Because these codes were not included, treated mental health conditions are likely underrepresented for this modality.
Another source of underestimation of the use of CAM procedures in this analysis is the inability to quantify CAM use during combat-related deployments despite known usage of at least acupuncture in this setting. [19, 20] Because some care is provided by medical personnel in remote or austere locations, not all medical encounters in theaters of operation are captured in TMDS. In addition, we ascertained CAM usage through CPT codes in medical encounters; although TMDS can capture CPT codes if entered, very few medical encounters had CPT codes entered. It is likely that acupuncture and other CAM procedures are not documented in theater using CPT codes. As a result, our method of ascertainment was insufficient to capture the use of these modalities in theater.
In summary, the findings of this analysis document that chiropractic/osteopathic manipulation, acupuncture, and biofeedback are used frequently among active component U.S. service members. Also, the uses of these CAM approaches have increased generally, and in some situations markedly, since 2010. The topic of CAM use among service members is of increasing importance as consensus grows that these approaches have some utility as adjunct treatments for psychological and other health conditions among the military. [21–27] Repeated deployments and the aging of service members result in increasing prevalences of musculoskeletal problems, traumatic brain injury, and psychological health conditions. [16] Because relatively few studies have focused on the reasons for CAM use, our understanding of why military personnel are using CAM and the role these procedures play in their health care is limited. Research that employs administrative data in conjunction with survey data could address this knowledge gap and also potentially help the Military Health System monitor the need for workforce training and programmatic planning.
References:
National Center for Health Statistics
Trends in the Use of Complementary Health Approaches Among Adults:
United States, 2002-2012
National Health Statistics Report 2015 (Feb 10); (78): 1–16Smith TC, Ryan MA, Smith B, et al.
Complementary and Alternative Medicine Use Among US Navy and Marine Corps Personnel
BMC Complement Altern Med. 2007 (May 16); 7: 16Bray RM, Hourani LL, Rae Olmsted KL, et al.
2005 Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel.
A Component of the Defense Lifestyle Assessment Program (DLAP).
Report prepared for the U.S. Department of Defense, Cooperative Agreement No. DAMD17-00-2-0057.
Research Triangle Park, NC, RTI International, 2006.Goertz C, Marriott BP, Finch MD, et al.
Military Report More Complementary and Alternative Medicine Use Than Civilians
J Altern Complement Med. 2013 (Jun); 19 (6): 509–517Armed Forces Health Surveillance Center.
Uses of complementary and alternative medicine (CAM) procedures, U.S. Armed Forces, active component, 2006–2007.
MSMR. 2008;15(7):6–10.Jacobson IG, White MR, Smith TC, et al.
Self-reported health symptoms and conditions among complementary and alternative medicine users
in a large military cohort.
Ann Epidemiol. 2009;19(9):613–622.Kent JB, Oh RC.
Complementary and Alternative Medicine Use Among Military Family Medicine Patients in Hawaii
Military Medicine 2010 (Jul); 175 (7): 534–538White MR, Jacobson IG, Smith B, et al.
Health care utilization among complementary and alternative medicine users in a large military cohort.
BMC Complement Altern Med. 2011;11:27.Ross EM, Darracq MA.
Complementary and Alternative Medicine practices in military personnel and families presenting
to a military emergency department.
Mil Med. 2015;180(3):350–354.Sniezek DP.
Community-based Wounded Warrior Sustainability Initiative (CBWSI):
an integrative medicine strategy for mitigating the effects of PTSD.
J Rehabil Res Dev 2012;49(3):ix–xix.Williams JW, Gierisch JM, McDuffie J, Strauss JL, Nagi A.
An Overview of Complementary and Alternative Medicine Therapies for Anxiety and Depressive Disorders:
Supplement to Efficacy of Complementary and Alternative Medicine Therapies for
Posttraumatic Stress Disorder [Internet].
Washington, DC: Department of Veterans Affairs; 2011 August.
http://www.ncbi.nlm.nih.gov/pubmed/22238805
Accessed on 1 June 2016.Koffman RL.
Downrange acupuncture.
Med Acupunct. 2011;23(4):215–218.Davis MT, Mulvaney-Day N, Larson MJ, Hoover R, Mauch D.
Complementary and Alternative Medicine Among Veterans and Military Personnel:
A Synthesis of Population Surveys
Medical Care 2014 (Dec); 52 (12 Suppl 5): S83–90Christine M. Goertz, Cynthia R. Long, Robert D. Vining, Katherine A. Pohlman,
Bridget Kane, Lance Corber, Joan Walter, and Ian Coulter
Assessment of Chiropractic Treatment for Active Duty, U.S. Military Personnel
with Low Back Pain: Study Protocol for a Randomized Controlled Trial
Trials. 2016 (Feb 9); 17 (1): 70Integrative Medicine in the Military Health System Report to Congress
Washington, DC: Department of Defense; 2014.
http://health.mil/Reference-Center/Reports?query=integrative+medicine
Accessed on 1 June 2016.Armed Forces Health Surveillance Branch.
Absolute and relative morbidity burdens attributable to various illnesses and injuries, U.S. Armed Forces, 2015.
MSMR. 2016;23(4):2–7.Clark LL, Hu Z.
Low back pain, active component, U.S. Armed Forces, 2010–2014.
MSMR. 2015;22(12):8–11.American Association of Colleges of Osteopathic Medicine.
Glossary of Osteopathic Terminology.
Chevy Chase, MD: American Association of Colleges of Osteopathic Medicine; 2011.
http://www.aacom.org/docs/default-source/insideome/got2011ed.pdf?sfvrsn=2
Accessed on 14 July 2016.Edwards E, Belard JL, Glowa J, Khalsa P, Weber W, Huntley K.
DoD-NCCAM/NIH Workshop on Acupuncture for Treatment of Acute Pain
J Altern Complement Med. 2013 (Mar); 19 (3): 266–279Plunkett A, Turabi A, Wilkinson I.
Battlefield analgesia: a brief review of current trends and concepts in the treatment of pain
in US military casualties from the conflicts in Iraq and Afghanistan.
Pain Manag. 2012;2(3):231–238.Moore M, Brown D, Money N, et al.
Mind-body Skills for Regulating the Autonomic Nervous System;
Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
Arlington, VA; 2011.Chalbi, A, Tuchin, PJ, and Russell, MB.
Manual Therapies for Migraine: A Systematic Review
J Headache Pain. 2011 (Apr); 12 (2): 127–133Schlenger W, Marmar C, Kulka R, et al.
National Vietnam Veterans Longitudinal Study Final Report.
Washington, DC: Department of Veteran Affairs,
Office of Research and Development; 2013.Brantingham JW, Cassa TK, Bonnefin D, et al.
Manipulative and multimodal therapy for upper extremity and temporomandibular disorders:
a systematic review.
J Manipulative Physiol Ther. 2013;36(3):143–201.Chaibi and Russell, 2014
Manual Therapies for Primary Chronic Headaches: A Systematic Review
of Randomized Controlled Trials
J Headache Pain. 2014 (Oct 2); 15: 67Trinh K, Graham N, Irnich D, Cameron ID, Forget M.
Acupuncture for neck disorders.
Cochrane Database Syst Rev. 2016 May 4;(5):CD004870.National Research Council.
Gulf War and Health: Volume 7:
Long-Term Consequences of Traumatic Brain Injury.
Washington, DC: The National Academies Press; 2008.
Return to ALT-MED/CAM ABSTRACTS
Return to CHIROPRACTIC CARE FOR VETERANS
3-23-2020


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |