

Attention Deficit/Hyperactivity Disorder (ADHD) in Children:
Rationale for Its Integrative ManagementThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Alternative Medicine Review 2000 (Oct); 5 (5): 402428 ~ FULL TEXT
OPEN ACCESS Parris M. Kidd, PhD
Attention Deficit/Hyperactivity Disorder (ADHD) is the most common behavioral disorder in children. ADHD is characterized by attention deficit, impulsivity, and sometimes overactivity ("hyperactivity"). The diagnosis is empirical, with no objective confirmation available to date from laboratory measures. ADHD begins in childhood and often persists into adulthood. The exact etiology is unknown; genetics plays a role, but major etiologic contributors also include adverse responses to food additives, intolerances to foods, sensitivities to environmental chemicals, molds, and fungi, and exposures to neurodevelopmental toxins such as heavy metals and organohalide pollutants. Thyroid hypofunction may be a common denominator linking toxic insults with ADHD symptomatologies. Abnormalities in the frontostriatal brain circuitry and possible hypofunctioning of dopaminergic pathways are apparent in ADHD, and are consistent with the benefits obtained in some instances by the use of methylphenidate (Ritalin®) and other potent psychostimulants. Mounting controversy over the widespread use of methylphenidate and possible life-threatening effects from its long-term use make it imperative that alternative modalities be implemented for ADHD management. Nutrient deficiencies are common in ADHD; supplementation with minerals, the B vitamins (added in singly), omega-3 and omega-6 essential fatty acids, flavonoids, and the essential phospholipid phosphatidylserine (PS) can ameliorate ADHD symptoms. When individually managed with supplementation, dietary modification, detoxification, correction of intestinal dysbiosis, and other features of a wholistic/integrative program of management, the ADHD subject can lead a normal and productive life. (Altern Med Rev 2000; 5 (5): 402-428)
Introduction
Attention Deficit/Hyperactivity Disorder (ADHD) is a loosely defined assemblage of neuropsychiatric symptom clusters that emerge in childhood and often persist into adulthood. [1] Though the means to its diagnosis is only empirical, ADHD increasingly is being employed as a diagnostic label for individuals who display a wide range of symptoms, such as restlessness, inability to stay focused, mood swings, temper tantrums, problems completing tasks, disorganization, inability to cope with stress, and impulsivity. [2] The etiology of ADHD is not understood, yet potent drugs are being employed for its medical management while safe and effective alternatives are being neglected. [2, 3] ADHD is the most prevalent behavioral disorder in children, [4] and frequently its symptoms are commingled with learning problems, oppositional conduct, and depression, which altogether compound the family's emotional burden. Particularly since the dominant mode of treatment to date has involved the drug methylphenidate (Ritalin®), which acts on the CNS much like cocaine and has marked potential for severe side-effects and addictive abuse, ADHD has become a lightning rod for controversy. The scientific literature on ADHD is voluminous, with more than 4,000 peer-reviewed articles published since 1966. [5]
An intense debate has developed around the diagnosis, etiology, and medical management of ADHD. Parent groups, consumer advocacy organizations, and progressive physicians are calling for alternatives to methylphenidate and the many other potent stimulants used to treat ADHD, while pharmaceutical interests and physicians particularly oriented to prescribing pharmaceuticals attempt to defend the status quo (currently in the United States, between 1.5 million and 3 million ADHD children are likely taking methylphenidate). This review is intended to bring the medical and scientific issues surrounding ADHD into sharper focus, to better define a wholistic/integrative strategy for its medical management.
Background and Scope of the ADHD Problem
A condition in children somewhat resembling ADHD was first described by Still in 1902. [6] He discussed 43 cases of children with aggression, defiance, emotionality, limited sustained attention, and deficient rule-governed behavior. Although his population possessed normal intellectual capacity, he commented, "...the control of activity in conformity with moral consciousness is markedly defective." He suggested, "inhibitory volition," that is, the capacity to exercise good judgment, might be imperfectly developed in these subjects. From 1940 through 1960, the condition was identified with "minimal brain damage or dysfunction," and its etiology was speculated to be insults to the brain such as head injury, infection, and toxic damage.6 In the 1960s it became "hyperactivity" or "poor impulse control," reflecting that no underlying organic damage had been identified.
By the 1970s1980s, the "hyperactivity" symptomatology had taken on more diagnostic significance in comparison with the other symptoms. In 1980, the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM-III) listed the term "hyperkinetic reaction of childhood," which then evolved through "hyperkinetic syndrome" and "hyperactive child syndrome," to "attention deficit disorder" (ADD), either "with hyperactivity" or "without hyperactivity." By 1987, in the revised DSM-III (DSM-III-R), the earlier focus on hyperactivity had shifted toward inattention and impulsivity. [7]
As the research on ADHD progressed, the balance between the three major diagnostic symptom clusters was subsequently further refined, so that in the 1994 DSM-IV the official term was Attention Deficit/Hyperactivity Disorder, or ADHD, with three subtypes. [1] Inattention and impulse control are now regarded more as the cardinal defects than is hyperactivity. [5] Some professionals continue to reserve the term ADD for children who are only inattentive and ADHD for children who are also hyperactive, but all official reports or other records are required to use ADHD.
ADHD is usually diagnosed in school-age children, and is conservatively estimated to occur in 36 percent of this population from diverse cultures and geographical regions. [5, 812] In some U.S. cities the percentage may reach 1015 percent. [8] As of 1993, more than two million U.S. children were diagnosed ADHD, the number having increased steadily from 902,000 in 1990. Currently, as many as four million carry this diagnosis, which is responsible for 3050 percent of the referrals to mental health services for children. [9, 10] Elsewhere, ADHD estimated prevalence ranges from 1.710.0 percent in Canada, Puerto Rico, the United Kingdom, Norway, the Netherlands, Germany, and New Zealand. [1012] ADHD routinely continues into adolescence, and also can persist into adulthood in as many as half of those individuals who manifest the disorder in adolescence. [10]
The adverse social, familial, and personal consequences of ADHD cannot be overstated. Most ADHD subjects develop emotional, social, and family problems as a consequence of their primary difficulties. ADHD is a major problem both for society and for the child, as it causes friction in school or at the workplace, depresses the academic performance of the student's entire class, interferes with peer relationships, and increases intra-family stress. For the individual afflicted, until ADHD symptomatologies can be recognized and brought under medical management, daily existence is likely to be severely compromised along with the lives of those around him (or her, although ADHD is more prevalent in boys by a 3:1 margin). [5] Parents and children express desperation for interventions that will work, but without the adverse effects inflicted by the pharmaceutical management model.
The first report of stimulant use to treat ADHD was in 1937. [13] The current overwhelming reliance on methylphenidate and other stimulants for ADHD treatment belies the ample evidence that ADHD symptomatologies can be ameliorated without the use of drugs. This degree of reliance on methylphenidate is unfortunate because its action is virtually identical with cocaine, to such an extent that in the United States it is a Schedule II controlled drug. [1416] The frequent practice of maintaining ADHD subjects on methylphenidate over many years increases the potential for its abuse. In fact, it is fast becoming a "street drug" among teenagers. [17] The controversies over methylphenidate use and the ever-increasing frequency of ADHD diagnosis are now so politicized that they are interfering with society's urgent need to better serve the children (and adults) involved. Fortunately, a balanced examination of the available scientific and clinical evidence reveals an improved prognosis for ADHD.
The Diagnosis and Progression of ADHD
No matter how well trained the physician may be in this area, making the diagnosis of ADHD is anything but straightforward. No "hard" clinical tests-physical, laboratory, or neurological-are available with which to unequivocally correlate the symptoms. Rather, the definitive diagnosis must be deduced from a highly detailed clinical history, as synthesized from information provided by parents, teachers, and (last but hopefully not least), the afflicted individual. [18, 19] The conscientious clinician will do an in-depth parent and patient interview along with a physical examination, solicit corroborative information from adults in other settings (especially teachers), and obtain an assessment of academic functioning. Many clinicians use standardized rating scales in order to assess the age- and sex-matched relative symptom severity. [18, 20]
For U.S. practitioners official ADHD diagnostic guidelines are found in the DSM-IV, which is related to the World Health Organization ICD-9 and ICD-10 categories. [1, 21] In North America, ADHD is viewed as a common but heterogeneous developmental disorder linked with diverse co-morbidities. By contrast, in Europe the diagnosis (i.e., of hyperkinetic syndrome) is reserved for ADHD uncomplicated by co-morbid psychopathology. With this relatively narrow definition the condition becomes relatively rare, but the European perspective appears to be gradually shifting toward that of North America. [5]
The symptoms of ADHD are most often first recognized by the child's teacher. ADHD children have difficulty sitting still, maintaining their attention on the task at hand, and thinking through their answers before they respond to questions. Although ADHD is distinctly different from learning disability per se, the behavioral features that define this disorder-short attention span, distractibility, impulsivity, overactivity-occur on a continuum across the population, thus the ADHD diagnosis requires thorough consideration of the severity of the symptoms and the relative degree of functional impairment.
ADHD per DSM-IV is diagnosed in five major steps, each with specific criteria. [1] The symptoms must appear before age seven, persist for at least six months, and appear in the school environment as well as the home. The first step is to establish EITHER (a) abnormal and persistent inattention, from at least six symptoms continuing over a minimum six months, OR (b) abnormal and persistent hyperactivity-impulsivity, also from at least six symptoms over six months. The second step is to establish that these symptoms were present before seven years of age. Third, these symptoms must be present in two settings, usually at school (or work, if an adult) and at home. Fourth, there must be clear evidence of "clinically significant impairment in social, academic, or occupational functioning." The fifth criterion is exclusionary-that the symptoms not be secondary to some other disorder. Whereas some of the ADHD symptomatologies can be linked to family changes (e.g., divorce) or other life events (e.g., head trauma), ADHD typically begins early in life, is chronic, and is pervasive.
Once the basic ADHD diagnosis is established per the above-described criteria, three subtypes can be differentiated.1 These are (1) ADHD, combined type, applied where both inattention and hyperactivity-impulsivity-(a) and (b) above-are extant for at least 6 months; (2) ADHD, predominantly inattentive type, if only the inattention criteria are met; and (3) ADHD, predominantly hyperactive-impulsive type, if only the hyperactivity-impulsivity criteria are met. There is also a DSM-IV criterion of ADHD In Partial Remission, for individuals (usually adolescents or adults) who exhibit only some of the required symptoms but are otherwise experiencing significant functional impairment. Then come the assessments for the learning disabilities and other neurologically based disorders with which ADHD is often associated.
Between 3040 percent of ADHD subjects have learning disabilities, [18, 19] but the ADHD child is not mentally retarded and can be realigned toward a productive life path. To help make this possible the physician and the other professionals involved must work closely with parents and teachers to assess the child as a total individual. They must objectively discern the entire range of difficulties the child is experiencing, and make the degree of commitment necessary to treat the child wholistically with all the resources available. Unfortunately, the current norm for ADHD management is to do a minimal psychological assessment, then prescribe methylphenidate. [2, 3, 19]
Other neurobiological difficulties encountered in the ADHD population are motor tic disorder or Tourette's disorder, anxiety disorder, anger control problems, and depression. [22, 23] Some children will have two, three, or more of these difficulties without having ADHD, but Biederman studied a large population of ADHD children and found that more than half also had depression, anxiety, and conduct disorder. [23] The clinician must therefore verify, document, and prioritize these various symptom clusters, both to assess their relative contributions to the child's apparent ADHD patterns and to develop means for their medical management concurrently with ADHD.
ADHD Medical Management-Current Status
The conventional management of ADHD formally involves a multimodal approach. [18, 19, 2325] Currently, this approach includes individual and family education, counseling, behavioral therapy, school remediation, and medication. [24] Close coordination between the subject, the family, the practitioner and the school system ought to be integral to this approach, but in mainstream pediatric practice medication with pharmaceuticals is practically the sole component of medical management. [25] Typically, it falls on the family of the afflicted child to implement additional modes of management that have proven effectiveness, such as clearing allergies, regulating the diet, and supplementing with nutrients.
Psychostimulant medications are generally the first choice in medication of ADHD. Approximately 70 percent of the children treated show improvement in the primary ADHD symptoms and in co-morbidity such as conduct disorder, [24, 25] although the benefits may not hold beyond two years. Currently, methylphenidate is the drug of choice; other first-line stimulants include dextroamphetamine (Dexedrine®) or a mixture of four salts of dextroamphetamine (Adderall®). [18, 19] The second-line stimulants include methamphetamine (Desoxyn® or the longer-lasting Desoxyn Gradumet®), or pemoline (Cylert®), which causes hepatotoxicity in about three percent of subjects treated and can cause death, so must be closely monitored. In practice, the use of any of these stimulants is so fraught with uncertainties and potential complications that only the most intrepid practitioners prescribe them with comfort. [17, 2425, 2729]
The psychostimulants ought to be severely limited in their applicability, due to their marked and sometimes severe adverse effects. [29] Decreased appetite secondary to anorexia or nausea may occur, leading to weight loss. Insomnia may also occur, as can headache. Lowering the dose and changing the timing may eliminate these side-effects. Rarely, psychostimulants may cause tics to develop, and cases of leukopenia and psychosis have been reported. [25] Methylphenidate (Ritalin), dextroamphetamine (Dexedrine), and Adderall are all classified as Schedule II agents in the U.S., consonant with their significant abuse potential. [25, 29] As blood levels of the stimulant decrease over time, irritability may manifest as a "rebound" type of withdrawal symptom.
Some subjects are very prone to abusing stimulants and must be placed on non-stimulant, alternative medications. A subgroup with more depression and anxiety may respond better to tricyclic antidepressants (imipramine, desipramine) than to stimulants, [24] although both can have major adverse effects, with desipramine linked to sudden death. [25] The antidepressant bupropion (Wellbutrin") can, like the stimulants, exacerbate an underlying tic disorder. This drug is also contraindicated in children with anorexia nervosa, bulimia, or epilepsy. ADHD subjects have a higher risk of moving into drug abuse, [34] and there is now a trend toward placing ADHD children on Prozac®, withdrawal from which has been linked to violence and other possibly disastrous outcomes. [27, 28]
Certain non-stimulant medications can serve as allopathic alternatives in ADHD when stimulants have failed. Among these are the alpha-adrenergics clonidine (Catapres®) and guanfacine (Tenex®). Both are less well validated than the stimulants and not as efficacious. Clonidine can cause sedation and dysphoria, and both of these drugs require blood pressure monitoring because they are also antihypertensives. [24, 25]
The psychological disorders that often coexist with ADHD also require management. The more serious of these include tics or Tourette's syndrome; depression, including the bipolar type which is quite prevalent; anxiety; and obsessive-compulsive disorder. For children who have tic disorders, extreme overactivity, oppositional or conduct disorder, or hyperarousal, clonidine may prove useful. [24] ADHD also can be associated with impulse control problems more extreme than the usual ADHD spectrum; sometimes antipsychotics are prescribed, although their risks outweigh their advantages. [25] In summary, pharmacologic management of ADHD and the coexisting conditions can challenge even the most experienced practitioner, and safer modes of management are urgently indicated for this unfortunate patient population.
Ritalin-Its Benefits and Risks
The continuing status of methylphenidate, or Ritalin, as the single-most common intervention for the symptomatic management of ADHD is the basis for considerable, oftentimes bitter disagreement and controversy. The author considers methylphenidate to be a highly cerebroactive pharmaceutical that offers symptomatic benefit in ADHD but carries high potential for abuse and possible life-threatening effects over the long term. [30]
Ritalin and Ritalin-SR® are preparations of methyl-alpha-phenyl-2-piperidineacetate hydrochloride. Methylphenidate acts on the central nervous system with a dopamine-agonistic effect that is slower in onset but mechanistically almost identical to cocaine and amphetamines. [1416] Advocates of methylphenidate attest that it works more effectively than any other single intervention to enhance attention span and impulse control. [31] Yet methylphenidate does not consistently benefit academic performance. Opponents of the drug (along with some of its advocates) point to its many serious adverse effects, [26] and many critics argue that children should not be put at risk for the known major adverse effects of a drug that is virtually banned for use by adults. Methylphenidate also has potential for abuse, and the abuse pattern is very similar to cocaine and amphetamines. [17]
A majority of ADHD children-up to 70 percent of those treated-do seem to derive a degree of benefit from methylphenidate, [24, 31] but its benefits have been overstated and there are compelling reasons to believe this drug is being overprescribed. Citing credible survey data, Swanson and collaborators [9] documented a dramatic increase in outpatient visits for ADHD in the early 1990s, accompanied by a near-tripling in Ritalin production-in 1993, more than 2.5 million Ritalin prescriptions were written for ADHD. They attributed the markedly increased frequency of ADHD diagnosis to heightened public awareness and to policy changes that have forced public schools to identify students with ADHD. But as so many of the "mainstream" practitioners tend to do, they dismissed the increase in methylphenidate prescribing as merely "required to meet the demand for stimulant medication."
This intensifying confrontation is fueled by the realization that methylphenidate can (and does) exert serious adverse effects. [29, 30] Scarnati [29] listed the most severe effects reported in the professional literature: psychic (hypomania, mania, delusions, paranoid delusions, paranoid psychosis, toxic psychosis); hallucinations, auditory and visual; exacerbation of schizophrenia and autism; muteness, extreme withdrawal, partial dissociation; boundary loss, disorganization; nervousness, agitation, terrifying affect, aggressiveness, assaultiveness, anxiety, panic; drug abuse-rebound depression, psychic dependence, increased euphoria, and cocaine-like activity. The Indiana Prevention Resource Center [30] circulated information on the major street abuse of methylphenidate currently occurring in Indiana and the potential for life-threatening damage.
When methylphenidate is used with antidepressants (such as the tricyclics and Prozac), seizures, hypertension, hypothermia, and convulsions can ensue. [29] Over the long term, weight loss can occur, as can scalp hair loss, vasculitis, leukopenia, visual disturbances, and anemia. A no less recognized authority than the Physicians' Desk Reference [32] carries a long list of potential adverse reactions in children and also has this to say about methylphenidate:
"In children, loss of appetite, abdominal pain, weight loss during prolonged therapy, insomnia and tachycardia, may occur...Periodic CBC, differential, and platelet counts are advised during prolonged therapy...Ritalin should be periodically discontinued to assess the child's condition...Drug treatment should not and need not be indefinite...Patients with an element of agitation may react adversely; discontinue therapy if necessary."-Physicians' Desk Reference, 53rd Edition, 1999, pgs. 20789.
The PDR section on methylphenidate also starkly states, "Sufficient data on safety and efficacy of long-term use of methylphenidate in children are not yet available..."
In 1994, U.S. Government researchers reported that Ritalin caused liver cancer in male mice. [32] The carcinogenic doses were equivalent to just 2.5 times higher than the highest human prescribed dose. The U.S. National Toxicology Program has concluded that methylphenidate is a "possible human carcinogen." This revelation about methylphenidate, taken together with the major adverse effects of the other psychostimulants, makes it imperative that alternative modalities be implemented for the management of ADHD.
ADHD Etiology and Contributory Factors
ADHD is highly inhomogeneous in the biological sense, and although classed as a disorder it amounts to hardly more than an assemblage of symptom clusters. Its etiology also is far from homogeneous, with many likely contributory factors. Certainly some of these etiological factors generate symptomatologies that closely resemble ADHD. Among these are sensitivities to food additives, intolerances to foods, nutrient deficiencies and imbalances, heavy metal intoxication, and toxic pollutant burden. Also, evidence is mounting that abnormal thyroid responsiveness, perhaps engendered perinatally by environmental pollutants, is on the rise and predisposes to ADHD. [35]
ADHD has been linked to inherited susceptibilities; for a critical review refer to Tannock. [5] Findings from twin studies and adoption studies support some degree of heritability for the disorder, [32] though co-morbid conditions complicate the analyses. Numerous familial-genetic studies have documented a higher prevalence of psychopathology, particularly ADHD, in the parents and other relatives of children with ADHD, and there is a statistically and clinically significant risk for ADHD to occur in children where either biological parent had onset in childhood. [3640] Sophisticated studies confirm a higher incidence of ADHD in the closest relative of ADHD males. [5]
The actual degree to which genetic heritability may predispose to childhood onset of ADHD is still an open question. Population studies indicate attentional problems, conduct problems, and emotional problems tend to cluster within families. [41] Genetics and environment are notoriously difficult to separate within the family unit, and Fisher suggested the genetic predisposition to ADHD might fuel a negative family atmosphere that exacerbates latent ADHD in the child. [19]
Twin and adoption studies are generally the most precise means for estimating relative heritability of a trait. Such studies in ADHD suggest a relatively high degree of heritability. [5] They also suggest that rather than being a discrete disorder, ADHD may be viewed as the extreme end of a behavior continuum that varies genetically throughout the population. [42] Both inattention and impulsivity/hyperactivity appear to be heritable and share a genetic component, [39, 43] but no one gene is likely to be the culprit.
Important advances have been made in the pursuit of genes for ADHD. [5] To date, the evidence for single-gene inheritance is unconvincing; rather, a polygenic mode of inheritance is more likely-either several strong genes or many genes with weak effect. Genes within the dopamine transmitter system are the most likely to be most involved, given: (1) the effective reduction of symptoms by dopamine agonists such as methylphenidate; (2) results from brain imaging studies that implicate brain structures with rich dopaminergic innervation, such as the frontostriatal circuitry; [44] and (3) early results from gene isolation studies. [5]
The heritability of the associations between ADHD and its various co-morbid conditions may span the entire spectrum of possibilities. Biederman and his colleagues suggest ADHD and major depressive disorders may have common familial vulnerabilities. [22, 23] ADHD with co-morbid conduct disorder also may be preferentially associated, whereas the anxiety and learning disorders may segregate separately. ADHD relatives of patients with ADHD do have markedly higher risk for major depressive disorder, antisocial disorders, and substance abuse. To date there is insufficient data to quantify any relative degree of co-heritability of ADHD with a trait for any of these co-morbid conditions.
Food Additives and Food Intolerances in ADHD
In the mid-1970s, Feingold broke new ground with his claim that up to 50 percent of all hyperactive children were sensitive to food additives (artificial food colors, flavorings, and preservatives) as well as to salicylates that occur naturally in some foods. [45, 46] Feingold's basic finding of the connection between food additives and ADHD symptomatology was not new. As early as 1922, Shannon had published on the successful treatment of children with hyperactivity and learning disorders using an elimination diet. [47] On this regimen 3050 percent of children improved. Most recently, Schardt reviewed 23 double-blind studies that examined whether food dyes or ordinary foods worsened behavior in children with ADHD or other behavioral problems. [48] In eight of the nine studies conducted with ADHD children, the behavior of some children worsened after consumption of food dyes or improved on an additive-free diet. The symptomatology of these adverse responses mimicked ADHD.
The other 14 studies reviewed by Schardt looked at children with ADHD plus asthma, eczema, or food allergies, irritability or sleep disturbances, or more severe behavioral or neurological disorders. In 10 of the 14 studies, some children improved when they ate diets free of additives or certain foods. Some deteriorated when they ate food dyes or foods like corn, wheat, milk, soy, oranges, eggs, or chocolate. Schardt concluded his critique with suggestions from experts that dietary modification be systematically attempted before the decision is made to place an ADHD child on a pharmaceutical regimen.
Feingold's original case histories covered 1,200 pediatric cases in which food additives were linked to behavioral and learning disorders, and pointed the finger at some 3,000 different additives, yet subsequent research to "verify" his work focused on less than a dozen additives. The majority of the double-blind studies designed to test Feingold's hypothesis reported their outcomes as negative, yet a careful review of the data from these studies by Murray and Pizzorno concluded that a full half of the children placed on the Feingold diet in these studies actually showed a decrease in hyperactivity. [49] A pattern is evident, as discerned by Boris: single-agent elimination studies tended to show limited improvement or no improvement at all, while multi-agent elimination studies were almost universally successful. [50, 51]
Rippere has criticized in depth [52, 53] the methodologies of the "double-blind" studies conducted by Conners and other critics of Feingold. [54, 55] She points out: (a) the conscious design of active, potentially allergenic placebos (such as chocolate cookies); (b) the decisions to use dosages of test additives lower than known to be consumed in foods; (c) the use of highly unreliable laboratory tests for allergy determination; and (d) formulation of imprecise rating scales as outcome measures. Perhaps the most serious criticism by Rippere is that of investigator bias; i.e., the researchers ignored study outcome data that supported the Feingold interpretation while overemphasizing contrary data. Boris, [50, 51] Weiss, [56, 57] Crook, [5861] Egger, [62, 63] and others have conducted their own studies and trials, reviewed the cumulative data, and come out in support of the Feingold hypothesis. It is interesting to note that studies conducted in non-U.S. countries produced results markedly more favorable to the Feingold interpretation, [49] and that most of the U.S. investigations were sponsored by a corporate food lobby group, the Nutrition Foundation.
Food additives are big business, especially in the United States (see Murray and Pizzorno for an overview). [49] There are some 5,000 additives in widespread use, including but not limited to: anticaking agents such as aluminosilicates; synthetic antioxidants such as BHA and BHT; bleaching agents such as hydrogen peroxide; colorants such as artificial azo dye derivatives; preservatives such as benzoates, nitrates, and sulfites; and many others. Per capita daily consumption of food additives in the U.S. is 1315 grams, and the population's total annual consumption of food colors alone is approximately 100 million pounds. Other countries have significantly restricted artificial food additives whereas the United States has never done so.
The removal of artificial food colorings and preservatives from the diet is an indispensable and practicable clinical intervention in ADHD, but rarely is sufficient to eliminate symptomatology. Up to 88 percent of ADHD children react to these substances in sublingual challenge testing, [49] but in blinded studies no child reacted to these alone. Allergies to the foods themselves must also be identified and eliminated. Doris Rapp, MD, a pediatrician with considerable experience in this area, has claimed that two-thirds of children diagnosed ADHD have unrecognized food allergies that generate most, if not all, of their symptoms, These can usually be detected and the symptoms cleared using a simple one-week elimination diet. She has thoroughly documented her findings in books, professional articles, and videotapes. [6466]
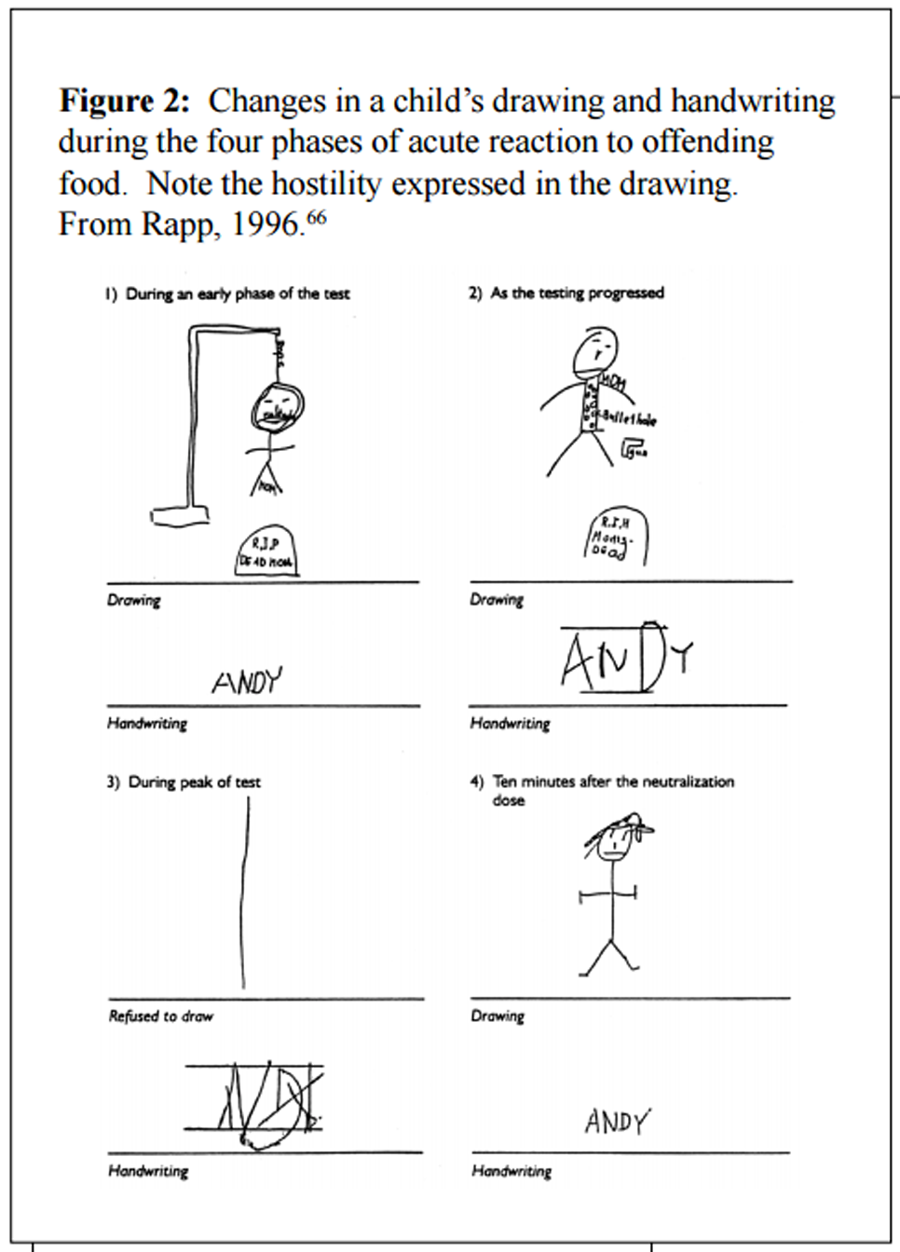
Figure 2.
Changes in a childs drawing and handwriting during the four phases
of acute reaction to offending food. Note the hostility expressed
in the drawing. From Rapp, 1996. [66]
Data from two double-blind studies indicated 7376 percent of ADHD children responded favorably to food elimination diets. [61, 67] Maintenance on even more-restricted, low-antigen (oligoantigenic) diets raised the success rate to as high as 82 percent. [62, 63, 68] Invariably in these studies, reintroduction of the offending foods led to reappearance of symptoms.
Sugar intake makes a marked contribution to hyperactive, aggressive, and destructive behavior. [49, 61, 69] A large study by Langseth and Dowd found 74 percent of 261 hyperactive children manifested abnormal glucose tolerance in response to a sucrose meal. [70] Other studies have been conducted, but industry interests may have influenced their outcomes in a manner inconsistent with good scientific research.
Wolraich and collaborators conducted a trial on sugar and hyperactivity that was published in the New England Journal of Medicine in 1994. [55] The findings were portrayed by the study investigators and the media as proving that sugar did not significantly contribute to hyperactivity. Yet the control, "low-sugar" diet averaged 5.3 teaspoons of refined sugar per day, fed to children aged 610 years. This "baseline" level of sugar intake is arguably so high that the investigators should not have been surprised the "test" group on a higher sugar diet did not show significantly more symptoms than the "controls." No attempt was made to eliminate dietary allergens such as milk, wheat, and egg, which trigger behavioral problems in some hyperactive children, and all the children were allowed to consume soda drinks during the study. At the end of their report, the authors acknowledged their gratitude to General Mills, Coca-Cola, PepsiCo, and Royal Crown.
Metal Pollutants in ADHD
An amazing variety of toxins extant in the modern environment have deleterious effects on the central nervous system that range from severe organic destruction to subtle brain dysfunction. [71, 72] Toxic metals are ubiquitous in the modern environment, as are organohalide pesticides, herbicides, and fumigants, and a wide range of aromatic and aliphatic solvents. [35] All these categories of environmental pollutants have been linked to abnormalities in behavior, perception, cognition, and motor ability that can be subtle during early childhood but disabling over the long term.
Children exposed acutely or chronically to lead, arsenic, aluminum, mercury, or cadmium are often left with permanent neurological sequelae that include attentional deficits, emotional lability, and behavioral reactivity. [72] Lead is damaging to cognition and behavior in children, and can cause developmental delay and mental retardation as well. The many studies conducted on the neurotoxicity of lead serve rather as a model for studies with the other toxic metals. Perhaps their most significant consensus finding is that lead toxicity observes no threshold for causing damage. [73]
A meta-analysis of cognitive damage from lead exposure concluded there was no threshold for damage down to blood lead levels of 7µg/dl, [73] and levels as low as 10µg/dl have been linked to psychobehavioral deficits. In the U.S., more than three million children are estimated to have blood lead levels of 10µg/dl or higher. [73] In addition, increased tooth dentine-lead and hair-lead levels have been linked to increased distractibility and attentional deficit. Tuthill's group sampled hair lead levels from 277 first-grade children in Massachusetts who were diagnosed ADHD. [73] Hair levels ranged from 1µg/g to 11.3µg/g, and a striking dose-response relationship was found between hair lead level and the likelihood of being diagnosed ADHD by a physician and the rated severity of attention deficit.
Some deleterious effects ascribed to lead may include contributions from other metals. In ADHD subjects found to be loaded with more than one toxic metal, whether at high or threshold levels, the metals may be acting in combination to increase the totality of the toxic effect. [72] Thus, combinations of lead with aluminum, lead with arsenic, lead with cadmium, and aluminum with arsenic all have the potential for synergistic toxicity. [7577] As documented by Marlowe and collaborators, learning disabilities follow a pattern similar to ADHD, with lead, cadmium, and aluminum being the main culprits. [76] Lead and aluminum seem especially synergistic, and mercury has great potential for synergy with lead.
This growing body of pessimistic data strongly indicate that children with ADHD should be screened for heavy metal load, either where prior exposure is established and/or where other ADHD risk factors have been ruled out. Moon and collaborators [72] called for teachers to have parents complete a Metal Exposure Questionnaire in order to assist with this process. Where levels are found to be high, children can be detoxified via lead chelation therapy. David et al reported that chelation therapy significantly improved hyperactivity, impulsivity, conduct problems, and learning problems in children diagnosed ADHD with no apparent risk factors. [71]
Environmental Illness Affects Behavior
Doris Rapp, MD, is a foremost authority on environmental illness (EI) and ADHD. For over a quarter of a century in her pediatric practice she has documented the myriad response patterns children can display in response to dust, mold, or chemicals present in their environment. Symptomatologies of hyperactivity and impulsivity/loss of self-control are common. Rapp, together with a growing number of physicians and environmentalist scientists, believes that more and more individuals are falling prey to EI because of the continued widespread pollution of food, water, air, homes, workplaces, and schools.
The school environment is a major offending source of EI, for adults as well as children. Rapp [66] cited data that indicate 25,000, or one-third of all U.S. schools, need extensive repair or replacement due to significant contamination with lead, asbestos, radon, or sewage; leaking underground storage tanks; poor plumbing or ventilation; termites; or structural inadequacies. There are also the additional, and at times more significant, roles of dust, molds, indoor chemicals, foods, and microorganisms. Placed in a contaminated classroom environment, a child can quickly become tired and irritable and suddenly seem incapable of learning. According to Rapp, the child (as well as the teacher) "can feel confused, perplexed, bewildered, and depressed, when for no apparent reason they become irritable, moody, angry, sad, aggressive, vulgar, or can't think clearly." [66] Ironically, the adverse effects of daytime exposure to a contaminated school environment may not manifest fully until the end of the day, after the child is home. This can foster confusion between teachers and parents about the source(s) of the offending exposures.
Nor is the home a necessarily safe, clean, and protected environment. [66, 78] Chemicals in carpets and wall materials, dust, molds, microorganisms, lead in paint, radon contamination, and pollutants in air, water, and food can be as offensive and toxic in some home environments as in the worst schools. The modern parent must be vigilant for environmental insults and observant of their child, never abdicating this responsibility to the teacher or pediatrician, especially since most physicians are not skilled at diagnosis of EI. Rapp has a "Big Five" list of symptoms that, when used before and after an adverse exposure, are surprisingly effective at pinpointing an EI response. [66] These are:1. How does the child feel, behave, and remember?
2. How does the child's appearance change?
3. Is there any handwriting or drawing change? (for a typical example, refer to Figure 2)
4. Does asthma or other breathing problem appear?
5. Is there a change in the pulse rate or rhythm? (especially a sudden 20-point increase in the rate)Rapp maintains that in many children the signs of EI can be traced all the way back to infancy, even as far back as in utero, where they are hyperactive and hiccup frequently in response to foods their mothers ate, beverages she drank, or odors she smelled. As a child grows the symptoms of EI may change (e.g., the responses to milk and other dairy products differ between fetus, infant, toddler, child, adolescent, and adult). [66, 79] But these are merely different manifestations of adverse responses to the same food or other offending agent.
The environment surrounding the home, school, or community may not be any friendlier to the susceptible child. Indeed, the entire planetary environment is now suffused with organochlorines and other persistent organic pollutants. [35, 80, 81] Children are especially vulnerable to these substances, as they have higher cell-level turnover and relatively immature detoxification capacities. [82] Children are more susceptible to loss of brain function if exposed to neurotoxins during critical development periods, however low the exposure level, as is evident from studies on irradiation, drug, alcohol, and lead toxicities. [35, 80, 83]
Pesticides capable of injuring the central nervous system include metals, chlorinated hydrocarbons, organophosphates, and carbamates. [35, 78, 80, 81] The so-called "inert" pesticide ingredients include benzene, formaldehyde, and petroleum distillates, but all these are far from being inert to children. Crinnion recently reviewed the extent to which these toxic pollutants are ubiquitous in the air, water, soil, foods, and human indoor and outdoor environments. [78] Children may be exposed prior to birth, and/or after birth by ingestion, inhalation, transfer through mother's milk or baby food, and through skin contact.
Literally all residents of the industrialized countries can be shown to carry "background" levels-parts per billion to parts per trillion-of organochlorine pollutants in their tissues. [78, 80] Several studies of infants prenatally exposed to background environmental levels of organochlorine compounds demonstrated subtle damage to the thyroid system, associated with measurable changes in neurodevelopmental parameters. [75, 80]
Thyrotoxins and Neurodevelopmental Damage
Thyroid hormones help regulate neuro-transmitter systems-dopaminergic, noradrenergic, serotonergic-in the brain, and are pivotal to the very process of fetal maturation. [35, 84, 85]Regarding the possible contributory factors in ADHD, suspicion is growing around a possible role for thyroid hypofunction during early childhood development. A link between hypothyroidism during pregnancy and diminished mental function in the offspring has been recognized for more than 100 years, [85] and in 1969 came the first solid indication that mild maternal hypothyroidism could lower IQ values in the offspring.
The condition of generalized resistance to thyroid hormone, or GRTH, features reduced tissue responsiveness to thyroid hormone. [85] In children with GRTH attentional function is abnormal, [88] and among this population ADHD is very common, occurring in 4661 percent. [87] Studies with animals established that adequate thyroid system integration is required for the development of the same brain zones found to have subtle anomalies in ADHD, such as the caudate, cerebellum, corpus callosum, cortex, and hippocampus. [5] Children with ADHD have a higher frequency of occurrence of GRTH (estimated at 5.4%, versus <1% for non-ADHD children). [87,89]
In 1999, Haddow and a large collaborative group reported in the New England Journal of Medicine on a multi-center study that first screened blood samples from 25,216 mothers to assess thyroid adequacy, then tested their seven- to nine-year-old children for IQ, attention, language, reading ability, school performance, and visual-motor performance. [85] When the children from hypothyroid mothers (untreated during pregnancy) were compared with those of euthyroid (control) mothers, statistically significant impairments were documented for attention (WISC-III freedom from distractibility score, Continuous Performance Test of Conners) and school difficulties and learning problems, along with several measures of IQ and visual-motor performance.
The emerging evidence for involvement of thyroid damage in ADHD begs the question of what factors might be responsible for thyroid damage. Synthetic chemicals released into the environment (pesticides and herbicides) are the main suspects, along with industrial chemicals. [35, 84, 9093] In a major review of thyrotoxicity from chemicals, Brucker-Davis [35] listed 77 chemicals proven to damage the mammalian thyroid. Her list includes the most ubiquitous and persistent environmental pollutants, among them PCBs (polychlorinated biphenyls), dioxins, furans, chlorophenols, chlorobenzenes, phenols, and related substances, which are widespread in human tissues and routinely detectable in mother's milk. [78, 92, 93] The degrees of thyroid toxicity from these various chemical categories can be severe to mild, depending on the specifics of exposure. Severe thyroid damage does not appear necessary to effect developmental brain damage; in the landmark Haddow study, mild and asymptomatic thyroid hypofunction significantly correlated with attentional and other cognitive impairment in children in the U.S. Northeast. [85]
PCBs remain ubiquitous in the environment. In 1996, Jacobson and Jacobson reported in the New England Journal of Medicine on their study of 212 children born to women who had eaten Lake Michigan (USA) fish contaminated with PCBs. [91] The children were tested at 11 years of age. Prenatal PCB exposure was significantly associated with lower cognitive performance scores; the strongest deficits were related to attention and memory. Incidentally, this same pediatric population evidenced reduced weight and head circumference at the time of birth. [90, 94]
The Neurobiology of ADHD
Modern brain monitoring techniques have established that ADHD can be organically expressed in the brain. Neuropsychological assessments were the first techniques to successfully measure alterations in frontal cortical and frontal-basal ganglia information processing in the disorder. [5, 40] Ever more precise neurochemistry, neuroimaging, and functional neuroimaging techniques implicate these brain regions as well.
Neurochemical studies suggest alterations in catecholaminergic-mainly dopaminergic and noradrenergic-transmitter functions markedly contribute to the symptoms of ADHD (see Tannock [5] and Glanzmann [40] for reviews). The symptoms of ADHD are significantly ameliorated by agents that specifically influence these neurotransmitter systems, and animal studies implicate areas of the brain in which these neurotransmitters are most dominant. [96] Studies of these catecholamines and their metabolites in the blood, urine, and spinal fluid did not initially provide definitive results, [95] but with better study design there is promise for positive results in this area. [40]
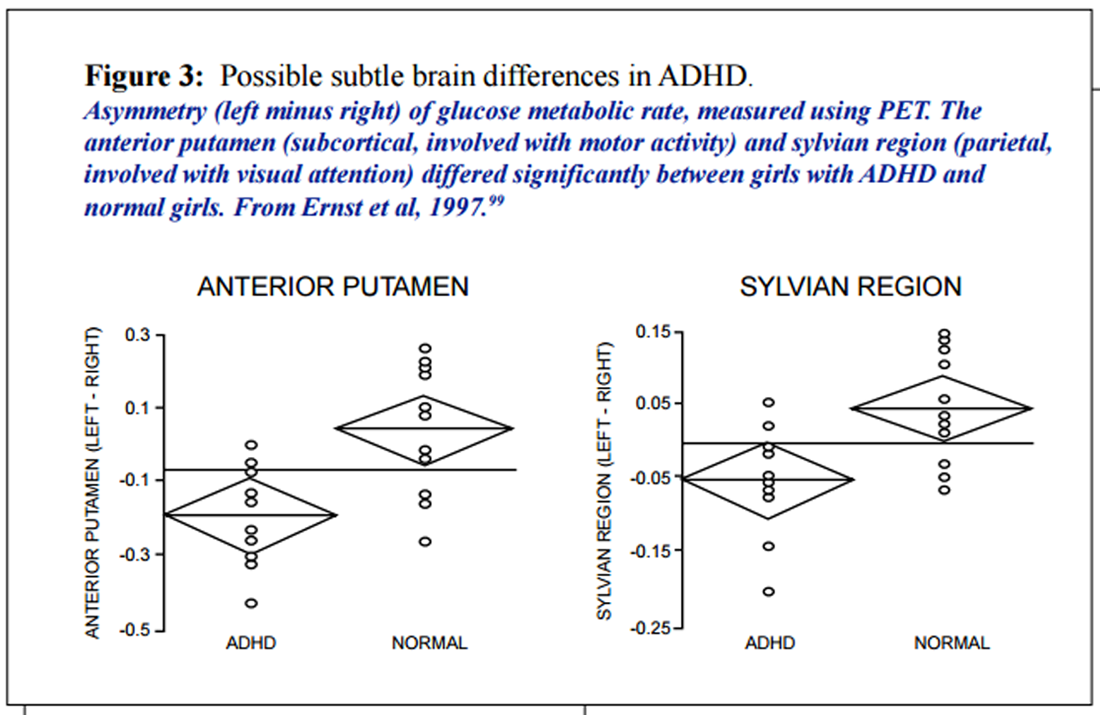
Magnetic Resonance Imaging (MRI) scanning can be used to reliably measure the size of a specific brain region. Fourteen studies using volumetric analysis by MRI were conducted on ADHD subjects and controls; they suggest localized abnormalities in the prefrontal cortex, basal ganglia, and corpus callosum of children with ADHD. [5, 40, 140 ] Smaller frontal lobe or right prefrontal cortex was found for the ADHD groups in all studies that examined this measure. Five of six studies found a smaller anterior or posterior corpus callosum. Four of six found loss of the normal caudate asymmetry (left side greater than right, see Figure 3, and these four also found a smaller left or right globus pallidus. [5] In two more recent studies, smaller volumes of right prefrontal cortex and of other structures involved in impulse control-the caudate and globus pallidus-correlated with deficient performance on response inhibition tasks in boys with ADHD. [97, 98]
Figure 3.
Possible subtle brain differences in ADHD
Functional/dynamic neuroimaging is a field undergoing particularly rapid development. The techniques include positron emission tomography (PET), single-photon PET (SPECT), quantitative electroencephalography (QEEG), and functional MRI (fMRI). These help quantify brain metabolic activity and correlate it with anatomical differences in the brain, on a real-time basis. Certain QEEG measures do consistently differ between ADHD and normals, but their functional meaning is not yet evident. Measures of event-related potentials document P300 wave differences consistent with ADHD children being deficient in response selection and organization. [95] With PET, abnormal regional blood perfusion is evident in the striatal region of ADHD children. [100] Zametkin obtained similar findings in adults101 but fell short of statistical replication in children. [102] Meanwhile, the first SPECT study in children revealed the ADHD group had greater overall metabolic asymmetry, with less activity in the left frontal and left parietal regions. [103]
From the neurobiological studies a consensus is emerging that motor and attentional functions associated with the frontal cortex are adversely affected in ADHD. [2, 40, 104]Taken altogether, the volumetric and correlational functional analyses roughly point to the frontostriatal circuitry, and possibly intracortical connections via the corpus callosum, in the neuropsychological deficits associated with ADHD. These zones are predominantly dopaminergic, and hypofunction of dopamine pathways is a consistent feature of the disorder. The diagnostic potential of this information is becoming evident. The cerebellum is functionally linked with the prefrontal cortex, and three anatomical measures, namely the right globus pallidus volume, caudate asymmetry, and left cerebellum volume, correlate highly with ADHD in children. [5] But overall, with the differences running as small as five percent less than normal, [98] definitive conclusions on brain region differences in ADHD must await further quantitative and qualitative analyses. The rapidly increasing understanding of the normal growth cycles of the brain should enable better design of controlled normal vs ADHD comparisons in this area.
Roles of Nutrient Deficiencies and Imbalances
Nutrients are required by the brain, as they are by every other organ, so virtually any nutrient deficiency can impair brain function. [49] Assessment of ADHD children often reveals nutrient deficiencies or imbalances which, when corrected, result in considerable behavioral and academic improvement. Little controlled research has been conducted into dietary supplementation effects on ADHD, but the sparse data available do indicate significant potential for benefit in this realm. This subject recently was reviewed by Galland. [106]Multiple vitamin-mineral supplements Dietary supplementation can improve academic performance in healthy school-aged children. In a series of studies that spanned 18 years and culminated in a double-blind trial, Schoenthaler et al found that a vitamin-mineral supplement produced significantly less antisocial behavior than did placebos in healthy elementary school children and teenage delinquents. [107] Cognitive performance also was significantly improved, but the researchers found no clinical improvement could be expected unless at least one nutrient was abnormally low by blood test. Pyridoxine, folic acid, thiamin, niacin, and vitamin C were the nutrients most commonly found to be low in children who responded to supplementation with measurable improvement. Deficiencies of vitamins A, E, B12, pantothenic acid, riboflavin, and of minerals also were linked to bad behavior. Improvement could not be expected unless all deficiencies were corrected.
B Vitamins in Combination Two early controlled trials utilized combinations of B vitamins against ADHD and reported no benefit. [108, 109] Later, Brenner successfully used B vitamin combinations to treat hyperkinetic children who had not responded favorably to Feingold's diet. [110] They also found that ADHD children responded variably to different B vitamins, with pyridoxine and thiamine antagonizing each other's benefits. Treatment with single B vitamins rather than combinations may sometimes be necessary in order to normalize lowered blood levels and selectively increase transmitters in ADHD; for example, pyridoxine can be used to normalize lowered blood serotonin. [106]
Vitamin B6 (pyridoxine) This vitamin might help ameliorate hyperactivity, as indicated from widespread physician experience and one small double-blind trial conducted to date. Vitamin B6 is an essential cofactor for a majority of the metabolic pathways of amino acids, including decarboxylation pathways for dopamine, adrenaline, and serotonin. In 1979, Coleman et al reported that B vitamins improved the behavior of some children with ADHD in a double-blind crossover comparison with methylphenidate. [111] Coleman's group took note of physician observations that in some hyperactive children blood serotonin levels are low, and that high-dose B6 often benefited the symptoms while boosting serotonin into the normal range. They investigated six children ages 8-13, diagnosed with Hyperkinetic Reaction of Childhood (DS-II) and known to be responsive to methylphenidate. In a double-blinded, multiple crossover trial, each child received placebo, low and high doses of methylphenidate (averaging 10.8 mg/day and 20 mg/day, respectively), and low and high doses of B6 as pyridoxine (averaging 12.5 mg/kg/day and 22.5 mg/kg/day) over 21 weeks. Blood serotonin levels increased dramatically on B6, and teacher ratings showed a 90 percent level of statistical trend in favor of B6 being slightly more effective than methylphenidate.
Iron This is the most common of all nutrient deficiencies in U.S. school-age children. [49] Iron deficiency is associated with markedly decreased attentiveness, narrower attention span, decreased persistence, and lowered activity levels, which respond positively to supplementation. An uncontrolled Israeli study of boys with ADHD found a 30 percent improvement in Conners Rating Scale scores following iron supplementation. [112]
Magnesium According to Galland, [106] the magnesium deficiency status often observed in ADHD is reminiscent of Latent Tetany Syndrome, which features lowered red cell levels of the mineral. This disorder is believed related to three factors: inadequate dietary magnesium (Mg) intake, genetic susceptibility, and the Mg-depleting effects of catecholamines and related stress hormones which are elevated in the blood and urine of ADHD children. A Polish team reported reduced Mg levels in 95 percent of a group of 116 children with ADHD; [113] dietary supplementation with Mg significantly decreased their hyperactivity. [114]
Zinc Several studies conducted in different countries have found this mineral to be low in ADHD (for references see Galland). [106] Serum zinc can be markedly below normal, [115] and also urinary zinc clearance can be lower; both findings suggestive of poor zinc intake and/or absorption. Findings from one placebo-controlled trial suggest poor zinc status also may predict poor response to amphetamine treatment of the disorder. [116]
Essential fatty acids (EFA) These oily, vitamin-like nutrients have shown promise in the non-pharmaceutical management of ADHD. The two main classes-omega-3 and omega-6-have a complementary, "yin-yang" relationship, functioning as pro-homeostatic constituents of cell membranes and as precursors to smaller molecules (eicosanoids) that transduce information inward to the cell interior, and outward from each cell to influence other cells. The longer-chain, 20- and 22-carbon species are both crucial for prenatal and postnatal early brain development. Some adult humans can generate the longer-chain molecular species from the shorter-chain, but infants are less competent in this regard. [117] The C22:6 omega-3 (docosahexaenoic acid, DHA) and the C20:4 omega-6 (arachidonic acid, AA) are homeostatically balanced in human mother's milk, and both are now added to infant feeding formulas.
One reliable symptom of EFA deficiency in both animals and humans is excessive thirst (polydypsia), without matching polyuria. Colquhoun and Bunday, [118] working with the Hyperactive Children's Support Group of the United Kingdom, were the first to report that children with hyperactivity were significantly more thirsty (and without comparable polyuria) than children who were not hyperactive. Mitchell et al [119] measured plasma fatty acids in 44 hyperactive children and 45 matched control subjects, and found the hyperactive children had significantly lower concentrations of DHA, AA, and the AA precursor DGLA (dihomo-gamma linolenic acid, C20:3 omega 6). Stevens et al [120] extended these promising results, and Stordy correlated the symptoms with omega-3 deficiencies and learning disabilities. [132]
Stevens and her collaborators at Indiana University measured plasma and red cell fatty acid levels in 53 boys with ADHD and 43 controls, aged 612 years. [120] They also took detailed histories, compared clinical symptom patterns, and tracked daily dietary EFA intakes. They confirmed Mitchell's earlier report [119] of lowered plasma concentrations of DHA and AA (but not of DGLA); and found plasma eicosapentaenoic acid (EPA, C20:5 omega 3) was decreased, as was red cell arachidonic acid. As tracked by the parents, the ADHD group had significantly greater thirst, frequency of urination, and dry skin-all indicators of EFA deficiency-than did the control subjects. [121] Within the ADHD group, a subgroup with higher scores for EFA deficiency also had the lowest levels of plasma EFA. [124]
The omega-6 fatty acid GLA (gamma-linolenic acid) is a metabolic precursor to AA. [141] GLA was administered to ADHD children in two placebo-controlled studies. In the first, parents' ratings suggested benefit from GLA but teachers' ratings did not. [122] In the second, parents' ratings did not suggest benefit but one teachers' rating of benefit the Conners Hyperactivity Factor did achieve statistical significance. [123] Future studies might be more definitive if objective measures are taken to establish EFA status and if mixed omega-3 and omega-6 long-chain fatty acid preparations are administered.
The polyunsaturated, long-chain DHA and AA affect the biological and physical properties of cell membranes, as well as the functionality of numerous important membrane proteins. The biochemical fates of DHA and AA are structurally and functionally intertwined with the phospholipid substances that make up the bulk of the cell's membrane systems.
Phosphatidylserine (PS) and Other Phospholipids [105] Most of the reactions that collectively amount to life occur on or in cell membranes. These are the physical-chemical entities on which the vast majority of the cell's enzyme assemblies are mounted. The phospholipids (PL) are the main foundational molecules for all cell membranes, serving much as building blocks for the membrane matrix into which the proteins are inserted. Within the membrane, the phospholipid (PL) molecules act as "parent" molecules for the long-chain, essential fatty acid molecules. They hold the EFA in position within the membrane, enabling enzymes of the membrane to metabolize the EFA to eicosanoids and other regulatory messenger molecules as appropriate.
Of the phospholipids, phosphatidylcholine (PC) is quantitatively the most common in all membranes. PC is also the body's main reservoir for choline, a small amine that is a component of the neurotransmitter acetylcholine. The PC precursor dimethylaminethanol (DMAE) is a major substrate for making PC in the body; it can have a stimulant-type action in the ADHD brain, and has been used with moderate success in the treatment of children with ADHD and developmental disorders. [125] DMAE does have adverse side-effects at high doses, [126] but was effective against "hyperkinesis" in one double-blind trial and against learning disorders in another. [125]
Phosphatidylserine (PS) is clinically proven to benefit a wide range of brain functions. [105] This phospholipid occurs in the brain at far higher concentrations than it does in the other organs. It is a key constituent of nerve cell synaptic membranes, which are deeply involved in the production of neurotransmitters, their packaging for subsequent release, and their action via receptors located at the synaptic junctions. Ingested as a dietary supplement, PS energizes the human brain, facilitating synaptic connectivity and specifically boosting dopamine transmitter functions, i.e., its production, release, and postsynaptic receptor actions. In a physician in-office study of 21 consecutive ADHD cases aged 419, dietary supplementation with PS benefited greater than 90 percent of the cases. [127] At intakes of 200300 mg/day of PS for up to four months, attention and learning were most consistently improved. Oppositional conduct proved most resistant to PS treatment.
Other Nutrients Many of the neurotransmitters are metabolically derived from amino acids. Analyses of plasma amino acid levels determined that phenylalanine, tyrosine, tryptophan, and isoleucine were lower in ADHD patients than in controls. [128] In adults with ADHD, L-tyrosine treatment produced transient improvement. [128, 130] Also in ADHD adults, S-adenosyl methionine seemed beneficial in one small, short-term, uncontrolled study. [131]
A complex mixture of bioflavonoids (oligomeric proanthocyanidins or OPCs), which have potent antioxidant activity, were reported to benefit ADHD in an undisclosed proportion of children seen in a pediatric practice. [133] The symptom clusters related to attention and distractibility seemingly responded more significantly than hyperactivity and impulsivity. Side-effects were said to be minor.
Many among the wholistic/integrative practitioners who have substantial experience with ADHD believe intestinal dysfunction and dysbioses are important contributors to ADHD symptomatology. A proprietary mixture of oligosaccharides, which sometimes serve as substrates for probiotic intestinal bacteria, was reported to decrease the severity of ADHD in children during a six-week observation period. [134]
With the numerous nutrient deficiencies documented in ADHD, and the promise offered by a range of nutrients in controlled and non-controlled clinical trials, Galland's approach is a proven blueprint for success. [79, 106] He tests for signs and symptoms of EFA deficiencies, and corrects these through supplementation. Using a similar approach, he selects candidates for magnesium therapy. With the B vitamins, to avoid the potential for paradoxical responses he suggests careful titration using individual vitamins rather than beginning with mixtures; e.g., pyridoxine first, followed by thiamine, then by the others one by one. Serum ferritin and hair zinc levels can be useful as rough guides for supplementation with these minerals. In his view the nutrients PS and DMAE are particularly deserving of further study, especially for those ADHD children with learning disabilities. [106]
Developing an Integrative Treatment Model
Modalities for medical management of ADHD, other than the use of psychostimulants, have historically been minimized by the medical mainstream. Even so, ADHD has become a testing ground for modern wholistic/integrative medical management, at least as an alternative to the current "mainstream" predilection for carte blanche prescription of methylphenidate.
Safer and more effective treatment options are readily available to the interested practitioner; when combined and individualized to the ADHD child the success rate approaches 100 percent. First in order is dietary revision: removal of food additives, sensitizing foods, and sugar (sucrose) from the diet invariably results in some degree of improvement. [135137] Then the child should be thoroughly assessed for allergies, nutrient deficiencies, and intolerances to foods and chemicals. The toxic burden should be assessed and corrected, including lowering the body burden of organics [78] and potentially toxic metals. [71] Lead contamination is an obvious culprit in some cases of hyperactivity; aluminum cookware and silver-mercury dental fillings should be avoided.
In ADHD every effort should be exerted to pursue the benefits from dietary modification and nutrient supplementation prior to resorting to psychostimulant pharmaceuticals. One clear benefit is that nutrients predictably have broader effect spectra and superior benefit-to-risk profiles. The foundational, pro-homeostatic benefits afforded by vitamins, minerals, essential fatty acids, phospholipids, and other nutrients to brain function would seem more compatible with the wide range of behavioral and cognitive symptom overlap seen in the ADHD population. Pharmaceuticals, by contrast, are mechanistically much more exclusive and therefore demanding of more precise symptom differentiation and diagnosis. Up to this point, nutrients and nutrient combinations have not been given a fair evaluation against ADHD and its constellation of co-morbid conditions.
For the practitioner managing ADHD, making a commitment to explore dietary supplementation as a treatment modality does not mean abandoning the use of stimulants and other pharmaceutical medications. The use of nutrients for symptom control in ADHD is not incompatible with the use of drugs; nutrients are compatible with drugs to a degree far superior to the compatibility of drugs with other drugs.
Charles Gant, MD, PhD, is one practitioner who has evolved from an allopathic philosophy of medical practice to a fully integrative practice for managing ADHD. He has advocated striking a balance between the conventional approaches to treating ADHD, with the strikingly bad drug side-effects involved, and the safer though less formally established, "alternative" or "complementary" approaches. Gant continues the tradition of other wholistic/integrative physicians who employ a wide spectrum of modalities to successfully treat ADHD. [49, 5861, 6466, 79, 106, 136137] Gant's idealized "nine-point" program is summarized in Figure 4.
Figure 4.
Possible subtle brain differences in ADHD
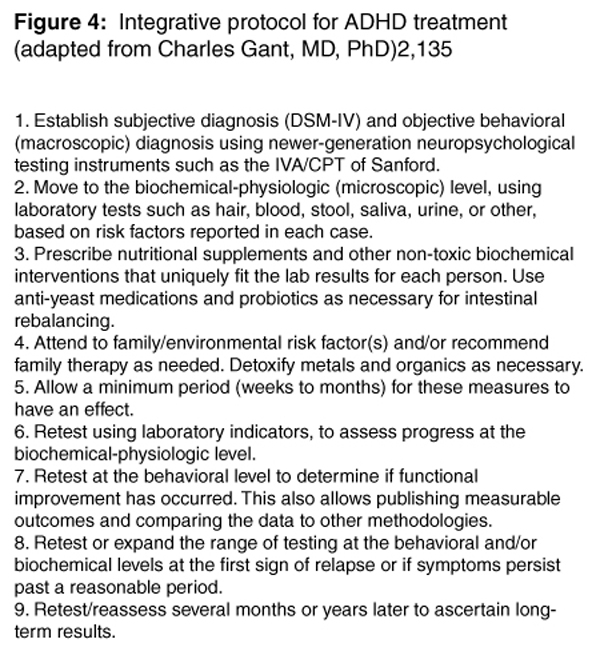
Gant does an intake screening on the patient suspected of having ADHD and searches for seven target symptoms-hyperactivity, impulsivity, inattention, mood lability, temper outbursts, disorganization, and stress sensitivity. He then applies the more extensive DSM-IV diagnostic criteria,1 and with the diagnosis established he proceeds with his "Ideal Protocol" as summarized in Figure 4. He treats approximately 50 percent of his ADHD patients with antibiotics and other medications, mostly to remove gastrointestinal dysbiotic organisms and to chelate heavy metals.
Many children presenting with mental and behavioral abnormalities have intestinal bacterial imbalances from antibiotic overuse, as from treatment for ear infections, which are a proven risk factor for ADHD. [61] These children tend to have impaired speech and language development, and may have a two-fold higher risk of becoming learning disabled. [49] Gut dysbiosis-imbalances of the symbiotic bacteria, presence of nematode or protozoan parasites, yeast (Candida) overgrowth caused by antibiotic overuse-once corrected can manifest as multisystem improvement, including sometimes marked clearing of the mental-behavioral symptoms. [61] Fungi and their metabolites also play a role, and can be detected and treated. [138]
To most effectively treat ADHD, the integrative medical practitioner must also work closely with the subject and/or the parents to further eliminate toxic metals (e.g., lead, mercury) and chemicals (including cigarette smoke, home building materials, pesticide-contaminated foods, lawn and garden chemicals, etc.) from the child's environment-this can have the added benefit of improving the parents' health. Allergies must be tested for and eliminated, whether of the food-related or the inhalant type (pollen, mold, dust, volatile chemical).
The next phase in the integrative medical management of ADHD is to identify and correct nutrient deficiencies, especially of minerals (iron, magnesium, zinc, selenium, others); essential fatty acids; B vitamins; and other nutrients on a case-by-case basis. By this point the vast majority of hyperactive ADHD children are likely to be noticeably improved.
Objective testing of patients undergoing treatment for ADHD is important. Continuous performance tests (CPT) measure response preparation, planning and inhibition, and neuropsychological performance via the frontal lobes. CPT involve a period of testing during which numbers or letters are presented in rapid sequence on a computer screen and the subject is asked to respond selectively to them. Errors of omission are felt to represent inattention, while errors of commission (premature responses) may represent impulsivity; the total number of correct responses is thought to represent capacity for sustained attention. The IVA (Intermediate Visual and Auditory) CPT is probably the best of these. In two pilot projects, Harding, Judah and Gant used the IVA CPT to objectively assess improvements in ADHD children not sorted for co-morbidity. [135] They treated with methylphenidate or via nutraceutical interventions, and with or without their usual full workups for metal toxicity, gut dysbiosis, allergies and intolerances, and nutritional deficiencies prior to intervention. They found nutraceutical management was statistically superior over pharmaceutical management for improving response control and attention, including cases where the in-depth workups were NOT carried out.
After 36 months of testing-retesting and calibrating nutritional corrections, the use of medication may be considered if the child has not significantly improved or continues to be particularly impaired or oppositional. In any case, lower doses of medication can be used, and titrated upward only as necessary to meld with the benefits evident from the other interventions. The responsible integrative physician will use medication only when the non-pharmacologic protocols have been exhausted; Crook suggests that the non-allergic, non-hyperactive ADHD children are the subpopulation most likely to benefit from stimulant medication.
ADHD in the Future
The current extreme diversity of professional opinion about ADHD-whether debating the many possible contributory factors, speculating on its neuropsychology and neurobiology, dogmatically supporting or opposing the use of stimulant medications, spawning honest disagreement as to whether the disorder truly exists-promises to continue into the future. Some of the areas of controversy should soon take on new clarity, most notably the neurobiology of ADHD.
As the 1990s progressed, emphasis began to shift away from a purely "attentional deficit" as underlying ADHD, to a perhaps "intentional" deficit involving inappropriate response to an incoming stimulus, or a more delocalized deficit in the development of the inhibition of behavior. [5, 40] Increasingly it is becoming evident that ADHD subjects do pay attention, and do receive stimuli, but may have trouble processing the information and formulating an appropriate response.
With more research into the neurobiology of ADHD, more focused wholistic/integrative treatment regimens might be forthcoming. Increasing controversy over the widespread use of methylphenidate and possible life-threatening effects from its long-term use make it essential that complementary/alternative treatment regimens be implemented for ADHD management. Correction of nutrient deficiencies commonly found in these patients, along with dietary modification, allergy treatment, detoxification, correction of intestinal dysbiosis, family counseling, and behavior therapy can ameliorate symptomatology and allow the child diagnosed with ADHD to lead a normal and productive life.
References and Full-Text
Return to ADD/ADHD
Since 11052000


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |