

Adolescent Neck and Shoulder Pain--The Association
with Depression, Physical Activity, Screen-based
Activities, and Use of Health Care ServicesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Adolesc Health 2014 (Sep); 55 (3): 366–372 ~ FULL TEXT
Solbjørg Makalani Myrtveit, Børge Sivertsen, Ph.D., Jens Christoffer Skogen, Ph.D., Lisbeth Frostholm, Ph.D. et al
Department of Clinical Science,
University of Bergen,
Bergen, NorwayPurpose: Neck and shoulder pain is frequent in adolescents, and multiple factors seem to affect the risk of such symptoms. We aimed to investigate the prevalence of neck and shoulder pain in Norwegian adolescence and to examine whether behavioral and emotional factors were associated with the risk of neck and shoulder pain. Finally we aimed to investigate whether neck and shoulder pain was related to the use of health services.
Method: Data from the population-based study ung@hordaland were used. Participants were asked how often during the last 6 months they had experienced neck and shoulder pain. The association between frequent neck and shoulder pain and physical activity, symptoms of depression, and screen-based activities was evaluated using logistic regression analyses stratified by gender. The relative risk of visiting health services when reporting neck and shoulder pain was calculated using multiple logistic regression analyses.
Results: Frequent neck and shoulder pain was reported by 20.0% (1,797 of the total 8,990) and more often by girls than boys (p < .001). A high score of depressive symptoms was the strongest risk factor for neck and shoulder pain in both boys and girls (odds ratio = 6.14 [95% confidence interval 4.48-8.42] and odds ratio = 3.10 [95% confidence interval 2.63-3.67], respectively). Frequent screen-based activities slightly increased the risk while physical activity was protective. Individuals reporting neck and shoulder pain more often visited their general practitioner (47.1% vs. 31.8%) and school health services (24.6% vs. 13.5%).
Conclusion: Frequent neck and shoulder pain was reported in 20% of Norwegian adolescents. Symptoms of depression and screen-based activities increased the risk of neck and shoulder pain while physical activity was protective. Individuals reporting neck and shoulder pain visited health services more frequently than others.
Keywords: Adolescent health; Depression; Health services; Neck and shoulder pain; Physical activity; Risk factors; Screen-based activities.
From the Full-Text Article:
Background
Neck and shoulder pain (NSP) is frequent in adolescence [1], with prevalence estimates ranging from 21% to 42%. [2] Girls report NSP more frequently than boys [2–6], and the prevalence of NSP seems to increase from early to late adolescence. [4, 7]
Multiple factors, including behavioral and psychological, are related to neck pain. In cross-sectional studies, psychological factors such as depressive symptoms have been found to be associated with adolescent NSP [5, 8], and emotional distress seems to predict occurrence of weekly neck pain at follow-up among originally neck painefree adolescents. [9]
The use of computers has been suggested to increase the risk of neck pain, possibly due to insufficient recovery after local muscle fatigue related to static work and repetitive movements. [10] This hypothesis was supported in adults working at visual display units demonstrating increased risk of musculoskeletal problems, including neck pain. [11, 12] Only a fewstudies have investigated the association between screen-based activities and NSP in adolescents, with conflicting results. [5, 7] In a Dutch schoolebased study, no relation was found between computer use and NSP. [5] In contrast, a Finnish study found an increased risk of NSP in adolescents spending more than 2e3 hours per day on the computer. [7]
Physical activity has also been proposed to influence the risk of NSP, but findings are inconsistent. Physical activity has been found to be unrelated to NSP [1, 5], to decrease the risk of NSP [6, 13], or even to increase it. [3] Thus, while psychological factors have consistently proven to be related to NSP, the impact of physical activity and computer use is less certain.
The importance of understanding which factors are associated with NSP is strengthened by the chronicity of these health complaints. Individuals experiencing back and neck pain in their teens are at increased risk of similar symptoms later in life. [13] The costs related to neck pain are substantial [14], and young adults sick-listed for NSP or back diagnoses are at high risk of being granted disability pension awards. [15] Health care services may be an important venue for identifying NSP and co-occurring factors, with the possibility of preventive treatment efforts. However, little is known regarding the use of health care services among adolescents with NSP.
The aims of the present study were threefold. The first aim was to investigate the prevalence of NSP among Norwegian adolescent boys and girls. Based on the research reviewed, we hypothesized that NSP would be common and more frequent among girls. The second aim was to examine the association between NSP and several behavioral and psychosocial factors. We hypothesized that NSP would be significantly associated with time spent at computers/screens, physical activity, as well as symptoms of depression. Finally, we aimed to investigate the use of health services among adolescents experiencing NSP, and how this use is affected by symptoms of depression. As adolescents with other chronic pain conditions display a high use of health services, we hypothesized that adolescents with NSP would use health services more than others.
Method
Population
In this population-based study, information from the ung@hordaland-survey was employed. All adolescents born between 1993 and 1995 living in Hordaland, Western Norway, in the spring 2012 (n = 19,430) were invited to participate. [16, 17], Adolescents in upper secondary education received information per e-mail, and one school hour was allocated for completing the questionnaire. Those not in school received information by mail at their home addresses. The questionnaire was web based and covered a broad range of health issues, daily functioning, use of health and social services, and demographic variables. Uni Health, Uni Research collaborated with Hordaland County Council in conducting the study. A total of 10,220 (53%) adolescents participated.
Variables
Neck or shoulder pain
Participants were asked how often they had suffered from neck and shoulder pain during the last 6 months. The answer possibilities were “more or less every day,” “more than once a week,” “every week,” “every month,” and “seldom/never.” A dichotomous variable was created, dividing individuals experiencing frequent NSP (“more than once aweek” and “more or less every day”) from those rarely experiencing NSP.
The question on NSP used is similar to and has been evaluated with the items in the thoroughly validated HBSC (Health Behaviour in School-aged Children) symptom checklist. [18] The HBSC differentiates well between children who experience well being and those who do not and reflects functional ability. [18] The n = 363 participants not answering this question were excluded.
Hypothesized predictors of neck and shoulder pain
Physical activity.
Participants were asked how many days during the last week they had been physically active for more than 60 minutes. Individuals were divided into three groups: those reporting zero days of activity, those reporting 1e4 days, and those reporting 5–7 days.
Symptoms of depression.
Symptoms of depression were measured using the Short Mood and Feelings Questionnaire, a measure of depressive symptoms in children and adolescents. [19] The instrument consists of 13 items on feelings, thoughts, and actions the last 2 weeks. Each item has three levels differentiating between “true,” “sometimes true,” and “not true.” High internal consistency between the items and a strong unidimensionality has been shown in population-based studies [19] and was recently confirmed in the sample included in this study. [20] As in previous research [21], a dichotomous variable was created, using the 90th percentile of the sum score. Also, an ordinal variable was used, expressing the sum score attributed to each participant. As each of the 13 statements could yield a value between zero and two, this variable ranges from 0 to 26.
Screen-based activities.
The participants were asked how many hours per day, after school, they spent on TV games, PC games, chatting, reading, or writing e-mails or other activities at a computer/screen. For each activity, the participants could answer “no time,” “less than half an hour,” “half an hour to an hour,” “2 to 3 hours,” “4 hours,” and “more than 4 hours.” As reporting spending 2 or 3 hours or more per day at screen-based activities has been found to increase the risk of NSP [7], for each activity a dichotomous variable was created; individuals reporting “2 to 3 hours” or more were set as spending a lot of time on the activity. The n = 406 not answering questions on the hypothesized predictors of NSP were excluded.
Use of health services
Participants were asked whether they had been in contact with the school health services or their general practitioner (GP) during the last school year (dichotomous variable) and the frequency of these visits (every week, every month, every third month, every sixth month, less frequently). The n = 4 not answering questions on health services were excluded.
Background variables
Information on age and gender was retrieved from national registers, using a unique 11 digit personal identification number given to all citizens in Norway. Participants were asked what best characterized their vocational situation: “student in school,” “apprentice,” or “not in school.” Socioeconomic status in the family was measured by asking the participants if they considered their family economy compared to others to be “average,” “better”, or “worse.” The n = 459 not providing information on sociodemographics were excluded.
Statistical procedure
List-wise deletion was used to exclude individuals with missing information, leaving us with a study population of 8,990 individuals. Frequency of reported NSP was investigated. The percentage of individuals experiencing NSP was computed within groups based on background characteristics: age, gender, vocational situation, and perceived family economy. Logistic regression analyses stratified by gender were used to calculate the risk of frequent NSP related to symptoms of depression (dichotomous variable), physical activity, and screen-based activities. Analyses adjusted for background variables were conducted. The associations between NSP and physical activity and between NSP and screen-based activities were also adjusted for symptoms of depression (ordinal variable).
Logistic regression models using the variable describing depressive symptoms on an ordinal scale were conducted. Based on the information from this analysis, using postestimation analyses, the predicted mean probability of frequent NSP across Short Mood and Feelings Questionnaire sum score was calculated and expressed in a graph.
The relative risk ratio (RRR) for visiting health services (different frequencies) when reporting frequent NSP was investigated, using multinomial logistic regression. The association was adjusted for sociodemographic variables and symptoms of depression (ordinal variable).
Finally, using logistic regression, the relative risk for visiting health services (dichotomous variable) was investigated and compared between individuals reporting no NSP and no depression (reference group), those reporting NSP only, those reporting depressive symptoms (dichotomous variable) only, and those reporting both NSP and depressive symptoms (dichotomous variable).
STATA/IC 12.0 [22] for Windows was used.
Ethics
The Bergen Child Study was approved by the Regional Committee for Medical and Health Research Ethics, Region West.
Results
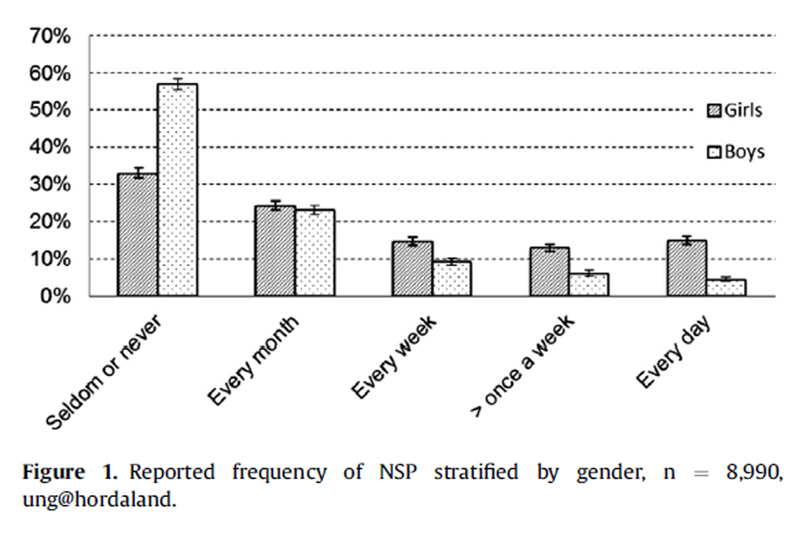
Figure 1

Table 1
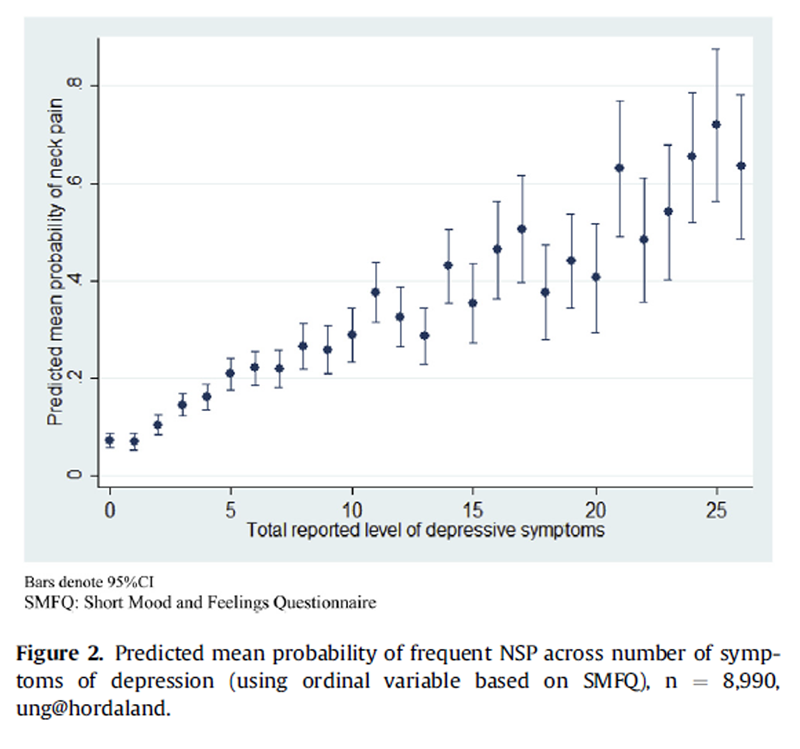
Figure 2

Table 2 The mean age in our sample was 17.8 years, and 53.7% were girls. About 98.1% were students, 1.3% were apprentices, whereas .7% were not in school. 20.0% (n = 1,797) reported frequent NSP (more than once a week). 28.0% of the girls reported frequent NSP, compared with 10.7% of the boys (p < .001; Figure 1).
In total, 12.1% of the participants were excluded due to missing data. These did not differ from those included regarding age, but significantly more boys than girls were excluded (p < .005). As boys report less NSP than girls, excluding more boys could lead to an overestimation of the proportion reporting NSP. This was taken into account by stratifying analyses by gender.
In our sample, age and vocational situation were not significantly associated with NSP (Table 1), but individuals reporting frequent NSP more often reported poor family economy.
Reporting a high score of depressive symptoms increased the risk of reporting NSP (odds ratio [OR] = 3.10, 95% confidence interval [CI] 2.65–3.67 for girls and OR = 6.14, 95% CI 4.48–8.42 for boys). Adjusting for background variables (age, school situation, and family economy) did not significantly alter the results. A doseeresponse relationship was founddthe higher the level of depressive symptoms, the higher the predicted mean probability of NSP (Figure 2).
As listed in Table 2, frequent screen-based activities slightly increased the risk of NSP for both boys and girls. The separate activities affected the risk of NSP differently, also between genders. The activities increasing the risk the most were for boys e-mailing (OR = 3.22 [95% CI 2.24–4.63]) and for girls PC games (OR = 1.89 [95% CI 1.45–2.46]). For none of the screen-based activities, adjusting for sociodemographic variables significantly altered the results. Adjusting for depression, however, reduced the association between screen-based activities and NSP. Consequently, only reporting e-mailing for 2 hours or more among boys and PC games for both genders remained significant risk factors for NSP.
Individuals reporting NSP were less physically active than those not reporting NSP. Performing physical activity 1e3 days a week reduced the risk of reporting NSP for both boys and girls (OR = .47, 95% CI .35–.63 and OR = .61, 95% CI .50–.73, respectively), and performing physical activity 4–7 days a week was more protective. Adjusting for sociodemographic variables did not significantly alter the results. Adjusting for symptoms of depression, however, reduced the protective effect of physical activity on NSP.
The use of health care services was significantly associated with NSP. Among adolescents with NSP, 47.1% had visited their GP compared with 31.8% in the non-NSP group. A similar pattern was found for school health services; 24.6% among adolescents with NSP had used this service compared with 13.5% in the non- NSP group (both Ps < .001).

Table 3 NSP was also related to the frequency of visits to health services. As listed in Table 3, therewas a doseeresponse relationship between NSP and frequency of visits to GPs and school health services. The RRR increased along with the frequency of visits, the RRR being highest for visiting GP and school health services every week (RRR = 6.59, 95% CI 3.11–13.97 and RRR = 4.32, 95% CI 2.77–6.74, respectively). Adjusting for sociodemographics only slightly attenuated the associations. Additional adjustment for symptoms of depression reduced the association between NSP and use of health services, but for the use of GP, all associations remained significant in the fully adjusted model. For the use of school health services, after controlling for both background variables and symptoms of depression, most associations were no longer significant.
Adolescents reporting NSP and co-morbid symptoms of depressionhad higheruse ofhealthservices (GP: RRR=2.40, 95% CI 1.96–2.93 and school health services: RRR=3.47, 95% CI 2.79–4.32) than adolescents reporting NSP only (GP: RRR = 1.81, 95% CI 1.61–2.04 and school health services: RRR= 1.94, 95%CI 1.68–2.25) or symptoms of depression only (GP: RRR = 1.22, 95% CI 1.00–1.49 and school health services: RRR = 2.49, 95% CI 1.99–3.11).
Discussion
Summary of findings
In this study, one fifth of adolescents, and more girls than boys, experienced frequent NSP. Adolescents experiencing NSP reported more symptoms of depression, less physical activity, and more screen-based activities than adolescents without NSP. The associations between NSP and physical activity and screen based activities were partly explained by depression. NSP was associated with frequent visits to the GP and school health services, co-morbid NSP and depression even more so.
Interpretation of findings
About one in five reported frequent NSP in our sample. Research investigating younger adolescents has found lower frequencies; for instance, in Finland, persistent weekly NP was reported by only 5% of 9- to 12-year-olds. [9] The frequency of NSP [3, 4, 7] and other subjective health complaints [23] seems to increase from early to late adolescence. In our sample, age did not significantly impact the risk of NSP. We did, however, investigate a narrow age span in late stages of puberty.
In accordance with the literature [3, 5], NSP was more frequently reported among girls. This is in line with the general pattern of women experiencing more musculoskeletal pain [24] and more chronic pain conditions [25] than men. In both medical samples and community samples, women tend to report more intense, numerous, and frequent bodily symptoms. [26] A number of factors have been proposed to contribute to this discrepancy, such as innate differences in somatic and visceral perception [26] and a lower pain threshold in women compared with men. [27] Further, symptom reporting may be affected by gender differences in readiness to acknowledge and disclose discomfort. [26]
In our study, depressive symptoms were strongly associated with NSP, confirming the well-established link between pain and depression. [28, 29] Also previous studies have found adolescent NSP associated with depressive symptoms [5, 8], and among originally neck paine free early adolescents, psychological symptoms predicted weekly neck pain during follow-up. [9] Multiple theories aim to explain the relationship between pain and depression, with a probable reciprocal relation as pain transmission might be altered by affective illness, while nociceptive input might induce or exacerbate depressive states. [28]
Physical activity was in our study associated with reduced risk of NSPdin accordance with several previous studies. [6, 13] This finding could be explained if individuals with NSP engage in less physical activity due to pain. In contrast, performing physical activity could prevent pain and lower the risk of developing NSP. This theory is supported by prospective findings where physical exercise was associated with lower prevalence of NSP 7 years later. [13] However, other studies have found physical activity unrelated to NSP [1, 5] or even to increase the risk of NSP [3]. This could imply that not only time spent being physically active but also type of activity is important in the association between physical activity and NSP.
As adjusting for symptoms of depression reduced the protective effect of physical activity on NSP, some of the effect of physical activity on NSP could be mediated through depression. Physical activity is thought to reduce the risk of common mental disorders [30, 31], and as discussed above, depression is linked to pain. In adolescents, physical activity has been found to be positively related to physical self-image, physical health status, quality of life, and quality of family and peer relations [32], strengthening such theories.
In our sample, spending much time on screen-based activities increased the risk of NSP. The activities increasing the risk the most were e-mailing for boys and PC games for girls. Also previous research has found computer use to be an independent risk factor for adolescent NSP. [7] Insufficient recovery after local muscle fatigue related to static work and repetitive movements could possibly explain this. [10] However, adolescents spending a lot of time at screen-based activities are not only at risk of musculoskeletal problems; both boys and girls spending much time on the Internet are more likely to report depression. [33]
Screen-based media use has been found to be negatively related to physical health status, quality of life, and quality of family relations. [32] Further, high school girls reporting computer gaming have been found to be more likely to report getting into serious fights and carrying a weapon to school [34], while boys spending a lot of time on the Internet have increased risk of being overweight. [33] In our study, adjusting analyses for depressive symptoms reduced the association between screen-based activates and NSP. In line with the literature, it thus seems that the risk related to screen-based activities is not necessarily dependent on actual number of hours spent at a screen or mediated through direct physical changes in muscles but is affected by gender, type of activity, and mental health.
Individuals reporting NSP visited their GP and the school health services significantly more frequently than others. Among individuals reporting NSP, 47.1% had seen their GP during the last yeardcomparable with figures seen in adults reporting similar problems. [35] A high percentage of children and adolescents experiencing chronic pain have been found to visit their GPs also in previous research. [36]
The association with NSP increased along more frequent visits, especially for GP. This could demonstrate a pattern of high health care use in adolescents with NSP, paralleling the frequent use of health care services in adults with similar symptoms. [37] The high use of health care services in adolescents may be a precursor of subsequent health service use and functional impairments, such as sick leave and work disability. At the same time, the frequent health care use may be a window of opportunity to identify these adolescents and to start prevention or treatment.
Co-morbid NSP and symptoms of depression were more strongly associated with health service use than reporting symptoms of depression only or NSP only. Pain has been found to precipitate worry and pessimism, while depression impairs patients’ abilities to cope with pain [28], possibly explaining some of the increased health services use among individuals reporting co-morbid symptoms of depression and NSP.
Strengths and limitations
The main strength of this study is the large sample size. Few studies investigating the association between NSP and physical activity and screen-based activities have been conducted, and findings have been inconsistent. Further, whereas most previous studies have focused on only one or two of the predictive factors here investigated, we had the advantage of using a sample large enough to enable evaluation of the association between NSP, screen-based activities, symptoms of depression, and physical activity in one sample. The large sample size further allowed for adjustment for sociodemographic variables as well as depression and gender-stratified analyses.
The primary limitation is the use of a cross-sectional sample precluding insight into the causality between NSP and the potential predictors. A further limitation is that no information on nonparticipants is available.
As previous research has indicated that different screenbased activities are associated with different health-related outcomes [33, 34], the ability to investigate the association between NSP and a range of different screen-based activities is a strength of the study. However, the information related to screen-based activities also has limitations. The answer categories for time spent at activities were not equally sized or spaced, making interpretation of a sum score that could have given valuable information on high users versus normal users difficult. Further, some participants reported spending more than 4 hours on multiple activities. This could indicate that some engage in, for instance, both chatting and gaming simultaneously and report the total hours spent doing bothdagain complicating the interpretation of a sum score.
Our findings rely on self-reported information with no medical confirmation. However, the questions used to evaluate NSP and symptoms of depression are widely used and have been validated. [3, 18–20] Previous research has found that adolescents’ self-report of health care received seems valid. [38] Although the use of self-reported information is a limitation of the study, the importance of self-reported information should not be undercut; for instance, self-reported health status has been found to strongly predict subsequent mortality. [39]
Clinical implications
In our study, adolescents reporting NSP used health services more frequently than others. This can enable identification, prevention, and treatment. Our results, in accordance with the literature, imply a broader perspective in adolescents with NSP, where information about mental health and life style factors should be part of the assessment. While preventive or treatment options should be based on the individual assessment, our results suggest that psychological interventions focusing on behavioral change, such as cognitive behavior therapy, may reduce pain and improve function in adolescents with NSP. [40]
REFERENCES:
Feldman DE, Shrier I, Rossignol M, Abenhaim L.
Risk factors for the development of neck and upper limb pain in adolescents.
Spine 2002;27: 523e8.Hogg-Johnson, S, van der Velde, G, Carroll, LJ et al.
The Burden and Determinants of Neck Pain in the General Population:
Results of the Bone and Joint Decade 2000–2010 Task Force on
Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976) 2008 (Feb 15); 33 (4 Suppl): S39–51Vikat A, Rimpelä M, Salminen JJ, et al.
Neck or Shoulder Pain and Low Back Pain in Finnish Adolescents
Scand J Public Health. 2000 (Sep); 28 (3): 164–173Hakala P, Rimpelä A, Salminen JJ, Virtanen SM, Rimpelä M.
Back, Neck, and Shoulder Pain in Finnish Adolescents:
National Cross Sectional Surveys
British Medical Journal 2002 (Oct 5); 325 (7367): 743–745Diepenmaat A, Van der Wal M, De Vet H, Hirasing R.
Neck/shoulder, low back, and arm pain in relation to computer use,
physical activity, stress, and depression among Dutch adolescents.
Pediatrics 2006;117:412e6.Niemi S, Levoska S, Kemilä J, et al.
Neck and shoulder symptoms and leisure time activities in high school students.
J Orthop Sports Phys Ther 1996;24: 25.Hakala PT, Rimpelä AH, Saarni LA, Salminen JJ.
Frequent computer-related activities increase the risk
of neckeshoulder and low back pain in adolescents.
Eur J Public Health 2006;16:536e41.Härmä A-M, Kaltiala-Heino R, Rimpelä M, Rantanen P.
Are adolescents with frequent pain symptoms more depressed?
Scand J Prim Health Care 2002; 20:92e6.Stahl M, Kautiainen H, El-Metwally A, Hakkinen A, Ylinen J, Salminen JJ, Mikkelsson M.
Non-specific Neck Pain in Schoolchildren: Prognosis and Risk Factors
for Occurrence and Persistence. A 4-year Follow-up Study
Pain. 2008 (Jul 15); 137 (2): 316–322Sjøgaard G, Lundberg U, Kadefors R.
The role of muscle activity and mental load in the development of pain
and degenerative processes at the muscle cell level during computer work.
Eur J Appl Physiol 2000;83: 99e105.Aarås A, Horgen G, Ro O.
Work with the visual display unit: Health consequences.
Int J Human-Computer Interaction 2000;12:107e34.Jensen C, Borg V, Finsen L, et al.
Job demands, muscle activity and musculoskeletal symptoms
in relation to work with the computer mouse.
Scand J Work Environ Health 1998:418e24.Siivola SM, Levoska S, Latvala K, et al.
Predictive factors for neck and shoulder pain:
A longitudinal study in young adults.
Spine 2004;29: 1662e9.Borghouts J, Koes BW, Vondeling H, Bouter LM.
Cost-of-illness of neck pain in The Netherlands in 1996.
Pain 1999;80:629.Borg K, Hensing G, Alexanderson K.
Predictive factors for disability pensiondan 11-year follow up of
young persons on sick leave due to neck, shoulder, or back diagnoses.
Scand J Public health 2001;29:104e12.Skogen JC, Bøe T, Knudsen AK, Hysing M.
Psychometric properties and concurrent validity of the CRAFFT among
Norwegian adolescents. Ung@hordaland, a population-based study.
Addict Behav 2013.Hysing M, Pallesen S, Stormark KM, et al.
Sleep patterns and insomnia among adolescents: A population-based study.
J Sleep Res 2013.Haugland S, Wold B.
Subjective health complaints in adolescenced reliability
and validity of survey methods.
J Adolesc 2001;24:611e24.Sharp C, Goodyer IM, Croudace TJ.
The short mood and feelings questionnaire (SMFQ):
A unidimensional item response theory and categorical
data factor analysis of self-report ratings from a
community sample of 7-through 11-year-old children.
J Abnorm Child Psychol 2006;34: 365e77.Lundervold AJ, Breivik K, Posserud M-B, et al.
Symptoms of depression as reported by Norwegian adolescents
on the short mood and feelings questionnaire.
Front Psychol 2013;4:613.Zwierzynska K, Wolke D, Lereya TS.
Peer victimization in childhood and internalizing problems
in adolescence: A prospective longitudinal study.
J Abnormal Child Psychol 2013;41:309e23.StataCorp.
Stata Statistical Software: Release 12.
College Station, TX: Stata Corporation LP; 2011.Haugland S, Wold B, Stevenson J, et al.
Subjective health complaints in adolescence
A cross-national comparison of prevalence and dimensionality.
Eur J Public Health 2001;11:4e10.Rollman GB, Lautenbacher S.
Sex differences in musculoskeletal pain.
Clin J Pain 2001;17:20.Tsang A, Von Korff M, Lee S, et al.
Common chronic pain conditions in developed and developing countries:
Gender and age differences and comorbidity with depression-anxiety disorders.
J Pain 2008;9:883.Barsky AJ, Peekna HM, Borus JF.
Somatic symptom reporting in women and men.
J Gen Intern Med 2001;16:266e75.Fillingim RB, King CD, Ribeiro-Dasilva MC, et al.
Sex, gender, and pain: A review of recent clinical and experimental findings.
J Pain 2009;10: 447e85.VonKorff M, Simon G.
The relationship between pain and depression.
Br J Psychiatry 1996;168:101e8.Romano JM, Turner JA.
Chronic pain and depression: Does the evidence support a relationship?
Psychol Bull 1985;97:18.Farmer ME, Locke B, Moscicki E, et al.
Physical activity and depressive symptoms:
The NHANES I epidemiologic follow-up study.
Am J Epidemiol 1988;128:1340e51.Dunn AL, Trivedi MH, O’Neal HA.
Physical activity dose response effects on outcomes
of depression and anxiety.
Med Sci Sports Exerc 2001.Iannotti RJ, Kogan MD, Janssen I, Boyce WF.
Patterns of adolescent physical activity, screen-based media use,
and positive and negative health indicators in the US and Canada.
J Adolesc Health 2009;44:493e9.Bélanger RE, Akre C, Berchtold A, Michaud P-A.
A U-shaped association between intensity of Internet use and adolescent health.
Pediatrics 2011; 127:e330e5.Desai RA, Krishnan-Sarin S, Cavallo D, Potenza MN.
Video-gaming among high school students:
Health correlates, gender differences, and problematic gaming.
Pediatrics 2010;126:e1414e24.Wolsko PM, Eisenberg DM, Davis RB, Kessler R, Phillips RS:
Patterns and Perceptions of Care for Treatment of Back
and Neck Pain: Results of a National Survey
Spine (Phila Pa 1976) 2003 (Feb 1); 28 (3): 292–297Perquin CW, Hunfeld JA, Hazebroek-Kampschreur AA, et al.
Insights in the use of health care services in chronic
benign pain in childhood and adolescence.
Pain 2001;94:205e13.Bot S, Van der Waal J, Terwee C, et al.
Incidence and prevalence of complaints of the neck and
upper extremity in general practice.
Ann Rheum Dis 2005;64:118e23.Klein J, Graff C, Santelli J, et al.
Developing quality measures for adolescent care:
Validity of adolescents’ self-reported receipt of preventive services.
Health Serv Res 1999;34(1 Pt 2):391.McGee DL, Liao Y, Cao G, Cooper RS.
Self-reported health status and mortality in a multiethnic US cohort.
Am J Epidemiol 1999;149:41e6.Eccleston C, Palermo TM, Williams A, et al.
Psychological therapies for the management of chronic
and recurrent pain in children and adolescents.
Cochrane Database Syst Rev 2009;2.
Return to PEDIATRICS
Return to NECK AND BACK PAIN
Return to CHRONIC NECK PAIN
Since 11-10-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |
