Evaluation and Treatment of Breastfeeding Difficulties
Associated with Cervicocranial Dysfunction:
A Chiropractic PerspectiveThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Clinical Chiropractic Pediatrics 2016 (Dec); 15 (3): 1301 ~ FULL TEXT
OPEN ACCESS Sharon Vallone, DC, FICCP
Private Practice,
KIDSPACE Adaptive Play and Wellness,
South Windsor, Connecticut, USA
Increasingly, parents are presenting to the chiropractic office with the chief complaint of breastfeeding dysfunction. Early and consistent breastfeeding support is paramount to the dyad’s ability to establish a functional breastfeeding relationship. It is critical that chiropractors treating this population recognize feeding dysfunction and understand the mechanics of breastfeeding, what might alter those mechanics, and the importance of the role of the International Board Certified Lactation Consultant (IBCLC) in supporting the restoration of functional breastfeeding after the chiropractic adjustments have reduced the NMSK dysfunction. This paper outlines some of the mechanical dysfunctions that might interfere with the normal transfer of milk for a neonate.
Key Words: Chiropractic, breastfeeding, breastfeeding difficulties, biomechanics, pediatric, neonate
From the Full-Text Article:
Introduction
Increasingly parents are presenting to the chiropractic office with the chief complaint of breastfeeding dysfunction. Through the efforts of organizations like La Leche League International [1, 2] and the International Association of Tongue Tie Professionals (IATP), [3] books [4, 5] and professional publications, [6–15] and a boom in activity on social media of both professionals and concerned parents, [16, 17] The International Board Certified Lactation Consultants (IBCLC) and other healthcare providers (such as midwives, nurses in the hospital, pediatric office and homecare settings, and pediatricians) who support the nursing dyad are becoming more familiar with and adept at recognizing neuromusculoskeletal (NMSK) dysfunction that might interfere with breastfeeding.
As has been previously described, [18] it is important that early and consistent breastfeeding support be implemented to assist the dyad’s ability to establish a functional breastfeeding relationship. Therefore, chiropractors working with this population should understand the mechanics of breastfeeding, what might alter those mechanics, and recognize the importance of the IBCLC in supporting the restoration of functional breastfeeding after the chiropractic adjustments have reduced the NMSK dysfunction. [6, 10] The purpose of this paper is to outline some of the mechanical dysfunctions that might interfere with the normal transfer of milk for a neonate.
The Craniocervical Junction
The anatomy of the craniocervical junction (C01) is an important consideration in the neonate who is not feeding functionally at the breast or on the bottle. The skull develops from viscerocranium and neurocranium, which develop into the facial bones and the portion of the skull that protects the brain. The neurocranium consists of the chondrocranium and dermatocranium which give rise to the skull base from endochondral ossification and the calvarial vault from membranous ossification respectively. The rapid growth of the neurocranium is stimulated by expansion of the size of the brain over the first 7 years of life with fontanels closing (at different times) over the first two years of life.
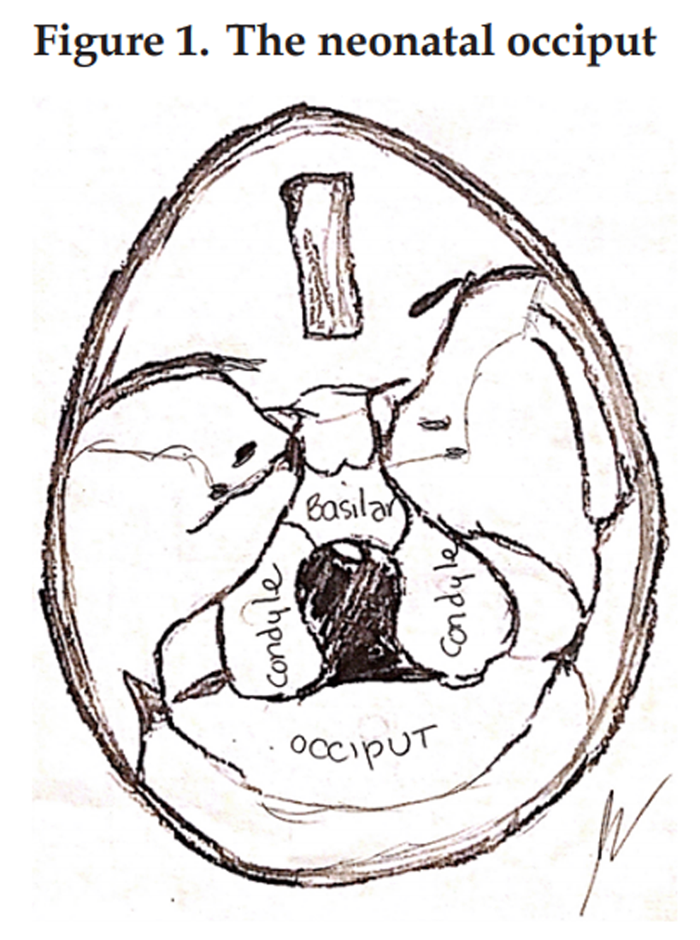
The occiput, not yet fused at birth, is in 4 segments [19, 20] which can be displaced (or misaligned) by the normal compression of the cranium during the birth process. They, like other plates of the cranium, may misalign or overlap and remain so, when subjected to inordinate or prolonged forces.
The lateral components of the occiput each possess a condyle that articulates with the first cervical vertebra (atlas or C1) at the superior articular surface of the lateral mass. The normal movements between the occiput and the atlas (C01) are: flexion and extension (nodding the chin to chest and back at the cranial base allowing an infant to lift their head when lying supine or tip their head back to adore their parent when resting on their shoulder, or the motion required to shake the head “yes”), rotation (shaking the head “no”) and lateral flexion (ear to shoulder) along with the possibility of an anterior, posterior or lateral translation of the full cranium on the atlas. Although subtle, identification of restricted movement in one of these planes helps determine the site of subluxation. Restricted movement can be due to inflammatory changes, misalignment of the articular structures, ligamentous injury, muscle spasm, tension in the fascial planes or asymmetry in development. It can also occur as a result of compensatory mechanisms put in place by the infant due to other physiologic, neurologic or structural obstructions to the normal mechanics of feeding. [21]Any misalignment of the condyles can interfere with function in a direct and obstructive way, functionally acting like a rubber wedge carefully placed under a door to prevent it from closing. Indirectly, if the misalignment results in nociceptive input (caused by a myriad of alterations ranging from fascial tension to an alteration in the patency of one of the foramen through which cranial nerves pass), it could also lead to a decrease or increase in muscle tone, the latter perceived as muscle tension or spasm. Change in muscle length or activity can adversely influence a functional joint. But when this involves muscles that have been demonstrated to bridge to the dura, via the fascia (like the rectus capitis posterior minor or the rectus capitis posterior major), nociception may be an even more critical factor in the ongoing dysfunction. Torsion or strain at the myodural bridge has been associated with cervicogenic headaches in adults and could potentially cause the same type of neurogenic pain for a neonate, as well as perpetuating the pain spasm cycle. [22, 23] If the condylar displacement affects foraminal patency for the cranial nerves, other systemic symptoms may ensue (for example, compression or traction of the fascial sleeve of the vagus nerve (CN X), can result in an alteration in vagal “tone” or autonomic dysregulation which could affect heart rate and blood pressure, respiratory rate, colic-like symptoms, swallowing – and the suck-swallow-breath synchrony – and cause an alteration in gut motility and excretion). [24]
If movement is altered at the level of the occiput and atlas, the brain will quickly initiate compensatory action of accessory muscles to attempt to accomplish important functions like breathing and eating. Breathing under stress or physical exertion will be quickly assisted by engaging the secondary muscles of respiration in the cervical spine. Feeding (particularly to secure the mouth around the nipple) will be supported by these same muscles as well as the submandibular muscles, the muscles of mastication and the muscles of the lips (primarily the orbicularis oris). The recruitment of these secondary muscles can result in functional “postural” changes (rounding of the shoulders, posterior translation of the cranium on the atlas, flexing the head on the chest, tilting of the head if unilaterally recruited, etc.).
Next let us consider how two examples how alteration in function of musculature can influence the mobility at C01.
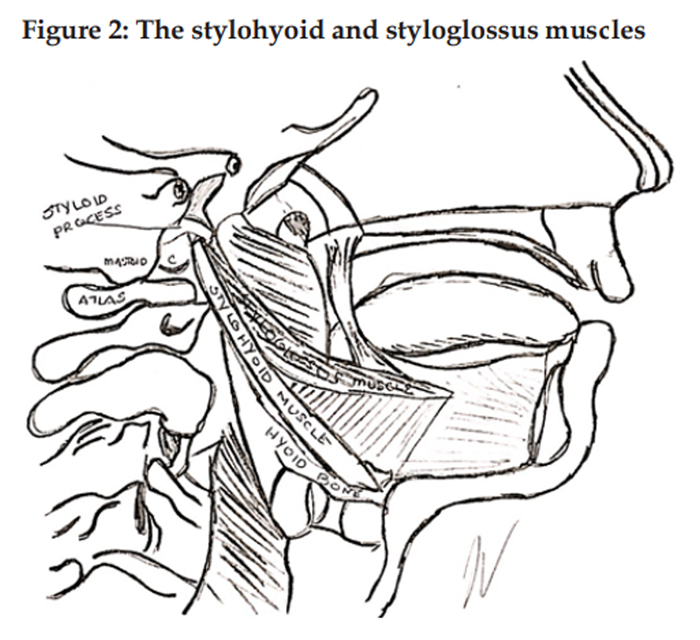
The styloglossus, the shortest and smallest of the three styloid muscles, arises from the anterior and lateral surfaces of the styloid process near its apex, and from the stylomandibular ligament. The styloglossus is innervated by the hypoglossal nerve (CN XII), it functions to draw up the sides of the tongue to create a trough for swallowing and retract the tongue. [19]
The stylohyoid muscle arises from the posterolateral surface of the styloid process of the temporal bone, near the base. It is a slender muscle, lying anterior and superior of the posterior belly of the digastric muscle and inserts onto the body of the hyoid bone at its junction with the greater cornu. A branch from the extracranial path of the facial nerve (CN VII) innervates the stylohyoid and the muscle functions to retract the hyoid and elevate the tongue. [19]If C01 is subluxated (fixed or immobile in any or all planes of motion), when either of these muscles contracts, the action of the muscle will be altered by the restricted mobility of its proximal attachment (the styloid process). This will result in increased movement of the distal attachment as demonstrated by retraction of the tongue or elevation and retraction of the hyoid bone. Likewise, if the tongue is tethered to the floor of the mouth or the movement of the hyoid is restricted by muscle activity or fascial tension, the proximal attachment (the styloid process) will be pulled towards the distal fixed attachment and affect the alignment of the cranium on C1 (permitted by the mobility allowed at C01 at the condyles).
Visible postural alterations and associated compensations due to dysfunction of the craniocervical junction can range from the subtle: slight head tilt, preferential rotation, chin to chest posture or the presence of a wry smile (as the mandible deviates) to more obvious distortion like torticollis or plagiocephaly as a result of repetitive or sustained asymmetric contraction over time. If unaddressed in infancy, postural changes can manifest in toddlerhood as toe walking, wide-based stance or gait, and increased AP curves of the spine as the continued compensatory recruitment disrupts the development of proprioceptive systems that determine position and balance for the toddler.
It is this author’s hypothesis that biomechanical restriction beginning with constraint or compensatory development of asymmetry in the womb could potentially be significant enough to negatively impact the normal egress of the fetus during labor resulting in potential compromised situations like an asynclitic presentation or shoulder dystocia because of the lack of full range of motion during the spiral decent. Other potentially far-reaching physiologic effects of altered biomechanics in infants and children can include failure to attain developmental milestones (due to decreased range of motion, for example), irritability, mouth-breathing, snoring, sleep apnea and disordered sleep, [25–27] feeding challenges at breast or by bottle [4, 6] and potential alterations in cranial nerve function which could result in dysregulation of respiratory, cardiac and or digestive function. [28]
Assessment of the cranial nerves is critical, as altered cranial nerve function may be the only indicator of articular dysfunction at C01. For example, vagal irritation (due to its proximity to the occipital condyle as it exits the skull through the jugular foramen) could potentially result in gastrointestinal distress or affect the function of cranial nerves V, VII, IX, X and XII and result in failure to root, suckle and swallow.
Manual Technique to Correct Dysfunctional Vertebral Segments
Chiropractic evaluation specifically identifies the areas of dysfunction and the chiropractic adjustment addresses it by restoring articular integrity, whether at the craniocervical junction or associated articulations. Both evaluative and adjusting techniques should be modified based on developmental anatomy, dictated by the neonate’s gestational age and concomitant conditions. Todd et al, published a review of the literature describing the level of force applied in a chiropractic adjustment or spinal manipulative therapy (SMT) for a pediatric patient based on age. A set of guidelines for different age groups has been developed by Marchand, “drawing on findings from an extensive study of tensile strength and osteoligamentous failure rates in pediatric spines as well as a report of transient bradycardia and apnea events that occurred with thrusts of 50 N to 70 N in infants younger than 3 months. Marchand has recommended that SMT be applied at a maximum cervical loading of 20 N for neonates.” [29–31]
A chiropractic evaluation should be multidimensional and should include a clear image in the chiropractor’s mind of the anatomy of the pediatric patient along with his or her active and passive assessment of range of motion and visual assessment of posture and attitude coupled with listening for altered or strained breath sounds, clicking of the tongue, swallowing or sucking in of air, the sound (and sometimes smell) of the burp, hiccup or flatulence (or stooling) are just a few of the sensory impressions that a chiropractor will integrate with the infant’s history to differentially diagnosis and plan a therapeutic approach.
Evaluation of the infant should begin with a soft tissue evaluation appreciating the connective tissue components that can interfere with joint mobility and function. Manual techniques employed are too varied to cover in this paper. Many current chiropractic techniques include soft tissue release to facilitate mobilization. Extensive study of fascia “based on functional relevance of myofascial chains” is recommended by Wilke,et al.(2016) in his systematic review. [32] An appreciation of the anterior and posterior superficial lines and anterior deep lines as outlined by Myers [33] and applied to the infant with breastfeeding dysfunction might prove to facilitate shorter, more effective courses of treatment.
Manual assessment of each of the individual cranial bones would be a part of the comprehensive assessment of the infant with breastfeeding difficulty. For the purposes of this paper, we will limit our discussion to the occipital bone, but a comprehensive assessment is holistic and will assist the practitioner in evaluating the intimate balance of mobile articulations and the soft tissue that both moves and supports them.
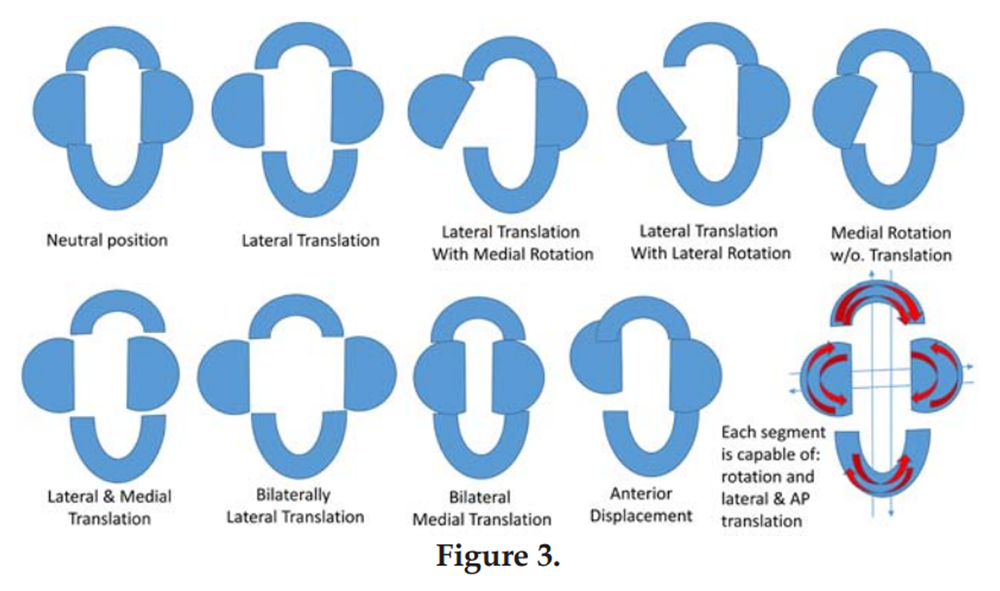
Palpation of the occiput will include the evaluation of all the aforementioned ranges of motion and the motion of the occiput as it articulates with the sphenoid at the sphenobasilar junction. This junction normally flexes and extends with respiration, but may be fixed in flexion, extension, lateral flexion or torsion. Palpation should also include evaluation of the individual segments of the occiput (anterior, posterior and lateral condylar segments) to assess medial and lateral translation or internal and external rotation, as well as anterior and posterior translations of the individual segments. (Figure 3).
Figure 3.
As stated earlier, all chiropractic techniques taught in the academic setting are modifiable for gestational age and anatomy. For example, methods of choice for this author are cranial adjusting (for example, as taught by DeJarnette [34, 35] and Upledger [36]), low velocity, low amplitude (low force) (manually (digitally) or with a pediatric drop head piece), percussive instrumentation (like the Activator Technique) [37] delivering a measurable, short range, reproducible force, or non-force techniques maintaining steady digital contact (“press and hold”) as a fulcrum about which a neonate moves until they release the restriction at their own pace. In the press and hold technique, the emphasis is on acting as a stationary fulcrum and letting the neonate “lead” the myofascial release which ultimately restores vertebral motion. This avoids force or excessive range-induced trauma and reduces the risk of tissue injury and activation of the sympathetic response which can lead to autonomic dysregulation if the trauma exceeds the neonate’s adaptive threshold. The author refers the reader to the Marchand article that reviews quite a number of chiropractic techniques and age-appropriate modifications beyond the scope of this commentary. [29]
Gently supporting the head with fingertip contact along the occiput using two fingers to assess the “spread” and position of the condyle or using all fingers to encourage anterior translation or extension at C01 will gently accomplish mobilization, often without distressing the neonate. At times, they will express intermittent distress as they “unwind” the fascia (connective tissue components that may have been injured during the birth process or from misuse) or if a trigger point in a suboccipital muscle is compressed. Patience and a consistently firm but gentle digital contact usually allows them to work through the discomfort until they are relaxed and at ease, often falling asleep as the parasympathetic system becomes more dominant than the sympathetic system that had been engaged when all systems were not functioning properly.
Developing a discerning touch involves understanding the neonatal anatomy. For example, that the occiput has four individual pieces with each segment’s position and mobility influenced by its own fascial envelope (or as mentioned earlier, from a distal restriction along one of the associated myofascial trains). The misalignment of one segment may subtly change or be completely released by effectively releasing the soft tissue or another subluxated segment. Consider releasing the taut fascial envelope and use good clinical judgment and develop precise manual skills before applying any direct force (no matter how modified) to a motion segment. In most cases, inducing nociceptive input is more likely to cause more restriction than less.
Highly developed observation and palpation skills; familiarity with anatomy and function; discernment; clinical experience; appreciation of the role of myofascial components in dysfunction; and a skilled, specific adjustment are the tools that will allow the chiropractor to facilitate normal motion and neurologic regulation for the neonate demonstrating breastfeeding difficulties, interference with the suck-swallow-breath synchrony or potentially other physiologic challenges.
Conclusion
Although only one articulation was specifically, and not necessarily exhaustively discussed in this paper, the implication that multiple articulations and myofascial components may be compromised is implicit in this discussion. Therefore, it is important that the neonate experiencing any feeding (or breathing) challenges should also be evaluated for NMSK dysfunction and be sent for evaluation by a qualified International Board Certified Lactation Consultant (IBCLC).
REFERENCES:
Brussel C.
Considering CranioSacral Therapy in Difficult Situations
LEAVEN August-September 2001; 37(4):82-83; accessed October 3, 2016.Vallone S.
Chiropractic Care for the Breastfeeding Dyad
LEAVEN December 2003-January 2004; 9(6): 126-27International Association of Tongue Tie Professionals.
Accessed on August 21, 2016 at:
http://tonguetieprofessionals.org/ Also at:
https://www.facebook.com/IATP-International-Affiliation-of-Tongue-tieProfessionals-
154327071396819/Watson Genna C.
Supporting sucking skills in breastfeeding infants. Third Edition. 2017,
Jones and Bartlett Learning, Burlington, MA.Kotlow, L.
SOS 4 TOTS, 2016,
The Troy Bookmakers, Troy, NY.Vallone SA, Carnegie-Hargreaves F.
The Infant with Dysfunctional Feeding Patterns –
The Chiropractic Assessment
J Clinical Chiropractic Pediatrics 2016 (May); 15 (2): 1230Hewitt, E.
Chiropractic care for infants with dysfunctional nursing: a case series.
Journal of Clinical Chiropractic Pediatrics 1999; 4(1):241-244.Holtrop DP.
Resolution of Suckling Intolerance in a 6-month-old Chiropractic Patient
J Manipulative Physiol Ther 2000 (Nov); 23 (9): 615–618Vallone S.
Chiropractic Evaluation and Treatment of Musculoskeletal Dysfunction
in Infants Demonstrating Difficulty Breastfeeding
J Clinical Chiropractic Pediatrics 2004 (Dec); 6 (1): 349–366Tow J and Vallone SA.
Development of and Integrative Relationship in the Care of the Breastfeeding Newborn: Lactation Consultant and Chiropractor.
Journal of Clinical Chiropractic Pediatrics 2009 June; 10(1).626-632.Miller, J. E., Miller, L., Sulesund, A. K., & Yevtushenko, A.
Contribution of Chiropractic Therapy to Resolving Suboptimal Breastfeeding:
A Case Series of 114 Infants
J Manipulative Physiol Ther 2009 (Oct); 32 (8): 670–674Holleman, A. C., Nee, J., & Knaap, S. F.
Chiropractic Management of Breast-feeding Difficulties: A Case Report
Journal of Chiropractic Medicine 2011 (Sep); 10 (3): 199–203Holleman AC. Nee J. Knaap S.
Chiropractic management of breastfeeding difficulties: A case report.
Journal of Chiropractic Medicine. 2011; 10(3):199-203.Fry LM.
Chiropractic and Breastfeeding Dysfunction: A Literature Review
Journal of Clinical Chiropractic Pediatrics 2014 (Mar); 14 (2): 1151-1155Drobbin D. Stallman J.
Resolution of Breastfeeding and Latching Difficulty Following Subluxation Based Chiropractic Care: Case Report and Review of the Literature.
Journal of Pediatric, Maternal & Family Health. July 2015; 3:102-108.Kotlow L,
Accessed on August 21, 2016 at:
www.kiddsteeth.comConnecticut Tongue-tie (& tethered oral tissue) Resource and Support Group:
Accessed on August 21, 2016 at:
https://www.facebook.com/groups/ConnecticutTetheredTissueRelease/Chiurco A. Montico M. Brovedani P. Monasta L.
An IBCLC in the Maternity Ward of a Mother and Child Hospital: A Pre- and Post-Intervention Study. International
Journal of Environmental Research and Public Health. Aug 2015; 12(8):9938–9951.Standring S.
Gray’s Anatomy, The Anatomical Basis of Clinical Practice, 41st Edition, 2015,
Elsevier Health Sciences, Amsterdam, UK, US, Mexico, Brazil, Spain, Germany.Crelin E.
Functional Anatomy of the Newborn, 1973,
Yale University Press, New Haven, CT, USA and London, England, UK.Elad D, Kozlovsky P, Blum O, Laine AF, Po MJ, Botzer E, Dollberg S, Zelicovich M, Ben Sira L.
Biomechanics of milk extraction during breastfeeding.
Proceedings of the National Academy of Science USA. 2014 Apr 8;111(14):5230-5.Hack GD, Korizer RT, Robinson WL, et al.
Anatomic relation between the rectus capitis posterior minor muscle and the dura matter.
Spine. 1995; 20:2484-2486.Scali R, Pontell ME, Enix DE, Marchall E.
Histologic analysis of the rectus capititis posterior major’s myodural bridge.
The Spine Journal. May 2013; 13(5):558-563.Berthoud, H. R.; Neuhuber, W. L.
Functional and chemical anatomy of the afferent vagal system.
Autonomic Neuroscience. 2000; 85 (1–3): 1–17.Palmer B.
Breastfeeding: Reducing the Risk for Obstructive Sleep Apnea.
Breastfeeding Abstracts (LLLI), February 1999; 18(3):19-20.
Accessed on 10/3/2016 at:
http://www.llli.org/ba/feb99.html .Levrini L et al.
Model of oronasal rehabilitation in children with obstructive sleep apnea syndrome undergoing rapid maxillary expansion: Research review.
J Sl Sci 2014; (7)225-233.Ruoff C and Guilleminault C.
Orthodontics and sleep-disordered breathing. Editorial.
Sleep Breath, 2012 16 (2). 271-273.Schmidt A. Thews G
“Autonomic Nervous System”
in Janig W. Human Physiology, 2nd ed, 1989,
Springer-Verlag, New York, USA.Todd AJ, Carroll MT, Mitchell EK.
Forces of Commonly Used Chiropractic Techniques for Children:
A Review of the Literature
J Manipulative Physiol Ther. 2016 (Jul); 39 (6): 401–410Marchand AM.
A Proposed Model With Possible Implications for Safety and Technique Adaptations
for Chiropractic Spinal Manipulative Therapy for Infants and Children
J Manipulative Physiol Ther 2015 (Nov); 38 (9): 713–726Koch LE. Koch H. Graumann-Brunt S. Stolle D. Ramirez JM. Saternus KS.
Heart rate changes in response to mild mechanical irritation of the high cervical spinal region in infants.
Forensic Science International 2002;128(3):168-176.Wilke J. Krause F. Vogt L. Banzer W.
What is evidence-based about myofascial chains: a systematic Review.
Archives of Physical Medicine and Rehabilitation 2016; 97:454-461.Myers TW.
Anatomy Trains: myofascial meridians for manual and movement therapists, 3rd edition, 2014,
Elsevier Health Sciences, Amsterdam, UK, US, Mexico, Brazil, Spain, Germany.SORSI International.
Accessed on 10/3/2016 at:
www.sorsi.comSOTO U.S.A.
Accessed on 10/3/2016 at:
www.sotousa.comThe Upledge Institute.
Accessed on 10/3/2016 at:
http://upledger.comThe Activator Method.
Acessed on 10/3/2016 at:
https://www.activator.com/research/
Return to PEDIATRICS
Since 11–17–2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |