Taking a Wrist Series:
It's About the CarpalsThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Dynamic Chiropractic ~ January 15, 2012
By Deborah Pate, DC, DACBR
Routine radiographic examination of the wrist is not difficult, but does require some attention to positioning. Keep in mind that to evaluate a joint on X-ray, one must be able to visualize the joint in two planes at 90 degrees to one other. The routine series for a wrist includes PA and lateral views. For further evaluation, oblique projection may also be necessary if trauma or arthritis is evident.
The PA View
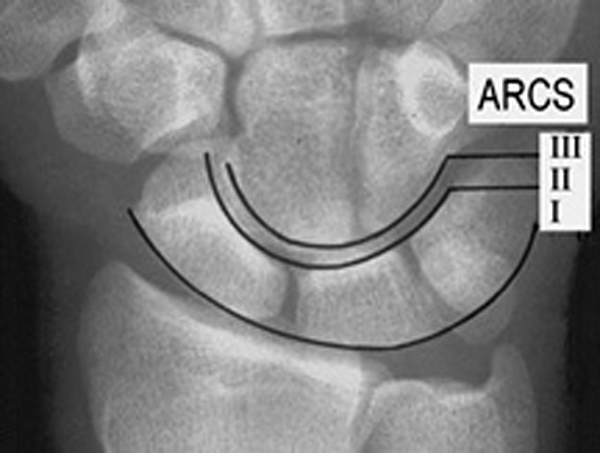
The PA radiograph of the wrist is best obtained with the arm abducted 90 degrees from the trunk and the forearm flexed 90 degrees at the elbow. The wrist should lie flat on the cassette with the hand in a relaxed position, but with the fingers slightly cupped or flexed, or curled in a relaxed fist. A wedge also can be placed underneath the fingers to keep the wrist in contact with the cassette. The thumb should be extended parallel to the other fingers. (Figure 1: PA Wrist)
The most common problem I've seen is that the PA projection is performed with the hand extended flat on the cassette, which elevates the wrist slightly, causing the carpals to appear jammed together. If the clinician instructs the patient to place their hand in a gentle fist position, this will help place the carpal bones of the wrist closer to the cassette. (Figure 2: PA wrist with hand in gentle fist)

Technical factors that are important to keep in mind include the following: 10 x 12 inch (24 x 30 cm) crosswise for two or more images on one cassette; for a digital screen, use lead masking to get more than one image one the cassette; for a detail screen, use the tabletop technique; 50-60 kVp range, mAs 4-5; and minimum SID of 100 cm.
The Lateral View
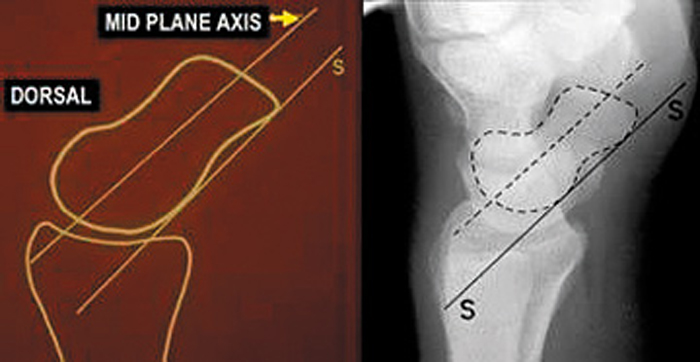
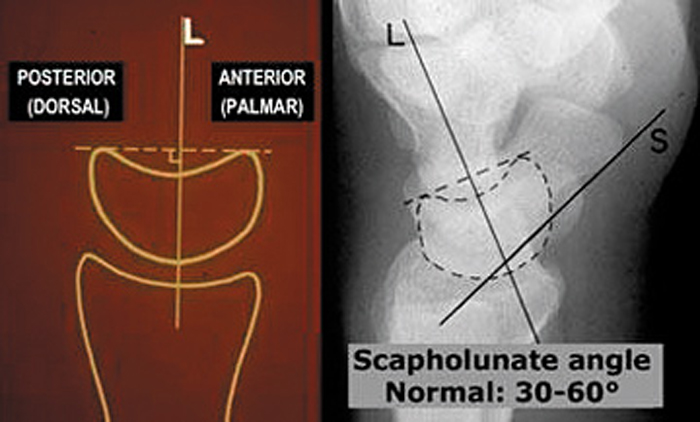
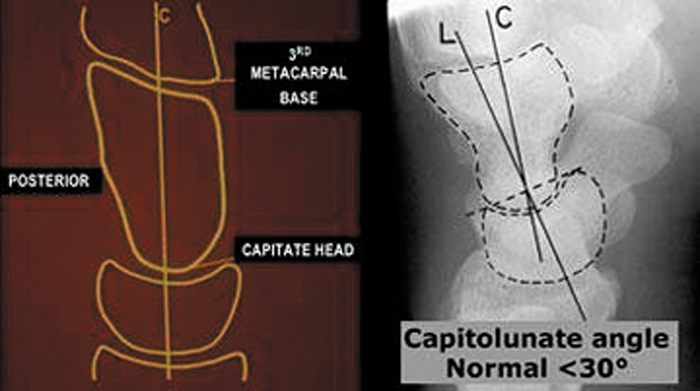
The lateral radiograph of the wrist is obtained with the arm adducted with the ulnar side of the forearm on the cassette. The elbow is flexed to 90 degrees, adjusting the hand and wrist to make certain they are in a true lateral position. The same technical factors can be used for the lateral projection as for the PA projection. (Figure 6: Lateral wrist positioning) If an X-ray table is not available, any sturdy table will do. This is a non-bucky technique.
On a standard lateral view, the palmar cortex of the pisiform bone should overlie the central third of the interval between the palmar cortices of the distal scaphoid pole and the capitate head. (Figure 8)
The Oblique View
The other common view performed in a wrist series is the oblique view, which allows for visualization of the trapezio-trapezoidal joint. Again, this is a tabletop film. The patient is seated with the elbow flexed 90 degrees and the hand/wrist supinated. The fingers and hand should be slightly flexed to align the carpal bones. Rotate the wrist and hand internally 45 degrees toward the cassette; a 45 degree angle sponge can be used for support and stability. (Figure 12)
Deborah Pate is a licensed chiropractor and a diplomate of the American Chiropractic Board of Radiology. A 1982 graduate of National College of Chiropractic, she was the first chiropractor accepted into a fellowship in osteoradiology at the medical center of the University of California, at San Diego. Dr. Pate served as a research associate in the radiology department at the VA hospital from 1984 to 1986, and as chiropractic director of the American Chiropractic Network (now American Specialty Health Plans), both in San Diego, California, for several years. Still a consultant for several insurance companies, she has practiced as a clinician and radiology consultant since 1984, and maintains a radiology consulting practice. Dr. Pate is also a state-appointed qualified medical examiner and a certified disability evaluator. She has taught postgraduate courses at Parker College of Chiropractic, Los Angeles College of Chiropractic, the University of California at San Diego, and other respected institutions.
Return to RADIOLOGY
Since 5-02-2012


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |