Nonspecific Low Back Pain: Inflammatory Profiles
of Patients With Acute and Chronic PainThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Clinical J Pain 2019 (Oct); 35 (10): 818-825 ~ FULL TEXT
OPEN ACCESS Julita A. Teodorczyk-Injeyan, PhD, John J. Triano, DC, PhD, and H. Stephen Injeyan, DC, PhD
Research and Clinical Education Programs,
Canadian Memorial Chiropractic College,
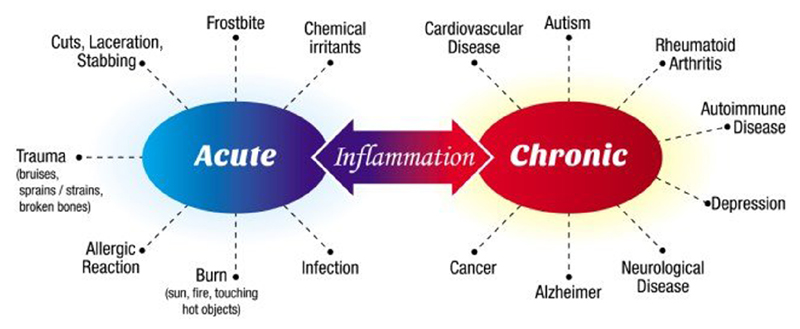
Toronto, ON, Canada.BACKGROUND: The pathogenesis of low back pain (LBP) remains unclear. However, recent studies suggest that the inflammatory response may be inherent in spinal pain. The purpose of this study was to discern inflammatory profiles in patients with nonspecific acute and chronic LBP in relation to those in asymptomatic individuals.
MATERIALS AND METHODS: Peripheral blood samples were obtained from asymptomatic controls and patients with nonspecific acute and chronic LBP reporting a minimum pain score of 3 on a 10-point Visual Analogue Scale (VAS). The levels of in vitro production of proinflammatory (tumor necrosis factor α [TNFα], interleukin [IL] 1β, IL-6, IL-2, interferon γ) and anti-inflammatory (IL-1 receptor antagonist, soluble receptors of TNF2, and IL-10) mediators were determined by specific immunoassays.
RESULTS: The mean VAS scores were comparable between the acute and chronic LBP patient groups. Compared with asymptomatic group, the production of TNFα, IL-1β, IL-6 and their ratios to IL-10 levels were significantly elevated in both patient groups (P=0.0001 to 0.003). In acute LBP group, the ratio of IL-2:IL-10 was also significantly increased (P=0.02). In contrast, the production of interferon γ was significantly reduced compared with the other study groups (P=0.005 to 0.01), nevertheless, it was positively correlated (P=0.006) with pain scores. In chronic LBP patients, the production of TNFα, IL-1 receptor antagonist, and soluble receptors of TNF2 was significantly increased (P=0.001 to 0.03) in comparison with the control and acute LBP groups, and TNFα and IL-1β levels were positively correlated (P<0.001) with VAS scores.
CONCLUSIONS: The inflammatory profiles of patients with acute and chronic LBP are distinct. Nonetheless, in both patient groups, an imbalance between proinflammatory and anti-inflammatory mediator levels favors the production of proinflammatory components.
Key Words: low back pain, inflammation, cytokines, inflammatory mediators
CLINICAL TRIAL REGISTRY Clinical Trials.gov (NCT01766141).
From the FULL TEXT Article:
Background
Although nonspecific low back pain (LBP) is very common, [1] treatment outcomes remain questionable both for acute [2] and chronic LBP. [3] The pathophysiology of LBP remains poorly understood, and its diagnosis is based on excluding other spinal pain disorders for which there are clear diagnostic criteria. [1]
Several studies have reported on the possible involvement of inflammatory cytokines in heterogenous cohorts of LBP patients. Systemic levels of inflammatory markers including interleukin (IL) 6, tumor necrosis factor α (TNFα) or C-reactive protein (CRP) were found to be elevated in diverse groups of LBP patients. [4–6] Li et al [7] described elevated IL-6, and reduced IL-10 levels in peripheral blood of chronic LBP patients, thereby suggesting that an imbalance between proinflammatory and anti-inflammatory mediators contributes to the pathophysiology of LBP. Increased plasma levels of IL-6 in chronic LBP have been reported to correlate with pain intensity levels. [8] Also, the production of nociceptive chemokines CCL2, CCL3, and CCL4, as well as the inflammatory marker, soluble E-selectin, have been shown to be significantly augmented in patients with nonspecific acute and chronic LBP. [9]
The interactions of proinflammatory and anti-inflammatory molecules within the local inflammatory milieu are complex. It is expected that the nature of LBP-related inflammatory changes and thereby response to applied therapies may vary in patients due to different factors including the intensity and duration of pain and chronicity of the condition.
Investigations into pain mechanisms in spinal pain patients with herniated disks and those with diskogenic pain have suggested an imbalance of catabolic and anabolic processes leading to increased expression of inflammatory mediators. [10, 11] An imbalance in inflammatory cytokine network has been suggested for degenerative joint disease generally [12] and a shift towards “pain susceptible” (inflammatory) cytokine profile has been also reported in patients with painful neuropathies. [13]
Physiologically, anti-inflammatory cytokines such as IL-10 inhibit the production of proinflammatory cytokines by activated macrophages and enhance the production of natural inhibitors of their biologic activity including interleukin-1 receptor antagonist (IL-1RA) and soluble receptors of tumor necrosis factor (sTNFRs). [14] To our knowledge, no studies have explored the possible interplay between proinflammatory and anti-inflammatory mediators in the pathophysiology of nonspecific LBP. As part of an ongoing study of the role of inflammatory response in nonspecific LBP, we examined the production of mediators with the functional ability to promote the inflammatory response (TNFα, IL-1β, IL-6, IL-2, and interferon γ [IFNγ]) or deliver an anti-inflammatory effect (IL-1RA, IL-10, sTNFR2, and soluble IL-6 receptor [sIL-6R]) in acute and chronic LBP patient groups. Data on pain intensity and functional ability of patients were collected at presentation to assess any possible relationships with inflammatory cytokine levels.
MATERIALS AND METHODS
Patient recruitment and most laboratory methods have been described previously [9] and are briefly outlined below for convenience. This study was approved by the institutional Research Ethics Board of the Canadian Memorial Chiropractic College (CMCC) and was registered with Clinical Trials.gov (NCT01766141).
Patients

Figure 1 A total of 56 female and male patients between the ages 22 and 60, presenting with nonspecific LBP1 localized to the lumbosacral area, involving the L1-L5 spine and/or the sacroiliac joints, were enrolled into the study through the CMCC outpatient clinics (Figure 1).
Patient selection criteria were based on the accepted definition of acute (<4 wk) versus chronic (>12 wk) LBP. [15] For the purposes of this study, acute LBP patients were recruited if it was the first occurrence or that they were pain-free for a minimum of 1 year. Chronicity was defined by LBP exceeding 3 months and characterized by persistent albeit fluctuating pain over a period of months or years.
Exclusion criteria at intake were as follows: reporting a pain level <3 on a 10-point Visual Analogue Scale (VAS), receiving any form of physical treatment in the preceding 15 days, having taken anti-inflammatory medications in the preceding 48 hours, having any type of unresolved known inflammatory conditions (including systemic or musculoskeletal conditions such as radiculopathies, sprain or strain injuries, other than the presenting LBP), autoimmune conditions, coagulopathies, infections and neoplastic diseases, being pregnant, unwilling to sign the study consent form, or unwilling/unable to adhere to study protocol. The absence of other possible comorbid conditions including psychiatric and immune system disorders were deduced from the history of medication usage obtained from each patient. The lack of recent medication usage, other than Acetaminophen, further confirmed the absence of comorbid conditions in the cohorts recruited into the study. Eligible LBP patients completed clinic intake forms including a pain diagram indicating location and type of pain, an Oswestry Disability Index (ODI), [16] and a 10-point VAS pain score, as described previously.
Asymptomatic Controls
A cohort of age-matched and sex-matched asymptomatic participants, who had not experienced LBP previously or had been free of LBP for a minimum of 1 year, was recruited from the general population to serve as the control group (Fig. 1).
Laboratory StudiesBlood Samples Following the initial screening and obtaining written consent, heparinized samples of peripheral blood (7 mL each) were obtained by venipuncture from the antecubital fossa area of the arm. All samples were obtained between the hours of 10:00 am and 2:00 pm and were transferred to the laboratory and processed within 60 minutes of blood withdrawal.
Culture System Whole blood (WB) culture system was utilized. This has been shown to be a valid, fully reproducible over long-time periods and a low-cost method to evaluate the production of inducible cytokines. [17] Duplicate WB cultures were prepared essentially as described by Yaqoob et al. [18] Briefly, blood samples were diluted 10-fold with RPMI 1640 (Gibco, Invitrogen, Grand Island, NY) supplemented with 5×10–5 mol/L of 2-mercaptoethanol and commercial solution of l-glutamine-penicillin-streptomycin (Gibco, Life Technologies, Burlington, ON, Canada). The production of the studied mediators was investigated in inducer–activated cultures cultivated under optimal stimulation condition and harvested at optimal poststimulation time. [19] To induce the production of TNFα, IL-1β, IL-6, and IL-1RA WB cultures were cultivated for 24 hours at 37°C, in a humidified 5% CO2 incubator, in the presence of lipopolysaccharide (LPS) from Escherichia coli serotype 055:B5 (LPS; Sigma-Aldrich, St. Louis, MO) at a concentration of 1 µg/mL. To assess the levels of IL-2 and IFNγ production, parallel WB preparations were cultured for 48 hours in the presence of 10 µg/mL of phytohemagglutinin (Sigma-Aldrich). Finally, the combination of LPS and phytohemagglutinin at the above concentrations was used for 48 hours of stimulation to induce the release of the sTNFR2 and the production of IL-10. At the conclusion of the respective incubation periods, supernatants from duplicate WB cultures were pooled, centrifuged to remove any contaminating cellular material, aliquoted and frozen at –80°C until further analysis.
Plasma Samples Aliquots of blood samples for determination of plasma levels of sIL-6R were obtained before WB cultures preparation. Cells were removed from the plasma by centrifugation for 15 minutes at 2000g at 4°C.Determination of Mediator Levels
Specific enzyme-linked immunosorbent assays (DuoSet ELISA development system) for natural and recombinant human cytokines and for natural sTNFR2 (R&D Systems, Minneapolis, MN) were used to quantify the levels of studied mediators in culture supernatants. The plasma levels of sIL-6R were determined by specific Quantikine ELISA kit (R&D Systems). All quantitative determinations were performed according to the manufacturer’s recommendations. Each of the studied samples was tested a minimum of 3 times at 2 to 4 different dilutions.
Concentrations of the tested mediators were determined using Gen5 Data Analysis Software (Bio-Tech). Detection limits for TNFα, IL-2, and IFNγ was 15.6 pg/mL; and for IL-1β, IL-6, sTNFR2, IL-10, IL-1RA, and sIL-6R detection limits were 3.9, 9.4, 12.5, 32, 39, and 31.2 pg/mL, respectively.
Determination of Proinflammatory to Anti-inflammatory Cytokine Ratios

Figure 2 The ratios of the key proinflammatory cytokine concentrations to anti-inflammatory IL-10 concentrations were calculated to assess changes in the balance between proinflammatory and anti-inflammatory mediators in the 3 study groups. These were calculated for each study participant by dividing the concentration of a given proinflammatory cytokine, that is, TNFα, IL-1β, IL-6, and IL-2 by that of IL-10 determined in a corresponding culture from the same individual. Figure 2 presents the means of ratios determined for each study group.
Sample Size
From Cohen table [20] based on a power of 0.8 and a 2-tailed test with a P-value <0.05, the sample size was estimated to be no <17 per group. As shown in Figure 1, the number of participants in each of the study groups was higher.
Data Analysis

Table 2 Statistical analyses of data were carried out using PAST 3.18 beta software. [21] All data were tested for normality using the Shapiro-Wilk test. Where non-normal distributions were found, data were transformed (Box-Cox). The primary outcomes for this study were established as differences in the production of mediators between the study groups, that is, between asymptomatic controls and acute and chronic LBP patients; and between acute and chronic LBP patient groups. Testing for differences between the study groups was performed using independent samples t test. The nonparametric Kruskal-Wallis or Mann-Whitney U tests were also used for data without normal distribution to confirm results. Unless otherwise indicated, the results depicted in Table 2 and in the text are presented as mean±SEM. P-values ≤0.05 were accepted as being significant.
Spearman correlation coefficients and their statistical significance were also determined to assess the relationship between self-reported pain and functional disability scores and levels of inflammatory mediator production in patients with acute and chronic LBP.
RESULTS

Table 1 The study was completed by 22 acute, 25 chronic LBP patients and 24 asymptomatic control participants (Fig. 1). Demographic data (Table 1) indicates the study groups were comparable. Mean VAS scores were comparable between acute (6.1±1.6) and chronic (5.2±1.8) LBP groups. Mean ODI scores were higher, although not significantly, in the acute LBP group (37.0±13.7) compared with those in chronic LBP patients (28.1±8.6). Mean Body Mass Index (BMI) values did not differ between the 3 study groups. Consistent with the study exclusion criteria none of the patients described their pain as being indicative of radiculopathy. The predominant symptom was described as being “dull and achy” or “stiff and tight” (Table 1).
Table 2 depicts the means of the production of 8 inflammatory mediators in inducer-stimulated cultures from controls and LBP patients. Figure 2 presents the ratios of proinflammatory cytokines (TNFα, IL-1 β, IL-6) to anti-inflammatory IL-10 production assessed in corresponding culture supernatants. Given the limited biological material available for culture, assessment of the constitutive (spontaneous) secretion of cytokines was examined only in preliminary experiments. Under the experimental conditions utilized in the present study (10% WB cultures) and in concordance with our earlier observations, [22] constitutive in vitro production of inflammatory mediators in patients with spinal pain is observed only occasionally and their levels do not differ significantly from those in asymptomatic individuals.
Proinflammatory Mediator Production (TNFα, IL-1β, IL-6, IFNγ, IL-2)
Compared with asymptomatic controls, baseline levels of TNFα, IL-1β, IL-6 were all significantly (P=0.0001 to 0.003) increased in both groups of LBP patients (Table 2). In contrast, the production of TNFα alone, but not that of IL-1β and IL-6 was also significantly higher (P=0.003) in patients with chronic versus acute LBP (Table 2).

Table 3 The mean levels of IL-2 production in the control group and in chronic LBP patients were comparable. However, in patients with acute LBP, the mean IL-2 production was noticeably augmented (by over 30%) although it did not reach the level of significance. This was contrasted by a significant decrease in the production of IFNγ in this study group, compared with both the control (P=0.01) and chronic (P=0.005) LBP cohorts (Table 2). Furthermore, in patients with acute LBP, a positive correlation was apparent between the production of IFNγ and VAS scores. In patients with chronic LBP the levels of TNFα and IL-1β production were positively correlated (P<0.001) with self-assessed pain scores. In both patient groups, levels of other inflammatory mediators correlated only weakly with pain scores (Table 3). In both patient groups, only IL-6 levels correlated significantly (P<0.001) with ODI scores.
Anti-inflammatory Mediator (IL-1RA, sTNFR2, IL-10, and sIL-6R) Production
When compared with both the asymptomatic control and patients with acute LBP, the production of IL-1RA was significantly increased in patients with chronic LBP (P=0.006 and 0.03, respectively). Similarly, in this patient group, the production of sTNFR2 was significantly increased in comparison with asymptomatic controls (P=0.0001) and patients with acute LBP (P=0.001) (Table 2). In contrast, the production of IL-10 in both acute and chronic LBP patients was significantly reduced when compared with the controls (P=0.008 and 0.03, respectively).
Plasma levels of sIL-6R were tested to assess the potential impact of changes in its release on the level of bioavailable (unbound) IL-6 production in WB cultures. The concentration of sIL-6R ranged from 27 to 51 ng/mL in asymptomatic grpup and from 30 to 68 ng/mL in both LBP patient groups. The mean levels of sIL-6R were comparable in all study groups.
Ratios of Proinflammatory Cytokines (TNFα, IL-1β, IL-6, IL-2) to Anti-inflammatory IL-10
Figure 2 presents the means of the ratios of TNFα, IL-1β, and IL-6 concentrations to those of IL-10 determined in corresponding control and patient cultures. Compared with asymptomatic controls, these ratios were significantly increased (P=0.0001) in both LBP patient groups. However, the ratio of IL-2:IL-10 production levels was significantly higher than that in the control only in the acute LBP patient group (Fig. 2).
DISCUSSION
To our knowledge, this report is first to characterize and compare inflammatory profiles of patients reporting acute and chronic LBP. Differences were found in the capacity for the inducible production of inflammatory mediators between all nonspecific LBP patients and asymptomatic controls, as well as between acute and chronic LBP patient groups (Table 2). In both LBP patient groups, the production of proinflammatory cytokines, TNFα, IL-1β, and IL-6 was significantly elevated and that of the anti-inflammatory cytokine, IL-10, significantly reduced when compared with the asymptomatic control cohort. Consequently, the ratios of monocytic cytokines, proinflammatory TNFα, IL-1β, and IL-6 to anti-inflammatory IL-10 were significantly increased in both patient groups (Fig. 2).
The principal differences between the acute and chronic LBP cohorts included the following:(1) the production of TNFα and 2 anti-inflammatory mediators, IL-1RA and sTNFR2 was significantly augmented in the chronic LBP group relative to acute LBP (Table 2);
(2) in the acute LBP cohort, the production of the CD4 Th1-lymphocytes–derived inflammatory cytokines, IL-2 and IFNγ, were altered relative to chronic LBP group. The production of IL-2 increased markedly (by over 30%), resulting in a significant increase in the ratio of IL-2:IL-10. In contrast, the production of IFNγ was significantly reduced (Table 2, Fig. 2);
(3) positive correlation between self-assessed pain level (VAS) and IFNγ levels was found in patients with acute LBP, whereas TNFα and IL-1 production levels correlated positively with VAS sores in patients with chronic LBP (Table 3).The system of WB cultures used in the present study allowed us to assess the state of immunocompetence and activation of the inflammatory activated human peripheral blood T cells and monocytes with distinctive proteome profiles. [23] Nociceptive chemokines, G-protein-linked chemokine receptors and inflammatory cytokines such as TNFα are generated at the site of local inflammation and regulate leukocyte trafficking, migration, and adhesiveness to the inflamed tissues. [24] In contrast, these processes are also involved in maintaining inflammatory cells within the circulation. [25] The quantitative differences in response to an exogenous inflammatory inducer (LPS) observed in the present investigation may suggest that the state of activation of innate immunity cells was enhanced particularly in patients with chronic LBP as suggested by the magnitude of TNFα and IL-1RA production in this study group (Table 2). The primary cellular source of these cytokines is proinflammatory, nonclassical CD14+CD16+ monocytes. [26, 27]
Typically, binding of a ligand (LPS) to Toll-like receptors (TLRs) on their surface prompts the transcription of TNFα to synergize with the available IFNγ and to trigger the production of proinflammatory cytokines. [28, 29] Strong upregulation of inflammatory mediator production in patients with chronic LBP might have been associated with a similar way of activation. The production of IFNγ in the chronic LBP group was elevated by close to 25% compared with asymptomatic patients. Furthermore, it was significantly higher than that in the acute pain group (Table 2). Highly elevated production of TNFα and IL-1RA in this patient group could also result from enhanced signaling by the inducer (LPS). In chronic pain patients, the in vitro responsiveness of TLRs to agonists including TLR4-binding LPS has been reported to be increased. [30] Altered responsiveness to LPS stimulation has also been reported in obese patients. [31] This is not likely the case in the current study as BMI values were comparable in all study groups (Table 1).
It has been shown that under inflammatory conditions monocytes/macrophages produce IL-1β and IL-1RA concomitantly. [32] It is therefore of interest that in our study the production of IL-1RA was significantly augmented only in chronic LBP patients, whereas both patient groups produced comparable amounts of IL-1β (Table 2). This apparent discrepancy may be explained by reports that opposite regulation of IL-1/IL-1RA production controlled by PI-3 kinases occurs following contact-mediated activation of monocytes by activated T cells. [33] This induces expression of the stable IL-1RA transcripts correlating with its highly elevated production in chronic inflammatory diseases. [34, 35] Thus, in the context of LBP, it is possible that chronicity may enhance monocyte-T cell contact at the inflammatory site(s) and favor IL-1RA synthesis over that of IL-1β as a protective mechanism to abrogate the inflammatory response.
Significantly elevated release of sTNFR2 in chronic LBP patients (Table 2) may play a similarly protective role against the pathologic activity of its ligand. Nanomolar concentrations of sTNFR2 have been shown to significantly attenuate inflammatory events in human intervertebral disk cells. [36] Proteolytic shedding of sTNFR2 is accelerated following monocyte activation and release of TNFα. [37] It is therefore feasible that compared with the asymptomatic control and acute LBP cohorts, elevated secretion of sTNFR2 in chronic LBP patients is associated with upregulated TNFα secretion. It is of interest that alongside augmented sTNFR2 secretion, the production of IL-10 was significantly reduced in both LBP patient groups. Elevated sTNFR levels have been found to parallel suppressed IL-10 production in cerebrospinal fluid of chronic pain patients. [38] Levels of IL-10 plasma concentrations were also reported to be reduced in patients with chronic LBP [7] and chronic widespread pain. [39]
The production of CD4+Th1-lymphocyte–derived cytokines, IFNγ and IL-2, in patients with acute LBP was altered. IFNγ levels were down-regulated, whereas those of IL-2 were markedly increased. Elevated levels of systemic IL-2 have been reported in patients with different etiologies of LBP. [40] However, physiological processes resulting in such polarization of Th1 response in patients with nonspecific acute LBP are unclear. IL-2 is a multifunctional modulatory cytokine and can demonstrate both proinflammatory and anti-inflammatory properties. [41] Firstly, IL-2 controls the level of Th1 activity by induction of T-regulatory cells (Treg) [42] which then inhibit IFNγ production without interference with further Th1 differentiation and thereby IL-2 production. [43] Secondly, in inflammatory conditions, the anti-inflammatory action of IL-2 encompasses suppression of the development of Th17, an inflammatory subset of Th cells. [44] Thus, the observed polarization of Th1 response towards supporting IL-2 production in acute LBP patients may represent an early physiological response to(1) reduce potential detrimental effects of inflammatory action of IFNγ via the expansion of Treg, and
(2) attenuate inflammatory response by decreasing the development of Th17 cells.Indeed, disrupted Th17/Treg balance in patients with chronic LBP [45] and in other inflammatory conditions has been reported. [46] Of interest is, that despite reduced production of IFNγ in patients with acute LBP, its levels correlated significantly with patients’ VAS scores (Table 3). This novel observation may suggest that the role of IFNγ in the pathophysiology of LBP should be further explored. Recently, levels of serum IFNγ were reported to parallel higher pain intensity in patients with failed back surgery syndrome [47] and immunoreactivity of this cytokine in epidural lavage is highly correlated with therapy-modulated pain scores in patients with lumbar degenerative changes and LBP. [48]
Unlike diskogenic pain or pain associated with herniated disk syndromes, in which inflammatory markers have been shown to be synthesized in local cells and tissues, [10, 11] nonspecific LBP is not attributed to a single anatomic structure or tissue. [1] Thus attempts have been made to identify nociceptive inflammatory markers in plasma or serum of such patients and several studies have been published with variable findings. For example, elevated levels of TNFα, IL-1β, CRP, and IL-6 in peripheral blood of patients with acute or chronic LBP have been reported. [4–6, 8] However, in other studies, these mediator levels were not different from physiological ranges observed in asymptomatic individuals. [49, 50] Nonetheless, the results of the present in vitro study are in general agreement with reports demonstrating that inflammatory alterations are inherent in patients with LBP. [4–9] Also, elevated plasma/serum levels of some inflammatory mediators may be correlated with pain levels [6, 8, 49] and disability in elderly patients. [5] In the current study, a positive correlation between pain level and the production of IFNγ, and TNFα and IL-1β, respectively, was observed in acute and chronic LBP patients.
In contrast, in both study groups, a correlation between altered production of inflammatory markers and functional disability scores was found only in relation to IL-6. However, a direct comparison of data from the current study with the published literature is not possible due to the use of different patient cohorts and study models. The short half-life of locally produced inflammatory mediators, as well as physiological variability in levels of cytokine production in asymptomatic individuals, may limit the value of plasma/serum biomarkers as indicators of localized inflammation. [51] In contrast, it is feasible that the presence of inflammatory markers in the circulation of patients with LBP may reflect the state of activation of local inflammation-primed recirculating leukocytes, which may be better assessed in vitro. To date, studies to support this notion are limited. [7, 9, 21] The present study suggests that in patients with nonspecific LBP the response of peripheral blood leukocytes to specific stimulants in vitro is altered in relation to the intensity and duration of the reported pain.
A strength of this investigation was the application of stringent exclusion criteria in accepting participants into the study. Nevertheless, there are a few limitations which necessitate interpretation/discussion of the results with caution. For ethical reasons, and bound by clinical decision making, radiographic evaluation of all recruited patients was avoided. Furthermore, we made no attempt to stratify the data by age as sample size and the relatively narrow age range of participants included in the study precluded us from doing so. Thus, possible structural anomalies and age-related degenerative changes, which might have affected the outcomes were not ruled out. Similarly stratification of data according to the duration of pain within the 4-week acute LBP cohort, patient BMIs, work, and educational status, which may affect outcomes, could yield more robust and additional data. Such an approach would require a much larger sample size and be not feasible in this study. As it is, however, our results have been presented in the general scheme of acute versus chronic nonspecific back pain and can potentially help to generate questions and hypotheses for further studies.
Acknowledgements
The authors express their appreciation and gratitude to Dr A. Teitelbaum, MD, BSc, MSc, Department of Anatomy, CMCC, Toronto, Canada, for performing phlebotomy. The excellent technical assistance of A. Corless, BSc, Biotechnologist, Life Sciences laboratory, CMCC, Toronto, Canada, is deeply appreciated.
Footnotes
Supported by funds from Canadian Memorial Chiropractic College, Toronto, ON, Canada.
The authors declare no conflict of interest.
References:
Maher C, Underwood M, Buchbinder R.
Non-specific low back pain.
Lancet. 2017;389:736–747Paige NM, Myiake-Lye IM, Booth MS, et al.
Association of Spinal Manipulative Therapy with Clinical Benefit and Harm
for Acute Low Back Pain: Systematic Review and Meta-analysis
JAMA. 2017 (Apr 11); 317 (14): 1451–1460Coulter ID, Crawford C, Hurwitz EL, Vernon H, Khorsan R, Suttorp Booth M, Herman PM.
Manipulation and Mobilization for Treating Chronic Low Back Pain:
A Systematic Review and Meta-analysis
Spine J. 2018 (May); 18 (5): 866–879Wang H, Schiltenwolf M, Buchner M.
The role of TNF alpha in patients with chronic low back pain: a prospective, comparative longitudinal study.
Clin J Pain. 2008;24:273–278de Queiroz BZ, Pereira DS, Lopes RA, et al.
Association between the plasma levels of mediators of inflammation with pain and disability
in the elderly with acute low back pain: data from the back complaints in the elders.
Spine. 2016;41:197–203Gebhardt K, Brenner H, Sturmer T, et al.
The course of high sensitive C-reactive protein in correlation with pain and clinical function
in patients with acute lumbosciatic pain and chronic low back pain—a 6 months prospective longitudinal study.
Eur J Pain. 2006;10:711–719Li Y, Liu J, Liu Z, et al.
Inflammation in low back pain may be detected from the peripheral blood: suggestions for biomarker.
Biosci Rep. 2016;36:e00361Licciardone JC, Kearns CM, Hodge LM, et al.
Associations of cytokine concentrations with key osteopathic lesions and clinical outcomes in patients
with nonspecific chronic low back pain: results from the OSTHEOPATHIC trial.
J Am Osteopath Assoc. 2012;112:596–605Teodorczyk-Injeyan JA, McGregor M, Triano JJ, Injeyan SH.
Elevated Production of Nociceptive CC-chemokines and sE-selectin
in Patients with Low Back Pain and the Effects of Spinal Manipulation:
A Non-randomized Clinical Trial
Clin J Pain. 2018 (Jan); 34 (1): 68–75Le Maitre CL, Hoyland JA, Freemont AJ.
Catabolic cytokine expression in degenerate and herniated human intervertebral discs:
IL-1 beta and TNF alpha expression profile.
Arthritis Res Ther. 2007;9:R77Wuertz K, Haglund L.
Inflammatory mediators in intervertebral disk degeneration and discogenic pain.
Global Spine J. 2013;3:175–184Wojdasiewicz P, Poniatowski LA, Szukiewicz D.
The role of inflammatory and anti-inflammatory cytokines in the pathogenesis of osteoarthritis.
Mediators Inflamm. 2014;2014:561459Uceyler N, Rogausch JP, Toyka KV, et al.
Differential expression of cytokines in painful and painless neuropathies.
Neurology. 2007;69:42–49Moore KW, de Waal Malefyt R, Coffman RL, et al.
Interleukin-10 and interleukin-10 receptor.
Annu Rev Immunol. 2001;19:683–765Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Fairbank JC, Pynsent PB.
The Oswestry Disability Index
Spine (Phila Pa 1976) 2000 (Nov 15); 25 (22): 2940–2952Damsgaard CT, Lauritzen L, Calder PC, et al.
Whole blood culture is a valid low-cost method to measure monocytic cytokines-a comparison of
cytokine production in human whole-blood, mononuclear cells and monocytes.
J Immunol Methods. 2009;340:95–101Yaqoob P, Newsholme D, Calder PC.
Comparison of cytokine production on cultures oh whole human blood and purified mononuclear cells.
Cytokine. 1999;11:600–605Lagrelius M, Jines P, Franck K, et al.
Cytokine detection by multiplex technology useful for assessing antigen specific cytokine profiles
and kinetics in whole blood cultured up to 7 days.
Cytokine. 2006;33:156–165Cohen J.
Statistical Power Analysis for the Behavioral Sciences, 2nd edition
Hillsdale, NJ: Lawrence Erlbaum Associates; 1988Hammer Ø, Harper DA, Ryan PD.
PAST: paleontological statistics software package for education and data analysis.
Palaeontol Electron. 2001;4:1–9Teodorczyk-Injeyan JA, Triano JJ, McGregor M, et al.
Elevated Production of Inflammatory Mediators Including Nociceptive Chemokines in Patients
With Neck Pain: A Cross-Sectional Evaluation
J Manipulative Physiol Ther. 2011 (Oct); 34 (8): 498-505Haudek-Prinz VJ, Klepeisz P, Slany A, et al.
Proteome signatures of inflammatory activated primary human peripheral blood cells.
J Proteomics. 2012;76:150–162Vaday GG, Franitza S, Schor H, et al.
Combinatorial signals by inflammatory cytokines and chemokines mediate leukocyte interactions with extracellular matrix.
J Leukoc Biol. 2001;60:885–892Xu H, Manivannan A, Crane I, et al.
Critical but divergent roles for CD62L and CD44 in directing monocyte trafficking in vivo during inflammation.
Blood. 2008;112:1166–1174Thaler B, Hohensinner PJ, Krychtiuk KA, et al.
Differential in vivo activation of monocyte subsets during low-grade inflammation through experimental
endotoxemia in humans.
Sci Rep. 2016;6:30162Ritz BW, Alexander GM, Nogusa S, et al.
Elevated blood levels of inflammatory monocytes (CD14+CD16+) in patients with complex regional pain syndrome.
Clin Exp Immunol. 2011;163:108–117Sabroe I, Parker LC, Dower SK, et al.
The role of TLR activation in inflammation.
J Pathol. 2008;214:126–135Qiao Y, Giannopoulou EG, Chan CH, et al.
Synergistic activation of inflammatory cytokine genes by interferon-γ-induced chromatin remodeling
and toll-like receptor signaling.
Immunity. 2013;39:454–469Kwok YH, Hutchinson MR, Gentgall MG, et al.
Increased responsiveness of peripheral blood mononuclear cells to in vitro TLR 2, 4, and 7 ligand
stimulation in chronic pain patients.
PLoS ONE. 2012;7:e44232Devêvre EF, Renovato-Martins M, Clément K, et al.
Profiling of the three circulating monocyte subpopulations in human obesity.
J Immunol. 2015;194:3917–3923Garlanda C, Dinarello CA, Mantovani A.
The interleukin-1 family: back to the future.
Immunity. 2013;39:1003–1018Molnarfi N, Gruaz L, Dayer JM, et al.
Opposite regulation of IL-1β and secreted IL-1 receptor antagonist production by phosphatidylinositide-3
kinases in human monocytes activated by lipopolysaccharides or contact with T cells.
J Immunol. 2006;178:446–454Malyak M, Swaney E, Arend WP.
Levels of synovial fluid interleukin-1 receptor antagonist in rheumatoid arthritis and other arthropathies;
potential contribution from synovial fluid neutrophils.
Arthritis Rheum. 1993;36:781–789Dinarello CA.
Therapeutic strategies to reduce IL-1 activity in treating local and systemic inflammation.
Curr Opin Pharmacol. 2004;4:378–385Sinclair SM, Shamji MF, Chen J, et al.
Attenuation of inflammatory events in human intervertebral disk cells with a tumor necrosis factor antagonist.
Spine. 2011;36:1190–1196Carpentier I, Coornaert B, Beyaert R.
Function and regulation of tumor necrosis factor receptor type 2.
Curr Med Chem. 2004;11:2205–2212Backonja MM, Coe CI, Muller DA, et al.
Altered cytokine levels in the blood and cerebrospinal fluid of chronic pain patients.
J Neuroimmunol. 2008;195:157–163Uceyler N, Valenza R, Stock M, et al.
Reduced levels of anti-inflammatory cytokines in patients with chronic widespread pain.
Arthritis Rheum. 2006;54:2656–2664Weber KT, Satoh S, Olivier Alipui D, et al.
Exploratory study for identifying systemic biomarkers that correlate with pain response in
patients with intervertebral disc disorders.
Immunol Res. 2015;63:170–180Hoyer K, Dooms H, Barron L, et al.
Interleukin-2 in the development and control of inflammatory disease.
Immunol Rev. 2008;226:19–28Workman CJ, Szymczak-Workman A, Collison LW, et al.
The development and function of regulatory T cells.
Cell Mol Life Sci. 2009;66:2603–2622Sojka DK, Fowel DJ.
Regulatory T cells inhibit acute IFN-γ synthesis without blocking T-helper cell type 1 (Th1)
differentiation via compartmentalized requirement for IL-10.
Proc Natl Acad Sci USA. 2011;108:18336–18341Laurence A, Tato CM, Davidson TS, et al.
Interleukin-2 signalling via STAT5 constrains T helper 17 cell generation.
Immunity. 2007;26:371–381Luchting B, Rachinger-Adam B, Zeitler J, et al.
Disrupted TH17/Treg balance in patients with chronic low back pain.
PLoS ONE. 2014;9:e104883Noak M, Miossec P.
Th17 and regulatory T cell balance in autoimmune and inflammatory diseases.
Autoimmun Rev. 2014;13:668–677Kamieniak P, Bielewicz J, Grochowski C, et al.
The elevated serum level of IFN-γ in patients with failed back surgery syndrome remains unchanged
after spina cord stimulation.
Dis Markers. 2019;2019:2606808Cuellar JM, Golish SR, Reuter MW, et al.
Cytokine evaluation inindividuals with low back pain using discogenic lavage.
Spine J. 2010;10:2212–2218Klyne DM, Barbe MF, Hodges PW.
Systemic inflammatory profiles and their relationship with demographic, behavioral and clinical
features in acute low back pain.
Brain Behav Immun. 2017;60:84–92Klyne DM, Barbe MF, van den Hoorn W, et al.
Longitudinal analysis of inflammatory, psychological, and sleep-related factors following an acute
low back pain episode—the good, the bad and the ugly.
Eur Spine J. 2018;27:763–777Zhoua X, Fragala MS, McElhaney JE, et al.
Conceptual and methodological issues relevant to cytokine and inflammatory marker measurements in clinical research.
Curr Opin Clin Nutr Metab Care. 2010;13:541–547
Return to LOW BACK PAIN
Return to the MEDICARE Page
Since 4-11-2020


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |