

Sensorimotor Function and Dizziness in Neck Pain:
Implications for Assessment and ManagementThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Orthop Sports Phys Ther. 2009 (May); 39 (5): 364–377 ~ FULL TEXT
OPEN ACCESS Eythor Kristjansson, PhD, ManipTher, BSc, Julia Treleaven, PhD, BPhty
Faculty of Medicine,
The University of Iceland,
Reykjavik, Iceland.
FROM: J Orthop Sports Phys Ther 2009The term sensorimotor describes all the afferent, efferent, and central integration and processing components involved in maintaining stability in the postural control system through intrinsic motor-control properties. The scope of this paper is to highlight the sensorimotor deficits that can arise from altered cervical afferent input. From a clinical orthopaedic perspective, the peripheral mechanoreceptors are the most important in functional joint stability; but in the cervical region they are also important for postural stability, as well as head and eye movement control. Consequently, conventional musculoskeletal intervention approaches may be sufficient only for patients with neck pain and minimal sensorimotor proprioceptive disturbances. Clinical experience and research indicates that significant sensorimotor cervical proprioceptive disturbances might be an important factor in the maintenance, recurrence, or progression of various symptoms in some patients with neck pain. In these cases, more specific and novel treatment methods are needed which progressively address neck position and movement sense, as well as cervicogenic oculomotor disturbances, postural stability, and cervicogenic dizziness. In this commentary we review the most relevant theoretical and practical knowledge on this matter and implications for clinical assessment and management, and we propose future directions for research.
Keywords: cervical, head, postural stability, proprioception, sensorimotor
From the FULL TEXT Article:
Background
Persistent neck pain of greater than 6 months' duration is a frequent occurrence in both men and women, [41] and patients with neck pain are the second largest group (after patients with low back pain) attending physical therapy and chiropractic clinics for relief of their symptoms. [2] Further research shows that about one third of patients diagnosed with whiplash-associated disorder (WAD) (a variety of clinical manifestations due to bony or soft tissue neck injuries following an acceleration-deceleration energy transfer sustained from a motor vehicle accident [119]) only gain short-term relief by conventional musculoskeletal interventions, [12, 82, 123] which, by definition, are an ineffective treatment. Preventing a portion of patients with neck pain to enter the chronic phase of their condition represents a great challenge for clinicians.
The cervical spine, especially the upper cervical spine, is the most mobile part of the vertebral column. Its mobility comes at the expense of its mechanical stability. [7, 22] The highly developed proprioceptive system provides neuromuscular control to the mobile cervical spine and allows efficient utilization of the vital organs in the head [42] via unique connections to the vestibular and visual systems. [22, 77, 80, 87, 109] This may explain why the cervical spine is an extremely vulnerable structure, especially where trauma is involved (eg, whiplash injury), and is a source of a plethora of symptoms that do not arise from any other musculoskeletal region of the body. [58]
Disturbances to the afferent input from the cervical region in those with neck pain may be a possible cause of symptoms such as dizziness, unsteadiness, and visual disturbances, as well as signs of altered postural stability, cervical proprioception, and head and eye movement control. Conventional approaches to management may be sufficient for patients with neck pain with minimal sensorimotor proprioceptive disturbances. However, clinical experience and research indicates that significant sensorimotor proprioceptive disturbances in the cervical spine might be an important factor in the maintenance, recurrence, or progression of various symptoms in patients with neck pain. [52, 122] Thus, addressing these deficits is likely to be an important step towards better management of some patients with neck pain.
The scope of this paper is to highlight the sensorimotor deficits that can arise from altered cervical afferent input. While the cervical spine should always be considered in the differential diagnosis of dizziness and unsteadiness, as well as visual disturbances, other potential causes, such as peripheral or central vestibular pathology and pathology in the central nervous system (CNS) along with vertebrobasilar insufficiency, must also be considered and excluded. [57] The mere combination of dizziness and neck pain should not be interpreted as necessarily indicating the neck to be the source of the dizziness.64 Dizziness and visual disturbances as a consequence of altered afferent input from the cervical spine structures are a controversial subject and not widely accepted by the medical profession. The primary reason for this lack of recognition is that conventional testing methods cannot verify the patient's subjective complaints in most instances. [57] Generally, cervicogenic deficits appear to be more subtle and less severe when compared to those that present with primary CNS or vestibular system pathologies. [31, 134] Nevertheless, the presence of CNS signs in the absence of a diagnosis or other explanation should be considered a red flag and the physical therapist should immediately refer the patient to a physician for further workup.
The Cervical Spine and the Postural Control System
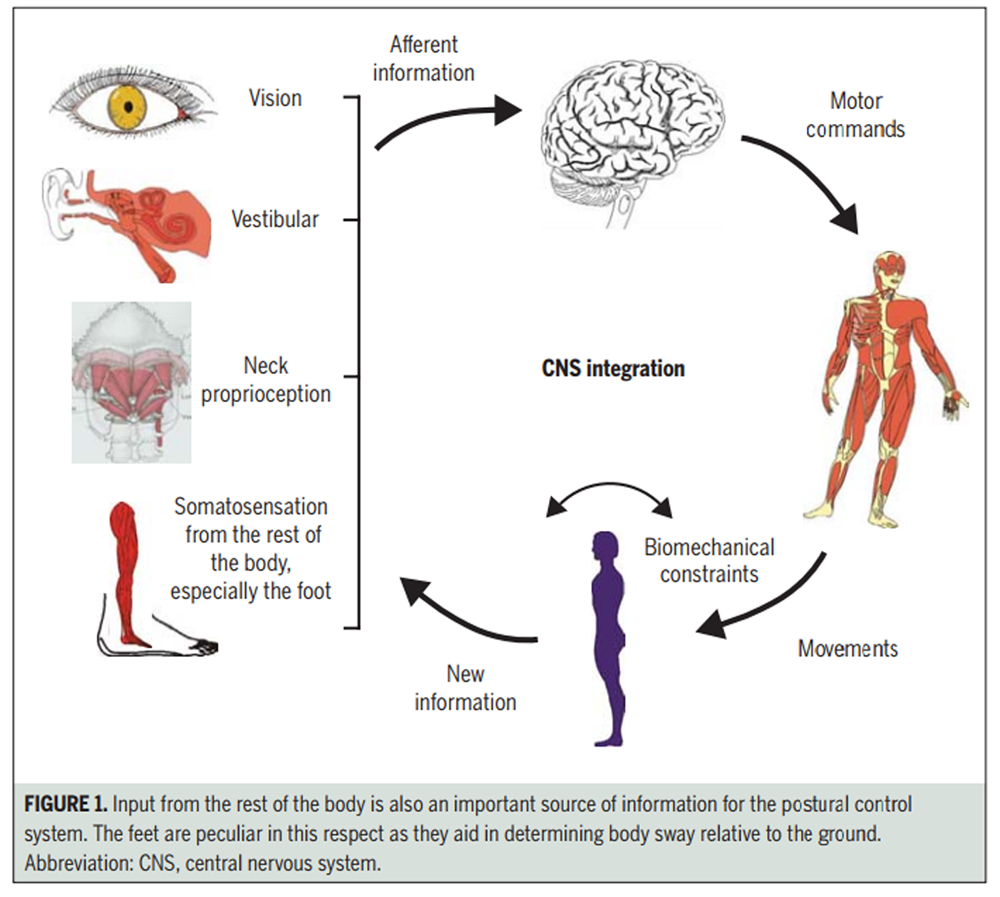
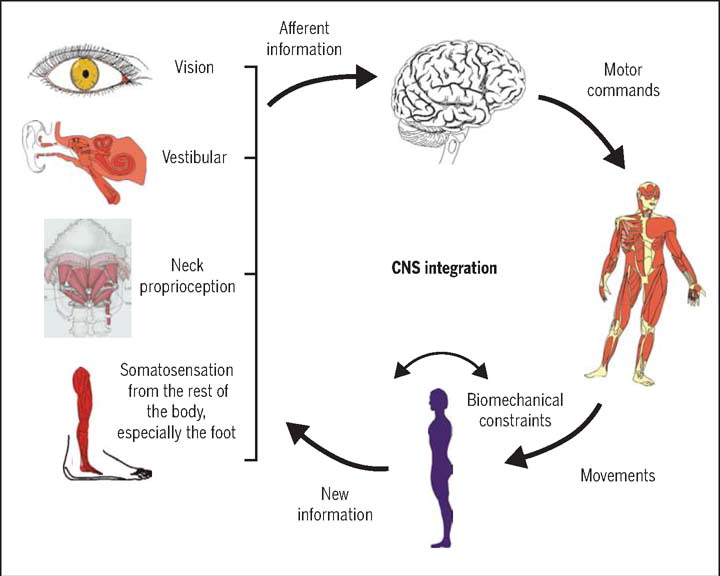
Figure 1 The postural control system includes all the sensorimotor and musculoskeletal components involved in the control of 2 important behavioral goals: postural orientation and postural equilibrium. Postural orientation is the relative positioning of the body segments with respect to each other and to the environment, whereas postural equilibrium is the state in which all the forces acting on the body tend to keep the body in a desired position and orientation (static equilibrium) or to move in a controlled way (dynamic equilibrium). Postural control provides a stable body platform for the efficient execution of focal or goal-directed movements. [56] Figure 1 provides an overview of the subsystems in the postural control system. The somatosensory, vestibular, and visual systems are the subsystems that provide sensory input to the postural control system.
The Somatosensory Subsystem This system encompasses all of the mechanoreceptive information arising from the periphery [43] which leads to the perception of pain, temperature, touch, and proprioception. [110] The proprioceptive system of the cervical spine, in particular, is extremely well developed, as reflected by an abundance of mechanoreceptors, especially from the ?-muscle spindles in the deep segmental upper cervical muscles. [73, 76, 122] The ?-muscle spindle system serves as the final common pathway for the regulation of the muscle stiffness required for various neuromuscular performances. [116] Muscle spindle afferents appear particularly important, as they play the first violin in the proprioceptive ensemble, while other mechanoreceptors, such as the joint receptors and golgi tendon organs, fine tune the muscle spindle information, predominantly by reflex effects on the ?-motoneurones. [116]
The dense network of mechanoreceptors in the soft tissues in this region not only controls multiple degrees of freedom of movements about each of its joints but, more importantly, gives the CNS information about the orientation of the head with respect to the rest of the body via direct neurophysiological connections to the vestibular and visual systems. Somatosensory information from the cervical region is the only region that has this direct access to the sense of balance and sense of sight. [23, 57]
The Vestibular Subsystem This system is specially designed to maintain adequate postural tone in the muscles of the trunk and extremities to provide overall balance during posture and locomotion. Neck, eye, trunk, and limb muscle reflexes evolved to meet these requirements. The specialized mechanoreceptors in the semicircular canals are sensitized during changes in rate of motion; that is, angular velocity, and the specialized mechanoreceptors in the otolith systems of the utricular and saccular maculae provide information about the position and velocity of the head relative to the direction of the forces of gravity. [50] Sensory information from the vestibular system converges in all nuclei comprising the vestibular nuclear complex (VNC) via the vestibular nerve and in the cerebellum. [95].
The Visual Subsystem Vision plays a dominant role in the guidance of movements and this is reflected by the fact that when somatosensory inputs and vision disagree, it is usually the visual version of events that prevails. [121] The visual postural system consists of 3 different eye movement systems: the smooth pursuit system, the saccadic system, and the optokinetic system. [129] The smooth pursuit system stabilizes images of smoothly moving targets on the fovea by slow eye movements. The saccadic system, on the other hand, is responsible for rapid, small movements of both eyes simultaneously in changing a point of fixation. The optokinetic system stabilizes images on the entire retina whenever the entire visual field is moving (eg, when walking). [129]
Relevant Neurophysiological Connections
There are many direct neurophysiological connections between these 3 subsystems and from the cervical region to the postural control system, which provides further evidence for the plausability of the varied signs and symptoms that occur as a consequence of disturbed cervical afferent input in those with neck pain.
Mechanoreceptor input from the uppermost cervical segments (Occiput-Atlas, Atlas-Axis, Axis-C3), particularly from the upper cervical spine muscles, has direct access to the VNC and the superior colliculus, a reflex centre for coordination between vision and neck movement. [17] It also converges in the central cervical nucleus (CCN), [94] which serves as a pathway to the cerebellum where vestibular, ocular, and proprioceptive information is integrated. [129] The CCN also has important connections to the VNC. [94] This allows the postural control system to quickly receive information about the position and movement of the head in relation to the body and to integrate cervical information with that from the labyrinths and eyes so that different information from the subsystems can be compared and equalized.
Reflex Pathways Close connections between the cervical somatosensory, vestibular, and visual systems are also demonstrated in a number of reflexes influencing head orientation, postural stability, and eye movement control. [89, 102] The cervicocollic reflex, the cervico-ocular reflex, and the tonic neck reflex are generated by cervical afferents and work in conjunction with other vestibular and visual reflexes for coordinated stability of posture, as well as head and eye movement control. The cervicocollic reflex works with the vestibulocollic reflex to activate neck muscles and protect the cervical spine against overrotation. [102, 103] The cervico-ocular reflex works with the vestibulo-ocular and optokinetic reflexes to control the extraocular muscles, creating clear vision with head movement. The tonic neck reflex maintains a stable posture via alteration in limb muscle activity when the body moves with respect to the head and is integrated with the vestibulospinal reflex. [145]
Translating Relevant Research Into Clinical Practice
The importance of the above neurophysiological connections between the cervical spine structures and the vestibular and visual systems is demonstrated by the adverse effects on postural stability and eye and head movement control following artificial disturbance to cervical afferents in healthy human subjects. For example, stimulation of the muscle spindle afferents, via neck muscle vibration induces eye position changes, visual illusory movements, and head movement illusions, [69, 79, 126] and has been shown to influence postural stability and the velocity and direction of gait and running. [9, 18, 79] Even wearing a restrictive brace (hard collar) for 5 days or being exposed to sustained isometric neck muscle contraction has been demonstrated to lead to altered eye movement control, increased postural sway, and disturbed head-neck awareness in healthy persons. [21, 39, 66, 98, 113, 114, 140]
The upper cervical region has an abundance of muscle spindle receptors and greater contributions to reflex activity and connections to the visual and vestibular systems when compared to the lower cervical spine. [77, 80, 93, 94] This might suggest that patients with neck pain with upper cervical complaints have greater potential for balance and visual disturbances than those with complaints from the lower cervical spine. [128]
In patients with neck pain, there are several mechanisms that could disturb cervical afferent activity. Sensitivity of the receptors can be affected by chemical changes brought about by ischemic or inflammatory events, [127] as well as reflex joint inhibition of the muscle spindles. [86, 127, 142] Pain at many levels of the CNS can change muscle spindle sensitivity and alter the cortical representation and modulation of cervical afferent input. [34, 78, 127] Psychosocial distress also has the potential to alter muscle spindle activity via activation of the sympathetic nervous system. [101] Functional impairment of the muscles, such as increased fatigability, [28] and degenerative changes, such as fiber transformation, [139] fatty infiltration, and atrophy of the neck muscles, [25, 72, 88] may alter their proprioceptive capabilities, joint mechanics, and muscle spindle sensitivity, thus affecting cervical afferent input. [20]
Sensorimotor control deficits such as disturbances to head-neck awareness, [45,7 3, 81, 107, 136] neck movement control,74 postural stability, [1, 84, 90, 112, 118, 135, 138] and oculomotor contro [l53, 124, 129, 134] can present in patients with idiopathic neck pain and in those not specifically complaining of dizziness, unsteadiness, or visual disturbances as symptoms. [31, 73, 130] However, these sensorimotor control deficits have been shown to be more pronounced in patients with whiplash injury and those with complaints of dizziness, unsteadiness, or visual disturbances. [128, 130, 134, 136] Furthermore, there does not appear to be a direct relationship between the impairments, such that an individual patient may present with dysfunction in either 1 or several systems, and thus evaluation of each area of sensorimotor control should be considered appropriate for all patients with neck pain. [133]
Clinical Research
Clinical Presentation Relocation tests that either relocate the natural head posture or the head to a set point in range have most commonly been used to verify poor awareness of the head-neck region in patients with neck pain to reflect impaired cervical position sense. These methods address a patient's ability to consciously indicate when a prespecified position has been reproduced. Impairments have been demonstrated by these methods in subjects with neck pain of both idiopathic and traumatic origin (ie, whiplash injury). [45, 73, 81, 107, 136] Patients who overshoot targets when position sense is measured may have disordered cervicocollic reflex inhibition. [103]
Clinical Presentation Patients with neck pain seem to have a poor awareness of their head-neck posture, and some indeed complain about “a wobbling head,” [75] which may be resultant of impaired cervical position sense.
Clinical Assessment Cervical position sense can be assessed clinically by using a laser pointer mounted onto a lightweight headband. Patients are asked to focus on the natural resting head position for a few seconds, sitting 90 cm away from a wall. With the eyes closed, they actively move the head and then try to come back to the resting position as accurately as possible. The difference between the starting and resting position of the laser beam on the wall can be measured in centimeters and then converted into degrees (angle = tan-1[error distance/90 cm]). Thus an approximately 7.1-cm error distance would translate to a meaningful error of 4.5° (as long as the subject is sitting 90 cm from the wall) and is called the joint position error (JPE). [107, 111] JPE can be assessed on return from all active cervical movements. Errors of greater than 4.5° are thought to suggest impairment in relocation accuracy of the head-neck. [107, 111] Patients might also demonstrate jerky or altered movement patterns, overshooting of the position in order to gain more proprioceptive feedback for the task, or “searching” for the position. Occasionally patients will also experience a reproduction of dizziness and/or unsteadiness with the task. A computerized method for assessing position sense in the clinical setting is currently being developed. The goal is to improve measurement accuracy and to provide more sophisticated feedback than the laser beam method, while ensuring that each patient can start the treatment for improving head-neck awareness at his/her impairment level.
]19 and, recently, segmental hypermobility was demonstrated in the lower cervical spine in some women with chronic whiplash. [76] In these individuals, management directed towards the stabilizing musculature and optimal neuromuscular control of movement is thought to be particularly important.
Disturbed Neck Movement Control
Clinical Research Despite many attempts to quantify intersegmental movements in the spine and to describe the movements qualitatively, no method has yet been validated to reliably detect minor segmental instabilities in the cervical spine. [35] Minor segmental instabilities or segmental hypermobilities, therefore, remain an intensely controversial topic, as there is no consensus about its precise definition. [3, 100, 125] Nevertheless, early spinal degenerative change has been recognized as a potential physiological basis for minor segmental instabilities,
The importance of the deep stabilizing musculature of the neck for spinal segmental support and control has been demonstrated [15, 85] and clinical research indicates that many patients with neck pain have inadequate support from these muscles. [26, 29, 62] Insufficiency in the pre-programmed activation of the cervical muscles, altered motor control recruitment patterns, and increased fatigability have also been found in patients with neck pain. [27, 28] Further, the measured increased activation of the superficial cervical musculature in those with neck pain is thought to be a compensation for poor passive or active segmental support. [28, 73]
These changes in muscle function have potential to overload painful cervical structures and affect cervical movement sense and control. This may cause uncertainty for the patient, automatically leading to further increased muscle cocontraction, [36] diminishing range of motion for self-protection of the cervical spine movements. This could reduce the frequency and duration of muscle relaxation periods, causing release of inflammatory substances and promoting a vicious cycle. [6] Patients with chronic whiplash present as a difficult clinical condition as the initial trauma can also compromise joint stability by permanent changes in tissue compliance or cause direct damage to the mechanoreceptors and their axons, because they have lower tensile strength than the surrounding collagen fibers. [73, 87]
Recently a computerized method to measure accuracy of head and neck movement called “the Fly” was developed. [74] It measures the patient's ability to correct cervical spine movements on a moment-to-moment basis, while moving the head-neck. This method has demonstrated impaired head-neck movement accuracy in patients with a history of whiplash injury when compared to controls. [74]
Clinical Presentation Subjective complaints of a painful stiff neck are often accompanied by associated complaints like “my neck movements feel jerky,” “intense tiredness in the back of the neck,” and “the head feels heavy.” [75] Clinicians often suspect these patients to have disturbed neck movement control as a consequence of the aforementioned clinical research findings.
Clinical Assessment In the Fly, [74] the patient sits in front of a computer with sensors on the head, which accurately measure the positions and movements of the head-neck in space. Two cursors are visible on the computer screen: 1 cursor is black, indicating the movements of the head-neck, and the other cursor is blue, derived from the Fly software program. At the very beginning of the test, both cursors match each other in the middle of the screen. Then the blue cursor starts to move, tracing slow and unpredictable movement patterns of short duration. The patient is instructed to follow the Fly with the black cursor by moving the head-neck as accurately as possible. The deviation or amplitude accuracy between the 2 cursors is continuously recorded during 3 randomly ordered test sequences. [74] The Fly method has recently been revised and can be used to grade the deficits of movement control in patients with neck pain much more accurately than the prior Fly method, and, consequently, a treatment can be prescribed that starts at each patient's impairment level. Hitherto, the laser method (as used for joint position sense) has been used by some therapists to trace an intricate pattern such as a figure-of-eight placed on the wall 90 cm in front of the patient. A subjective clinical judgment can be made based on the patient's ability to trace the pattern accurately and smoothly.
Disturbed Postural Stability: Dizziness and/or Unsteadiness
Clinical Research Cervical induced balance disturbances can be caused by several different pathophysiological processes, including irritation of the sympathetic vertebral plexus, vertebrobasilar insufficiency, and sensorimotor disturbances from the cervical spine structures. [4] Emerging evidence draws attention to the last explanation. [74, 84, 136, 141] Altered sensory input, especially mediated via the direct neurophysiological connections between the upper cervical spine structures and the vestibular system, has the potential to disturb an intact vestibular subsystem. [32, 55, 93, 95] This makes the patient—in this case a patient with neck pain and faulty neck mechanoreceptor input—less able to utilize internal vestibular orienting information to resolve inaccurate information from the somatosensory and visual subsystems. [112] This is in accordance with the “sensory mismatch” theory, which holds that sensations of dizziness and unsteadiness arise because of a conflict between the converging input from the different sensory subsystems and the expected sensory patterns. [10]
Clinical research and experience indicates that some patients with neck pain do not seem to be aware that they have standing balance disturbances until their standing balance is challenged. [11, 74] A possible explanation is that the symptoms of cervicogenic dizziness may abate once the CNS has adapted to the altered neurophysiological inputs, even though the underlying dysfunction remains. [16] It is hypothesized that the vestibular and the somatosensory subsystems may compensate for the balance disturbances by increasing the muscle stiffness in the body as a whole, [11] which may also explain the unrelenting hyperactivity in the musculature in some patients with neck pain. [24] This may serve as one explanation for why some patients with WAD develop fibromyalgia. [13, 14] It is, therefore, important to screen patients with neck pain for balance disturbances, even in the absence of subjective complaints about balance problems.
Several studies have demonstrated disturbed postural stability in patients with neck pain, [1, 31, 67, 68, 84, 90, 104, 118, 135, 138] especially in those with neck pain from whiplash injury and those complaining of dizziness. [31, 135] Most of the research has been conducted with respect to static standing balance where an increase in postural sway or rigidity is noted even in simple tests of standing comfortably on a firm surface with eyes closed. An increased rate of failure to maintain stability for 30 seconds in the more challenging tandem stance position has also been seen in those with neck pain when compared to asymptomatic individuals. [31, 90, 135, 138] Recently, it has been suggested that cervical muscle fatigue may be an important contributing factor to altered postural stability in those with neck pain. [120] One study has demonstrated a correlation between fatty infiltration of the suboccipital muscles and balance deficits, [88] and further research into this hypothesis is currently underway.
Clinical Presentation Cervical induced dizziness is characterized by subjective complaints of unsteadiness, insecurity, and lightheadedness. [58, 64] Some patients also complain about a feeling of spinning, but this is more like a feeling of “spinning in the head” rather than spinning of the patient or the surroundings, as in typical vertigo of vestibular origin. [58] Often cervical dizziness presents as a tipsy state as a consequence of “noise” in the postural control system and may be accompanied by nausea. It is rarely described as strong attacks of dizziness or vertigo. [136]
The subjective complaints are often more pronounced early in the morning when the neck is stiff and late in the afternoon as the patient becomes tired. Quick movements of the cervical spine, especially in the transverse plane but also in the sagittal plane, most commonly provoke these symptoms; but they may also occur when watching moving objects [94] or walking in the dark.
Clinical Assessment Karlberg et al [65] proposed a scientific method to measure cervical-related balance disturbances in individuals with acute neck pain, but this method has not yet been validated to measure more longstanding cervicogenic balance disturbances where compensatory mechanisms might be present. A clinical diagnosis of cervical-induced dizziness and/or unsteadiness is, therefore, a diagnosis of exclusion of other possible causes. [65] However, research suggests that balance disturbances in neck pain present differently than those with a vestibular disorder, in whom balance disturbances appear to be easily noticeable on difficult tests, such as narrow stance on a foam surface, when compared to those with whiplash, who showed more subtle deficits in all tests. [65, 137] At present, clinical tests of postural stability are not useful to differentiate between a vestibular or neck etiology of balance disturbances. But, as mentioned, the clinical presentation of these 2 conditions is different. Nevertheless, balance in comfortable and narrow stance with the eyes open and closed should be assessed with the patient standing on a firm surface then a soft surface, such as a piece of 10-cmthick dense foam. Inability to maintain stance for 30 seconds, noticeably large increases in sway, slower responses to correct sway, or rigidity to prevent sway are considered abnormal responses. The patient's ability to maintain tandem and single-leg stance on a firm surface with eyes open and closed for up to 30 seconds can also be assessed; although care in interpretation of the results in these more difficult tests is needed in older individuals, where the ability to maintain tandem stance can be impaired in normal adults above the age of 45 years. [31, 138]
To date, little research has been conducted to determine any changes to functional or dynamic balance in individuals with neck pain; however, disturbances to the velocity and direction of gait and running have been seen in response to neck muscle vibration in asymptomatic control subjects, [9, 18] and, recently, older patients (65–80 years of age) with neck pain demonstrated significant differences in the dynamic gait index (DGI), timed 10-meter walk with head turns, and the step test, when compared to elders without neck pain. [63, 104] The DGI rates the control of 8 functional mobility tasks that include walking at comfortable and changing speeds, walking with horizontal and vertical head movements, walking, pivot turning, stepping over and around an object, and walking up and down stairs. [144] The timed 10-meter walk with head turns48 measures the time and number of steps taken to complete the task. [8] The step test [54] is the number of steps completed on and off a 7.5-cm step in 15 seconds for each limb.
Thus clinicians should consider such dynamic tests particularly for patients with neck pain complaining of dizziness, unsteadiness, or loss of balance. Normative values for these tests are generally provided for elders (65–80 years of age; DGI score, 21/24; timed 10-meter walk with head turns, 15 steps in 8 seconds; and the step test, 14–15 steps).63,104 However, a recent study looked at a younger group of subjects between 43 and 57 years of age.83 Normative values provided in this study were a DGI score of 23 to 24, a timed 10-meter walk with head turns of 15 steps in 8 seconds, and a step test of 21 steps.83 Further research into younger subjects (less than 40 years of age) is required.
Oculomotor Disturbances
Clinical Research Deficits in oculomotor control, such as decreased smooth pursuit velocity gain, altered velocity and latency of saccadic eye movements, and an increased gain of the cervico-ocular reflex have been seen in patients with neck pain. [38, 47, 53, 70, 91, 124, 129, 130, 134, 141] In people with vestibular disorders and in the elderly, an increased gain of the cervico-ocular reflex is considered a compensation response to a decrease in vestibulo-ocular gain. [92] However, a compensatory decrease in the vestibulo-ocular gain has not been seen in those with an increased cervico-ocular gain secondary to whiplash, and this imbalance between the reflexes has been suggested as a potential cause of disturbances to the visual system. [92] There is also some evidence that eye movement dysfunction may be associated with a poorer prognosis in those with a whiplash injury. [52, 53] Altered cervical somatosensory input is thought to adversely influence eye movement control. Further, there is also some evidence that normal reflexive neck muscle activity seen during eye movements in individuals without neck pain is altered with respect to timing in those with neck pain. [5] Abnormal neck muscle activity associated with eye movement will have further implications for the control of neck posture and movement, and, again, could contribute to a vicious cycle of altered cervical afferent input and altered sensorimotor control. [5]
The smooth pursuit neck torsion test developed by Tjell et al [129] is considered to be specific for detecting eye movement disturbances due to altered cervical afferent input. This test measures the difference in smooth pursuit eye movement control with the head and trunk in a neutral position, compared to when the trunk and neck are rotated relative to the stationary head. [130] A decrease in velocity gain of smooth pursuit eye movements when the head is in a relatively torsioned (rotated) position, when compared to the neutral position, is only seen in those with neck pain (ie, not in those with vestibular or CNS disorders) and is most evident in those with whiplash and in those complaining of dizziness. [129, 130, 134]
Recently, a pilot trial of case studies of individuals with whiplash reporting visual disturbances indicated deficits in head-eye coordination when compared to control subjects. [40] Specifically, a decreased range of head movement during gaze fixation, a decreased head velocity during tasks involving head-eye coordination, and compensatory head movements during isolated eye rotation were noted that suggest disturbances in gaze stability and head-eye coordination in some of those with whiplash. [40]
Clinical Presentation Patients with neck pain sometimes complain about symptoms relating to the visual system such as blurred vision, reduced visual field, grey spots appearing in the visual field, temporary blinding, photophobia, and disordered fusion. [57, 143] These visual disturbances may explain reading problems reported by some patients with neck pain. [37] Diplopia, which is common in patients with vertebrobasilar insufficiency, is rare in somatic neck dysfunctions. If patients with neck pain report double vision, it is most often not true diplopia but rather the contours of an object that become unclear. [57]
Clinical Assessment While we are just starting to develop clinical assessment methods, it is currently suggested that the clinical examination of oculomotor control in those with neck pain should include a qualitative analysis of eye follow (smooth pursuit) while keeping the head still (comparing neck neutral to neck torsion), head movement while maintaining focus on an object (gaze stability), head and eye movement coordination, and quick movements of the eyes to refocus (saccades).
Clinical assessment of eye movement in those with neck pain can be conducted by assessing the quality of eye movements and eye movement control, as well as any reproduction of symptoms during the tests described below. Such tests are not exclusive to, nor can specifically differentiate, those with cervical disorders and are often used in those with vestibular or CNS disorders; although some tests have been modified in an attempt to bias a cervical component to the testing.
Smooth Pursuit The patient is asked to accurately and smoothly follow a slow-moving target with his/her eyes, while keeping the head still. The target is moved from side to side. Quick saccadic eye movements to catch up to the target rather than smooth eye movement, especially during midrange eye movement, are an indication of impairment in the task. [134] Reproduction of dizziness and blurred vision may also occur. Deterioration of eye follow (increase in catch-up saccades), when the patient's trunk is subsequently turned to 45° (in either direction), while the head is kept still, suggests a cervical afferent component to the deficits as seen on the smooth-pursuit neck torsion test. [129] If a poor performance is noted when the head is in neutral, and is unchanged by adding neck torsion by rotating the trunk 45°, this would imply a CNS disorder.
Gaze Stability The patient is asked to focus on a point directly in front of him/ her and maintain visual focus as the patient actively moves the head into rotation and flexion and extension. Despite the patient having the available rotation range of motion and ability to perform the task accurately when not fixating the patient's gaze, patients with neck pain often [40] are unable to keep focus or move the head as far or as quickly or smoothly as asymptomatic individuals (45°). They may also deviate into cervical lateral flexion. Reproduction of dizziness and/or blurred vision may occur. This is similar to the dynamic visual acuity test used for those with vestibular disorders; however, head movement is performed actively and slowly rather than passively and quickly. This approach is better suited to cervical-related gaze disorders, as the cervical afferents are stimulated at lower movement frequencies compared to fast movements that stimulate the vestibular afferents. [49]
Saccadic Eye Movement The patient quickly moves the eyes to fix his/her gaze between several targets. The targets are placed in several different movement directions. Inability to fixate on target, overshooting the target, and taking more than 2 eye movements to reach the target might indicate a poor performance. Again reproduction of dizziness and or blurred vision may also occur.
Eye-Head Coordination The patient first moves the eyes to a point to focus and then, while maintaining focus, moves the head to that point. This can be performed to the left and right, and up and down. Asymptomatic individuals are able to perform isolated eye and head movements and maintain focus. Often, patients with neck pain are unable to keep their head still while their eyes move or lose focus during the head movements. [40] Eye and head movements to follow a trunk or an arm movement can also be assessed.
Clinical Management
Evidence to date would suggest that management of disturbed sensorimotor control due to cervical somatosensory dysfunction might need to address the local causes of abnormal cervical afferent input. The important links between the cervical somatosensory, vestibular, and visual systems, and secondary adaptive changes in the sensorimotor control system need also to be considered. This is of the utmost importance to understand for the optimal management of patients with neck pain, as secondary disturbances in the vestibular and visual systems can occur via plasticity in the CNS. [115] Therefore, a combined approach is likely to best address the perpetuation of a vicious cycle of events where secondary adaptive changes in the sensorimotor control system could lead to altered cervical muscle function and joint mechanics further altering cervical afferent input.
Addressing Altered Cervical Afferent Input
Physical therapy interventions such as pain management, manipulative therapy, active range-of-motion exercises, and exercises to improve neuromuscular control will all be important in reducing possible causes of altered afferent cervical input and subsequent disturbances to sensorimotor control. Some physical interventions have been shown to improve aspects of sensorimotor deficits. For example, manipulative therapy has been shown to improve joint position sense and dizziness [46, 99, 105, 106]; specific neuromuscular control training [60] has improved cervical position sense; and cervical muscle endurance training has been suggested to improve balance. [120] Acupuncture has also been demonstrated to improve cervical joint position sense, vertigo, [46] and standing balance. [30] However, clinical experience suggests that this alone may not be sufficient nor the most efficient way of addressing all of the sensorimotor deficits. [56]
Addressing Secondary Adaptive Changes In The Sensorimotor Control System
Addressing any secondary effects on the visual and vestibular systems will also be important in the management of sensorimotor control disturbances in those with neck pain. [33, 51] This is where a tailored approach to sensorimotor control becomes important. There is evidence that specific treatment programs that have trained cervical joint position sense, eye-neck coordination, and gaze stability [60, 108, 124] have resulted in improvements not only in sensorimotor impairments but also improved neck pain and disability and range of motion. [108] Recently, a vestibular rehabilitation program improved balance and dizziness in patients with whiplash injury. [44] Again, it is unknown whether such an approach provided in isolation is able to address all of the deficits or is the most efficient approach.
Incorporating Manual Therapy/Exercises and Tailored Sensorimotor Control Approaches

Table 1 Intertwining manual therapy/exercises approaches with tailored sensorimotor control programs would seem an appropriate approach, as it will address the primary causes of the altered cervical afferent input as well as secondary adaptive changes. There is evidence that an exercise program combining manipulation, proprioceptive neuromuscular facilitation, acupressure on trigger points, and range-of-motion exercises, intertwined with exercises to improve head relocation accuracy, significantly improved the physical status of individuals with neck pain compared to a control neck pain group of similar patients treated with information and advice. [99] Recently, a pilot trial of a combined progam that used eye-neck coordination, balance, and task-dependent exercises, in conjunction with retraining the deep cervical flexors and position and movement sense (Table 1), demonstrated significant improvements in postural stability in those with chronic whiplash. [97]

Table 2

Table 3 A

Table 3 B However, research into the efficacy of such a broad, intertwining approach is in its infancy and the following guidelines for the intertwined treatment program are built on both available clinical research into this area and clinical experience. The specifics of such programs can be found in recent publications by Jull et al [59] and Treleaven. [131, 132] Table 2 summarizes an example of a typical approach for combining the tailored sensorimotor approach with other aspects of physical therapy treatment. Table 3 outlines specific tasks and progressions suggested for the tailored sensorimotor control program, although each individual's response and effort during a given intervention guides the treatment progression.
It is important that such a program does not produce an increase in pain or headache, but some temporary exacerbation of dizziness, nausea, unsteadiness, and/or visual disturbances is acceptable. The latter is acceptable to allow vestibular habituation. If pain or headache is exacerbated, the tasks can be attempted in more supported positions, such as in lying, with less repetitions of each task and a graduated introduction to each exercise. Each exercise should be performed at least once, preferably twice per day. Three to 5, building to 10, repetitions per exercise should be sufficient in most cases but can be less if a number of different exercises are required. Exercises should be performed at a speed and range of movement that allow the patient to perform with precision and continuous correction, gradually increasing speed and range as able. Exercises should also be performed in a position where precision is paramount, progressing to more difficult positions, such as tandem stance, on soft surface, etc.
The observed individuality in sensorimotor disturbances in patients with neck pain suggests that it may be important to develop specific rehabilitation programs for specific dysfunctions and to use objective and quantitative methods for evaluation of the effects of rehabilitation. [117] The primary sensorimotor deficits and the consequential compensatory mechanisms can vary in one patient with neck pain to another. [71] Good skills in clinical examination and clinical reasoning are, therefore, mandatory for effective management.
Specific Exercises for Use in the Tailored Sensorimotor Program
Neck Proprioception New advances in physical therapy indicate that principles of motor control [115] that address sensorimotor deficits in a more specific manner may be important for patients with complicated musculoskeletal problems. [61] Coordination of movements is a core term in motor control and can be defined as the sensorimotor processes that organize and activate large and small muscles with the optimal amount of force in the most efficient sequence. [96]
Currently, cervical joint position sense can be retrained using a laser pointer mounted onto a headband with the light projected onto a wall, as described in the section on assessment. Patients practice relocating the head to a neutral position (guided by the laser beam) from their most difficult movement directions (for example, rotation to the right or following neck extension). This can then be performed with the eyes closed, using the laser for feedback with the eyes open on completion of the task. The task can be progressed by asking the patient to relocate the head position to different points throughout the range of motion (eg, left rotation 20°, 40°, and 60°) rather than the neutral head position. Performing these activities in more challenging standing positions can also be used as a progression for the exercises.
Cervical movement sense can be improved by moving the head, thus moving the laser, to trace patterns placed on a wall such as a figure-of-eight pattern. Patients can practice performing the task as accurately as possible, keeping the laser on the lines of the pattern. In both exercises accuracy should be encouraged at the outset; but once this has been established, the patient can attempt to perform the activities as quickly and as accurately as possible.
More sophisticated computerized versions of retraining of neck proprioception, both position sense and movement sense, are currently being developed and designed to enhance treatment progression, with graduated levels of difficulty built into the programs. The training of neck position sense is aimed at better perception of body posture, dissociation between body parts, and better awareness of the body's position in space, especially improvement of the patients' awareness of the head-neck and shoulder girdle posture, and is dependent on proprioceptive, visual, auditory, and vestibular cues. In the training of movement sense by the new Fly Exercise Program the patient begins to use additional degrees of freedom by moving the cervical spine in larger ranges of movements and performing unpredictable, incrementally difficult movement patterns at different velocities.
Oculomotor Tasks Exercises to improve oculomotor control can be divided into exercises performed with the head stationary and while the head is moving. The exercises with the head stationary can be implemented at the same time as the exercises for improving head-neck awareness and cervical position sense. The oculomotor exercises performed while moving the head can be implemented at the same time as retraining cervical movement sense. Patients with severe neck pain may benefit by starting the treatment regime by just moving the eyes with the head stationary so as to avoid symptom exacerbation.
Smooth pursuit can be practiced by following a moving target with the eyes as accurately as possible, while keeping the head still. Performing this task in neck torsion positions will also be important to bias the cervical influence on the eyes.
Gaze stability can be practiced by focusing on a spot directly in front of the patient. The patient moves the head into movement directions of difficulty, maintaining optimal movement and range of motion, while fixating the gaze on the focus point. The patient can also move the trunk, or the therapist can passively move the trunk, while the patient maintains focus on the point ahead. These tasks can be progressed by altering the focus point (a word or group of words, such as a business card), the background behind the focus point (stripes or checks), the speed and range of the movement, restricting the peripheral vision (wearing goggles blackened out at the sides), and/or by altering the position the patient is in to perform the task (eg, standing instead of sitting).
Eye-head coordination can be practiced as it is assessed, with attention to correctly isolate eye and head movement and perform accurate cervical movement. These tasks can be progressed by using the eyes to follow arm and trunk movements. Saccades can be practiced by quickly moving the eyes from one point to another and refocusing. Again, these tasks can be progressed by altering the speed and range of the movement, restricting the peripheral vision (wearing goggles blackened-out at the sides), and/ or by altering the position the patient is in to perform the task (eg, standing instead of sitting).
Postural Stability Generally, dizziness is provoked with balance training. However, care and slow progression without extremes is vital for successful treatment in patients with whiplash and those with equilibrium disorders of cervical origin. [128] This is important, as patients with neck pain may react with compensatory increased muscle activity in the neck and other regions to achieve stabilization. This is ordinarly not a problem for patients with dizziness of noncervical origins; but for the patient with neck pain, such training may be harmful, as it leads to augmented neck muscle tension in already tensed neck muscles and a vicious circle of increased muscle activity and pain and altered cervical afferent input may develop, further exacerbating the cervicogenic dizziness. [128]
Attempts at sustaining static standing balance for up to 30 seconds can be practiced according to the extent of impairment found on the initial assessment. Progressions can be made by altering the stance position, closing the eyes, and/or altering the support surface, such as using a soft surface or an unstable surface such as a wobble board.
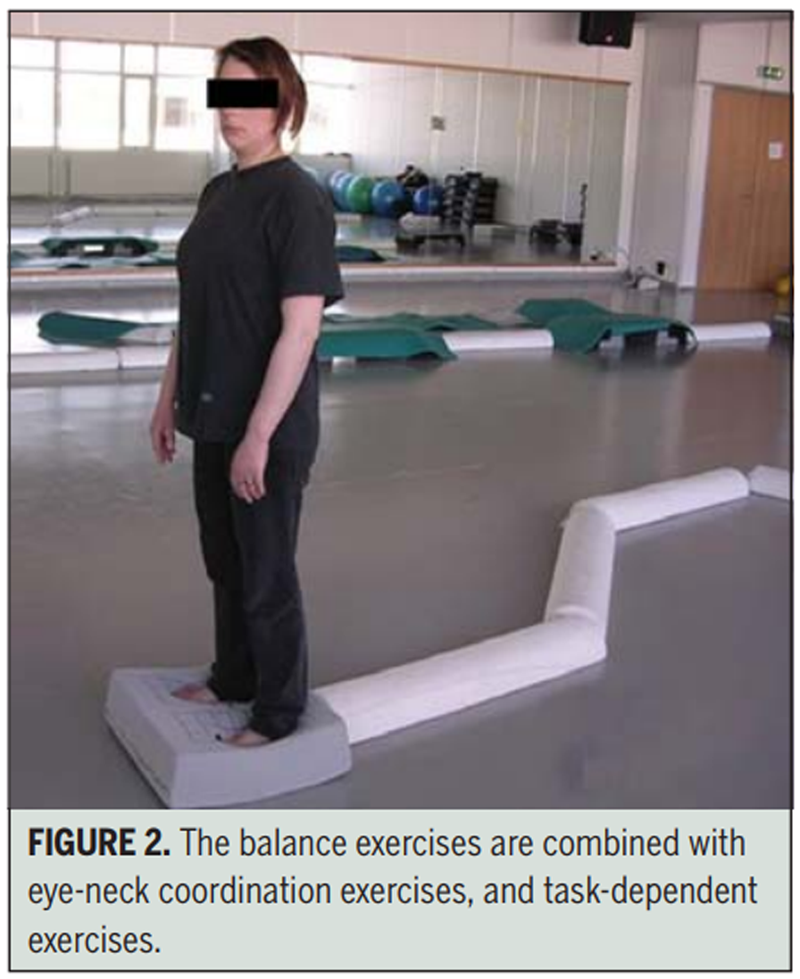
Figure 2
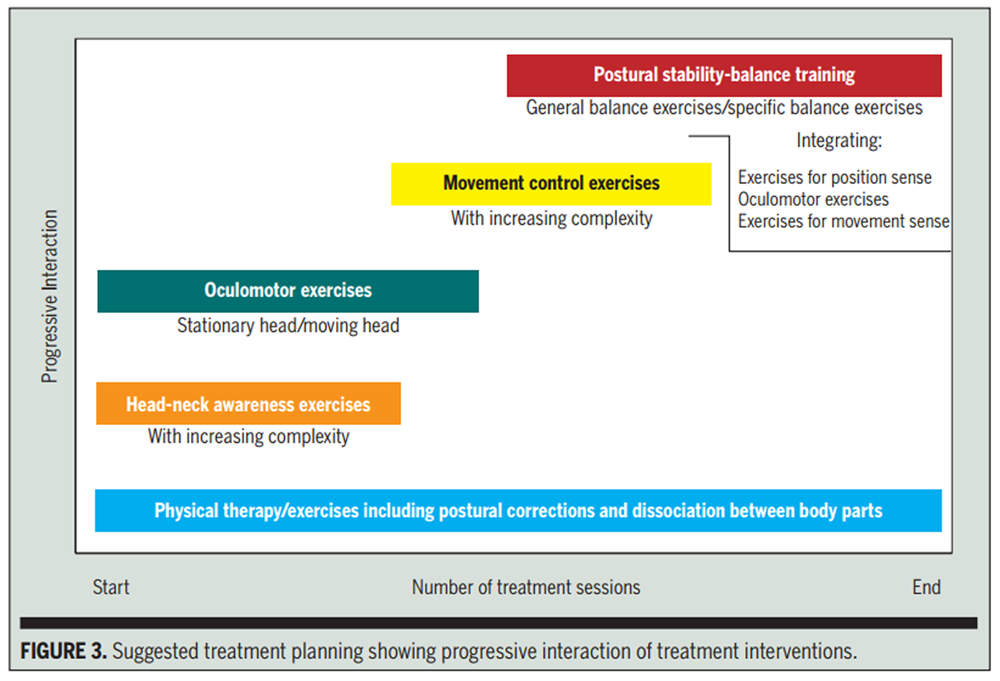
Figure 3 Functional and more dynamic tasks, such as walking with head turns to the left and right or up and down while maintaining the direction and velocity of walking, can also be incorporated depending on the level of impairment. This can be progressed by varying the walking surface and speed of the activity, as well as the walking task (Table 1, Figure 2).
Figure 3 provides a suggestion for the treatment planning for a patient with neck pain who, at the same time, has all the sensorimotor impairments that can possibly be of cervicogenic origin. Physical therapy/exercises are performed throughout the management to make favorable conditions for the sensorimotor training and to treat any compensatory reactions that may prevail after the sensorimotor exercises have been performed. Disturbed head-neck awareness, which requires normal range of motion, and oculomotor disturbances are then addressed before training of disturbed neck movement control. Normal oculomotor control is required before training of disturbed neck movement control, as the patient has to be able to follow the target (the Fly) by moving the head, using vision to appreciate the relative movements between the target (the Fly) and the cursor on the head, which follows the Fly on the computer screen. The same applies if a laser pointer is used to treat disturbed neck movement control. Disturbed postural stability—dizziness and/or unsteadiness, which may improve by implementing the aforementioned approaches first, is addressed at a later stage to minimize the commonly observed reactions of compensatory increased muscle activity in the neck and other regions to achieve stabilization when balance is challenged. The training of position sense, oculomotor control, and movement sense is integrated into the balance exercise program to enhance modulation of the sensorimotor circuits in the CNS and to make the balance exercises progressively more difficult.
REFERENCES:
Alund M, Ledin T, Odkvist L, Larsson SE. Dynamic posturography among patients with common neck disorders. A study of 15 cases With suspected cervical vertigo. J Vestib Res. 1993; 3: 383– 389.
Anderson G. Epidemiology of spinal disorders. In: Frymoyer J, ed. The Adult Spine. New York, NY: Raven Press; 1991: 107– 146.
Ashton-Miller J, Schultz A. Spine instability and segmental hypermobility biomechanics: a call for definition and standard use of terms. Semin Spine Surg. 1991; 3: 136– 148.
Baloh R, Halmagyi G. Disorders of the Vestibular System. New York, NY: Oxford University Press; 1996.
Bexander CS, Mellor R, Hodges PW. Effect of gaze direction on neck muscle activity during cervical rotation. Exp Brain Res. 2005; 167: 422– 432
Björklund M. Effects of Repetitive Work on Proprioception and of Stretching on Sensory Mechanisms: Implications for Work-Related Neuromuscular Disorders [dissertation] . Umeå, Sweeden: Umeå University; 2004.
Bogduk N, Mercer S. Biomechanics of the cervical spine. I: Normal kinematics. Clin Biomech (Bristol, Avon). 2000; 15: 633– 648.
Bohannon RW. Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age Ageing. 1997; 26: 15– 19.
Bove M, Courtine G, Schieppati M. Neck muscle vibration and spatial orientation during stepping in place in humans. J Neurophysiol. 2002; 88: 2232– 2241
Brandt T. Vertigo: Its Multisensory Syndromes. 1st ed. London, UK: Springer-Verlag; 1991.
Bränström H, Malmgren-Olsson E, Bernekow-Bergkvist M. Balance performance in patients with whiplas associated disorders and patients with prolonged musculoskeletal disorders. Advances in Physiother. 2001; 3: 120– 127
Brison RJ, Hartling L, Pickett W. A prospective study of acceleration-extension injuries following rear-end motor vehicle collisions. J Musculoskeletal Pain. 2000; 8: 97– 113
Buskila D, Neumann L. The development of widespread pain after injuries. J Musculoskeletal Pain. 2002; 10: 261– 267.
Buskila D, Neumann L, Vaisberg G, Alkalay D, Wolfe F. Increased rates of fibromyalgia following cervical spine injury. A controlled study of 161 cases of traumatic injury. Arthritis Rheum. 1997; 40: 446– 452.
Cholewicki J, Panjabi MM, Khachatryan A. Stabilizing function of trunk flexor-extensor muscles around a neutral spine posture. Spine. 1997; 22: 2207– 2212.
Clendaniel R. Cervical Vertigo. In: Herdman S, ed. Vestibular Rehabilitation. Philadelphia, PA: FA Davis Co; 2000: 494– 509.
Corneil BD, Olivier E, Munoz DP. Neck muscle responses to stimulation of monkey superior colliculus. I. Topography and manipulation of stimulation parameters. J Neurophysiol. 2002; 88: 1980– 1999
Courtine G, Papaxanthis C, Laroche D, Pozzo T. Gait-dependent integration of neck muscle afferent input. Neuroreport. 2003; 14: 2365– 2368.http://dx.doi.org/10.1097/01.wnr.0000091300.11924.89
Dai L. Disc degeneration and cervical instability. Correlation of magnetic resonance imaging with radiography. Spine. 1998; 23: 1734– 1738.
Davis C. Chronic pain/dysfunction in whiplash-associated disorders. J Manipulative Physiol Ther. 2001; 24: 44– 51
Duclos C, Roll R, Kavounoudias A, Roll JP. Long-lasting body leanings following neck muscle isometric contractions. Exp Brain Res. 2004; 158: 58– 66
Dutia MB. The muscles and joints of the neck: their specialisation and role in head movement. Prog Neurobiol. 1991; 37: 165– 178.
Edney DP, Porter JD. Neck muscle afferent projections to the brainstem of the monkey: implications for the neural control of gaze. J Comp Neurol. 1986; 250: 389– 398
Elert J, Kendall SA, Larsson B, Mansson B, Gerdle B. Chronic pain and difficulty in relaxing postural muscles in patients with fibromyalgia and chronic whiplash associated disorders. J Rheumatol. 2001; 28: 1361–1368
Elliott J, Jull G, Noteboom JT, Darnell R, Galloway G, Gibbon WW. Fatty infiltration in the cervical extensor muscles in persistent whiplash-associated disorders: a magnetic resonance imaging analysis. Spine. 2006;31:E847–855
Falla D, Bilenkij G, Jull G. Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine. 2004;29:1436–1440.
Falla D, Jull G, Hodges PW. Feedforward activity of the cervical flexor muscles during voluntary arm movements is delayed in chronic neck pain. Exp Brain Res. 2004; 157: 43– 48.http://dx.doi.org/10.1007/s00221-003-1814-9
Falla DL. Unravelling the complexity of muscle impairment in chronic neck pain. Man Ther. 2004; 9: 125– 133.
Falla DL, Jull G, Dall'Alba P, Rainoldi A, Merletti R. An electromyographic analysis of the deep cervical flexor muscles in performance of craniocervical flexion. Phys Ther. 2003; 83: 899– 906
Fattori B, Borsari C, Vannucci G, et al. Acupuncture treatment for balance disorders following whiplash injury. Acupunct Electrother Res. 1996; 21: 207– 217.
Field S, Treleaven J, Jull G. Standing balance: a comparison between idiopathic and whiplash induced neck pain. Man Ther. 2008; 13: 183– 191.http://dx.doi.Org/10.1016/j.math.2006.12.005
Fischer AJ, Huygen PL, Folgering HT, Verhagen WI, Theunissen EJ. Vestibular hyperreactivity and hyperventilation after whiplash injury. J Neurol Sci. 1995; 132: 35– 43.
Fischer AJ, Verhagen Wl, Huygen PL. Whiplash injury. A clinical review with emphasis on neurootological aspects. Clin Otolaryngol Allied Sci. 1997; 22: 192– 201.
Flor H. Cortical reorganisation and chronic pain: implications for rehabilitation. J Rehabil Med. 2003;66–72.
Frobin W, Leivseth G, Biggemann M, Brinckmann P. Sagittal plane segmental motion of the cervical spine. A new precision measurement protocol and normal motion data of healthy adults. Clin Biomech (Bristol, Avon). 2002; 17: 21– 31.
Ghez C, Sainburg R. Proprioceptive control of interjoint coordination. Can J Physiol Pharmacol. 1995; 73: 273– 284.
Gimse R, Bjorgen IA, Tjell C, Tyssedal JS, Bo K. Reduced cognitive functions in a group of whiplash patients with demonstrated disturbances in the posture control system. J Clin Exp Neuropsychol. 1997; 19: 838– 849.
Gimse R, Tjell C, Bjorgen IA, Saunte C. Disturbed eye movements after whiplash due to injuries to the posture control system. J Clin Exp Neuropsychol. 1996; 18: 178– 186.
Gosselin G, Rassoulian H, Brown I. Effects of neck extensor muscles fatigue on balance. Clin Biomech (Bristol, Avon). 2004; 19: 473– 479.http://dx.doi.Org/10.1016/j.clinbiomech.2004.02.001
Grip H, Jull G, Treleaven J. Head eye co-ordination using simultaneous measurement of eye in head and head in space movements: potential for use in subjects with a whiplash injury. J Clin Mon Computing. 2009; 23: 31– 40.
Guez M, Hildingsson C, Nilsson M, Toolanen G. The prevalence of neck pain: a population-based study from northern Sweden. Acta Orthop Scand. 2002; 73: 455– 459.
Guitton D, Kearney RE, Wereley N, Peterson BW. Visual, vestibular and voluntary contributions to human head stabilization. Exp Brain Res. 1986; 64: 59– 69.
Guyton AC. Textbook of Medical Physiology. 8th ed. Philadelphia, PA: W.B. Saunders Company; 1991.
Hansson EE, Mansson NO, Ringsberg KA, Hakansson A. Dizziness among patients with whiplash-associated disorder: a randomized controlled trial. J Rehabil Med. 2006; 38: 387– 390.http://dx.doi.org/10.1080/16501970600768992
Heikkila H, Astrom PG. Cervicocephalic kinesthetic sensibility in patients with whiplash injury. Scand J Rehabil Med. 1996; 28: 133– 138
Heikkilä H. , Johansson M. and Wenngren B.I.
Effects of Acupuncture, Cervical Manipulation and NSAID Therapy on
Dizziness and Impaired Head Repositioning of Suspected Cervical Origin:
A Pilot Study
Manual Therapy 2000 (Aug); 5 (3): 151–157Heikkila HV, Wenngren Bl. Cervicocephalic kinesthetic sensibility, active range of cervical motion, and oculomotor function in patients with whiplash injury. Arch Phys Med Rehabil. 1998; 79: 1089– 1094.
Herdman S. Vestibular Rehabilitation. 2nd ed. Philadelphia, PA: Davis; 2000.
Herdman SJ, Tusa RJ, Blatt R, Suzuki A, Venuto PJ, Roberts D. Computerized dynamic visual acuity test in the assessment of vestibular deficits. Am J Otol. 1998; 19: 790– 796
Highstein H. How does the vestibular part of the inner ear work?In: Baloh R, Halmagyi G, eds. Disorder of the Vestibular System. New York, NY: Oxford University Press; 1996.
Hikosaka O, Maeda M. Cervical effects on abducens motoneurons and their interaction with vestibulo-ocular reflex. Exp Brain Res. 1973; 18: 512– 530.
Hildingsson C, Toolanen G. Outcome after softtissue injury of the cervical spine. A prospective study of 93 car-accident victims. Acta Orthop Scand. 1990; 61: 357– 359.
Hildingsson C, Wenngren Bl, Bring G, Toolanen G. Oculomotor problems after cervical spine injury. Acta Orthop Scand. 1989; 60: 513– 516.
Hill K, Bernhardt J, McGann A, Maltese D, Berkovits D. A new test of dynamic standing balance for stroke patients: reliability, validity and comparison with healthy elderly. Physiother Can. 1996; 48: 257– 262
Hinoki M. Vertigo due to whiplash injury: a neurotological approach. Acta Otolaryngol Suppl. 1984; 419: 9– 29
Horak F, Macpherson J. Postural orientation and equilibrium. In: Rowell LB, Shepherd JT, eds. Section 12, Exercise: Regulation and Integration of Multiple Systems. New York, NY: Oxford University Press, Inc; 1996: 255– 292.
Hülse M. Klinik der funktionsstörungen des kopfgelengbereichs. In: Hülse M, Neuhuber WL, Wolff HD, eds. Der Kranio-Zervikale Übergang. Berlin, Germany: Springer; 1998 : 43– 97
Hülse M, Holzl M. [Vestibulospinal reactions in cervicogenic disequilibriumCervicogenic imbalance]. HNO. 2000; 48: 295– 301.376
Jull G, Falla D, Treleavan J, Sterling M, O'Leary S. A therapeutic exercise approach for cervical disorders. In: Boyling JD, Jull G, eds. Grieve's Modern Manual Therapy. The Vertebral Column. Edinburgh, UK: Churchill Livingstone; 2004: 451– 469.
Jull G, Falla D, Treleaven J, Hodges R, Vicenzino B. Retraining cervical joint position sense: the effect of two exercise regimes. J Orthop Res. 2007; 25: 404– 412.http://dx.doi.org/10.1002/jor.20220
Jull G, Sterling M, Falla D, Treleaven J, O'Leary S. Whiplash, Headache, and Neck Pain: Research-Based Directions for Physical Therapies. Edinburgh, UK: Elsevier; 2008.
Jull GA. Deep cervical flexor muscle dysfunction in whiplash. J Musculoskel Pain. 2000;8:143–154
Kajewski H, Poole E, LowChoy N. Does idiopathic neck pain affect balance and mobility in community dwelling adults aged 65 and over? Aust J on Ageing.[In review].
Karlberg M. The Neck and Human Balance: A Clinical and Experimental Approach to “Cervical Vertigo” [dissertation]. Lund, Sweden: University Hospital of Lund; 1995.
Karlberg M, Johansson R, Magnusson M, Fransson PA. Dizziness of suspected cervical origin distinguished by posturographic assessment of human postural dynamics. J Vestib Res. 1996; 6: 37– 47.
Karlberg M, Magnusson M, Johansson R. Effects of restrained cervical mobility on voluntary eye movements and postural control. Acta Otolaryngol. 1991; 111: 664– 670.
Karlberg M, Magnusson M, Malmstrom EM, Melander A, Moritz U. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Arch Phys Med Rehabil. 1996; 77: 874– 882.
Karlberg M, Persson L, Magnusson M. Impaired postural control in patients with cervicobrachial pain. Acta Otolaryngol Suppl. 1995;520 Pt 2: 440– 442
Karnath HO, Reich E, Rorden C, Fetter M, Driver J. The perception of body orientation after neckproprioceptive stimulation. Effects of time and of visual cueing. Exp Brain Res. 2002; 143: 350– 358.http://dx.doi.org/10.1007/s00221-001-0996-2
Kelders WP, Kleinrensink GJ, van der Geest JN, et al. The cervico-ocular reflex is increased in whiplash injury patients. J Neurotrauma. 2005; 22: 133– 137.http://dx.doi.org/10.1089/neu.2005.22.133
Kristjansson E. The cervical spine and proprioception. In: Boyling JD, Jull G, eds. Grieve's Modern Manual Therapy. London, UK: Churchill Livingstone; 2004: 243– 256.
Kristjansson E. Reliability of ultrasonography for the cervical multifidus muscle in asymptomatic and symptomatic subjects. Man Ther. 2004; 9: 83– 88.http://dx.doi.org/10.1016/S1356-689X(03)00059-6
Kristjansson E, Dall'Alba P, Jull G. A study of five cervicocephalic relocation tests in three different subject groups. Clin Rehabil. 2003;17:768–774.
Kristjansson E, Hardardottir L, Asmundardottir M, Gudmundsson K. A new clinical test for cervicocephalic kinesthetic sensibility: “the fly”. Arch Phys Med Rehabil. 2004; 85: 490– 495.
Kristjansson E, Jonsson H. Symptom characteristics in women with chronic WAD, grades I-II, and chronic insidious onset neck pain. J Whiplash and Rel Disorders. 2004; 3: 3– 17
Kristjansson E, Leivseth G, Brinckmann P, Frobin W. Increased sagittal plane segmental motion in the lower cervical spine in women with chronic whiplash-associated disorders, grades I-II: a case-control study using a new measurement protocol. Spine. 2003;28:2215–2221. http://dx.doi.org/10.1097/01.BRS.0000089525.59684.49
Kulkarni V, Chandy MJ, Babu KS. Quantitative study of muscle spindles in suboccipital muscles of human foetuses. Neurol India. 2001; 49: 355– 359
Le Pera D, Graven-Nielsen T, Valeriani M, et al. Inhibition of motor system excitability at cortical and spinal level by tonic muscle pain. Clin Neurophysiol. 2001; 112: 1633– 1641.
Lennerstrand G, Han Y, Velay JL. Properties of eye movements induced by activation of neck muscle proprioceptors. Graefes Arch Clin Exp Ophthalmol. 1996; 234: 703– 709.
Liu JX, Thornell LE, Pedrosa-Domellof F. Muscle spindles in the deep muscles of the human neck: a morphological and immunocytochemical study. J Histochem Cytochem. 2003;51:175–186.
Loudon JK, Ruhl M, Field E. Ability to reproduce head position after whiplash injury. Spine. 1997; 22: 865– 868.
Lovell ME, Galasko CS. Whiplash disorders— a review. Injury. 2002; 33: 97– 101.
LowChoy NL, Johnson N, Treleaven J, Jull G, Panizza B, Brown-Rothwell D. Balance, mobility and gaze stability deficits remain following surgical removal of vestibular schwannoma (acoustic neuroma): an observational study. Aust J Physiother. 2006; 52: 211– 216.
Madeleine R, Prietzel H, Svarrer H, Arendt-Nielsen L. Quantitative posturography in altered sensory conditions: a way to assess balance instability in patients with chronic whiplash injury. Arch Phys Med Rehabil. 2004; 85: 432– 438.
Mayoux-Benhamou MA, Revel M, Vallee C, Roudier R, Barbet JP, Bargy F. Longus colli has a postural function on cervical curvature. Surg Radiol Anat. 1994; 16: 367– 371.
McCrea DA. Spinal cord circuitry and motor reflexes. Exerc Sport Sci Rev. 1986; 14: 105– 141.
McLain RF. Mechanoreceptor endings in human cervical facet joints. Spine . 1994; 19: 495– 501.
McPartland JM, Brodeur RR, Hallgren RC. Chronic neck pain, standing balance, and suboccipital muscle atrophy--a pilot study. J Manipulative Physiol Ther. 1997; 20: 24– 29
Mergner T, Rosemeier T. Interaction of vestibular, somatosensory and visual signals for postural control and motion perception under terrestrial and microgravity conditions--a conceptual model. Brain Res Brain Res Rev. 1998; 28: 118– 135.
Michaelson P, Michaelson M, Jaric S, Latash ML, Sjolander P, Djupsjöbacka M. Vertical posture and head stability in patients with chronic neck pain. J Rehabil Med. 2003; 35: 229– 235.
Montfoort I, Kelders WP, van der Geest JN, et al. Interaction between ocular stabilization reflexes in patients with whiplash injury. Invest Ophthalmol Vis Sci. 2006; 47: 2881– 2884.http://dx.doi.org/10.1167/iovs.05-1561
Montfoort I, Van Der Geest JN, Slijper HR, De Zeeuw CI, Frens MA. Adaptation of the cervico-and vestibulo-ocular reflex in whiplash injury patients. J Neurotrauma. 2008; 25: 687– 693.http://dx.doi.org/10.1089/tieu.2007.0314
Neuhuber WL. [Characteristics of the innervation of the head and neck]. Orthopäde. 1998; 27: 794– 801
Neuhuber WL. Der kraniozervikale ubergang: entwicklung, gelenke, muskulatur und innervation. ln: Hülse M, Neuhuber WL, Wolff HD, eds. Der Kranio-Zervikale Übergang. Berlin, Germany: Springer; 1998: 11– 31
Neuhuber WL, Bankoul S. Der “halsteil” des gleichgewichtsapparate-verbindungen zervikaler rezeptoren zu vestibulariskemen. Manuelle Medizine. 1992; 30: 53– 57.
Newell KM. Coordination, control, and skill. In: Goodman D, Wilberg RB, Franks IM, eds. Differing Perspectives in Motor Learning, Memory, and Control. Amsterdam, The Netherlands: Elsevier Science Publishers; 1985.
Oddsdottir G. Cervical Induced Balance Disturbances After Motor Vehicle Collisions: The Efficacy of Two Successive Physical Treatment Approaches [thesis]. Reykjavik, Iceland: University of Iceland; 2006.
Owens EF, Jr., Henderson CN, Gudavalli MR, Pickar JG. Head repositioning errors in normal student volunteers: a possible tool to assess the neck's neuromuscular system. Chiropr Osteopat. 2006; 14: 5– .http://dx.doi.org/10.1186/1746-1340-14-5
Palmgren PJ, Sandstrom PJ, Lundqvist FJ, Heikkila H.
Improvement After Chiropractic Care in Cervicocephalic Kinesthetic
Sensibility and Subjective Pain Intensity in Patients
with Nontraumatic Chronic Neck Pain
J Manipulative Physiol Ther 2006 (Feb); 29 (2): 100–106Panjabi MM, Lydon C, Vasavada A, Grob D, Crisco JJ, 3rd, Dvorak J. On the understanding of clinical instability. Spine. 1994; 19: 2642– 2650.
Passatore M, Roatta S. Influence of sympathetic nervous system on sensorimotor function: whiplash associated disorders (WAD) as a model. Eur J Appl Physiol. 2006; 98: 423– 449.http://dx.doi.org/10.1007/s00421-006-0312-8
Peterson BW. Current approaches and future directions to understanding control of head movement. Prog Brain Res. 2004; 143: 369– 381
Peterson BW, Goldberg J, Bilotto G, Fuller JH. Cervicocollic reflex: its dynamic properties and 377 interaction with vestibular reflexes. J Neurophysiol. 1985; 54: 90– 109
Poole E, Treleaven J, Jull G. The influence of neck pain on balance and gait parameters in community-dwelling elders. Man Ther. 2008; 13: 317– 324.http://dx.doi.Org/10.1016/j.math.2007.02.002
Reid S, Rivett D.
Manual Therapy Treatment of Cervicogenic Dizziness: A Systematic Review
Man Ther. 2005 (Feb); 10 (1): 4–13Reid SA, Rivett DA, Katekar MG, Callister R. Sustained natural apophyseal glides (SNAGs) are an effective treatment for cervicogenic dizziness. Man Ther. 2008; 13: 357– 366.http://dx.doi.org/10.1016/j.math.2007.03.006
Revel M, Andre-Deshays C, Minguet M. Cervicocephalic kinesthetic sensibility in patients with cervical pain. Arch Phys Med Rehabil. 1991; 72: 288– 291
Revel M, Minguet M, Gregoy P, Vaillant J, Manuel JL. Changes in cervicocephalic kinesthesia after a proprioceptive rehabilitation program in patients with neck pain: a randomized controlled study. Arch Phys Med Rehabil. 1994;75:895–899.
Richmond FJ, Bakker DA. Anatomical organization and sensory receptor content of soft tissues surrounding upper cervical vertebrae in the cat. J Neurophysiol. 1982; 48: 49– 61
Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train. 2002; 37: 71– 79
Roren A, Mayoux-Benhamou MA, Fayad F, Poiraudeau S, Lantz D, Revel M. Comparison of visual and ultrasound based techniques to measure head repositioning in healthy and neckpain subjects. Man Ther. 2008;http://dx.doi.org/10.1016/j.math.2008.03.002
Rubin AM, Woolley SM, Dailey VM, Goebel JA. Postural stability following mild head or whiplash injuries. Am J Otol. 1995; 16: 216– 221.
Schieppati M, Nardone A, Schmid M. Neck muscle fatigue affects postural control in man. Neuroscience. 2003; 121: 277– 285.
Schmid M, Schieppati M. Neck muscle fatigue and spatial orientation during stepping in place in humans. J Appl Physiol. 2005; 99: 141– 153.http://dx.doi.org/10.1152/japplphysiol.00494.2004
Shumway-Cook A, Woollacott MH. Motor Control: Theory and Practical Aplications. 2nd ed. Baltimore, MD: Lipincott Williams & Wilkins; 2001.
Sjolander P, Johansson H, Djupsjobacka M. Spinal and supraspinal effects of activity in ligament afferents. J Electromyogr Kinesiol. 2002; 12: 167– 176.
Sjölander P, Michaelson P, Jaric S, Djupsjobacka M. Sensorimotor disturbances in chronic neck pain--range of motion, peak velocity, smoothness of movement, and repositioning acuity. Man Ther. 2008; 13: 122– 131.http://dx.doi.org/10.1016/j.math.2006.10.002
Sjöstrom H, Allum JH, Carpenter MG, Adkin AL, Honegger E, Ettlin T. Trunk sway measures of postural stability during clinical balance tests In patients with chronic whiplash injury symptoms. Spine. 2003; 28: 1725– 1734.http://dx.doi.org/10.1097/01.BRS.0000083170.34304.A3
Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Stapley PJ, Beretta MV, Dalla Toffola E, Schieppati M. Neck muscle fatigue and postural control in patients with whiplash injury. Clin Neurophysiol. 2006; 117: 610– 622.http://dx.doi.org/10.1016/j.clinph.2005.11.007
Stein JF, Glickstein M. Role of the cerebellum In visual guidance of movement. Physiol Rev. 1992; 72: 967– 1017
Sterling M, Jull G, Vicenzino B, Kenardy J, Darnell R. Development of motor system dysfunction following whiplash injury. Pain. 2003; 103: 65– 73.
Stewart MJ, Maher CG, Refshauge KM, Herbert RD, Bogduk N, Nicholas M. Randomized controlled trial of exercise for chronic whiplashassociated disorders. Pain. 2007; 128: 59– 68.http://dx.doi.Org/10.1016/j.pain.2006.08.030
Storaci R, Manelli A, Schiavone N, Mangia L, Prigione G, Sangiorgi S. Whiplash injury and oculomotor dysfunctions: clinical-posturographic correlations. Eur Spine J. 2006; 15: 1811– 1816.http://dx.doi.org/10.1007/s00586-006-0085-0
Szpalski M. The mysteries of segmental instability. Bull Hosp Jt Dis. 1996; 55: 147– 148
Taylor JL, McCloskey DI. Illusions of head and visual target displacement induced by vibration of neck muscles. Brain. 1991;114(Pt 2):755–759.
Thunberg J, Hellstrom E, Sjölander R, Bergenheim M, Wenngren B, Johansson H. Influences on the fusimotor-muscle spindle system from chemosensitive nerve endings in cervical facet joints in the cat: possible implications for whiplash induced disorders. Pain. 2001; 91: 15– 22.
Tjell C, Hailing Wl, Tenenbaum A. Why do not all recover after a whiplash injury? A hypothesis from an otoneurologic viewpoint. J Whiplash Rel Disorders. 2007; 5: 7– 23
Tjell C, Rosenhall U. Smooth pursuit neck torsion test: a specific test for cervical dizziness. Am J Otol. 1998; 19: 76– 81
Tjell C, Tenenbaum A, Sandstrom S. Smooth pursuit neck torsion test: a specific test for whiplash associated disorders? J Whiplash Rel Disorders. 2002; 1: 9– 24
Treleaven J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man Ther. 2008; 13: 2– 11.http://dx.doi.Org/10.1016/j.math.2007.06.003
Treleaven J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control-Part 2: case studies. Man Ther. 2008; 13: 266– 275.http://dx.doi.org/10.1016/j.math.2007.11.002
Treleaven J, Jull G, LowChoy N. The relationship of cervical joint position error to balance and eye movement disturbances in persistent whiplash. Man Ther. 2006; 11: 99– 106.http://dx.doi.org/10.1016/j.math.2005.04.003
Treleaven J, Jull G, LowChoy N. Smooth pursuit neck torsion test in whiplash-associated disorders: relationship to self-reports of neck pain and disability, dizziness and anxiety. J Rehabil Med. 2005; 37: 219– 223.http://dx.doi.org/10.1080/16501970410024299
Treleaven J, Jull G, Lowchoy N. Standing balance in persistent whiplash: a comparison between subjects with and without dizziness. J Rehabil Med. 2005; 37: 224– 229.http://dx.doi.org/10.1080/16501970510027989
Treleaven J, Jull G, Sterling M. Dizziness and unsteadiness following whiplash injury: characteristic features and relationship with cervical joint position error. J Rehabil Med. 2003; 35: 36– 43.
Treleaven J, LowChoy N, Darnell R, Panizza B, Brown-Rothwell D, Jull G. Comparison of sensorimotor disturbance between subjects with persistent whiplash-associated disorder and subjects with vestibular pathology associated with acoustic neuroma. Arch Phys Med Rehabil. 2008; 89: 522– 530.http://dx.doi.org/10.10167j.apmr.2007.11.002
Treleaven J, Murison R, Jull G, LowChoy N, Brauer S. Is the method of signal analysis and test selection important for measuring standing balance in subjects with persistent whiplash? Gait Posture. 2005; 21: 395– 402.http://dx.doi.org/10.1016/j.gaitpost.2004.04.008
Uhlig Y, Weber BR, Grob D, Muntener M. Fiber composition and fiber transformations in neck muscles of patients with dysfunction of the cervical spine. J Orthop Res. 1995; 13: 240– 249.http://dx.doi.org/10.1002/jor.1100130212
Vuillerme N, Pinsault N, Vaillant J. Postural control during quiet standing following cervical muscular fatigue: effects of changes in sensory inputs. Neurosci Lett. 2005; 378: 135– 139.http://dx.doi.org/10.1016/j.neulet.2004.12.024
Wenngren Bl, Pettersson K, Lowenhielm G, Hildingsson C. Eye motility and auditory brainstem response dysfunction after whiplash injury. Acta Otolaryngol. 2002; 122: 276– 283.
Windhorst U, Kokkoroyiannis T. Dynamic behaviour of alpha-motoneurons subjected to recurrent inhibition and reflex feedback via muscle spindles. Neuroscience. 1992; 47: 897– 907.
Wolff HD. Neurophysiologische Aspekte des Bewegungssystems. Berlin, Germany: Springer; 1996
Wrisley DM, Marchetti GF, Kuharsky DK, Whitney SL. Reliability, internal consistency, and validity of data obtained with the functional gait assessment. Phys Ther. 2004; 84: 906– 918
Yamagata Y, Yates BJ, Wilson VJ. Participation of Ia reciprocal inhibitory neurons in the spinal circuitry of the tonic neck reflex. Exp Brain Res. 1991; 84: 461– 464.

Return to CHRONIC NECK PAIN
Return to VERTIGO and BALANCE
Since 7–02–2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |