

|
). The transverse processes, which arise at the junction of the pedicles and laminae, project laterally and slightly backwards and increase in length progressing caudally. The neural ring is triangular, and the vertebral canal is larger than that of the thoracic spine but smaller than that of the cervical spine.Chapter 5:
The Lumbar Spine
From R. C. Schafer, DC, PhD, FICC's best-selling book:
“Motion Palpation”
Second Edition ~ The Motion Palpation Institute & ACAPress
The following materials are provided as a service to our profession. There is no charge for individuals to copy and file these materials. However, they cannot be sold or used in any group or commercial venture without written permission from ACAPress.
All of Dr. Schafer's books are now available on CDs, with all proceeds being donated
to chiropractic research. Please review the complete list of available books.Basic Considerations The Interview Applied Anatomical Considerations Biomechanical Considerations Kinematics of the Lumbar Spine Diagnostic Considerations Significant Neurologic and Orthopedic Tests Lumbar Fixations Motion Palpation of the Lumbar Spine Applied Roentgenography Differential Diagnosis Therapeutic Approach Adjusting Lumbar Fixations Integrated Treatment Approach Motion Palpation on a Mobile Adjusting Table Closing Remarks Bibliography
The Lumbar Vertebrae
Because vertebral segments increase in size and strength progressing caudally to sustain increasing weight load, the lumbar vertebra are relatively large (Fig. 5.1). The centra are kidney shaped, larger in width than from front to back, and thicker anteriorly (except L2). A line crossing horizontally at the uppermost aspect of the iliac crests normally cuts the body of L4.
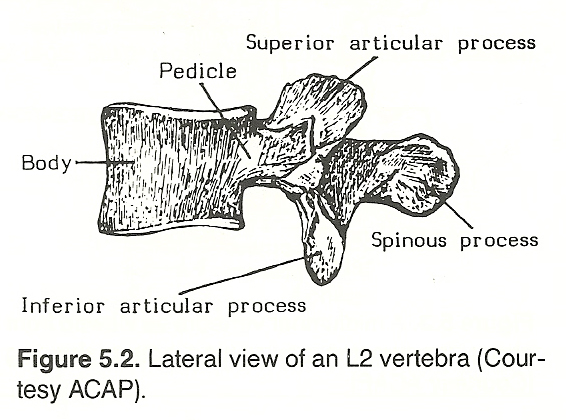
Each lumbar vertebra exhibits strong stout laminae, pedicles, and spinous processes that project directly backward on a horizontal plane (Fig. 5.2
 |
There are about twice as many sensory fibers than motor fibers in the lumbar roots. When the anterior nerve root is irritated, pain is felt in the
peripheral distribution of the fibers affected and the pain often becomes
self-perpetuating from the focal spasm produced. When the posterior root is
irritated, the pain can be perceived to be in the dermatome, myotome, sclerotome, or possibly the viscerotome.
Planes of Articulation in the Lumbar Spine (Normal and Abnormal)
Lumbar facets have moderately sloped surfaces rather than a single-plane
angle as seen in the cervical and thoracic area, and they are near parallel to
the vertical plane. The convex inferior facets mate with concave superior
facets. From L1 to L5, the plane of the articular facets generally change from
mediolateral to anteroposterior and lie in the sagittal plane.
The lumbosacral facet planes are slightly more horizontal than those above
and allow greater A-P, P-A, and lateral motion but less joint locking as compared to the vertebrae above. This horizontal and anterior inclination of L5,
spreading out toward the coronal plane, becomes progressively more vertical
upward from L4 to L1.
An important influence on interspinal posture is that of the facet facing
of each posterior intervertebral joint, with alterations of the facings most
commonly occurring in the lumbar and lower cervical regions. These facings are
more frequently altered between L4 and L5 than at any other level in the
vertebral column.
Symmetric facets glide with little friction produced. If the facets
deviate in their direction of movement, however, the unparallel articulating
surfaces "scrub" upon one another, which leads to degenerative changes. Variances of the articular structures often occur even in the absence of injury at
the level of abnormality. They are characterized by thickening of the covering
of the facet and marginal sclerosis. This hardening process is usually followed by hypertrophy or exostosis that produces an irregular articular surface
when the facet is viewed in profile in roentgenography. Coexistent with this
finding, the interarticular spaces gradually become narrowed, hazy, obscured,
and even obliterated on x-ray films.
Because these various facet and interarticular manifestations are from
either chronic abnormal weight-bearing or specific trauma, the term arthrosis
is often used today rather than the phrase posterior intervertebral osteoarthritis. Arthrosis is a more reasonable descriptor because of the implications
of the suffix "itis." Although there may not be evidence of direct bony encroachment from the process of arthrosis directly into the IVFs, one must consider that the process of arthrosis does produce a general narrowing of the
diameters of the IVFs and hence can predispose interference with the normal
expression of nerve impulse and axoplasmic flow transmission.
When the spine is in good postural balance, facet articulation offers
minimal friction. In scoliosis, the articular surfaces are no longer parallel
and the result is articular friction leading to erosion, arthrosis, and
impingement. This is the result of normally reciprocal articulating surfaces
operating in an abnormal relationship.
Biomechanical Considerations
From the middle of the anterior surface of T12, the body's gravity line
extends downward to the anterior aspect of the sacral base. Weight distribution in the lumbar region is governed chiefly by the inclination of each vertebral body. The lumbosacral articulations are slightly more horizontal than
those above them, allowing for greater P-A and lateral motion and offering
less joint locking during extension as compared to the vertebrae above.
The horizontal inclination of L5, spreading out toward the coronal plane,
becomes progressively more vertical from L4 to L1 as the dorsolumbar articulation is approached. These changes in articular planes allow the lower back to
bend and twist to accommodate gravitational force during movement. The upper
lumbar joints are J-shaped when viewed from the lateral, thus their anterior
aspect resists forward displacement.
The lateral center line of gravity falls on different points in the lumbar
spine because of gradual changes in the angles of the inclined planes of the
various articular surfaces. This tends to force each lumbar segment more
inferior, medial, and anterior or posterior until gravity brings the apex of
the curve back toward the balancing point. The lateral line of gravity in the
pelvic area passes just anteriorly to the S2 segment.
Except for the lesser role of the pelvic basin, superimposed body weight
is carried in the lower back essentially by the L5 disc and then dispersed to
the sacral base, sacroiliac joints, and acetabulae. This burden on the L5 disc
is forced slightly forward on the load-bearing surfaces. Defective weight
bearing is usually caused by some impairment in the anterior portion of the
vertebral motion unit (eg, disc deficit, anterior ligament fixation). In
contrast, faults in the direction of distortions can usually be attributed to
the posterior aspect of the motion unit; eg, total or partial fixations
involving the apophyseal joints, pillar erosion and distortion, osseous pathology, etc. The anterior portion of the motion unit is mechanically designed
for weight bearing, the posterior pillars are not. Thus, when the pillars are
forced to assume the constant role of weight bearing because of some biomechanical fault altering spinal equilibrium and the distribution of load
(intrinsic or extrinsic), structural failure and compensatory remodeling of
the posterior elements is likely to occur eventually.
Kinematics of the Lumbar Spine
 |
Extension. Because P-A trunk motions are the most common movements used in daily living and as flexion is assisted by gravity, the spinal extensors are the most important muscles of the trunk from a biomechanical viewpoint. Muscles of the back are rarely weak unless paralysis is present. Kendall places the incidence of weak spinal erectors at less than 1% in the nonparalytic. When signs of extension weakness are evident, differentiation must be made between weak spinal extensors and weak hip extensors. A screening test can easily be done with the patient prone (Fig. 5.4).
Lateral Flexion. Trunk raising from the lateral recumbent position exhibits the strength of trunk lateral flexors and hip abductors. A simple screening test to differentiate weakness in these groups is shown in Figure 5.5.
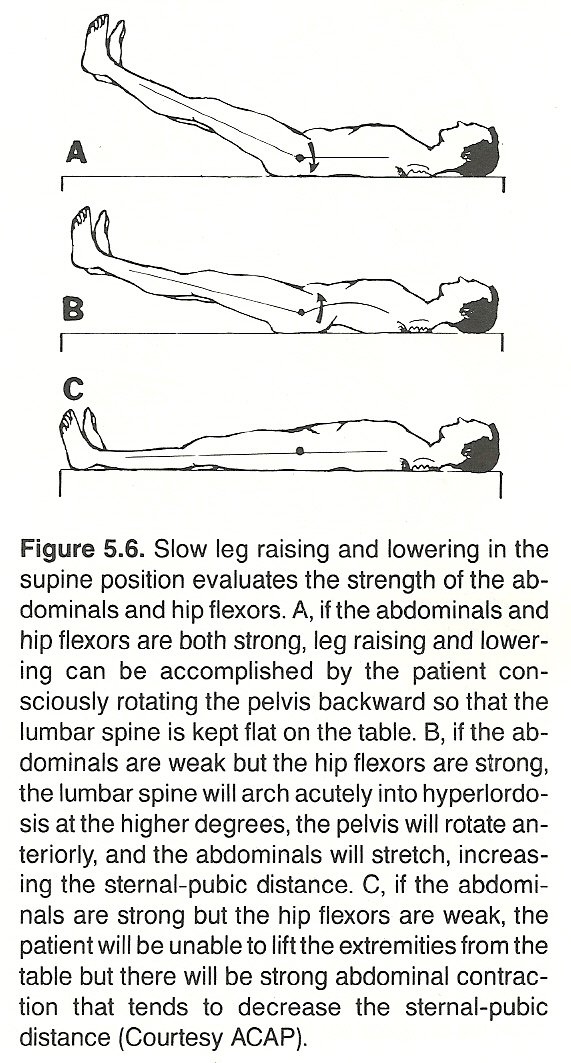
Flexion. Leg raising from the supine position is a two-phase combination between strong abdominals and strong hip flexors. A screen test to differentiate weakness of the two groups is shown in Figure 5.6.
 |
 |
In chronic low-back pain cases, it is important to take a series of lateral lumbar radiographs: neutral, forward flexion, and backward flexion positions. An unstable motion unit will appear to be normal in the neutral view but demonstrate antero- or postero-listhesis in stress films. This sign makes for a worse prognosis and the possible necessity for spinal fusion if disc degeneration is advanced or if correcting the etiological dysfunction does not cause a tightening of the ligaments involved. I x-ray again after 4-6 months of symptom relief. Continual severely painful episodes should suggest an orthopedic consultation.
Lumbar Extension
Gillet's studies found that lumbar flexion-extension movements are similar
to those of other regions of the spine but with less forward or backward
gliding. Extension is, states Gillet, also a movement that takes place in two
parts with the anterior interbody space opening only after backward bending
has reached its limit. This opening anteriorly is, however, a smaller movement
than that which occurs in other regions of the spine.
The extent of lumbar extension is primarily controlled by the tautness of
the anterior longitudinal ligament, the elasticity of the posterior ligaments,
and the tonicity of rectus abdominis anteriorly and the spinal extensor muscles
posteriorly. See Figure 5.10. In IVD herniation posteriorly, facet inflammation,
or spondylolisthesis, pain will be increased during extension but not on
flexion. This is a helpful point in differential diagnosis.
According to McKenzie, reduced lumbar extension is frequently the result
of poor sitting posture and/or inadequate extension mobilization following
injury in which scar tissue prevents a full range of extension. Reduced extension
(1) causes chronic stress on the soft tissues of the posterior motion unit and an increased intradiscal pressure during sitting;
(2) restricts a fully upright posture during relaxed standing, leading to a stooped appearance in stance and gait; and
(3) produces a premature fully stretched lumbar posture when arising from a forward flexed posture.
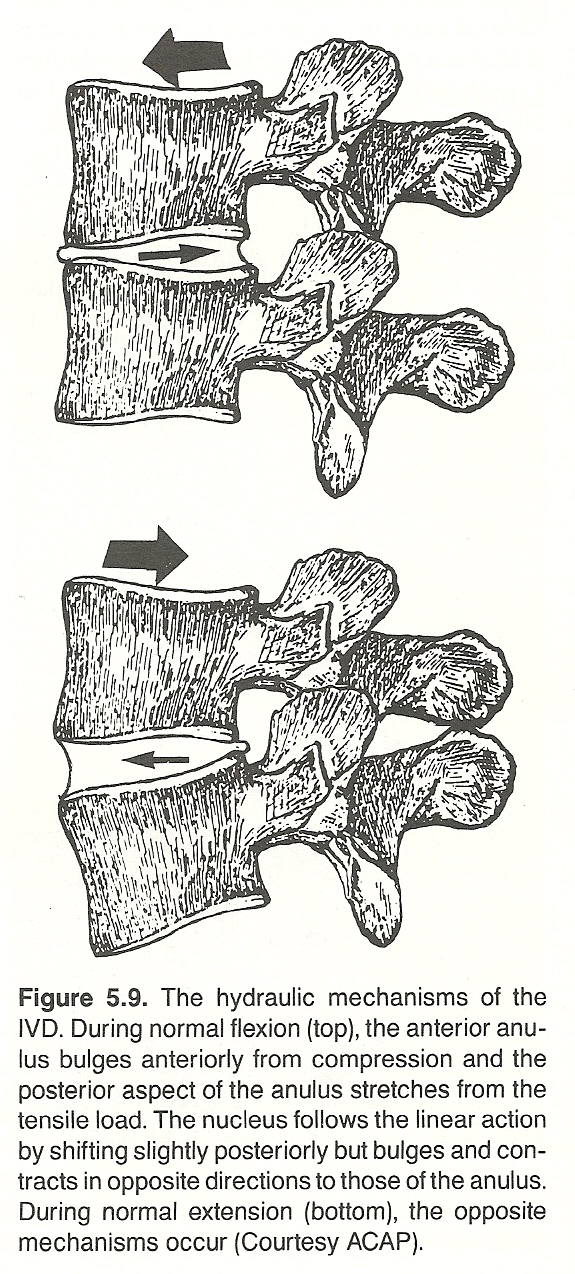
Keep in mind that the fibers of the posterior anulus are the weakest. The
anterior and lateral aspects of the anulus are almost twice as thick as the
posterior aspect. The anular fibers at the posterior aspect of the disc are
less numerous, narrower, and more parallel to each other than at any other
portion of a disc.
If a person must work habitually in a prolonged forward flexed position,
periodic lumbar extension will relieve the stress of the posterior anulus and
tend to shift a loose nucleus pulposus anteriorly; ie, away from the spinal
cord and IVF. Many manual laborers do this stretching maneuver instinctively.
 |
(1) the size of the joint surfaces,
(2) the height of the segmental centers of gravity above the joint surface,
(3) the horizontal distance of the common gravity line to the joint's center, and
(4) the integrity of the supporting ligaments. While these facts are true in all areas of the spine, their importance are increased in the lumbar spine because of the increased weight load.
 |
 |
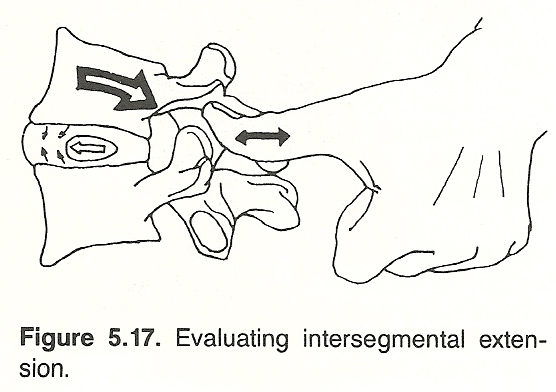 |
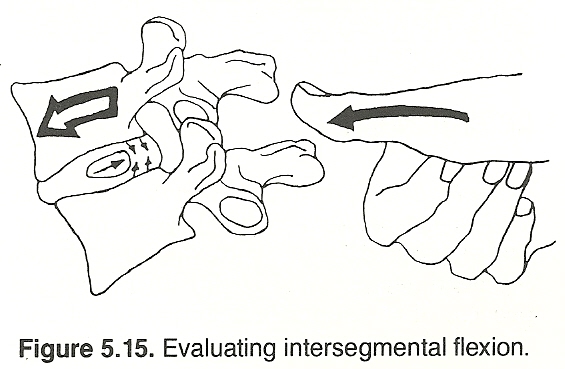
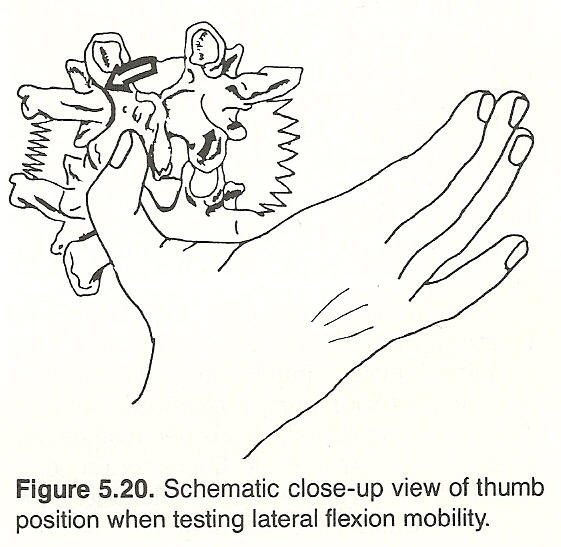
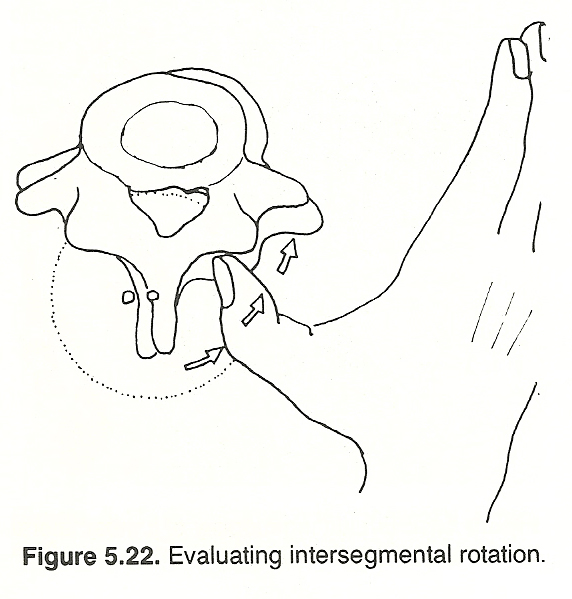
Extension of the zygapophyses (negative theta x). Extension freedom of the posterior aspect of the motion unit is indirectly tested by extending the patient's spine a few degrees and then pushing the articular process of the superior segment of the motion unit anteriorly (further into extension) with your palpating thumb (Figs. 5.17 and 5.18). You should feel a subtle springy movement under your thumb signifying that the joint has closed.
This motion, which evaluates the integrity of the posterior aspect of the superior segment of the motion unit, may appear normal even though an anterior fixation exists. Although fibers of degenerated ligaments lose their elasticity and plasticity to tensile forces, they still retain a large degree of their flexibility and are able to twirl to some degree.Extension, as determined by anterior longitudinal ligament testing in hyperextension. The examiner's thumb is placed over the spinous process of the superior segment of the motion unit being evaluated. The patient's lumbar region is slightly hyperextended by the examiner's stabilizing arm, and then a forward push is made with the examiner's palpating hand (Fig. 5.19). Once the end of the ROM is reached, check for the normal springy end feel. If the anterior ligaments have degenerated, this springy end feel will be absent and the patient will report feeling quite uncomfortable.
 |
 |
(1) ipsilateral iliac crest;
(2) ipsilateral buttock;
(3) ipsilateral groin, scrotum, labium occasionally; or
(4) leg, usually above the knee. There are no conclusive neurologic signs (reflexes +2, sensory negative, motor negative).
There is usually no pain on coughing or sneezing, but the skin rolling test may be positive over the level of inflammation. Faye also states that the most common sites of causation fixation are at the
(1) sacroiliac joints,
(2) thoracolumbar or lumbar joints, or
(3) the hip joints.
Lumbar Disc and Radiculitis Syndromes: General Considerations
One early clinical concern is to differentiate inflammatory conditions
from noninflammatory joint dysfunction syndromes. If a patient can point
specifically to an exact joint as the source of the pain, it is likely the
pain arises from that joint. If the patient moves the whole hand over a
general area, then a specific joint is not usually the correct diagnosis.
Percussing the area of pain causes a sharp pain in dysfunction: an "ouch"
reaction. However, more serious pathology is suggested if percussion produces
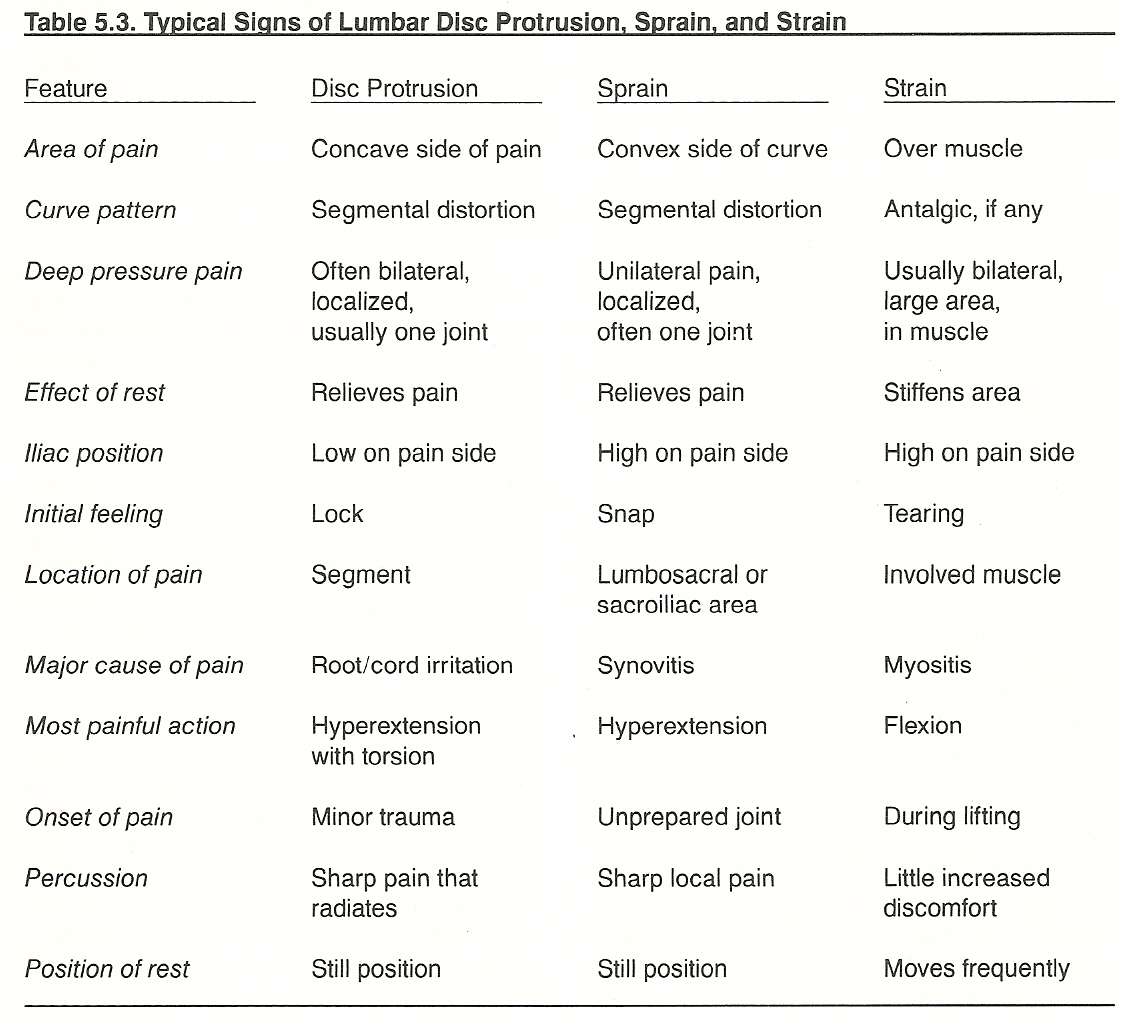
a deep, throbbing, aching pain. Differentiating signs of lumbar disc protrusion, sprain, and strain are shown in Table 5.3.
With either IVD lesions or lumbar radiculities, Faye describes that the
patient usually presents with an acute antalgic posture, bent either laterally
or anteriorly. There may or may not have been a traumatic onset. There is pain
on coughing or sneezing, and it may radiate down either leg. The leg pain extends from below the knee to the foot. There may be neurologic signs such as
paresthesia, weakness of the big toe, weak foot and ankle dorsiflexion, and/or
weak plantar flexion eversion. Atrophy of the affected limb is possible.
SLR, leg-lowering, and Kemp's tests will be positive. Bragard's, Minor's,
and Neri's bowing tests may be positive or negative. The patient's discomfort
becomes worse with activity, improves with rest; is worst in the evening; and
improves in morning. The most common causative fixations are at the
(1) thoracolumbar junction,
(2) sacroiliac joints,
(3) hip joints.
Intervertebral Disc Lesions in the Lumbar Spine
The firm diagnosis of IVD rupture can only be made during surgical inter-
vention; myelography is no exception. Thus, only a tentative diagnosis of disc
protrusion can be made when the conclusions are drawn from clinical signs and
symptoms.
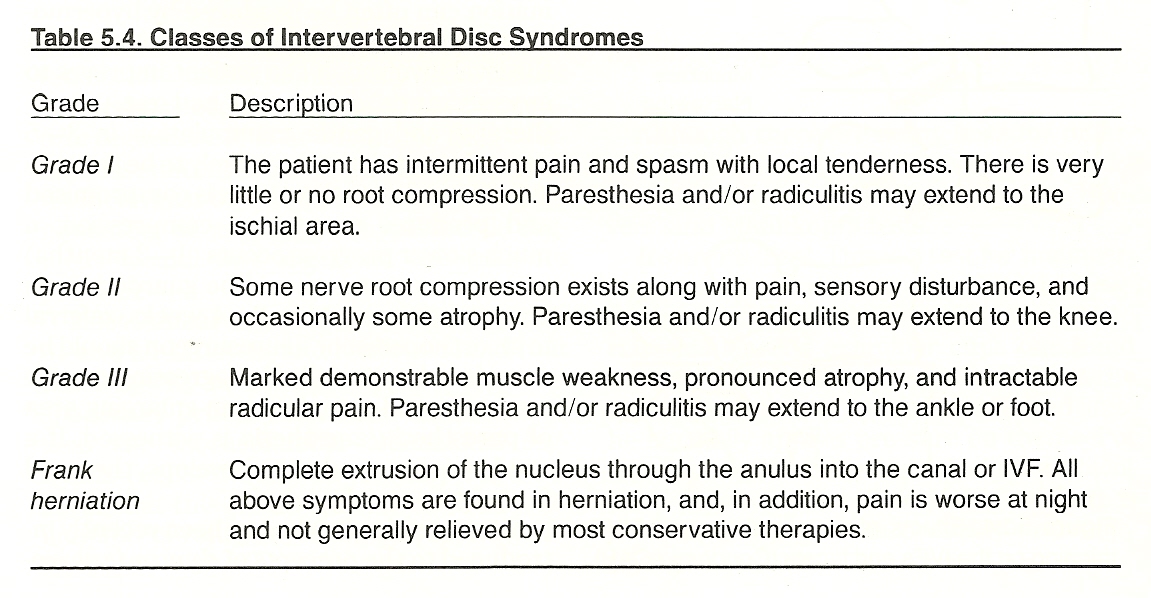
A classification of IVD syndromes is shown in Table 5.4.
 |
Type I: acute sprain, usually from unexpected loading. There typically are severe pain and muscle spasm. Nonsciatic referred pain is usually associated. Rupture of some of the peripheral or central anular fibers, slight end plate fracture, and stress to the capsular or interspinous ligaments and posterior arch muscle fibers occur. Lasegue's straight-leg raising test is negative.
Type II: a nontraumatic, idiopathic, sudden intake of fluid by the nucleus pulposus, causing irritation of the peripheral anular fibers because of the nuclear pressure being transmitted horizontally. There are back pain and muscle spasm without referred pain or sciatica. Lasegue's test is negative.
Type III: slight abnormal bulging of some of the posterolateral fibers with slight IVF encroachment. In addition to local back pain, pain may be referred into the sacroiliac area, buttocks, hip, and posterior thigh. There is no neuromuscular deficit, and Lasegue's sign is negative.
Type IV: herniation of part of the nucleus into the peripheral anulus that, in turn, bulges into the vertebral canal (Fig. 5.25). Local back pain increased with Valsalva's straining maneuvers, true sciatica, and a positive Lasegue's test occurs. These are signs of irritation of a nerve root.
Type V: floating nuclear fragment. This chronic condition is sometimes associated with disc degeneration. There are episodes of back pain, with or without sciatica, depending on the position of the fragment and the magnitude of stress.
Type VI: anchored nuclear fragment. This disorder is often the aftermath of Type V where the nucleus is fixed within the peripheral anulus or vertebral canal with probable IVF encroachment. The nerve root becomes chronically irritated from mechanical pressure, chemical irritation, autoimmune response, or a combination of these factors. True sciatica with a positive Lasegue's sign occurs. A narrowing of the IVD space is usually associated.
Type VII: advanced disc degeneration. When a disc is not well hydrated and nourished, it is unable to serve its hydraulic function. Disc narrowing and arthrotic processes of the vertebral bodies are invariably associated. Symptoms vary from severe to none and may be chronic or intermittent.
Lumbar Radiculitis
Signs and symptoms of lumbar radiculopathy vary somewhat depending on
which root(s) are involved. See Table 5.5. In general, it can be said that
painful lumbar attacks of radiculogenic erector splinting, often with brief
episodes of paresis and paresthesiae, are sudden in onset and frequently bilateral as opposed to the invariably unilateral pain of a posterolateral disc protrusion. In this syndrome, the paravertebral ligaments are extremely
tender, and pain is increased by rotation. Neurologic signs and Lasegue's SLR
test are usually negative or unconclusive. The acute attacks of instability
are often quickly relieved by rest and support. See Figure 5.26.
L3 Root L4 Root L5 Root S1 Rootz
Feature L2–L3 IVD L3–L4 IVD L4–L5 IVD L5–S1 IVD
Ankle reflex Normal Normal Normal Diminished
Back pain Buttocks, Buttocks, Buttocks, Buttocks,
radiates to: dorsal thigh, dorsal thigh, lateral calf, mid-calf,
anterior knee medial calf dorsal foot, plantar foot,
great toe heel
Lasegue's Usually + at 80° + at 50–60° + at 30–40°
supine sign negative or more or more or more
(SLR)
Muscle Quadriceps Quadriceps Gluteus med., Gluteus max.,
weakness femoris group iliopsoas ant. tibialis, hamstrings,
hallucis ext. gastrocnemius,
soleus
Patellar Normal Diminished Normal Normal
reflex
Sensory sign Knee numbness Lower medial Numbness at Numbness
leg numbness cleft between inferoposterior
1st and 2nd to lateral
toe, dorsal maleolus, heel,
foot dorsal calf,
lateral foot
Several authorities suggest and clinical observation concurs that radicular inflammation can often be produced by hypermobility and consequential
nerve root stress at the level involved. If the patient improves to any
substantial degree with bed rest, physiotherapy, and gentle manipulation in
3 5 days, disc herniation is unlikely to be the etiologic factor. When disc
tissue is compromised and produces nerve root compression, a much slower
progress occurs (1-3 months) and the prognosis should be guarded. If no
progress occurs within 2-4 weeks, referral to an orthopedist or neurosurgeon
should be considered, especially if progressing muscle weakness and atrophy or
an enlarging area of paresthesia/anesthesia is witnessed. If a cauda equina
syndrome develops, the need for surgery may be urgent.
The practitioner who has been recently introduced to the precepts of
dynamic chiropractic will soon realize that almost all IVD lesions and local
inflammatory nerve lesions (radiculitis) occur at the level of hypermobile
segments. It is at such sites that overstress is concentrated. Thus, primary
sites of fixation must be sought and corrected. Manipulating or adjusting a
hypermobile segment would only aggravate the patient's problem.
Most lumbar disc lesions occur at the L5-S1 and L4-L5 levels, and it will
be found that the majority of associated (and often responsible) primary fixations will be at or near the thoracolumbar transitional segments (eg, between
T10 and L2). Faye believes that this is also true for cases of well-adapted
chronic lower lumbar spondylolisthesis.
Malingering-Oriented Tests
Although there are many tests for differentiating malingering from a somatic, visceral, or psychic cause, Faye emphasizes Hoovers' and Mannkopf's tests.
Hoover's Test. This is a test for malingering associated with an active straight-leg-raising test. When the patient attempts to raise his leg, the examiner cups one hand under the heel of the opposite foot. When the typical patient tries to raise his affected limb, he normally applies pressure on the heel of the opposite limb for leverage and a downward pressure can be felt. If this pressure is not felt, the patient is probably not really trying.
Mannkopf's Test. This is an old, but reliable, objective test for pain, and it is not restricted to musculoskeletal complaints. The patient is placed in a relaxed position and the pulse is taken. The examiner then precipitates the pain (eg, by probing, applying heat or electrostimulation, etc). The pulse rate is then re-evaluated. In situations of true pain, the pulse rate will increase a minimum of 10%.