

|
Chapter 3:
Physical Examination of the Neck and Cervical Spine
From R. C. Schafer, DC, PhD, FICC's best-selling book:
“Spinal and Physical Diagnosis”
All of Dr. Schafer's books are now available on CDs, with all proceeds being donated |
Inspection of the Neck Lymphadenopathy Motion Palpation Active and Passive Range of Motion Muscle Strength Evaluating Neurologic Levels Auscultation of the Neck Classification of Musculoskeletal Disorders Selected Disorders in or of the Neck Orthopedic and Neurovascular Compression Tests Major Effects of Upper Cervical Subluxations Occipital and Upper Cervical Vertebral Listings Miscellaneous Syndromes
As with all gross and regional inspection, the observation process begins when the examiner first is introduced to the patient and continues through the history and examination process. Abnormalities in the neck may be of local etiology (eg, infection, neoplasm, trauma) or be a manifestation of a general disorder (eg, curvature, spondylosis, leukemia, systemia).
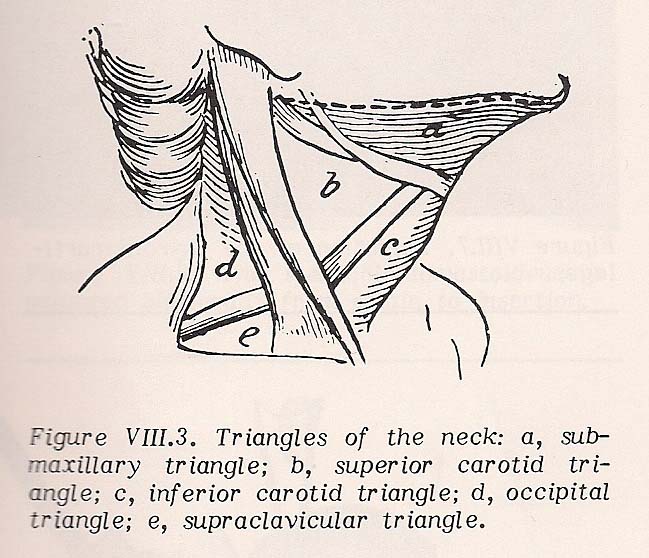
The anterior zone (triangle) of the neck is bordered laterally by the two sternocleidomastoid muscles, caudal by the suprasternal notch, and cephalad by the jaw.
With the patient sitting, the thyroid gland should be carefully inspected, ausculted, and palpated during the examination of the anterior aspect of the neck. Is is helpful to have a glass of water available to test swallowing several times. Infectious processes: infectious mononucleosis, diffuse skin inflammations, secondary syphilis, toxoplasmosis, sarcoidosis, brucellosis, tuberculosis. Primary hematopathic diseases: chronic lymphocytic leukemia, Hodgkin's disease, non-Hodgkin's lymphoma, chronic granulocytic leukemia (blast crisis), Waldenstrom's macroglobulinemia. Endocrine and metabolic states: hyperthyroidism, various lipidoses, hypoadrenalism, hypopituitary disorders. Hypersensitivity states and collagen-vascular diseases: rheumatoid arthritis, systemic lupus erythematosus, Still's disease, dermatomyositis, drug hypersensitivity, serum sickness. Upper Cervical Area: Infection, neoplastic disease. Nodes behind the ear drain the scalp, often enlarging in scalp diseases, rubella, and mononucleosis; nodes in front of the ear and below the angle of the jaw drain the face and eye orbit, enlarging in inflammatory lesions of the eye and conjunctiva; the submaxillary and submental nodes drain the pharynx, mouth, and tongue, enlarging in throat and mouth infections, or cancer of the mouth, pharynx, or larnyx. Lower Cervical and Supraclavicular Area: These nodes drain the head, upper extremity, mediastinum (right nodes) and abdomen (left nodes) and serve as a common site for metastatic neoplastic processes; eg, thyroid, larynx, upper esophagus, Hodgkin's disease, lungs, stomach, gallbladder, pancreas, kidney, ovary, testicle. A midline swelling in the area may point to a low-thyroid disorder. Enlarged nodes in the lower cervical or supraclavicular area must be differentiated from brachial plexus nodes, brachial cysts, dermoid cysts, sebaceous cysts, and bony abnormalities.
Axilla: Node enlargement is often secondary to streptococcal or staphylococcal upper-limb infections, or to neoplasms which drain to this area such as of the breast. Epitrochlear area: Enlargement of nodes is commonly from hand and forearm infections, infectious mononucleosis, and non-Hodgkin's lymphomas. Inguinal-femoral area: Nodes here drain the anterior and posterior pelvis, and most of the lower extremity. Enlargement of nodes is associated with chronic inflammatory diseases, venereal diseases, tinea, pediculosis, rectal cancer, and genital cancer with the exception of ovarian and testicular malignancies. Popliteal space: Node enlargement is usually the result of an infectious process existing in the foot or leg.
In motion palpation, each cervical vertebrae is palpated during flexion, extension, rotation, and lateral flexion to assess mobility. The amount of motion in any particular joint depends upon:
(1) shape of the joint surface,
Without any neck participation, the head can be moved 35° in flexion (10°) --- extension (25°) taking place between the occiput and atlas. Flexion and extension between C2 and C7 occur as a gliding movement of the upper and lower segments accompanied by disc distortion. The site of greatest movement in flexion is at the C4–5 level, while extension movement is fairly well diffused. The foramina open on flexion and narrow on extension, and close on the side of lateral flexion. In lateral flexion and rotation of the head and neck, the occiput and atlas move as one piece because of the planes of the articular facets. Fifty percent of total neck rotation occurs between C1 and C2 (capable of 90° rotation) before any rotation is noted from C2 to C7. Cervical flexion and extension: Have patient flex head as far forward as possible, keeping goniometer arm along mastoid process, and record end of flexion motion. Then, starting from the neutral position, have the patient extend head as far back as possible, keeping goniometer arm along the mastoid process, and record end of extension motion. In cases of ankylosis, place goniometer as if measuring the neutral position and record deviation from this point. Cervical lateral flexion: Place patient in neutral position with his arms abducted to steady the shoulders. Center goniometer over the back of the neck with the base on the vertebra prominans and the goniometer arm extending along the midline of the neck. Record neutral reading. Then record reading after the patient has bent neck as far to the left as possible, recording the reading after the end of lateral flexion motion. Then record reading for the right side in a converse manner. In cases of ankylosis, record deviations from the neutral position. Cervical rotation: Place patient in neutral position and steady patient's shoulders with your hands. Have patient rotate head as far to the right and left as possible. Estimate arc of motion separately for right and left motion by position of the patient's chin in relation to the shoulder. The goniometer is not necessary for this evaluation. In situations of ankylosis, estimate and record angle at which cervical region is fixed by position of the patient's chin.
Chapter 8: Physical Examination of the Neck and Cervical Spine
In general, the neck viscerally serves as a channel for vital vessels and nerves, the trachea, esophagus, spinal cord, and as a site for lymph and endocrine glands. From a musculoskeletal viewpoint, the neck provides stability and support for the cranium, and a flexible and protective spine for movement, balance adaptation, and housing of the spinal cord and vertebral artery. Cervical flexion, extension, and rotation contribute to one's scope of vision.
From a biomechanical viewpoint, primary cervical dysarthrias may reflect themselves in the total habitus; from a neurologic viewpont, insults many manifest themselves throughout the motor, sensory, and autonomic nervous systems. Many peripheral nerve symptoms in the shoulder, arm, and hand will find their origin in the brachial plexus and cervical spine. Nowhere in the spine is the relationship between the osseous structures and the surrounding neurologic and vascular beds as intimate or subject to disturbance as it is in the neck.
Neck pain must be differentiated as to its date of onset and chronology, site and distribution, type (intermittent, constant), duration (acute, chronic), character (sharp, dull, lanciating), relation to posture (rest, occupation, recreation), and associated problems. Nonpharyngeal pain on swallowing may be traced to an anterior cervical spinal pathology such as bony protuberance or osteophytes, infection, mass or tumor. Pain is often referred to the neck from the TMJ, mandibular or dental infection, or sinus infection.
Inspection of the Neck
With the patient in the sitting position, inspect first for gross abnormalities and then details. Some examiners prefer to inspect and palpate the anterior neck in the supine position and palpate the posterior aspect in the supine position.
Check for scars (eg, surgical, tubercular adenitis, trauma), blisters, discolorations, skin texture and lesions, and pulsatile movements. Observe congenital defects such as pteryigium colli (webbed neck) or congenital torticollis.
Note any parotid or submaxillary gland enlargement (eg, infection, duct stone, tumor) if this has not been done previously. Check for fixed or movable masses, and transilluminate if present. Thyroglossal cysts, usually in the midline, often move headward when the tongue is protruded.
Have the patient swallow, and note the function of the cricoid cartilage area and possible superior movement of the thyroid gland. Check the trachea for midline alignment. If the thyroid is visible, note its size, shape, symmetry, and presence of nodules.
Inspect for abnormal shadows, neck contours, curvatures, and restricted movements. Note relationship of neck, head, and shoulders from an A–P, lateral, and rotational standpoint. Check head tilt, sway, carriage during rest and gait, and other abnormal postural expressions.
Keep in mind that tumors of the cervical spine are usually secondary and that chronic degenerative disc disease and congenital anomalies may be asymptomatic for many years. Unlike the lumbar region, cervical disc herniations are not frequently associated with severe trauma; however, nerve root or cord compression has a high incidence.
Venous thrombosis, mediastinal tumors, and inflammatory exudates may produce visible and palpable edema in the neck.
Bony and Soft Tissue Palpation
The neck is usually palpated with the patient supine so that the muscles are relaxed and the head may be passively controlled. With the patient supine, the following general landmarks should be noted: The C1 transverse process (the widest in the neck) lies between the angle of the jaw and the mastoid process, the hyoid bone is above the body of C3, the top of the thyroid cartilage (Adam's apple) is above the C4 body, the bottom of the thyroid cartilage is above the C5 body, and the first cricoid ring is above the body of C6.
If abnormal nodes or masses are palpable in the neck, they should be recorded as to size in millimeters and number (single, multiple).
Anterior Aspect of the Neck
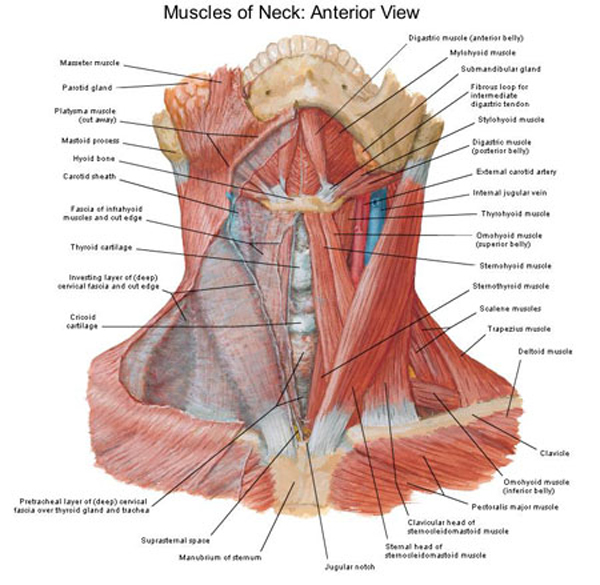
Palpate each sternocleidomastodius muscle individually after passively rotating the patient's neck first toward one direction and then the other, opposite the muscle being examined. Check for possible strain, from traumatic or postural hyperextension, from its origin on the sternum and clavicle to the mastoid process. Note any abnormal size, shape, tension, tenderness, or mass. The sternocleidomastoideus and the trapezius have a common attachment at the mastoid process and occiput; they divide and have individual attachments at the clavicle. Both of these muscles are innervated by the spinal accessory cranial nerve.
During palpation of the sternocleidomastoideus and cervical trapezius, there is an opportunity to palpate the lymph node chain which extends along the anteromedial border of the muscles. The nodes are normally not palpable unless inflamed (eg, upper respiratory infection) or calcified. Lymphadenopathy will be discussed further in this chapter.
Palpate the hyoid, situated cephalad from the thyroid cartilage, by probbing from the midline laterally and posteriorly with thumb and first finger. Note distinct movement when the patient swallows.
Move caudal from the hyoid and palpate the thyroid cartilage in the anterior midline in the same manner. The thyroid gland, which overlies the thyroid cartilage in a "H" pattern, is normally smooth and quite indistinct. When diseased, cysts, nodules, swelling, and/or tenderness may be noted. More on this subject later.
Next palpate the first cricoid ring, located just caudal to the thyroid cartilage. Be gentle to avoid stimulating the gag reflex. Slight movement should be palpable upon swallowing.
Palpate the small, deep carotid tubercles, located on each side about 1 inch lateral from the carotid ring and just anterior to the transverse process of C6. Palpate gently, quickly, and unilaterally (to avoid stimulating a carotid reflex) by placing the fingers of one hand deeply posterior between the cricoid ring and lateral cervical muscles.
Palpate the carotid pulse, next to the carotid tubercle, with the index and middle fingers. Note pulse strength and compare bilaterally.
Palpate the supraclavicular fossa, beginning at the sternum and moving laterally. Search for abnormal swellings (eg, traumatic edema), masses (eg, tumors, swollen lymph nodes, cervical rib), or unusual depth of the fossa (eg, clavicular fracture).
The vertebral bodies may often be palpated from the anterior by pressing the index and middle fingers through an imaginery surgical approach to the neck between the carotid sheath and the sternocleidomastoideus laterally and the trachea, esophagus, and thyroid gland medially.
Thyroid Gland Examination
Keep in mind that the thyroid may be congenitally located as high as in the sublingual area or as low as in a substernal position. If the latter is the case, percussion over the upper sternum will reveal a flat tone rather than the normal resonant sound.
The thyroid may be palpated from either the back of the patient with bimanual palpation or at each side of the patient using one active hand and the other offering counterpressure.
When the examiner is behind the patient, the examiner's fingertips are placed bilaterally on each side of the Adam's apple as an initial landmark. Drop the fingers slightly below the cricoid cartilage where the thyroid isthmus crosses the midline. Have the patient swallow and check the normal upward movement. With the patient taking small slips of water, search laterally and cephalad to determine if the upper lobes can be delineated and if their consistency, size, and contour can be appreciated. A normal thyroid feels smooth and "fleshy" to the touch as would a normal muscle. Increased firmness will be noted upon inflammation or an early neoplastic process. A bruit may be heard over the gland in hyperthyroid states.
A single or multiple nodule may indicate a toxic nodule of hyperthyroidism such as seen in the diffuse hyperplasia of Grave's disease, hypersecreting adenomata, or autoimmune thyroiditis where areas of induration may be palpable. Nodules palpated within the parenchyma of the gland usually indicate cysts (benign or malignant), neoplastic benign adenomas, local malignant carcinoma, or secondary metastases.
The gland is usually not palpable in hypothyroidism; in thyroiditis, the pyramidal lobe on the isthmus is usually prominent and painful when palpated. Rarely, a pyogenic abscess of the thyroid may be found which features an extremely tender indurated area in the thyroid. Hashimoto's thyroiditis is characterized by a firm gland, often presenting firm nodules, that is tender in the acute stage but nontender in the chronic stage.
Posterior Aspect of the Neck
Palpate the posterior aspect of the occiput generally and then for details. Note tension and tenderness by palpating laterally from the inion across the nuchial areas to the mastoid process. Palpate suboccipital ligaments for tenderness, tension, and signs of acute or chronic sprain. The greater occipital nerves are distinctly palpable by probbing both sides at the base of the skull from the inion laterally. Search for signs of inflammation.
Palpate the cervical spinal processes, beginning at the base of the skull and progressing to T1. The spinous of the axis will be felt at about a finger width below the occiput and is the largest and first palable spinous process in the upper cervical area. The spinous process of the atlas is represented by a small tubercle, usually lieing too deep to be felt. Note spinous bifurcations, alignment, and abnormal masses.
Various factors can mislead in palpation. Common conditions are bent spinous processes, irregularities and exostoses on spinous processes, thick aponeuroses, unpalpable bifurcations, unequal bifurcations, and bifurcations not in the midline.
The superior nuchial ligament is palpated at the same time as the spinous processes as the ligament extends from the base of the skull to each of the cervical spinous processes. It normally is not palable but tenderness may be elicited if a ligament defect is present or a stretch injury has occurred.
Carefully palpate the cervical facets, located about 1 inch lateral to the spinous processes and felt as small domes beneath the trapezius muscle. Note tenderness and trigger points. Check C5 and C6 areas especially for possible osteoarthritic spur formations.
The trapezius is usually palpated with the patient seated. One side should constantly be compared with the other. Note abnormal tension, size, shape, and tenderness. Check the muscle's origin along the spinous processes from the inion to the T12 and then to its insertion at the clavicle, acromion, and scapular spine. Carefully examine its superior aspect from the neck to the acromion; this portion is usually injured in lateral flexion strains. Check the point of insertion at the scapular spine for possible hematoma or strain from whiplash.
Lymphadenopathy
The average body contains more than 500 lymph nodes whose function serves to mount an immune response. Children 12 years old have about double as much lymphoid tissue as the adult of 20 years or older. A lyphoid tissue response in the young is dramatic with prompt swelling and hyperplasia; this response diminishes with age.
Except for the "buck-shot" nodes often found in the inguinal-femoral area, normal superficial lymph nodes are not palpable. Palpable nodes of a diameter under 1 cm are usually not significant. Enlarged nodes should be recorded as to site, size, softness or hardness, tenderness, fluctuation, pulsation, or if movable or fixed.
Nodes in the neck are best appreciated by the examiner when standing behind the sitting patient during bimanual palpation. This position also presents an opportunity to examine the nodes in the axilla.
The following areas in the neck should be palpated: subocciput, around the ears, below the jaw, along the anterior sternocleidomastoideus and trapezius muscles, posterior sternocleidomastoideus, and the supraclavicular space. Nodes are palpated by rolling the balls of the fingertips up and down and laterally.
If enlarged nodes are found in the neck, they should be searched for in other areas such as the axilla, epitrochlear area with elbow flexed 90°, inguinal ligament area, femoral canal, and the popliteal space with the knee slight flexed. As the spleen is an important part of lymphatic system, an associated splenomegaly is a significant finding and will be discussed in the abdominal examination.
Lower cervical nodes are unlikely to enlarge secondary to infection. Axillary and inguinal nodes frequently respond to extremity trauma and minor infections.
Node enlargement can usually be traced to infections, primary hematopathic disease, cancer, allergic reactions, metabolic disorders, connective tissue diseases, endocrine disturbances, and rarely to foreign-substance infiltration such as in anthracosis and silicosis.
Generalized Adenopathy
Generalized adenopathy, above or below the diaphragm but rarely both, suggests a systemic disorder presenting a lyphoid reaction. Common causes are infectious processes, primary hematopathic diseases, endocrine and metabolic disturbances, and hypersensitivity states.
Regional Adenopathy
Regional adenopathy may represent either a localized disorder or an early stage of generalized adenopathy such as Hodgkin's disease. Below are specific sites related to common causes for node enlargement:
Specific Considerations
The most common causes of enlarged lymph glands are tonsilitis, syphilis, Hodgkin's disease, leukemia, mumps, and measles.
Tonsilitis and other inflammations within and around the mouth such as diphtheria, the exanthemata, herpes, carious teeth, etc, produce glandular swellings that are usually acute and more or less tender. Most of them disappear within a few days, but some persist, without pain, indefinitely.
Long-standing cervical adenitis in children and young adults, with a tendency to involve the skin and to suppurate, is characteristic of tuberculosis.
Small, nonsuppurating glands, occurring in the neck and about the occiput in adults, often accompany syphilis, but the diagnosis depends on the presence of unmistakable syphilitic lesions elsewhere and blood tests. Occasionally, syphilitic glands are large and soft.
Chronic, large, rarely suppurating glands in the neck, axillae, and groins, with slight splenic enlargement and near-normal blood picture, suggest Hodgkin's disease, but further referred laboratory tests (eg, biopsy) are necessary to exclude tuberculosis.
Primary or secondary malignant disease may enlarge the cervical glands early. Cancer of the lip, tongue, or tonsil, and, among distant lesions, cancer of the stomach or lung are common causes. Frequently, no distinguishing characteristics can be found in the glands in early lymphoid leukemia, but any nodular enlargement in the neck mandates further laboratory analyses.
If the parotid gland alone is swollen and there are fever and pain on chewing, the case is probably one of mumps, especially if there are other cases in the community. Malignant disease may also attack the parotid.
German measles may be accompanied by swelling of the posterior cervical or occipital glands without the involvement of any other glands.
Motion Palpation
(2) laxity or tautness of supporting ligaments, and
(3) condition of the related musculature. Essentially, the extent of movement below the axis is dependent upon ligamentous and muscular laxity and the distortion and compressibility of the IVDs.
In appreciating the physical signs of cervical subluxations and fixations, the research and writings of Drum on functional concepts and of Gillet on motion palpation and its measurement cannot be ignored. Thus, the below is a brief summary of their findings.
Fixation Subluxations
A vertebra may be fixed in a position it could normally occupy during any phase of a physiologic movement; thus a fixated segment is hypomobile, enjoying less than a full range of movement but still occupying a position possible to a normal motor unit. Such states are the most common form of spinal dysarthria. While not visible on static x-ray films, motion palpation reveals the subtleties of incomplete fixations as an erratic, jumpy motion at some point during the arc of movement or as a paradoxical movement where the involved segment moves in the opposite direction to the overall spinal movement, as frequently occurs in the upper cervical spine.
In a vertebral fixation, nothing is actually subluxated or "out of place". On the contrary, the segments are too much "in place"; ie, their full expression of movement is blocked.
Hypermobile Subluxations
Hypermobility is permitted by ligamentous laxity, disc degeneration, and remolding of the posterior articulations. It may be primary (ie, localized trauma or pathology limited to one or more motor units) or secondary (ie, resulting from a primary problem often far removed from the spine such as lower limb asymmetries, eccentric weight bearing, misuse-overuse of spinal tissues associated with postural-occupational stresses, and systematic disorders such as hypoglycemia which may increase the degree of spinal curvatures through chronic fatigue).
As segmental instability requires stabilization, the primary question in spinal diagnosis is "Where and what is the primary problem or maladaption that is overloading and chronically stretching the involved motor unit? A hypermobile unit is not tighten by spinal adjustment.
Hypermobility is the variant of subluxation that is most apparent in roentgenology: traction spurs, interruption of Hadley's "S" curve, excessive A–P body shift at extremes of flexion-extension, abnormal opening and closing of disc space during lateral bending, appearance of segmental hyperextension on neutral lateral films, change in articular relations to the joint-body line, reactive spondylosis and arthrosis, etc.
In hypermobility subluxation, the examiner is considering the "subluxation" as defined by allopaths, at least in the more gross stages of loosening of the vertebral holding elements. This is a positional relationship of two vertebrae in which their bodies or apophyseal joint surfaces or both are in a position which they could never occupy during any phase of a physiologic spinal movement. It is particularly obvious in spondylolisthesis, laterolisthesis, and retrolisthesis, and in excessive disc-space gaping in the sagittal or frontal plane. Instability in these cases becomes even more obvious at the extremes of movement, hence the value of stress films.
These subluxations are permanent; but on top of such a relatively irreversible subluxation, a fixation subluxation in one particular arc of movement (eg, forward flexion from an internal disc derangement) may develop. Thus, the "chiropractic" subluxation which is often not radiographically demonstable is a dysfunction clinically discernable through motion and muscle palpation.
All subluxations appear to follow a progression. For example, a spondylolisthetic vertebra may start off with essentially normal mechanics, slowly becoming hypermobile with middle age. An evident subluxation must be viewed in the context of the entire clinical picture, and this functional classification is clinically oriented.
Motion Measurements
Several investigators of cervical mobility have noticed that it is quite difficult to determine the effects of specific fixations on the overall mobility of the cervical region because each fixation is accompanied by an area of hypermobility. It appears that a degree of exaggerated mobility is capable of compensating for fixation restriction wherein the overall measurement appears normal.
Gillet states that when the degree and number of fixations are such that there is no place for areas of consequent hypermobility, the overall ranges of movement are much more visibly restricted. This is especially true when the fixations are bilateral; in which case, other grosser methods can then be used in assessment such as the measurement of anteroposterior mobility.
If during passive extension it is found that the patient's neck stops sharply at a point far short of normal extension, Gillet refers to this "brick wall" sign of strong restriction as an indication of cervical osteophytes. This is a classic sign of chronic degeneration found in the cervical joints of the elderly presenting a thin, dry cervical spine. These fixations usually produce the different types of brachialgias.
The degree of extension possible is calculated by Gillet by pulling the head and neck backwards to a maximum degree short of pain and inspecting the patient in profile. An imaginary line is then made at the posterior edge of the ear, and a mark is made with a skin pencil at the point where this line cuts the shoulder. There will usually be a gain in mobility of a few centimeters after an adjustment. In nonosteophytic types of fixations of principally a ligamentous or muscular nature, the post-adjustive change will be much greater.
The examiner measures the degree of anterior flexion by placing his chest against the patient's mid-dorsals to prevent thoracic movement, and then directing the patient's head down and forward to a maximum short of pain. While the patient is in this positin, the 7C spinous is marked with a skin pencil. Then with a spirit-level placed horizontally from that point to the ear, another mark is made where the horizontal line cuts the imaginary ear line. In a normally mobile neck, this point should meet the top of the auricle while the line in a stiff neck will cut its base.
This offers the examiner two measures, one indicating restriction caused by fixation at the anterior aspect of the cervical spine and the other at the posterior aspect; one of these usually being greater than the other.
Gillet's research has shown that nearly all partial fixations found in the cervical region are secondary to more primary fixations in the remainder of the spine or in extraspinal joints (disappearing upon correction of the primary factors). The effects of these extra-cervical primary factors upon cervical rotation and lateral flexion mobility can be measured. The examiner sits directly behind the patient and reaches forward, grasping the occiput of the patient in one hand and the chin in the other. The head of the patient is then rotated to an easy maximum with care taken not to force the patient's shoulders around at the same time. The examiner may hold the patient's shoulders back with his forearm. Then, holding the head in rotation with one hand, a point is drawn with a skin pencil on the patient's shoulder exactly under an arbitrary point to the ear. The head is then turned to the opposite side and a point made on the other shoulder, exactly under the one made on the same area of the other ear. A third point is then marked on the 7C process, and the space between the two exterior points and the 7C will indicate the relative degree of mobility in rotation of the whole cervical spine. In a fairly supple neck, this distance should not be more than a centimeter; in a stiff neck, it may be up to 4 centimeters. These measurements can be used for all fixations in the cervical area; but because of the lesser degree of normal movement between the occiput and atlas, it will not be influenced as much by fixation there.
Bilateral fixations will restrict mobility, while unilateral fixations will produce a space which will be visibly smaller on one side. Theoretically, a unilateral fixation on one side plus another on the other side will also produce a bilateral restriction. This is rare, however.
Some partial fixations hinder lateral flexion more than any other movement. This is especially true of the uncovertebral fixations which are quite frequent in the C4–C6 region on the left. To measure these fixations, the patient's head is flexed to the side to an easy maximum with one hand on the skull and the other on the ipsilateral shoulder to prevent it from following the movement. Again, an arbitrary point on the ear is selected and a mark is made on the shoulder directly under it while the patient's neck is in maximum lateral flexion. The same is done in lateral flexion of the opposite side, and, as in rotation, the space between the two shoulder points and the 7C process is measured. In a supple neck, the points should be quite close to the 7C spinous and may overlap it. In a stiff neck, this space may measure up to 3 centimeters on either side, which is rare. Naturally, painful conditions of the neck influence the above measurements. In fact, they may be very difficult to measure in cases of acute torticollis.
Gillet found that almost every patient seemed to turn his head less to the right than to the left, and no fixation could be found to be responsible for this anomaly in mobility. This appears normal in right-handed people, and the opposite appears true for left-handed people.
Active and Passive Range of Motion
Flexion, extension, rotation, lateral flexion, and circumduction are the basic movements of the cervical region. Bone, muscle, tendon, ligament, and lumph node abnormalities tend to restrict motion. Tissue tears and lax ligaments without muscle spasm may manifest in hypermovements. Passive motion should never be attempted if spinal fracture, dislocation, advanced arteriosclerosis, or severe instability is suspected.
Active and passive cervical motions are tested with the patient sitting unless the patient is unable to hold his head erect.
A great deal of cervical motion is concentrated in specific spinal areas. About half of flexion and extension movement occurs at the occipitoatlantal joints, with the other half being distributed among the remaining cervical joints. Approximately half of rotational movement takes place at the atlanto-axial joints, with the remaining half distributed fairly evenly among the other cervical joints. Lateral flexion is accompanied by a rotational torsion below C2, distributed fairly equal in the normal cervical joints.
Flexion and Extension
Active cervical flexion and extension is tested by having the patient lower and raise his chin as far as possible without moving his shoulders. Note smoothness of motion and degree of limitation bilaterally.
Passive cervical flexion and extension is examined by placing your hands on the sides of the patient's skull and rolling the skull anterior-inferior so that the chin approximates the sternum and posterior-superior so that the nose is perpendicular to the ceiling.
Rotation
Active rotation is tested by having the patient move his nose as far as possible to the left and right without moving his shoulders. Note smoothness of motion and degree of limitation bilaterally.
Passive rotation is examined by placing your hands on the patient's skull and turning the head first to one side and then to the other so that the chin is in line with the shoulder.
Lateral Flexion
Active lateral flexion is tested by having the patient attempt to touch each ear on the respective shoulder without moving the shoulders. Normally, about a 45° tilt can be observed.
Passive lateral flexion is tested by placing your hands on the patient's skull and bending the head sideward toward the shoulder on each side.
Goniometry
Place patient in neutral position, centering goniometer with its base on line with the superior border of the larynx and the goniometer arm along the mastoid process. Record neutral reading.
Muscle Strength
Muscle strength is recorded as from 5 to 0 or in a percentage, and compared bilaterally whenever possible. Grading has been previously described.
Flexion and Extension
Flexion of the neck is conducted primarily by the sternocleidomastoideus (XI innervated) with secondary assistance from the scalenus and prevertebral muscles. Extension is controlled by the splenius, semispinalis, and capitis forming the paravertebral extensor mass and the trapezius innervated by the XI cranial nerve. Secondary assistance is provided by several small intrinsic neck muscles.
Muscle strength of flexors is tested by the examiner stabilizing the patient's sternum with one hand to prevent thoracic flexion and placing the palm of his other hand's against the patient's forehead. Muscle strength is evaluated by having the patient slowly attempt to flex his neck against the examiner's resistance.
Muscle strength of extensors is evaluated by the examiner placing a stabilizing hand in the patient's upper dorsal area preventing thoracic extension and the palm of his resisting hand over the occiput of the patient. Muscle strength is measured by having the patient slowly extend his neck against the doctor's resistance. The stabilizing hand may be placed on the superior aspect of the trapezius between the neck and the humerus to palpate muscle contraction at the same time.
Rotation
The primary rotator involved in cervical rotation is the sternocleidomastoideus with some secondary assistance provided by the small intrinsic muscles of the neck.
Muscle strength of the cervical rotators is tested with the examiner, in front of the patient, placing his stabilizing hand on the patient's left shoulder and his resisting palm against the patient's right cheek when right rotation is being measured. The examiner's positions of hands are switched for testing left rotation strength. Rotational strength is evaluated by having the patient attempt to slowly rotate his head against the doctor's resistance for each side.
Lateral Flexion
Lateral flexion is accomplished by the scalenus anticus, medius, and posticus supplied by the lower cervical nerves. Secondary assistance is provided by the small intrinsic muscles of the neck.
Muscle strength of the lateral flexors is tested by the examiner, standing at the side of the patient, placing his stabilizing hand on the patient's shoulder to prevent thoracic movement and his resisting palm on the patient's skull above the ear. Muscle strength is evaluated by having the patient slowly lateral flex his neck against the doctor's resistance.
Evaluating Neurologic Levels
Table 8.1: NERVE FUNCTION OF THE CERVICAL AND BRACHIAL PLEXUSES
| CERVICAL PLEXUS (C1–C4) | |
| Lesser occipital | Sensory to skin behind ear and mastoid process. |
| Greater auricular | Sensory to skin over parotid, jaw angle, ear lobule, and front of mastoid process. |
| Cervical cutaneous | Sensory to skin over anterolateral portion of neck. |
| Supraclaviculars | Sensory to skin over medial infraclavicular area, pectoralis major and deltoid. |
| Muscular branches | Motor to capitus anterior and lateralis, longus capitus, longus colli, hyoid muscles, sternocleidomastoideus, trapezius, levator scapulae, scalenus medius. |
| Phrenic | Sensory to costal and mediastinal pleura and pericardium. Motor to diaphragm. |
| BRACHIAL PLEXUS (C5–T1) | |
| Radial | Motor for wrist and thumb extension; sensory to dorsal web space between thumb and index finger. |
| Ulnar | Motor for little finger abduction; sensory to distal ulnar aspect of little finger. |
| Median | Motor for thumb opposition and abduction; sensory to distal radial aspect of index finger. |
| Axillary | Motor to deltoid muscle; sensory to lateral arm and deltoid patch on upper arm. |
| Musculocutaneous | Motor to biceps muscle; sensory to lateral forearm. |
| CERVICAL PLEXUS (C1–C4) | |
| Segment | Function |
| C1 | Motor to head and neck extensors, infrahyoid, rectus capitus anterior and lateral, and longus capitus. |
| C2 | Sensory to lateral occiput and submandibular area; motor, same as C1 plus longus colli. |
| C3 | Sensory to lateral occiput and lateral neck, overlapping C2 area; motor to head and neck extensors, infrahyoid, longus capitus, longus colli, levator scapulae, scaleni, and trapezius. |
| C4 | Sensory to lower lateral neck and medial shoulder area; motor to head and neck extensors, longus coli, levator scapulae, scaleni, trapezius, and diaphragm. |
| BRACHIAL PLEXUS (C5–T1) | |
| Segment | Function |
| C5 | Sensory to clavicle level and lateral arm (axillary nerve); motor to deltoid, biceps; biceps tendon reflex. Primary root in shoulder abduction, emits between C4–C5 discs. |
| C6 | Sensory to lateral forearm, thumb, index and half of 2nd finger (sensory branches of musculocutaneous nerve); motor to biceps, wrist extensors; brachioradialis tendon reflex. Primary root in wrist extension, emits between C5–C6 discs. |
| C7 | Sensory to second finger; motor to wrist flexors, finger extensors, triceps; triceps tendon reflex. Primary root in finger extension, emits between C6–C7 discs. |
| C8 | Sensory to medial forearm (medial antebrachial nerve), ring and little fingers (ulnar nerve); motor to finger flexors, interossei; no reflex applicable. Primary root in finger flexion, emits between C7–T1 discs. |
| T1 | Sensory to medial arm (medial brachial cutaneous nerve); motor to interossei; no reflex applicable. Primary root in finger abduction, emits between T1–T2 discs. |
| Rupture Site | Features |
| C4–C5 Disc | Shoulder and arm pain and paresthesia, hypesthesia of 5C root distribution, deltoid or biceps weakness. |
| C5–C6 Disc | Hypesthesia of lateral forearm and thumb, biceps and supinator weakness. |
| C6–C7 Disc | Hypesthesia of the index and middle fingers, triceps, and grip weakness. |
| C7–T1 Disc | Uncommon; ulnar hypesthesia and intrinsic muscle weakness in the hand. |
Auscultation of the Neck
Auscultation of the neck is performed to assess carotid bruits and venous hums. Bruits result from vibrations within arterial walls and are usually produced from a partial obstruction. Bruits may also result from increased blood velosity or flow. A venous hum from the internal jugular vein results from the whining noises of the vein's circulation.
Carotid Bruits
Carotid bruits are usually either systolic or continuous. A systolic bruit may continue into diastole, however. Carotid and subclavian bruits are not uncommon in the healthy young. In the adult, the cause is most likely a manifestation of:
(1) atherosclerosis, producing a loud, high-pitched, extended bruit over the site of obstruction,
(2) arteriovenous fistula, producing a loud, continuous bruit related to bounding pulses,
(3) anemia, or
(4) thyrotoxicosis. A palpable thrill is often associated with a loud bruit.
As with most symptoms and signs, bruits are significant only when compared to other manifestations to form a clinical picture. A most positive indication of carotid artery disease is evidence of Hollenhorst crystals during ophthalmoscopy. These are bright-orange atherosclerotic emboli fixed at the bifurcation of retinal arteries and are assumed to be one cause of transient ischemic attacks of the retina.
With the patient sitting, auscult the carotid from the base of the neck up to the jaw. Apply the bell lightly to the artery as the patient holds his breath to eliminate respiratory noise. There is a good opportunity here to also auscult the subclavian areas in search of bruits arising from the subclavian arteries.
In addition to locally caused bruits, a cervical bruit may be the result of a heart murmur (eg, aoric stenosis) radiating into the neck. A cervical bruit is often confused with a cervical venous hum. Thus, differentiation as to the cause of an ausculted whine or roar is necessary.
Cervical Venous Hum
Cervical venous hums are invariably found in 90% or more of healthy children and from 40% of normal adults. They are loudest when the patient is upright with his head turned contralaterally, louder during diastole than systole, and louder during inspiration than expiration. Hums are rarely heard over large veins other than in the neck. They occur less often on the left side than the right and are rarely bilateral.
With the patient sitting, apply the bell lightly to the base of the neck above the clavicle lateral to the attachment of the sternocleidomastoideus. The patient is told to hold his breath to eliminate respiratory noises and asked not to strain or bear down.
Abnormal hums are usually quite loud. When hums are manifestations of an abnormal state, the cause can usually be traced to a high cardiac output as a result of anemia, aortic insufficiency, hyperthyroidism (invariably), or an intracranial or peripheral fistula or arteriovenous malformation. It is possible in some conditions for the transverse of the atlas to compress the internal jugular vein causing a turbulent flow with a resulting hum.
Because hums are found in 90%+ of normal children, their absence is significant in the young. Most common causes are right ventricular congestive heart failure, obstruction in the superior vena cava, tricuspid insufficiency, constrictive pericarditis, polycythemic vera, or pericardial tamponade.
Hums are differentiated from bruits by the fact that hums can be erased by compression of the internal jugular vein, the Valsalva maneuver, or assuming a prone position. Also, a bruit is loudest during systole. If a hum is found during auscultation, see if it can be turned on and off by applying slight-to-moderate pressure directly above the bell with your free hand's thumb or fore-finger. This will obliterate a hum but not a bruit. Differentiation must also be made from respiratory noises and muscle tremors. Loud hums may be referred to the left 1st and 2nd intercostal spaces and be confused with a patent ductus arteriosus or the right 1st and 2nd intercostal spaces and be misdiagnosed as aortic insufficiency.
Classification of Musculoskeletal Disorders of the Neck
Table 8.4: CLASSIFICATION OF MUSCULOSKELETAL DISORDERS OF THE NECK
| Adulthood Cervical Disorders Trauma of the cervical spine and cord Subluxation-fixation Soft tissue or disc injury Without neural deficit With neural deficit Root signs Cord signs Acute herniated disc Fracture or Dislocation Without neural deficit Stable Unstable With neural deficit Complete quadriplegia Incomplete quadriplegia Anterior cord syndromes Central cord syndromes Brown-Sequard syndrome Nerve root injury Degenerative disc disease Traumatic Geriatric Spondylosis Congenital anomalies Congenital stenosis Cervical ribs Systemic disease causing bone-texture alterations Anemia Leukemia Paget's disease Osteoporosis Hodgkin's disease Inflammatory diseases Ankylosing spondylitis Rheumatoid arthritis Infections Tumors Primary, of bone Secondary, metastatic Men: prostate, lung Women: breast | Childhood Cervical Disorders Trauma Soft tissue or disc injury Cervical sprain Cervical strain Subluxation Fracture or dislocation Acquired torticollis Congenital deformities Metabolic disease and bone dysplasias Morquior's disease Spondyloepiphyseal dysplasia Diastrophic dwarfism Central disc calcification Inflammatory disease Juvenile rheumatoid arthritis Ankylosing spondulitis Vertebral/disc infections Tumors of the cervical spine Primary (uncommon) Secondary (rare) Infantile Cervical Disorders Congenital disorders of the cervical spine Congenital torticollis Atlanto-occipitalization Basilar invagination Odontoid process dysplasia Vertebral fusion Spinal dystrophia Birth Injuries Delivery-related subluxations Cord injuries Nerve injuries Epidural hemorrhages Bone injuries |
Selected Disorders in or of the Neck
Inflammatory Musculoskeletal Disorders
Rheumatoid arthritis, ankylosing spondylitis, and various infectious diseases may attack the cervical spine in infancy, childhood, and adulthood. Cervical rheumatoid arthritis manifests as neck pain, severe but paroxysmal, associated with a mono- or poly-arthritis. In time, ankylosis develops, especially in the upper cervicals, and is demonstrated by restricted motion from ossification of the posterior facets and interspinous ligaments. During this process, ligaments loosen in the upper and lower cervical areas encouraging gross vertebral subluxations and dislocations that may possibly be asymptomatic. In late stages, the odontoid may migrate into the foramen magnum and produce cord pressure with various characteristic neurologic signs.
Ankylosing spondylitis is a common adolescent and adult arthritic disorder, attacking the spine and larger joints. It is characterized by ankylosis, joint deformity, spinal pain and rigidity, muscle spasm, and loss of chest expansion. Motion is lost greatest in the lower cervical region first. There may be loose ligaments above a rigid segment leading to atlantoaxial dislocation. Disc spaces are rarely narrowed as ligaments and discs ossify. The patient moves as if his spine were a metal rod, with head and shoulders moving as a unit. A related fracture, usually lower cervical, through an ossified disc produces a characteristic chin-on-chest deformity, without or with paralysis from an associated epidural hemorrhage.
Pyogenic infection, most common in middle age, produces an exudative inflammation with hyperemia leading to osteoporosis and osteomyelitis. Early diagnosis is vital. The first clues are neck pain (possibly referred to the scapula or shoulder), fever, muscle spasm, and sometimes dysphagia with a large anterior abscess which may be palpable. In time, the end plate becomes involved and the infection enters the disc space and possibly the cord. Bone destruction leads to collapse. The abscess may enter the cord or a paravertebral abscess may extend into the thorax or vice versa.
Abscess or Scars
Abscess or scars in the sides and front of the neck generally result from glandular tuberculosis, hence the presence of scars may be of value in the diagnosis of doubtful cases with a suspicion of tuberculosis in later life. Aside from glandular abscesses (tubercular or septic), it is rare to find any suppuration in the neck, except in the nape, where deep septic abscess (carbuncle) and superficial boils are common. High Pott's disease may be complicated by abscess.
Primary retroesophageal abscesses occur in children in association with local infections such as tonsillitis, lymphadenitis, oral and pharyngeal abscesses. These may invade the anterior cervical spine and cord.
Thyroid Tumors
Thyroid tumors occur chiefly in two diseases:
(1) simple goiter (unilateral or bilateral), and
(2) goiter with exophthalmos, tachycardia, tremor, sweating, and loss of weight (thyrotoxicosis or Grave's disease).
The tumor may look the same in these two diseases, varying in outline and consistency according to the amount of gland tissue and fibrous or cystic degeneration present. Owing to its connection with the larynx, it moves up and down when the patient swallows, but it is not attached to any other structures in the neck. The enlargement is often unilateral or largely so. If highly vascular, the tumor may vary greatly in size from moment to moment or at certain times (ie, menstruation, pregnancy). Since the normal gland can rarely be felt distinctively, atrophy of the gland (eg, in myxedema) is unrecognizable in the gland itself.
When cancer occurs in the thyroid, it may be difficult to distinguish from goiter. Malignant tumors are usually painful, grow fast, are accompanied by emaciation and anemia, are often harder and more nodulated than benign goiters, and invade the neighboring tissues and lymphatics. Histological examination is usually necessary to decide.
Torticollis and Similar Disorders
Congenital torticollis (a counterpart of club foot) is due to shortness of the muscles without spasm. It is almost always right-handed and associated with facial asymmetry. The head tilts toward the spastic sternocleidomastoideus, and the chin is rotated to the contralateral side. There is usually a palpable mass of fibrous tissue in the midline of the affected muscle in the infant. Gross asymmetrical facial distortion appears with progression.
Wry-neck spasm (tonic, rarely clonic) of the sternocleidomastoideus and trapezius may be due to irritation of the spinal accessory nerve by swollen glands, abscess, acute upper respiratory infections, scar, or tumor, but more often occurs in traumatic cervical dysarthrias or idiopathically in "rheumatic" or "nervous" individuals. The muscles are rigid and tender, presenting the same picture as congenital torticollis.
Dislocation of the upper cervical vertebrae causes a distortion of the neck much like that of torticollis. The diagnosis depends on the history of injury, the absence of true muscular spasm, and roentgenologic evidence.
Nelson points out that wry neck may also be the result of subdiaphragmatic irritation being mediated reflexly into the trapezius and cervical muscles. Subclinical visceral irritation is often the reason.
Compensatory cervical deviations:
(1) When there is marked lateral curvature of the spine, with or without Pott's disease, the head may be inclined so far to the opposite side that torticollis is simulated.
(2) When the power of the two eyes is markedly different, as in some varieties of astigmatism, the head may be habitually canted to one side to assist vision.
(3) In some cases due to none of the above causes, habitual or occupational postures may produce the condition.
(4) Forced attitude from cerebellar disease may resemble torticollis. The diagnosis depends on other evidence of intracranial disease, however.
Cervical Pott's Disease
Cervical vertebral tuberculosis has the characteristics of joint tuberculosis; viz, stiffness due to muscular spasm, malposition of the bones and of the head, and abscess formation. Physical diagnosis depends greatly on wry neck with stiffness of the muscles of the back and neck and pain in the occiput a characteristic symptom group. The patient is very protective of neck motion. The chin is often supported by the hand if an abscess is present. Tenderness is present posteriorly on percussion and anteriorly on palpation where an abscess may be felt. Neck pain exists both day and night, often relieved somewhat when recumbent, frequently radiating to the occiput and shoulders. Rheumatic or traumatic torticollis, however, may present all these symptoms, and diagnosis may be impossible without the aid of other tests and roentgenology. If in Pott's disease the abscess causes pressure on the anterior spinal cord, a usually spastic paralysis occurs which is characterized by hyperactive reflexes, positive Babinski, sustained clonus, and difficulty or inability to void.
Branchial Cysts and Fistula
These disorders, due to persistence of parts of the fetal branchial clefts, are not considered uncommon. A branchial cyst is a globular or ovoid fluctuating sac, hanging or projecting from the side of the neck or the region of the hyoid bone, painless and slow growing. It may transmit the motions of the carotids and be mistaken for aneurism but has no expansile pulsation and occurs in youth when aneurism is practically unknown. Some such cysts may be emptied by external pressure. Branchial cysts may contain serous, mucous, or serosanuineous fluid, or hair and sebaceous material; accordingly, as their lining wall is derived from ectoderm or entoderm. Diagnosis depends on the position and consistency of the growth and on the results of aspiration.
Congenital branchial fistulae may open externally in the neck and occasionally are complete from neck to pharynx. They may become occluded and result in suppuration.
Actinomycosis
Actinomycosis, though it usually arises in the lower jaw, may appear externally in the neck. A dense infiltration with bluish semifluctuating areas in it, but without any distinct lumps or sharp outlines, is strongly suggestive. Fistulae may form but are less common than in tuberculosis.
Neck Trauma
Physical accidents (eg, slips and falls), athletic and recreational injuries, and automobile accidents are the common causes of cervical trauma. Effects may be found in the soft tissues, discs, or bone fracture and/or a degree of dislocation.
In youth, acquired torticollis, atlantoaxial and other cervical subluxations, axial epiphyseal injury, and atlas fracture are common. Congenital fusions and stenosis may predispose a child to spinal cord trauma during a sporting activity.
Cervical sprain and disc rupture are more common in adults. Cervical sprain in adults, associated with great generalized pain and muscle spasm, is more common than in children because of the reduced elasticity of supporting tissues. Pain is often referred when the brachial plexus is involved, in which case there will be arm and hand paresthesias and occipital headache.
Degenerative Disc Disease
The cervical spine is subject to degenerative disc disease because of its great mobility and because it serves as a common site for various bony congenital defects. Bone changes are more common posteriorly in the upper cervicals and anteriorly in the lower cervicals. Cervical degenerative changes can be seen in about half the people at 40 years of age and 70% of those at 65 years, many of which may be asymptomatic. However, cervical stiffness, muscle spasm, spinous process tenderness, and restricted motion is common. When pain is present, it is usually poorly localized and often referred to the occiput, shoulder, between the scapulae, arm or forearm (lower cervical lesion), and may be accompanied with paresthesias. Radicular symptoms are rarely present unless a herniation is present.
Cervical Spondylosis
Cervical spondylosis may produce compression of either the nerve root or spinal cord. Deep tendon reflexes in the area are decreased or absent. Preexisting spinal stenosis, thickened ligamentum flavum, herneated disc, and spur formation not uncommonly complicate the picture of cervical spondylosis. There is almost no correlation between the degree of perceived pain in the neck and the degree of arthritic changes noted in x-ray films.
The classic picture is one of a middle-aged person with greatly restricted cervical motion with marked muscle spasm, positive cervical compression test, insidious neck and arm pain and paresthesia aggravated by sneezing or coughing, acute radiculopathy from superimposed disc herniation (central herniation produces central neck pain while lateral herniation produces upper extremity pain), and there are usually some muscle weakness and atrophy or fasciculations.
Specific signs of acute disc herniation are:
C4–5 disc rupture: shoulder and arm pain and paresthesia, hypesthesia of 5C root distribution, deltoid or biceps weakness.
C5–6 disc rupture: hypesthesia of lateral forearm and thumb, biceps and supinator weakness.
C6–7 disc rupture: hypesthesia of the index and middle fingers, triceps, and grip weakness.
C7–T1 disc rupture (uncommon): ulnar hypesthesia and intrinsic muscle weakness in the hand.
Due to the constant weight of the head, postural strains, occupational insults, degrees of congenital anomalies, post-traumatic or post-infection effects, with or without an associated disc involvement, the development of chronic degenerative spondylosis offers some distinct progressive characteristics:
(1) flattening of the cervical spine from muscular spasm and adhesion development,
(2) A–P fixation and restricted mobility,
(3) thinning of the atlanto-occipital and atlantoaxial articular plates resulting in motion restriction,
(4) middle and lower cervical disc wearing and thining which narrows the IVFs,
(5) disc thining and weakness encouraging disc herniation contributing to nerve encroachment,
(6) osseous lipping and spur formation with extensions into the IVFs, and (7) infiltration and ossification of perivertebral ligaments adding to inflexibility and pain upon movement.
Nelson points out that head weight and postural strains are overemphasized. "Using the findings of Mackenzie as a start, Bennett has established clinically that unless overt trauma can be shown, most neck problems are the result of reflex vasospasm where the reflex originates in the viscera below the diaphragm. Everyone would be affected if weight of the head and postural strains were common causes."
Tumors of the Cervical Spine
Metastatic tumors are more common in adulthood than in youth. In men, metastasis is usually from the prostate gland or lung; in women, from the breast. Most tumors are associated with some degree of bone destruction. A mass may or may not be palpable. Osseous tumors, benign or malignant, intramedullary or extramedullary, uncommonly occur in youth.
Neck pain is usual, and paralysis may or may not be present. In metastatic lesions, pain is constant, day and night, and not relieved with rest. Pain is increased by palpation, percussion, and movement. Cord tumors usually present pain with an insidious onset but other early neurologic symptoms and signs are not always present.
Lhermitte's Test: With the patient sitting, flexing of the patient's neck and hips simultaneously with the knees in full extension may produce sharp pain radiating down the spine and into the upper or lower extremities. When such a pain is present, this positive sign suggests irritation of the spinal dura matter either by tumor or a protruded cervical disc.
Meniere's Disease
Lewit writes of the relationship of the cervical spine to Meniere's disease (Review of Czechoslovak Medicine, 1961, VII:2) after 120 cases of Meniere's disease and similar forms of vertigo were sent by leading ear departments of Prague for manipulative treatment. The conclusions reached were:
The results of manipulative treatment in Meniere's disease whether there is any noticeable symptomatology from the cervical spine at the same time or not and in cases of vertigo (Barre-Lieou syndrome) are practically the same.
There are gradual transitions between all the groups of vertigo, sometimes even in one and the same patient.
The vertebral origin of Meniere's disease can frequently be directly proved by the aid of tests; ie, experimentally. Thus cases of cervical origin can be diagnosed from the start. And
although Meniere's disease (labyrinthine vertigo) may be provoked by other ways than that of the cervical spine; eg, by labyrinthitis, it appears that we have to do with a syndrome that in the large majority of cases is connected with functional disturbances of the cervical spine; therefore, it should be indicated for manipulative treatment."
Lower Cervical Subluxations
A subluxation of one or more of the lower cervical vertebrae often involves the brachial plexus (C4–T1). Inasmuch as the distribution of the brachial plexus is so extensive, a multitude of abnormal reflections may be seen in areas of distribution which must be appreciated by knowledge of the pathophysiology involved.
A few of the more common disturbances caused by lower cervical subluxations would include shoulder neauralgias including "frozen shoulder", neuralgias along the medial arm and forearm or elbow, unclassified wrist drop and hand dystrophies, acroparesthesia, weak grip strength, and vague "rheumatic" wrist or hand complaints.
Cervical Rib and Related Syndromes
A cervical rib arising from the 7C and ending free or attached to the T1 rib appears in the neck as an angular fullness which may pulsate owing to the presence of the subclavian artery on top of it. It rarely produces any symptoms and is generally encountered when percussing the apex of the lung. The bone can be felt behind the artery by careful palpation in the supraclavicular fossa and demonstrated by roentgenology. Pain or wasting in the arm, and occasionally thrombosis or gangrene, may occur.
The symptoms of cervical rib and scalenus syndrome are similar and since the scalenus anticus muscle is the primary factor in the production of neurocirculatory compression, whether a cervical rib is present or not, it is appropriate to group the two conditions under one heading. The scalenus anticus and cervical rib syndrome is sometimes called Coote's syndrome, Coote-Hunauld-Cooper syndrome, Adson's syndrome, or Naffziger's syndrome.
When symptoms are presented, they are usually from compression of the lower cord of the brachial plexus and subclavian vessels such as paresthesias and pain in the ulnar nerve distribution. Pain is worse at night because of pressure from the recumbent position. Pain of varying intensity, tiredness and weakness of the extremity, finger cramps, numbness, tingling, coldness of the hand, areas of hyperesthesia, muscle degeneration in the hand, a lump at the base of the neck, tremor, and discoloration of the fingers are characteristic. Work and exercise accentuate the symptoms, while rest and elevation of the extremity relieve the symptoms. Adson's and other such signs will be positive. The 4th and 5th decades mark the highest incidence, probably because of regressive muscular changes. Trauma may be a factor. Aneurysms of the subclavian artery are rare. Differential diagnosis must exclude infectious neuritis, arthritis of the shoulder joint, cervical arthritis, subachromial bursitis, deformities, and cardiac disease.
The cervicobrachial syndrome is similar to the scalenus anticus syndrome but some authorities are of the opinion that the vascular and nerve trunk symptoms should be expressed by a more inclusive term. The symptoms are classified into neurologic symptoms, vascular symptoms, or a combination of the two. Compression of nerve tissue results in numbness, pain, paralysis, and loss of function. Compression of vascular structures results in moderate pain, edema, swelling, obstruction of circulation resulting in cloting within the vessels with possible consequent infarction in the tissues supplied. These unilateral phenomena are limited to the cervicobrachial distribution. The etiologic theories of the cervicobrachial syndrome are compression of the nerve trunks, trauma to nerve trunks, injuries to the sympathetic and vasomotor nerves, trauma to the scalenus anterior muscle, embryologic defects, postural or functional defects, narrowing of the upper thoracic cap as a result of adjacent infections or anatomic defects, acute infection producing myositis, intermittent traumatism to the subclavian artery, or a cervical rib.
Orthopedic and Neurovascular Compression Tests
As there are several syndromes to consider under the classification of neurovascular compression syndromes (also termed thoracic outlet or inlet syndromes), each of which may produce the symptom complex or radiating pain over the shoulders and down the arms, atrophic disturbance, paresthesias, and vasomotor disturbances. It is also important to keep in mind that these syndromes do not necessarily give the cause of the problem. In some cases, poor posture, anomalies, muscle contractures, or other factors may be responsible. In addition, subluxation syndromes may initiate these and other disturbances the shoulder girdle and must be further evaluated. Differentiation must be made wherever possible.
Always x-ray prior to performing a cervical compression test, especially when the patient has been involved in an accident, to rule out possible disc compression, line fracture, avulsion, gross subluxation, or dislocation.
Jahn and others offer the following as standard orthopedic tests of the cervical region.
NOTE: Any test that involves rotation and extension of the spine may be contra-indicated in any new or existing patient who presents with signs suggestive of the onset of a transient ischemic attack. Please refer to the Stroke and Chiropractic for more on that topic.
Active Cervical Rotary Compression Test
With the patient sitting erect, the examiner observes from the front while the patient voluntarily laterally flexes his head toward the side being examined. With the neck flexed, the patient is then instructed to rotate his chin towards the same side. This lateral flexion and rotation by the patient narrows the IVF diameters. Findings of pain or reduplication of other symptoms probably indicates a physiologic narrowing of one or more IVFs.
Passive Cervical Rotary Compression Test
With the patient sitting, the examiner stands behind the patient and the patient's head is laterally flexed and rotated slightly toward the side being examined. The examiner places both hands with interlocked fingers on the vertex of the patient's head and gently presses caudally. If an IVF is physiologically narrowed, this maneuver will further insult the foramen by compressing the disc and narrowing the IVF, causing pain and reduplication of other symptoms.
Cervical Hyperextension Compression Test
With the patient sitting, the examiner stands behind the patient and the patient's neck is extended by the examiner. The examiner then places interlocked hands on the patient's vertex and gently presses caudally. If an IVF is physiologically narrowed, this maneuver mechanically compromises the IVF diameters bilaterally, causing pain and reduplication of other symptoms.
Shoulder Depression Test
With the patient sitting, the examiner stands behind the patient and the patient's head is laterally flexed away from the side being examined. This is done by the doctor stabilizing the patient's shoulder with one hand and applying pressure along side the patient's head with the palm of the other hand.
This maneuver stretches the dural root sleeves and nerve roots, aggravating radicular pain if the nerve roots are adhered to the foramina. Extravasations, edema, encroachments, and conversion of fibrinogen into fibrin may result in interfascicular, foraminal, and articular adhesions and inflammations that will restrict fascicular glide and the ingress and egress of the foraminal contents. Thus, pain and reduplication of other symptoms during the test probably indicate adhesions between the nerve roots and the capsular structures within the IVF.
Cervical Distraction Test
With the patient sitting, the examiner stands to the side of the patient, placing one hand under the patient's chin and the other hand under the base of the occiput. The doctor slowly and gradually lifts (distracts) the patient's head to remove its weight from the cervical spine. Such a maneuver widens the IVFs, decreases the pressure on the joint capsules around the facet joints, and stretches the paravertebral musculature. If the maneuver decreases pain and relieves other symptoms, it is a probable indication of physiologic narrowing of one or more IVFs, cervical facet syndrome, or spastic paravertebral musculature.
Cervical Percussion
The examiner percusses either manually or with a reflex hammer:
(1) over the cervical spinous processes and
(2) along the paravertebral muscles.
Pathophysiologic changes in a sprain are formation of hematoma with swelling or edema; while in a strain, changes are an irritative or inflammatory process with swelling, edema, and discomfort on function of the tendon or muscle. By percussing over these areas of inflammation, there is caused a proprioceptive input into the cord via the lateral spinothalamic tract which is interpreted as pain or tenderness by the patient. Thus,
(1) if pain or tenderness is elcited during the test over the spinous processes, a ligamentous or joint sprain is probably indicated;
(2) if pain is elicited along the paravertebral muscles, then injury of the muscle-tendon unit is probably present. Pain elicited along both the spinous processes and the paravertebral muscles suggests a sprain-strain injury.
The cervical spine is highly flexible because of its structural osseous and ligamentous design. The vertebral bodies are relatively small, yet stability is maintained because of interlocking oblique posterior intervertebral articulations of adjacent segments and their articular capsules. The chief band of union between the the vertebrae is made by the tough yet elastic IVDs, assisted mainly by the anterior and posterior longitudinal ligaments, the interspinal and supraspinal ligaments, and the ligamenta flava. All discs are ovid in shape with convex superior and inferior surfaces. The ends of the fibrocartilagenous framework of the discs are embedded in the bodies of adjacent vertebrae.
Cailliet points out that the vertebral nerve (sympathetic) runs along the vertebral artery within the arterial foramen of the cervical transverse processes. Irritation to this nerve is considered to occur from mechanical irritation to the vertebral artery anywhere along its course producing symptoms of a vasomotor nature; eg, headache, vertigo, tinnitus, nasal disturbances, facial pain, facial flushing, and pharyngeal paresthesias. Although sympathetic fibers have not been found along the cervical nerve roots, surgical decompression of an entrapped nerve root relieves symptoms attributed to the sympathetics. The mechanism is unclear. Lesser occipital nerve neuralgia: involving the area of the occipitalis muscle, mastoid process, and upper posterior aspect of the auricle. Greater auricular nerve neuralgia: extending in front and behind the auricle, skin over the parotid gland, paralleling the distribution of the auriculotemporal branch of the trigeminus and easily misdiagnosed as chronic trifacial neuralgia. Cervical cutaneous nerve neuralgia: involving the area of the middle third of the platysma to the midline, possibly extending from the chin to the sternum. Supraclavicular nerve neuralgia: depending upon which rami are affected, the neuralgia may involve the suprasternal area, pectoral area, or deltoid area. Thus, sternoclavicular and acromioclavicular neuralgias may originate in the spinal levels of the supraclavicular nerve.
De Rusha points out that dysphagia and dysarthria may at times be due to upper cervical involvement rather than a central nervous system situation. The C1 joins the hypoglossal cranial nerve which supplies the intrinsic muscles of the tongue. It then descends to join the descending cervical which is derived from C2 and C3. A loop of nerves, the ansi hypoglossi which supplies muscles necessary for degutition and speaking, is derived from C1–3.
Scalene Maneuver (Adson's Test)
With the patient sitting, the doctor palpates the radial pulse and directs the patient to bend the head obliquely backward to the opposite side being examined, take a deep breath, and tighten the neck and chest muscles on the side tested. The maneuver decreases the interscalene space (anterior and middle scalene muscles) and increases any existing compression of the subclavian artery and lower components (C8 and T1) of the brachial plexus against the first rib.
Marked weakening or loss of the pulse or increased paresthesias indicate a positive sign of pressure on the neurovascular bundle, particularly of the subclavian artery as it passes between or through the scaleni musculature, thus indicating a probable cervical rib or scalenus anticus syndrome.
Costoclavicular Maneuver
With the patient sitting, the examiner monitors the radial pulse of the patient from the posterior on the side being examined. The examiner brings the patient's shoulder and arm posterior and then depresses the shoulder on the side being examined. This maneuver narrows the costoclavicular space by approximating the clavicle to the first rib, tending to compress the neurovascular structures between. When the shoulder is retracted, the clavicle moves backward on the sternoclavicular joint and rotates in a counterclockwise direction. An alteration or obliteration of the radial pulse or a reduplication of other symptoms is a probable indication of compression of the neurovascular bundle passing between the clavicle and T1 rib (costoclavicular syndrome).
Allen's Test
The sitting patient elevates his arm and is instructed to make a tight fist to express blood from palm. The examiner occludes radial and ulnar arteries by finger pressure. The patient lowers hand and relaxes fist, and examiner releases arteries one at a time. Some examiners prefer to test the radial and ulnar arteries individually in two tests. The sign is negative if the pale skin of the palm flushes immediately when the artery is released. The patient should be instructed to not hyperextend the palm as this will constrict skin capillaries and render a false positive sign. The sign is positive if the skin of the palm remains blanched for more than 3 seconds. This test, which should be performed before Wright's test, is significant in vascular occlusion of the artery tested.
Wright's Test
With the patient sitting, the radial pulse is palpated from the posterior in the downward position and as the arm is passively moved through an 180° arc. If the pulse diminishes or disappears in this arc or if neurologic symptoms develop, it is suspect of pressure on the axillary artery and vein under the pectoralis minor tendon and coracoid process or compression in the retroclavicular spaces between the clavicle and first rib, thus a hyperabduction syndrome.
Eden's Test
With the patient sitting, the examiner palpates radial pulse and instructs the patient to pull shoulders backward and throw the chest out in a "military posture" manner and to hold deep inspiration as the pulse is examined. Test is positive if weakening or loss of pulse occurs, indicating pressure on the neurovascular bundle as it passes between the clavicle and the 1st rib, thus a costoclavicular syndrome.
Major Effects of Upper Cervical Subluxations
A circular transverse-process foramen transmits the vertebral artery, vein, and associated vertebral plexus of sympathetic nerves, and each transverse process has a deep groove for a spinal nerve which is bounded anteromedially by the uncinate ridge. In the cervical region, the transverse processes lie opposite the first spinous-process interspace above.
To accommodate for the spinal cord's cervical enlargement and cervical mobility, the vertebral canal is shaped as a rounded triangle larger than that of the lower regions. In the cervical region, the IVFs are bounded anteriorly by the bodies of two adjacent vertebrae and the IVD; posteriorly, by the articular processes; and superiorly and inferiorly, by the pedicles. In all regions of the spine, the greatest diameter of the IVF is from superior to inferior, and the smallest diameter is from anterior to posterior. Thus, the foramina are oval.
Frequent anomalies in the cervical area predispose subluxations from minor stress. The weight of the head along with postural and occupation stress frequently leads to chronic degenerative spondylosis often superimposed upon asymptomatic anomalies. Clinically, a vicious cycle is seen where subluxation contributes to degenerative processes and these processes contribute to subluxation.
The circulation of the spinal cord and much of the brain is directly proportional to spinal movement. Thus, loss of mobility of any one or more segments of the spine correspondingly influences circulation. The resulting partial anoxia has a harmful influence upon nerve function.
All spinal nerves are oval in shape, and each has its long diameter lying in the plane of the short diameter of the IVF. Each nerve is embedded in areolar tissue which connects it to the borders of the foramen and suspends it within the foramen. The artery and vein supplying a spinal nerve are situated in the foramen between the nerve and the fibrous tissue in the anterior portion of the foramen. It is unlikely that circulation to the nerve would be be disrupted without first irritating or compressing the nerve because the arteries and veins are much smaller, blood pressure within the lumen makes them not easily compressed, and nerve tissue is much more responsive to encroachment irritation.
Once a vertebra loses its ideal relationship with contiguous structures (subluxation) and becomes relatively fixed at some point (fixation) within its normal scope of movement, it is no longer competent to fully participate in ideal coordinated spinal movement. The subluxated-fixated area becomes the target for unusual and abnormal stresses, weight bearing and otherwise. In addition to the attending circulatory, neuromechanical, and static changes in the involved area, there is disturbed reflex activity which may manifest itself in such objective symptoms as changes in superficial and deep reflexes, hyperkinesia, pupiliary changes, excessive lacrimation, tremors and spasms. Symptoms are expressed over the autonomic bed as cardiac arrythmia, glandular disturbances, and changes in gastrointestinal activity.
Vertebral Veins and Deep Cervical Veins
Spasm of the suboccipital muscles may cause a decided impediment of venous drainage from the suboccipital area via vertebral and deep cervical veins resulting in a passive congestion with consequent pressure upon the sensory nerve endings in the area. This is perceived by the patient as unilateral or bilateral pain and a throbbing discomfort, and may be palpated as knotty lumps within the suboccipital musculature. The condition appears to be of a reflex nature more common among people under mental tension or those who work closely with their eyes.
Vertebral Arteries
Janse relates that any cervical subluxation (particularly atlantal, axial, or occipital) producing muscle spasm, may produce constriction unilaterally or bilaterally of the vertebral arteries resulting in circulatory impediment. An extensive number of symptoms may follow, of which only a few of the major ones are:
Cerebrospinal Circulation
Any event that would cause constriction in the connecting area between the cerebral subarachnoid space and the vertebral canal limits the cerebrospinal fluid to escape into the inferior vertebral canal, resulting in a degree of increased intracranial pressure. The clinical picture is usually one of intractable recurring headaches, mild or moderate cerebellar syndromes, etc.
An atlanto-occipital subluxation may cause the dura matter of the cisterna cerebellaris to be pressed against the posterior medullary velum and partially occlude the foramina of Luschka and Magendie interfering with flow from the 4th ventricle. The resulting increase of intraventricular fluid accumulation may create a large variety of symptoms such as deep-seated intractible "internal pressure" headaches, nausea, tendency towards projectile vomiting, bizzare and unusual visual disturbances, and protopathic ataxias.
Medulla Oblongata
The medulla oblongata extends well into the lower reaches of the foramen magnum and the ligamentous ring that connects it with the atlas, thus any type of occiput or atlantal subluxation may produce abnormal pressure on this portion of the brain stem.
Bilateral posterior shifting of the occiput or atlas may cause pressure upon the pyramids or adjacent olivary bodies producing a syndrome of upper motor neuron involvement characterized by spastic paralysis or a degree of ataxia.
A lateral shifting of the occiput may cause pressure upon the tubercle of Rolando producing pain in the trigeminal distribution, headache, sinus discomforts, occular neuralgias, and dull aches in the jaws.
Superior Cervical Ganglion
Rotary subluxations of one or more of the upper three vertebrae (particularly the axis) may cause pressure upon the superior cervical ganglion. The syn- drome produced may incorporate excessive facial and forehead perspiration, dry mouth and nasal mucous membranes, dryness and tightness of throat, dilated pupils tending towards exopthalmos, pseudo-migrainous attacks due to unilateral angioneurotic edema, facial vasomotor disturbances with possible angioneurotic swelling, and moderate tachycardia with functional arrythmias.
Vagus Nerve (X Cranial)
As the vagus lies almost in immediate contact with the transverse process of the atlas, rotary subluxation of the atlas may cause pressure producing a wide range of symptoms. The syndrome produced may exhibit as nasal and sinus congestions, swallowing and speech difficulties, cardiac arrythmias, functional coronary artery spasm, gastric and intestinal colic, and other symptoms of vagal disturbance.
Greater Occipital Nerve (C2)
Rotary subluxations of the axis are common mechanical causes of cervical migraine. This cervical neuralgia is invariabley unilateral, beginning in the upper neck and extending over the skull into the temporal and possibily orbital areas by myalgia extension.
Cervical Plexus (C1–4)
In considering the effects of upper cervical distortion, De Rusha emphasizes the fact that the dura mater of the spinal cord is firmly fixed to the margin of the foramen magnum and to the 2nd and 3rd cervical vertebrae. In other spinal areas, it is separated from the vertebral canal by the epidural space. Since both the C1 nerve and the vertebral artery pass through this membrane and both are beneath the superior articulation of the atlas and beneath the over-hanging occiput, it is responsible to except that atlanto-occipital distortion may cause traction of the dura mater, thus producing tractional irritation of the artery and nerve unilaterally and compressional occlusion contralaterally. This helps us understand those cases of suboccipital neuralgia where a patient upon turning his head to one side increases headache and vertigo which are relieved when the head is turned in the opposite direction.
In addition, there is a synapse between the upper cervical nerves and the great sensory nerve of the head and face (trigeminal) which also supplies the dura mater. This explains why irritation of suboccipital C1 results in a neuralgia not only confined to a small area at the base of the skull but is also referred to the forehead or eye via the supraorbital branch of the trigeminal. The greater occipital (C2) does not tend to do this, but (emitting as it does between the posterior arch of the atlas and above the lamina of the axis) refers pain over the vertex and top of the head.
The superficial sensory cutaneous set of the cervical plexus (C1–4) is frequently involved in subluxations of the upper four segments, particularly when there are predisposing spondylotic degenerative changes. Janse describes four resultant neuralgias:
Irritative lesions involving the cervical region and its articulations may in turn irritate the sympathetic nerve plexuses ascending into the head via the vertebral and carotid arteries. Many cases of visual and aural symptoms are commensurate with upper cervical distortion wherein the arch of the atlas snugly hugs the occiput, thus possibly irritating the sympathetic plexus of nerves on the vertebral arteries as well as partial compression of the vessels. To appreciate this, we must remember that the visual cortical area of the occipital lobe (cuneate lobe and calcarine fissue area) require an ideal blood supply which is dependent on the sympathetics ascending the great vessels of the neck, and this holds true for the inner ear as well. To test this syndrome, De Rusha suggests having the supine patient read some printed matter while the examiner places gentle traction on the skull cephally, separating occipital and atlantal articulations. A positive sign is when the patient, often to his surprise, experienecs momentarily enhanced visual acuity or a reduction in tinnitus.
Phrenic Nerve (C3–5)
A subluxation of one or more of the C3, C4, or C5 segments may involve the phrenic nerve and produce symptoms of severe chronic hiccough and other diaphragmatic disorders.
Occipital and Upper Cervical Vertebral Listings
There are no bony intervertebral foramina for passage of C1 and C2 spinal nerves, thus avoidance of IVF encroachment as in the lower spine. Disturbances usually arise from muscular spasm of one or more of the six muscle bundles which have their origins and insertions on the occiput, atlas, or axis. Unequal tension and untimate fibrotic changes within the paravertebral structures can readily influence the delicate nerve fibers and vascular flow.
Neurologic disturbances may result from muscular and fibrotic changes along the cranial nerve pathways which emit from the skull and pass intimately between and under suboccipital fasciculi. Five of the cranial nerves are thus vulnerable: facial, glossopharyngeal, vagus, spinal accessory, and hypoglossal. In addition, circulatory impairment of major and minor nerves of the neck may alter the function of those cranial nerves that do not exit from the skull proper such as the olfactory, optic, oculomotor, trochlear, trigeminal, abducens, and auditory, but which are contained within the cranium and remote from vertebral subluxation encroachment effects.
Nelson points out that we should not overlook the fact that it is essentially muscle which produces and maintains the subluxation. Concern must be given to why the subluxation is produced.
Positional Listings
Inasmuch as all freely movable articulations are subject to subluxation, the atlanto-occipital diarthrosis is no exception. The stress at this point is unusual when one considers that the total weight of the cranium (about 10% of total adult weight) is supported by the ring of the atlas 1/20th the circumference of the skull and a variety of spinal muscles, subject to spasm, have their attachments on the occiput.
Occipital listings are usually made on the basis of condyle position. The common listings are:
| I | Bilaterally inferior (suboccipital jamming) |
| LI | Left inferior |
| LS | Left superior |
| LIP | Left inferior and posterior |
| LIA | Left inferior and anterior |
| LSP | Left superior and posterior |
| LSA | Left superior and anterior |
| RI | Right inferior |
| RS | Right superior |
| RIP | Right inferior and posterior |
| RIA | Right inferior and anterior |
| RSP | Right superior and posterior |
| RSA | Right superior and anterior |
| L | Lateral left |
| R | Lateral right |
| I | Inferior posterior arch and superior posterior arch |
| S | Superior posterior arch and inferior anterior arch |
| LSA | Left, superior, and anterior |
| LP | Left posterior rotation (Sp. PR) |
| LA | Left anterior rotation |
| RSA | Right, superior, and anterior |
| RP | Right posterior rotation (Sp.PL) |
| RA | Right anterior rotation |
| A | Bilaterally anterior |
| LI | Left inferior |
| LP | Left posterior |
| LIP | Left inferior and posterior (Sp. PRS) |
| LSP | Left superior and posterior (Sp. PRI) |
| RI | Right inferior |
| RP | Right posterior |
| RIP | Right inferior and posterior (Sp. PLS) |
| RSP | Right superior and posterior (Sp. PLI) |
SUBOCCIPITAL JAMMING This common subluxation of a trigeminal (ophthalmic division) reflex nature is often seen in people under severe visual or mental stress. Irritative impulses result in contraction of the suboccipital musculature which pulls the occiput down upon the posterior arch of the atlas creating a painful bilateral condylar jamming. Palpation discerns suboccipital spasm, tenderness, nodular swellings, and an approximation of the inferior nuchial ridge upon the posterior arch of the atlas.
RIGHT OR LEFT CONDYLE INFERIOR A unilateral suboccipital muscle spasm causes the affected condyle to be pulled down into the articulating concavity of the atlantal lateral mass on one side. This may not be attended by a degree of rotation. The term "sunken" condyle is often used in designation of the condition. Listing is RI or LI. Inspection from the back shows a low medially inclined mastoid process and ear on the side of involvement. Palpation discloses the mastoid riding close to the transverse process of the atlas, tension and tenderness in the groove between themastoid and the lower jaw, and fullness in the groove between the occiput and the posterior ring of the atlas on the side of involvement.
RIGHT OR LEFT CONDYLE SUPERIOR Many authorities consider this subluxation (RS or LS) the converse aspect of a right or left condyle inferior (RI or LI). That is, as one condyle is pulled inferior and anterior, for instance, the other condyle will present a superior and posterior picture, or vice versa. Some authorities, however, feel there are certain situations which indicate a unilateral abnormality without converse adaptation.
RIGHT OR LEFT INFERIOR CONDYLE WITH ASSOCIATED ANTERIOR ROTATION All occipital-atlantal movements are inclined to be associated with a degree of rotary movement because the occipital condyles and the articulating surfaces of the lateral masses of the atlas approximate each other more at the anterior than the posterior. Thus most sunken condyles will be associated with a relative amount of rotation. The listing would be either RIA or LIA. On the side of involvement:(1) inspection from the back will show a medial head tilt accompanied by less of the face showing from the effect of anterior rotation;
(2) palpation will reveal approximation of the mastoid and transverse process of the atlas and approximation of the inferior nuchal ridge and the posterior arch of the atlas on the involved side. These points will be widened on the opposite side.
RIGHT OR LEFT SUPERIOR CONDYLE WITH ASSOCIATED POSTERIOR ROTATION Again, many consider this subluxation (RSP or LSP) the contralateral aspect of a right or left inferior condyle attended by an anterior rotation (RIA or LIA). Illi feels this type of subluxation is always attended by a degree of arthritis and determines the primary subluxation roentgenologically by the side showing the greatest degree of degenerative articular alterations.
RIGHT OR LEFT INFERIOR CONDYLE WITH ASSOCIATED POSTERIOR ROTATION This subluxation (RIP or LIP) or its contralateral representation (RSA or LSA) is less common than a RIA or LIA subluxation. It is usually the result of vigorous twisting trauma such as in athletic activities. On the side of involvement:(1) inspection from the back shows the head held in a stiff inferior position with some posterior deviation; ie, there will be a medial head tilt on the side of involvement with more of the face showing from the effect of posterior rotation;
(2) palpation discloses a mastoid that is inferior and posterior in relation to the transverse process of the atlas, and the inferior nuchal ridge approximating the posterior arch of the atlas.
RIGHT OR LEFT SUPERIOR CONDYLE WITH ASSOCIATED ANTERIOR ROTATION This subluxation (RSA or LSA) is usually considered the contralateral aspect, and associated with opposite findings, of the above RIP or LIP listing.
Common Atlas Subluxations
RIGHT OR LEFT LATERAL ATLAS This atlantal side slip between the atlas and axis articulations is usually attended by a degree of superiority and anteriority on the side of laterality because of the inclination of the articulating surfaces (LSA or RSA). Only in cases of severe twisting trauma or force will this not be the case. On the side of involvement, palpation will disclose the transverse process of the atlas to be more lateral and slightly superior and anterior than its counterpart.
BILATERAL SUPERIOR OR INFERIOR ATLAS In this type of subluxation, the atlas tips up or down bilaterally (S or I) in its transverse axis without an attending sideslip. Deep palpation may reveal the posterior arch of the atlas either approximating the occiput with a gap between the posterior tubercle of the atlas and the spinous of the axis (S) or approximating the spinous process of the axis with a gap between the posterior tubercle and the occiput (I).
RIGHT OR LEFT ANTERIOR ROTATIONS OF THE ATLAS These subluxations are often associated with vagal syndromes because the anteriorly rotated transverse of the atlas may easily cause pressure on the vagus nerve. In such a rotatory state, the counterpart of an atlas listed right anterior (RA) would be left posterior (LP). On the side of involvement:(1) inspection from the back reveals suboccipital fullness, and
(2) bilateral palpation of the posterior ring of the atlas reveals a prominence on the side of posteriority, with the transverse process of the atlas being closer to the mastoid and its counterpart closer to the lower jaw.Another test, suggested by Goodheart, is to have the patient lying supine, then passively rotate the head right and left. If the anterior atlas exists on the left, the atlas has already turned to the right so that the patient's head will turn much further to the right. But when it is turned from right to left, the atlas has to first come out of its relatively anterior position on the left, thus motion is relatively restricted.
Common Axis Subluxations
With the possible exception of L5, no other vertebrae is probably subluxated more frequently than C2. The most common symptom is a unilateral suboccipital neuralgia on the side of posteriority. On the side of posteriority, palpation discloses a tender prominence over the articulating process and a deviation of the spinous process away from the midline. Some authorities feel that posterior axial subluxations are too frequently misdiagnosed as anterior atlantal subluxations.