

A Randomized Trial of Chiropractic Manipulation and
Mobilization for Patients With Neck Pain: Clinical
Outcomes From the UCLA Neck-Pain StudyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Am J Public Health 2002 (Oct); 92 (10): 1634–1641 ~ FULL TEXT
OPEN ACCESS Eric L. Hurwitz DC, PhD • Hal Morgenstern PhD • Philip Harber MD, MPH
Gerald F. Kominski PhD • Fei Yu PhD • Alan H. Adams DC, MS
Department of Epidemiology,
UCLA School of Public Health,
University of California-Los Angeles,
Box 951772, Los Angeles, CA 90095-1772, USA
Objectives: This study compared the relative effectiveness of cervical spine manipulation and mobilization for neck pain.
Methods: Neck-pain patients were randomized to the following conditions: manipulation with or without heat, manipulation with or without electrical muscle stimulation, mobilization with or without heat, and mobilization with or without electrical muscle stimulation.
Results: Of 960 eligible patients, 336 enrolled in the study. Mean reductions in pain and disability were similar in the manipulation and mobilization groups through 6 months.
Conclusions: Cervical spine manipulation and mobilization yield comparable clinical outcomes.
From the FULL TEXT Article:
Background
Neck pain is one of the most prevalent and costly health problems in the United States. [1-3] Among US residents, 50% to 70% will experience neck pain at least once in their lives, [4-6] as many as one third are affected each year, [4] and about 10% suffer from neck pain at any given point in time. [4, 7] Neck pain is the second most prevalent chief complaint reported by patients seeking chiropractic care, and it follows only low back pain as the most common reason for provision of manipulative therapy. [8, 9] An estimated 31% of all alternative health care visits occurring in the United States in 1997 were visits to chiropractors.9
There is little information available from randomized clinical trials to support manipulation, mobilization, or other approaches for treating neck pain. [10, 11] A 1996 systematic review of randomized clinical trials involving cervical spine manipulation and mobilization revealed that manipulation or mobilization may be more effective than muscle relaxants or usual medical care in producing short-term pain relief among some patients; however, manipulation was found to be associated with rare but serious complications. [10] The Quebec Task Force on Whiplash-Associated Disorders concluded that the value of manipulation has not been established for patients with postwhiplash head and neck symptoms [12] and that mobilization may be effective for some patients in the short term, but long-term effectiveness is unknown. [12]
Although 2 previous randomized clinical trials compared the immediate effects of manipulation and mobilization on neck pain, [13, 14] no published studies, to our knowledge, have assessed the long-term effectiveness of manipulation vs mobilization for patients with neck pain. Despite being the 2 most common physical therapeutic modalities that chiropractors use as adjuncts to spinal manipulation, [8] heat and electrical muscle stimulation (EMS) have not been tested in a randomized design. The purpose of the present study was to assess the relative effectiveness of neck-pain treatment approaches commonly used by chiropractors.
METHODS
Study Design and Source Population
Neck-pain patients were randomized in a balanced 2 × 2 × 2 factorial design to one of the following groups: manipulation with and without heat, manipulation with and without EMS, mobilization with and without heat, or mobilization with and without EMS. Participants were followed for 6 months, with assessments for pain and disability at 2 and 6 weeks and at 3 and 6 months. The source population was made up of approximately 90,000 to 110,000 members of a Southern California health care network that had chiropractors on staff at 4 of its clinics.
Inclusion and Exclusion Criteria
Patients were eligible for the study if they(1) were health maintenance organization (HMO) members;
(2) had sought care at one of the 4 study sites from February 9, 1998, through June 30, 2000;
(3) had presented with a complaint of neck pain (defined as pain in the region from the upper thoracic spine to the occiput and the surrounding musculature);
(4) had not received treatment for neck pain in the past month; and
(5) were aged 18 to 70 years.Potential participants were excluded if they
(1) had neck pain due to fracture, tumor, infection, severe spondyloarthropathy, or other nonmechanical cause;
(2) had progressive neurological deficit, myelopathy, herniated nucleus pulposus, or severe incapacitating pain;
(3) had severe coexisting disease;
(4) were being treated with electrical devices;
(5) had a blood coagulation disorder or were using corticosteroids or anticoagulant medications;
(6) had a history of stroke or transient ischemic attacks;
(7) had plans to relocate;
(8) were not easily accessible by telephone;
(9) lacked the ability to read English; or
(10) had pain involving third-party liability or workers’ compensation.Patient Screening and Enrollment Protocol
All patients presenting with neck pain were interviewed by a field coordinator and given an information sheet describing the study. In the case of each patient who initially agreed to participate, a history was taken, a physical examination was conducted, and radiology and laboratory tests were ordered if necessary. The field coordinator administered consent forms and answered any questions.
Randomization was conducted in blocks of 12 and stratified by site. Separate groups of site-specific, sequentially numbered sealed envelopes were used in making assignments. When a patient consented to be involved in the study, the field coordinator opened the site-specific envelope in sequence, informed the patient of his or her assignment, and instructed the patient to complete the baseline questionnaire.
Treatment Protocols
All participants received information about posture and body mechanics and one or more of the following, as appropriate: stretching, flexibility, or strengthening exercises and advice about ergonomics and workplace modifications. Participants assigned to 1 of the spinal manipulation groups received at least 1 controlled dynamic thrust, applied with high-velocity and low-amplitude force with minimal extension and rotation (according to patient tolerance), directed at 1 or more restricted upper thoracic or cervical spine joint segments. Those assigned to 1 of the spinal mobilization groups received 1 or more low velocity, variable amplitude movements applied within the patient’s passive range of motion directed to 1 or more restricted upper thoracic or cervical spine joint segments. These types of manipulation and mobilization are the most common types of care delivered by chiropractors in the United States, [15, 16] and our definitions were consistent with those developed by the Mercy Center Consensus Conference in establishing guidelines for chiropractic quality assurance and practice parameters. [17]
Participants assigned to 1 of the heat groups were given a 10-minute application of moist heat before the manipulation or mobilization. Participants assigned to one of the EMS groups received a 10-minute application of this modality before manipulation or mobilization. Finally, participants assigned to receive both heat and EMS received the heat treatment and EMS simultaneously, followed by manipulation or mobilization.
Data Collection and Variables
Baseline data. We used 11-point numerical rating scales (0 = no pain, 10 = unbearable pain) to assess most severe pain and average pain intensity during the previous week. We assessed disability due to neck pain with the 10-item Neck Disability Index (NDI), [18, 19] a modified version of the Oswestry Low Back Pain Disability Index [20] with a score range of 0 to 50. The NDI has been shown to have high internal consistency and high test–retest reliability, to be responsive to change, and to correlate well with the McGill Pain Questionnaire. [19]
We assessed health status with the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36). [21] We used 5 of the 8 subscales of this previously validated instrument, those assessing(1) limitations in physical activities because of physical or emotional problems,
(2) limitations in usual role activities because of physical health problems,
(3) limitations in usual role activities because of emotional health problems,
(4) general health perceptions, and
(5) general mental health. [22]Follow-up data and outcome variables. Pain and disability were measured via 11-point scales (0 = no pain, 10 = unbearable pain) and the NDI at each follow-up assessment. Participants were interviewed at 4 weeks postrandomization regarding potential adverse reactions and satisfaction with care. The primary outcome variables were changes in neck-pain intensity and related disability. Each outcome was treated as both a continuous and a dichotomous variable. Cutpoints of 2 points or above (vs less than 2 points) on the 11-point scales and 5 points or above (vs less than 5 points) on the NDI were used as dichotomous outcomes. These cutpoints were chosen because they were most strongly associated with patients’ global assessments of their improvement (“better” or “a lot better” vs no improvement). Differences between groups of 2 or more points on the 11-point scales and 5 or more points on the NDI were considered clinically meaningful.
Statistical Analyses
The primary comparisons were as follows:(1) manipulation vs mobilization,
(2) heat vs no heat, and
(3) EMS vs no EMS.Descriptive statistics were used to summarize characteristics measured at baseline for each treatment group. Means, standard deviations, and medians were computed by treatment group for continuous variables, and frequency distributions were generated for categorical variables. Normality for each continuous variable was assessed, time trends of outcome variables within each treatment group were graphed, and differences from baseline measurements were computed and plotted over time. All analyses were intention-to-treat analyses.
Three analytic strategies were used to estimate treatment effects. First, ordinary least squares regression models were used to estimate differences in mean change for each continuous outcome from baseline to follow-up assessment. Second, logistic regression was used to estimate the effects of treatments on dichotomous outcomes. Finally, mixed-effects linear models were used to identify changes by treatment group in each outcome over the 6-month follow-up.
Age, sex, SF-36 mental health score, baseline outcome value, and history, frequency, and duration of neck pain were included as covariates in the ordinary least squares and logistic models. The mixed-effects models included the same covariates except baseline outcome value. The logistic model results were used to estimate odds ratios and 95% confidence intervals for each treatment contrast; odds ratios were then converted to risk ratios by setting the model covariates to sample means. Interaction effects between treatments were estimated and found to be clinically irrelevant and consistent with chance variation (P > .2).
RESULTS
Screening, Enrollment, and Follow-Up
We screened a total of 1848 patients. We excluded 834 patients for the following nonmedical reasons: pain not primarily in the neck (n = 283), older than 70 years (n = 169), third-party liability or workers’ compensation (n = 112), fee-for-service or non-HMO insurance (n = 104), treatment in the past month (n = 100), younger than 18 years (n = 24), inability to read English (n = 24), plans to relocate (n = 14), and not easily accessible by telephone (n = 4). Also, patients were excluded for the following medical reasons: severe coexisting disease (n = 21); fracture, tumor, infection, or spondyloarthropathy (n = 13); blood coagulation disorder or use of anticoagulant or corticosteroid medications (n = 9); history of stroke or transient ischemic attacks (n = 6); progressive neurological deficit, myelopathy, herniated nucleus pulposus, or severe incapacitating pain (n = 3); and treatment with an electrical device (n = 2).
Of the 960 eligible patients, 624 (65%) refused to participate, and 336 were enrolled. Reasons for declining participation were as follows: lack of interest (n = 460), inconvenience (n = 103), and specific treatment preferences (n = 60). One patient was not enrolled owing to cognitive impairment. Two-week and 6-week follow-up questionnaires were returned by 316 (94%) and 301 (89.6%) participants, respectively; 3- and 6-month questionnaires were returned by 292 (89.6%) and 269 (80.1%) participants.
Baseline Characteristics

Table 1

Table 2
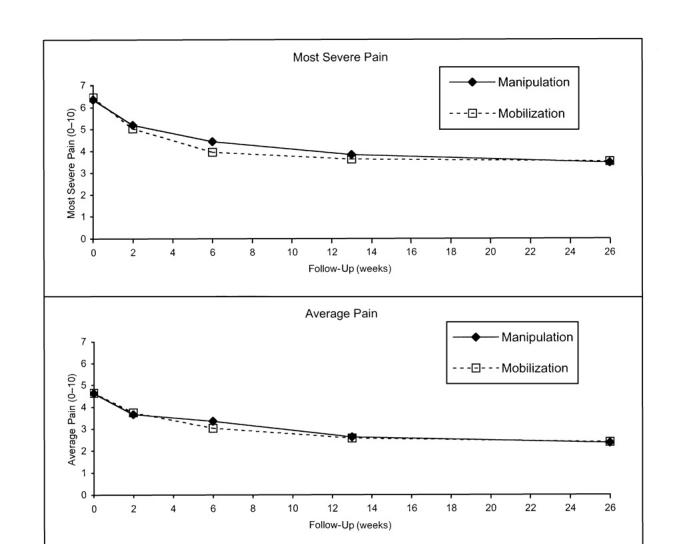
Figure 1

Table 3 Table 1 shows baseline distributions of selected sociodemographic and health characteristics by type of manual therapy. The participants were predominantly middle aged, female, White, college educated, married, and employed. Most participants had subacute or chronic pain, two thirds had headaches, and many reported having arm pain, numbness, or tingling in the past week. The majority of the NDI scores were consistent with mild to moderate disability. The treatment groups did not differ appreciably with respect to demographic or clinical factors.
Outcomes
Unadjusted mean reductions in reports of most severe pain were approximately 1.5 points at 2 weeks, 2.5 points at 6 and 13 weeks, and approximately 3 points at 6 months. Mean reductions in reports of average pain were approximately 1.3 points at 2 weeks, almost 2 points at 6 weeks, and approximately 2 and 2.5 points at 3 and 6 months, respectively. Adjusted mean changes in pain from baseline to each follow-up assessment were similar in the manipulation and mobilization groups (Table 2 and Figure 1). Participants assigned to the heat therapy condition improved slightly more, on average, than did participants not assigned to this condition; however, the differences were clinically negligible.
More than 50% of the participants exhibited pain reductions of 2 or more scale points at 6 weeks, and about 65% exhibited such reductions at 6 months. Clinical improvements in pain from baseline to each follow-up assessment were similar in the manipulation and mobilization groups (Table 3). At 2 weeks, however, clinically meaningful reductions in most severe pain were 60% more likely among those assigned to heat therapy (vs no heat).
Unadjusted mean reductions in disability (on the 0–50-point scale) were about 3.5 points at 2 weeks; 5 and 5.5 points at 6 and 13 weeks, respectively; and slightly more than 6 points at 6 months. Adjusted mean changes in disability from baseline to each follow-up assessment were similar in the manipulation and mobilization groups (Table 2 and Figure 1). About 50% of the participants exhibited disability reductions of 5 or more scale points at 6 and 13 weeks, and about 60% exhibited such reductions at 6 months; there was little difference between groups (Table 3). However, only 30% were free from clinically significant pain and disability at 6 months. Numbers of disability days were not appreciably different between the groups at any of the follow-up assessments.
Adverse Events
There were no known study-related adverse events requiring institutional review board notification. However, participants assigned to manipulation were more likely than those assigned to mobilization to experience transient minor discomfort during the initial 4-week treatment period (16% vs 8.7%; P = .051).
DISCUSSION
To our knowledge, this study is the first randomized clinical trial of manipulation vs mobilization for neck pain among chiropractic patients in managed care, the first randomized study to assess the possible effect of heat and EMS with manipulation or mobilization on patients with neck pain, and only the third randomized clinical trial to compare manipulation and mobilization for neck pain. Manipulation and mobilization with or without heat and with or without EMS yielded similar improvements in pain severity and disability after 6 months of follow-up. Although 10 randomized clinical trials have addressed the effectiveness of manipulation or mobilization for neck pain, manipulation and mobilization were directly compared in only 2 of these trials, [13, 14] and only immediate outcomes following a single treatment were measured. Whereas in the first study the 2 groups showed equivalent decreases in pain, [13] in the second study the group receiving manipulation showed an improvement in pressure pain threshold (the amount of pressure required to produce pain) in the neck. [14]
The relative effectiveness of cervical spine manipulation vs other (nonmobilization) interventions has been tested in 5 randomized clinical trials. The effects of manipulation in combination with a muscle relaxant relative to those of a muscle relaxant alone were assessed in 2 randomized clinical trials conducted among patients with subacute and chronic neck pain. [23, 24] Greater proportions of the manipulated groups reported improvement in pain 3 weeks following treatment. Another study included patients with both chronic neck pain and chronic back pain and compared manual therapy, physical therapy, placebo, and usual care by a general practitioner. [25-28] In the case of the 64 patients with neck pain, no appreciable differences in severity of pain were detected between the groups receiving the various types of therapy at 3 and 12 weeks.
Another study of subacute and chronic neck pain compared salicylate and mobilization with salicylate and massage, traction, and electrical stimulation and with a third condition involving salicylate alone. [29] After 3 weeks of treatment, the patients receiving mobilization exhibited greater improvements in self-reported pain. A 1998 randomized comparison of intensive training of the neck musculature, physiotherapy, and chiropractic manipulation for patients with neck pain of at least 3 months’ duration showed no differences between treatment groups with respect to pain, disability, or medication use. [30]
The relative effectiveness of cervical mobilization vs other (nonmanipulative) interventions has been tested in 3 randomized clinical trials. In 1 of these studies, neck collar, neck collar plus transcutaneous electrical nerve stimulation (TENS), and neck collar plus mobilization were compared in patients with neck pain of less than 3 days’ duration. [31] Although the mobilization group exhibited greater mean improvements in pain reduction at 1 week, no differences between groups were detected at 6 weeks and 3 months. The other 2 studies compared Maitland mobilization (repetitive and passive neck movements within patients’ tolerance) with other treatments for acute flexion–extension sprains. [32-34] The first compared rest plus analgesics, Maitland mobilization plus McKenzie exercises (a series of gentle neck exercises that patients are taught to perform on their own), and neck collar plus advice on posture and exercises, and the second compared Maitland mobilization and neck collar. In the first study, the groups receiving Maitland mobilization and neck collar plus advice exhibited similar decreases in pain intensity after 1 and 2 months, and these decreases were greater than those among the group receiving rest plus analgesics. In the second study, patients receiving Maitland mobilization had less pain, on average, after 4 and 8 weeks than did collar recipients.
Manipulation and mobilization are 2 of many alternative and conventional neck-pain treatments with little or no evidence to support their use. These treatments includespray and stretch, [35]
laser therapy, [36, 36]
pulsed electromagnetic therapy, [38, 39]
infrared light therapy, [40]
acupuncture, [41]
electroacupuncture, [42]
short-wave diathermy, [42]
traction, [42-45]
TENS, [31]
exercise, [25–28, 34, 43–46]
massage, [46]
cervical collar, [31–34, 44]
education, [25–29, 31–33, 44]
analgesics, [25–29]
anti-inflammatory drugs, [25–28, 47] and
muscle relaxants. [23, 24, 48, 49]A systematic review of conservative methods of neck-pain management yielded little information from randomized clinical trials to support many of the routine treatment approaches. [11] The authors concluded that physical medicine methods (e.g., traction, TENS, acupuncture), patient education, exercise, and medications have not been studied in sufficient detail to allow adequate assessment of their effectiveness. The Quebec Task Force on Whiplash-Associated Disorders found cervical pillows, postural training, acupuncture, spray and stretch, TENS, ultrasound, diathermy, heat, ice, massage, injections, muscle relaxants, and psychosocial interventions to have no proven value for patients with postwhiplash neck pain. [12]
Two comprehensive reviews of complications related to cervical spine manipulation have been published, both in 1996. [10, 50] One review documented more than 110 cases of harmful events, predominantly vertebrobasilar artery (VBA) dissections resulting in brain-stem or cerebellar infarction. Estimates of VBA dissection or stroke rates associated with cervical manipulation have ranged from 1 per 400 000 to 1 per 10 million manipulations, although the estimate of 1 per 5.85 million manipulations—based on medical record and chiropractic malpractice insurance data from Canada for the years 1988 through 1997—may be the most accurate. [51] A Canadian case–control study involving administrative data hospitalization and insurance billing records from 1993 to 1998 revealed a fivefold increase in the odds of VBA dissection among persons younger than 45 years who had visited a chiropractor within the past week, but no association was detected among persons 45 years or older. [52]
A systematic review of reported cases of VBA dissections from manipulation, other forms of neck trauma, and spontaneous dissections failed to yield any risk factors for these incidents. [53] In prospective studies from 1996 and 1997, manipulation was found to be associated with side effects such as local discomfort, headache, and, much less commonly, nausea and dizziness. [54-56] Although no systematic data are available, the risk of complications from mobilization is probably very small. Complication rates from medications, surgery, and other neck-pain treatments are estimated to be higher than those from manipulation or mobilization. [10, 57]
The primary limitation of the present investigation is that the results may be difficult to generalize to other populations in which patients or chiropractors differ from our sample. For example, the chiropractors who took part in our study do not necessarily use spinal manipulation and mobilization techniques as they are used in other communities. Also, because many eligible patients refused to participate, the study population was composed of self-selected volunteers. Although these problems do not threaten the validity of our findings, they may limit their generalizability to other populations and settings. However, our chiropractors used the spinal manipulation and mobilization techniques most commonly used by practicing chiropractors in the United States. [15, 16] Also consistent with modern chiropractic practice, they routinely had their patients engage in stretching, flexibility, and strengthening exercises and provided them with information about posture and body mechanics and advice about ergonomics and workplace modifications.
CONCLUSIONS
Our results suggest that cervical spine mobilization is as effective as manipulation in reducing neck pain and related disability among chiropractic patients. In addition, they show that neither heat nor EMS, alone or in combination with manipulation or mobilization, appreciably improves clinical outcomes, although heat may be of short-term benefit for some patients. Given the comparable outcomes and the risk of serious complications resulting from cervical spine manipulation, chiropractors may obtain equally effective results with less risk of adverse effects by treating neck-pain patients with mobilization rather than manipulation. However, manipulation may be more effective than mobilization for specific clinical indications. Future studies should be designed and conducted to help identify such patient subgroups. The therapeutic effects, side effects, and costs of manipulation and mobilization vs other common treatments for neck pain should also be assessed in subsequent investigations.
Acknowledgements
This study was funded by a grant from the Health Resources and Services Administration (R18 AH10008). Dr Hurwitz was also supported by a grant from the National Center for Complementary and Alternative Medicine (K23 AT00055).
We wish to thank Dr Gary Pirnat and his staff of chiropractors for their active involvement and cooperation during the study. We offer special thanks as well to the clinic management teams from La Habra, Brea, Buena Park, and Fullerton, Calif, and their front-office personnel for their help with patient enrollment. We also wish to acknowledge the efforts of Karen Hemmerling and Christina MacIsaac in coordinating patient recruitment, Stan Ewald and Jennifer Sanz in patient follow-up, and Emerlinda Gonzalez and Silvia Sanz in assisting with patient enrollment and tracking. Finally, thanks to He-Jing Wang for her data management expertise.
Notes
E. L. Hurwitz contributed to designing the study, developing the study hypotheses, and analyzing and interpreting the data. He also supervised data collection, reviewed the literature, and drafted the article. H. Morgenstern contributed to designing the study, developing the study hypotheses, analyzing and interpreting the data, and revising the article. P. Harber and G. F. Kominski contributed to interpreting the data and reviewing the article. F. Yu contributed to analyzing and interpreting the data and reviewing the article. A. H. Adams contributed to interpreting the data and reviewing the article.
References:
McCaig LF, Burt CW.
National Hospital Ambulatory Medical Care Survey:
1999 emergency department summary.
Adv Data Vital Health Stat. June 25, 2001;320Cherry DK, Burt CW, Woodwell DA.
National Ambulatory Medical Care Survey:
1999 summary.
Adv Data Vital Health Stat. July 10, 2001;322.Clark W, Haldeman S.
The development of guideline factors for the evaluation
of disability in neck and back injuries.
Spine. 1993;18:1736–1745.Bovim G, Schrader H, Sand T.
Neck pain in the general population.
Spine. 1994;19:1307–1309.Nygren A, Berglund A, von Koch M.
Neck-and-shoulder pain, an increasing problem.
Strategies for using insurance material to follow trends.
Scand J Rehabil Med. 1995;32(suppl):107–112.Makela M, Heiliovara M, Sieveers K, Impivaara O, Knekt P, Aromaa A.
Prevalence, determinants and consequences of chronic neck pain in Finland.
Am J Epidemiol. 1991;134:1356–1367.van der Donk J, Schouten JASAG, Passchier J, Romunde LKJ, Valkenburg HA.
The associations of neck pain with radiological abnormalities of the cervical
spine and personality traits in a general population.
J Rheumatol. 1991;18:1884–1889.Hurwitz EL, Coulter ID, Adams AH, Genovese BJ, Shekelle PG.
Use of chiropractic services from 1985 through 1991
in the United States and Canada.
Am J Public Health. 1998;88:771–776.Coulter, ID, Hurwitz, EL, Adams, AL, Genovese, BJ, Hays, R, and Shekelle, PG.
Patients Using Chiropractors in North America:
Who Are They, and Why Are They in Chiropractic Care?
Spine (Phila Pa 1976) 2002 (Feb 1); 27 (3): 291–298Hurwitz EL, Aker PO, Adams AH, Meeker WC, Shekelle PG.
Manipulation and Mobilization of the Cervical Spine:
A Systematic Review of the Literature
Spine (Phila Pa 1976) 1996 (Aug 1); 21 (15): 1746–1760Aker PD, Gross AR, Goldsmith CH, Peloso P.
Conservative management of mechanical neck pain:
systematic overview and meta-analysis.
BMJ. 1996;313:1291–1296.Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Cassidy JD, Lopes AA, Yong-Hing K.
The immediate effect of manipulation versus mobilization on pain and
range of motion in the cervical spine: a randomized controlled trial.
J Manipulative Physiol Ther. 1992;15:570–575.Vernon HT, Aker P, Burns S, Viljakaanen S, Short L.
Pressure pain threshold evaluation of the effect of spinal manipulation
in the treatment of chronic neck pain: a pilot study.
J Manipulative Physiol Ther. 1990;13:13–16.Cherkin DC, Mootz RD, eds.
Chiropractic in the United States: Training, Practice, and Research
Rockville, Md: Agency for Health Care Policy and Research,
Public Health Service, US Dept of Health and Human Services; 1997.
AHCPR publication 98-N002.Christensen MG, Kerkoff D, Kollasch MW.
Job Analysis of Chiropractic 2000
Greeley, Colo: National Board of Chiropractic Examiners; 2000:129.Haldeman S, Chapman-Smith D, Petersen DM, eds.
Guidelines for Chiropractic Quality Assurance and Practice Parameters
The Mercy Conference ~ Major Recommendations
Gaithersburg, Md: Aspen Publishers Inc; 1993.Vernon H, Mior S (1991)
The Neck Disability Index: A Study of Reliability and Validity
J Manipulative Physiol Ther 1991 (Sep); 14 (7): 409–415Vernon H.
The Neck Disability Index: patient assessment and
outcome monitoring in whiplash.
J Musculoskeletal Pain. 1996;4:95–104.Fairbank JCT, Couper J, Davies JB, O’Brien JP.
The Oswestry Low Back Pain Disability Index.
Physiotherapy. 1980;66:271–273.Ware JE, Sherbourne CD.
The MOS 36-Item Short-Form Health Survey (SF-36), I:
conceptual framework and item selection.
Med Care. 1992;30:473–483.McHorney CA, Ware JE.
Construction and validation of an alternate form general mental health scale
for the Medical Outcomes Study Short-Form Health Survey.
Med Care. 1995;33:15–28.Sloop PR, Smith DS, Goldenberg E, Dore C.
Manipulation for chronic neck pain. A double-blind controlled study.
Spine. 1982;7:532–535.Howe DH, Newcombe RG, Wade MT.
Manipulation of the cervical spine—a pilot study.
J R Coll Gen Pract. 1983;33:564–579.Koes BW, Bouter LM, van Mameren H, et al.
A randomized clinical trial of manual therapy and physiotherapy for
persistent back and neck complaints: subgroup analysis
and relationship between outcome measures.
J Manipulative Physiol Ther. 1993;16:211–219.Koes BW, Bouter LM, van Mameren H, et al.
A blinded randomized clinical trial of manual therapy and physiotherapy
for chronic back and neck complaints: physical outcome measures.
J Manipulative Physiol Ther. 1992;15:16–23.Koes BW, Bouter LM, van Mameren H, et al.
Randomised Clinical Trial of Manipulative Therapy and Physiotherapy
for Persistent Back and Neck Complaints:
Results of One Year Follow Up
British Medical Journal 1992 (Mar 7); 304 (6827): 601–605Koes BW, Bouter LM, van Mameren H, Essers AHM.
The effectiveness of manual therapy, physiotherapy, and treatment
by the general practitioner for nonspecific back and
neck complaints: a randomized clinical trial.
Spine. 1992;17:28–35.Brodin H.
Cervical pain and mobilization.
Manual Med. 1985;2:18–22.Jordan A, Bendix T, Nielsen H, Hansen FR, Host D, Winkel A.
Intensive training, physiotherapy, or manipulation for patients with
chronic neck pain: a prospective, single-blinded, randomized clinical trial.
Spine. 1998;23:311–319.Nordemar R, Thorner C.
Treatment of acute cervical pain—a comparative group study.
Pain. 1981;10:93–101.McKinney LA.
Early mobilisation and outcome in acute sprains of the neck.
BMJ. 1989;299:1006–1008.McKinney LA, Dornan JO, Ryan M.
The role of physiotherapy in the management of acute
neck sprains following road-traffic accidents.
Arch Emerg Med. 1989;6:27–33.Mealy K, Brennan H, Fenelon GC.
Early mobilization of acute whiplash injuries.
BMJ. 1986;292:656–657.Snow CJ, Aves Wood R, Dowhopoluk V, et al.
Randomized controlled clinical trial of spray and stretch
for relief of back and neck myofascial pain.
Physiother Canada. 1992;44:S8.Thorsen H, Gam AN, Svensson BH, et al.
Low level laser therapy for myofascial pain in the neck
and shoulder girdle. A double-blind, cross-over study.
Scand J Rheumatol. 1992;21:139–141.Waylonis GW, Wilke S, O’Toole D, Waylonis DA, Waylonis DB.
Chronic myofascial pain: management of low-output helium-neon laser therapy.
Arch Phys Med Rehabil. 1988;69:1017–1020.Foley-Nolan D, Barry C, Coughlan RJ, O’Connor P, Roden D.
Pulsed high frequency (27 MHz) electromagnetic therapy for persistent
neck pain: a double blind, placebo-controlled study of 20 patients.
Orthopaedics. 1990;13:445–451.Foley-Nolan D, Moore K, Codd M, Barry C, O’Connor P, Coughlan RJ.
Low energy high frequency pulsed electromagnetic therapy for acute
whiplash injuries. A double blind randomized controlled study.
Scand J Rehabil Med. 1992;24:51–59.Lewith GT, Machin D.
A randomized trial to evaluate the effect of infra-red stimulation
of local trigger points, versus placebo, on the pain
caused by cervical osteoarthrosis.
Acupunct Electrother. 1981;6:277–284.Petrie JP, Langley GB.
Acupuncture in the treatment of chronic cervical pain. A pilot study.
Clin Exp Rheumatol. 1983;1:333–335.Loy TT.
Treatment of cervical spondylosis. Electroacupuncture versus physiotherapy.
Med J Aust. 1983;2:32–34.Goldie I, Landquist A.
Evaluation of the effects of different forms of physiotherapy in cervical pain.
Scand J Rehabil Med. 1970;2–3:117–121.Pennie B, Agambar L.
Whiplash injuries: a trial of early management.
J Bone Joint Surg Br. 1990;72:277–279.van der Heijden GJMG, Beurskens AJHM, Koes BW, Assendelft WJJ.
The efficacy of traction for back and neck pain:
a systematic, blinded review of randomized clinical trial methods.
Phys Ther. 1995;75:93–104.Levoska S, Keinanen-Kiukaanniemi S.
Active or passive physiotherapy for occupational cervicobrachial disorders?
A comparison of two treatment methods with a 1-year follow-up.
Arch Phys Med Rehabil. 1993;74:425–430.Coletta R, Maggiolo F, Di Tizio S.
Etofenamate and transcutaneous electrical nerve
stimulation treatment of painful spinal syndromes.
Int J Clin Pharmacol Res. 1988;8:295–298.Basmajian JV.
Cyclobenzaprine hydrochloride effect on skeletal muscle spasm in the
lumbar region and neck: two double-blind controlled
clinical and laboratory studies.
Arch Phys Med Rehabil. 1978;59:58–63.Bercel NA.
Cyclobenzaprine in the treatment of skeletal muscle spasm
in osteoarthritis of the cervical and lumbar spine.
Curr Ther Res. 1977;22:462–468.Assendelft WJ, Bouter LM, Knipschild PG.
Complications of spinal manipulation: a comprehensive review of the literature.
J Fam Pract. 1996;42:475–480.Haldeman S, Carey P, Townsend M, Papadopoulos C.
Arterial Dissections Following Cervical Manipulation:
The Chiropractic Experience
Canadian Medical Association Jou (CMAJ) 2001 (Oct 2); 165: 905–906Rothwell DM, Bondy SJ, Williams JI.
Chiropractic Manipulation and Stroke:
A Population-based Case-control Study
Stroke 2001 (May); 32 (5): 1054-1060Haldeman S, Kohlbeck FJ, McGregor M.
Risk Factors and Precipitating Neck Movements Causing Vertebrobasilar
Artery Dissection After Cervical Trauma and Spinal Manipulation
Spine (Phila Pa 1976) 1999 (Apr 15); 24 (8): 785–794Senstad O, Leboeuf-Yde C, Borchgrevink CF.
Side effects of chiropractic spinal manipulation:
types, frequency, discomfort and course.
Scand J Prim Health Care. 1996;14:50–53.Senstad O, Leboeuf-Yde C, Borchgrevink CF.
Frequency and characteristics of side effects
of spinal manipulative therapy.
Spine. 1997;22:435–441.Leboeuf-Yde C, Hennius B, Rudberg E, Leufvenmark P, Thunman M.
Side effects of chiropractic treatment: a prospective study.
J Manipulative Physiol Ther. 1997;20:511–515.Dabbs V Lauretti WJ
A Risk Assessment of Cervical Manipulation vs. NSAIDs
for the Treatment of Neck Pain
J Manipulative Physiol Ther 1995 (Oct); 18 (8): 530–536
Return to CHRONIC NECK PAIN
Since 9-18-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |