

Spinal Manipulative Therapy for Acute Neck Pain:
A Systematic Review and Meta-Analysis of
Randomised Controlled TrialsThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Clinical Medicine 2021 (Oct 28); 10 (21): 5011 ~ FULL TEXT
OPEN ACCESS Aleksander Chaibi, Knut Stavem and Michael Bjørn Russell
Head and Neck Research Group,
Division for Research and Innovation,
Akershus University Hospital,
1478 Oslo, Norway

Background: Acute neck pain is common and usually managed by medication and/or manual therapy. General practitioners (GPs) hesitate to refer to manual therapy due to uncertainty about the effectiveness and adverse events (AEs)
Method: To review original randomized controlled trials (RCTs) assessing the effect of spinal manipulative therapy (SMT) for acute neck pain. Data extraction was done in duplicate and formulated in tables. Quality and evidence were assessed using the Cochrane Back and Neck (CBN) Risk of Bias tool and the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria, respectively
Results: Six studies were included. The overall pooled effect size for neck pain was very large –1.37 (95% CI, –2.41, –0.34), favouring treatments with SMT compared with controls. A single study that showed that SMT was statistically significantly better than medicine (30 mg ketorolac im.) one day post-treatment, ((–2.8 (46%) (95% CI, –2.1, –3.4) vs. –1.7 (30%) (95% CI, –1.1, –2.3), respectively; p = 0.02)). Minor transient AEs reported included increased pain and headache, while no serious AEs were reported.
There is more like this @ our:
CHRONIC NECK PAIN Page and our
NON-PHARMACOLOGIC THERAPY PageConclusions: SMT alone or in combination with other modalities was effective for patients with acute neck pain. However, limited quantity and quality, pragmatic design, and high heterogeneity limit our findings.
KEYWORDS: acute neck pain; physiotherapy; chiropractic; osteopath; spinal manipulation; randomized controlled trial; systematic review; meta-analysis; appropriateness; effectiveness
From the FULL TEXT Article:
Introduction
Acute neck pain is very common in the adult general population, as up to 50% experienced neck pain within the last year, and recurrence is frequent. [1, 2] The Global Burden of Disease study ranks musculoskeletal neck pain along with low back pain as the leading cause of non-fatal disability in almost all age groups. [3, 4] The point prevalence estimate of neck pain is 4.9–7.6%. [5, 6] The total cost to society of neck pain is unknown; however, a recent review estimated that the annual spending on personal health care and public health for lower back and neck pain combined was USD 87.6 billion in the US alone. [7]
About one third of general practitioner (GP) consultations are due to musculoskeletal pain, mainly from neck- and lower back. [8] Patients are often advised to wait for an expected favourable natural course, usually supported with analgesic medication, and/or referred to physiotherapy treatment. [9, 10] Topical NSAIDs can be beneficial and muscle relaxants are recommended as a reasonable treatment choice for acute neck pain. [6, 11]
In people refraining from medicine or in which medicine has an insufficient effect, manual therapy has traditionally been considered as an alternative treatment option. Nevertheless, GPs refer about 8% of people with neck pain to manual therapy, which often includes spinal manipulative therapy (SMT) intervention. [10] Fear of complications associated with cervical SMT and limited support in current guidelines towards the evidence about the effectiveness are important barriers to referrals by GPs. [10]
Randomized controlled trials (RCTs) including a placebo group provide the best approach to assessing efficacy and safety. However, most manual therapy RCTs are pragmatic or use no intervention as a control group. [12, 13] A recent Cochrane review of manual therapy for acute, subacute and chronic neck pain included 51 trials (2920 participants) and reported some evidence of an effect of SMT on neck pain. [14] Another recent systematic review on the efficacy of manual therapy and exercise for treating neck pain, including 23 RCTs, reported evidence for cervical spine manipulation and exercise in favour of thoracic spine manipulation and exercise for acute- and subacute neck pain. [15]
The primary objective of this systematic review of RCTs was to determine the effect of SMT on acute neck pain of less than 6 weeks in duration. Secondary objectives were to determine the pooled effect size using unimodal SMT intervention vs. control/placebo and multimodal interventions vs. control/placebo, descriptively present the effect of SMT on disability, quality of life measures and descriptively report adverse effects (AEs).
Materials and Methods
This systematic review identified RCTs that measured the effectiveness of SMT for patients with acute neck pain. It follows the preferred reporting of items for systematic reviews and meta-analyses (PRISMA). [16]
Data Sources and Searches
A comprehensive literature search was conducted on the medical databases Ovid MEDLINE, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL, Web of Science and OpenGrey. In order to specify and limit the search to the area of interest, the following key words were used in various combinations: “neck pain”, “neck ache”, “cervical pain”, “cervicalgia”, “cervicodynia”, “chiropractic”, “physiotherapy”, “physical therapy”, “manual therapy”, “manipulation”, “osteopathic”, ”randomized controlled trial”, and/or “controlled clinical trial”. We identified studies by a comprehensive computerized search from inception to 27 August 2020. We further restricted the search to RCTs and studies conducted in adult humans and published in English or Scandinavian. An expert librarian at the Division for Research and Innovation, Akershus University Hospital, performed the searches, while AC reviewed titles, abstracts, and full texts. In addition, reference lists of the selected RCTs and previous systematic reviews and meta-analyses were cross-checked to identify additional relevant studies.
Study Selection
Acute neck pain was defined as neck pain of <6 weeks duration as the primary complaint. [17] Pilot or feasibility studies were excluded, as were studies with sub-acute (6–11 weeks duration) and/or chronic neck pain (#8805;12 weeks duration) that did not present individual results for the acute neck pain population. Studies in which we could not determine the duration of pain and studies that did not include pain intensity as an outcome measure were also excluded. The intervention had to include SMT alone (unimodal intervention) or in combination with any other interventions (multimodal intervention). The SMT intervention could be conducted by any type of clinician, i.e., physiotherapist, chiropractor, osteopath. Physician was defined as a passive controlled manoeuvre that uses directional high-velocity low amplitude (HVLA) thrust directed at a specific joint past the physiological range of motion without exceeding the anatomical limit. [18] Simple advice, reassurance, and encouragement to continue normal activities were not considered as multimodal interventions. Any comparison group was included.
Data Extraction and Quality Assessment
Two authors (AC and MBR) independently extracted data, with discrepancies resolved through consensus. Extracted information was formatted in a table and included country/year, study population, method, intervention, and results.
The methodological quality and internal validity of the evidence were assessed by the same two authors (AC and MBR) using the Cochrane Back and Neck (CBN) Risk of Bias tool. [19] This tool has 12 items in the following domains: randomization, concealment, baseline differences, blinding (patient, care provider and outcome assessor), co-interventions, compliance, outcomes adequately addressed, drop-outs, timing, and intention-to-treat. Prior research has shown the ability of the CBN Risk of Bias tool to identify studies at an increased risk of bias using a threshold of 5 or 6 as a summary score. [19] Thus, studies were classified as higher quality (6–12 points) or lower quality (0–5 points). In case of uncertainty regarding an item, the RCT did not receive a point and was marked with not applicable (n/a) or question mark (?).
We attempted to contact the authors of the included papers if the information appeared unclear or was highly important in order to calculate effect size.
Main Outcomes
Pain intensity measured by any visual analogue scale (VAS) or numeric rating scale (NRS) was the primary outcome measure, while disability, quality of life measures and AEs were descriptively presented as secondary outcomes.
Data Synthesis and Analyses
The primary analysis focused on the standardized mean difference in pain intensity between the groups receiving either SMT alone or in combination with a multimodal intervention vs. control/placebo (sham) or no treatment. All pain intensity outcomes were converted to a 0 to 10 scale to enable pooling of the results. As the included studies had different numbers of sessions and timings of assessments which complicated the analysis. We used data from the first assessment for each study, ranging from 1 h to 3 weeks after the baseline assessment. Random effects meta-analysis was conducted using the Hartung-Knapp-Sidak-Jonkman (HKSJ) method [20, 21], which is recommended for analysis with few studies. [22–24]
We grouped RCTs and calculated the pooled effect size of SMT alone vs. control/placebo and multimodal approach vs. control/placebo and conducted a similar analysis with pooled effects for VAS vs. NRSs. An effect size of >0.2 was regarded as small, >0.5 as medium, >0.8 as large, and >1.3 as very large. [25]
Heterogeneity of the study results was analysed using the generalized I2 statistic; a percentage of 25%, 50%, and 75% has been suggested to indicate low, medium, and high heterogeneity, respectively. [26] We further examined heterogeneity using meta-regression with dichotomized independent variables.
We assessed the impact of a priori identified sources of sources of heterogeneity:(1) length of time from baseline to follow-up (<1 week vs. #8805;1 week),
(2) unimodal vs. multimodal intervention,
(3) type of scale used (VAS vs. NRS),
(4) publication year (below/above the median: 2005–2009 vs. 2010–2013),
(5) CBN risk of bias score (below/above the median: <7 vs. #8805;7).We also prepared funnel plots and used Egger’s test for funnel plot asymmetry to identify possible publication bias with p <0.05 suggesting asymmetry. [27]
As a secondary analysis, we analysed the standardized mean difference of change in pain intensity for the studies with available data using a similar method. Because there were only three studies for this analysis, we did not prepare forest plots for subgroups, funnel plots or any further analyses.
Rating the Body of Evidence
The evidence in the included articles was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria, which uses the domains of study design limitations, inconsistency, indirectness, and imprecision in results, and was assessed as “high”, “moderate”, “low” or “very low” by KS. [28, 29]
Patient and Public Involvement
Patients were not involved in the development of the research question or its outcome measures, conduct of the research, or preparation of the manuscript. The findings will, however, be disseminated to patients via social media, relevant professional associations and news media.
Results
Study and Subject Selection and Characteristics

Figure 1 Six RCTs on acute neck pain including a total of 446 participants, met the inclusion criteria of this review (Figure 1).
The studies were conducted in Australia, Spain and USA and published from 2005 to 2013. The interventions were conducted by physiotherapists or osteopaths, except one study, which recruited through 12 private physiotherapy, chiropractic, and osteopathy clinics combined.
Two studies explicitly evaluated SMT alone, while four studies used multimodal interventions. The patients’ mean age was 34.3 years (SD 6.1), with a mean acute neck pain duration of 20.1 days (SD 22.2) and a mean pain intensity of 5.3 (SD 1.2) on a 0–10 NRS/VAS.
Methodological Quality

Table 1

Table 2 The methodological quality score ranged from 5 to 8 points (mean 6.5, SD 1.9) out of maximum score on 12 point (Table 1). Agreement between authors was 100% at each stage. Five RCTs were considered to be of good quality [30–34] and one of low quality (score < 6). [35] Performance and reporting bias was introduced in all RCTs, as none of the RCTs blinded patients or published their research protocol. Detection bias was introduced in all but one RCT, which concealed the outcomes for the assessor. [33]
Pain Outcomes
Table 2 gives an overview of the six individual RCTs study population, methods, intervention and results. The results focus on mean within- and between-group change in acute neck pain intensity between baseline and after the intervention. Neck pain intensity was statistically significant between the two treatment groups in five of the six studies, favouring SMT compared to other treatments. The mean pain intensity reduction, calculated by the authors was 66% (SD 19%) at 1 day to ≤1 week follow-up, 74% (SD 17%) at >1 week to ≤4 weeks follow-up, and 86% (SD 12%) at >4 weeks follow-up (Table 2). A single study showed that SMT was better than the NSAIDs (30 mg ketorolac im.) one day post-treatment, i.e., (–2.8, SD 1.7 (46%) (95% CI, –2.1, –3.4) vs. (–1.7, SD 1.7 (30%) (95% CI, –1.1, –2.3), respectively; p = 0.02)) (Table 2).

Figure 2
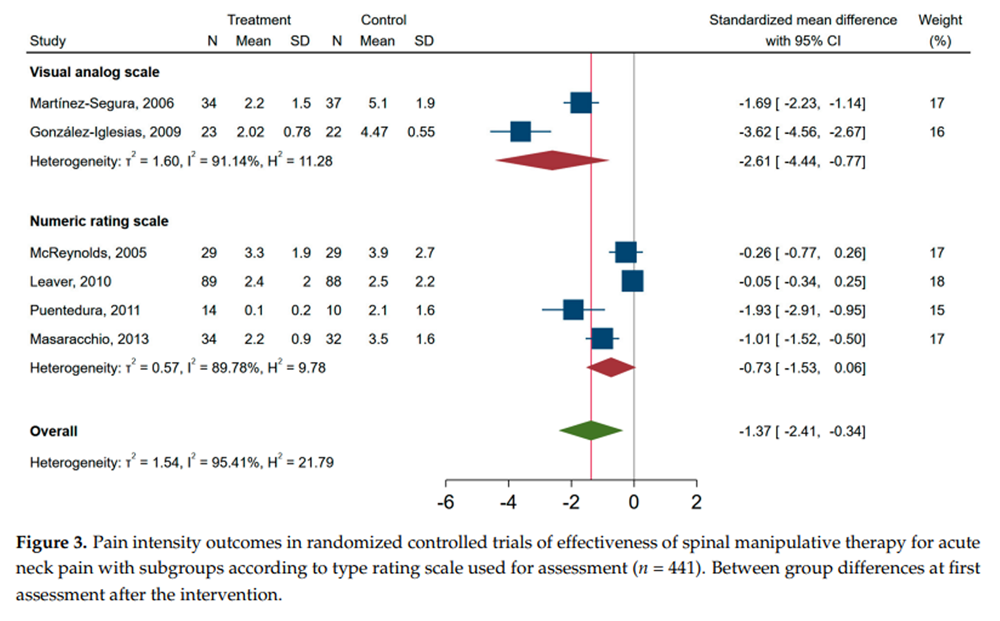
Figure 3 When pooling the unimodal and multimodal studies in the meta-analysis, those receiving SMT had lower neck pain intensity at the time of the first assessment point compared to other treatments, i.e., standardized mean difference of –1.37 (95% CI, –2.41, –0.34) (Figure 2). A similar forest plot is shown for studies with an end point of less than 1 week and studies with end points 1–3 weeks (Supplement Figure S1). The standardized mean difference in pain score between SMT and controls was lower in studies investigating neck pain with VAS as compared to NRS, i.e., in favour of SMT (Figure 3). In the secondary analysis of change scores from baseline to after the intervention, only three studies were included. The pooled standardized mean difference was –2.76 (–4.96 to –0.60), and I2 was 96% (Supplement Figure S2).
Overall, the six RCT studies included were highly heterogeneous, irrespective of modality, duration of end-point assessment and pain measurement scale used, as indicated by a I2 > 90% for subgroups in the pooled analyses (Figure 2 and Figure 3 and Supplement Figure S1). When exploring the sources of heterogeneity in meta-regression analysis, only type of rating scale (NRS vs. VAS) was associated with a worse outcome, unstandardized beta (95% CI) 1.82 (0.09 to 3.56), whereas multimodal vs. unimodal, time to follow-up (1–3 weeks vs. <1 week), publication year (2010–2013 vs. 2005–2009), or CBN risk of bias score (<7 vs. ≥7) was not associated with pain at the time of assessment. A funnel plot of the six RCTs indicated that publication bias was possible (Supplement Figure S3), and Egger’s test (p = 0.003) supported asymmetry of the funnel plot.
The overall level of the body of evidence was rated as very low, i.e., we have very little confidence in the effect estimate, and the true effect is likely to be substantially different from the estimate of effect. For details, see Supplement Table S1.
Disability, Function, and Quality of Life Outcomes
Two RCTs did not report outcomes for disability, function, or quality of life measures. [30, 35]
Disability, Function, and Quality of Life Outcomes in Unimodal Intervention Studies
One unimodal RCT found no statistically significant between-group differences between the cervical SMT and the cervical spinal mobilization group for the neck disability index (NDI), patient-specific functional scale or health-related quality of life, respectively, from baseline to 4 and 12 weeks follow-up (all p #8805; 0.30). [32] The cervical SMT group had an improved neck disability index, patient specific functional scale and health-related quality of life by 60%, 105% and 11%, respectively, at 4 weeks follow-up, and 67%, 115% and 17%, respectively, at 12 weeks follow-up, while the cervical mobilization group improved by 53%, 81% and 9%, respectively, at 4 weeks, and 63%, 100% and 16%, respectively, at 12 weeks. [32]
Disability, Function, and Quality of Life Outcomes in Multimodal Intervention Studies
Three multimodal RCTs presented results for disability. [31, 33, 34] One RCT showed within-group statistically significant reduction in Neck Pain Questionnaire (NPQ) (both p < 0.001), while between-group statistically significant improvement was found in favour of the experimental group, i.e., electro- and thermotherapy plus thoracic SMT at post-treatment (p < 0.001). The electro/thermal group improved by 14%, while the electro/thermal plus thoracic SMT group improved by 46% from baseline to post-treatment. [31]
The second RCT showed lower NDI scores for the cervical SMT group as compared to the thoracic SMT group at all follow-up time points (all p ≤ 0.003). The cervical SMT group reduced NDI by 38%, 69%, and 72% from baseline to 1, 4, and 24 weeks follow-up, while the thoracic group reduced NDI by 14%, 28%, and 21% from baseline to 1, 4, and 24 weeks follow-up, respectively. [33]
The third RCT reported a statistically significant between-group difference for NDI in favour for the cervical SMT plus thoracic SMT group at 1–week follow-up (p < 0.001). The cervical spinal mobilizations plus thoracic SMT group and the cervical spinal mobilization group reduced NDI by 57% and 28%, respectively, from baseline to 1 week post-treatment. [34]
Adverse Events
Two RCTs did not report AEs [30, 31], and one RCT mentioned that no AEs were recorded. [34]
Three RCTs reported AEs.
The RCT that also administered im. ketorolac (30 mg) recorded AEs in eight participants (28%) due to medicine, i.e., arm soreness, bad taste in mouth, dizziness, drowsiness, dyspepsia, heart palpitations, light headedness, nausea or vomiting, while one participant (3%) in the osteopathic cervical SMT group reported transient feeling of a “funny” arm (without motor weakness when assessed in the emergency department). [35]
The second RCT reported increased neck pain in 28 participants (32%) and 24 participants (27%) in the SMT and spinal mobilization group, respectively, headache (22 (25%) and 17 participants (19%), respectively), dizziness/vertigo (7 (8%) and 6 participants (7%), respectively), nausea (4 (5%) and 7 participants (8%), respectively), paraesthesia (8 (9%) and 5 participants (6%), respectively), and “others” defined as upper limb pain, neck stiffness, fatigue, mild lower back pain and unpleasant change in spinal posture (7 (8%) and 3 participants (3%), respectively). [32]
The third RCT reported minor and transient increased neck pain at post-treatment in one participant (7%) in the cervical SMT group by a physiotherapist, while eight participants (80%) reported minor and transient (<24 h) increased neck pain, fatigue, headache, and upper back pain in the thoracic SMT group. [33]
No severe or serious AEs were reported.
Discussion
To our knowledge, this is the first systematic review on the effectiveness of SMT treating acute neck pain. The main conclusion is that SMT alone or in combination with another modality is likely to be effective in the treatment of acute neck pain, and the RCTs reported few, mild and transient AEs.
Methodological Considerations
The methodological quality of manual therapy RCTs is frequently being criticised for being too low. [36] However, manual therapy studies cannot reach what is considered the gold standard in pharmacological RCTs, because the manual therapist cannot be blinded.
The included RCTs support SMT as a non-pharmacological treatment option for acute neck pain; however, the studies are very heterogeneous and comprise small numbers of subjects. Therefore, the results should be interpreted with caution. Other methodologically challenges were the lack of patient and outcome blinding, which introduces serious methodological flaws. None of the RCTs included a sham placebo intervention arm. Although experts disagree on what is an appropriate placebo for a manual therapy clinical trials [37], we have previously shown that patient blinding is possible. [13, 38]
Furthermore, none of the included studies included a control group arm, i.e., not receiving any form of intervention or simply await treatment till study completion. Thus, all six RCTs were pragmatic trials that compared two active treatment arms. RCTs comparing a placebo group and a control group are advantageous to pragmatic RCTs that compare two active treatment arms to produce a true net effect. [12, 13] It is also important to quantify a likely placebo response in all manual therapy RCTs. Double-blinded studies are not possible because the investigator cannot be blinded for obvious reasons. [13, 39]
The Bone and Joint Decade 2000–2010 Task Force on neck pain presented evidence-based guidelines for primary care clinicians to inform their assessments of neck pain. [40] For grade I, complaints of neck pain may be associated with stiffness or tenderness, but no significant neurological complaints; for grade II, neck pain interferes with daily activities, but no signs or symptoms are evident to suggest major structural pathology or significant nerve root compression; for grade III, complaints of neck pain are associated with significant neurological signs; and for grade IV, neck pain includes complaints of neck pain and/or its associated disorders, and the examining clinician detects signs or symptoms suggestive of major structural pathology. None of the included RCTs used a grading guideline when including neck pain patients, although a similar classification was proposed by the Quebec Task Force in 1995. [41]
Studies with unimodal approaches isolate (statistically) the individual effects of SMT better than multimodal approaches do, unfortunately; only two studies were unimodal. [30, 32] Multimodal programs may, however, better represent actual clinical practice and therefore, be more relevant. Assessing the effect of multimodal programs is nevertheless problematic, because it is difficult to isolate the impact of a specific single intervention such as SMT. This challenge persists in meta-analysis of multimodal interventions. Multimodal RCTs also introduce a major risk of contextual biases as compared to unimodal RCTs, which was the case for four of our included RCTs. [31, 33–35]
The methodological scores indicated high quality in all but one study [35]. The treatment sessions ranged from 1 to 5 sessions (mean 3.2, SD 3.3) with a trial duration from one single day to 6 months (mean 27, SD 59 days) which leaves knowledge gaps in terms of dose-response and numbers needed to treat.
Discussion of Results
The 55 previous systematic reviews of manual therapy for neck pain (Figure 1) included an unspecified broad spectrum of clinical entities, i.e., acute-, sub-acute- and chronic and combined disorders, such as spinal pain with or without whiplash and/or headache disorders and/or shoulder pain and/or radiculopathy, which complicate the evaluation to draw specific conclusions. Our review rigorously restricted RCTs to acute neck pain alone, which is important in clinical practice, because acute and chronic patients respond differently to treatment. [42]
Two of the 55 systematic reviews we retrieved included four of the RCTs in the present study, i.e., a Cochrane review (2015) [14, 30–33] and a recent meta-analysis (2019) [30, 31, 33, 34, 43]. The Cochrane review concluded that for acute and sub-acute neck pain, multiple sessions of cervical SMT were more effective than medications in reducing pain and improving function at immediate- and long-term follow-up, but produced similar changes in pain, function and quality of life when compared with multiple sessions of cervical mobilisation at immediate-, short- and intermediate-term follow-up. The recent meta-analysis (2019) [43] found an effect favouring the thoracic SMT for pain (mean difference –13.63; 95% CI: –21.79, –5.46) and disability (mean difference –9.93; 95% CI: –14.38, –5.48) as compared to thoracic or cervical mobilization for mechanical neck pain. No differences were found for thoracic SMT as compared to cervical SMT. Both reviews reported that there was an increased risk of bias due to inadequate provider and participant blinding. [4, 43]
A recent clinical practice guideline from the Orthopedic Section of the American Physical Therapy Association recommended thoracic SMT, a program of neck range of motion exercises, and scapula-thoracic and upper extremity strengthening to enhance program adherence (level B), and cervical SMT and/or mobilization (level C) for acute neck pain with mobility deficit. [44] However, the guideline only included one of the six RCTs in the present study in their analysis [32], which questions the literature search conducted. Nevertheless, the conclusion in the practice guideline is in accordance with the findings from a recent published Danish national clinical guideline for non-surgical treatments for acute neck pain that recommended manual therapy directed to the cervical and/or thoracic spine for acute neck pain. [45] The latter guideline, however, also concluded that they had very little confidence in the effect estimate, and that the true effect was likely to be substantially different from the estimate reported. [45]
NSAIDs are the most frequently prescribed medications by GPs worldwide and are widely used for patients with low back pain [46], but similarly unproven for acute neck pain. [6, 11] To our knowledge, one randomized, placebo- and active-controlled, multi-country, multi-centre parallel group trial has investigated the effect of NSAIDs for acute neck pain and found no significant superiority for 400 mg ibuprofen plus 100 mg caffeine or 400 mg ibuprofen alone over placebo. [11]
NSAIDs have frequent AEs, such as abdominal pain, diarrhea, edema, dry mouth, rash, dizziness, headache, tiredness, etc. [46] In comparison, The World Health Organization acknowledges manual therapy to be a safe and effective treatment with few mild and transient AEs. [47] i.e., local tenderness and tiredness on the treatment day [48], while serious AEs are very rare. [49] Thus, AEs appears to be substantially less in manual therapy than in pharmacological management using NSAIDs.
Limitations
This study has limitations. First, there were limited quantity and quality of original research. Secondly, the six included RCTs were very heterogeneous with regard to study design and results, which limit our findings. Therefore, the results should be interpreted with caution. Thirdly, non-English RCTs are missed. Fourthly, it is possible that reporting bias exists, as indicated by asymmetry of the funnel plot and because none of the trial protocols was published. Finally, although the methodological quality of studies published after 2005 was high, all studies failed to blind patients. This leaves unanswered questions about the true net-effect and safety. Omission of blinding the outcome assessor further introduces a possible bias to the results.
Conclusions
In spite of important methodological shortcomings, our analysis shows that SMT alone or in combination with another modality are likely to be effective in the treatment of acute neck pain and the RCTs reported few AEs. However, due to the large heterogeneity of the included RCTs, small sample sizes, lack of blinding, and unanswered placebo effects, future more robust RCTs are required for firm conclusions.
Supplementary Materials
The following are available here:Figure S1: (forest end by time). Pain intensity outcomes in randomized controlled trials of effectiveness of spinal manipulative therapy for acute neck pain with subgroups according to time from intervention to assessment (n = 441). Between group differences at first assessment after the intervention,
Figure S2: (forest change overall). Pain intensity outcomes in randomized controlled trials of effective-ness of spinal manipulative therapy for acute neck pain (n = 174). Between group differences in change in pain intensity from before to first assessment after the intervention,
Figure S3: (funnel plot overall). Funnel plot of included randomized controlled trials of effectiveness of spinal manipulative therapy for acute neck pain. Asymmetry of plot indicates possible publication bias.
Table S1: Rating of quality of the body of evidence across studies of short-term effects of manipulation therapy vs. control.Author Contributions
A.C. conceived the review and drafted the initial manuscript.
A.C. and M.B.R. performed the methodological assessment of the included studies.
K.S. performed the statistical analysis.
All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors would like to acknowledge Åse Marit Hammersbøen, Division for Research and Innovation, Akershus University Hospital, Norway, for her technical and administrative competency and support throughout the in-depth literature search.
Conflicts of Interest
The authors have completed the ICMJE uniform disclosure form and declare no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
References:
Carroll LJ, Hogg-Johnson S, van der Velde G, Haldeman S, Holm LW, et al.
Course and Prognostic Factors for Neck Pain in the General Population:
Results of the Bone and Joint Decade 2000–2010 Task Force on
Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S75–82Hogg-JohnsonS, van derVelde G, Carroll LJ, HolmLW, Cassidy JD,GuzmanJ, et al.
The Burden and Determinants of Neck Pain in the General Population:
Results of the Bone and Joint Decade 2000–2010 Task Force on
Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S39–51Vos T, Allen C, Arora M, et al.
Global, Regional, and National Incidence, Prevalence, and Years Lived
with Disability for 310 Diseases and Injuries, 1990-2015: a Systematic
Analysis for the Global Burden of Disease Study 2015
Lancet. 2016 (Oct 8); 388 (10053): 1545–1602Kamper SJ, Henschke N, Hestbaek L, Dunn KM, Williams CM.
Musculoskeletal Pain in Children and Adolescents
Brazilian J Physical Therapy 2016 (May); 20 (3): 275–284Hoy D, March L, Woolf A, et al.
The Global Burden of Neck Pain: Estimates From the Global Burden of Disease 2010 Study.
Ann Rheum Dis. 2014 (Jul); 73 (7): 1309–1315Cohen, S.P.; Hooten, W.M.
Advances in the diagnosis and management of neck pain.
BMJ 2017, 358, j3221Dieleman JL, Baral R, Birger M, et al.
US Spending on Personal Health Care and Public Health, 1996-2013
JAMA 2016 (Dec 27); 316 (24): 2627-2646Kinge, J.M.; Knudsen, A.K.; Skirbekk, V.; Vollset, S.E.
Musculoskeletal disorders in Norway: Prevalence of chronicity
and use of primary and specialist health care services.
BMC Musculoskelet. Disord. 2015, 16, 75.Vos, C.; Verhagen, A.; Passchier, J.; Koes, B.
Management of acute neck pain in general practice: A prospective study.
Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 2007, 57, 23–28.Dikkers, M.F.; Westerman, M.J.; Rubinstein, S.M.; van Tulder, M.W.
Why Neck Pain Patients are Not Referred to Manual Therapy:
A Qualitative Study among Dutch Primary Care Stakeholders.
PLoS ONE 2016, 11, e0157465.Predel, H.G.; Ebel-Bitoun, C.; Lange, R.; Weiser, T.
A randomized, placebo- and active-controlled, multi-country, multi-center
parallel group trial to evaluate the efficacy and safety of a fixed-dose
combination of 400 mg ibuprofen and 100 mg caffeine compared with
ibuprofen 400 mg and placebo in patients with acute lower back or neck pain.
J. Pain Res. 2019, 12, 2771–2783.Tramer, M.R.; Reynolds, D.J.; Moore, R.A.; McQuay, H.J.
When placebo controlled trials are essential and equivalence trials are inadequate.
BMJ 1998, 317, 875–880.Chaibi A, Saltyte Benth J, Bjorn Russell M.
Validation of Placebo in a Manual Therapy Randomized Controlled Trial
Sci Rep. 2015 (Jul 6); 5: 11774Gross, A.; Langevin, P.; Burnie, S.J.; Bedard-Brochu, M.S.; Empey, B.et al.
Manipulation and mobilisation for neck pain contrasted against
an inactive control or another active treatment.
Cochrane database Syst. Rev. 2015, 9, Cd004249Hidalgo, B.; Hall, T.; Bossert, J.; Dugeny, A.; Cagnie, B.; Pitance, L.
The efficacy of manual therapy and exercise for treating non-specific neck pain:
A systematic review.
J. Back Musculoskelet. Rehabil. 2017, 30, 1149–1169.Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.
The PRISMA statement for reporting systematic reviews and meta-analyses
of studies that evaluate health care interventions: Explanation and elaboration.
Ann. Intern. Med. 2009, 151, W-65–W-94Dionne, C.E.; Dunn, K.M.; Croft, P.R.; Nachemson, A.L.; Buchbinder, R.; et al.
A consensus approach toward the standardization of back pain definitions
for use in prevalence studies.
Spine 2008, 33, 95–103Esposito, S.; Philipson, S.
Spinal Adjustment Technique the Chiropractic Art;
S. Philipson and S. Esposito:
St. Ives, Australia, 2005; Volume 2005van Tulder, M.W.; Suttorp, M.; Morton, S.; Bouter, L.M.; Shekelle, P.
Empirical evidence of an association between internal validity and
effect size in randomized controlled trials of low-back pain.
Spine 2009, 34, 1685–1692.Hartung, J.
An Alternative Method for Meta-Analysis.
Biom. J. 1999, 41, 901–916.Knapp, G.; Hartung, J.
Improved tests for a random effects meta-regression with a single covariate. Stat.
Med. 2003, 22, 2693–2710IntHout, J.; Ioannidis, J.P.; Borm, G.F.
The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis
is straightforward and considerably outperforms the standard
DerSimonian-Laird method.
BMC Med Res. Methodol. 2014, 14, 25Bender, R.; Friede, T.; Koch, A.; Kuss, O.; Schlattmann, P.
Methods for evidence synthesis in the case of very few studies.
Res. Synth. Methods 2018, 9, 382–392.Veroniki, A.A.; Jackson, D.; Bender, R.; Kuss, O.; Langan, D.
Methods to calculate uncertainty in the estimated overall effect size
from a random-effects meta-analysis.
Res. Synth. Methods 2019, 10, 23–43.Cohen, J.
Statistical Power Analysis for the Behavioral Sciences;
Academic Press: Cambridge, MA, USA, 2013.Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G.
Measuring inconsistency in meta-analyses.
BMJ 2003, 327, 557–560.Egger, M.; Smith, G.D.; Phillips, A.N.
Meta-analysis: Principles and procedures.
BMJ 1997, 315, 1533–1537.Guyatt GH, Oxman AD, Vist GE, et al.
GRADE: An Emerging Consensus on Rating Quality of Evidence
and Strength of Recommendations
British Medical Journal 2008 (Apr 26); 336 (7650): 924–926Balshem, H.; Helfand, M.; Schünemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; et al.
GRADE guidelines: 3. Rating the quality of evidence.
J. Clin. Epidemiol. 2011, 64, 401–406.Martinez-Segura R, Fernandez-de-las-Penas C, Ruiz-Saez M.
Immediate Effects on Neck Pain and Active Range of Motion After a Single
Cervical High-velocity Low-amplitude Manipulation in Subjects Presenting
with Mechanical Neck Pain: A Randomized Controlled Trial
J Manipulative Physiol Ther 2006 (Sep); 29 (7): 511–517González-Iglesias, J.; Fernández-de-las-Peñas, C.; Cleland, J.A.
Thoracic spine manipulation for the management of patients with neck pain:
A randomized clinical trial.
J. Orthop. Sports Phys. Ther. 2009, 39, 20–27.Leaver, A.M.; Maher, C.G.; Herbert, R.D.; Latimer, J.; McAuley, J.H.
A randomized controlled trial comparing manipulation with mobilization
for recent onset neck pain.
Arch. Phys. Med. Rehabil. 2010, 91, 1313–1318.Puentedura, E.J.; Landers, M.R.; Cleland, J.A.; Mintken, P.E.; Huijbregts, P.
Thoracic spine thrust manipulation versus cervical spine thrust manipulation
in patients with acute neck pain: A randomized clinical trial.
J. Orthop. Sports Phys. Ther. 2011, 41, 208–220.Masaracchio, M.; Cleland, J.A.; Hellman, M.; Hagins, M.
Short-term combined effects of thoracic spine thrust manipulation
and cervical spine nonthrust manipulation in individuals with
mechanical neck pain: A randomized clinical trial.
J. Orthop. Sports Phys. Ther. 2013, 43, 118–127McReynolds, T.M.; Sheridan, B.J.
Intramuscular ketorolac versus osteopathic manipulative treatment
in the management of acute neck pain in the emergency department:
A randomized clinical trial.
J. Am. Osteopath. Assoc. 2005, 105, 57–68.Alvarez, G.; Núñez-Cortés, R.; Solà, I.; Sitjà-Rabert, M.; Fort-Vanmeerhaeghe, A..
Sample size, study length and inadequate controls were the most common
self-acknowledged limitations in manual therapy trials: A methodological review.
J. Clin. Epidemiol. 2021, 130, 96–106Hancock, M.J.; Maher, C.G.; Latimer, J.; McAuley, J.H.
Selecting an appropriate placebo for a trial of spinal manipulative therapy.
Aust J Physiother. 2006, 52, 135–138.Chaibi, A.; Knackstedt, H.; Tuchin, P.J.; Russell, M.B.
Chiropractic Spinal Manipulative Therapy for Cervicogenic Headache:
A Single-blinded, Placebo, Randomized Controlled Trial
BMC Res Notes. 2017 (Jul 24); 10 (1): 310Kendall, J.M.
Designing a research project: Randomised controlled trials and their principles.
Emerg. Med. J. EMJ 2003, 20, 164–168.Guzman J, Haldeman S, Carroll LJ, et al.
Clinical Practice Implications of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders:
From Concepts and Findings to Recommendations
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S199–S212Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Grotle, M.; Foster, N.E.; Dunn, K.M.; Croft, P.
Are prognostic indicators for poor outcome different for acute
and chronic low back pain consulters in primary care?
Pain 2010, 151, 790–797Masaracchio, M.; Kirker, K.; States, R.; Hanney, W.J.; Liu, X.; Kolber, M.
Thoracic spine manipulation for the management of mechanical neck pain:
A systematic review and meta-analysis.
PLoS ONE 2019, 14, e0211877Blanpied, P.R.; Gross, A.R.; Elliott, J.M.; Devaney, L.L.; Clewley, D.; Walton, D.M.; et al.
Neck Pain: Revision 2017.
J. Orthop. Sports Phys. Ther. 2017, 47, A1–A83.Bolette, S.; Peter, D.; Anne, G.; Henrik, H.L.; Alexander, I.-J.; Martin, B.J.; et al.
National Klinisk Retningslinje for Ikke-Kirurgisk Behandling af Nyopståede
Uspecifikke Nakkesmerter; Report No.: 1.0 Contract;
Sundhedsstyrelsen: Copenhagen, Denmark, 2016; ISBN 978-87-7104-816-2Roelofs, P.D.; Deyo, R.A.; Koes, B.W.; Scholten, R.J.; van Tulder, M.W.
Nonsteroidal anti-inflammatory drugs for low back pain:
An updated Cochrane review.
Spine 2008, 33, 1766–1774World Health Organization (WHO)
WHO Guidelines on Basic Training and Safety in Chiropractic
Geneva, Switzerland: (November 2005)Chaibi, A.; Benth, J.S.; Tuchin, P.; Russell, M.B.
Adverse Events in a Chiropractic Spinal Manipulative Therapy Single-blinded,
Placebo, Randomized Controlled Trial for Migraineurs
Musculoskelet Sci Pract. 2017 (Mar 14); 29: 66–71Chaibi, A.; Russell, M.B.
A Risk-benefit Assessment Strategy to Exclude Cervical Artery Dissection
in Spinal Manual-therapy: A Comprehensive Review
Annals of Medicine 2019 (Mar 19): 51 (2): 118–127
Return to CHRONIC NECK PAIN
Return NON-PHARMACOLOGIC THERAPY
Since 8-20-2020


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |