

Adverse Impacts of Chronic Pain on Health-related
Quality of Life, Work Productivity, Depression
and Anxiety in a Community-based StudyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Family Practice 2017 (Nov 16); 34 (6): 656–661 ~ FULL TEXT
Kosuke Kawai, Alison Tse Kawai, Peter Wollan, Barbara P Yawn
Clinical Research Center,
Boston Children's Hospital,
Harvard Medical School,
Boston, MA, USA.

Background: Chronic pain has major clinical and social consequences. Few studies have examined any variation in the extent of impairment on quality of life and work productivity by site and type of chronic pain.
Objective: The objective of our study is to examine adverse impacts of chronic pain on physical and psychological health and work productivity.
Methods: Our community-population study was based on a phone-interview of adults with chronic pain, residing in Olmsted County, MN. Chronic pain groups were categorized into abdominal pain, back pain, joint pain, multisite pain, neuropathic pain or no chronic pain. We used standardized instruments, including the Brief Pain Inventory, the Patients Health Questionnair-9, and Work Productivity and Activity Impairment Questionnaire.
Results: We evaluated 591 patients suffering from chronic pain and 150 participants with no chronic pain. Almost one third of patients with multisite pain (33%) and neuropathic pain (32%) reported mild/major depressive symptoms. Patients suffering from chronic pain, particularly from multisite pain and neuropathic pain, reported significant pain interferences with daily activities and impairments in physical function. Chronic pain was significantly associated with reduced performance at work but not with missed work hours. The average reported reduction in work productivity ranged from 2.4 hours (±5.6) per week for adults with joint chronic pain to 9.8 hours (±11.1) per week for adults with multisite chronic pain.
Conclusions: Chronic pain, particularly multisite pain and neuropathic pain, significantly affected physical and psychological health. Chronic pain is a multifaceted health condition that requires a multidisciplinary treatment approach.
Keywords: Chronic pain; depression; epidemiology; pain; primary health care; quality of life.
From the FULL TEXT Article:
Introduction
Chronic pain is a common condition that has major clinical and social consequences in communities. [1, 2] Chronic pain can be manifested in different locations and types, including low back pain, abdominal pain, joint pain, multisite pain and may be neuropathic in nature. Differing types and sites of chronic pain, may differentially impact physical and psychological well-being and work productivity. [2] Few studies have examined the reduction in work productivity by type and location of chronic pain. Most prior studies focused on specific types of pain rather than locations of pain or did not differentiate by type or location of pain. [3–5] Furthermore, they often included patients recruited in the clinic or hospital setting, and thus results may not generalize to community populations.
The objective of our community population-based study was to characterize chronic pain by location and whether or not it was neuropathic to examine adverse impacts on interference with daily activities, work and physical and psychological well-being compared to a group of patients without chronic pain. By sampling participants from the community rather than from health care utilization databases, we were able to examine these associations in chronic pain sufferers with and without healthcare seeking for their symptoms. Our study was based on a phone-interview of adults with chronic pain, residing in Olmsted County, Minnesota (MN).
Methods
Study population
The study participants for Olmsted County Health Study were selected from the Rochester Epidemiology Project (REP), which links and indexes virtually all residents of Olmsted County in MN. In 2003, a random sample of 5,897 residents who were of ages 30 years and older and who had a health care visit in the last 3 years was selected from REP and mailed a questionnaire on demographics, health status and pain. A total of 3,575 (61%) residents completed the questionnaire. [6, 7] From December 2004 through January 2006, we conducted in-depth telephone interviews in a stratified random sample of survey respondents who had reported having chronic pain (defined as having any pain for 3 months or longer) or no chronic pain. Telephone interviews, which lasted approximately 45 minutes collecting only quantitative information, were conducted by trained research coordinators using a Computer Assisted Telephone Interview system. Among 907 patients (89.6% of all invited) who completed the telephone interview, we excluded 166 patients who reported chronic pain on the mailed survey but whose pain had resolved at the time of the telephone interview. This analysis thus includes 741 participants, of whom 591 participants reported having chronic pain and 150 patients did not report having chronic pain.
Chronic pain groups were divided into the following categories: abdominal pain, back pain, joint pain, multisite pain, neuropathic pain at any of the sites of interest or no chronic pain. A definition of multisite pain was substituted for chronic widespread pain. [8] Multisite pain was defined as having pain in three or more of the following groups: head and face/jaw; neck, upper back, mid back and low back; upper abdomen, lower abdomen, pelvis or genitals; or upper arm, lower arm, upper leg and lower leg. Neuropathic pain was based on Self-Administered Leeds Assessment of Neuropathic Signs and Symptoms (S-LANSS) score of ≥12 or reported having nerve pain. [9] The no pain control group was selected from survey participants without chronic pain, the majority of whom did not have any pain but some did report acute or sub-acute pain (pain lasting less than 3 months).
The Brief Pain Inventory (BPI) inquires about the severity of pain on an 11–point scale ranging from 0 (corresponding to ‘no pain’) to 10 (‘pain as bad as you can imagine’) [10]. We categorized worst pain in the last week as a measure of severity of pain as follows: mild pain (1–3), moderate pain (4–6) and severe pain (7–10). Pain interference with daily activities, specifically general activity, mood, walking ability, normal work, relations with other people, sleep and enjoyment of life, were each evaluated on a similar 11–point scale. For each of those items, we defined pain interference as a score of five or greater. Depressive symptoms were assessed using the Patients Health Questionnaire-9 (PHQ-9) [11] and anxiety symptoms were assessed using the Beck Anxiety Index [12], both of which were scored according to published guidelines. Physical functioning was assessed with the use of a summary score generated from 10 questions in the Medical Outcomes Study Physical Functioning (MOS-SF). [13] The mean score of MOS-SF ranges from 0 to 100, with 100 being the best health state.
The Work Productivity and Activity Impairment Questionnaire (WPAI) was used to measure work productivity loss. [14] The WPAI inquires about the number of hours per week missed from work for a health-related reason (absenteeism) and the percentage of health-related reduced performance while at work (presenteeism). Lost productive time was calculated by summing health-related missed work hours and total hours equivalent of reduced performance at work.
We also inquired about complementary and alternative medicine use, including use of chiropractic, nutritional advice or lifestyle diets, spiritual healing or prayer, massage therapy, herbal remedies, acupuncture and others, which were based on questions from Medical Expenditure Survey. [15]
Data analysis
Descriptive statistics were used to assess patient’s demographic, clinical characteristics and health seeking behaviours. Chi-square or Fisher’s exact test was used for categorical variables and Wilcoxon rank-sum or Kruskal–Wallis test for continuous variables. We evaluated the impact of chronic pain by site and neuropathic categories on pain interference with daily activities, physical functioning and also work productivity. The multivariate generalized linear model using the robust variance estimator was build to assess the impact of chronic pain on physical functioning score. The multivariate binomial regression model with log-link function was used to estimate the impact of chronic pain on any work productivity loss time. In the multivariate model, we adjusted for following potential confounding factors based on prior studies: age category, gender, education, general health status, obesity and mild/major depressive symptoms.
Results
Characteristics of study patients by chronic pain

Table 1 Chronic pain sufferers were more likely to be women (64% versus 47%; P < 0.001), in fair or poor general health (18% versus 5%; P < 0.001), and have less than a college education compared to those without chronic pain (40% versus 52%; P = 0.016; Table 1). They were also more likely to be obese (31% versus 20%; P = 0.012), and exhibit mild/major depressive symptoms (25% versus 5%; P < 0.001) and anxiety (14% versus 5%; P = 0.001). Patients with chronic pain reported experiencing a long (median of 9 years; IQR = 4, 20) and frequent pain (85% experiencing pain ≥8 days per month). About 14% of participants reported difficulties in obtaining care and that they did not receive needed care. Almost 15% of participants reported no prior physician diagnosis of chronic pain.
Severe chronic pain (worst pain score in the last week ≥7) as compared to less severe pain (worst pain score 1–3) was also associated with female gender, low education level, obesity and depressive symptoms and anxiety model (Supplementary Table 1). Patients with severe chronic pain were less likely to be working as compared to those with less severe pain (55% versus 72%; P = 0.004).
Alternative medicine use was reported in 81% of chronic pain patients, which was higher than those without chronic pain (64%; P < 0.001). Use of chiropractic (46%), spiritual healing or prayer (40%) and nutritional or lifestyle diets (39%) were reported among chronic pain patients.

Table 2
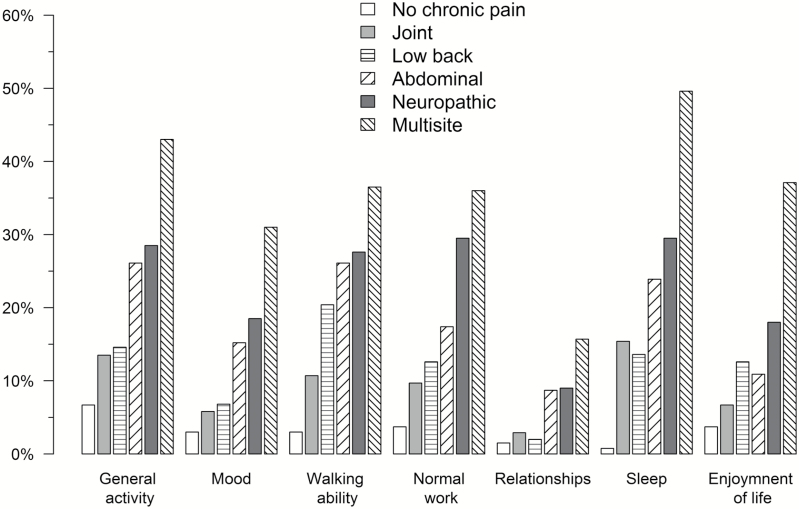
Figure 1

Table 3 Participants with multisite chronic pain were more likely to be women (76%) and in fair or poor general health (35%) as compared to those with other categories of chronic pain or the no chronic pain participants (Table 2). Patients suffering from multisite chronic pain were more likely to have long duration, frequent and intense pain. Patients suffering from neuropathic pain, abdominal pain, joint chronic pain and low back pain also reported long duration and frequent pain. Almost one-third of patients with multisite pain (33%) and neuropathic pain (32%) reported mild/major depressive symptoms.
Interference with daily activities and physical functioning by chronic pain Patients suffering from chronic pain reported significant pain interferences (scale ≥5) in general activity (26%), mood (16%), walking ability (25%), normal work (23%), sleep (28%) and enjoyment of life (18%; P < 0.001 for all comparisons with non-chronic pain group). Multisite pain and neuropathic pain substantially interfered with all daily activities (Figure 1). A substantial proportion of patients with multisite pain (49%) and neuropathic pain (30%) reported pain interference with sleep.
Chronic pain was also significantly associated with impaired physical functioning (Medical Outcomes Study PF score 72.9 ± 24.0 versus 89.4 ± 18.1; P < 0.001), with multisite chronic pain showing the greatest impairment (60.9 ± 26.5). Chronic pain remained significantly associated with lower physical functioning score after adjusting for age, gender, education, obesity and depressive symptoms in the multivariate model (Table 3).
Work productivity loss by chronic pain

Table 4 Employed participants with chronic pain reported significantly greater degree of lost productivity (mean 5.4 hours (±9.3) per week among participants with chronic pain versus 2.0 hours (±5.6) per week among participants without chronic pain; P < 0.001). Chronic pain was significantly associated with reduced performance at work (presenteeism) but not with missed work hours (absenteeism; Table 4). Reported average reduction in work productivity varied from 2.4 hours (±5.6) per week for adults with joint chronic pain to 6.1 hours (±9.7) per week for adults with abdominal chronic pain and 9.8 hours (±11.1) per week for adults with multisite chronic pain. Chronic pain was significantly associated with productivity loss after adjusting for depressive symptoms and other factors in the multivariate model (Supplementary Table 2).
Discussion
Chronic pain adversely affected daily activities, physical and psychological health, and work productivity in our community-based study. Patients suffering from severe chronic pain and also multisite chronic pain were more likely to be women, unemployed, obese, in a fair or poor general heath and from low socioeconomic status. Our findings add to the prior literature by characterizing different categories of chronic pain and their adverse impact on health-related quality of life and work productivity. Patients with multisite pain and neuropathic pain were most affected. Most prior studies included only patients reporting moderate or severe pain, recruited in the clinic or hospital setting. One of the strengths of our study is that we included patients with chronic pain of all intensities, from mild to severe, in the community.
Consistent with prior literature, patients with chronic pain reported a higher prevalence of anxiety and depressive symptoms. [4, 5, 16] We also found that increasing severity of pain and chronic multisite pain to be associated with higher prevalence of depressive symptoms. Chronic pain and psychological comorbidities may aggravate one another and create a vicious cycle. [1, 17] Pain increases the risk of developing depression, whereas depression may in turn result in exacerbation and persistent of pain, and cause sleep deprivation and interference with daily activities. [17] Thus, it is important for physicians to identify and address comorbid psychological symptoms to effectively treat chronic pain. [1]
We also evaluated societal burden of chronic pain. Chronic pain was associated with loss of work productivity on average of 5.4 hours per week. The reduction in work productivity varied widely from an average of 2.4 hours per week for joint chronic pain to 9.8 hours per week for multisite chronic pain. Importantly, majority of lost productivity due to chronic pain was from reduced performance at work. Similar to our findings, a prior study reported that arthritis or back pain results in work productivity lost of 5.2 hours per week. [18] Previously, reduced performance at work was reported to be 28% of their working time for back pain, 32% for arthritis pain and 45% for fibromyalgia pain. [19] While we were unable to identify fibromyalgia, our definition of multisite pain was used as a proxy for chronic widespread pain and fibromyalgia. Chronic pain affects working adults and contributes to substantial lost productivity. [18, 19] It has been estimated that persistent pain affects 100 million adults and leads to approximately $560 to $635 billion annually in total societal costs, including healthcare costs and work productivity, in the USA, greater than the costs of heart disease, cancer or diabetes. [20]
Our study also shows challenges in obtaining needed medical care. Despite experiencing long and severe duration of pain and interference with daily activities, 15% of study participants reported they have not informed their physician about their chronic pain. These results confirm prior work demonstrating a large unmet medical need in chronic pain sufferers. [6] The majority of pain sufferers (81%) reported the use of alternative medicine, which may help treat chronic pain but must be communicated to primary care physicians so that it can be fully integrated into patient care.
Our study has strengths and limitations. We were able to use a community based sample which identifies those with chronic pain despite use of health care services for pain. By using a sample of individuals who reported on pain a year prior to this study, we were able to identify those with truly long standing chronic pain. We used the patient’s description of site and type of pain to categorize pain and illustrated variation by chronic pain category. However, our study was cross-sectional and we were unable to assess the effect of comorbid conditions or treatment on the future occurrence of pain or intensity or duration of pain. The majority of adults participated in the Olmsted Country Health Study were White, which may have limited the generalizability of findings to other populations. Although our study is based on the data from 2004 to 2006, our findings are likely generalizable to the present. The clinical practice for patients with chronic pain has not changed over the last decade, with the exception of greater awareness of opioid addiction.
Conclusions
We assessed the burden of chronic pain from patients’ perspective in multiple domains of physical, psychological, and social functioning and well-being. Chronic pain, particularly multisite pain and neuropathic pain, significantly affected physical and psychological health. In addition to the negative impacts on the psychological and physical of the individual, chronic pain places a significant burden on society through lost work productivity and reduced performance at work. Our study emphasizes the importance of understanding chronic pain as a multifaceted health condition that requires a multidisciplinary treatment approach.
Supplementary data
Funding:
the Division of Epidemiology of Astra Zeneca; the resources of the Rochester Epidemiology Project was supported by research grant R01 AR030582, from the National Institute on Aging of the National Institutes of Health, US Department of Health and Human Services.
Ethical approval:
the Olmsted Medical Center and Mayo Clinic Institutional Review Boards approved the study.
Conflicts of interest:
none.
References
Marcus D.
Chronic pain: a primary care guide to practical management.
2nd edn Humana Press; 2009.Henschke N, Kamper SJ, Maher CG.
The epidemiology and economic consequences of pain.
Mayo Clin Proc 2015; 90: 139–47Gormsen L, Rosenberg R, Bach FW, Jensen TS.
Depression, anxiety, health-related quality of life and pain
in patients with chronic fibromyalgia and neuropathic pain.
Eur J Pain 2010; 14: 127.e1–8Elliott TE, Renier CM, Palcher JA.
Chronic pain, depression, and quality of life:
correlations and predictive value of the SF-36.
Pain Med 2003; 4: 331–9Kroenke K, Outcalt S, Krebs E, et al.
Association between anxiety, health-related quality of life and
functional impairment in primary care patients with chronic pain.
Gen Hosp Psychiatry 2013; 35: 359–65Watkins E, Wollan PC, Melton LJ, III, Yawn BP.
Silent pain sufferers.
Mayo Clin Proc 2006; 81: 167–71Yawn BP, Wollan PC, Weingarten TN, et al.
The prevalence of neuropathic pain:
clinical evaluation compared with screening tools in a community population.
Pain Med 2009; 10: 586–93MacFarlane GJ, Croft PR, Schollum J, Silman AJ.
Widespread pain: is an improved classification possible?
J Rheumatol 1996; 23: 1628–32Weingarten TN, Watson JC, Hooten WM, et al.
Validation of the S-LANSS in the community setting.
Pain 2007; 132: 189–94Cleeland CS, Ryan KM.
Pain assessment: global use of the Brief Pain Inventory.
Ann Acad Med Singapore 1994; 23: 129–38Kroenke K, Spitzer RL, Williams JB.
The PHQ-9: validity of a brief depression severity measure.
J Gen Intern Med 2001; 16: 606–13Beck AT, Epstein N, Brown G, Steer RA.
An inventory for measuring clinical anxiety: psychometric properties.
J Consult Clin Psychol 1988; 56: 893–7Stewart AL, Greenfield S, Hays RD, et al.
Functional status and well-being of patients with chronic conditions.
Results from the Medical Outcomes Study.
JAMA 1989; 262: 907–13Reilly MC, Zbrozek AS, Dukes EM.
The validity and reproducibility of a work productivity and activity impairment instrument.
Pharmacoeconomics 1993; 4: 353–65Cohen JW, Cohen SB, Banthin JS.
The medical expenditure panel survey: a national information resource
to support healthcare cost research and inform policy and practice.
Med Care 2009; 47(7suppl 1): S44–50Jensen HI, Plesner K, Kvorning N, Krogh BL, Kimper-Karl A.
Associations between demographics and health-related quality of life
for chronic non-malignant pain patients treated at a
multidisciplinary pain centre: a cohort study.
Int J Qual Health Care 2016; 28: 86–91Elliott AM, Smith BH, Hannaford PC, Smith WC, Chambers WA.
The course of chronic pain in the community: results of a 4-year follow-up study.
Pain 2002; 99: 299–307Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R.
Lost productive time and cost due to common pain conditions in the US workforce.
JAMA 2003; 290: 2443–54McDonald M, DiBonaventura Md, Ullman S.
Musculoskeletal pain in the workforce: the effects of back, arthritis,
and fibromyalgia pain on quality of life and work productivity.
J Occup Environ Med 2011; 53: 765–70Gaskin DJ, Richard P.
The Economic Costs of Pain in the United States
Journal of Pain 2012 (Aug); 13 (8): 715–724
Return LOW BACK PAIN
Return to SPINAL PAIN MANAGEMENT
Since 8-21-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |