

Resolution of Hearing Loss
After Chiropractic ManipulationThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Topics in Integrative Health Care 2014 (Sep 30); 5 (3) ~ FULL TEXT
OPEN ACCESS Melissa Ferranti, DC, Kimberly Keene, DC, Chelsea Prothero, DC
Assistant Professor and Faculty Clinician
Palmer College of Chiropractic
Port Orange, FL, USAIntroduction: While chiropractic care is often associated with the treatment of musculoskeletal conditions, there are other, non-musculoskeletal conditions which may benefit from spinal manipulation (SM). This paper reports on the return of hearing in a woman treated with chiropractic adjustments after 8 months of lack of improvement through allopathic care. Pre and post audiograms were used for comparison.
Case Presentation: In this report, a 46 year old white female with neck pain, tinnitus, and hearing loss was treated with cervical spinal manipulation with positive results. A pre-treatment audiogram indicated low-frequency hearing loss, worse in the left ear.
Intervention and Outcomes: After being unsuccessfully medically treated over an 8 month period, she sought chiropractic care for the above symptoms. After 3 chiropractic adjustments, her hearing and associated symptoms were significantly improved. She received 12 treatments over a 4–month period. When asked to rate her hearing and fullness sensation in the ear on a Patient Specific Functional Scale with a 0–10 measure, where 0 is no deficits and 10 is completely impaired, initially she rated her symptoms as 7, and 5 months after the conclusion of care, her rating dropped to 1. Following treatment her audiogram was normal.
Conclusion: This report details the condition and treatment of a female patient with cervicalgia and associated hearing loss (HL). Possible mechanisms for these results are discussed. This case along with others previously published, [1–4] aid in the consideration of (SM) as a possible intervention for HL associated with cervicalgia.
From the Full-Text Article:
Introduction
While there have been anecdotal accounts of resolution of hearing loss following spinal manipulation (SM), and several case studies published, [1–4] no randomized controlled trials (RCTs) are present in the scientific literature in which patients with hearing loss (HL) are randomly treated with SM, placebo, or other interventions.
In 2003–2004 the prevalence of speech-frequency HL in United States adults was estimated to be 16.1%. [5] HL, which can lead to functional decline and depression, is the most wide spread sensory impairment in aging people. It is the 3rd most common chronic condition in older Americans, after hypertension and arthritis. [6]
Audiograms test the ability to hear sounds. Sounds vary based on their loudness (intensity) and the speed of sound wave vibrations (tone). In detailed audiometry, hearing is normal if one can hear tones from 250 Hz – 8,000 Hz at 25 dB or lower. The minimum intensity (volume) required to hear a tone is graphed. An attachment called a bone oscillator is placed against the bone behind each ear (mastoid bone) to test bone conduction. [7]
Some causes of hearing loss include damage to the inner ear, buildup of earwax, infections, and tympanic membrane perforation. Other common reasons include aging, heredity, occupational noises, recreational noises, deep diving pressure changes, medications or illnesses. [8]
Conductive HL is caused by a mechanical problem in the middle or outer ear. While not as common as sensorineural loss, it is still common in older adults. In conductive HL, ossicles may not conduct sound properly, the eardrum may not vibrate in response to sound, or there may be fluid in the middle ear. Most commonly the cochlea and the middle ear are involved; rarely are the brainstem or auditory nerve involved. [9] There may also be an association between cervical spine trauma, such as whiplash, and HL. The U.S. Census data for 2003 estimates the incidence of Cervical Acceleration Deceleration (CAD) injury at 1,472,867 million per year. [10] Approximately 10% of patients who have suffered whiplash injury will develop otological symptoms such as tinnitus, deafness and vertigo. [11] Tinnitus, which was an associated symptom in this case, affects up to one-third of all adults sometime in their life, and 15% of adults have prolonged tinnitus associated with HL, requiring medical attention. [9]
Usual medical treatment of these disorders depends on the etiology. Medication, hearing aids, and/or surgery can be expensive and less than optimal. [6] If there were a safe and effective manual therapy which could address this problem, patients could utilize SM first, and if non-responsive, could then resort to more invasive measures.
Case Presentation
A 46–year-old female sought care for chronic neck pain with associated left-sided tinnitus and HL, which she first noticed after swimming. This began as a “ringing” in her left ear, and progressed to a “fullness sensation” in her left ear and temporal region, with difficulty hearing out of that ear. She had been previously seen by an ear, nose, and throat (ENT) specialist for evaluation and treatment. An audiogram had been performed which showed conductive HL on the left at 500 Hz (low frequency). (Figure 1A) The finding was conductive hearing loss due to nerve damage diagnosed by the ENT. Patient received medications, which patient reported provided no help.
In our examination of the patient, bilateral cervical lateral flexion as well as extension were painful and restricted. Patient’s blood pressure was 100/80, and she has a family history of diabetes and high blood pressure. Anterior weight bearing of the head and cervical hypolordosis was noted. Spinal palpation revealed tenderness on the left at levels C1, C2, and C3. No abnormalities were detected on otoscopic or the remainder of the physical examination. A diagnosis of conductive HL and associated cervical spine segmental dysfunction was made.
Intervention and Outcomes
Patient was seen for 12 total visits, with a frequency of 1 time per week for a period of 4 months. Her care included full spine adjustments determined by static and motion palpation, and electrical muscle stimulation in the upper thoracic region, as well as home cervical exercises. Manipulative treatment of the cervical spine consisted of supine diversified technique, in which she was placed face up and the spinal level of involvement was contacted on the lamina-pedicle junction on the side of vertebral body rotation. Her head was laterally flexed over the contact hand and rotated away. A high-velocity, low-amplitude (HVLA) thrust was then given to the specific levels (C1 through C3), depending on findings each visit. Thoracic and lumbar spine was also adjusted as restrictions were detected throughout treatment plan. Segments from T3–T5 were corrected with Double Thenar Technique, and lumbar spine segments L1–L5 were treated with Flexion Distraction.
Various outcome assessment tools were utilized to track her progress over the course of care. First, a Quadruple Visual Analog Scale (QVAS) was utilized, in which the patient rated her neck pain from 0 (no pain) to 10 (severe pain). Her neck pain scores fluctuated significantly, from 18% to 65% to 33% and then 12% at the conclusion of care. An additional outcome assessment, the Patient Specific Functional Scale (PSFS) was used to further track progress of HL. This scale measured the intensity of the “fullness sensation” in her ear; 0 indicated no fullness and 10 indicated very severe fullness. Prior to care she rated this fullness sensation as 7/10, and five months after the conclusion of care her rating was 1/10. Before and after audiograms which showed improvement were also performed (Figures 1 and 2). After her third treatment, she stated that the fullness sensation in her ear and her hearing were significantly improved. She continued to improve and was released after 12 visits.
Figure 1. Pre-treatment audiogram
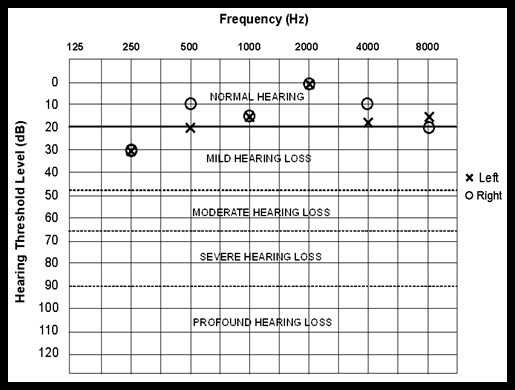
12/14/09: Audiogram shows audible thresholds for standardized frequencies
to determine the extent of patient-reported hearing loss. Both the left (X)
and right (O) ears were tested. Mild hearing loss was noted at 30 decibels
(dB) and 250Hz in both ears.
Figure 2. Post-treatment audiogram
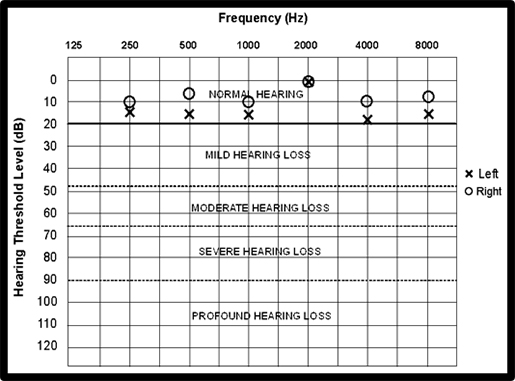
12/13/10: Post audiogram shows audible thresholds for standardized frequencies
to determine the extent of change in patient-reported hearing loss.
Both the left (X) and right (O) ears were tested, and all measured points
bilaterally fell within normal hearing standards.
Discussion
In reviewing the literature listed in the electronic databases of PubMed and Index of Chiropractic Literature, several reports make mention of an association between cervical spine disorders and hearing loss. For example, one study shows that in 420 patients with fullness in the ear, vertigo, fluctuating hearing, and tinnitus, 60% had a history of whiplash injury. [12] Further, most had been to a physiotherapist or chiropractor for the treatment of back or neck problems. 51 patients showed normal hearing levels, a mild Eustachian tube dysfunction, mydriasis, and a functional disorder of the upper cervical spine, diagnosed as cervicogenic otoocular syndrome. There appears to be an association between musculoskeletal complaints and eye and/or ear complaints in these patients. [12]
In a reported case from Germany, a 36–year-old soccer player hit his head with the ball and had sudden hearing loss in his right ear. After a single manipulation to the thoracic spine (T6), the right sacroiliac joint, and the right side of the neck (C2–C4) his hearing immediately improved. [13] In another report, 15 hearing-impaired patients instantly had improved hearing following 1 cervical SM per audiograms. [1] Kessinger reported that when a 75–year-old woman with a longstanding history of vertigo, tinnitus, and HL received upper cervical-specific chiropractic care, her hearing improved as measured by audiogram. [14] Following chiropractic care of the upper cervical spine and cervical distraction exercises, marked resolution of a 3–year-old girl’s HL and painful effusive otitis media was reported by Brown. [15] Results were confirmed by the patient’s pediatrician and audiology tests.
In our case, the patient did not seek chiropractic care until 8 months after her initial diagnosis by the ENT, and, in spite of the chronicity of her complaint, within 3 treatments the tinnitus and HL were largely resolved. Therefore, we do not believe that this is a case of spontaneous remission. It might be argued that she simply had water in her ear from swimming, causing the conduction loss, and that SM facilitated the fluid draining from the ear. However, 2 otoscopic examinations detected no abnormalities. Also, while the non-musculoskeletal complaints of tinnitus and HL largely resolved early in care, her neck pain seems to not have been substantially affected, dropping from 18% to 12% on the QVAS, which is not a significant change. Ergo, the musculoskeletal complaint did not respond as well as the non-musculoskeletal complaint.
Guzman et al. looked at numerous manual therapies and made recommendations for the treatment of neck pain. Seventeen studies were reviewed and positive evidence was found for both mobilization and manipulation, particularly when combined with exercise was noted. [16] The relation between manual treatments and serious complication is controversial; however, a systematic review of the literature published in 2013 found no epidemiological studies that validate that there is an association between ischemic stroke after cervical spine manipulation. [17] It is suggested by Cassidy et al. that the odds of having a stroke following a visit to a doctor of chiropractic are no greater than the odds of having a stroke following a visit to a primary care doctor. [18] Since the patient had a blood pressure within normal limits, and presented with no abnormal vascular symptoms, she was deemed a candidate for SM.
Improvement in non-musculoskeletal complaints is a common finding among practicing chiropractors: a patient presents with a musculoskeletal complaint such as neck or back pain, and while those symptoms often improve under care, the patient may have improvement in other complaints that are unrelated and unexpected. For example, patients commonly report improvements in breathing, circulation, and digestion, among other problems. [19] There are several possible mechanisms to explain how cervical SM may affect hearing. One of these is cortical neuroplasticity, which is an important property of the auditory system. [1] Central plastic changes are most likely the result of relatively simple alterations in the balance of excitatory and/or inhibitory inputs produced by chiropractic manipulation. [1] There may also be central plastic changes which occur in the brainstem at the level of the vestibular nerve. The vestibular nuclei integrate signals from the vestibular organs and visual system with those of the somatic system. [1] Neurophysiologic changes associated with speech-sound perception can be measured, thereby indicating that central sensory representation is plastic. [20]
Pickar has suggested that SM has a physiological effect on the inflow of sensory information into the central nervous system (CNS), affecting primary afferent neurons from par spinal tissues. [21] Mechanical and chemical changes in the spinal structures such as the intervertebral foramen can affect the dorsal root ganglia and cause reflex changes in the CNS. He suggests that perhaps central sensory processing is altered through SM by removing subthreshold mechanical or chemical stimuli affecting somatosomatic reflexes. While he does not directly apply this theory to conductive hearing loss, if one extrapolates, it may be that mechanical and/or chemical noxious stimuli within the ear reflexively affect the cervical spine via the dorsal root ganglia contributing to cervical segmental dysfunction.
Another possible mechanism involves activating thalamic and cortical pathways via cervical SM. Carrick examined the changes in brain function after manipulation of the cervical spine by mapping the physiological cortical maps in 500 test subjects. By examining the visual field’s blind spot dimension changes, he suggested that cervical manipulation has a significant ability to increase contralateral thalamic and cortical activity. Cervical SM activates specific neurological pathways and may be associated with an increase or decrease in brain function depending upon the side of the manipulation and the cortical hemisphericity of a patient. [22]
To extrapolate from Carrick’s findings, another explanation involves the manner in which auditory communication is conveyed to the brain. There are 2 different pathways: the primary auditory pathway which carries messages from the cochlea, and the reticular sensory pathway which carries all types of sensory messages. The first relay of the primary auditory pathway and the reticular sensory pathway occurs in the cochlear nucleus in the brain stem. It is possible that cervical SM, by way of joint receptors, evokes primary afferents of the auditory nerve, possibly at this cochlear level in the brainstem, affecting the ipsilateral cerebellar projection in the reticular sensory pathway and the ipsilateral cerebellar projection to the contralateral thalamocortical tracts of the primary auditory pathway. [22, 23] When these pathways are disrupted either through trauma or otherwise, altered auditory processing may be associated with difficulties in hearing and understanding speech. [24]
Whatever the mechanism, it appears that cervical SM had a positive impact in the hearing and associated symptoms of this patient.
Conclusion
This case suggests that upper cervical spine manipulation may have positively affected hearing loss and tinnitus associated with cervicogenic pain in this patient. While there are other treatment options to aid such complaints in adult patients, something as simple and safe as SM should be considered a possible intervention. Several mechanisms may explain the neuropathophysiology of this condition and how it is affected by SM; however, this has not been well-explored and warrants additional study.
Acknowledgements
The authors report no conflicts of interest or funding support. The authors would like to thank Dana Lawrence D.C. and Philip Afghani, D.C. for their assistance in editing.
References
Di Duro JO.
Improvement in Hearing After Chiropractic Care: A Case Series
Chiropractic & Osteopathy 2006 (Jan 19); 14 (1): 2Emary PC.
Chiropractic Management of a 40–year-old Female Patient With Ménière Disease
J Chiropr Med. 2010 (Mar); 9 (1): 22–27Hulse M.
Cervicogenic hearing loss.
Die Zervikogene Horstorung 1994;42:604-613
Oser A, Steinhauser J.
Manual treatment of the cervical spinal column for tinnitus after acute hearing loss-a case report.
Forsch Komplementmed 2010;17:3:147-8
Agrawal Y, Platz EA, Niparko JK.
Prevalence of hearing loss and differences by demographic characteristics among US adults data from the National Health and Nutrition Examination Survey, 1999-2004.
Arch Intern Med 2008;168:14:1522-30
Bogardus ST JR, Yueh B, Shekelle PG.
Screening and management of adult hearing loss in primary care: clinical applications.
JAMA 2003;15:1986-90
Audiometry.
Medline Plus.
http://www.nlm.nih.gov/medlineplus/ency/article/003341.htm
Accessed July 8, 2014
Hearing loss causes.
Mayo Clinic.
http://www.mayoclinic.org/diseases-conditions/hearing-loss/basics/causes/con-20027684.
Accessed July 8, 2014
American Speech-Language-Hearing Association:
Incidence and prevalence of hearing loss and hearing aid use in the United States. 2008:
http://www.asha.org/research/reports/hearing.html.
Accessed July 7, 2012. 10
Quinlan KP, Annest JL, Myers B, Ryan G, Hill H.
Neck strains and sprains among motor vehicle occupants- United States, 2000.
Accid Anal Prev 2004;36:1:21-7
Tranter RM, Graham JR.
A Review of the Otological Aspects of Whiplash Injury
Journal of Forensic and Legal Medicine 2009 (Feb); 16 (2): 53–55Franz B, Altidis P, Altidis B, Collis-Brown G.
The cervicogenic otoocular syndrome: a suspected forerunner of Meniere’s disease.
Int Tinnitus J 1999;5:2:125-30
Wagner UA, FJ,
Treatment of sudden deafness by manipulation of the cervical spine.
Manuelle Medizin 1998;36:269-71
Kessinger RC, Boneva DV.
Vertigo, Tinnitus, and Hearing Loss in the Geriatric Patient
J Manipulative Physiol Ther 2000 (Jun); 23 (5): 352–362
Brown CD.
Improved hearing and resolution of otitis media with effusion following chiropractic care to reduce vertebral subluxation.
J Pediatr Matern & Fam Health – Chiropr 2009;1:7
Guzman J, Haldeman S, Carroll LJ, et al.
Clinical Practice Implications of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders:
From Concepts and Findings to Recommendations
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S199–S212Chadwick LR, Cote P, Stern P, L’Esperance G.
The association between cervical spine manipulation and carotid artery dissection: a systematic review of the literature;
J Manipulative Physiol Ther Advance online publication. DOI: 10.1016/j.jmpt.2013.09.005
Cassidy JD, Boyle E, Cote P, et al.
Risk of Vertebrobasilar Stroke and Chiropractic Care: Results of a Population-based
Case-control and Case-crossover Study
Spine (Phila Pa 1976) 2008 (Feb 15); 33 (4 Suppl): S176–183Leboeuf-Yde, C., Pedersen, E.N., Bryner, P., Cosman, D., Hayek, R.
Self-reported Nonmusculoskeletal Responses to Chiropractic Intervention:
A Multination Survey
J Manipulative Physiol Ther 2005 (Jun); 28 (5): 294–302Kraus N, McGee TJ, Koch DB.
Speech sound representation, perception, and plasticity: A neurophysiologic perspective.
Audiology & Neurotol 1998;3:168-82
Pickar JG.
Neurophysiological Effects of Spinal Manipulation
Spine J (N American Spine Society) 2002 (Sep); 2 (5): 357–371Carrick FR.
Changes in brain function after manipulation of the cervical spine.
J Manipulative Physiol Ther 1997;529-45
Pujol R.
Journey into the world of hearing.
http://www.cochlea.org/en/spe/auditory-brain-2.html.
Accessed July 7, 2012
Almeida CIR,
Logoaudiometria utilizando sentenças sintéticas
[The role of the cerebellum in auditory processing using the SSI test].
Braz J Otorhinolaryngol 1988;54:3:68-72
Return to CHIROPRACTIC AND DEAFNESS
Since 10-06-2014


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |