

Sagittal Standing Posture and its Association with Spinal Pain:
A School-based Epidemiological Study of 1196 Flemish
Adolescents Before Age at Peak Height VelocityThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Spine (Phila Pa 1976). 2012 (Sep 1); 37 (19): 1657-1666 ~ FULL TEXT
Mieke Dolphens; Barbara Cagnie; Pascal Coorevits; Guy Vanderstraeten; Greet Cardon; Roseline D'hooge; Lieven Danneels
Department of Rehabilitation Sciences and Physiotherapy,
Faculty of Medicine and Health Sciences,
Ghent University, Artevelde University College, Ghent, Belgium
STUDY DESIGN: Cross-sectional baseline data set on the sagittal standing posture of 1196 adolescents.
OBJECTIVE: To describe and quantify common variations in the sagittal standing alignment in boys and girls who are in the same phase of growth and to explore the association between habitual standing posture and measures for spinal pain.
SUMMARY OF BACKGROUND DATA: Data on postural characteristics and spinal pain measures in adolescence are sparse, especially when somatic and biological maturity status is to be considered. Our understanding of the relationship between standing posture in the sagittal plane and spinal pain is also deficient.
METHODS: A total of 639 boys (age [mean ± SD], 12.6 ± 0.54 yr) and 557 girls (10.6 ± 0.47 yr), with predicted years from peak height velocity (PHV) being 1.2 ± 0.71 and 1.2 ± 0.59 pre-PHV, respectively, were studied. Postural examination included the assessment of global alignment and local spinopelvic characteristics, using post hoc analyses of digital images and direct body measurements (palpation, digital inclinometry, and wheeled accelerometry). Spinal pain experience was assessed by questionnaire.
RESULTS: A wide interindividual variation in sagittal posture characteristics was observed. Logistic regression analyses yielded global alignment parameters to be associated with low back pain (lifetime prevalence), neck pain (lifetime prevalence, 1–mo prevalence, and doctor visit), and thoracic spine pain (doctor visit) outcome measures. None of the included local spinopelvic parameters could be identified as an associated factor with measures of spinal pain.
There are more articles like this @ our: SPINAL ALLIGNMENT/CERVICAL CURVE Page Page CONCLUSION: The orientation of gross body segments with respect to the gravity line seems superior to local spinopelvic features in terms of clinical importance, at least in the current pre-PHV cohort. Opportunities may exist for postural subgrouping strategies to begin with global alignment parameters in order to gain further insight into the relationship between sagittal alignment and the relative risk of developing spinal pain/seeking medical consultation for this pain.
From the FULL TEXT Article:
Introduction
There is a belief among clinicians that “nonneutral” postures when compared with “neutral” or “ideal” postures involve different patterns of mechanical loading and motor control, resulting in a mechanism with tissue strain and pain. Consequently, postural retraining has traditionally been an integral part of physiotherapeutic intervention in the prevention and treatment of spinal pain disorders. Evidence from epidemiological studies, however, does not support an association between sagittal spinal curves and spinal pain. [1, 2] It is also well established that the physiological upright standing posture can be reached in a different way for each person with a unique and individual pattern of spinopelvic balance and sagittal alignment. [3, 4] Accordingly, previous publications have documented a high degree of variability in the sagittal standing alignment of the human spine and pelvis in healthy adolescents, [5–7] adults, [3, 5 ,8 ,9] middle-aged and older subjects, 10 and populations experiencing spinal pain. [11–13] Characteristic changes in sagittal alignment have also been identified throughout the entire time of ontogenesis. [5, 14–18]
Two separate yet intermingled control mechanisms are involved in building up standing posture: one relating to the control of the center of mass projection with respect to the feet, and another relating to the orientation of body segments with respect to the vertical. [19] The center of gravity projection or the gravity line has been shown to be located within a narrow perimeter in relation to the feet in standing subjects. [18, 20] On the contrary, when regarding the geometry of the body, one viewpoint in the literature is that posture is based on the superimposed segments (head, trunk, and legs), each of which is linked to the next, preserving the specifi c orientation of each segment with respect to the external world and/ or adjacent segment. [19] Only a relatively few studies regarding posture or its clinical relevance have addressed the orientation of gross body segments in space by implementing a type of a sagittal plumb line assessment, [16, 21–27] whereas a multitude of studies have focused on regional or segmental spinopelvic features. [10, 11, 14, 28–30] It should be noted that most of the studies that have considered global alignment were radiological examinations, implying that an accurate representation of the relaxed standing posture might be challenged. [31] Furthermore, anatomically remote factors, such as the alignment of the lower limb segment, have been largely overlooked despite their potential signifi cance in closed kinematic chain activities such as standing. [32]
In a recent systematic overview of the research literature on the epidemiology of adolescent spinal pain, [33] it was concluded that idiopathic adolescent spinal pain (IASP) is a significant public health issue, with prevalence figures increasing with age in the adolescent period and approaching those in adults by around 18 years of age. As IASP may result in a risk factor for spinal pain as in adult, [33] the focus in relation to research, prevention, and treatment may be predominantly on the young population. Researching individuals in puberty is a challenge because puberty is accompanied by major physical growth and substantial brain maturational changes. [34] Although so-called “growing pains” are reported to be common in younger adolescents [35] and back pain might be considered a “normal life experience” for many young people, [36] the fact that the early adolescent increase in back pain is associated with pubertal status is striking. [37–41] Accordingly, a potential infl uence of puberty on pain, pain perception, or both has been postulated. [34] Furthermore, it has been argued that spinal deformities can easily develop during adolescence, with the development and progression of these deformities can be explained in biological and mechanical terms. [42, 43] Adolescent idiopathic scoliosis, for instance, is shown to be linked to peak growth velocity during puberty [44] and late pubarche, [43] and other conditions, for example, Scheuermann disease, seem to have a peak around puberty. [45]
Although the potential influence of puberty-directed mechanisms on both posture and IASP seems well recognized, maturity status has rarely been applied in research on aforementioned issues or their interrelation. It is well known that girls, on average, mature 2 years before boys. 46 Therefore, the aims of this study were(1) to document normal variations in the sagittal standing alignment including gross body segment indexes and spinopelvic characteristics and
(2) to explore the association between habitual standing posture and measures for spinal pain within a representative sample of young adolescents in Flanders (Belgium), taking into account their maturity status.
MATERIALS AND METHODS
Subjects
A total of 639 boys of mean age 12.6 ± 0.54 years (range, 11.4– 15.0 yr) and 557 girls of mean age 10.6 ± 0.47 years (range, 9.6–13.0 yr) participated in this study. All boys were first-grade students of mainstream secondary education in the Flemish Community of Belgium, whereas girls were all fifth graders of primary education. Schools were selected to obtain a representative sample of youth in Flanders regarding educational networks and educational levels. Subjects were excluded if they had a history of neurological conditions, rheumatic disorders, metabolic or endocrine diseases, major congenital anomalies, skeletal disorders (major leg length discrepancy, spondylolysis, spondylolisthesis, major scoliosis), connective tissue disorders, previous spinal fracture, or previous spinal surgery. All children and guardians provided written informed consent, and ethical approval was granted by the ethics committee of the Ghent University Hospital.
Procedures
Testing included sagittal plane posture assessment during habitual standing, anthropometric measurements, and completion of self-report spinal pain measures. As part of a larger study, an extended selection of physical characteristics, lifestyle factors, and medical issues were recorded, as were sociodemographic, psychological, and psychosocial factors. However, this is beyond the scope of this study. Evaluation occurred during a 6–month period from September 2008 to February 2009 and was organized at schools and local pupil guidance centers.Experimental Protocol—Habitual Posture To quantify global alignment characteristics and local spinopelvic features, post hoc analysis of digital images and a clinical screening protocol (consisting of direct palpation, inclinometry, and wheeled accelerometry) were used, respectively (see Angular Measures Describing Global Sagittal Alignment and Spinopelvic Sagittal Alignment Parameters). Retroreflective markers were first placed on the C7 spinous process, the apex of the thoracic kyphosis, the infl ection point where the spine transitions from kyphosis to lordosis, the apex of the lumbar lordosis, the L5 spinous process, the left greater trochanter, left lateral malleolus, left anterior superior iliac spine (ASIS), and left posterior superior iliac spine (PSIS) by 1 trained examiner. Participants were instructed to stand in their normal, comfortable, relaxed posture, arms resting by the sides, with feet shoulder-width apart and equally balanced on both feet. To standardize the head posture, participants viewed a visual target set 1.5 m in front of them at eye level. Postural data were obtained at the end from 3 standing trials, with each trial lasting 30 seconds. Participants were asked to walk between trials for several steps.
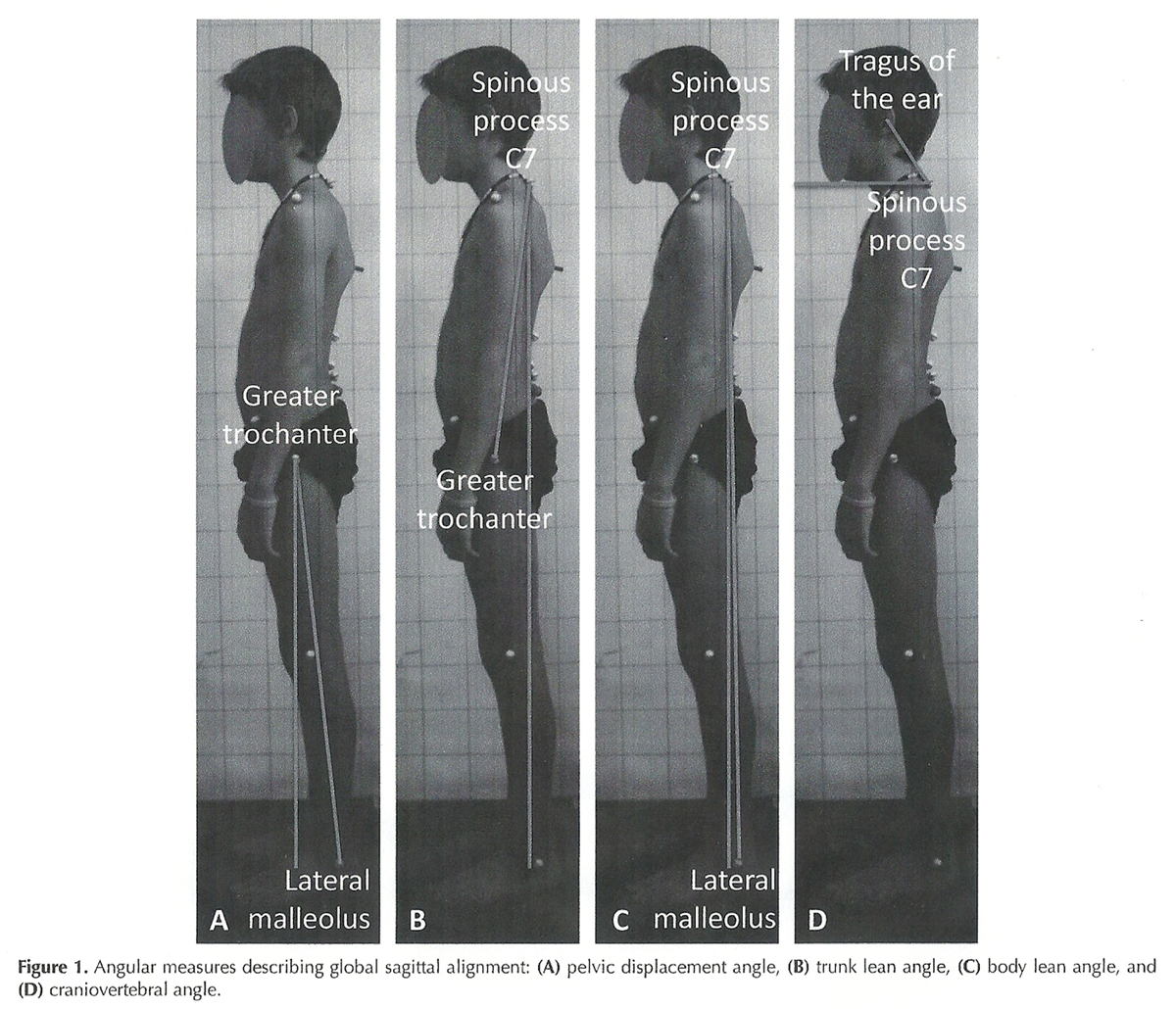
Figure 1 Angular Measures Describing Global Sagittal Alignment For the assessment of global alignment characteristics, 4 angular measures were determined from photographs of the left lateral view obtained by a 12.40–megapixel digital camera (EOS 450D digital camera; Canon, Lake Success, NY), using a standardized photographic setup. Specifi cally, parameters were calculated from the third lateral digitized photograph of the subjects with retrorefl ective markers placed on bony landmarks, using ImageJ software (National Institutes of Health, Bethesda, MD) as follows (Figure 1):
Pelvic displacement angle: Angle between the line joining the greater trochanter and the lateral malleolus and the vertical through the former. A positive value represents a forward carriage of the pelvis relative to the base of support as measured at the ankle, whereas a negative value indicates a backward carriage of the pelvis.
Trunk lean angle: Angle sustained by the line joining the greater trochanter and spinous process C7 with respect to the vertical through the latter. By convention, this angle is expressed as a positive value if the spinous process C7 is posterior to the greater trochanter (backward inclination of the trunk) and negative if it is anterior to the greater trochanter (forward inclination of the trunk).
Body lean angle: Angle between the line joining the lateral malleolus and the spinous process C7 and the vertical through the latter. A positive value indicates the vertical projection of the C7 spinous process to be posterior to the lateral malleolus; a negative value indicates this projection to be anterior to the lateral malleolus.
Craniovertebral angle: Angle formed by the horizontal drawn through the C7 spinous process and the line joining the C7 spinous process with the tragus of the ear. The smaller this angle, the greater the forward head posture.
Spinopelvic Sagittal Alignment Parameters Six lumbopelvic and 3 thoracic parameters were assessed. In this study, the “lumbar” segment of the spine was located between the inflection point where the spine transitions from lordosis to kyphosis and the L5–S1 interspace. Similarly, the “thoracic” segment was defined as existing between the C7–T1 interspace and the inflection point. The determination of lordotic and kyphotic segments was independent of the anatomic location of the thoracolumbar junction at T12–L1.
Lumbopelvic features: Lumbar characteristics that were assessed included the number of vertebrae in the lumbar lordosis, the vertebral level of the lumbar apex, and the total degrees of included curvature. The first 2 parameters were determined by 1 trained examiner via visual inspection and palpation; the degree of lumbar lordosis was calculated using the sum of segmental angles of appropriate vertebral sections obtained by a skin-surface electromechanical device, the Spinal Mouse (Idiag; Voletswil, Switzerland). The intratester and intertester and day-to-day reliability of this wheeled accelerometer has been published in previous studies. [47–49]
To describe the pelvic orientation in the sagittal plane, 2 angular pelvic measures were assessed: pelvic tilt and sacral inclination. Pelvic tilt was quantified via the ASIS-PSIS angle (i.e. , the angle between the horizontal and the line connecting the ASIS and the PSIS), using the Pro 3600 digital inclinometer (SPI-Tronic; Penn Tool Co, Maplewood, NJ) mounted on a caliper with an accuracy of 0.1°. In this study, the left side of the subjects was used for measurement. By convention, the pelvic tilt angle is expressed as a positive value if the ASIS is inferior to the PSIS and as a negative value if it is superior to the PSIS. The sacral inclination with respect to the vertical was measured using the Spinal Mouse device, with positive values indicating a forward inclination of the sacrum and negative values representing backward inclination. In addition, the vertebral level of the intercristal line was determined as a measure of pelvic height. This was done via palpation.
Thoracic spine parameters: The geometric thoracic features that were assessed included the vertebral level of the inflection point where the spine transitions from kyphosis to lordosis, the apex of the thoracic curve, and the degree of included kyphosis. The first 2 parameters were determined via visual inspection and palpation; the degree of thoracic kyphosis was calculated as the sum of segmental angles of appropriate vertebral sections obtained by the Spinal Mouse.Anthropometric Measurements Four anthropometric variables (chronological age, stature, sitting height, and body mass) were measured along the guidelines recommended by the Saskatchewan Childhood Growth and Development research group (written personal communication, Prof Mirwald) and were used in sex-specific regression equations to predict age from peak height velocity (PHV), a maturity offset. By using this method, age from PHV maturity offset can be estimated within an error of ± 1 year 95% of the time. [50]
Questionnaire on Spinal Complaints Participants completed a survey for the assessment of low back pain (LBP). [51] LBP was defi ned as follows: A discomfort or pain in the back that is considered to be a local, uncomfortable feeling in the lumbar or lumbosacral part of the back, with the possibility of radiation to other parts of the body. Problems due to fatigue related to a single exercise are not considered as back problems.
The discomfort or pain can be intermittent or constant, gradually developed or with a sudden onset. Back pain due to menstruation is not taken into account. The defi nition as such was not presented to the adolescents, but it was orally “translated” in a language that could be understood by the adolescents. This was done during the instructions before completion. During completion, an examiner blinded to the results of spinal measurements was present to provide assistance if needed. The questions relevant to this study included the following: “Have you ever had LBP?” “Has your low back been painful in the last 4 weeks?” “Have you ever visited a doctor for low back complaints?” (“yes” or “no”). Analogue questions on lifetime prevalence, 1–month prevalence, and concomitant doctor visitation were inquired regarding neck pain (NP) and thoracic spine pain (TSP).Statistical Analysis
The data were analyzed using PASW Statistics version 18.0 (SPSS Inc., Chicago, IL). Analyses were conducted in 3 steps and were performed separately for boys and girls.
First, intertrial reliability of measures obtained by Spinal Mouse (thoracic kyphosis, lumbar lordosis, and sacral inclination) and digital inclinometer (pelvic tilt) was evaluated using intraclass correlation coeffi cient (ICC [2,1]) for absolute agreement [52] and standard error of measurements (SEM). [53] The minimum difference (MD) to be considered “real” was also calculated (MD = SEM × 1.96 × √2). [54] Second, standard descriptive statistical analyses were performed on sagittal postural characteristics and spinal pain variables; independent samples t test was performed, with sex as a grouping variable. Third and finally, the relationship between postural measures and spinal pain variables was analyzed with logistic regression. In logistic regression, univariate analysis was first performed and combined with the indications of previously published studies to identify the postural covariates for multivariate analyses regardless of the P values. Variables were used in binary logistic regression with forward likelihood ratio test to screen the variables and to identify associated factors. All P values were 2–sided, and P < 0.05 was considered significant.
RESULTS
Description of the Study Sample
The response rate was 82.4% for boys and 85.6% for girls. Samples were representative for youth in Flanders regarding educational networks and levels. Predicted years from PHV, a maturational benchmark, were 1.2 ± 0.71 and 1.2 ± 0.59 years pre-PHV in boys and girls, respectively. A total of 93.6% of the boys and 96.2% of the girls were classifi ed as pre-PHV. The average predicted age of boys and girls at PHV was 13.8 ± 0.53 and 11.8 ± 0.44 years, respectively.
Reliability of the Field Measurements

Table 1

Table 2A

Table 2b Reliability for measures obtained by Spinal Mouse and digital inclinometer is presented in Table 1. In general, 5 of 8 ICC values were in the excellent range (ICC ≥ 0.75). The other 3 ICC values were in the higher portion of the good range (0.5 < ICC < 0.75). 52 The SEM (% of mean) ranged from 3.66% to 8.31%.
Sagittal Standing Alignment
Table 2 provides descriptive data on the variation in the sagittal standing alignment in young adolescents. As can be seen, significant variations were present in parameters describing global and spinopelvic postural alignment. Regarding the lumbopelvic characteristics, for instance, the average values for the degree of lumbar lordosis were 28.9° in boys and 30.7° in girls, with a range of 7.7° to 48.7° and 10.0° to 55.7° , respectively. The number of vertebrae in lordosis was, on average, approaching 5, with a range from 1.5 to 8.5 both in boys and in girls, implying the inflection point where the spine transitioned from kyphosis to lordosis was, on average, somewhat below the T12 level, near the anatomic location of the thoracolumbar junction. However, this transition was noted to occur as proximally as the T8–T9 interspace and as distally as the L3–L4 interspace. The apex of lumbar lordosis was located, on average, just above the L3 level, with a range from the T12–L1 interspace (boys) and T12 level (girls) proximally to the L5 level distally. Pelvic tilt averaged 12.3° (boys) and 13.2° (girls), with a range from –1.6° to 25.5° and –1.5° to 26.0° , respectively. The sacral inclination angle , defined as the angle between the dorsum of the sacrum and the vertical axis as measured externally, averaged 17.7° forward inclination in boys and 19.7° in girls, with a range from 4.7° (boys) or 2.3° (girls) backward inclination to 35.7° (boys) or 40.3° (girls) forward inclination. The height of the iliac crests was located near the L3 level, on average. This measure of pelvic morphology, however, was noted to occur as proximally as the L1 level and as distally as the L5 level.
The results of the independent samples t test showed significant sex differences for all mean pre-PHV postural parameters except for the craniovertebral angle, indicating a similar forward incline of the neck-head segment relative to the horizontal in both sexes. Boys were found to have a significantly bigger pelvic displacement angle ( i.e. , more forward translation of the pelvis over the base of support as measured at the ankle) ( P = 0.017), a smaller trunk lean angle (i.e. , less posterior tilt of the trunk with respect to the vertical) (P = 0.003), and a smaller body lean angle ( i.e. , more anterior body lean) (P < 0.001) than girls. Regarding lumbopelvic features, the mean overall lumbar lordosis was smaller in boys than in girls (P < 0.001), boys had less vertebrae included in lordotic curve (P = 0.002), their lumbar apex and iliac crests were situated at a lower vertebral level (both P < 0.001), and less anterior pelvic tilt and less forward inclination of the sacrum (both P < 0.001) were noted. Furthermore, the mean overall thoracic kyphosis was more pronounced in boys than in girls (P < 0.001), with boys having more vertebral units included in the kyphotic curve (P = 0.002) and a thoracic apex being at a lower vertebral level (P < 0.001) than girls.
Spinal Pain Prevalence and Doctor Visit Rates for Spinal Pain
In boys, the lifetime prevalence of LBP was 28.5%. A total of 13.8% of boys reported LBP in the month preceding completion of the questionnaire, whereas 3.3% had ever consulted a doctor because of LBP. In girls, prevalence on LBP parameters amounted to 24.0%, 9.6%, and 5.4% for lifetime prevalence, 1–month prevalence, and doctor visit, respectively.
With regard to NP, lifetime and 1–month prevalence were 25.0% and 8.9%, respectively, in boys. About 3.3% of all boys visited a doctor because of NP. In girls, 30.2% and 10.1% complained of NP ever and in the past month, respectively, and 3.4% of girls had ever visited a doctor for their NP.
Among the boys, 10.5% mentioned to have ever experienced TSP, whereas the 1–month prevalence accounted 5.0%. A total of 1.7% of boys had ever visited a doctor for their TSP. In girls, these prevalence rates for TSP variables were 11.7%, 4.9%, and 2.9%, respectively.
Associations Between Sagittal Postural Parameters and Spinal Pain MeasuresLBP Measures The dependent variables were lifetime prevalence LBP, 1–month prevalence LBP, and doctor visit because of LBP, successively. The candidate covariates included the 4 global sagittal alignment parameters and the 6 lumbopelvic variables. All these were continuous variables.
In boys, among the 10 postural parameters screened by multivariate analysis, pelvic displacement angle (odds ratio [OR] = 1.074; 95% confidence interval [CI]: 1.008–1.144; P = 0.027) remained in the model using binary logistic regression, with forward likelihood ratio test regarding lifetime prevalence of LBP. An increase in 1° pelvic displacement has a 7.4% increase in odds of ever having experienced LBP Results of multivariate logistic regression, however, yielded this parameter to account for only 1.1% of the variability in lifetime prevalence of LBP in boys (Nagelkerke R 2 = 0.011). Regarding 1–month prevalence and doctor visit for LBP none of the postural variables remained in the model. In girls, none of the variables remained in the model for none of the LBP measures.
NP Measures The candidate covariates for the dependent variable (lifetime prevalence, 1–month prevalence, and doctor visit for NP, successively) included the 4 global sagittal alignment parameters. In boys, 2 variables stayed in the model when considering lifetime prevalence of NP: the craniovertebral angle (OR = 0.954; 95% CI: 0.924–0.985; P = 0.004) and the trunk lean angle (OR = 1.077; 95% CI: 1.007–1.152; P = 0.031). Less anteroposition of the head was associated with an approximately 5% decrease in odds of lifetime prevalence of NP, whereas an increase in posterior trunk tilt was associated with significantly higher lifetime odds of NP.
Results of multivariate logistic regression yielded the model to account for 3.2% of the variability in lifetime prevalence of NP in boys (Nagelkerke R 2 = 0.032). Regarding NP month prevalence in boys, the only variable to stay was the trunk lean angle (OR = 1.233; 95% CI: 1.110–1.369; P < 0.001). Here, an increase in 1° trunk lean angle had a 23.3% increase in odds of having experienced NP in the past 4 weeks in target boys, explaining 5.8% of the variability in NP outcome (Nagelkerke R 2 = 0.058). None of the variables was significantly related to doctor visit rate for NP.
In girls, the craniovertebral angle stayed in the model when considering lifetime prevalence of doctor visit for NP (OR = 0.905; 95% CI: 0.824–0.994; P = 0.037). A 1° increase in craniovertebral angle (i.e. , less forward held head) has a 9.5% decrease in odds of having sought medical help for NP. Analyses yielded this parameter to account for 3.5% of the variability in doctor visit rate for NP (Nagelkerke R 2 = 0.035). No associations were found between posture and the other NP parameters.
TSP Measures The candidate covariates for the dependent variable (lifetime prevalence, 1–month prevalence, and doctor visit for TSP, successively) included the 4 global sagittal alignment parameters and the 3 thoracic parameters. The only significant association between posture and TSP measures was found with respect to doctor visit for TSP in boys, with the trunk lean angle staying in the model (OR = 1.290; 95% CI: 1.041–1.598; P = 0.020): an increase in 1° in trunk lean (i.e. , more backward reclination of the trunk) has a 29.0% increase in odds of having visited a doctor for TSP, with this parameter explaining 5.3% of the variability in doctor visit rate for TSP.
DISCUSSION
This study yields physiological standards for several indicators of alignment, both global and spinopelvic, measured in a representative cohort of young adolescents in Flanders (Belgium), using a screening protocol with clinical applicability. A key aspect of the study design was the recruitment of subjects according to a common maturational landmark, the age of attainment of peak height velocity (PHV), yielding a developmental age baseline as opposed to a chronological baseline. To the best of the authors’ knowledge, no epidemiological studies have been reported on sagittal full-body posture — including global and local postural characteristics — in the growing individual, factoring in maturity status. As shown in previous research, [50] age from PHV can be predicted with a reasonable degree of accuracy from a 1–time measurement of basic anthropometric variables, using sex-specific multiple regression equations taking into consideration the differential timing of the adolescent spurt in body dimensions and their interactions with chronological age. Predicted age at PHV within our sample (13.8 years among boys and 11.8 years among girls) was similar to previous reported values from North American and European populations. [46]
The pre-PHV baseline data of this study demonstrate the sagittal body profi le to be highly variable already in a standardized standing position, in young adolescence. For example, in our cohort, the vertebral level where the spine transitions from kyphosis to lordosis was, on average, somewhat below the T12 level, near the anatomic location of the thoracolumbar junction. This transition was noted to occur as proximally as the T8–T9 interspace and as distally as the L3–L4 interspace, implying that the number of kyphotic and lordotic vertebral units can vary significantly. A comparable wide variation in the length of the spinal kyphotic and lordotic segments has been noted in a normal, young adult population [6, 8 ,55] but has not yet been reported within a pre-PHV pediatric population. Accordingly, in this study, thoracic and lumbar curvatures of the spine were defi ned independent of the anatomic location of the thoracolumbar junction at T12–L1, allowing for a better evaluation of the full magnitude of the sagittal curves of the spine.
In this study, the standing human body posture was represented by a series of 3 solid links representing 3 major body segments (lower limbs, trunk, and head) and several local shape indices within the spinopelvic axis. The postural parameters we have proposed (i.e. , 4 “global” alignment parameters: pelvic displacement, trunk lean, body lean, and craniovertebral angle, and 9 “local” spinopelvic features: total degrees of lumbar lordosis and thoracic kyphosis, the number of vertebras in lordosis and kyphosis, the vertebral level of the lumbar and thoracic apices, pelvic tilt, sacral inclination, and pelvic height) were based on a critical literature review and clinical insights and were intended to identify certain morphologic features that may have an association with the pathogenesis of spinal pain. According to our fi ndings, none of the included “local” spinopelvic parameters could be identifi ed as an associated factor with any measure of spinal pain (i.e. , lifetime and 1–month prevalence of LBP, NP, or TSP, and concomitant doctor visit rates). Instead, results suggest global alignment parameters to be associated with LBP (lifetime prevalence), NP (lifetime prevalence, 1–month prevalence, and doctor visit for NP), and TSP measures (visiting a doctor for TSP). Therefore, it can be suggested that the orientation of various body segments with respect to the gravity plumb line ( i.e. , anteroposterior translations of the head, trunk, and pelvis) may be paramount compared with the local spinopelvic characteristics with respect to the development of symptomatic IASP and concomitant medical care seeking, at least in pre-PHV boys and girls. The associations between posture parameters and spinal pain measures found in this cross-sectional data set; however, it cannot be said to be causal, because spinal pain itself may alter posture.
On the basis of the current data set, it is diffi cult to determine whether the statistical sex differences for all postural parameters, except for the craniovertebral angle, are also of clinical relevance. The patterns of sexual dimorphism seem to be in line with previous reports. [3, 17, 21, 26, 56] Nonetheless, caution is required in comparing study results, given the particular profi le of this study sample with regard to biological/ chronological age. In any case, the fi nding that the association pattern between sagittal posture and spinal pain seems strongly sex-specific in boys and girls within the same phase of growth was somewhat surprising. In girls, only one association was found between a spinal pain–related outcome variable (having sought medical help for NP) and the candidate postural predictors (forward held head). In boys, on the contrary, associations were found with regard to higher odds of lifetime prevalence LBP (forward translation of the pelvis over the base of support, as measured at the ankle), lifetime prevalence NP (anteroposition of the head and backward reclination of the trunk with respect to the vertical), 1–month prevalence NP (backward reclination trunk), and doctor visit because of TSP (backward reclination trunk). The reason for this discrepancy between sexes is unclear, yet possible mechanisms might include the difference in chronological age between boys and girls or, purely hypothetical, sex-related differences in the domination of contributing factors within the widely accepted multifactorial nature of the risk for children’s and adolescents’ experience of spinal pain symptoms. [57–61] Interestingly, in a recent study conducted in 766 adolescents aged 13.0 to 15.1 years not controlling for maturity status, there was also some suggestion that sex may infl uence the association between postural types and back pain measures. [62]
We think that part of the reason for the limited and conflicting evidence linking spinal pain to posture may be that emphasis in research on habitual posture has been predominantly on “local” postural characteristics whereas studies on the overall postural presentation are rather sparse. Within this context, arm position should be considered attentively to obtain postural data that are representative for the alignment in the relaxed standing position. Furthermore, sex and somatic maturity have rarely been taken into consideration.
A potential limitation of this study is the use of postural measures external to the body: global posture was assessed by post hoc analysis of digital images, and local parameters were assessed using direct body measurements (palpation, digital inclinometry, and Spinal Mouse). The assessment protocol used can be substantiated by its applicability in both large-scale population studies and evidence-based practice. [26, 47–49, 62, 63] The use of palpation in general, [64] and the determination of the vertebral levels of thoracic and lumbar apices and the transition between kyphosis and lordosis via visual evaluation and palpation in particular, may come under criticism, [65–67] the more so because a “level of ambiguity” [68] may occur when 2 or more vertebrae have a similar orientation. However, palpation and marker placement on the entire study sample were performed by 1 single researcher with clinical experience who used judgment and experience to select the limit vertebras.
Another potential limitation is that the vertebral level where the cervical lordosis transitions into a thoracic kyphosis was not noted. Instead, the anatomic location of the cervicothoracic transition was used in all subjects. The authors of this study are aware that interindividual variations in transition from the cervical to thoracic curves may exist, yet the implementation of a variable cervicothoracic transition would have interfered with the use of the Spinal Mouse, as this device applies a recursive algorithm on the data obtained between a fixed starting and end point (C7 spinous process and top of anal crease, respectively).
A third and last potential limitation is that the postural measures account only for small percentages of the variability in spinal pain outcome measures despite significant associations are shown. We speculate that there may be opportunities for postural subgrouping strategies to begin with global alignment parameters, as it may be that it is the interaction between segments that is of importance. We have completed this study to establish an initial pre-PHV cross-sectional data set describing sagittal alignment and its association with spinal pain measures in healthy, young adolescents. An attempt will be made to prospectively follow these subjects in a longitudinal fashion. significant work is now directed at developing a classification system of habitual standing posture in the sagittal plane.
Key Points
Although the potential infl uence of puberty-directed mechanisms on both posture and IASP seems well recognized, maturity status has rarely been applied in research on aforementioned issues or their interrelation.
Using a screening protocol with clinical applicability, this study yields physiological standards for several indicators of both “global” alignment and “local” spinopelvic features, measured in a representative cohort of adolescents in Flanders (Belgium) before age of attainment of PHV, a maturation benchmark.
This pre-PHV baseline data set demonstrates a wide interindividual variation in sagittal body profi le in stance.
Results suggest the orientation of gross body segments to the gravity line to be superior in terms of clinical importance; the association patterns, however, seem strongly sex-specific.
There may be opportunities for postural subgrouping strategies to begin with global alignment parameters to gain further insight in the relationship between sagittal alignment and the relative risk of developing spinal pain/seeking medical consultation for this pain.
Acknowledgments
The authors are grateful to Gizem Irem Güvendik and Tom Barbe for the generous assistance with data collection and to all of the school teams, local pupil guidance centers, and participants for their cooperation in this study.
References:
Christensen ST , Hartvigsen J.
Spinal curves and health: a systematic critical review of the epidemiological literature
dealing with associations between sagittal spinal curves and health.
J Manipulative Physiol Ther 2008 ; 31 : 690–714.Lederman E.
The fall of the postural-structural-biomechanical model in manual and physical therapies:
exemplified by lower back pain.
J Bodyw Mov Ther 2011 ; 15 : 131–8.Vialle R , Levassor N , Rillardon L , et al.
Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects.
J Bone Joint Surg Am 2005 ; 87 : 260–7.Legaye J , Duval-Beaupere G.
Gravitational forces and sagittal shape of the spine. Clinical estimations of their relations.
Int Orthop 2008 ; 32 : 809–16.Poussa MS , Heliövaara MM , Seitsamo JT , et al.
Development of spinal posture in a cohort of children from the age of 11 to 22 years.
Eur Spine J 2005 ; 14 : 738–42.Mac-Thiong JM , Labelle H , Berthonnaud E , et al.
Sagittal spinopelvic balance in normal children and adolescents.
Eur Spine J 2007 ; 16 : 227–34.Nissinen M.
Spinal posture during pubertal growth.
Acta Paediatr 1995 ; 84 : 308–12.Roussouly P , Gollogly S , Berthonnaud E , et al.
Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis
in the standing position.
Spine 2005 ; 30 : 346–53.Keller TS , Colloca CJ , Harrison DE , et al.
Influence of spine morphology on intervertebral disc loads and stresses in asymptomatic adults:
implications for the ideal spine.
Spine 2005 ; 5 : 297–309.Gelb DE , Lenke LG , Bridwell KH , et al.
An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers.
Spine 1995 ; 20 : 1351–8.Jackson RP , McManus AC.
Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low
back pain matched for age, sex, and size. A prospective controlled clinical study.
Spine 1994 ; 19 : 1611–8.Kumar MN , Baklanov A , Chopin D.
Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion.
Eur Spine J 2001 ; 10 : 314–9.Mac-Thiong JM , Wang Z , de Guise JA , et al.
Postural model of sagittal spino-pelvic alignment and its relevance for lumbosacral developmental spondylolisthesis.
Spine 2008 ; 33 : 2316–25.Cil A , Yazici M , Uzumcugil A , et al.
The evolution of sagittal segmental alignment of the spine during childhood.
Spine 2005 ; 30 : 93–100.Mac-Thiong JM , Berthonnaud E , Dimar JR II , et al.
Sagittal alignment of the spine and pelvis during growth.
Spine 2004 ; 29 : 1642–7.Kuo YL , Tully EA , Galea MP.
Video analysis of sagittal spinal posture in healthy young and older adults.
J Manipulative Physiol Ther 2009 ; 32 : 210–5.Lafond D , Descarreaux M , Normand MC , et al.
Postural development in school children: a cross-sectional study.
Chiropr Osteopat 2007 ; 15 : 1.Schwab F , Lafage V , Boyce R , et al.
Gravity line analysis in adult volunteers: age-related correlation with spinal parameters,
pelvic parameters, and foot position.
Spine 2006 ; 31 : E959–67.Massion J.
Postural control systems in developmental perspective.
Neurosci Biobehav Rev 1998 ; 22 : 465–72.Lafage V , Schwab F , Skalli W , et al.
Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters.
Spine 2008 ; 33 : 1572–8.Janssen MM , Drevelle X , Humbert L , et al.
Differences in male and female spino-pelvic alignment in asymptomatic young adults:
a three-dimensional analysis using upright low-dose digital biplanar x-rays.
Spine 2009 ; 34 : E826–32.Van Niekerk SM , Louw Q , Vaughan C , et al.
Photographic measurement of upper-body sitting posture of high school students:
a reliability and validity study.
BMC Musculoskelet Disord 2008 ; 9 : 113–23.Harrison DE , Janik TJ , Cailliet R , et al.
Upright static pelvic posture as rotations and translations in 3-dimensional from three 2-dimensional
digital images: validation of a computerized analysis.
J Manipulative Physiol Ther 2008 ; 31 : 137–45.Lafage V , Schwab F , Patel A , et al.
Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults
with spinal deformity.
Spine 2009 ; 34 : E599–606.Mac-Thiong JM , Roussouly P , Berthonnaud E , et al.
Sagittal parameters of global spinal balance: normative values from a prospective cohort of seven hundred
nine Caucasian asymptomatic adults.
Spine 2010 ; 35 : E1193–8.McEvoy MP , Grimmer K.
Reliability of upright posture measurements in primary school children.
BMC Musculoskelet Disord 2005 ; 6 : 35.Vialle R , Ilharreborde B , Dauzac C , et al.
Is there a sagittal imbalance of the spine in isthmic spondylolisthesis? A correlation study.
Eur Spine J 2007 ; 16 : 1641–9.Jackson RP , Hales C.
Congruent spinopelvic alignment on standing lateral radiographs of adult volunteers.
Spine 2000 ; 25 : 2808–15.Troyanovich SJ , Cailliet R , Janik TJ , et al.
Radiographic mensuration characteristics of the sagittal lumbar spine from a normal population with
a method to synthesize prior studies of lordosis.
J Spinal Disord 1997 ; 10 : 380–6.Vedantam R , Lenke LG , Keeney JA , et al.
Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults.
Spine 1998 ; 23 : 211–5.Marks M , Stanford C , Newton P.
Which lateral radiographic positioning technique provides the most reliable and functional representation
of a patient’s sagittal balance ?
Spine 2009 ; 34 : 949–54.McGregor AH , Hukins DW.
Lower limb involvement in spinal function and low back pain.
J Back Musculoskelet Rehabil 2009 ; 22 : 219–22.Jeffries LJ , Milanese SF , Grimmer-Somers KA.
Epidemiology of adolescent spinal pain: a systematic review of the research literature.
Spine 2007 ; 32 : 2630–7.Patton GC , Viner R.
Pubertal transitions in health.
Lancet 2007 ; 369 : 1130–9.Friedland O , Hashkes PJ , Jaber L , et al.
Decreased bone speed of sound in children with growing pains measured by quantitative ultrasound.
J Rheumatol 2005 ; 32 : 1354–7.Balagué F , Dudler J , Nordin M.
Low-back pain in children.
Lancet 2003 ; 361 : 1403–4.Wedderkopp N , Andersen LB , Froberg K , et al.
Back pain reporting in young girls appears to be puberty-related.
BMC Musculoskelet Disord 2005 ; 6 : 52.LeResche L , Mancl LA , Dransholt MT , et al.
Relationship of pain and symptoms to pubertal development in adolescents.
Pain 2005 ; 118 : 201–9.Duggleby T , Kumar S.
Epidemiology of juvenile low back pain: a review.
Disabil Rehabil 1997 ; 19 : 505–12.Rhee H.
Relationships between physical symptoms and pubertal development.
J Pediatr Health Care 2005 ; 19 : 95–103.Feldman DE , Shrier I , Rossignol M , et al.
Risk factors for the development of low back pain in adolescence.
Am J Epidemiol 2001 ; 154 : 30–6.Dickson RA.
Aetiology of idiopathic spinal deformities.
Arch Dis Child 1985 ; 60 : 508–11.Grivas TB , Vasiliadis ES , Koufopoulos G , et al.
Study of trunk asymmetry in normal children and adolescents.
Scoliosis 2006 ; 1 : 19.Loncar-Dusek M , Pec´ina M , Prebeg Z.
A longitudinal study of growth velocity and development of secondary gender characteristics versus onset
of idiopathic scoliosis.
Clin Orthop Relat Res 1991 ; 270 : 278–82.Tsirikos AI.
Scheuermann’s kyphosis: an update.
J Surg Orthop Adv 2009 ; 18 : 122–8.Malina RM , Bouchard C , Bar-Or O.
Growth, Maturation, and Physical Activity. 2nd ed.
Champaign, IL : Human Kinetics ; 2004.Mannion AF , Knecht K , Balaban G , et al.
A new skin-surface device for measuring the curvature and global and segmental ranges of motion of the spine:
reliability of measurements and comparison with data reviewed from the literature.
Eur Spine J 2004 ; 13 : 122–36.Kellis E , Adamou G , Tzilios G , et al.
Reliability of spinal range of motion in healthy boys using a skin-surface device.
J Manipulative Physiol Ther 2008 ; 31 : 570–6.Kiss RM.
Verification of determining the curvatures and range of motion of the spine by
electromechanical-based skin-surface device.
Period Polytech-Civ 2008 ; 52 : 3–13.Mirwald RL , Baxter-Jones AD , Bailey DA , et al.
An assessment of maturity from anthropometric measurements.
Med Sci Sports Exerc 2002 ; 34 : 689–94.Staes F , Stappaerts K , Vertommen H , et al.
Reproducibility of a survey questionnaire for the investigation of low back problems in adolescents.
Acta Paediatr 1999 ; 88 : 1269–73.Shrout PE , Fleiss JL.
Intraclass correlations: uses in assessing rater reliability.
Psychol Bull 1979 ; 86 : 420–8.Weir JP.
Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM.
J Strength Cond Res 2005 ; 19 : 231–40.Charter RA.
Revisiting the standard errors of measurement, estimate, and prediction and their application to test scores.
Percept Mot Skills 1996 ; 82 : 1139–44.Vaz G , Roussouly P , Berthonnaud E , et al.
Sagittal morphology and equilibrium of pelvis and spine.
Eur Spine J 2002 ; 11 : 80–7.Whitcome KK , Shapiro LJ , Lieberman DE.
Fetal load and the evolution of lumbar lordosis in bipedal hominins.
Nature 2007 ; 450 : 1075–8.Kovacs FM , Gestoso M , Gil del Real MT , et al.
Risk factors for non-specifi c low back pain in schoolchildren and their parents: a population based study.
Pain 2003 ; 103 : 259–68.Szpalski M , Gunzburg R , Balagué F , et al.
A 2-year prospective longitudinal study on low back pain in primary school children.
Eur Spine J 2002 ; 11 : 459–64.Watson KD , Papageorgiou AC , Jones GT , et al.
Low back pain in schoolchildren: the role of mechanical and psychosocial factors.
Arch Dis Child 2003 ; 88 : 12–7.Siivola SM , Levoska S , Latvala K , et al.
Predictive factors for neck and shoulder pain: a longitudinal study in young adults.
Spine 2004 ; 29 : 1662–9.Briggs AM , Bragge P , Smith AJ , et al.
Prevalence and associated factors for thoracic spine pain in the adult working population: a literature review.
J Occup Health 2009 ; 51 : 177–92.Smith A , O’Sullivan P , Strakeer L.
Classification of sagittal thoraco-lumbo-pelvic alignment of the adolescent spine in standing
and its relationship to low back pain.
Spine 2008 ; 33 : 2101–7.Fortin C , Feldman DE , Cheriet F , et al.
Clinical methods for quantifying body segment posture: a literature review.
Disabil Rehabil 2011 ; 33 : 367–83.Moriguchi CS , Carnaz L , Silva LC , et al.
Reliability of intra- and inter-rater palpation discrepancy and estimation of its joint angle measurements.
Man Ther 2009 ; 14 : 299–305.Shin S , Yoon DM , Yoon KB.
Identification of the correct cervical level by palpation of the spinous processes.
Anesth Analg 2011 ; 112 : 1232–5.Snider KT , Kribs JW , Snider EJ , et al.
Reliability of Tuffi er’s line as an anatomic landmark.
Spine 2008 ; 33 : E161–5.Teoh DA , Santosham KL , Lydell CC , et al.
Surface anatomy as a guide to vertebral level for thoracic epidural placement.
Anesth Analg 2009 ; 108 : 1705–7.Potter BK , Rosner MK , Lehman RA Jr , et al.
Reliability of end, neutral, and stable vertebrae identification in adolescent idiopathic scoliosis.
Spine 2005 ; 30 : 1658–63.
Return to SPINAL ALLIGNMENT
Since 12-28-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |