

The Role of Forward Head Correction in Management
of Adolescent Idiopathic Scoliotic Patients:
A Randomized Controlled TrialThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Clin Rehabil. 2012 (Dec); 26 (12): 1123–1132 ~ FULL TEXT
Aliaa A Diab
Basic Science Department,
Cairo University,
Egypt.
Ola_1174@hotmail.comOBJECTIVE: To investigate the effectiveness of forward head correction on three-dimensional posture parameters and functional level in adolescent idiopathic scoliotic patients.
DESIGN: A randomized controlled study with three-month follow-up.
SETTING: University research laboratory.
SUBJECTS: Seventy-six adolescent idiopathic scoliotic patients with Cobb angle ranged from 10° to 30° and craniovertebral angle less than 50° were randomly assigned to a study or a control group.
INTERVENTIONS: All the patients (n = 76) received traditional treatment in the form of stretching and strengthening exercises. In addition, patients in the study group (n = 38) received a forward head posture corrective exercise programme.
OUTCOME MEASURES: Craniovertebral angle, Functional Rating Index and posture parameters, including: lumbar lordosis, thoracic kyphosis, trunk inclination, trunk imbalance, lateral deviation, surface rotation and pelvis torsion were measured before treatment, after 10 weeks, and at three-month follow-up.
RESULTS: There was a significant difference between the study and control groups adjusted to baseline values at 10 weeks post treatment with respect to the following parameters: craniovertebral angle (P = 0.006), trunk inclination (P = 0.005), lordosis (P = 0.01), kyphosis (P = 0.001), trunk imbalance (P = 0.001), lateral deviation (P = 0.001), pelvic torsion (P = 0.004) and surface rotation (P = 0.013). At three-month follow-up, there were still significant differences in all the previous variables (P < 0.005). In contrast, while there was no significant difference with respect to Functional Rating Index at 10 weeks (P = 0.8), the three-month follow-up showed a significant difference (P = 0.001).
CONCLUSION: A forward head corrective exercise programme combined with conventional rehabilitation improved three-dimensional scoliotic posture and functional status in patients with adolescent idiopathic scoliosis.
Keywords Exercise, posture, scoliosis, randomized controlled trial
From the Full-Text Article:
Introduction
Adolescent idiopathic scoliosis is a life-long condition, probably systemic, of unknown cause. Although it is common to speak of scoliosis in terms of spinal curvature in the coronal plane, it is actually a threedimensional problem comprising torsion, angulation and translation occurring simultaneously in the transverse, coronal and sagittal planes. [1] A recent review by Everett and Patel found that management of scoliosis is closely dependent on the ability to promote symmetry of the global spine, thus removing asymmetrical gravitational loading. [2]
Through the years, many studies have supported that many of our postural reflexes, such as the vestibulocollic reflex, [3] cervicocollic reflex, [4] pelvoocular reflex, [5] vestibulo-ocular reflex, [6] cervico-ocular reflex and cervical somatosensory input, [7–9] are housed, or occur, within the head and neck region. A correction of altered head posture therefore, could be imperative to achieve optimal full spine postural correction, where the rest of the spine orients itself in a top-down fashion. [10]
Although the forward head posture is one of the most prevalent conditions in western society, [11] occurring more frequently in patients with scoliosis than in a normal population, [12–14] one component that is universally lacking in nearly all forms of scoliosis treatment today is the effect of the head posture in determining overall spinal posture.
To date, no randomized controlled trials have been published to address the issue of correction of forward head posture and its impact on overall spinal posture. Only a few correlational studies have been conducted. [15–17] Despite the importance of these studies, they were limited to certain body regions. Moreover, the results of these studies mostly only elucidated an open linear chain linking the head to the pelvis in the sagittal plane only.
Accordingly, the main purpose of this study was to investigate the effect of forward head posture correction on spinal posture parameters occurring in the transverse, coronal and sagittal planes in adolescent idiopathic scoliosis as well as on functional status which considered a more accurate reflection of patient clinical state and progress than many objective clinical or physiological indexes measures upon which we have traditionally relied. [18]
Methods
A prospective, randomized, controlled study was conducted in the research laboratory of my university. All the patients were conveniently selected from my institution’s outpatient clinic. They participated in the study after signing an informed consent form prior to data collection. Recruitment began after approval was obtained from local institutional review board. Patients were recruited from April 2010 to February 2011 with three-month follow-up.
Participants were screened prior to inclusion by measuring craniovertebral angle. If the angle was less than 50°, then a participant was referred to the study. All the patients underwent careful clinical and radiologic examinations to confirm a diagnosis of adolescent idiopathic scoliosis. Patients were included if they had mild to moderate scoliotic curve (Cobb angle 10–30°, [19] Risser grade 0, 1 or 2 to ensure skeletally immaturity). They also were included if they were under the category of ‘1A–’ according to the new classification method of Lenks et al., [20] which emphasizes consideration of sagittal and coronal alignment. In this classification, type 1 identified patients with main thoracic curves, modifier A is used when the centre sacral vertical line runs between the lumbar pedicles to the level of the stable vertebra, and the minus (–) sign identifies a sagittal thoracic curve of less than +10°. Exclusion criteria included true leg length discrepancy, previous spinal surgery and associated pathologies of lower limbs that may interfere with global spinal posture, such as foot, knee and hip deformities.
Patients were randomly assigned into two groups by an independent person who picked one of the sealed envelopes, which contained numbers chosen by random number generator. Randomization was restricted to permuted blocks of different size to ensure that equal numbers were allocated to each group. Each random permuted block was transferred to a sequence of consecutively numbered, sealed, opaque envelopes and these were stored in a locked drawer until required. As each participant formally entered the trial, the researcher opened the next envelope in the sequence in the presence of the patient.
Patients in both the study (n = 38) and the control group (n = 38) received the same traditional treatment. This included stretching the tight structures on the concave side of the spine, erector spine muscles and tight hamstring muscle. These exercises would be conducted in conjunction with strengthening the trunk muscles necessary for postural control and trunk stability; abdominal, thoracic and lumbar extensors and trunk musculatures on the convex side of the curve. This conventional treatment was to be repeated 3 times a week for 10 weeks. Those in the control group received this conventional treatment only.
The exercise group also received a corrective exercise programme for forward head posture in the form of two strengthening (deep cervical flexors and shoulder retractors) and two stretching (cervical extensors and pectoral muscles). The exercise programme was carried out according to the protocol devised by Harman et al.: [21]
Strengthening deep cervical flexors: From supine lying position the patient was instructed to tuck his or her chin in and keep the head straight, without turning to either side. The progression of this exercise was to lift the head off the floor in tucked position and hold it for varying lengths of time (2–second holds starting at 2 seconds, i.e. 2, 4, 6 and 8 seconds).
Stretching cervical extensors through a chin drop in sitting: The progression of this exercise was to drop the chin with hand assistance.
Strengthen shoulder retractors: The exercise was first performed from standing position using a theraband pulling the shoulders back. The patient was asked to pinch the scapulae together without elevation or extension in the shoulders and to hold this position for at least 6 seconds then relax. The first progression was to conduct the shoulder retraction from prone using weights. The second progression was through using elastic resistance and weights. Participants performed each progression for two weeks. At consultation, if they could complete three sets of 12 repetitions correctly for the strengthening, they were progressed to the second progression.
Unilateral and bilateral pectoralis stretches alternating each two-week period: For bilateral pectoralis stretching, the patient was seated on a treatment table or mat with the hands behind the head. The therapist kneeled behind the patient, grasping the patient’s elbows and gently pushing them back. No forceful stretch is needed against the elbows, because the ribcage is elongating the proximal attachment of the pectoralis major muscles bilaterally. For unilateral stretching, the arm on the involved site was moved into abduction and external rotation. To stretch the costal division, the ram should be elevated to approximately 135°. For sternal division, the arm is abducted to 90°. For clavicular division, the arm is rested at the side. Participants completed three sets of 12 repetitions of the strengthening exercises and three stretching exercises held for 30 seconds each. This exercise programme was to be repeated 4 times per week for 10 weeks. Patients in both groups were instructed to avoid any other exercise programmes that may interfere with the results.
The main outcome measurement used to assess the forward head posture was the craniovertebral angle, which is considered to be a valid and reliable assessment tool. [22] All the measurement procedures were done following the protocol of Falla et al. [23] The craniovertebral angle was measured by taking a lateral photograph. The patients were asked to sit on a chair as usual as they were and a lateral photograph was taken. A digital camera was positioned on a tripod at a distance of 0.8 m from the subject at shoulder height. Adhesive markers were fixed on the tragus of the ear and the spinous processes of the seventh cervical vertebra. The head forward angle was measured as an angle between a horizontal line passing through C7 and a line extending from the tragus of the ear to C7.
Other outcome measures used to compare effectiveness of the treatment between the study and control groups included three-dimensional posture parameters using the Formetric II device and Functional Rating Index. Rasterstereography (Formetric II, Diers International GmbH, Schlangenbad, Germany) was used to examine posture and back shape characters. All testing procedures were carried out following Lippold’s protocol. [24] The patient was positioned in front of a black background screen 2 m from the measurement system. The column height was aligned to move the relevant parts of the patient’s back into the centre of the control monitor by using the column up/down button of the control unit. To ensure the best lateral and longitudinal position of the patient a permanent mark on the floor was used. The patient’s back (including upper buttocks) was completely bare in order to avoid disturbing image structures. The hair was tied back so that the neck (in particular the vertebral prominence) was uncovered.
When the patient and the system were correctly positioned, the system was ready for image recording. The projector lamp was automatically switched on under programme control and the exposure control was started. The best moment for releasing image capture was the (slightly) breathed out state. The patient was first asked to breathe normally. The moment of breathing out was observed on the control monitor. The patient was then asked to stop breathing for a few seconds while the image capture was released. The print-out of the Formetric system itself gives a lot of data: sagittal plane parameters (lumbar angle, thoracic angle and trunk inclination), frontal plane parameters (trunk imbalance and lateral deviation) and transversal plane parameters (vertebral surface rotation and pelvis torsion) were selected to cover the posture profile in three planes. A representative example of a Formetric system print-out is shown in Figures A1 and A2 (on-line).
The Functional Rating Index [25] was selected as it is considered to be a responsive outcome measure of spinal pain and function. It is a self-reporting instrument consisting of 10 items, each item is scored with a 5–point scale ranging from 0 (no pain or full ability to function) to 4 (worst possible pain or unable to perform a specific function at all). The 10 items fall within four constructs – pain, sleep, work, and daily activity – that fit within the three domains of WHO-ICF: (1) activity limitations daily activity with six items – personal care, travel, recreation, lifting, walking and standing; (2) impairment with three items and two constructs of pain and sleep – pain frequency, pain intensity and sleep; and (3) participation restriction with one construct and item – work. The final score ranges from 0 (representing absence of disability) to 100% (representing severe disability).
The outcome assessor, who also applied the treatment intervention programmes, was not masked during the study. To determine the number of samples in this study, estimates of mean difference and standard deviation for the primary outcome craniovertebral angle were collected from a pilot study consisting of eight patients who received the same programme between September 2009 and March 2010. The mean difference value and standard deviation were estimated as 3.07 and 3.6 respectively, a two-tailed test, an alpha level of 0.05 and desired power of 90%. These assumptions generated a sample size of 30 patients per each group. To account for some drop-out rates, the sample size was increased by 20%.
Both the mean and standard deviation were calculated for each variable. The differences in the baseline data between the study and control group were analysed using t-test for the continuous variables and chi-square test for the categorical variables. To compare the exercise group and the control group, statistical analysis was based on the intention-to-treat principle and P-values less than 0.05 were considered significant. We used multiple imputations to handle missing data. To impute the missing data we constructed multiple regression models including variables potentially related to the fact that the data were missing and also variables correlated with that outcome. We used Stata (Stata Corp, College Station, Texas, USA). Analysis of covariance (ANCOVA) at two follow-up points (after 10 weeks of treatment and at follow-up of three months) was performed for all variables, the baseline value of the outcome as covariates was used to assess between-group differences (baseline outcome in the mode = baseline value – overall mean baseline value).
Results
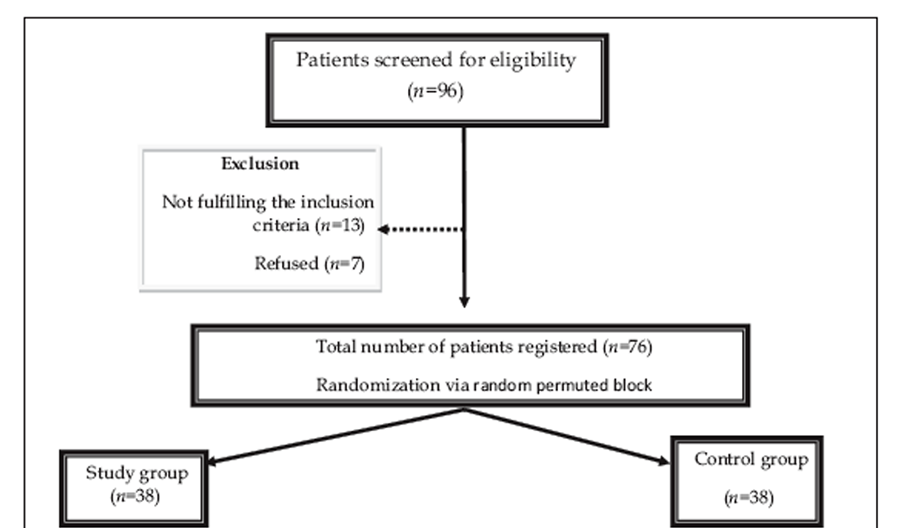
Figure 1

Table 1

Table 2 A diagram of patient retention and randomization throughout the study is shown in Figure 1. The figure shows that 96 were initially screened, after the screening process 76 patients were eligible to participate in the study and 76 completed the first follow-up, and 68 of them completed the study. Demographics of the participants are described in Table 1. The study and control groups were similar with regard to age, height, weight, gender and past use of physiotherapy. Specific measurements of the study (craniovertebral angle, functional index scale, and all the posture parameters) were also well balanced between the groups at baseline (P > 0.05 for all variables).
Results are summarized and presented as mean (SD) in Table 2. After 10 weeks of treatment, the ANCOVA revealed a significant difference between the study and control groups adjusted to baseline value of outcome for all measured variables; craniovertebral angle (F = 10.08, P = 0.006), trunk inclination (F = 10.6, P = 0.005), lordosis (F = 8.5, P = 0.01), kyphosis (F = 17.6 P = 0.001), trunk imbalance (F = 17.3, P = 0.001), lateral deviation (F = 14.2, P = 0.001), pelvic torsion (F = 11.1, P = 0.004 ), surface rotation (F = 7.3, P = 0.013). The only exception was Functional Rating Index where the F-value was 0.06 with associated probability of 0.8. At three-month follow-up, the analysis showed that there were still significant differences between the study and control groups for all the measured variables without any exception; craniovertebral angle (F = 14.9, P = 0.002), Functional Rating Index (F = 14.3, P = 0.001), trunk inclination (F = 6.6, P = 0.02), lordosis (F = 7.01, P = 0.017), kyphosis (F = 10.9, P = 0.004), trunk imbalance (F = 31.4, P = 0.000), lateral deviation (F = 13.007, P = 0.002), pelvic torsion (F = 39.7, P = 0.00), surface rotation (F = 16.6, P = 0.001).
Discussion
This study demonstrates that the group receiving a forward head correction exercise programme in addition to traditional treatment in the form of stretching exercises for tight muscles and strengthening exercises for weak muscles showed more improvement than the control group in forward head angle, three-dimensional postural parameters based on the decrease in trunk inclination, lateral deviation, trunk imbalance, thoracic kyphosis, surface rotation, and pelvic torsion and increase in craniovertebral angle and lumbar lordosis. Furthermore, after three months, these significant changes were maintained.
Functionally, it is interesting that traditional treatment alone and traditional treatment in conjunction with an intervention programme for forward head correction seem roughly equally successful in improving functional status after 10 weeks of treatment. However, the three-month follow-up revealed a significant decline in functional index for the control group. It seems logical and is generally admitted that exercise-based therapies are a logical approach to improve and maintain flexibility and function in adolescent idiopathic scoliosis patients, [26] while the transient improvement in the control group may be attributed to the continuous asymmetrical loading from biomechanical dysfunction represented in forward head posture, sagittal and coronal abnormal spinal posture that results in continuous pathological and histological changes of spinal soft tissues.
The association between normal spinal configuration and long-term health of the spine in scoliosis management was confirmed by Rhee and colleagues who noted that correction of the sagittal curves might be related to the long-term health of the spine in scoliosis management. [27] The improvement in the forward head posture recorded by the study group is similar to those reported in other studies that showed the effectiveness of exercise programmes in reducing this abnormal posture. [21, 28] This improvement may be attributed to the fact that muscle imbalance is considered to be an aetiological factor for this abnormal posture. [29]
In the current study we found that the study group which received the intervention programme for forward head correction experienced significant changes in posture parameters in the sagittal, transverse and coronal planes. These significant changes may suggest the important role of forward head correction on global spinal posture. These results are in agreement with a neurophysiological basis reported in many studies which implies that neurological regulation of static upright human posture is largely dependent on head posture. [3–9] It is apparent from the literature we searched that posture is largely maintained by reflexive, involuntary control. The reflexive components for postural control are housed, or occur, within the head and neck region primarily. Because this involuntary control is largely dependent upon cervical joint mechanoreceptors and afferent input from ligament and musculotendinous sources, [30] correcting the postural distortions responsible for the dysafferentation process may be beneficial in correcting scoliotic posture, where postural control is significantly altered.3 [31]
Forward head posture as a direct cause for dysafferentation was supported by another study which reported that the resultant lack of blood flow in response to increased strain placed upon various spinal muscles, such as the splenius capitis, trapezius, sternocleidomastoid and levator scapula, forces the muscle to rely on anaerobic metabolism. [32] As anaerobic metabolism progresses, metabolites such as substance P, bradykinin and histamine build up and excite chemosensitive pain receptors, causing a barrage of nociceptive afferent input, [33] resulting in dysafferentation. [34]
The role of the cervical spine and position of the head in postural adaptation due to undisturbed proprioception by cervical vertebra facets was confirmed by a number of authors. [35, 36] Therefore, regardless of the cause of the cervical vertebral imbalance and changes of head position (whiplash injury, cervical syndrome or adolescent idiopathic scoliosis), it will result in an inadequate postural adaptation and a problem of proprioception. Coppieters et al. [37] emphasized a correct perception of the surroundings and the role of head and eye position in order to maintain normal postural adaptation. Looking into the matter further, while there were no previous published studies that had identified an association between forward head posture correction and sagittal profile of the spine, the current results are in agreement with the findings of another study which reported that changes in sagittal profile of the spine may be attributed to a strong association between forward head and pelvo-ocular reflex, which causes an anterior pelvic translation to balance the head’s centre of gravity. [38] As reported in the literature, modifications of sagittal spinal curvature have been connected with changes in pelvic orientation. [39] Similarly, these results are in agreement with the concept of Levangie and Norkin, [40] who stated that relocation of a body segment causes a shift in the centre of mass, and thus the line of gravity shifts in relation to the base of support.
Concerning the significant changes of posture parameters in transverse and coronal planes, while there were no studies have investigated the role of forward head correction on spinal posture in transverse and coronal planes, the explanation behind these findings may be attributed to the resultant changes in the sagittal contour of the whole spine. This explanation concurred with several authors who have confirmed the association between the sagittal and coronal spinal contour. [41–43] Similarly, Kadoury et al. [44] have even been able to predict the thoracic kyphosis by evaluating the coronal thoracic curvature, the lumbar lordosis and the slope of the first lumbar vertebra. New research has discovered that a kyphotic cervical curvature (sagittal deformity) occurs more frequently in patients with severe scoliosis (coronal deformity) than in a normal population. [14] In addition, the resultant changes in sagittal contour of the whole spine may be attributed to the significant changes in transverse plane as confirmed by Veldhuizen et al. [45] who reported the positive correlation between sagittal configuration of the spine and axial rotation.
Another study which highlighted the role of the head in correction of axial rotation deformity was conducted by Parry, [46] who reported that human walking, unique among animals, involves axial pelvi-spinal rotations and axial spinal counter rotation. Body axial rotations start at the feet and are eliminated by the upper cervical spine. As the forward head posture is considered a direct cause for dysafferentation, [34] postural control – especially for spinal rotation and counter rotation – is markedly affected.
It may be that improving the posture parameters are attributed to stretching and strengthening exercises. However, we found no statistically significant differences in the control group which was subjected to traditional treatment only. It is interesting to note that there are no objective data to indicate that exercise will lead to postural deviations. Given the available evidence, it is questionable as to whether resistance training alone or in combination with stretching exercises will produce an adaptive shortening of a muscle and hence elicit postural changes. [47]
The unique contribution of the current study is that it evaluated the independent effect of structural rehabilitation in the form of forward head correction on long-term global spinal posture in the transverse, coronal and sagittal planes, which, to my knowledge, has not been previously reported. In conclusion, the effectiveness of forward head correction in improving three-dimensional spinal posture introduces the possibility of new guidelines in the treatment of adolescent idiopathic scoliosis. As effective prevention strategies for spinal disorders demand a detailed understanding of the interrelationship among different body segments, as supported by many studies, we hypothesized that the results of the current study could be particularly helpful in the evaluation and treatment planning of patients with idiopathic adolescent scoliosis.
The analysis has some potential limitations, however, each of which points toward directions of future study. The primary limitation was the lack of investigator blinding. In addition, the sample was a convenient sample rather than a random sample of the whole population. Furthermore, short-term follow-up after only three months may be considered a major limitation. Despite the limitations, the present randomized controlled study indicates that correction of biomechanical dysfunction, especially in terms of forward head posture, is essential in the management of adolescent idiopathic scoliosis.
The strengths of this study were(1) the randomized control design with the control group,
(2) analysis using the intention-to-treat principle,
(3) participants in both intervention groups received the same number of interventions,
(4) the high follow-up rate (greater than 90%).In the current study we assessed trunk surface symmetry because the cosmetic improvement of the trunk after any treatment is of paramount importance to the patient under treatment and his or her family. Trunk surface symmetry is also an important element in improving quality of life, an issue vital for any human being. [48]
Clinical messages
Forward head correction leads to a significant and permanent improvement
in functional status.Stretching and strengthening exercises temporally improve functional status.
Forward head correction was effective in improving scoliotic posture in
the transverse, coronal and sagittal planes.
Acknowledgement
I express my sincere gratitude to all the patients who kindly participated in the study. I am grateful to the Faculty of Physical Therapy, Cairo University for facilities and equipment.
Conflict of interest
None.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References:
Liu L, Zhu Y, Han X, Wu Y.
The creation of scoliosis by scapula-to-contralateral ilium tethering procedure in bipedal rats: a kyphoscoliosis model.
Spine (Phila Pa 1976) 2011; 17: 1340–1349.Everett CR, Patel RK.
A systematic literature review of nonsurgical treatment in adult scoliosis.
Spine 2007; 32: S130–S134White AA, Panjabi MA.
Clinical biomechanics of the spine, second edition.
Philadelphia, PA: Lippincott, Williams & Wilkins, 1990.Peterson BW, Goldberg J, Bilotto G, Fuller JH.
Cervicocollic reflex: its dynamic properties and interaction with vestibular reflexes.
J Neurophysiol 1985; 54: 90–109Morningstar MW, Strauchman MN, Weeks DA.
Spinal manipulation and anterior head weighting for the correction of forward head posture and cervical hypolordosis: a pilot study.
J Chiropr Med 2003; 2: 51–54Pompeiano O, Allum JH.
Vestibulospinal control of posture and locomotion: Progress in brain research: Volume 76.
London: Elsevier Science Publishers, 1988, pp. 137–143.Schieppati M, Nardone A, Schmid M.
Neck muscle fatigue affects postural control in man.
Neuroscience 2003; 121: 277–285Ledin T, Hafstrom A, Fransson PA, Magnusson M.
Influence of neck proprioception on vibration-induced postural sway.
Acta Otolaryngol 2003; 123: 594–599Yoganandan N, Knowles SA, Maiman DJ, Pinter FA.
Anatomic study of the morphology of human cervical facet joint.
Spine 2003; 28: 2317–2323Floman Y.
Thoracic scoliosis and restricted neck motion: a new syndrome?
Eur Spine J 1998; 7: 155–157Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA.
Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects.
Phys Ther 1992; 72: 425–431Lawrence G, Woggon D.
Pettibon spinal biomechanics scoliosis correction seminars.
St. Cloud, Minn: Dennis Woggon, 2002.Morningstar MW, Woggon D, Lawrence G (2004)
Scoliosis Treatment Using a Combination of Manipulative and Rehabilitative Therapy:
A Retrospective Case Series
BMC Musculoskeletal Disorders 2004 (Sep 14); 5: 32Morningstar M, Stitzel C.
The relationship between cervical kyphosis and idiopathic scoliosis.
J Vert Sublux Res 2008; 1–4.Kuo YL, Tully EA, Galea MP.
Video analysis of sagittal spinal posture in healthy young and older adults.
J Manipulative Physiol Ther 2009; 32: 210–215Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F.
The impact of positive sagittal balance in adult spinal deformity.
Spine 2005; 30: 2024–2029Lau KT, Cheung KY, Chan KB, Chan MH, Lo KY, Chiu TT.
Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity and disability.
Manual Ther 2010; 15: 457–462Epstein AM.
The outcomes movement: will it get us where we want to go?
N Engl J Med 1990; 323: 266–270Gstoettner M, Sekyra K, Walochnik N, Winter P, Wachter R, Bach CM.
Inter- and intraobserver reliability assessment of the Cobb angle: manual versus digital measurement tools.
Eur Spine J 2007; 16: 1587–1592Lenke LG, Betz RR, Harms J, .
Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis.
J Bone Joint Surg Am 2001; 83: 1169–1181Harman K, Hubley-Kozey C, Butler H.
Effectiveness of an exercise program to improve forward head posture in normal adults: a randomized, controlled 10-week trial.
J Man Manip Ther 2005; 13: 163–176.Niekerk S, Louw Q, Vaughan C, Grimmer-Somers K, Schreve K.
Photographic measurement of upper body sitting posture of high school students: a reliability and validity study.
BMC Musculoskelet Disord 2008; 9: 113Falla D, Jull GA, Russell T, Vicenzino B, Hodges P.
Effect of neck exercise on sitting posture in patients with chronic neck pain.
Phys Ther 2007; 87: 408–417Lippold C, Danesh G, Hoppe G, Drerup B, Hackenberg L.
Trunk inclination, pelvic tilt and pelvic rotation in relation to the craniofacial morphology in adults.
Angle Orthod 2007; 77: 29–35Feise RJ, Menke JM.
Functional rating index: literature review.
Med Sci Monit 2010; 16: RA25–36Fusco C, Zaina F, Atanasio S, Romano M, Negrini A, Negrini S.
Physical exercises in the treatment of adolescent idiopathic scoliosis: An updated systematic review.
Physiother Theory Pract 2011; 27: 80–114Rhee JM, Bridwell KH, Won DS, Lenke LG, Chotigavanichaya C, Hanson DS.
Sagittal plane analysis of adolescent idiopathic scoliosis.
Spine 2002; 27: 2350–2356Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D.
The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers.
Br J Sports Med 2010; 44: 376–381Moore MK.
Upper Crossed Syndrome and Its Relationship to Cervicogenic Headache
J Manipulative Physiol Ther 2004 (Jul); 27 (6): 414—420Grod JP, Diakow PR.
Effect of neck pain on verticality perception: A cohort study.
Arch Phys Med Rehabil 2002, 83: 412–415Gauchard GC, Lascombes P, Kuhnast M, Perrin PP.
Influence of different types of progressive idiopathic scoliosis on static and dynamic postural control.
Spine 2001, 26: 1052–1058Sjogaard G, Savard G, Juel C.
Muscle blood flow during isometric activity and its relation to muscle fatigue.
Eur J Physiol 1988; 57: 327–335.Travell JG, Simons D.
Myofascial pain and dysfunction: the trigger point manual.
Philadelphia: Williams & Wilkins, 1973.Seaman DR, Winterstein JF.
Dysafferentation: A Novel Term to Describe the Neuropathophysiological Effects
of Joint Complex Dysfunction. A Look at Likely Mechanisms of Symptom Generation
J Manipulative Physiol Ther 1998 (May); 21 (4): 267-280Filipovi V, Ciliga D.
Postural adaptation of idiopathic adolescent scolioses (IAS).
Kinesiology 2010; 42: 16–27.Michaelson P, Michaelson M, Jari? S, Latash ML, Sjolander P, Djupsjobacka M.
Vertical posture and head stability in patients with chronic neck pain.
J Rehabil Med 2003; 35: 229–235Coppieters MW, Knox JJ, Hodges PW.
Eccentric intra-orbit eye positions reduce postural control of the neck.
In: van Oordt M, Lando A (eds)
Proceedings of the 8th International Conference of Orthopedic Therapy,
Cape Town, 2004, International Physiotherapy – Manual Therapy.
Cape Town: The University of Cape Town, 2004, pp. 634–640.Lewit K.
Muscular and articular factors in movement restriction.
Manual Med 1985; 1: 83–85.Eiji I.
Roentgenographic analysis of posture in spinal osteoporotics.
Spine 1991; 16: 750–756Levangie PA, Norkin CC.
Joint structure & function, a comprehensive analysis, fourth edition.
Philadelphia, PA: FA Davis Co., 2005.Rigo M, Quera-Salvá G, Villagers M.
Sagittal configuration of the spine in girls with idiopathic scoliosis:
progressing rather than initiating factor.
Stud Health Technol Inform 2006; 123: 90De Jonge T, Dubousset JF, Illés T.
Sagittal plane correction in idiopathic scoliosis.
Spine 2002; 27: 754–760Dobosiewicz K, Durmala J, Jendrzejek H, Czernicki K.
Influence of method of asymmetric trunk mobilization on shaping of a physiological thoracic kyphosis in children and youth suffering from progressive idiopathic scoliosis.
Stud Health Technol Inform 2002; 91: 348–51Kadoury S, Cheriet F, Labelle H.
Prediction of the T2-T12 kyphosis in adolescent idiopathic scoliosis using a multivariate regression model.
Stud Health Technol Inform 2008; 140: 269–272Veldhuizen AG, Wever DJ, Webb PJ.
The etiology of idiopathic scoliosis: biomechanical and neuromuscular factors.
Eur Spine J 2000; 9: 178–184Parry E.
The influence of rotation of the trunk on the anatomy of the inguinal canal.
Br J Surg 1966; 53: 205–210Negrini S, Antonini G, Carabalona R, Minozzi S.
Physical exercises as a treatment for adolescent idiopathic scoliosis. A systematic review.
Pediatr Rehabil 2003; 6: 227–235Vasiliadis E, Grivas TB.
Quality of life after conservative treatment of adolescent idiopathic scoliosis.
Stud Health Technol Inform 2008, 135: 409–413
Return to SCOLIOSIS
Return to FORWARD HEAD POSTURE
Since 9-22-2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |