

Colorado Workers' Compensation: Medical vs Chiropractic
Costs for the Treatment of Lowback PainThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Chiropractic Medicine 2008 (Dec); 7 (4): 127–133 ~ FULL TEXT
OPEN ACCESS David Gilkey, DC, PhD, Laine Caddy, BS, Thomas Keefe, PhD, George Wahl, MS,
Richard Mobus, DC, Brian Enebo, DC, PhD, Kirby Duvall, MD, MSPH, Kimberly Griffiths, MSHS
Assistant Professor and Director of Undergraduate Education,
Department of Environmental and Radiological Health Sciences,
Colorado State University,
Ft Collins, CO 80523-1681.
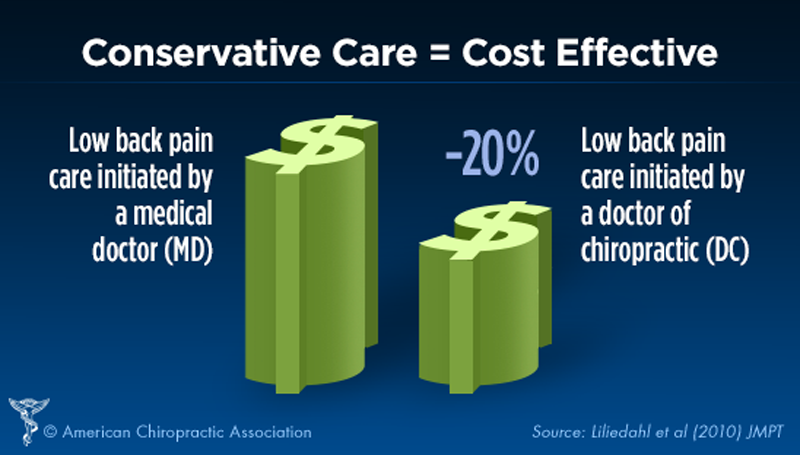
FROM: Liliedahl ~ JMPT 2010 (Nov)OBJECTIVE: Low back disorders (LBDs) are the most common complaint among workers; therefore, many questions arise about cost-effective treatment approaches. This investigation evaluated the differences in cost-related factors among a population of patients selecting chiropractic vs allopathic care for the treatment of nonspecific LBDs. The study hypothesis was that chiropractic care would be more cost-effective or equivalent to allopathic care for the noncomplicated LBDs.
METHODS: Cases were extracted from an insurance company database of patients reporting work-related low back injuries who were treated with either chiropractic or allopathic approaches. Cases were matched using the International Classification of Diseases, Ninth Revision, codes 722 (intervertebral disk disorders), 724 (other and unspecified disorders of the back), and 847 (sprains and strains of other and unspecified parts). The data set included 76 chiropractic cases and 2386 medical cases.
RESULTS: The total amount paid by the insurance company was 1.7 times higher for patients treated by doctors of chiropractic (DCs) compared with those treated by medical doctors (MDs), and the cost of clinical treatment was 3.3 times higher for the DCs than MDs.
CONCLUSION: The cost for treatment by DCs was greater than that of MDs for similarly classified conditions affecting the low back. The amount paid by the insurance company was primarily related to the number of services given by each provider.
Key indexing terms: Low back pain, Health care costs, Chiropractic, Medicine, workers' compensation
From the FULL TEXT Article:
Introduction
Low back pain (LBP) is among the most common medical complaints in the United States. An estimated 65% of low back disorders (LBDs) are work related. [1] Low back disorders continue to be reported as one of the most expensive conditions for working-age adults. [2] For example, back disorders account for approximately 33% of all health care and indemnity costs under workman's compensation. [3] Although 90% of LBP cases resolve within 6 weeks regardless of care, [2] for persons younger than 45 years, back injury is the most common cause of disability. [4] It is also estimated that 80% of costs are associated with 10% of cases. [5] It was our purpose to evaluate LBD cases treated by both doctors of chiropractic (DCs) and medical doctors (MDs) for comparison of costs and other parameters available in the workers' compensation database.
In the present study, all LBP cases were reported as injuries as required by Colorado workers' compensation law. However, up to 50% of back disorder cases lack a precipitating event, leading researchers to conclude that most LBP is a multifactorial syndrome. [6] Symptoms are usually attributed to one or more potential causes including poor muscle tone; muscle tension; muscle tears; injury to tendons, ligaments, nerves, or disks; and the resulting inflammation, [7] although in most cases there is no definite diagnosis made of the pain generator.
Doctors of chiropractic and MDs treat various forms of LBDs and back pain and often use different treatment approaches. Treatment techniques vary widely among disciplines and specialties and can cause disagreements. The differences in treatment approaches become problematic when there is lack of consensus about necessity of financing by third-party payers who are attempting to allocate scarce resources for indemnity, treatment, and/or rehabilitation.
Doctors of chiropractic favor spinal manipulative therapy to reduce pain, increase mobility, and restore the biomechanical and anatomical relations between spinal segments to facilitate rapid recovery, often within the first month. [7] Spinal manipulation therapy has been reported to prevent the onset of a chronic disorder associated with immobility and result in successful recovery, especially when the patient actively participates in strength and conditioning exercises and practices good body mechanics to help restore and maintain health. [8] Doctors of chiropractic focus on manual therapies, nutrition, and other physical modalities to restore and maintain health. [7] The average duration of care for chiropractic patients with nonspecific, uncomplicated LBP is approximately 3 to 6 weeks; for more severe cases with significant loss of spinal mobility, up to 10 weeks of care has been reported. [9]
Allopathic physicians (MDs) tend to favor medications, such as analgesics, muscle relaxants, and anti-inflammatory medications, as the primary treatment of nonspecific LBP. [7] Prescription drug expenditures for back pain have increased more rapidly than any other expenses involved in relieving LBP and account for more than 15% of the total health care expenses. [10] In addition to nonnarcotic medication, MDs may also recommend bed rest for no more than 4 days, aerobic exercise, physical therapy modalities, and work conditioning programs to help decrease LBP while retaining function. [11]
Methods
Data for this study were identified within a large insurance database held by Pinnacol Assurance in Denver, CO. Pinnacol Assurance is a quasi-State agency providing workers' compensation insurance policies to more than 60,000 businesses in Colorado. [12] They insure throughout the State and provided standard claims information on low back cases for this investigation. Cases of nonspecific low back injuries were extracted from a larger set of closed claims for the years 2000, 2001, and 2002. Common diagnoses for this population of injured workers were the International Classification of Diseases, Ninth Revision (ICD-9), codes 722, 847, and 724, representing intervertebral disk disorders, sprains and strains of other and unspecified parts, and other and unspecified disorders of the back, respectively. [13] The most common diagnosis for DCs and MDs was ICD-9 code 724. All cases within these 3 ICD-9 codes that were not related to the lumbar region were excluded. A total of 10,262 claims met these criteria. Included within this larger data set were complex and more serious cases that were defined by as many as 34 diagnostic ICD-9 codes. The cases also included those treated with multiple providers, hospitalization, and surgery. It was felt that this heterogeneous group of LBD cases would not provide a valid comparison between providers for conditions that were not necessarily similar as defined by ICD-9 codes. In an effort to create a more homogeneous group for comparison, a subset of 2,456 of these claims was identified with 3 or fewer ICD-9 codes. Therefore, a final data set in this evaluation contained only cases with 3 or less ICD-9 codes and included 76 DC-treated cases and 2,380 MD-treated cases. Of the 76 chiropractic cases, 68.4% had 1, 26.3% had 2, and 5.2% had 3 ICD-9 codes. This was very similar to the percentages of medically treated cases, whereby 70% had 1, 23.6% had 2, and 6.4% had 3 ICD-9 codes. Using ICD-9 codes facilitated better comparability between cases, as they were fairly well matched by type for each treatment approach.
Case variables provided by Pinnacol were limited and included the(1) amount of medical treatment benefits paid by the insurance company,
(2) amount of indemnity benefits paid,
(3) gross amount paid,
(4) days between first service date and last service date,
(5) days from injury to treatment,
(6) number of services, and
(7) days to claim closure.The data were analyzed using Statistical Package for the Social Sciences, version 14.0 (SPSS, Chicago, IL). Because the data were not normally distributed, a nonparametric test was selected. Comparisons were made between DC and MD groups for the variables of interest using the Mann-Whitney U test statistic, which compares the medians of the 2 groups on the basis of the ranks of the data values.
Results

Table 1

Table 2

Table 3 Descriptive statistics for 76 DC-treated cases are presented in Table 1. Table 2 presents the data from the 2,380 MD-treated cases. On average, the amount paid for treatment, as well as the gross amount paid, was greater for DCs than for MDs, differences that were found to be statistically significant (P < .001, Table 3). Furthermore, the number of services and days from first service to last service were significantly greater for DCs than MDs (P < .001, Table 3).
Treatment costs paid by the insurance company (med amount paid) were found to be approximately 3.3 times higher for a DC-treated LBP patient than for an MD-treated LBP patient (P < .001, Table 3). In addition, the total amount paid (gross paid) for treatment of an LBP patient was 1.7 times higher for DCs than for MDs (P < .001, Table 3). The number of days to completely close a case after the first treatment was 1.5 times longer for LBP patients treated by a DC than for LBP patients treated by an MD (P < .001, Table 3). Indemnity paid and days to first treatment after the injury (days to tx) were not significantly different between DC-treated and MD-treated LBP patients (P > .25, Table 3). Patient treatment periods were essentially the same regardless of approach, as seen in Table 3.
Discussion
Chiropractic care has been scrutinized because of the higher cost differential compared with allopathic approaches for the treatment of LBP. Previous research has indicated that consultation costs and total treatment costs of DCs are higher than those of MDs, [14] as seen in our study. Overall costs of treatment by DCs has been reported to be 16% to 25% higher than treatment costs from MDs. [15] This evaluation demonstrated a 3-fold differential between the treatment costs paid for DCs and MDs when comparing treatment approaches for nonspecific LBP. Differences seen in this study could be influenced by many variables, such as the low number of DC-treated cases compared with the much larger number of cases treated by MDs. Doctors of chiropractic who use longer-term spinal manipulative therapy regimens can significantly add costs to cases. However, most DCs are committed to treatment goals that include cost containment as a priority. [15]
Complicated disorders are likely to incur higher costs, whereas simple cases of back strain are less costly when treated by DCs compared with MDs. [6, 16, 17] For example, according to Jarvis et al, [16] compensation costs were 10 times more for medical claims. Furthermore, cost for total care was significantly less for chiropractic claimants. The number of office visits for DCs was higher; however, the cost per visit was lower. The investigation by Jarvis et al stratified claims into ICD-9 categories and concluded that chiropractic care was less costly for certain ICD-9 categories and no more costly than medical care in the remaining ICD-9 categories. [16] One study evaluated 7 other studies and found that chiropractic care was shown to be less costly than medical care. [17] Tuchin and Bonello [6] reported that the average medical payment was more than the average chiropractic payment. Their study concluded that chiropractic involvement for select, but not necessarily less severe, conditions of the back may be more cost-effective than other forms of intervention.
Our study found that chiropractic care is more expensive than medical care to treat nonspecific, uncomplicated LBP in the workers' compensation system in Colorado. The gross amount paid on average was higher for chiropractic care ($933 for DCs compared with $538 for MDs) because of the higher treatment costs ($868 for DCs compared with $264 for MDs). This finding is directly linked to the number of chiropractic services: an average of 9 services compared with an average of 3 services for medically treated cases. Chiropractic patients received care and supervision for longer periods of time, averaging 59 days, whereas MD-treated patients received care for an average of 23 days. According to Anderson et al, [18] when comparing the cost of treatment with spinal manipulation to treatment without manipulation, the difference in costs is explained partially by time differentials in days to closure. This study found that chiropractic cases required more services and more days to closure than medically treated cases, thus resulting in higher costs for managing the injury/disorder.
A significant component of workers' compensation costs is wage replacement for lost workdays. Indemnity benefits compensate the injured worker's lost wage until they can return to work. On average, most patients with a less severe episode of LBP will return to work immediately and nearly all within 1 month; however, many may not lose any time of gainful employment. [3] Although the difference in indemnity costs was not statistically significant, DC-treated cases was on average 3 times less than those treated by MDs ($49 for the patients treated by DCs compared with $179 for the MD group). In our study, only 174 cases were associated with lost-time wage replacement and only 9 were DC managed. With prolonged total temporary disability, the cost of claims rises dramatically.
Several studies found that chiropractic patients experienced fewer lost workdays than medically treated patients. [17, 19, 20] It was reported that patients who received chiropractic care returned to work on average 2.3 days sooner than patients who received medical care. [17] Assendelft et al [14] evaluated the costs of workers' compensation claims and concluded that DCs were able to return their patients back to work with fewer compensated days and lower treatment costs than did allopathic physicians. Bergemann and Cichoke [20] found that 82% of patients treated by DCs resumed work within 1 week, whereas only 41% of those treated by MDs did the same. As supported by several studies, on average, DC-treated patients are able to return to work either sooner or at least as rapidly as those treated by MDs. [17] Because employers and insurance companies experience significant losses associated with LBP cases, it is paramount to use strategies to return patients back to work rapidly.
There are many limitations in our study: lack of any patient follow-up, no available data collected on measure of satisfaction, no patient history, and the use of ICD-9 classification codes for primary case definitions. Workers' compensation data have a number of limitations, and using summary data provided by the third-party insurer organization has even greater limitations. Workers' compensation data are usually derived from original source documents called the First Report of Injury (FRI). [21] These data provide much detail about each case including personal identifiers, worker characteristics, as well as specifics about the injury and body part affected. Standardized codes were developed and have been used since 1976 by the Bureau of Labor Statistics to then describe information that may be in the FRI including a designation for body part injured (such as the back), nature of injury (such as sprain or fracture), the type of event causing the injury (such as lifting, pushing, pulling resulting in overexertion), and the source of the injury (as in materials, supplies, tools). [22] These codes that have been used by all states participating in the supplemental data system, including Colorado, form the basis for comparisons of WC data on injuries. [21] As the case is managed and documented, the insurer develops additional cost-related data pertaining to treatment activities and lost work time. In this study, only the summary data on cost-related factors were provided. No details from the FRI about the claimant, workplace, or injury event were available.
Patients choose chiropractic over allopathic approaches for many reasons. This choice can result in different expectations and outcomes from treatments, as well as differential cost impacts. For example, patients with chronic or recurrent back pain tend to seek DCs more often than those with the same condition seeking MD care; 15% to 22% more patients with recurring back pain visit a DC rather than an MD. [23] According to Nyiendo and Lamm, [23] The higher proportion of DC claimants with a history of low back pain may be reflective of a social phenomenon in which ‘first time’ back injury claimants seek care from traditional medical providers, while those who have previously gone the medical route, and continue to have back pain (chronic patients), are more willing to seek care from a chiropractor” (p 182).
Assendelft and Bouter [14] reported in their review of the literature that more chiropractic patients than MD patients had back pain symptoms for longer periods of time and more of them had been unable to work. Doctors of chiropractic are often viewed as spine specialists, so patients with greater levels of pain and with more frequent episodes of pain may be more likely to visit a doctor of chiropractic. This was also found by Nyiendo and Lamm [23] who reported that, of the patients who seek care for back pain, 66% of the patients that go to a DC for LBP treatment have a history of the condition, whereas 44% of patients who go to an MD for treatment have a history of LBP. It also appears that DCs have a higher patient return rate among patients having a second episode: 92% compared with 75% with physicians. [24] In our study, the clients' medical history was not available or taken into account, only the diagnosis based upon standard medical codes, thus resulting in a potential misclassification bias. Because it is known that more patients with chronic injuries return to chiropractors more frequently, overall treatment time and cost would be greater for DC cases, resulting in misclassification bias away from the null hypothesis. [23, 24] Other confounders that could cause potential bias include the patient's history; collagen diseases, age, smoking, and previous injuries.
There was no follow-up patient evaluation in the data file used in this study. Investigators do not really know the long-term outcome of either treatment approach. In the future, to assess the long-term effectiveness of the treatments, research should include follow-up studies of patient outcomes and include multiple quality of life variables as measures of effectiveness. Another parameter that would be important to note is how functional the patient is when he/she returns to work and resumes his/her activities of daily living. If the patient returns to work quickly but cannot perform his/her original job for an additional period, then the treatment would be less successful from a full- recovery standpoint. In addition, it is important to know how effective the treatment was in the prevention of further LBP flare-ups or reinjury; long-term follow-up should take place with patients to identify relapsing conditions vs stability.
Because of the cost implications related to the treatment options, third-party payers are very concerned with the cost of alternative (DC) vs allopathic (MD) methods. Health care plans favor the least expensive methods that return the patient back to work rapidly without considering many patient and provider goals. [25] When cost containment is the primary goal, patient preference is often ignored; and the quality of interactions and care may suffer. Our research compares the cost of DC care to the cost of traditional MD care, as well as how rapidly the client returned to work; but it does not look at the patient's quality of life during or after termination of treatment. Because a person does not have to be free from pain to return to work, [9] it should be a priority to evaluate stability and condition after the treatment termination to accurately and comprehensively determine the effectiveness of the approach undertaken.
According to several studies, most back pain patients are more satisfied with chiropractic care than with medical care. [7, 16, 26, 27] Patients consistently express more satisfaction with chiropractic care than allopathic care and also return more often to doctors of chiropractic when their symptoms recur. [7] It was found that 95.8% of chiropractic patients indicated an overall satisfaction with chiropractic care and chiropractic services. [26] Chiropractic patients have reported receiving more self-care advice, as well as clearer explanations about their conditions and rationale for treatment, than do patients of MDs. Investigators concluded that patients who have a better understanding of their conditions and treatment rationale tend to be more satisfied than patients who do not. [8] According to Wolsko et al, [27] chiropractic care was rated as “very helpful” for neck and LBP by 61% of the study population, whereas medical care was rated as “very helpful” for neck and LBP by only 27%.
Another limitation in the data was the possible discrepancies between disciplines in diagnosing injuries/disorders. Doctors of chiropractic possibly diagnose differently than MDs because of differences in education and training. Because the precise pathophysiology of most back injuries is usually unknown, it is up to each individual doctor to determine a diagnosis. The inconsistency between and within disciplines may make it difficult to accurately compare individuals with the assigned same diagnosis, thus possibly resulting in bias away from the null. A limitation with using ICD-9 codes in the study is that DCs and MDs may use them differently in clinical practice. Doctors of chiropractic tend to use more than 1 ICD-9 code 3 times more often than MDs. [23] Therefore, patients seeking care for the same condition may be diagnosed more extensively in one form of practice than the other. With the exception of diagnosing the patient with a sprain or strain, DCs use nonspecific codes much less often than do MDs. [16] This is problematic when patients have the same diagnosis on paper but, in reality, have different conditions. The resulting discrepancies in reporting conditions result in making it difficult to accurately compare the actual costs of 2 differing conditions.
Conclusion
This study adds to the understanding of differences associated with costs and services provided by DCs and MDs when treating simple and nonspecific LBP. It does not bring about an understanding of patient satisfaction for each provider or explain all potential benefits that might have been achieved by treatment. Results from our study appear to demonstrate that chiropractic care is more expensive than medical care when treating relatively simple forms of LBP. Because costs can greatly increase because of repeated treatments, the difference in expenses is mainly due to more services and longer treatment periods. Further research is needed to evaluate quality of life and patient satisfaction related to different treatment approaches, as well as follow-up of patient's functional status and stability upon return to work, resumption of activities of daily livings, and impacts of relapses. Future evaluations should also examine effectiveness when treating more complex disorders causing spine and LBP. Cost-effectiveness has become very important when choosing a heath care provider for most third-party payers. However, because patients respond differently to different forms of treatment, it would be in the best interest of both the insurance company and the patient for the patient to be provided preferred treatment options for his/her condition and to take an active role in his/her overall treatment plan.
References:
Guo H., Tanaka S., Halperin W.E., Cameron L.L.
Back pain prevalence in US industry and estimates of lost workdays.
Am J Public Health. 1999;89(7):1029–1035Deyo R.A., Cherkin D., Conrad D., Volinn E.
Cost, controversy, crisis: low back pain and the health of the public.
Annu Rev Public Health. 1991;12:141–156Williams D.A., Feuerstein M., Durbin D., Pezzullo J.
Health care and indemnity costs across the natural history of disability in occupational low back pain.
Spine. 1998;23(21):2329–2336Smith M.D., McGhan W.F.
Treating back pain without breaking the bank.
Bus Health. 1998:50–52Spengler D.M., Bigos S.J., Martin N.A.
Back injuries in industry: a retrospective study I: overview and cost analysis.
Spine. 1986;11:241–245Tuchin P.J., Bonello R.
Preliminary Findings of Analysis of Chiropractic Utilization and Cost in the Workers'
Compensation System of New South Wales, Australia
J Manipulative Physiol Ther 1995 (Oct); 18 (8): 503–511Cooper R.A., McKee H.J.
Chiropractic in the United States: trends and issues.
Milbank Q. 2003;18(1):107–138Hertzman-Miller RP, Morgenstern H, Hurwitz EL, et al.
Comparing the Satisfaction of Low Back Pain Patients Randomized to Receive Medical or Chiropractic Care:
Results From the UCLA Low-back Pain Study
Am J Public Health 2002 (Oct); 92 (10): 1628–1633Cote P., Clarke J., Deguire S., Frank J.W., Yassi A.
Chiropractors and return-to-work: the experiences of three Canadian focus groups.
J Manipulative Physiol Ther. 2001;24(5):309–316Luo X, Pietrobon R, Sun SX, Liu GG, Hey L.
Estimates and Patterns of Direct Health Care Expenditures Among Individuals
With Back Pain in the United States
Spine (Phila Pa 1976) 2004 (Jan 1); 29 (1): 79–86Bishop P.B., Wing C.
Knowledge transfer in family physicians managing patients with acute low back pain:
a prospective randomized control trial.
Spine J. 2006;6(3):282–288Pinnacol Assurance Colorado: Pinnacol fact sheet. 2006.
http://www.pinnacol.com/aboutpinnacol/reporterResources.htmlAustin P., Mettler A. Pearson/Prentice Hall; Upper Saddle River (NJ): 2006.
Medical office coding.Assendelft W.J.J., Bouter L.M.
Does the goose really lay golden eggs? A methodological review of workmen's compensation studies.
J Manipulative Physiol Ther. 1993;16(3):161–168Wojcik J.
Chiropractic care of workers blamed for higher comp costs; but if closely managed, chiropractors can be effective.
Bus Insur. 2003;37(42):10–12.Jarvis K.B., Phillips R.B., Morris E.K.
Cost Per Case Comparison of Back Injury Claims of Chiropractic Versus Medical Management
For Conditions With Identical Diagnostic Codes
J Occup Med 1991 (Aug); 33 (8): 847–852Johnson M.R., Schultz M.K., Ferguson A.C.
A Comparison of Chiropractic, Medical and Osteopathic Care for Work-related Sprains and Strains
J Manipulative Physiol Ther 1989 (Oct); 12 (5): 335–344Anderson D.M., Shepard T.A., Lane B.L. Pinnacol Assuance; Denver (Colo): 2000.
Cost analysis of conservative (non-surgical) treatment for low back pain in a workers' compensation
population: comparing treatment with manipulation to treatment without manipulation.Gilkey D.P., Keefe T.J., Hautaluoma J.E., Bigelow P.L., Sweere J.J.
Low back pain in residential construction carpenters: Hispanic and non-Hispanic chiropractic patient differences.
Top Clin Chiropr. 2002;9(4):26–32.Bergemann B.W., Cichoke A.J.
Cost effectiveness of medical vs. chiropractic treatment of low-back injuries.
J Manipulative Physiol Ther. 1980;3(3):143–147.Lipscomb H., Glazner J., Bondy J., Lezotte D., Guarini K.
Analysis of text from injury reports improves understanding of construction falls.
J Occup Environ Med. 2004;46(11):1166–1173US Department of Labor .
Bureau of Labor Statistics; Washington (DC): 1992.
Bureau of Labor Statistics, occupational injury and illness classification manual.Nyiendo J., Lamm L.
Disabling Low Back Oregon Workers' Compensation Claims Part I:
Methodology and Clinical Categorization of Chiropractic and Medical Cases
J Manipulative Physiol Ther 1991 (Mar); 14 (3): 177–184American Chiropractic Association .
American Chiropractic Association; Arlington (Va): 1998.
Chiropractic state of the art.LaRosa J. Dorland's Dictionaries; 1995.
Chiropractic services. Medical & healthcare marketplace guide 11: 222+00593467.Dobson A. 2nd ed. American Chiropractic Foundation; Arlington (Va): 1997.
Chiropractic professionals: part of your managed care team.Wolsko PM, Eisenberg DM, Davis RB, Kessler R, Phillips RS:
Patterns and Perceptions of Care for Treatment of Back
and Neck Pain: Results of a National Survey
Spine (Phila Pa 1976) 2003 (Feb 1); 28 (3): 292–297
Return to COST-EFFECTIVENESS
Return to WORKERS' COMPENSATION
Since 2–27–2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |