

Single-blind Randomised Controlled Trial
of Chemonucleolysis and Manipulation in
the Treatment of Symptomatic Lumbar Disc HerniationThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: European Spine Journal 2000 (Jun); 9 (3): 202–207 ~ FULL TEXT
OPEN ACCESS A. K. Burton, K. Malcolm Tillotson, John Cleary
Spinal Research Unit,
University of Huddersfield,
30 Queen Street,
Huddersfield HD1 2SP, UK
kburton@cix.co.uk
Tel.: +44-1484-535200,
Fax: +44-1484-435744
Forty patients with confirmed sciatica were treated with either osteopathic manipulation treatment or chemonucleolysis. The pain endured by the patient was measured at 2 weeks, 6 weeks and one year. After a year patients from both groups were very similar in recovery. However, at 2 and 6 weeks those receiving manipulation reported greater improvement.
This single-blind randomised clinical trial compared osteopathic manipulative treatment with chemonucleolysis (used as a control of known efficacy) for symptomatic lumbar disc herniation. Forty patients with sciatica due to this diagnosis (confirmed by imaging) were treated either by chemonucleolysis or manipulation. Outcomes (leg pain, back pain and self-reported disability) were measured at 2 weeks, 6 weeks and 12 months. The mean values for all outcomes improved in both groups. By 12 months, there was no statistically significant difference in outcome between the treatments, but manipulation produced a statistically significant greater improvement for back pain and disability in the first few weeks. A similar number from both groups required additional orthopaedic intervention; there were no serious complications. Crude cost analysis suggested an overall financial advantage from manipulation. Because osteopathic manipulation produced a 12-month outcome that was equivalent to chemonucleolysis, it can be considered as an option for the treatment of symptomatic lumbar disc herniation, at least in the absence of clear indications for surgery. Further study into the value of manipulation at a more acute stage is warranted.
Key words: Chemonucleolysis – Lumbar disc herniation – Manipulation – Osteopathy – Randomised controlled trial – Sciatica
From the FULL TEXT Article:
Introduction
Back pain with associated leg pain is a common complaint, while the lifetime prevalence of lumbar radicular syndrome is probably no more than 5% [7]. However, for those patients it is a particularly painful and distressing experience. Although the predominant complaint is leg pain, most patients report concomitant back pain with associated disability. The natural course of acute cases is favourable, and conservative management strategies usually are sufficient [17]. However, for some patients the pain will be unremitting and other therapeutic options need to be considered.
Manipulation is an accepted primary care treatment for back pain [15]. Although osteopathic and chiropractic texts have suggested manipulation is also a safe and effective treatment for sciatica due to lumbar disc herniation [5, 12], there is little beyond anecdotal evidence for its efficacy and it is considered to be contra-indicated by some authorities [17]. Nevertheless, osteopaths and chiropractors do treat many cases of lumbar radicular syndrome, and serious complications such as cauda equina syndrome seem to be rare [2]. Investigations into its efficacy are, therefore, desirable to inform clinical practice. The manipulative techniques used vary from one manipulator to another, but the main elements are soft tissue stretching manoeuvres, passive techniques to articulate the lumbar spine throughout its ranges of motion (sometimes known as ‘mobilisation’) and side posture high-velocity rotatory thrusts (sometimes termed ‘manipulation’). [5, 12] The term ‘manipulation’ is used in this paper to cover the range of manual techniques used by osteopaths, and not as a synonym for thrust-type techniques.
The two most common orthopaedic interventions for a lumbar radicular syndrome due to disc herniation are partial discectomy and chemonucleolysis. Conventional discectomy involves a spinal surgical procedure, with removal of a varying proportion of the disc material. Chemonucleolysis involves injection of an enzyme (chymopapain) into the nucleus to reduce the water-binding capacity of its proteoglycans, and thus reduce the amount of nuclear material. A recent systematic review has concluded that chemonucleolysis is an effective treatment, but that it is less effective than discectomy, with up to 30% of patients subsequently coming to surgery [9]. Chemonucleolysis can be considered an intermediate between conservative management and open surgery, which avoids the accepted, but rare, complications of a surgical procedure with its associated relatively high health care costs.
A consensus summary of a recent focus meeting on disc herniation [1] outlined some of the problems with current management. Whilst discectomy and chemonucleolysis can be accepted as proven treatments, there is concern about differential surgery rates, the optimal type of intervention, its timing, and the selection of appropriate patients. It was also felt that non-invasive interventions, such as manipulation, were of unknown efficacy due to the lack of prospective randomised trials. The present trial was proposed to address this latter issue.
The hypothesis to be tested was that manipulative treatment provides at least equivalent 12-month outcomes when compared with treatment by chemonucleolysis for patients with sciatica due to confirmed lumbar disc herniation, where chemonucleolysis is taken as a procedure known to be more effective than placebo [9]. It was also hypothesised that manipulation produces a more rapid improvement, particularly for disability and back pain.
Materials and methods
The trial participants were recruited from the orthopaedic department of a hospital in the north of England. They were patients complaining of unremitting sciatica, diagnosed as due to a lumbar disc herniation, for whom there was no clinical indication for surgical intervention.
The study design was a prospective randomised controlled trial to determine 2-week, 6-week and 12-month outcomes from manipulation compared with chemonucleolysis, where chemonucleolysis acted as the control. Local ethical committee approval was obtained for random allocation to treatment either by chemonucleolysis or osteopathic manipulation. Blinding of patients and treating clinicians to the treatment allocation was clearly not possible, but a blinded independent observer performed baseline and followup assessments, supplemented by validated self-report questionnaires.
Specific entry criteria were similar to those described elsewhere. [3, 13] All patients displayed the following:
Age range 18–60 years
Unilateral unremitting sciatica (with leg pain worse than back pain)
Positive straight leg raising test with positive nerve root tension signs, radiculopathy limited to a single nerve root.
In addition, there was unequivocal evidence of single-level non-sequestrated lumbar disc herniation on either computed tomography (CT) or magnetic resonance imaging (MRI), where imaging findings were consistent with the clinical picture. Exclusion criteria were:
Sequestrated herniation
Multiple-level marked lumbar degenerative changes
Previous lumbar surgery
Previous chemonucleolysis
Previous manipulative treatment for the present complaint
Involvement in litigation
Following diagnosis (and consideration of exclusion criteria) patients were informed of the nature of the trial and asked to sign a consent form. The randomisation sequence was generated by computer and balanced over order. A blinded envelope system was used to allocate patients to treatment. Those patients randomised to manipulation were contacted by the research team and given an appointment to see a private osteopathic manipulator (A.K.B.), whilst those randomised to chemonucleolysis were put on the waiting list of an orthopaedic surgeon (J.C.).
The manipulative treatment comprised a number of 15 min. treatment sessions over a period not exceeding 12 weeks, with the bulk of the sessions occurring in the first 6 weeks. The treatments followed a typical protocol for osteopathic management of sciatica [12]. Briefly, the procedures included soft tissue stretching of the lumbar and buttock musculature, low-amplitude passive articulatory manoeuvres of the lumbar spine and judicious use of high-velocity thrusts to one or more lumbar articulations [5]. (A high-velocity thrust is a manipulative technique that delivers a low-amplitude high-velocity movement, within the physiological range, intended to be perpendicular to a specific lumbar zygapophysial joint.) Any or all of these were performed on each occasion at the clinical discretion of the manipulator. Advice was given to continue normal daily activity so far as possible, whilst early return to work (for those employed) was encouraged.
The chemonucleolysis was administered as an in-patient procedure under general anaesthesia. A single injection of chymopapain (Chymodyactyl, Boots Co. Ltd, Nottingham, UK) was given. An 18-G spinal needle was placed into the centre of the nucleus of the disc under biplanar radiographic control, and a discogram performed with 0.5 ml contrast medium. Then, 2 ml (4000 units) chymopapain was gradually injected. Finally, the needle was retracted to clear the posterior spinal elements, and 10 ml of 0.25% bupivacaine was injected. Patients recovered overnight and were discharged the following day to the usual care of their family doctor.
Baseline data for all patients were obtained immediately before treatment, by a senior physiotherapist at the hospital who was blinded to the treatment allocation. The same physiotherapist performed the follow-up assessments (barring holidays, when a deputy stood in). Patients were asked not to reveal their treatment allocations. Clinical assessments were conducted to a simple structured protocol, supplemented by a booklet of questionnaires that was returned to the research office, where a blinded research assistant coded them onto the computer database. The clinical variables included measures of lumbar flexion, lumbar side bending and straight leg raising, along with details of the history of the complaint and work status. Disability was measured with the Roland Disability Questionnaire (RDQ) [14], whilst the extent of pain was measured with seven-point ‘annotated thermometer’ rating scales for leg pain and back pain [14]. Baseline psychological parameters were checked using additional questionnaires. Distress was estimated by the Distress and Risk Assessment Method [11], which involves measures of depression and somatic perceptions.
At each follow-up point, the clinical assessments were as at the pre-treatment assessment, with additional questions concerning complications and other treatments being sought. Outcomes at each point were assessed from self-reported disability (measured by the RDQ) along with pain ratings for back pain and leg pain (measured by the pain scales).
A total of 40 patients was recruited (20 in each treatment arm). Their mean age was 41.9 years (SD 10.6) and 19 were male. Twenty-five patients were allocated to treatment strictly through the randomisation protocol, but administrative difficulties, caused by movement of key hospital staff, resulted in 15 patients being allocated to treatment outside the randomisation sequence. A comparison between the baseline data of the properly randomised group and the remainder revealed no statistically significant differences; investigation of the recruitment patterns revealed no systematic bias. All 40 patients attended for follow-up at 2 weeks, whilst 37 (93%) were available at 6 weeks and 30 (75%) at 12 months. The loss to follow-up rate was the same in both treatment groups.
The average length of the presenting spell of similar leg pain at the point of diagnosis was 30 weeks (SD 34) for the manipulation group and 32 weeks (SD 36) for the injected group. A previous history of low back trouble was reported by 15 manipulated patients and 12 injected patients, with a previous history of sciatica being reported by 13 and 10 patients respectively. Seven manipulated and six injected patients were off work at baseline. None of these differences between groups were statistically significant. The mean delay before commencement of manipulative treatment in the manipulator’s office practice was 3 weeks (SD 3.6), whilst the mean delay for chemonucleolysis, performed at the hospital, was 12.9 weeks (SD 7.8).
The data were variously suitable for statistical analysis by two-tailed Student’s t-tests, chi-squared tests and multiple regression. Repeated measures analysis with general linear modelling was used to study trends and the influence of covariates. The level of statistical significance was set at 5%.
Results
There were no instances of major complications from either treatment, but a number of patients required additional orthopaedic intervention (between 6 weeks and 12 months) due to persisting symptoms; these we have termed ‘therapeutic failures’. Four of the manipulated patients received chemonucleolysis and one required lumbar discectomy. Three of the injected patients received epidural steroid injections and one of these also underwent manipulation under anaesthetic.

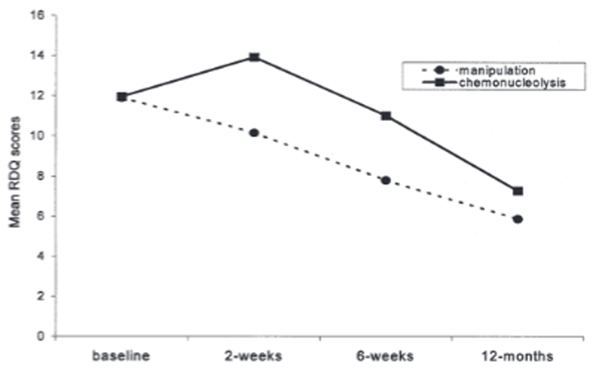
Table 1 The outcome data (means and standard deviations of scores for leg pain, back pain and disability) from baseline through 12 months are given in Table 1. For ease of interpretation of the patterns of response, the data are shown in graphical form in Figs. 1–3. By 12 months, both treatment groups showed statistically significant improvement for mean scores on all three measures, with no statistically significant differences between groups, although there were between-group differences during the first few weeks.
Both treatment groups followed a similar pattern of steady improvement in leg pain over time, with no statistically significant difference between the groups (Fig. 1). There was a statistically significant benefit from manipulation over chemonucleolysis for back pain at both 2 weeks and 6 weeks (Fig. 2). In contrast to the manipulation group, the chemonucleolysis group did not show a significant improvement in mean back pain score (compared with baseline) during the first 6 weeks. There was a statistically significant benefit from manipulation for mean disability score at 2 weeks compared with chemonucleolysis. At this point, the manipulation group had significantly improved on this measure, but the chemonucleolysis group had deteriorated somewhat. By 6 weeks there was no significant difference between the groups for mean disability scores; the manipulated patients, however, had significantly improved over baseline, but the chemonucleolysis group had not (Fig. 3).
Figure 1. Graph of the mean leg pain scores from
baseline though 12 months by treatment group.
Over time, the improvement was statistically
significant from baseline to 2 weeks for the
manipulated patients, and from baseline to 6
weeks for the injected patients. Between groups,
the differences were not statistically
significantly different at any assessment point.
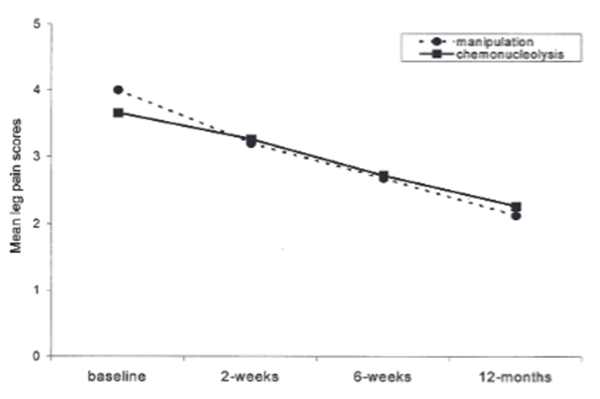
Figure 2. Graph of the mean back pain scores from
baseline though 12 months by treatment group.
Over time, the improvement was statistically
significant from baseline to 6 weeks for the
manipulated patients, and from baseline to 12
months for the injected patients. Between groups,
the difference was statistically significant
both at 2 weeks and 6 weeks.
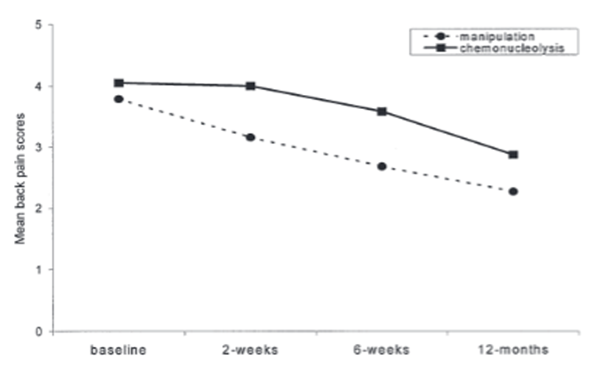
Figure 3. Graph of the mean Roland Disability
Questionnaire (RDQ) scores from baseline though
12 months by treatment group. Over time, the
improvement was statistically significant from
baseline to 2 weeks and from 2 weeks to 6 weeks
for the manipulated patients, and from 2 weeks
to 6 weeks and from 6 weeks to 12 months for the
injected patients. Between groups, the difference
was statistically significant only at 2 weeks.
Covariates (age, sex, initial degree of straight leg raising and lumbar mobility) had minimal and non-significant influences on marginal means for the outcome measures. Of the other baseline variables, higher baseline depression scores predicted a poorer prognosis in terms of pain but not disability, and a longer history of symptoms predicted an inferior prognosis only in respect of back pain.
Possible confounding influences were explored. There was no statistically significant difference in baseline scores for any of the outcome measures (leg pain, back pain and disability) between the manipulation patients and the chemonucleolysis patients, despite the average 9 week further delay between randomisation and commencement of treatment for the latter group. A sub-group analysis was performed to determine whether the breakdown in the randomisation procedure had any influence on the results. Comparing the properly randomised patients with the remainder revealed that the patterns of responses across all three follow-up points for all three outcome variables were statistically indistinguishable.
A formal cost analysis was not included in the study design but, in view of the interest in this measure, the crude treatment costs were estimated for patients who provided 12 months data. The average number of treatment sessions given to the manipulated patients was 11 (range 6–18). None of the injected patients remained in hospital beyond 24 h. The manipulator’s fee was £20 per session, whilst the cost of the chemonucleolysis (inclusive of all drug and hospital costs) was £800. A total of 165 manipulative sessions were given, at a total cost of £3,300. This can be compared with the overall cost for the 15 injections, at £12,000. To these figures must be added the costs incurred for treating therapeutic failures. Our best estimates for these, in this cohort, suggest that the extra principal costs incurred over 1 year for treatment by chemonucleolysis rather than manipulation would be of the order of £300 per patient.
Discussion
This study was a randomised controlled trial comparing osteopathic manipulative treatment with chemonucleolysis for symptomatic lumbar disc herniation confirmed by clinical criteria and imaging. Taking chemonucleolysis as an effective treatment [9], the trial sought to determine whether manipulation is a comparably safe and effective treatment option. So far as we are aware, it is the first report of a prospective randomised trial comparing manipulation with a proven effective treatment for this diagnosis. It may be argued that partial discectomy would have presented a more suitable control treatment, but the intention was to test the value of manipulation as an option in patients for whom there was no clear-cut clinical indication for surgical intervention (bearing in mind the favourable long-term prognosis [16]). In addition, it would have been exceedingly difficult to obtain patient consent to randomisation if the options were surgery or a non-surgical procedure.
The trial protocol was designed, so far as was reasonably possible, to avoid sources of bias. Whilst it was impossible to blind either the patients or the clinicians to the randomised treatment, the measures of outcome were assessed independently. Precautions were taken to ensure that the trial participants represented a homogeneous diagnostic category. There were no identifiable baseline differences between the two treatment groups, and the follow-up period was of sufficient length to reveal failures in both treatment arms.
Nevertheless, there are certain limitations that should be discussed. The most obvious problem is that some of the patients were not randomised according to the predetermined order, which was an unfortunate consequence of administrative difficulties. However, there were no discernible baseline or follow-up differences between the correctly and incorrectly randomised groups; we found no reason to suppose the breakdown in the randomisation procedure exerted any systematic bias on the results. Due to local factors governing the provision of hospital services that were beyond the control of the investigators, the chemonucleolysis patients experienced an extra 9 weeks delay on average between diagnosis and commencement of treatment compared with the manipulated patients. In view of the similar baseline scores for both groups, the differential delay is unlikely to have exerted any bias on the results.
The primary result was that osteopathic manipulation was no less effective than chemonucleolysis in reducing self-reported pain and disability when assessed at 12 months, and the number of therapeutic failures was not significantly different. In addition, the improvement for the manipulated patients occurred sooner and did not show the tendency for increased disability at 2 weeks seen in the injected patients, and there was some indication that there will be a moderate cost benefit. Manipulation can thus be considered an effective option for treatment of symptomatic lumbar disc herniation This patient population was relatively chronic and, since the length of history had some predictive value, it would be logical in future trials to explore the possibility that earlier manipulative intervention could have an enhanced effect.
The mechanism through which manipulation may exert an effect is unknown. Manipulative treatment is generally directed toward improving spinal mobility [5], but increases in mobility are found in only about half of back pain patients following lumbar manipulation [4], and were not statistically significant covariates here. Any effect is unlikely to be due to a reduction in the size of the herniation, because the CT appearance of the disc is unchanged by manipulation in most cases [5]. The mechanism of symptomatic improvement with chemonucleolysis is also unclear. There is certainly a permanent reduction in disc height in most cases [10], but this does not necessarily result in a reduction of the herniation [8]; any change in the size of herniation seems to depend largely on the natural history of the condition [6]. Lumbar disc herniation (in the absence of clear indications for surgery) has a favourable long-term prognosis under conservative therapy [16], so it may be that treatments such as chemonucleolysis and manipulation are effective through some, as yet unknown, influence on pain mechanisms rather than by any physical effect on the herniation.
Conclusions
This randomised controlled trial of manipulation and chemonucleolysis for unremitting lumbar radicular syndrome has shown no statistically significant difference in outcomes between the two treatments at 12-months’ follow-up, although there was a small statistically significant short-term benefit from manipulation for back pain and disability (though not for leg pain). The therapeutic failure rates did not differ between the treatment groups. There was an overall crude cost saving from manipulation, and no evidence was found to question its safety. We conclude, therefore, that osteopathic manipulation can be considered a safe and effective treatment option for patients with a lumbar radicular syndrome due to disc herniation, at least in the absence of clear clinical indications for surgical intervention.
Acknowledgements
Sincere thanks are due to Alison Sharp, MCSP, for undertaking the patient assessments during the trial. The contribution of Rebecca Burt, BSc, to the administrative management and data entry is gratefully acknowledged. The study was funded by the NHS Executive, Northern and Yorkshire, UK (project no. ND0020 T367).
References
Andersson GBJ, Brown MD, Dvorak J, Herzog RJ, Kambin P, Malter A, et al (1996)
Consensus summary on the diagnosis and treatment of lumbar disc herniation.
Spine 21:75S-78SAssendelft WJJ, Bouter LM, Knipschild PG (1996)
Complications of spinal manipulation: a comprehensive review of the literature.
J Fam Pract 42:475–48Benoist M, Bonneville J-F, Lassale B, Runge M, Gillard C, Vazquez-Suarez J, et al (1993)
A randomised, double-blind study to compare low-dose with standard-dose chymopapain in the treatment of herniated lumbar intervertebral discs.
Spine 18:28–34Burton AK, Tillotson KM, Edwards VA, Sykes DA (1990)
Lumbar sagittal mobility and low back symptoms in patients treated with manipulation.
J Spinal Disord 3:262–268Cassidy JD, Thiel HW, Kirkaldy-Willis WH (1993)
Side-posture manipulation for lumbar intervertebral disk herniation.
J Manipulative Physiol Ther 16: 96–103Castro WHM, Halm H, Jerosch J, Steinbeck J, Meyer M, Gohike KH, et al (1994)
Long-term changes in the magnetic resonance image after chemonucleolysis.
Eur Spine J 3:222–224Clinical Standards Advisory Group (1994)
Epidemiology review: the epidemiology and cost of back pain.
HMSO, LondonFraser RD, Sandhu A, Gogan WJ (1995)
Magnetic resonance imaging findings 10 years after treatment for lumbar disc herniation.
Spine 20:710–714Gibson JNA, Grant IC, Waddell G (1999)
The Cochrane review of surgery for lumbar disc prolapse (Cochrane review) and degenerative lumbar spondylosis.
Spine 24: 1820–1832, and The Cochrane Library, Issue 1.
Update Software, Oxford
www.update-soft-ware.com/ccweb/cochrane/cdsr.htmLeivseth G, Salvesen R, Hemminghytt S, Brinckmann P, Frobin W (1999)
Do human lumbar discs reconstitute after chemonucleolysis? A 7-year follow-up study.
Spine 24:342–348Main CJ, Wood PL, Hollis S, Spanswick CC, Waddell G (1992)
The distress and risk assessment method: a simple patient classification to identify distress and evaluate the risk of poor outcome.
Spine 17:42–52McClune T, Clarke R, Walker C, Burton K (1997)
Osteopathic management of mechanical low back pain.
In: Giles LGF, Singer KP (eds) Clinical anatomy and management of low back pain, vol. 1.
Butterworth Heinemann, Oxford, pp 358–368Nordby EJ, Fraser RD, Javid MJ (1996)
Chemonucleolysis.
Spine 21: 1102–1105Roland M, Morris R (1983)
A study of the natural history of back pain. I. Development of a reliable and sensitive measure of disability in low-back pain.
Spine 8: 141–144Royal College of General Practitioners.
Clinical Guidelines for the Management of Acute Low Back Pain
London: Royal College of General Practitioners; (1999). [UK]Weber H (1983)
Lumbar disc herniation. A controlled prospective study with ten years of observation.
Spine 8: 131–140Weber H (1994)
The natural history of disc herniation and the influence of intervention.
Spine 19:2234–2238
Return to ChiroZINE ARCHIVES
Return to COST-EFFECTIVENESS
Return to DISC HERNIATION & CHIROPRACTIC
Return to COST EFFECTIVENESS JOINT STATEMENT
Return to "Testimony to the Department of Veterans Affairs"
Since 9-18-2001


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |