

Global, Regional, and National Burden of Migraine
and Tension-type Headache, 1990-2016: A Systematic
Analysis for the Global Burden of Disease Study 2016This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Lancet Neurol. 2018 (Nov); 17 (11): 954976 ~ FULL TEXT
OPEN ACCESS GBD 2016 Headache Collaborators
Prof Lars Jacob Stovner,
Department of Neuromedicine and Movement Science,
Norwegian University of Science and Technology,
Trondheim N-7491, Norway
lars.stovner@ntnu.no

BACKGROUND: Through the Global Burden of Diseases, Injuries, and Risk Factors (GBD) studies, headache has emerged as a major global public health concern. We aimed to use data from the GBD 2016 study to provide new estimates for prevalence and years of life lived with disability (YLDs) for migraine and tension-type headache and to present the methods and results in an accessible way for clinicians and researchers of headache disorders.
METHODS: Data were derived from population-based cross-sectional surveys on migraine and tension-type headache. Prevalence for each sex and 5year age group interval (ie, age 5 years to ≥95 years) at different time points from 1990 and 2016 in all countries and GBD regions were estimated using a Bayesian meta-regression model. Disease burden measured in YLDs was calculated from prevalence and average time spent with headache multiplied by disability weights (a measure of the relative severity of the disabling consequence of a disease). The burden stemming from medication overuse headache, which was included in earlier iterations of GBD as a separate cause, was subsumed as a sequela of either migraine or tension-type headache. Because no deaths were assigned to headaches as the underlying cause, YLDs equate to disability-adjusted life-years (DALYs). We also analysed results on the basis of the Socio-demographic Index (SDI), a compound measure of income per capita, education, and fertility.
FINDINGS: Almost three billion individuals were estimated to have a migraine or tension-type headache in 2016: 1·89 billion (95% uncertainty interval [UI] 1·712·10) with tension-type headache and 1·04 billion (95% UI 1·001·09) with migraine. However, because migraine had a much higher disability weight than tension-type headache, migraine caused 45·1 million (95% UI 29·062·8) and tension-type headache only 7·2 million (95% UI 4·610·5) years lived with disability (YLDs) globally in 2016. The headaches were most burdensome in women between ages 15 and 49 years, with migraine causing 20·3 million (95% UI 12·928·5) and tension-type headache 2·9 million (95% UI 1·84·2) YLDs in 2016, which was 11·2% of all YLDs in this age group and sex. Age-standardised DALYs for each headache type showed a small increase as SDI increased.
INTERPRETATION: Although current estimates are based on limited data, our study shows that headache disorders, and migraine in particular, are important causes of disability worldwide, and deserve greater attention in health policy debates and research resource allocation. Future iterations of this study, based on sources from additional countries and with less methodological heterogeneity, should help to provide stronger evidence of the need for action.
There is more like this at our
Global Burden of Disease PageFUNDING: Bill & Melinda Gates Foundation.
From the FULL TEXT Article:
Introduction
Migraine and other headache disorders are among the most prevalent disorders worldwide, [1] but recognition of their importance for public health has come only since 2000. This delay has occurred in part because headache is not fatal and does not result in permanent or objective disability, and in part because headaches are experienced by most people from time to time, which has hindered the realisation that headache disorders are debilitating for a relatively large minority of the people who are affected.
The Global Burden of Diseases, Injuries, and Risk Factors (GBD) studies have as one of their main aims the evaluation not only of mortality but also of non-fatal health outcomes. GBD offers a method of quantifying health loss in time units, enabling comparisons over time and across conditions, cultures, and countries, and, from 2016, at subnational levels in some countries. GBD has become an important tool for priority setting and planning of health services by international health organisations and governments.
Migraine was not included in GBD 1990, but was added in GBD 2000. In GBD 2010, tension-type headache was added and in GBD 2013, medication overuse headache was included. In GBD 2000, migraine was ranked as the 19th cause of disability globally. [2] For the GBD 2000 study, data were absent for more than half of the world's population. When new data came from big countries like Russia, China, India, and some parts of Africa, and with tension-type headache and medication overuse headache also taken into account, headache disorders were collectively the third cause of disability in people under 50 years of age in GBD 2015. [3] Since GBD 2010, prevalence and burden of disability have been re-estimated for the full time period from 1990 until the most recent year for which data are available, each time incorporating new data sources and any updates to methods.
Research in context Evidence before this study
Since 2000, the Global Burden of Diseases, Injuries, and Risk Factors (GBD) studies have produced estimates of prevalence and burden of migraine. Since GBD 2010, tension-type headache and medication overuse headache have been added and estimates have been made by country spanning the period from 1990 to the most recent year for which data are available. Headache disorders, and in particular, migraine, have been found to be highly prevalent and a cause of large burden. To date, no research article has focused on the detailed methods and results of headache estimates from GBD. With the present study, we updated a previous systematic review covering 19802001 by doing a review that searched PubMed for articles using the terms migraine, tension, headache, medication, and epidemiology from Jan 1, 2001, until Dec 31, 2015. There were no language restrictions.
Added value of this studyIn 2016, of all GBD causes of disease, tension-type headache was the third most prevalent, and migraine the sixth. In terms of years of life lived with disability, migraine ranked second globally, and was among the ten most disabling disorders in each of the 21 GBD regions. It was particularly burdensome among young and middle-aged women. Unlike many other diseases and injuries quantified in GBD studies, headache showed no clear relation to sociodemographic development, as measured by the Socio-demographic Index. No risk factors have yet been established in the GBD studies for headache disorders, and headache epidemiological studies are absent in many countries and regions.
Implications of all the available evidenceThrough the GBD studies, headache disorders, and in particular, migraine, have been shown to be among the most disabling disorders worldwide. Many fatal and disabling disorders decrease with socioeconomic development, but this does not seem to be true for migraine and tension-type headache. Hence, their relative importance is likely to increase in the future. More high-quality headache epidemiological studies and studies aiming to identify modifiable risk factors should be done. Effective strategies to modify the course of headaches and alleviate pain exist, but many people affected by headache are not benefiting from this knowledge.
Given the importance of headache disorders for global public health, which has become evident through GBD, we wanted to inform an audience of headache specialists about these studies. The aims of the present Article are to provide an overview of the GBD methods as applied to headache, to present detailed results of the update for 19902016 on headache burden in different world regions and with time trends, and to discuss the implications of these results both for future iterations of GBD and for health policies around the world.
Methods
Overview
The main elements of the GBD methods, both general and pertaining to migraine and tension-type headache, are described in the appendix. In the main text of this Article, we concentrate on methods pertaining to estimation of the burden of migraine and tension-type headache. A flowchart of the different steps in these methods is shown in the appendix.
In the GBD cause hierarchy, migraine and tension-type headache are individual disorders on Level 3, under neurological disorders (Level 2) and non-communicable diseases (Level 1). No further subdivision exists for headaches, so each reappears at Level 4. In GBD 2013 and GBD 2015, medication overuse headache was treated as a separate disorder, but in GBD 2016 it was considered a sequela of either migraine or tension-type headache. The burden of medication overuse headache was therefore added to the burdens estimated for these headache types according to a meta-analysis of three studies reporting the proportions of medication overuse headache resulting from migraine (73·4%, 95% uncertainty interval [UI] 63·982·0) or tension-type headache (26·6%, 18·036·1). [46]
In GBD, disease burden is estimated in disability-adjusted life-years (DALYs), which are the sum of years of life lost (YLLs) to premature mortality and years of life lived with disability (YLDs). Because GBD does not estimate any deaths from headache disorders as the underlying cause, DALYs for headaches are equivalent to YLDs. YLDs for each headache disorder are calculated from its prevalence and the mean time patients spend with that type of headache multiplied by the associated disability weight. The determination of headache disability weights through population and internet surveys was on the basis of lay descriptions (appendix). [7, 8] The disability weight for migraine was 0·434, meaning that during an attack the affected person experiences health loss of 43·4% compared with a person in full health. The disability weight for medication overuse headache was 0·223 and for tension-type headache was 0·037. After all diseases were estimated separately, an adjustment was made to YLDs to account for comorbidity by use of simulation methods assuming a multiplicative, rather than additive, model. This adjustment led to a downward correction for YLDs for migraine in women and children by factors ranging from 2·1% (at ages 59 years) to 20·6% (at ages ≥95 years), reflecting a strong correlation between comorbidity and age. The corresponding figures in males were 2·1% and 20·7%, respectively.
Data sources
For headaches, the data sources were mostly published population-based studies of prevalence; however, survey data for which we had the individual record data were also included. The PubMed search terms are shown in the Appendix. Reference lists in published articles were reviewed and data were solicited from our GBD network of more than 2500 collaborators.
Only studies diagnosing the headaches according to the International Classification of Headache Disorders (ICHD) were considered. This classification was first published in 1988, updated in 2004 (ICHD-2), [9] and updated again in 2018 (ICHD-3). [10] In the three ICHD versions, no major differences exist with regard to diagnostic criteria of migraine, tension-type headache, and medication overuse headache. For evaluation of headache burden, these diagnoses were selected because they are, by far, the most common and of the greatest public health importance. [11] Cluster headache causes severe pain and disability, but with a lifetime prevalence of approximately 0·2% the effect on public health is much less. [1] Diagnosis of the many secondary headaches (eg, due to infections or brain tumours) is difficult in epidemiological studies, and the burden of these headaches should be attributed to the underlying disorder. [11] An exception is secondary headache caused by medication overuse, which occurs almost exclusively in patients with either migraine or tension-type headache.
For GBD 2016, data on migraine were extracted from 135 studies, covering 16 of the 21 GBD world regions. For tension-type headache, data were extracted from 76 studies covering 16 GBD regions. All data sources are available online. For medication overuse headache, data were extracted from 37 studies from ten regions (for details about the numbers of studies from each region see the appendix). In addition, hospital claims data from the USA on migraine and tension-type headache for 3 years (2000, 2010, and 2012) were used. [1214] Sets of claims data were included because, owing to their size, they provide more detailed information on age patterns and time trends than published epidemiological studies, and also provide estimates on subnational locations. Because claims data might not be nationally representative, do not refer to the ICHD criteria, and capture only those individuals who are able to seek health care, they are evaluated for systematic biases compared with data sources of high quality (appendix).
Approximately half of the 135 studies from which data were extracted were from three of the 21 GBD regions (western Europe, high-income North America, and high-income Asia Pacific), and no data on any of the headaches were available from the Caribbean, central sub-Saharan Africa, southern sub-Saharan Africa, or Oceania (see appendix) regions. In all regions and countries, prevalence was estimated with a Bayesian meta-regression model (DisMod-MR 2.1), and estimates were obtained in this way also for countries and regions where no relevant headache studies had been done.
Calculation of proportion of time in the symptomatic state
Headache disorders are modelled as chronic episodic conditions. The prevalence reflects the individuals in the population who have had at least one episode in the past 12 months fulfilling ICHD criteria. To calculate the average proportion of time with headache (ie, in the symptomatic state) necessary for YLD calculation, 13 population-based studies were identified that had data on frequency and duration of migraine attacks (appendix). From these studies, we estimated the average number of hours migraineurs spend in attacks, and expressed this as a proportion of a year, which was 8·5% (95% UI 5·811·2).
For tension-type headache, seven studies on duration and frequency of attacks showed that affected people spend, on average, 4·7% (95% UI 1·38·0) of their time with headache. For both migraine and tension-type headache, frequency and duration were reported most commonly in categories, and the midpoint was assumed to represent each category. For medication overuse headache, only one study included in GBD 2016 (from Russia) gave data on time in symptomatic state, reporting a mean headache frequency of 23·1 (SD 6·7) days per month. [15] According to the ICHD-3 definition, medication overuse headache is present on more than 15 days per month for more than 3 months. [10]
Modelling of prevalence
In the mathematical modelling, the mortality due to headache was set at zero, [16] as was occurrence below age 5 years. [17] In the sources used for this study, prevalence rates vary, but the degree to which this reflects real variation across borders and time, or methodological differences, is mostly not known. Method most probably plays a large role because results can be substantially influenced by relatively minor differences, such as variations in the screening question. [18] To adjust for differences in methodological quality, all prevalence studies included in GBD are scored according to a modified version (dichotomised variables) of published methodological quality criteria for headache epidemiological studies, [11] taking into account the representativeness of the population of interest (representative of country or community vs selected population), quality of sampling (random sample of the population of interest vs not random sample), recall period (1year prevalence vs other recall period), participation rate (≥70% vs <70%), survey method (face to face with headache expert or trained interviewer vs other), validation of diagnostic instrument (sensitivity or specificity ≥70% vs <70% or no validation), and application of ICHD criteria (strict criteria or reasonable modification of criteria vs other modification of criteria). In DisMod-MR 2.1, these methodological variables were evaluated for a systematic difference and corrected accordingly (appendix).
Socio-demographic Index (SDI)
We examined the relationships between migraine and tension-type headache DALYs and SDI, a composite measure of income per capita, education, and fertility. [19] We also present results by groupings of countries into quintiles (high SDI, middle-high SDI, middle SDI, middle-low SDI, and low SDI) based on their 2016 SDI value. Additional details on the SDI methods can be found online.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation or the writing of the report. All authors had full access to the data in the study and had final responsibility for the decision to submit for publication.
Results
In 2016, almost three billion individuals were estimated to have a headache disorder: 1·89 billion (95% UI 1·712·10) with tension-type headache and 1·04 billion (95% UI 1·001·09) with migraine (Table). All data on age-standardised prevalence and YLDs for all countries and regions, for both 1990 and 2016, are publicly available in online visualisations and results download tools. For tension-type headache, the global age-standardised prevalence was 26·1% (23·629·0) overall: 30·8% (28·034·0) for women and 21·4% (19·223·9) for men. All results for both sexes are publicly available online. For migraine, global age-standardised prevalence was 14·4% (13·815·0) overall: 18·9% (18·119·7) for women, and 9·8% (9·410·2) for men. Maps of age-standardised prevalence of migraine and tension-type headache in each country are shown in Figure 1, Figure 2. In 2016, the age-standardised prevalence of migraine was highest in Italy and Nepal, and that of tension-type headache was highest in Brazil and Afghanistan. The lowest prevalence of both disorders was in China.
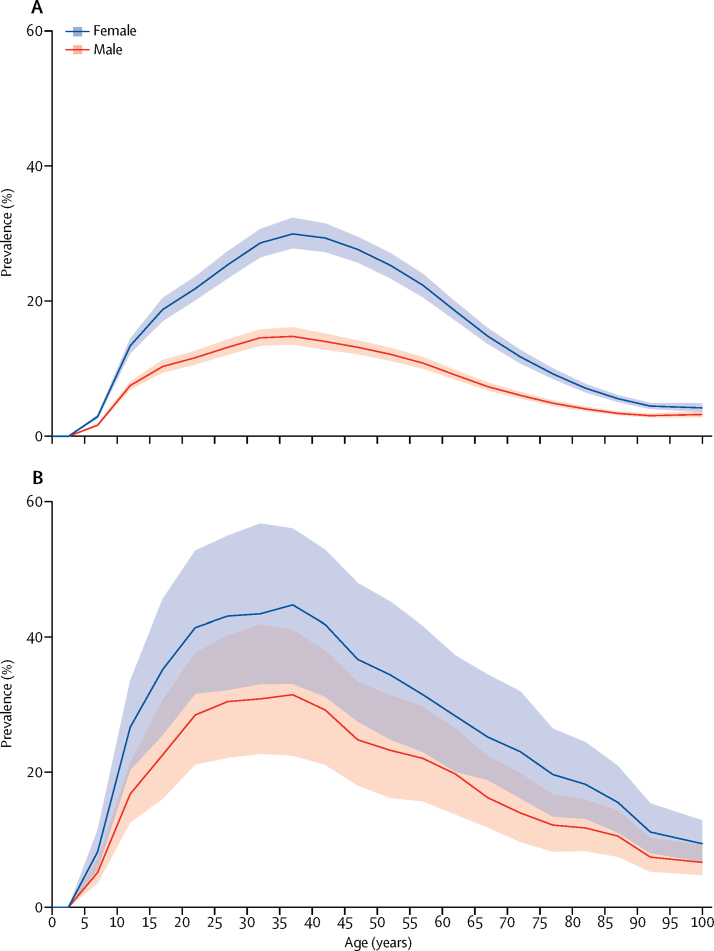
Figure 3
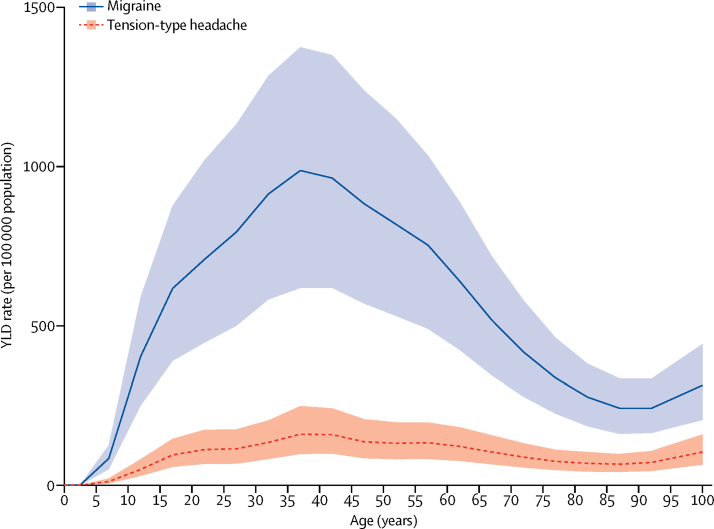
Figure 4
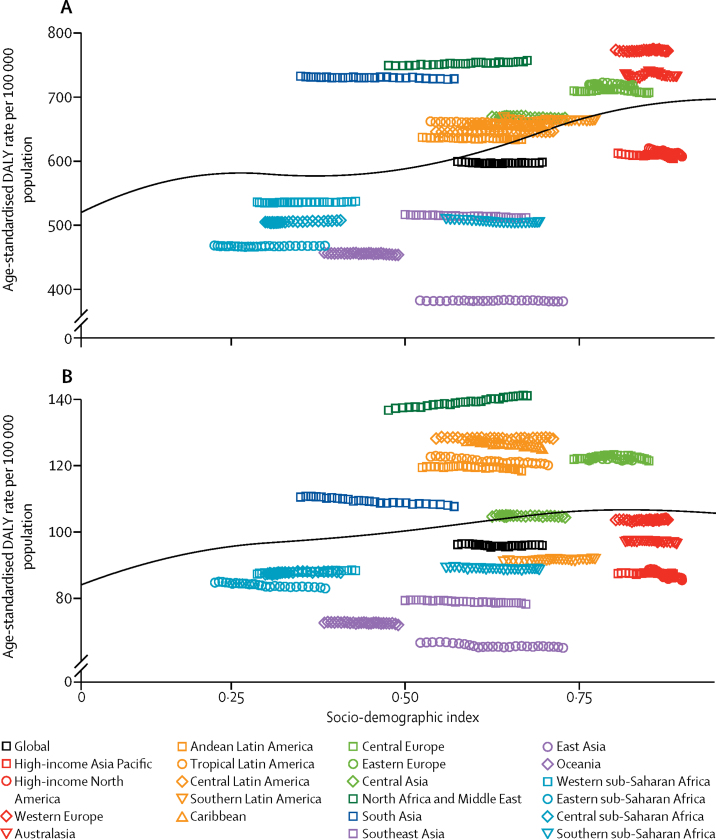
Figure 5 Migraine was estimated to have caused 45·1 million (95% UI 29·062·8) YLDs in 2016 (table), an increase of 51·2% (49·752·8) from the 29·8 million (19·141·8) YLDs in 1990 (see online results tool). Tension-type headache caused 7·2 million (4·610·5) YLDs in 2016 (table), an increase of 53·1% (47·558·4) from the 4·7 million (3·07·0) YLDs in 1990 (online results tool). Together, in 2016, migraine and tension-type headache caused 52·3 million (34·572·5) YLDs globally, which was 6·5% of all YLDs: 7·7% among women and 5·1% among men. The global age-standardised YLD rates per 100?000 population for migraine were 598·7 (95% UI 385·9833·3). The change from the 1990 values was 0·2% (0·8 to 0·4). For tension-type headache, the global age-standardised YLD rate per 100?000 population was 95·9 (61·5140·0), a change of 0·2% (2·5 to 1·9) from 1990 values. The age-standardised YLD rates in 2016 of both disorders were higher in women (migraine 777·6, 500·41083·6; tension-type headache 114·6, 73·6162·4) than in men (migraine 422·3, 274·3586·7; tension-type headache 77·4, 49·6113·2). The percentage of all YLDs due to migraine were 5·6% (4·07·2) overall: 6·8% (4·98·8) for women and 4·3% (3·15·5) for men. The corresponding values for tension-type headache were 0·9% (0·71·2) overall: 1·0% (0·71·3) for women and 0·8% (0·61·0) for men.
For both migraine and tension-type headache, a peak in prevalence and YLD rate occurred between ages 35 and 39 years (Figure 3, Figure 4). In both sexes, the percentages of all YLDs were highest in the group aged 1549 years (migraine 8·2%, tension-type headache 1·3%), but was also high in children aged 514 years (migraine 4·5%, tension-type headache 0·6%), in individuals aged 5069 years (migraine 4·2%, tension-type headache 0·7%), and in the elderly (ie, ≥70 years; migraine 1·3%, tension-type headache 0·3%). In women between ages 15 and 49 years, migraine caused 20·3 million (95% UI 12·928·5) and tension-type headache caused 2·9 million (95% UI 1·84·2) YLDs in 2016, which together were 11·2% of all YLDs in this age and sex group. The proportions of all DALYs for both sexes were 1·9% (1·32·5) for migraine and 0·3% (0·20·4) for tension-type headache. The values were 2·7% (1·83·6) and 0·4% (0·30·5) for women, and 1·2% (0·81·7) and 0·2% (0·30·3) for men. Globally, migraine ranked 12th of all disorders at GBD cause Level 4 in terms of DALYs for both sexes in 2016, up from 17th in 1990. In 2016, migraine ranked fifth for women (up from 13th in 1990), and 20th for men (up from 28th in 1990).
Migraine was among the top five Level 4 causes of age-standardised YLDs in all five SDI quintiles both in 1990 and 2016. Age-standardised DALYs for each headache type showed a small increase as SDI increased. The values estimated for the 21 world regions between 1990 and 2016 varied little over time, but markedly between regions (Figure 5). These results indicate that the SDI level of the country is not a major determinant of the size of the headache burden.
Discussion
Almost three billion people had a migraine and tension-type headache together in 2016; tension-type headache was the third most prevalent disorder (after dental caries and latent tuberculosis infection) and migraine the sixth most prevalent out of 328 diseases and injuries for which GBD 2016 made estimates. [20]
GBD 2016 shows that headache, and in particular, migraine, is one of the main causes of disability worldwide, particularly in young adult and middle-aged women (figure 3). Globally, migraine and tension-type headache together accounted for 6·5% of all YLDs: 7·7% among women and 5·1% among men. Headache is particularly burdensome in people aged 1549 years, being the cause of 9·5% of all YLDs in this group (11·2% among women and 7·5% among men) but the effect is not negligible in the group aged 514 years (5·1%), or among the group aged 5069 years (4·9%), and the group aged 70 years or older (1·6%). Together the two disorders are the cause of more than 2% of all DALYs: almost 3% in women and almost 1·5% in men.
When analysed at cause Level 4, migraine was the second cause of disability after low back pain and ranked among the top ten causes of YLDs (age-standardised) in all 195 countries, both in 1990 and in 2016. [20] In 2016, it ranked first in two regions, second in nine, third in five, fourth in two, fifth in two, and sixth in one region. Globally, tension-type headache ranked 28th in both 1990 and 2016.
The increase in YLDs between 1990 and 2016 reflects population growth and potentially some effect of a change in the age composition of many populations (ie, fewer children and adolescents and more middle-aged people). The fact that age-standardised YLD rates are unchanged indicates that, overall, the underlying causes of headache have remained the same. Any improvements in the efficacy of headache treatments during this period (which saw the introduction of triptans for migraine) have had no detectable effectperhaps partly a reflection of how poorly available they are worldwide [21] and of the scarcity of data on the proportion of time patients are symptomatic, which did not allow us to find a treatment effect over time and by location. In the DALY rankings, headaches are higher in 2016 than in 1990, because of an overall decrease in YLLs from fatal disorders. In general, DALY rates for non-communicable diseases increase rapidly with age; [22] hence, counts of deaths and DALYs from non-communicable diseases will increase in ageing populations. However, ageing has a lesser effect on headaches as these, and in particular migraine, are most common among young and middle-aged adults, and become less prevalent with old age.
The principal reason migraine has climbed from the seventh largest cause of YLDs in GBD 2015 to second place in GBD 2016 [20, 23] is that medication overuse headache used to be treated as a separate disease entity, but in GBD 2016 it was considered a sequela of either migraine or tension-type headache, with more than 70% of medication overuse headache burden being reattributed to migraine. We believe this change in the status of medication overuse headache is correct, from both clinical and pathophysiological viewpoints, because medication overuse headache virtually never develops de novo, but almost always from either migraine or tension-type headache, and the presence of a primary headache is considered to be a prerequisite for medication overuse headache. [10, 24]
A short supply of data is still a limitation in headache burden estimates. Although several epidemiological studies on headache have been done in the past decade in large and populous regions of the world where none existed before (ie, Russia, China, India, and parts of Africa), the majority of studies are still from high-income countries, and there remain five regions of low-income and middle-income countries without data for migraine. No data exist for populous countries like Indonesia, Vietnam, Bangladesh, Egypt, South Africa, and the Democratic Republic of Congo. In sub-Saharan Africa, only five countries have data on headache. For tension-type headache and medication overuse headache, the data are even scarcer. In addition, too few population-based studies give good estimates of average headache duration and frequency, which are necessary for calculation of time spent in the symptomatic state. The small number of studies did not allow us to differentiate the estimates of time spent with symptoms by location, although, in countries with better access to health care, the frequency and duration of migraine attacks would be expected to decrease with treatment. There is also a need to update results in many places, to get more reliable results (many old studies are of low quality) and possibly also to monitor secular trends in headache epidemiology. Because data on headache are poorly captured in national health surveys, and administrative data collections such as those from claims or primary care are unreliable measures of prevalence (appendix), it is desirable that surveys on headache be done in many more places, and preferably at regular intervals as part of national health reporting systems.
In GBD, DisMod-MR 2.1 makes it possible to adjust results of studies that were done using suboptimal case definitions or methods. However, an important aspect that has not yet been taken into account in the model is the distinction between definite and probable diagnoses of migraine and tension-type headache. People with a definite diagnosis fulfil all ICHD diagnostic criteria for the disorder, whereas those with probable diagnoses do not meet one of them; the probable diagnosis is not meant to signify a separate nosological entity. In a clinical setting, probable diagnoses are useful for patients for whom there is diagnostic uncertainty, but confirmation (or refutation) of the diagnosis is expected later. However, this will not be the case in epidemiological studies and, unless the large number of probable cases are included for either migraine or tension-type headache as appropriate, these people will not be counted, despite experiencing headache-related disability. Several studies have investigated, in more detail, participants in epidemiological studies who received probable diagnoses. In the great majority, a definite diagnosis of migraine was withheld because attacks reportedly lasted less than 4 h (the minimum allowed by the criteria). [2527] Otherwise, the diagnosis resembled migraine closely, and was associated with considerable disability. Until 2000, the majority of studies reported only definite migraine, and not both definite and probable diagnoses. After 2000, more studies reported both types, and these studies indicate that the prevalence of probable migraine is almost as high as that of definite migraine. [26, 28] Future iterations of GBD should therefore find a reasonable and consistent way to deal with probable migraine because it is a common cause of disability that otherwise will be unaccounted for. Similar arguments can be made for probable tension-type headache, although knowledge of this headache type is far less, and the YLDs missed by omitting this are fewer because of the much lower disability weight of tension-type headache compared with migraine.
Another problem is the handling of chronic headache disorders (ie, present on 15 or more days per month for more than 3 months). Many of these headaches will fall into the categories of chronic migraine, chronic tension-type headache, or medication overuse headache, but the high frequency of headaches tends to blur the features necessary for diagnosis. These headaches become even more difficult to diagnose with certainty in cross-sectional epidemiological studies based on questionnaires, especially when these are self-administered or applied by lay interviewers. With the exception of medication overuse headache, which is diagnosed by enquiry into medication use, these headaches are usually lumped into a descriptive category of headache on 15 or more days per month, and not counted in GBD. Hence, there might be additional, and perhaps considerable, headache-related morbidity that is not captured by the diagnoses used in GBD.
Despite efforts to adjust for methodological differences between studies, part of the variation between countries might be due to residual measurement error, rather than true variation. Efforts have been made to standardise the methods for studies on prevalence and burden of headache, [11] and in the future adherence to these will hopefully make it easier to compare the burden over geographical borders and time periods. One of the greater challenges in modelling headache is the poor knowledge of predictors. Such predictors help to stabilise disease models in the sense that they adjust data points that are affected by measurement error.
Another problem concerns how to estimate the proportion of time during which people with a headache disorder actually have headache (time in symptomatic state). This difficulty exists partly because average duration and frequency of headaches are usually reported in categories, and estimates thus depend on choice of mean value in each category, and partly because the present figures rely on older studies that are of rather poor general quality. Better estimates can probably be obtained with a more systematic analysis of individual record data in some of the major surveys done in the past 10 years that are of higher quality than earlier studies.
Despite these methodological challenges, headache disorders are ubiquitous and contribute to a large burden of lost health. Sizeable resources would be needed to prevent or alleviate this burden in the hundreds of millions of people with headache worldwide. Until now, most interventions have aimed at the management of symptoms, but preferable for such an immense public health problem might be modification at a population level of risk factors, if such can be identified. This intervention would require greater knowledge of the modifiable factors that drive headache: several have been suggested with varying degrees of scientific support, such as obesity, smoking, indoor and outdoor air pollution, level of physical activity, altitude, blood pressure, and level of stress. [2932] Of these factors, altitude and stress are not included as risks in GBD. For the other postulated risks, the evidence for an effect on headaches is, in our opinion, insufficient. Potential headache risk factors should be tested against GBD causal criteria for inclusion of risks and associated outcomes. [33] If none of these risk factors pass the criteria, more and better epidemiological and pathophysiological studies should be done to prove or refute hypotheses about causation.
Headache disorders do not appear to be strongly linked to socioeconomic development, as measured by SDI (table). The previous notion that headache was mainly a disorder of high-income countries and particularly prevalent among the wealthy, is refuted by the present study, but neither is the opposite true. Hence, no significant reduction in the global burden of headache can be expected from the demographic and epidemiological transitions [22] that large parts of the world are presently undergoing, because no clear pattern of decreasing YLD rate with increasing SDI exists. It can, however, be predicted that the relative importance of headaches will further increase as the importance of other disorders, such as malnutrition, infections, maternal and child diseases, and cardiovascular and other fatal non-communicable disorders decreases. Although a socioeconomic index like the SDI does not reflect differences in headache prevalence when applied across countries and cultures, the possibility that such factors are important within a country or region cannot be eliminated. A socioeconomic gradient, to the effect that low socioeconomic status is linked to higher headache prevalence, has been shown in countries of high, middle, and low income. [15, 3436]
Even if it proves difficult to establish, with reasonable certainty, that modifiable risk factors exist for headache, the results of GBD definitely give a strong call for improving health care for headache. This call involves the inclusion of headache care in existing health-care systems, and not only in the high-income part of the world. Implementation of a headache service in Georgia, a country where none existed previously, has been economically sustainable. [37] An educational programme among general practitioners in Estonia has been shown to reduce unnecessary referrals to specialists and special examinations. [38] A programme to increase competence in headache care in China is now being implemented. [39] Some simple remedies and methods, like aspirin for attack treatment and amitriptyline for prevention of migraine, together with provision of information for patients and education for health-care providers, should be highly cost-effective in low-income and middle-income countries. [40] A study from European and Latin American countries has shown that discontinuation of medication overuse can reduce the proportion of severely disabled patients with medication overuse headache by almost 60%. [41] This study also indicates that increased awareness of the danger of non-critical use of acute medication might prevent millions of people from developing this prevalent and disabling disorder.
In high-income parts of the world, the results presented here also highlight a strong moral obligation to allocate more resources to research aimed at understanding the mechanisms of headache to enable development of more effective prevention and treatments. At the same time, current treatments need to be recognised as ineffective more because of poor availability than inefficacy, and health services must do a better job of reaching people if new treatments are to have an effect. [42] For the pharmaceutical industry, the market for proven cost-effective remedies is huge, as is the potential for a large decrease in pain and disability, and an increase in productivity, for the global community.
In conclusion, major limitations still exist in the GBD headache burden estimations, the most notable being the short supply of epidemiological data from large parts of the world, the paucity of studies giving data on average time with headache, and great methodological heterogeneity. Nevertheless, GBD 2016 confirms that headache, and in particular, migraine, is a large public health problem in both sexes and all age groups worldwide, but most so in young and middle-aged women. Headache is not limited to the high-income part of the world and, unless action is taken, it is here to stay: there is no indication that the demographic and epidemiological transitions alone will improve the situation. Rather, these profound changes which reduce mortality will increase the relative importance of headache for public health.
Supplementary Material
GBD 2016 Headache Collaborators
Lars Jacob Stovner, Emma Nichols, Timothy J Steiner, Foad Abd-Allah, Ahmed Abdelalim, Rajaa M Al-Raddadi, Mustafa Geleto Ansha, Aleksandra Barac, Isabela M Bensenor, Linh Phuong Doan, Dumessa Edessa, Matthias Endres, Kyle J Foreman, Fortune Gbetoho Gankpe, Gururaj Gopalkrishna, Alessandra C Goulart, Rahul Gupta, Graeme J Hankey, Simon I Hay, Mohamed I Hegazy, Esayas Haregot Hilawe, Amir Kasaeian, Dessalegn H Kassa, Ibrahim Khalil, Young-Ho Khang, Jagdish Khubchandani, Yun Jin Kim, Yoshihiro Kokubo, Mohammed A Mohammed, Maziar Moradi-Lakeh, Huong Lan Thi Nguyen, Yirga Legesse Nirayo, Mostafa Qorbani, Anna Ranta, Kedir T Roba, Saeid Safiri, Itamar S Santos, Maheswar Satpathy, Monika Sawhney, Mekonnen Sisay Shiferaw, Ivy Shiue, Mari Smith, Cassandra E I Szoeke, Nu Thi Truong, Narayanaswamy Venketasubramanian, Kidu Gidey Weldegwergs, Ronny Westerman, Tissa Wijeratne, Bach Xuan Tran, Naohiro Yonemoto, Valery L Feigin, Theo Vos, Christopher J L Murray.
Contributors
LJS prepared the first draft. TJS, EN, and TV analysed the data and edited the first draft and final versions of the Article. LJS finalised all drafts, and approved the final version of the Article. All other authors provided data, developed models, reviewed results, provided guidance on methodology, or reviewed the Article, and approved the final version.
Declaration of interests
CEIS reports grants from the National Health and Medical Research Council, during the study; and grants from Lundbeck and the Alzheimer's Association, outside the submitted work. CEIS also reports the patent PCT/AU2008/001556. All other authors declare no competing interests.
References:
Stovner LJ, Hagen K, Jensen R.
The global burden of headache: a documentation of headache prevalence and disability worldwide.
Cephalalgia. 2007;27:193210WHO . World Health Organization;
Geneva: 2001. The World Health Report 2001.
http://www.who.int/whr/2001/en/index.htmlSteiner TJ, Stovner LJ, Vos T.
GBD 2015: migraine is the third cause of disability in under 50s.
J Headache Pain. 2016;17:104Katsarava Z, Muessig M, Dzagnidze A, Fritsche G, Diener HC, Limmroth V.
Medication overuse headache: rates and predictors for relapse in a 4-year prospective study.
Cephalalgia. 2005;25:1215Jonsson P, Hedenrud T, Linde M.
Epidemiology of medication overuse headache in the general Swedish population.
Cephalalgia. 2011;31:10151022Colas R, Munoz P, Temprano R, Gomez C, Pascual J.
Chronic daily headache with analgesic overuse: epidemiology and impact on quality of life.
Neurology. 2004;62:13381342Salomon JA, Vos T, Hogan DR.
Common values in assessing health outcomes from disease and injury:
disability weights measurement study for the Global Burden of Disease Study 2010.
Lancet. 2012;380:21292143Salomon JA, Haagsma JA, Davis A.
Disability weights for the Global Burden of Disease 2013 study.
Lancet Glob Health. 2015;3:e712e723Classification Subcommittee of the International Headache
Society The international classification of headache disorders, 2nd edn.
Cephalalgia. 2004;24(suppl 1):1160Headache Classification Committee of the International Headache
Society The International Classification of Headache Disorders, 3rd edn.
Cephalalgia. 2018;38:1211Stovner LJ, Al Jumah M, Birbeck GL.
The methodology of population surveys of headache prevalence, burden and cost:
principles and recommendations from the Global Campaign against Headache.
J Headache Pain. 2014;15:5Truven Health Analytics;
Ann Arbor: 2000. United States MarketScan Claims and Medicare Data.Truven Health Analytics;
Ann Arbor: 2010. United States MarketScan Claims and Medicare Data.Truven Health Analytics;
Ann Arbor: 2012. United States MarketScan Claims and Medicare Data.Ayzenberg I, Katsarava Z, Sborowski A.
The prevalence of primary headache disorders in Russia: a countrywide survey.
Cephalalgia. 2012;32:373381Asberg AN, Stovner LJ, Zwart JA, Winsvold BS, Heuch I, Hagen K.
Migraine as a predictor of mortality: The HUNT study.
Cephalalgia. 2016;36:351357Wober-Bingol C.
Epidemiology of migraine and headache in children and adolescents.
Curr Pain Headache Rep. 2013;17:341Hagen K, Zwart JA, Aamodt AH.
A face-to-face interview of participants in HUNT 3: the impact of the screening
question on headache prevalence.
J Headache Pain. 2008;9:289294GBD 2016 Mortality Collaborators Global, regional, and national under-5 mortality,
adult mortality, age-specific mortality, and life expectancy, 19702016:
a systematic analysis for the Global Burden of Disease Study 2016.
Lancet. 2017;390:10841150GBD 2016 Disease and Injury Incidence and Prevalence Collaborators Global,
regional, and national incidence, prevalence, and years lived with disability for 328 diseases
and injuries for 195 countries, 19902016: a systematic analysis for the Global Burden of Disease Study 2016.
Lancet. 2017;390:12111259WHO and Lifting The Burden .
In: ATLAS of headache disorders and resources in the world 2011.
Saxena S, Dua T, Saraceno B, editors.
World Health Organization; Geneva: 2011.Hay SI, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F et al (2017)
Global, Regional, and National Disability-adjusted Life-years (DALYs) for 333 Diseases and Injuries
and Healthy Life Expectancy (HALE) for 195 Countries and Territories, 19902016:
A Systematic Analysis for the Global Burden of Disease Study 2016
Lancet. 2017 (Sep 16); 390 (10100): 12601344Vos T Allen C Arora M et al.
Global, Regional, and National Incidence, Prevalence, and Years Lived
with Disability for 310 Diseases and Injuries, 1990-2015: a Systematic
Analysis for the Global Burden of Disease Study 2015
Lancet. 2016 (Oct 8); 388 (10053): 15451602Diener HC, Holle D, Solbach K, Gaul C.
Medication-overuse headache: risk factors, pathophysiology and management.
Nat Rev Neurol. 2016;12:575583Kim BK, Chung YK, Kim JM, Lee KS, Chu MK.
Prevalence, clinical characteristics and disability of migraine and probable migraine:
a nationwide population-based survey in Korea.
Cephalalgia. 2013;33:11061116Lanteri-Minet M, Valade D, Geraud G, Chautard MH, Lucas C.
Migraine and probable migraineresults of FRAMIG 3, a French nationwide survey
carried out according to the 2004 IHS classification.
Cephalalgia. 2005;25:11461158Arruda MA, Guidetti V, Galli F, Albuquerque RC, Bigal ME.
Primary headaches in childhooda population-based study.
Cephalalgia. 2010;30:10561064Patel NV, Bigal ME, Kolodner KB, Leotta C, Lafata JE, Lipton RB.
Prevalence and impact of migraine and probable migraine in a health plan.
Neurology. 2004;63:14321438Robberstad L, Dyb G, Hagen K, Stovner LJ, Holmen TL, Zwart JA.
An unfavorable lifestyle and recurrent headaches among adolescents:
the HUNT study.
Neurology. 2010;75:712717Westergaard ML, Glumer C, Hansen EH, Jensen RH.
Medication overuse, healthy lifestyle behaviour and stress in chronic headache:
results from a population-based representative survey.
Cephalalgia. 2016;36:1528Winsvold BS, Hagen K, Aamodt AH, Stovner LJ, Holmen J, Zwart JA.
Headache, migraine and cardiovascular risk factors: the HUNT study.
Eur J Neurol. 2011;18:504511Linde M, Edvinsson L, Manandhar K, Risal A, Steiner TJ.
Migraine associated with altitude: results from a population-based study in Nepal.
Eur J Neurol. 2017;24:10551061GBD 2016 Risk Factors Collaborators Global, regional, and
national comparative risk assessment of 84 behavioural, environmental and occupational,
and metabolic risks or clusters of risks, 19902016: a systematic analysis for the
Global Burden of Disease Study.
Lancet. 2016;390:13451422Hagen K, Vatten L, Stovner LJ, Zwart JA, Krokstad S, Bovim G.
Low socio-economic status is associated with increased risk of frequent headache:
a prospective study of 22718 adults in Norway.
Cephalalgia. 2002;22:672679Lipton RB, Bigal ME.
The epidemiology of migraine.
Am J Med. 2005;118(suppl 1):3S10SGururaj G, Kulkarni GB, Rao GN, Subbakrishna DK.
Prevalence and sociodemographic correlates of primary headache disorders:
results of a population-based survey from Bangalore, India.
Indian J Public Health. 2014;58:241248Giorgadze G, Mania M, Kukava M.
Implementation of effective, self-sustaining headache services in the Republic
of Georgia: evaluation of their impact on headache-related disability and
quality of life of people with headache.
Cephalalgia. 2018;38:639645Braschinsky M, Haldre S, Kals M.
Structured education can improve primary-care management of headache:
the first empirical evidence, from a controlled interventional study.
J Headache Pain. 2016;17:24Yu S, Steiner TJ.
Lifting the burden of headache in China: managing migraine in a SMART way.
J Headache Pain. 2017;18:79Linde M, Steiner TJ, Chisholm D.
Cost-effectiveness analysis of interventions for migraine in four low- and
middle-income countries.
J Headache Pain. 2015;16:496Bendtsen L, Munksgaard S, Tassorelli C.
Disability, anxiety and depression associated with medication-overuse headache
can be considerably reduced by detoxification and prophylactic treatment.
Results from a multicentre, multinational study (COMOESTAS project)
Cephalalgia. 2014;34:426433Steiner TJ, Stovner LJ, Vos T, Jensen R, Katsarava Z.
Migraine is first cause of disability in under 50s:
will health politicians now take notice?
J Headache Pain. 2018;19:17
Return to GLOBAL BURDEN OF DISEASE
Since 11-21-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |