The Global Burden of Selected Occupational Diseases
and Injury Risks: Methodology and SummaryThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: American J Industrial Medicine 2005 (Dec); 48 (6): 400-418 ~ FULL TEXT
Deborah Imel Nelson, PhD, Marisol Concha-Barrientos, MD, DrPH, Timothy Driscoll, MB, BS, PhD et. al.
Protection of the Human Environment,
World Health Organization,
Geneva, Switzerland.
BACKGROUND: Around the globe, work has a heavy impact on health. To better advise policy makers, we assessed the global burden of disease and injury due to selected occupational hazards. This article presents an overview, and describes the methodology employed in the companion studies.
METHODS: Using the World Health Organization (WHO) Comparative Risk Assessment methodology, we applied relative risk measures to the proportions of the population exposed to selected occupational hazards to estimate attributable fractions, deaths, and disability-adjusted life years (DALYs). Numerous occupational risk factors had to be excluded due to inadequate global data.
RESULTS: In 2000, the selected risk factors were responsible worldwide for 37% of back pain, 16% of hearing loss, 13% of chronic obstructive pulmonary disease (COPD), 11% of asthma, 8% of injuries, 9% of lung cancer, and 2% of leukemia. These risks at work caused 850,000 deaths worldwide and resulted in the loss of about 24 million years of healthy life. Needlesticks accounted for about 40% of Hepatitis B and Hepatitis C infections and 4.4% of HIV infections in health care workers.
There is more like this at our
Global Burden of Disease PageCONCLUSIONS: Exposure to occupational hazards accounts for a significant proportion of the global burden of disease and injury, which could be substantially reduced through application of proven risk prevention strategies.
KEY WORDS: burden of disease; occupational health; DALYs; comparative risk assessment; health impact assessment
From the FULL TEXT Article:
INTRODUCTION
Global Burden of Disease
The World Health Organization’s (WHO) ongoing Global Burden of Disease (GBD) project provides the most comprehensive and consistent estimates of mortality and morbidity for more than 135 causes of disease and injury. WHO recently conducted a Comparative Risk Assessment (CRA) to estimate the global burden of disease and injuries resulting from seven major categories of risk factors: childhood and maternal under-nutrition, other diet-related risk factors and physical inactivity, sexual and reproductive health, addictive substances, environmental risks, selected occupational risks, and other risks to health [WHO, 2002; Ezzati et al., 2004]. These categories were comprised of 26 specific risk factors. A consistent WHO methodology was used throughout the project so that the impacts of these risk factors could be compared. The major purpose of the CRA was to improve the evidence base on distribution and costs of diseases and injuries by risk factor, to support rational health policy decisions worldwide. All estimates were stratified by age, gender, and WHO subregions. The GBD is thus a summary of the health outcomes (death and disability), estimated by age, gender, and WHO subregion. The CRA is an estimate of these health outcomes owing to exposures to the various risk factors, again estimated by age, gender, and WHO subregion.
The 191 Member States are divided by WHO into six geographical regions (Africa, Americas, Europe, Eastern Mediterranean, Southeast Asia, and Western Pacific). These regions have been further subdivided into five mortality strata (A-E) on the basis of levels of child mortality under 5 years of age and 15-59-year-old male mortality [WHO, 2002], resulting in 14 epidemiological subregions (see Fig. 1). As an example, America A, which consists of Canada, Cuba, and the United States, has very low child and very low adult mortality. This convention is used throughoutWHO in cause of death analyses, burden of disease analyses, and comparative risk assessments.
Various measures have been developed to quantify population health, but the most useful for the WHO GBD studies are disability-adjusted life years (DALYs). This is a summary measure, which calculates the years lost from ideal lifespan due to morbidity and premature mortality. The DALY thus represents the gap between the current situation, and an ideal situation where everyone achieves standard life expectancy (per theWHOstandard, 82.5 years for women, 80 years for men) in perfect health. Use of the maximum average lifespan seen globally for all countries also facilitates interregional comparisons. A major benefit of calculating the disease burden in terms of DALYs is that it combines mortality and morbidity in a single measure, which considers only age and gender, and is independent of economic considerations, such as financial costs of disease or value of human life.
Comparative Risk Assessment
The heart of CRA is determining the number of DALYs and deaths attributable to exposure to the various risk factors, in a manner that allows comparisons to be made. This determination is based on attributable fractions, that is, the proportion of the incidence of a given health outcome in a given population that is identified as due to a given exposure [Pruss-Ustun et al., 2003]. Attributable fractions of a health outcome were calculated from estimates of the proportion of a population exposed to a risk factor (at various levels, if possible), combined with relative risks of disease or death due to that health outcome resulting from that exposure. The total number of deaths and/or DALYs attributable to the given exposure was then determined by multiplying the attributable fraction by the number of deaths and/or DALYs estimated by WHO for the relevant health outcome in the Global Burden of Disease analysis [e.g.,WHO, 2004]. These calculations were conducted by age, gender, and subregion. This single method was used throughout WHO in attributing the global burden of disease to the 26 risk factors under study [Ezzati et al., 2004]. Use of a consistent methodology for all risk factors allows comparisons and rankings to be made among them, thus providing further guidance for policy makers in weighing the merits of various interventions.
The resulting attribution of the global burden of disease, quantified as the number of deaths and disability-adjusted life years (DALYs) for each risk factor, by age, gender, and subregion, is summarized in The World Health Report 2002: Reducing Risks, Promoting Health Life [WHO, 2002], and more fully described in ComparativeQuantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors [Ezzati et al., 2004].
Previous Studies
Previous attempts have been made to quantify the burden of occupational disease and injury on a state-wide [Oleinick et al., 1993], national [e.g., Leigh et al., 1997, 2003; Loewenson, 1999; Nurminen and Karjalainen, 2001; Steenland et al., 2003], or global level [e.g., Murray and Lopez, 1997; Leigh et al., 1999; Takala, 1999].With few exceptions [e.g., Nurminen and Karjalainen, 2001], these studies have not been exposure-based. In 1999, Leigh et al. reported on a WHO study of the 1994 global burden of occupational disease and injury in which both direct and indirect methods were utilized. In the direct approach, injuries and fatalities were determined using all available published data. Where data were not available, estimates were made using calculated injury or mortality rates for comparable countries or groups of countries. Occupational disease incidence and mortality in absolute terms were also determined from all available published data, and where data were not available, by applying mean rates from like groups of countries. In the indirect approach, incidence rates for occupational disease from Finland were applied at the regional level; similarly, injury rates were based on Australian incidence rates. These rates were applied without adjustment for established market economies and former socialist economies of Europe, and were doubled for less developed economies. We are not aware of any other exposure-based studies of the global burden of occupational disease and injury.
Global Burden of Occupational Disease
Using the WHO CRA methodology, we assessed the global burden of occupational disease and injury resulting from four selected risk factors for which there were adequate data: occupational carcinogens, airborne particulates, noise, and ergonomic stressors. Owing to the lack of universal data on exposure to occupational hazards, our exposure assessment was based on national and regional data on the participation of the population in the work force, where people work, and the kinds of work they do. Risk estimates, including relative risks and mortality rates, were derived primarily from data from developed countries, adapted as appropriate to developing countries. Attributable fractions for occupational diseases and injuries were calculated by age, sex, and subregion, and were used to determine the number of deaths and DALYs resulting from exposure to selected occupational risk factors. Data limitations meant that two of our additional occupational analyses—injuries, and infections due to needlestick injuries in health workers—could not be based on the full CRA methodology.
Excluded Exposures and Outcomes
The criteria for selection of risk factors for this study included widespread exposures, adequacy of exposure information, applicability of health outcome data to all regions of the globe, and the inclusion of the relevant health outcomes in the GBD database of diseases and injuries [Ezzati et al., 2004]. These strict criteria precluded analysis of respiratory diseases other than chronic obstructive pulmonary disease (COPD), asthma, and pneumoconioses; some infectious diseases; less widespread cancers and carcinogens; musculoskeletal disorders other than low back pain; intentional injuries in the workplace; organ and systemic diseases resulting from occupational exposure to solvents, pesticides and heavy metals; maternal and perinatal conditions resulting from occupational exposures; skin disorders; coronary heart disease, and other outcomes associated with work-related stress. Child labor could not be considered due to the lack of consistent national definitions for the youngest ages included in the labor force, as well as lack of exposure and relative risk information on children.
Summary
This article describes the general methodology used to assess the burden of disease and injury resulting from exposure to selected occupational risk factors, and provides overall results. The companion studies provide further detail on the impacts of exposure to occupational carcinogens [Driscoll et al., 2005a], airborne particulates [Driscoll et al., 2005b], noise [Nelson et al., 2005], ergonomic stressors [Punnett et al., 2005], risk factors for injuries [Concha- Barrientos et al., 2005], and sharps injuries among health care workers [Pruss-Ustun et al., 2005]. Driscoll et al. [2005c] address the total impact of occupational hazards, including factors that could not be considered in this study, and compare our results with previous attempts to quantify the global burden of occupational disease and injury.
MATERIALS AND METHODS
Comparative Risk Assessment Methodology
The CRA sought to answer three questions: what is the global burden of disease and injury, apportioned by age, sex, and WHO subregion; what fraction of that burden is attributable to exposure to specific risk factors, and how much of that burden can be avoided by reducing exposures to those risk factors. For further explanation of attributable and avoidable burdens and DALYs, see Pruss-Ustun et al. [2003].
Global burden of disease and injury statistics
A ‘‘burden of disease’’ study estimates the gaps between current population health and a normative goal for population health, for a comprehensive set of disease and injury causes, and for major risk factors. The World Health Organization maintains statistics on deaths and DALYs for more than 135 diseases and injuries, apportioned by age, sex, and subregion, which constituted the list of health outcomes that could be included in the Comparative Risk Assessment study [Mathers et al., 2002].
Disability adjusted life years (DALYs) are a function of age of onset of a health effect or premature mortality, duration of the disability or time lost due to premature mortality, disability weighting, age-weighting corrections, and a discount rate (see Murray [1994] for the full equation). These latter terms account for the fact that societies seem to value a healthy year of life of a young adult more than of a young child or elderly person [Murray, 1996; Pruss-Ustun et al., 2003]. DALYs combine mortality and morbidity in a single term:DALY = Σ (YLL and YLD) (1)
where:
YLL = years of life lost due to premature mortality, and
YLD = the (weighted) years lived with a disability.
The basic formula for calculating YLD is:YLD = 1 x DW x L (2)
where:
I = the number of incident cases in the reference period,
DW = the disability weight (zero to 1), and
L = the average duration of disability in years [Mathers et al., 2002].
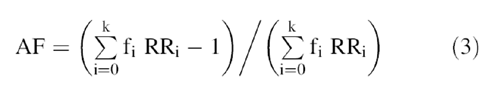
WHO uses a wide range of data sources to estimate YLD from various causes, including disease registers, population surveys, epidemiological studies, and health facility data. Disability weights are developed in collaboration with Member States by methods including general and specific population surveys.Attributable fraction. Determining the fraction of the burden attributable to specific risk factors requires input on current (or relevant past) exposures to the risk factor and on the risk factor-disease relationships. To calculate the attributable fraction (AF) of deaths or DALYs due to exposure to a specific health risk factor, the estimates of the proportion of a population (fi) exposed to the risk factor at k levels of exposure, and the relative risks of morbidity and/or mortality from a specific adverse health effect due to that exposure (RRi) are combined in Equation 3. Although aCRA analysis can be conducted with only two levels of exposure, for example, ‘‘nonexposed’’ and ‘‘exposed,’’ smaller values of k may compromise accuracy of the analysis.
The AF is then multiplied by the WHO estimates of deaths or DALYs due to that health outcome, to determine the number of deaths or DALYs attributable to the risk factor. These estimates are made by gender and age, globally and within each of the 14 WHO subregions.
Avoidable burden. Determining how much of the burden can be avoided by reducing exposures to the risk factors requires information on the counterfactual distribution of exposure, and on the rate of risk reversal once exposure has ceased. The counterfactual distribution is a WHO convention for an exposure distribution which will result in the lowest rate of adverse health effects. WHO assigns the term ‘‘theoretical minimum’’ exposure to the exposure level that results in the minimum level of adverse health outcome. The theoretical minima for each risk factor are described in the companion articles.
The conduct of our CRA of occupational risk factors thus required determining for 14 WHO subregions, by age and gender,(a) the proportion of the population exposed to each occupational risk factor under study, with a preference for multiple levels of exposure,
(b) the corresponding relative risk of adverse health outcome(s) resulting from those exposures, and
(c) the theoretical minimum exposure to the risk factor.The full WHO CRA methodology was applied to four occupational risk factors: occupational carcinogens, airborne particulates, noise, and ergonomic stressors. A modified approach was used for occupational injuries, because the lack of data in developing nations prevented estimation of exposure levels and relative risks by occupation or economic sector. The analysis of infections due to needlesticks was conducted solely for health care workers.
Data Sources for the CRA of Occupational Risk Factors
An exhaustive literature review was conducted to locate studies that evaluated exposures or described relative risks in such a way that they could be linked to a global assessment of the risk factor.1
Estimating the Proportion of the Population Exposed to Occupational Hazards
As described above, determining the attributable fraction requires estimates of the proportion of a population exposed to occupational hazards (fi), and the relative risks of those exposures. The model used for exposure prediction is presented in the Appendix; coefficients included here relate to this model.
The proportion of the population that is exposed to occupational hazards (represented in the overall model as "PEP"), and the levels of those exposures, is affected by a number of factors. The proportion of the population that works, where they work, and the kinds of jobs they do, and the presence and effectiveness of exposure controls are the primary factors. The basis of our exposure assessment was, therefore, the distribution of the working population into economic sectors and/or occupational categories, with refinements as necessary. For example, some occupational diseases have long latency periods, so it is necessary to know how many people have ever had exposure to the relevant occupational hazard. In these cases, the number of people who have ever held a specific job (estimated by the rate of occupational turnover) becomes important. Each of these factors is discussed below, along with our approach to obtaining subregion, gender, and age-specific estimates.
Economic Activity Rate (EAR)
The starting point for determining the proportion of the population with exposure to occupational hazards was the Economic Activity Rate (EAR). The EAR is calculated as the number of economically active people (Economically Active Population, or EAP) in a given age range, divided by the total population in that age range. The EAP includes people in paid employment, the self-employed, people who work to produce goods and services for their own household consumption, and the unemployed. It includes the majority of the informal sector (most of whom are considered as "employed," with the remainder as "unemployed") [ILO, 2002a], and, therefore, represents the most comprehensive accounting of persons who may be exposed to occupational hazards. While most workers could be counted in this approach, we were unable to include some groups of working women (e.g., some women who work on family farms), or working children under 15 (due to wide variations in the youngest age groups reported in country-level data). We could not capture the increased risk of occupational hazards faced by persons in precarious or contingent employment [Quinlan, 2002].
The primary data source for determining subregional values of EAR was the ILO Economically Active Population 1950-2010 (2002b), which uses a variety of sources to project the EAP at the country level, by age and gender. These data were compiled by subregion, and used to calculate subregion-specific EARs (see Table I). Variations between age groups reported by ILO and those used in the GBD project required that EARs for 60-69-year-olds be estimated from data for 60-64-year-olds. Data for people ≥65 were applied to the 70-79 age group. The ≥80 age group was estimated at one half of the rate for the ≥65 age group (by comparison with country-level data, which is reported by some countries for elderly workers) [ILO, 2001a].
Most of our exposure assessments were based on the distribution of the EAP ≥15 years of age into economic sectors and/or occupations (see below). In contrast, the exposed population for occupational injuries was based on the total number of economically active persons aged ≥15 in a subregion.
Proportion of the population working in each economic sector PW(es) or occupational category PW(oc)
After determining the fraction of the population that was economically active in a subregion, the next step was to determine where they worked (economic sector) and what jobs they held (occupational categories). Each exposure assessment was tailored to the format of existing exposure and/or hazard estimates. (For example, exposure estimates for carcinogens were available by economic sector, requiring an exposure assessment based on distribution of the EAP within economic sectors.) The EAP in each subregion was further distributed by occupation within economic sector to generate a cross-tabulation of economic sector by occupational category. This provided a consistent distribution of the EAP for all exposure analyses, which could be utilized with exposure data organized by economic sector or by occupational category (see Table II).
The World Bank [2001] provided data 1990 and 1996-1998 on the distribution of the labor force into the three major economic sectors for most countries. These economic sectors were further subdivided into the nine economic sectors seen in Table II using economic sector employment data from the ILO [2001a], resulting in Table III.
Limited data from the ILO (1995, the last year for which such data are available) on employment by occupation and economic sector for about 30 countries were used to construct subregional tables of occupation within economic sector distributions [ILO, 1995a]. Where data were available for more than one country in a subregion, the numbers of workers in each category were summed to generate a weighted average for the subregion. Where data were available for only one country, those data were assumed to represent all the countries in that subregion. Lack of data for some subregions necessitated the use of data from the most similar subregion (EMR-B based on EMR-D, EUR-C based on EUR-B and WPR-A based on AMR-A).
Because of limited data on occupational distribution by gender within economic sectors (and none by age), the same distribution of occupation within economic sectors was applied within a subregion to ages 15 and above, and to males and females. Within an economic sector, the A subregions had higher proportions of EAP in the professional, managerial and administrative categories, while the B, C, D, and E subregions had proportionally more workers in the production categories.
Proportion of workers with exposure to occupational hazards (PEW)
Exposures to occupational hazards vary within economic sectors and occupational categories; for example, some but not all workers in manufacturing have exposure to noise, and those exposures will vary. The next steps were to determine the proportion of workers within an economic sector and/or occupational category who had exposure to the occupational hazard being assessed (PEW), and the levels of those exposures (EPF, see next section). While the exposure distributions needed to estimate these parameters are available for developed countries, we were not able to locate reliable reports of exposure distributions in developing countries.
The CAREX database [FIOH, 1999; Kauppinen et al., 2000] provided a rich source of data on the numbers of workers with exposure to a long list of carcinogens, including asbestos and silica (which also have noncarcinogenic health effects). CAREX includes workers in all economic sectors, in nearly all European countries. NIOSH data on noise exposures included production workers in most economic sectors in the US. However, global data sources that provide estimates of the proportion of workers exposed, by economic sector and/or occupational category, are limited. Gaps in exposure data for workers worldwide limited our ability to establish the proportion of workers exposed to a specific risk factor. Therefore, exposure data from developed countries were usually applied to developing countries, and validated where possible.
To check the validity of this assumption, the literature was searched for estimates of the number of workers exposed to silica and benzene, which were chosen as indicators because there are more data available for developing countries than for other carcinogens. This search yielded a range of types of studies, from rough estimates [Zou et al., 1997] to studies in which air concentrations were measured in workplaces [Yin et al., 1987]. Estimates of the number of workers exposed to silica in China, Thailand, and Viet Nam, and to benzene in China, were compared to the number of persons employed, either in a specific economic sector or overall, in that country. The results obtained were compared with CAREX data. With few exceptions, the estimated fraction of workers exposed to silica or benzene is equal to or higher in these countries than indicated by the CAREX [Yin et al., 1987; Juengprasert, 1997; Zou et al., 1997; NIEHS, 1999; Phan Hong et al., 1999; Nguyen and Hong, 2001]. For example, the proportion of workers exposed to silica in manufacturing in Viet Nam is 3.7%, as compared to the CAREX estimate of 2.3%. Thus, the CAREX database was utilized as a conservative underestimate of the fraction of workers exposed to selected carcinogens world-wide.
Levels of exposure (exposure partition factor, or EPF)
Levels of exposure to occupational hazards can vary widely, even within similar job titles and economic sectors. For example, not all production workers in manufacturing will be exposed to the same levels of noise. For several occupational hazards (carcinogens, particulates, and noise), the proportion of the working population exposed at several levels was determined. The U.S. Occupational Safety and Health Administration (OSHA) Permissible Exposure Levels (PELs) were used to classify exposures as low (below the PEL) or high (above the PEL) exposures. Due to the greater prevalence of occupational health and safety regulatory programs and infrastructure in the A subregions [Roach, 1992; Hewett, 1996], we estimated that a larger proportion of workers was exposed at the lower levels in these subregions than in the B, C, D, and E subregions. Indications of actual exposure levels, such as contained in Pearce et al. [1994], provided anecdotal evidence that exposure levels are higher in BCDE countries. This is consistent with expectations, given that very few of these countries have occupational health programs. However, these data were not sufficient to develop estimates for each occupation by economic sector category, as needed for our model. Thus, we concluded that the data from CAREX were indicative of exposures in developed countries, but underestimates of exposures in developing countries. It is not possible based on the current state of knowledge to be more precise on a global level.
For carcinogens and the selected airborne particulates, it was assumed that 90% of exposed workers in the A regions had low exposures (below the relevant PELs) and 10% had high exposures (above the relevant PELs). For the B, C, D, and E subregions, it was assumed that half of the exposed workers had lowexposures, and half had high exposures [Yin et al., 1987; Myers et al., 1989; Rees et al., 1992; Dosemeci et al., 1995; Partanen et al., 1995; NIOSH, 1999; NIOSH, 2000]. Further, where it was necessary to specify an exposure level, for example, to estimate lifetime cumulative exposure to silica, or level of noise exposure, the exposures in the A subregions were estimated to be lower than in the B, C, D, and E subregions.
For exposures to agents leading to COPD, asthmagens, and ergonomic stressors causing low back pain, exposures were based on distribution of the work force into economic sectors and/or occupational categories; therefore, it was not necessary to partition exposures into low and high levels. Regarding application of ergonomic data from developed countries to less developed countries, Punnett et al. [2005] explain that although the degree of mechanization, general quality of working conditions, and ergonomic interventions might each be less in developing regions, the very limited evidence available shows no general trend according to degree of development.
Details for particular exposures are provided in the specific articles, which follow in this series.
Occupational turnover (OT)
Cancers and lung diseases have long latency periods and once the disease process has begun the worker continues to be at risk, even after exposure ceases. This means that persons who were exposed to carcinogens or some airborne particulates in the past must be considered as ever-exposed, even if they are currently working in nonexposed jobs or have retired. Occupational turnover (OT), which is the replacement of workers by other workers in a specific job, increases the number of persons ever exposed to an occupational risk. A conservative value of 10% annual turnover rate (ATR) was estimated, based on data from 12 countries representing the A, B, D, and E subregions and a wide range of economic sectors [e.g., Butler and Twaddle, 1979; EIU, 1995, 1996, and 2001; Johnson and Whyte, 1977; Koch and Rhodes, 1981; Lucifora, 1998; Moffett, 2002].
An OT adjustment factor (noted as OT) to account for turnover in jobs with exposure to occupational carcinogens or to the selected respirable particulates (silica, asbestos, and coal dust) was determined as follows:Adjustment factor, OT = Pt/P0
= [original workers + new workers - deaths]/
original workers = {P0 + [P0 x ATR x t]
- [(mortality rate) (P0 + (P0 x ATR x t)] /P0 (4)where:
Pt = the proportion who have ever been occupationally exposed to dust, during a period of 40 years, still living;
P0 = the proportion who are occupationally exposed to dust at time t = 0
ATR = turnover/year, taken as 0.10;
t = time, taken as 40 years, a typical working lifetime; and
mortality rate = 20% of total cohort, based on published death rates of about 5 deaths per thousand over a period of 40 years (USDHHS, 2001).Equation 4 results in an adjustment factor of OT=4 to correct for occupational turnover during a 40-year period, with a median exposure duration of 10 years based on cohort modelling (Steenland and Driscoll, 2002, personal communication). The use of an OT factor is consistent with the occupational experience of cohorts represented in the epidemiological studies from which relative risks were taken.
In summary, the model which we used to estimate the proportion of the population with exposure to occupational hazards includes terms (as appropriate) for the proportion of the population that was economically active, the distribution of the economically active population into economic sectors and/or occupational categories, the proportion of workers within an economic sector and/or occupational category with exposure to occupational hazards, the levels of those exposures, and a factor to account for turnover of workers within a job. Table IV includes a summary of the factors considered for each of the occupational diseases and injuries included in our analysis, along with the primary data sources for exposure assessment.
Linking Occupational Exposures to Hazard-Disease Relationships
Determining the fraction of the global burden of disease and injuries that is attributable to occupational hazards requires not only the estimation of the proportion of the global population which is exposed, but also estimates of the risk of morbidity and/or mortality of those exposures. Both assessments had to be closely linked. Ideally, the linkage is the causative agent itself, for example, exposure to asbestos at known levels and the relative risk of asbestosis resulting from those exposures. However, in some cases, data are not available in this format. For example, neither exposure nor relative risk data are available for the over 200 known asthmagens. Occupational category served as a suitable proxy for exposure to asthmagens, as relative risk data are available for asthma by occupational category.
Risk measures (relative risks or mortality rates) for the health outcomes resulting from exposures to the occupational hazards considered in this study were determined primarily from peer-reviewed, published studies. Adjustments were made, as appropriate, to account for differences in levels of exposure, exposure duration and/or age, sex, and subregion. A brief summary of both exposure and risk estimates is provided for each occupational hazard analyzed in the companion studies.
Occupational carcinogens
Many of the 150 agents classified as known or probable human carcinogens [IARC, 1994] are encountered in the workplace. Although many different malignant conditions can result, the main groups are relatively few—lung cancer, leukemia, and malignant mesothelioma. The frequency and risk of exposure, strength of evidence, and availability of data determined the exposures that were selected for assessment in this study. The exposure assessment for all occupational carcinogens was based on the CAREX database [FIOH, 1999; Kauppinen et al., 2000].
A relative risk for all lung carcinogens was developed using a method similar to that of Steenland et al. [1996] and Nurminen and Karjalainen [2001], in which mean relative risk for all exposures was determined by taking a weighted average of the substance-specific relative risks, then weighting the substance-specific relative risks by the proportion of workers exposed to each substance. Relative risks were weighted separately for each region, using the exposure prevalence of the workforce in each region to weight the exposure-specific risks. However, the resulting average relative risks were not meaningfully different between regions. Based on exposure estimates for American workers of 90% at or below the PEL, and 10% above the PEL, the mean relative risk of 1.6 was partitioned into a value of 1.3 for low-level exposures, and 1.9 for high-level exposures.
Similarly, for leukemogens the separate relative risks for the relevant occupational agents were combined into single summary relative risks, for low exposure and for high exposure. Relative risks were available for low exposures (1.86) and for high exposures (3.66), so it was not necessary to partition the values determined from the literature [BEIR, 1990; IARC, 1994; Lynge et al., 1997; Steenland et al., 2003].
For lung cancer and leukemia, the attributable fractions were calculated from the proportion of the population exposed and the matching relative risks (see Equation 3). These attributable fractions were then multiplied by theGBD estimates of deaths and DALYs [Murray and Acharya, 1997] for relevant causes of death in each subregion, to develop estimates of deaths and DALYs arising from exposures to lung carcinogens and leukemogens.
Malignant mesothelioma is almost exclusively an occupational disease, probably occurring only in persons who have had exposure to asbestos, and with most of the asbestos exposure being occupational. Since it is therefore not meaningful to calculate a relative risk, mortality rates were calculated for various cumulative lifetime exposures at low and high exposures in the A, and in the B, C, D, and E subregions. The number of deaths was estimated by applying these absolute risk estimates to estimates of absolute asbestos exposures. An attributable fraction was estimated by comparing the number of deaths from mesothelioma to the total number of deaths in the WHO disease category for "other neoplasms." This fraction was multiplied by the number of DALYs in the "other neoplasms" category (Global Burden of Disease Code 77) to estimate the DALYS due to mesothelioma. See Driscoll et al. [2005a] for further details.
Agents leading to COPD
Tobacco smoking is clearly the most important risk factor for chronic obstructive pulmonary disease (COPD), but many work-related exposures have been demonstrated to cause COPD [Hendrick, 1996]. Worldwide data to support exposure assessments to the main causative agents of COPD, that is, nonspecific dust and fumes [Becklake, 1989] do not exist.Work in specific economic sectors was, therefore, used as a surrogate for dust exposure, based on the work of Korn et al. [1987]. Their study provides a link between selfreported exposure to dust (current and past exposure) and some categories of economic activity among the currently employed, which were matched with our economic sector distribution data.
Korn et al. [1987] used a strict definition of COPD and determined relative risks for both men and women, based on a large number of participants. We partitioned these relative risks for high and low exposure categories, using slightly different values for developed and developing countries to take account of variations in the low exposure categories in agriculture and industry. These relative risks and the proportion of the population exposed were combined in Equation 3 to estimate the attributable fraction. This value was then multiplied by the number of deaths and DALYs in the GBD disease category for COPD, resulting in estimates of the number of deaths and DALYs attributable to occupational exposures to agents leading to COPD.
The risk values used for COPD took into account current and lifetime smoking history of the subjects on which the odds ratios were based.We did not consider smoking rates in individual countries, and to the extent that there may have been interaction between occupational exposures and smoking, we have not allowed for that over and above any allowance that is inherent in the relative risk measures we used. If there was more smoking, one could argue a larger proportion of all smoking morbidity and mortality will be due to factors other than occupational exposures. However, the available data and the study design did not allow for further analysis, and this factor probably would not have had any important influence on the major estimates.
Asthmagens
Asthma, which is probably the most common workrelated respiratory disorder in industrialized countries [Kogevinas et al., 1999], is a narrowing of the upper respiratory passages resulting in difficult breathing and wheezing. Many hundreds of biological and chemical agents, found in a wide variety of workplaces, have been associated with occupational asthma [Chan-Yeung and Malo, 1994; Venables and Chang-Yeung, 1997; Balmes et al., 2003]. It would not be possible to conduct exposure assessments and to obtain relative risk data for all contributing factors, especially since they often occur in combination, so we based our approach on the work of Karjalainen et al. [2001, 2002] and Kogevinas et al. [1999]. The study by Karjalainen et al. 2001, 2002 extended over 13 years and covered the entire Finnish population, providing relative risks for a large number of broad occupational categories. Kogevinas et al. [1999] conducted a cross-sectional study of asthma involving 15,000 people in 12 European countries.
As the relative risks derived in those studies were based on occupational categories, our exposure assessment was based on distribution of the workforce in occupational categories, matching our categories as closely as possible to those identified by Karjalainen et al. 2001, 2002 for which relative risk values were provided. Those not working and those employed in administration were together considered to be the nonexposed reference category (relative risk=1). The attributable fraction calculated from these relative risks and the proportion of the population exposed were applied to number of deaths and DALYs in theWHO disease category for asthma, yielding estimates for the number of deaths and DALYs resulting from occupational exposure to asthmagens.
Silica and asbestos
Exposure to silica and asbestos can lead to the development of silicosis and asbestosis, respectively. Assessment of the proportion of workers exposed to silica and asbestos was based on the distribution of the economically active population by economic sector and the percentage of workers exposed to these substances by economic sector. An adjustment factor of four was used to account for turnover in jobs with exposure to occupational silica and asbestos, as described earlier.
The primary data source on the proportion of workers exposed to silica and asbestos for each economic sector was the CAREX database, as described earlier. The PELs were used to classify exposures to silica and asbestos as lowor high level, with a larger proportion of workers in A subregions assumed to have low exposure, and absolute exposure levels assumed to be lower in A subregions.
Cumulative exposure estimates for workers of different ages were determined by modeling of an artificial cohort to estimate the average cumulative exposure for such a representative cohort in steady state. Cumulative exposures for asbestos took into account changes in the PELs for asbestos during the years of interest to the current analysis.
Coal dust
Exposure to coal dust can lead to the development of coal workers’ pneumoconiosis. Because the CAREX database does not include data on exposure to coal dust, it was necessary to use a different methodology for this exposure than that used for silica and asbestos. The estimates of the proportion of the population exposed to coal dust were based on global coal production, but the approach to partitioning of exposure into low/high categories was the same as described for silica and asbestos. As for silica and asbestos, a turnover factor of four was applied to account for persons not currently working in coal mining but who had been exposed previously. The "PEL" used for coal was the United States Mine Safety and Health Administration (MSHA) value of 2 mg/m3 [NIOSH, 1995].
For all three pneumoconioses, the attributable fraction was assumed to be 100%, since virtually all exposure occurs in an occupational setting. DALYs were estimated using the standard WHO approach based on the estimated number of deaths. For further discussion of nonmalignant respiratory disease due to occupational airborne particulates, see Driscoll et al. [2005b].
Noise
Exposure to excessive noise is one of the most pervasive occupational hazards, and may lead to elevated blood pressure, sleeping difficulties, annoyance, and stress, and interference with communications in the workplace. However, noise-induced hearing loss (NIHL) is the most serious effect and is irreversible. The availability of noise exposure data by occupations in the U.S. [NIOSH, 1998], and data on the risk of hearing loss at various sound levels [Prince et al., 1997], allowed us to use noise exposure levels as a direct measure for the risk of developing NIHL. As global data on the frequency of occurrence, duration, and intensity of noise exposure do not exist, it was necessary to model this exposure for workers in various occupational categories, based on the U.S. NIOSH data, adjusted for differences in prevalence of hearing conservation programs in developed and developing countries. Three levels of exposure were estimated by occupational category, and relative risk values were determined for each by comparing excess risk estimates for noiseexposed workers with excess risk estimates for the background population [Davis, 1989]. The relative risk estimates were adjusted to account for the different definition of NIHL used by WHO (≥41 decibels hearing loss at 0.5, 1, 2, and 4 kHz) compared to the more frequently used cut-off (>25 decibels of hearing loss at 1, 2, 3 and 4 kHz). Combining these relative risks with the proportions of the population exposed to occupational noise yielded estimates of the attributable fractions. Applying these attributable fractions to the number of DALYs in the GBD disease category for hearing loss (as deaths do not occur from noise exposures) resulted in the number of DALYs occurring from occupational exposures to noise. See Nelson et al. [2005] for further details.
Ergonomic stressors leading to low back pain
Pain in the soft tissues of the back is extremely common among adults throughout the world, and is associated with substantial financial costs and loss of quality of life. For example, in Canada, Finland, and the United States, more people are disabled from working as a result of musculoskeletal disorders (MSDs) -- especially back pain -- than from any other group of diseases [Pope et al., 1991; Badley et al., 1994; Riihimoki, 1995]. The physical ergonomic features of work that are most frequently cited as risk factors for MSDs include rapid work pace and repetitive motion patterns; insufficient recovery time; heavy lifting and other forceful manual exertions; nonneutral body postures (either dynamic or static); mechanical pressure concentrations; vibration (both segmental and whole-body); and low temperature.
Since it is not possible to assess all relevant physical and psycho-social exposures on a global basis, we used broad occupational category as a proxy for exposure to the combined stressors that produce excess risk of low back pain (LBP). As per Leigh and Sheetz [1989], the reference group (background risk) is comprised of professional and administrativeworkers. Clerical and sales workers were considered to have low exposures, and operators (production workers) and service workers were considered to have moderate exposures. Farmers were the only occupational category considered to have high exposure. Relative risks for these occupational categories ranged from 1.38 for clerical or sales workers, to 3.65 for farmers. These relative risks and the proportion of the population exposed were combined in Equation 3 estimate attributable fractions, which were applied to the number of DALYS in the GBD category for musculoskeletal disease (as deaths do not occur fromlowback pain) to yield the number of DALYs attributable to low back pain. Further discussion is provided in Punnett et al. [2005].
Risk factors for injuries
Due to lack of globally quantifiable measures of risks for unintentional injuries by occupation or economic sector, we used the Economically Active Population (EAP) as a surrogate of the population at risk for occupational injuries. Country-level injury fatality rates for insured workers were used to calculate WHO subregional rates, which were applied to the subregional EAP to estimate deaths and DALYs. Concha-Barrientos et al. [2005] provide a detailed discussion.
Contaminated sharps leading to infections in health care workers
Because occupational exposures to sharps injuries are a substantial source of infections with bloodborne pathogens among health-care workers, we estimated the global burden of hepatitis B (HBV), hepatitis C (HCV), and human immunodeficiency virus (HIV) infection due to percutaneous injuries among health care workers(HCWs).We modeled the incidence of infections attributable to percutaneous injuries in 14 geographical subregions on the basis of the probability of injury, the prevalence of infection, the susceptibility of the worker and the percutaneous transmission potential.
RESULTS
Table Vand Figure 2 provide the attributable fraction in DALYs for each of the selected occupational risk factors. Tables VI and VII provide the details of the distribution by gender. The companion studies provide a subregional comparison of the morbidity and mortality of the selected occupational risk factors.
The global burden of just these selected occupational diseases and injuries in the year 2000 included 850,000 deaths and approximately 24 million years of healthy life lost. Without correction for underestimation, these selected occupational risk factors alone accounted for about 1.5% of all mortality and about 1.6% of all DALYs in the world in the year 2000. The leading occupational causes of death (Table VI) were COPD (37%) and unintentional injuries (37%), followed by trachea, bronchus, or lung cancer (12%). Unintentional occupational injuries were the main cause of years of healthy life lost (Table VII), with 44% of the burden (10,531,000 DALYs). This was followed by hearing loss due to occupational noise (18%) and COPD due to occupational agents (16%). These three conditions accounted for nearly 80% of years of healthy life lost. Results for specific risk factors, including results by subregion, gender, and age group, are presented in the articles on individual risk factors.
Overall, the burden of disease due to occupational exposures is greater in developing countries, and in males than in females, reflecting differences in exposure, economic sectors, and types of occupation. The burden was about five times greater in males than in females, both for deaths (706,000 vs. 144,000) and DALYs (19,656,000 vs. 4,038,000). Years of healthy life lost were higher for those risk factors that particularly affected workers at younger ages, whereas mortality was higher in older age groups. Attributable fractions for the pneumoconioses (silicosis, asbestosis, and coal workers’ pneumoconiosis) and for mesothelioma were 100%, since these outcomes are virtually all due to occupational exposures. Attributable fractions for all other outcomes, for both sexes and all age groups together, ranged from 2% for leukemia to 37 % for low back pain. Overall, 16,000 HCV, 66,000 HBV, and 1,000 HIV infections may occur worldwide among health care workers due to sharps injuries. The fraction of infections with HCV, HBV, and HIV attributable to occupational exposure to percutaneous injuries fraction reaches 39%, 37%, and 4.4%, respectively [see Pruss-Ustun et al., 2005].
DISCUSSION
To our knowledge, this is the first time that a comparative risk factor approach using DALYs has been used to estimate the global burden of selected occupational disease and injury risk factors. The benefit of using the CRA is that it facilitates comparison of deaths and DALYs resulting from exposure to occupational hazards with those resulting from the other risk factors assessed in the WHO study. However, there are a number of limitations that are mainly due to incomplete data for exposures and hazard-disease relationships, particularly for developing countries. These limitations mean that it is not possible to quantify the uncertainty of the mortality and morbidity estimates generated in this study.
Perhaps the most important limitation is the lack of data on the percentage of the population exposed to the agents of interest.UsingCAREXdata on the proportion ofworkerswith exposure to occupational hazards also likely contributed to underestimates, as the limited data available indicate higher proportions of exposed workers in developing countries, who are probably exposed to higher levels of airborne contaminants and noise than their counterparts in the developed countries. Because of limitations in the available data on Economic Activity Rates, we could not include working children or certain categories ofworkers, such as somewomen working on family farms, nor could we quantify the increased risks facedbypersons inprecariousorcontingentemployment. Specific, focused research on working children is needed to quantifyexposures, health risks,and the resulting implications.
Another limitation is that the same risks were applied to each subregion. Direct risk data are not available for the exposures of interest in most regions, and there is virtually no information available to allow the precise extent of any possible differences to be determined for any of the exposuredisease relationships of interest. The same risks were also applied to males and females, and to all age groups.
We also did not attempt to take into account to what extent the risk of developing occupational disorders diminishes as a result of exposure ceasing. Unfortunately, there are little published data that address this issue. Most studies that provide information on risk consider people who have highly variable periods between end of exposure and end of follow-up, with periods varying between zero (still exposed) and many decades.
Finally, a major factor leading to an underestimate of the true burden of disease and injury due to occupational risk factors is exclusion ofmany health conditions, includingmany respiratory diseases, some infectious diseases; less widespread cancers and carcinogens; most musculoskeletal disorders, intentional injuries in the workplace; organ and systemic diseases resulting from occupational exposure to solvents, pesticides and heavy metals; reproductive health impacts; skin disorders; coronary heart disease and other outcomes associated with work-related stress. Available data were inadequate to meet the strict criteria of the WHO project.
In a companion study in this series, Driscoll et al. [2005c] have compared the results of this study with previous global analyses of occupational disease and injury. They concluded that these estimates are appropriate for the occupational exposures and conditions included, but that due to data limitations, the findings are a major underestimate of the true burden of disease attributable to occupational exposures, most likely by at least a factor of two. Therefore, the true extent of the global burden of disease resulting from occupational risk factors is likely to have been considerably more than the estimated 1.7% of all morbidity and mortality in 2000, probably as high as 3.4% [Driscoll et al., 2005c].
Themagnitude of these numbers belies their significance. The impacts of disease, injury, or death of workers extend beyond the individuals affected to include family members, employers, the wider community, and the economy. Further, the rates of disease, injury, and death do not impact all economic sectors and occupations equally. Certain industries, such as agriculture, mining, and construction are far more hazardous than others, such as provision of financial or educational services. Contingent workers and those in the informal sector face even higher risk than their counterparts in secure employment in the formal sector.
While there are many uncertainties in our estimates due to lack of global data on prevalence and level of exposures to occupational risk factors, this project has established an analytical framework for determining the impact of work on human health. Because estimates of the burden of disease and injury resulting from occupational exposures are used in the allocation of resources, it is important that they be as accurate as possible. Further work to increase data quality and availability would serve to improve estimates of the burden of occupational disease and injury. Since it is likely that our findings underestimate the true extent of morbidity and mortality due to occupational exposures, better data could contribute to a stronger case supporting the critical need to devote adequate resources to protecting worker health. It would also help to ensure that resources that are available are allocated appropriately.
CONCLUSION
Exposure to occupational hazards accounts for a substantial portion of the global burden of disease and injury. The impacts of these occupational deaths, diseases, and injuries extend far beyond the statistics reported here, to include reduced contributions by valuable employees in the workplace, economic loss to families, employers, and to nations, and untold human pain and suffering. The majority of these deaths, diseases, and injuries need not occur. The burden of occupational risk factors is largely preventable, as many examples from different countries have shown. Proven methods for reducing exposures are often quite simple: use of wet methods to reduce silica exposures, readjustment of work surfaces to reduce low back pain, substitution of safer chemicals or processes, and attention to electrical safety or machine guarding.We urge policy makers to use the evidence developed by this study to focus efforts to eliminate the preventable causes of occupational death, disease and injury.
Acknowledgments
The authors express their appreciation to Lucy Schoolfield of NIOSH, Cincinnati, for her generous help in locating reference materials, and to Norrey Hopkins of WHO, Geneva, for her assistance in preparing the manuscripts.
References:
Badley EM, Rasooly I, Webster GK. 1994. Relative importance of musculoskeletal disorders as a cause of chronic health problems, disability, and health care utilization: Findings from the 1990 Ontario Health Survey. J Rheum 21(3):505-514.
Balmes J, Becklake M, Blanc P, Henneberger P, Kreiss K, Mapp C, Milton D, Schwartz D, Toren K, Viegi G. Environmental and Occupational Health Assembly, American Thoracic Society. 2003.
American Thoracic Society Statement: Occupational contribution to the burden of airway disease. Am J Respir Crit Care Med 167(5):787-797.
Becklake M. 1989. Occupational exposures: Evidence for a causal association with chronic obstructive pulmonary disease.AmRev Respir Dis 140:S85-S91.
BEIR V (Committee on the Biological Effects of Ionizing Radiation). 1990. Health effects of exposure to low levels of ionizing radiation: BEIRV. Washington, DC: National Academy Press.
Butler S, Twaddle S. 1979. Turnover in the restaurant industry: A structural explanation. Mid-South Sociological Association. Sociol Abstr 27(4).
Chan-Yeung M, Malo J. 1994. Aetiological agents in occupational asthma. Eur Respir J 7:346-371.
Concha-Barrientos M, Nelson DI, Fingerhut M, Driscoll T, Leigh J. 2005. The global burden due to occupational injury. Am J Ind Med 48:470-481 (this issue).
Davis AC. 1989. The prevalence of hearing impairment and reported hearing disability among adults in Great Britain. Int J Epidemiol 18(4):911-917.
Desai MA, Mehta S, Smith KR. 2004. Indoor smoke from solid fuels: Assessing the environmental burden of disease at national and local level. WHO Environmental Burden of Disease Series, No. 4). World Health Organization, Geneva.
Dosemeci M, McLaughlin J, Chen J, Hearl F, Chen R, McCawleyM,Wu Z, Peng K, Chen A, Rexing S, et al. 1995. Historical total and respirable silica dust exposure levels in mines and pottery factories in China. Scand J Work Environ Health 21:39-43.
Driscoll T, Steenland NK, Nelson DI, Leigh J, Concha-Barrientos M, Fingerhut M, Pruss-Ustun A. 2005a. The global burden of disease due to occupational carcinogens. Am J Ind Med 48:419-431 (this issue).
Driscoll T, Steenland NK, Nelson DI, Leigh J, Concha-Barrientos M, Fingerhut M, Pru¨ss-U¨ stu¨n A. 2005b. The global burden of nonmalignant respiratory disease due to occupational airborne exposures. Am J Ind Med 48:432-445 (this issue).
Driscoll T, Takala J, Steenland K, Corvalan C, Fingerhut M. 2005c. Review of estimates of the global burden of injury and illness due to occupational exposures. Am J Ind Med 48:491-502 (this issue).
EIU. 1995. Business Operations Report India 4th Quarter, 1995. Shortage of managers. EIU. 1996. China Hand. Ch. 13—Human Resources: Knowing why staff leave. 1 Sept.
EIU. 2001. Country Forecast Africa. AIDS/Africa: Labour costs are set to increase substantially. 14 May.
Ezzati M, Lopez AD, Rodgers A, Murray CJL, editors. 2004. Comparative quantification of health risks: Global and regional burden of disease attributable to selected major risk factors. Geneva: World Health Organization.
Finnish Institute of Occupational Health (FIOH). 1999. CAREX database.
Hendrick DJ. 1996. Occupational and chronic obstructive pulmonary disease (COPD). Thorax 51(9):947-955.
Hewett P. 1996. Interpretation and use of occupational exposure limits for chronic disease agents. Occup Med: State of the Art Reviews 11(3):561-590.
IARC (International Agency for Research on Cancer). 1994. Some industrial chemicals. Lyon, France: IARC.
International Labour Organization. 1987. Resolutions adopted by the International Conference of Labour Statisticians. Annex 1. Major, submajor, minor and unit group titles. Available at
http://www.ilo.org/public/english/bureau/stat/download/res/isco.pdfInternational Labour Organization (ILO). 1995a. ILO Yearbook of Labour Statistics 1995. 54th issue, Geneva.
International Labour Organization (ILO). 1995b. Sectoral Activities Programme, Recent Developments in the Coalmining Industry, Coal Mines Committee , 13 th Session, Report I, Geneva.
International Labour Organization (ILO). 2001a. ILO Yearbook of Labour Statistics 60th issue, Geneva.
International Labour Organization (ILO). 2001b. Laborsta, The Labor Statistics Database. Available at: http://laborsta.ilo.org/. International Labour Organization (ILO). 2002a. The International Labor Conference, Report VI, Decent Work and the Informal Economy.
International Labour Organization (ILO). 2002b. Economically Active Population 1950-2010, Fourth Edition, Rev. 2, Geneva.
Johnson AG, Whyte WF. 1977. The Mondragon system of worker production cooperatives. Ind Labor Relations Rev 11:18-30.
Juengprasert W. 1997. Towards elimination of silicosis in Thailand. Mineral dusts and prevention of silicosis. Asian-Pacific Regional Network on Occupational Safety and Health Information (ASIA-OSH) 4(2) September 1997.
Karjalainen A, Kurppa K, Martikanen R, Klaukka T, Krjalainen J. 2001. Work is related to a substantial portion of adult-onset asthma incidence in the Finnish population. Am J Respir Critical Care Med 164:565- 568.
Karjalainen A, Kurppa K, Martikanen R, Karjalainen J, Klaukka T. 2002. Exploration of asthma risk by occupation-extended analysis of an incidence study of the Finnish population. Scand JWork Environ Health 28:49-57.
Kauppinen T, Toikkanen J, Pedersen D, Young R, AhrensW, Boffetta P, Hansen J, Kromhout H, Maqueda Blasco J, Mirabelli D, de la Orden- Rivera V, Pannett B, Plato N, Savela A, Vincent R, Kogevinas M. 2000. Occupational exposure to carcinogens in the European Union. Occup Environ Med 57:10-18.
Koch JL, Rhodes SR. 1981. Predictors of turnover of female factory workers. J Voc Beh 18(2):145-161.
Kogevinas M, Anto JM, Sunyer J, Tobias A, Kromhout H, Burney P. 1999. Occupational asthma in Europe. Lancet 353:1750-1754.
Korn RJ, Dockery DW, Speizer FE, Ware JH, Ferris BG Jr. 1987. Occupational exposures and chronic respiratory symptoms: A population based study. Am Rev Respir Dis 136:298-304.
Leigh JP, Sheetz RM. 1989. Prevalence of back pain among full-time United States Workers. Br J Ind Med 46:651-657.
Leigh JP, Markowitz SB, Fahs M, Shin C, Landrigan PJ. 1997. Occupational injury and illness in the United States. Estimates of costs, morbidity, and mortality. Arch Intern Med 157(14):1557- 1568.
Leigh J, Macaskill P, Kuosma E, Mandryk J. 1999. Global burden of disease and injury due to occupational factors. Epidemiology 10(5): 626-631.
Leigh JP, Yasmeen S, Miller TP. 2003. Medical costs of fourteen occupational illnesses in the United States in 1999. Scand J Work Environ Health 29(4):304-313.
Loewenson R. 1999. Assessment of the health impact of occupational risk in Africa: Current situation and methodological issues. Epidemiology 10(5):632-639.
Lucifora C. 1998. The impact of unions on labour turnover in Italy: Evidence from establishment level data. Int J Ind Org 16(3):353-376. Lynge E, Anttila A, Hemminki K. 1997. Organic solvents and cancer. Cancer Causes and Control 8:406-419.
Mathers CD, Stein C, Ma Fat D, Rao C, Inoue M, Tomijima N, Bernard C, Lopez AD, Murray CJL. 2002. Global Burden of Disease 2000: Version 2 methods and results. Global Programme on Evidence for Health Policy Discussion Paper No. 50. World Health Organization, October 2002.
Moffett M. 2002. New Mexico Labor Market Dynamics. Labor Market Review, Special Article, New Mexico Department of Labor, February. Available at:
http://www3.state.nm.us/dol/dol_lmrsa6.htmMurray CJ. 1994. Quantifying the burden of disease: The technical basis for disability-adjusted life years. Bull World Health Organ 72(3):429- 445.
Murray CJL. 1996. Rethinking DALYs. In: Murray CJL, Lopez AD, editors. The Global Burden of Disease. Cambridge: Harvard University Press, p 1-98.
Murray CJL, Acharya A. 1997. Understanding DALYs. J Health Econ 16:703-730.
Murray CJL, Lopez AD. 1997. Global mortality, disability, and the contribution of risk fators: Global Burden of Disease Study. Lancet 349:1436-1442.
Myers J, Lewis P, HofmeyrW. 1989. Respiratory health of brickworkers in Cape Town, South Africa: Background, aims, and dust exposure determinations. Scand J Work Environ Health 15:180-187.
National Institute for Occupational Safety and Health (NIOSH). 1995. Summary: Criteria for a recommended standard-occupational exposure to respirable coal mine dust. September 1995. Available at: http:// www.cdc.gov/niosh/coaldust.html.
National Institute for Occupational Safety and Health (NIOSH). 1998. Criteria for a recommended standard: Occupational noise exposure. Revised Criteria 1998. http://www.cdc.gov/niosh/98-126.html.
National Institute for Occupational Safety and Health, Cincinnati. National Institute for Occupational Safety and Health (NIOSH). 1999.
Work-related Lung Disease Surveillance Report 1999. U.S. Department of Health and Human Services, National Institute for Occupational Safety and Health.
National Institute for Occupational Safety and Health (NIOSH). 2000. Injuries, illnesses, and hazardous exposures in the mining industry, 1986-1995: A surveillance report. Washington, DC: U.S. Department of Health and Human Services, National Institute for Occupational Safety and Health.
National Institute on Environmental Health Sciences (NIEHS). 1999. A world-class program. Environmental Health Perspectives 107(7). Available at: http://ehpnet1.niehs.nih.gov/docs/1999/107-7/niehsnews.html.
Nelson D, Nelson R, Concha-Barrientos M, Fingerhut M. 2005. The global burden of occupational noise-induced hearing loss. Am J Ind Med 48:446-458 (this issue).
Nguyen Thi, Hong Tu. 2001. Personal correspondence. 31 August 2001. Nurminen M, Karjalainen A. 2001. Epidemiologic estimate of the proportion of fatalities related to occupational factors in Finland. Scand J Work Environ Health 27:161-213.
Oleinick A, Guire KE, Hawthorne VM, Schork MA, Gluck JV, Lee B, La S. 1993. Current methods of estimating severity for occupational injuries and illnesses: Data from the 1986 Michigan Comprehensive Compensable Injury and Illness Database. Am J Ind Med 23(2):231- 252.
Partanen T, Jaakkola J, Tossavainen A. 1995. Silica, silicosis and cancer in Finland. Scand J Work Environ Health 21:84-86.
Pearce N, Matos E, Vainio H, Boffetta P, Kogevinas M. 1994. Occupational cancer in developing Countries. Lyon: IARC Scientific Publications Number 129.
Phan Hong Son, Tran Ngoc Lan, Le Van Trung, et al. 1999. Use Geographical Information System to identify risk for silicosis and planning strategies for prevention, July, 1999. Funded by the Fogarty International Center. Washington, DC: NIH.
Pope MH, Andersson GBJ, Frymoyer JW, Chaffin DB, editors. 1991. Occupational low back pain: Assessment, treatment and prevention. St. Louis, MO: Mosby-Year Book, Inc.
PrinceMM,StaynerLT, Smith RJ, Gilbert SJ. 1997.Are-examination of risk estimates from the NIOSH Occupational Noise and Hearing Survey (ONHS). J Acoustic Soc Am 101:950-963.
Pruss-Ustun A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med 48:482-490 (this issue).
Pruss-Ustun A, Mathers C, Corvalan C, Woodward A. 2003. Environmental Burden of Disease Series, No. I. Introduction and methods: Assessing the environmental burden of disease at national and local levels. World Health Organization, Protection of the Human Environment, Geneva.
Punnett L,Pruss-Ustun A, Nelson DI, Fingerhut M,Leigh J, Tak S, Phillips S. 2005. Estimating the global burden of low back pain attributable to combined occupational exposures. Am J Ind Med 48:459-469 (this issue).
Quinlan M. 2002. Workplace Health and Safety Effects of Precarious Employment. In The Global Occupational Health Network, Issue No. 2, Winter 2001/2002. WHO, Geneva, Switzerland.
Rees D, Cronje R, du Toit R. 1992. Dust exposure and pneumoconiosis in a South African pottery. 1. Study objectives and dust exposure. Br J Ind Med 49:459-464.
Riihima¨ki H. 1995. Back and limb disorders. In: McDonald C, editor. Epidemiology of work related diseases. London: BMJ Publishing Group, p 207-238.
Roach S. 1992. Health Risks from hazardous substances at work- Assessment, evaluation and control. New York: Pergamon Press. Steenland K, Loomis D, Shy C, Simonsen N. 1996. Review of occupational lung carcinogens. Am J Ind Med 29:474-490.
Steenland K, Burnett C, Lalich N, Ward E, Hurrell J. 2003. Dying for work: The magnitude of US mortality from selected causes of death associated with occupation. Am J Ind Med 43:461-482.
Takala J. 1999. Global estimates of fatal occupational accidents. Epidemiology 10(5):640-646.
U.S. Department of Health and Human Services (USDHHS). 2001. Centers for Disease Control and Prevention, National Vital Statistics System. National Vital Statistics Reports 49(12) October 9, 2001. Deaths: Preliminary Data for 2000. AM Minino and BL Smith.
U.S. Energy Information Administration (USEAI). 2001. U.S. Energy Information Administration, U.S. Department of Energy, International Energy Database, January 2001, Available at: www.eia.doe.gov/emeu/ iea/coal.html.
United Nations (UN). 2000. International Standard Industrial Classification of all Economic Activities (ISIC) Third Revision. United Nations publication (St/ESA/STAT/SER.M/4/Rev.3).
Venables KM, Chang-Yeung M. 1997. Occupational asthma. Lancet 349:1465-1469.
World Bank. 2001. World Development Indicators 2001. Available at: http://worldbank.com.
World Health Organization (WHO). 2002. The World Health Report: Reducing Risks, Promoting Healthy Life. Geneva.
World Health Organization (WHO). 2004. Global Burden of Disease Estimates. Available at http://www3.who.int/whosis/menu.cfm? path=evidence,burden,burden_estimates&language=english
Yin SN, Li Q, LiuY, Tian F, Du C, Jin C. 1987. Occupational exposure to benzene in China. Br J Ind Med 44:192-195.
Zou Changqi, Gao Yun, Ma Qingyan. 1997. Pneumoconiosis in China: Current situation and countermeasures. Mineral dusts and prevention of silicosis 4(2) September 1997. Asian-Pacific Regional Network on Occupational Safety and Health Information (ASIA-OSH). Available at: http://www.ilo.org/public/english/region/asro/.
Return to LOW BACK PAIN
Return to GLOBAL BURDEN OF DISEASE
Since 9-16-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |