

Chiropractic Management of Shoulder Pain and
Dysfunction of Myofascial Origin Using
Ischemic Compression TechniquesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Can Chiropr Assoc 2002 (Sep); 46 (3): 192–200 ~ FULL TEXT
OPEN ACCESS Guy Hains, DC
2930 Côte Richelieu,
Trois-Rivières-Ouest,
Canada.
Shoulder pain and dysfunction is a chief complaint commonly presenting to a chiropractor’s office. The purpose of this article is to review the most common etiologies of shoulder pain, focusing on those conditions of a myofascial origin. In addition to a review of the literature, the author draws upon his own clinical experience to describe a method to diagnose and manage, patients with shoulder pain of myofascial origin using ischemic compression techniques. This hands-on therapeutic approach conveys several benefits including: positive therapeutic outcomes; a favorable safety profile and; it is minimally strenuous on the doctor and well tolerated by the patient.
Keywords: shoulder pain, dysfunction, myofascial pain syndromes, ischemic compression, chiropractic
From the FULL TEXT Article:
Introduction
Shoulder pain and dysfunction is a common chief complaint prompting a patient to seek out chiropractic care. According to the Job Analysis of Chiropractors 2000, upper extremity pain and injury account for 8.6% of the chief complaints among chiropractic patients (this number does not include those patients with upper extremity pain as a secondary complaint). [1] Moreover, after low back pain, shoulder pain is the second most common cause of occupational injury claims. [2] These statistics are not surprising when one reviews the anatomical structure of the shoulder. Being a multiaxial joint capable of complex movements, the shoulder is prone to a vast number of different pathologies. These include adhesive capsulitis (‘frozen shoulder’), any number of arthritides (osteoarthritis, rheumatoid arthritis, polymyalgia rheumatica, etc.), several inflammatory conditions, and impingement syndromes of different etiological sites. [3] Of all the different pathologies affecting the shoulder, impingement syndromes are the most common, especially those involving the rotator cuff tendons. [4–6] Several recent studies have shown that these conditions can be successfully managed with conservative therapies, including chiropractic care. [7–11] Foremost among these therapies are mobilization and ischemic compression techniques.
In addition to a review of the relevant anatomy of the shoulder, the author provides a review of the relevant literature, as well as drawing upon his own clinical experience with respect to the successful management of patients with shoulder pain and dysfunction. It is the author’s intent to provide the reader with a therapeutic model focussing on ischemic compression for the management of those patients presenting with shoulder pain of myofascial origin.
Anatomy review
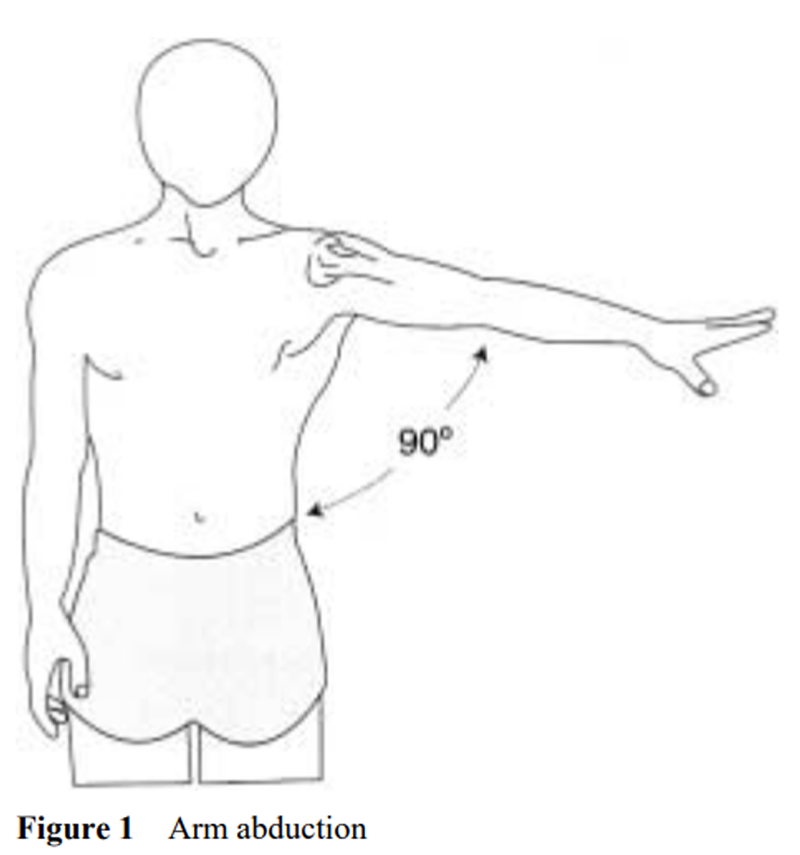
Figure 1 The shoulder is a complex, ball and socket synovial joint, comprised of the humerus, scapula and the clavicle. The labrum is a ring of fibrocartilage that surrounds and deepens the glenoid cavity of the scapula. The resting position of the glenohumeral joint is 55’ of abduction and 30’ of horizontal adduction. [12, 13] When relaxed, the humerus sits in the upper part of the glenoid cavity; with contraction of the rotator cuff muscle, it is pulled down in the lower aspect of the glenoid cavity. It is this ‘dropping down’ that permits abduction (Figure 1). There are three joints that are intimately involved with shoulder mechanics, permitting its multiaxial movements. These are the sternoclavicular joint, the acromioclavicular joint and the glenohumeral joint. [12, 13] In addition, although not a true joint, the scapulothoracic ‘joint’ functions to allow maximal shoulder motions, particularly abduction. [12, 13] What makes the shoulder unique among all the joints of the body is that its support, stability and integrity depend on muscles rather than bones or ligaments. [13]
Biceps
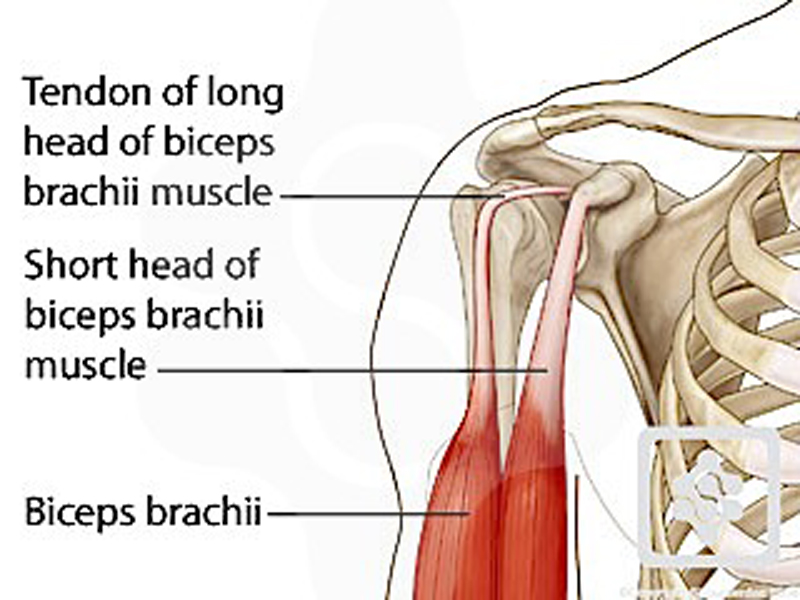
Rotator Cuff Several large muscles influence the stability and movement of the shoulder joint. For example, the tendon of the long head of the biceps muscle originates from the upper edge of the glenoid cavity, traverses anterior to the head of the humerus along the bicipital groove and inserts into the radial head. [12] Other important muscles involved with normal shoulder mechanics are the deltoid, trapezius, levator scapulae, pectoralis and rhomboid muscles. [12] However, recent studies have shown that it is the group of muscles known as the rotator cuff that is most commonly involved in myofascial pathologies of the shoulder. [4–6, 14, 15]
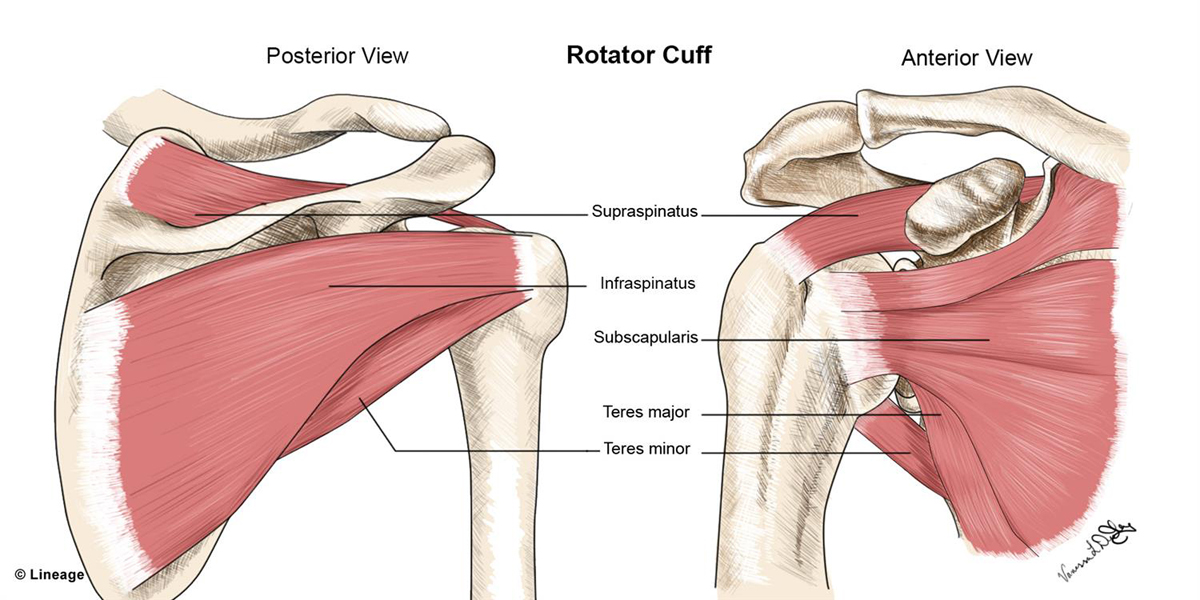
The rotator cuff muscle group is comprised of the supraspinatus, infraspinatus, teres minor and subscapularis muscles (the SITS muscles). Each muscle originates on different aspects of the scapula, and crosses the glenohumeral joint. The supraspinatus, infraspinatus, and teres minor each inserts into the greater tubercles of the humerus, whereas the subscapularis muscle inserts into the lesser tubercle of the humerus. [12] In addition to initiating most shoulder motions, the SITS muscles also serve to stabilize the glenohumeral joint. [13] The subacromial bursa is located between the tendons of the rotator cuff muscles and acromion, providing a frictionless surface upon which the tendons can glide during shoulder motions. [12, 13]
According to Kalb, [14] ninety-five percent of all cases of shoulder pain are attributable to the tendons of the rotator cuff becoming impinged between the greater tuberosity of the humerus and the anterior edge of the acromion, especially during motions that position the arm above the head. Thus, impingement syndromes are the most frequent types of shoulder pathology, and are often the result of the cumulative effect of the rotator cuff tendons constantly passing under the acromion hood. [14]
Clinical presentation
In a recent article, Norregaard et al. [15] suggested that there is terminology chaos within the field of shoulder pathologies, and even trained clinicians may disagree about the diagnosis when examining the same patient. Clinical conditions involving the rotator cuff muscles may interchangeably be referred to as rotator cuff tendonitis, supraspinatus tendonitis, impingement syndromes and subacromial pain syndrome. These authors go on to state that, since many of the orthopedic tests used to examine the shoulder are only cursorily validated, there is no consensus on clinical criteria. This had led to the use of different clinical criteria among those epidemiological studies conducted in this area. [15]
A patient experiencing an impingement syndrome usually presents with pain in the anterolateral region of the deltoid, which then radiates to the lateral upper arm. [4, 10] The pain typically does not radiate below the elbow. The pain is often worse at night, and is aggravated if the patient positions the arm over his or her head. [4, 10] Other pathognomonic signs of an impingement syndrome include crepitus, tenderness of the supraspinatus tendon, and a ‘painful arc’ experienced between 60 to 120 degrees of abduction, although the painful arc may also be observed in cases of subacromial bursitis. [11–14] However, the drop-arm or Codman’s test is positive only in cases of rotator cuff injury. For this test, the patient is asked to slowly lower his or her arm from a position of 90’ of abduction. A positive sign is indicated if the patient is unable to slowly lower the arm to the side of their body, or if he or she experiences severe pain while attempting to do so. [13] Other orthopedic tests that are often pain producing for patients with impingement syndromes are the Hawkins-Kennedy test (arm flexed to 90’ and forcibly medially rotated) and the Neer test (arm forcibly elevated through forward flexion). [13] According to Neer, [16] there are three consecutive pathological stages associated with an impingement syndrome. These are:(i) inflammation, edema and hemorrhage of the tendon,
(ii) fibrosing and thickening of the sub-acromial tissue, accompanied by partial tearing of the supraspinatus tendon and
(iii) tearing of the rotator cuff and osteophyte formation.Since the 1980s, a number of authors have discussed the importance of myofascial pain syndromes (MPS). [17–25] Within health care circles, MPS is now recognized as a leading cause of musculoskeletal pathologies, and it should be suspected in any patient suffering from chronic pain. [17] The most characteristic symptom of MPS is the presence of palpable nodules sensitive to digital pressure. Typically, the patient exhibits a jump sign if a sensitive nodule is palpated. [15] These nodules, which represent focal, hypersensitive points within a muscle, are referred to as trigger points (TPs). [21, 23] When compressed, they give rise to a characteristic pattern of referred pain distant from the point of contact. The pain is diffuse and often radiates to an area representing the symptomatic site. [25] In almost all cases, digital pressure on the painful point will reproduce the symptoms of the chief complaint, or even worsen the level of reported pain. The area of maximum tenderness, often approximately 1 square centimeter in size, is referred to as a tender spot (TS). [23] In other words, tender spots differ from trigger points in that the former are defined as discrete areas of soft tissue that are painful to about 4 kg of palpatory pressure, whereas the latter are defined as hyperirritable spots located within a taut band of skeletal muscle that are painful to compression and give rise to characteristic referred pain patterns and autonomic symptoms. [23] However, it should be noted that even experts find it difficult to distinguish between trigger points and tender points and no reliable diagnostic criteria have been established for myofascial pain syndromes. [15]
Both tender spots and trigger points may exist in muscle tendon, ligament, fascia or fibrous articular capsule. [25]
Differential diagnoses
Contrary to popular belief, partial or complete tearing of the rotator cuff is often asymptomatic. [26] For example, Sher [26] reported that, of 96 asymptomatic patients examined using MRI imagery, 15% had complete tearing of the rotator cuff, with an additional 20% showing signs of partial tearing. In that study, the frequency of tearing increased with the age of the patient. Of the 46 patients examined over the age of 60 years, 28% had a complete tear of the rotator cuff, and 26% had partial tears. These findings led Sher to conclude that tears of the rotator cuff often are compatible with normal painless use of the shoulder. [26]
The symptomatic characteristics of biceps tendonitis are pain and inflammation of the tendon of the long head of the biceps. The pain is felt along the anterolateral aspect of the shoulder. The biceps tendon will often be painful as it travels along the bicipital groove of the humerus. [10] Neer recently reported that one-third of patients suffering from impingement syndromes demonstrated bicipital tendon anomalies pre-operatively. [16] Both Yerguson’s test (resisted forearm supination with elbow flexed to 90’) and Speed’s test (resisted shoulder forward flexion) are often positive. [13] The author has found that bicipital tendonitis is a common finding among patients in private practice. For example, of 25 patients randomly selected who were experiencing shoulder pain, 21 displayed signs of bicipital tendon hyperirritability.
Other pathologies commonly found in the shoulder involve the muscles or tendons of supraspinatus and subscapularis. These can be differentiated by the Empty can test (resisted abduction with arm at 90’ abduction and medial rotation) and Lift-off sign (patient asked to lift hand off his or her lower back) respectively. [13]
Another common condition affecting the shoulder is adhesive capsulitis (frozen shoulder). [11, 27–30] Adhesive capsulitis is characterized by severe limitations of all shoulder motions with both active and passive movements. [27, 28] It is this limitation of passive motion that differentiates adhesive capsulitis from impingement syndromes. The etiology of frozen shoulder is often idiopathic, [4] but may be subsequent to trauma, periods of emotional stress, surgery, and other medical pathologies (diabetes, thyroid disease, myocardial infarction, cerebrovascular accident, and so on). [30] Plain film x-rays are typically unremarkable. [30] Paradoxically, according to Kozin, [27] upon examination, the capsule demonstrates neither inflammation nor adhesions. Although the natural history of adhesive capsulitis is for it to resolve on its own without treatment, this may take anywhere from 6 months to 2 years amd some patients may suffer residual discomforts for even longer. [28]
Some experts have cited shoulder joint calcification as a possible cause of shoulder pain. [31] However, in a study of patients with shoulder bone calcification, Welfing reported that of 925 symptomatic shoulder cases, 63 patients (6.8%) had some evidence of calcification. [31] By contrast, in another study of 200 asymptomatic patients, 7.5% had calcific deposits in the shoulder. This led the investigators to conclude that the frequency of shoulder calcification is virtually identical in both symptomatic and asymptomtic patients. [31]
Lastly, shoulder pain may originate from the spine or the viscera. Shoulder pain of cervicogenic origin is suspected in cases where neck movements (flexion, extension, rotation and lateral flexion) reproduce the chief complaint. [13, 32] Conversely, shoulder pain originating from the shoulder seldom radiates to the neck. Furthermore, shoulder pain may stem from the thoracic or lumbar spine [33] and pathologies of the gall bladder (cholecystitis) have been known to refer pain to the shoulder. [34]
Management technique: medical
Green recently carried out a systematic review of the 31 clinical trials investigating the effectiveness of various therapeutic interventions for shoulder pain. [11] These included anti-inflammatory medications, intra-articular cortisone injections, physiotherapy, manipulation under anesthesia, hydrodilation and surgery. According to Green, only sub-acromial cortisone injections were found to be more effective than placebo to increase abduction. This led Green to conclude that there was little scientific evidence to support the effectiveness of many of the most commonly used medical therapies for shoulder pain. [11] Similarly, Hanten et al. posited that, although ice, heat, ultrasound and massage are routinely used for temporary relief for patients with trigger points, there are no controlled studies that support their use to decrease pain in symptomatic patients. [9]
Roubal et al. reported on their results for patients experiencing adhesive capsulitis using glenohumeral gliding manipulation under anesthesia. [8] In that study, 8 patients (4 men and 4 women ranging in age from 31 to 55 years) with symptoms of adhesive capsulitis from 3 to 16 months duration underwent interscalene brachial nerve block and were immediately sent for manipulation by a physiotherapist. The authors reported that all patients experienced improvement in shoulder flexion, abduction, external and internal rotation, as well as overhead activities, dressing activities, and hair care. In addition, 5 patients prior to manipulation reported positive impingement signs. None of these patients had positive impingement signs postmanipulation and at the time of discharge. Unfortunately, the authors did not comment on whether or not patients experienced any adverse effects as the result of the anesthesia. [8]
Management techniques: chiropractic
Favoring techniques that are low-tech, non-invasive and hands-on, chiropractors typically use cryotherapy, mobilization, manipulation and soft tissue techniques for the management of disorders of the spine and peripheral joints. [1, 35] Among the most popular method of treatment of myofascial pain syndromes is ischemic compression. This approach, also known as Pennel’s technique, Nimmo technique, trigger point therapy or acupressure has been used by chiropractors and other manual therapists for at least 40 years. [1] According to the 2000 Job Analysis of the National Board of Chiropractic Examiners, over 90% of chiropractors use trigger point therapy for passive adjustive care, 68% use acupressure, and 40% report using NIMMO or Receptor tonus technique. [1] It should also be mentioned chiropractors often provide patient education, lifestyle modifications and ergonometric suggestions to augment the care administered in office. [1]
Several studies have demonstrated that inactivation of TPs or TSs often alleviates the pain the patient is experiencing immediately, although some studies suggest that these results may last for up to 2 years. [17] Travel and Simons are among the leading experts in the area of trigger point therapy, and they have described the characteristic pain pattern associated with different muscle groups. [25] Active trigger points in the supraspinatus muscle, for example, often produce a deep pain in the medial region of the deltoid. Trigger points of the infraspinatus muscle often cause pain in the anterior region of the deltoid, and TPs of the teres minor muscle often lead to pain in the posterior deltoid. Trigger points originating from deltoid muscle itself often result in local pain.
Leahy has provided a slightly different method to treat myofascial symptoms, especially those causing mechanical compromise of peripheral nerves. [7] First described as a myofascial release technique, Leahy now refers to his soft therapy method as Active Release Therapy (ART). The distinguishing feature of ART is that, unlike other myofascial techniques, ART requires the patient to perform particular actions while the practitioner applies a static pressure along the length of the affected muscle. In one study, Leahy et al. reported that this technique is very effective for peripheral nerve entrapment conditions such as carpal tunnel and thoracic outlet syndromes. The only reported side effect is considerable pain or discomfort that may exceed the pain tolerance of some patients. [7]
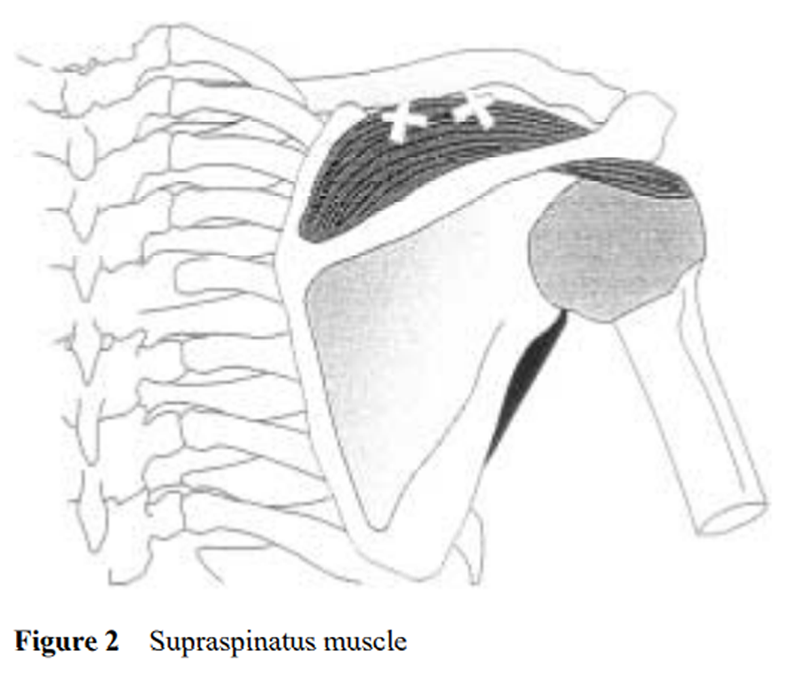
Figure 2
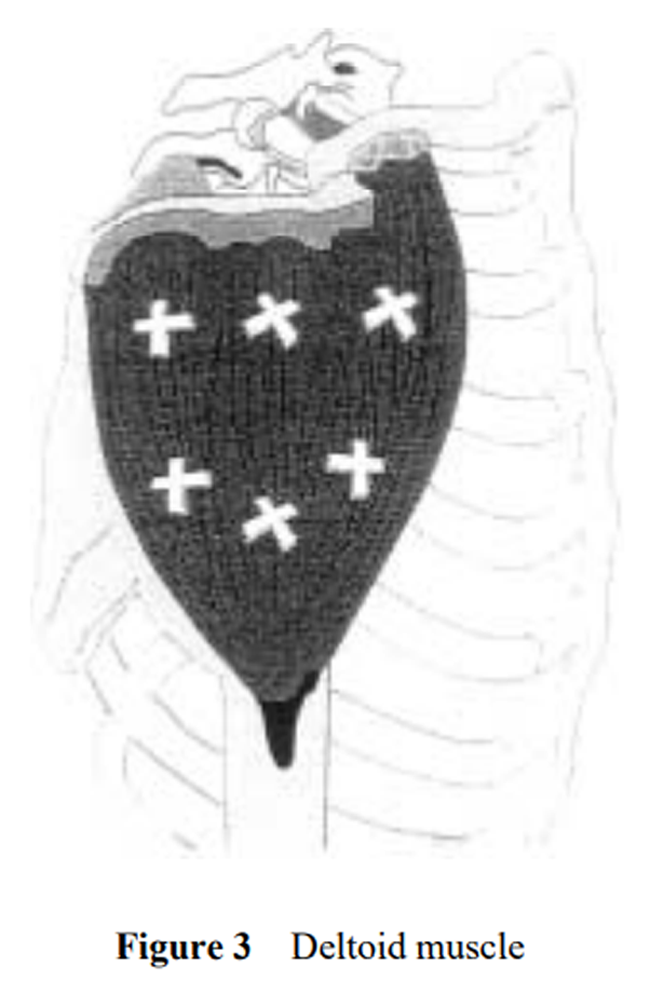
Figure 3
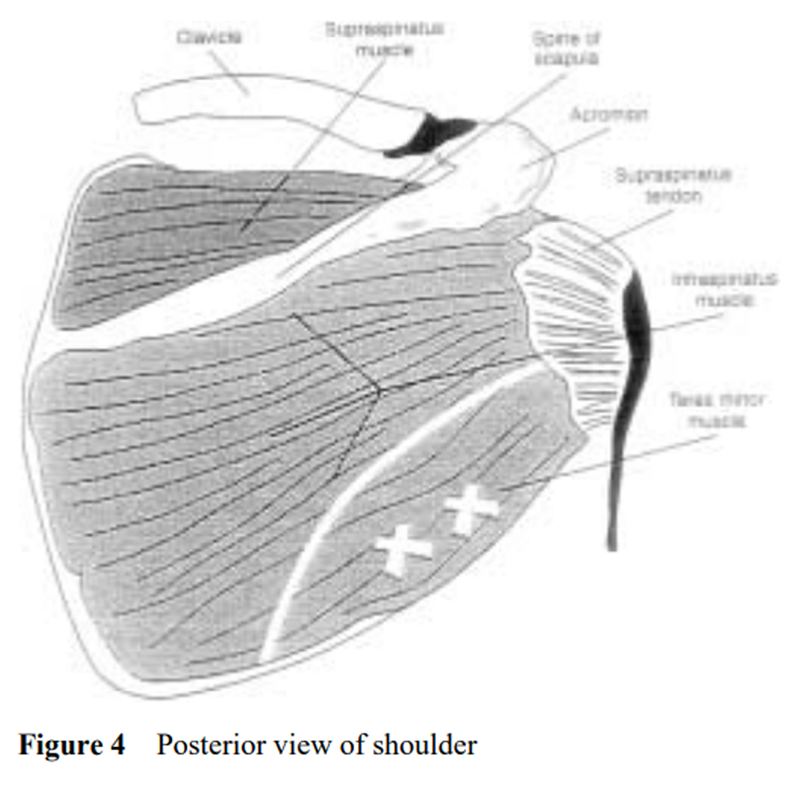
Figure 4
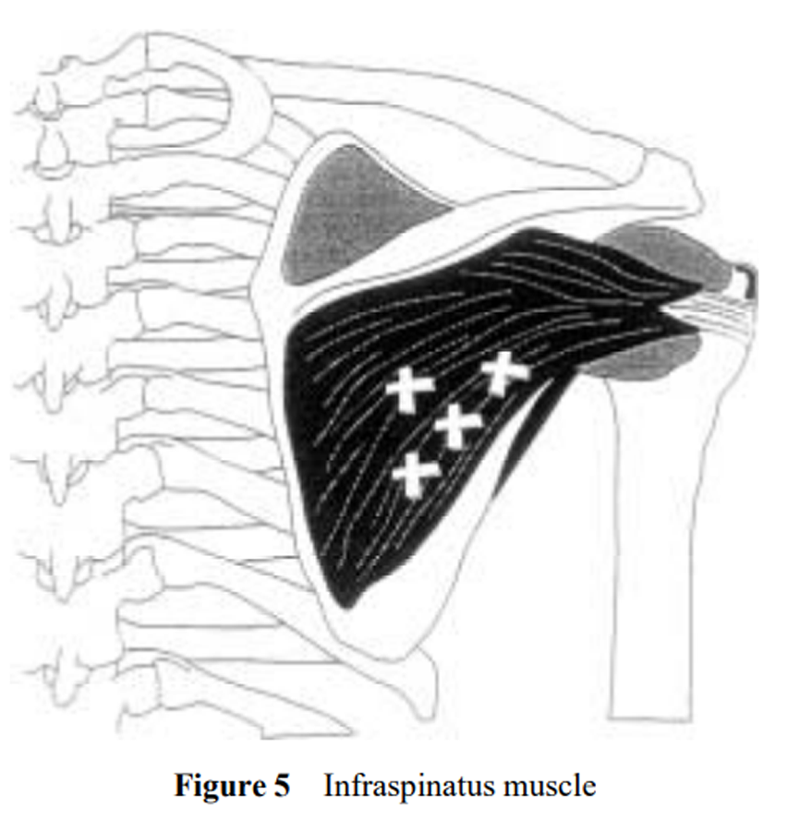
Figure 5
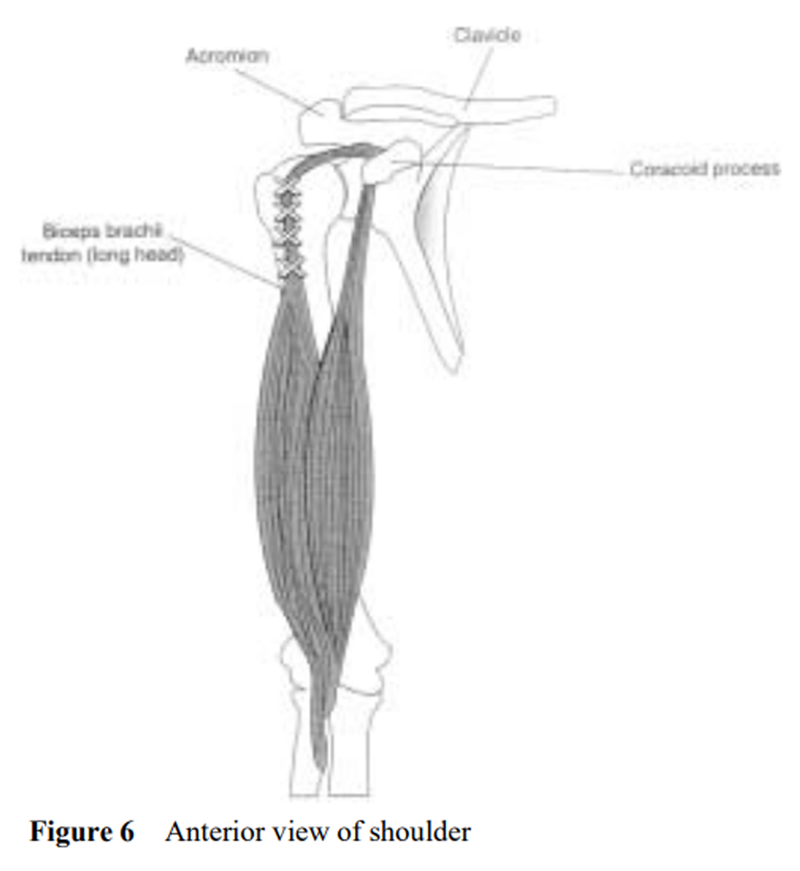
Figure 6 Example of ischemic compression technique
During clinical practice, the author has found it to be most beneficial to exam the entire shoulder complex, and to provide ischemic compression to any trigger points elicited. The author relies on both his palpatory skills and patient reaction to static pressure in order to identify the muscle groups in need of treatment, and has developed specific protocols. According to the author, the anatomical locations mentioned below are the focus of most of the major irritation points in shoulder pain. Once the TGs and TSs are localized only these points are treated at each visit.
Supraspinatus (Figure 2): While prone, the patient’s arm is flexed, pronated and placed on his or her head. The patient’s arm is allowed to rest on the practitioner’s knee. The practitioner then applies digital pressure along the posterior aspect of the clavicle, with special attention given to elicited trigger points.
Deltoid (Figure 3): The patient’s arm is placed in the same position as it is for the supraspinatus. The practitioner applied digital pressure along the entire surface of the deltoid.
Teres minor (Figure 4): While prone, the patient’s arm is flexed and braced along the side of his or her body. Using his or her thigh, the practitioner can brace the patient’s arm in this position while applying digital pressure along the inferolateral aspect of the scapula.
Infraspinatus (Figure 5): The patient’s arm is placed in the same position as it is for treatment of the teres minor muscle. The practitioner applies pressure along the region below the spine of the scapula.
The coracoid process (Figure 6): The patient is placed in supination, the arms along the side of the body. The therapist uses his thigh to maintain pressure on the patient’s arm in order to ensure that the arm is fully relaxed. This position is the same for the examination of the whole front part of the shoulder.
The tendon of the long head of the biceps (Figure 6): The tendon originates from the upper edge of glenoid cavity and transverse anterior to the head of the humerus along the bicipital groove. TSs are often located along that tendon over a length of 2 to 3 centimeters.
During each of these maneuvers, the practitioner applies digital pressure to areas of elicited pain for between 5 and 15 seconds. The practitioner should begin with light, firm pressure and gradually increase it until the pressure reaches the patient’s maximum pain tolerance. Pressure should be evenly applied and only once to each trigger point each treatment session. Elicited pain to the area of the chief complaint confirms the diagnosis.
In general, the duration of applied digital pressure varies inversely with the number of elicited trigger points. For example, if many trigger points are elicited, each should be held for less time than if few trigger points were found. This is because there are limits to what a patient can endure in any treatment session. Leahy recommends treatment schedules not exceed every other day to permit tissue healing between appointments. [7] Treatments are continued until trigger points are no longer elicited with digital palpation. In the author’s experience, this may require in chronic cases 15 to 30 treatments. Besides minor pain or tenderness of limited duration in the area treated, no serious side effects are associated with this type of therapy. In addition, the application of ischemic compression for myofascial trigger points is not very strenuous on the practitioner.
Home-care
Home-care is important to augment the effectiveness of treatments received in office. Hanten et al. [9] recently conducted a study to determine the effectiveness of a home program of ischemic pressure followed by sustained stretching for the treatment of myofascial trigger points. Forty adults (17 men, 23 female) aged 23 to 58 years who had one or more trigger points in the neck or upper back were randomly placed in two groups. One group received a 5-day program consisting of ischemic pressure followed by sustained stretching of the neck and upper back muscles. The other group (control group) performed only active range of motion exercises. The group of patients who were to include muscle stretching were instructed to maintain a constant, sustained pressure unitl the muscle felt like it was ‘letting go’ or ‘melting’. Patients were assessed using a pressure algometer to monitor trigger pain sensitivity (also referred to as pressure pain threshold in this study) and a pain visual analog scale (VAS) prior to the 5-day program and three days following it. The patients in the treatment group showed statistically significant improvements in terms of VAS pain scores and pressure pain threshold. No differences were found between the groups in terms of the percentage of time in pain. Based on the results obtained from their study and a review of the literature, the authors concluded that a home care program involving stretching of affected muscles is necessary to provide patients with long term pain relief. [9]
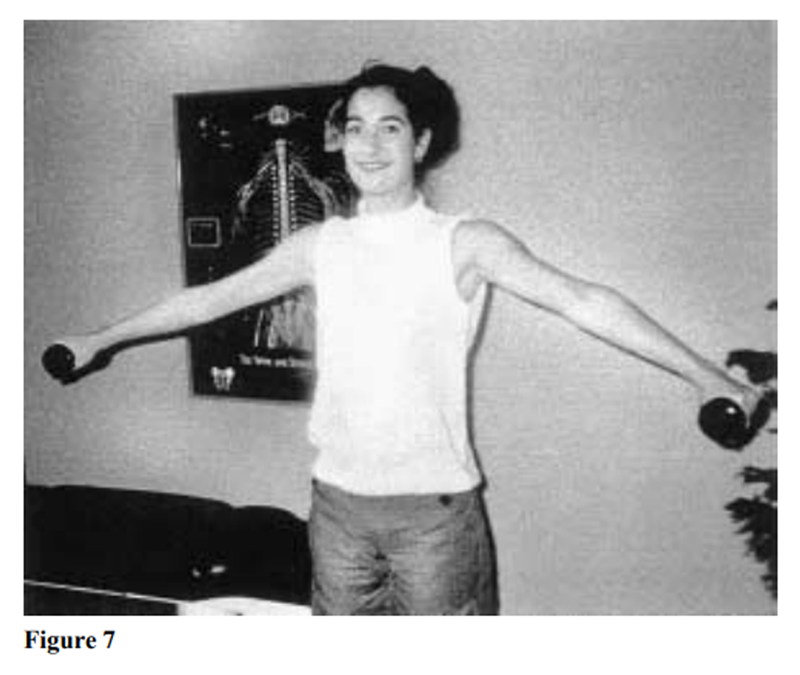
Figure 7 In the author’s experience, hand-held weights can be used in order to stretch the affected muscles, and to increase their strength (Figure 7). However, the author cautions patients to slowly and gradually increase the amount of weight used, and the range of motion covered. For example, at the beginning of their treatment program in office, the author advises patients not to lift a 1 or 2-kg hand weight beyond 90’ of abduction, and to perform this exercise only once or twice a day. At the beginning, 10 to 15 abductions may be the maximum number possible without suffering from fatigue or excessive pain. As strength increases, the patient can gradually increase to 50 abductions a day.
Summary
This article described a therapeutic approach to successfully manage a patient with shoulder pain of myofasical origin using ischemic compression techniques. It can either be the primary mode of therapy, or it may augment other therapeutic interventions the practitioner may wish to use, such as mobilization and manipulation. This approach allows for patient feedback in order to enhance the accuracy of the diagnosis, it helps guide the practitioner towards the clinical target and it ensure the tolerability of digital pressure during the treatment itself. Apart from its historical attractiveness, this soft tissue approach has been shown to be an effective, safe and well tolerated approach to manage shoulder pain, especially when combined with a home exercise program.
Acknowledgement
The author very gratefully acknowledges the expertise of Dr. Brian Gleberzon DC in reviewing and assisting with this paper
References:
Christensen MG.
Job Analysis of Chiropractic 2000
National Board of Chiropractic Examiners 2000.
Greeley, Co. p 78–79.McDermott FT.
Repetitive strain injury: a review of current understanding.
Med J Australia 1986; 144:196–200.Souza TA.
Differential diagnosis and management for the chiropractor:
Protocols and algorithms. 2nd Ed.
Aspen Pub. Gaithersburg, Maryland. 2001;165–168, 179–189.Curtis AS, Wilson P.
Shoulder pain in the work place.
Orthopedic Clinics of North America 1996; 27:763–781.Farber JF, Singleton SB, Hawkins RJ.
Rototor cuff disease: Diagnosing a common cause of shoulder pain.
J Musculoskeletal Med 1998; 15:15–25.Bergman TF, Conley RN, Davidson WT.
Grand Rounds: Right shoulder pain in a 73 year old man.
JNMS 1997; 5:74–81.Leahy MP, Mock LE.
Myofascial release technique and mechanical compromise
of peripheral nerves of the upper extremity.
Chiropractic Technique 1992; 6(4):139–150.Roubal PJ, Dobritt D, Placzek JD.
Glenohumeral gliding manipulation following interscalene
brachial plexus block in patients with adhesive capsulitis.
JOSPT 1996; 24(2):66–76.Hanten WP, Olson SL, Butts NL, Nowicki AL.
Effectiveness of a home program of ischemic pressure followed
by sustained stretch for treatment of myofascial trigger points.
Physical Therapy 2000; 80(10):997–1003.Daigneault J, Cooney LM.
Shoulder pain in older people.
J Am Geriatr Soc 1998; 46:1144–1151.Green S, Buchbinder R, Glazier R, Forbes A.
Systematic review of randomized controlled trials of intervention
for painful shoulder: selection criteria, outcome assessment, and efficacy.
BMJ 1998; 316:354–360.Moore KL, Dalley AF.
Clinically Oriented Anatomy. 4th ed.
Lippincott, Williams and Wilkins. Baltimore, MA. 1999:664–830.Magee DJ.
Orthopedic Physical Assessment. Third Ed.
WB Saunders Co. Philadelphia, PA. 1997:175–246.Kalb RL.
Evaluation and treatment of shoulder pain.
Hospital Practice 1998; 119–122.Norregaard J, Jacobsen S, Kristensen JH.
A narrative review on classification of pain conditions of the upper extremity.
Scand J Rehab Med 1998; 31:153–164.Neer CS.
Anterior acromioplasty for the clinic impingement syndrome in the shoulder.
J Bone Joint Surgery 1972; 54:41–50.Imamura M, Fischer M, Imamura S.
Treatment of myofascial pain components of plantar fascitis
speeds up recovery: documentation by algometry.
J Musculoskeletal Pain 1998; 6:91–110.Simons DG.
Clinical and etiological update of myofascial pain from trigger points.
JMPT 1996; 4:93–121.Duarte M.
Primary fibromyalgia syndrome and myofascial pain syndrome:
clinical features and criteria for diagnosis.
Chiropractic Technique 1989; 1(3):97–100.Goldenberg D.
Fibromyalgia, chronic fatigue and myofascial pain syndromes.
Current opinion.
Rheumatology 1992; 4:247–257.Fischer A.
Algometry in diagnosis of musculoskeletal pain evaluation
of treatment outcomes: An update.
Musculoskeletal Pain 1998; 6:5–32.Russell IJ.
The reliability of algometry in the assessment of
patients with fibromyalgia syndrome.
J Musculoskeletal Pain 1998; 6:139–152.Schneider M.
Tender points/ fibromyalgia vs. trigger points/ myofascial pain syndromes.
A need for clarity in terminology and differential diagnosis.
JMPT 1995; 18:398–406.Hains G, Hains R.
Combined ischemic compression and spinal manipulation in
the treatment of fibromyalgia.
JMPT 2000; 24:225–230.Travel JG, Simons DG.
Myofascial pain and dysfunction: The trigger points manual.
Williams and Wilkins, Baltimore.1983. Vol 1:2Sher JS, Uribe JW, Posada A et al.
Abnormal findings on magnetic resonance images of asymptomatic shoulders.
J Bone Joint Surgery 1995; 77A:10–15.Kozin F.
Two unique shoulder disorders, adhesive capsulitis and
reflex symptomatic dystrophy syndrome.
Post-Graduate Med 1986; 73:207–216.Polkington BS.
Chiropractic Treatment of Frozen Shoulder Syndrome
(Adhesive Capsulitis) Utilizing Mechanical Force,
Manually Assisted Short Lever Adjusting Procedures
J Manipulative Physiol Ther 1995 (Feb); 18 (2): 105–115Pearsal AW, Speer KP.
Frozen shoulder syndrome:
diagnostic and treatment strategies in the primary care setting.
Med and Science in Sports and Exercise 1998; 30:S33–39.Kazemi M.
Adhesive capsulitis: a case report.
J Can Chiropr Assoc 2000; 44(3):169–176.Welfing J, Kahn MF, Desroy M et al.
Les calcifications de l’epaule.
Revue du Rhumatisme 1965; 32:325–334.Ginn KA, Herbert RD, Khoum W, Lee R.
A randomized, controlled clinical trial of a treatment of shoulder pain.
Physical Ther 1997; 77:802–809.Young JL, Herring SA, Press JM, Casazza BA.
The influence of the spine on the shoulder in the throwing athlete.
J Back Musculoskeletal Rehab 1996; 7:5–17.Seidel HM, Ball JW, Dains JE. Benedict GW.
Mosby’s guide to physical examination. 4th ed.
St. Louis, MI. 1999:546Hawk C, Byrd L, Jansen RD et al.
Use of complementary health care practices among chiropractors in the United States.
Altern Ther Heatlh Med 1999; 5(1):56–62.
Return to SHOULDER
Return to MYOFASCIAL TRIGGER POINTS
Since 3-10-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |