

Association Between Utilization of Chiropractic Services for
Treatment of Low-Back Pain and Use of Prescription OpioidsThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Altern Complement Med. 2018 (Jun); 24 (6): 552–556 ~ FULL TEXT
James M. Whedon, DC, MS, Andrew W.J. Toler, MS, Justin M. Goehl, DC, MS, and Louis A. Kazal, MD
Health Services Research,
Southern California University of Health Sciences,
Whittier, CA.
OBJECTIVE: Pain relief resulting from services delivered by doctors of chiropractic may allow patients to use lower or less frequent doses of opioids, leading to reduced risk of adverse effects. The objective of this investigation was to evaluate the association between utilization of chiropractic services and the use of prescription opioid medications.
DESIGN: The authors used a retrospective cohort design to analyze health insurance claims data.
SETTING: The data source was the all payer claims database administered by the State of New Hampshire. The authors chose New Hampshire because health claims data were readily available for research, and in 2015, New Hampshire had the second-highest age-adjusted rate of drug overdose deaths in the United States.
SUBJECTS: The study population comprised New Hampshire residents aged 18-99 years, enrolled in a health plan, and with at least two clinical office visits within 90 days for a primary diagnosis of low-back pain. The authors excluded subjects with a diagnosis of cancer.
OUTCOME MEASURES: The authors measured likelihood of opioid prescription fill among recipients of services delivered by doctors of chiropractic compared with nonrecipients. They also compared the cohorts with regard to rates of prescription fills for opioids and associated charges.
RESULTS: The adjusted likelihood of filling a prescription for an opioid analgesic was 55% lower among recipients compared with nonrecipients (odds ratio 0.45; 95% confidence interval 0.40-0.47; p < 0.0001). Average charges per person for opioid prescriptions were also significantly lower among recipients.
CONCLUSIONS: Among New Hampshire adults with office visits for noncancer low-back pain, the likelihood of filling a prescription for an opioid analgesic was significantly lower for recipients of services delivered by doctors of chiropractic compared with nonrecipients. The underlying cause of this correlation remains unknown, indicating the need for further investigation.
KEYWORDS: analgesics; chiropractic; low-back pain; opioid
From the FULL TEXT Article:
Introduction
Epidemic of opioid prescribing
More aggressive pain management efforts that began in the 1990s have led to an epidemic of prescriptions for opioid pain medications in the United States (U.S.). More than 650,000 opioid prescriptions are dispensed per day in the United States. [1] An estimated one out of five patients with noncancer pain or pain-related diagnoses is prescribed opioids in office-based settings. Prescribing rates are high among providers of pain medicine, surgery, and physical medicine/ rehabilitation, but overall, primary care clinicians account for nearly 50% of opioid prescriptions. [2]
Safety
There is little evidence that opioids improve chronic pain, function, or quality of life, and long-term use of opioids, particularly at higher dosages, is associated with overdose, misuse, abuse, and opioid use disorder. [3] Other adverse effects include tolerance, physical dependence, increased sensitivity to pain, constipation, nausea, vomiting, drymouth, sleepiness, dizziness, confusion, depression, anxiety, itching and sweating, and lower sex drive and energy in men due to reduced testosterone levels. [4] Previous use of prescription opioids is also linked to an increased risk of heroin abuse and addiction. [5] After as few as 5 days of taking opioids, the chance of an opioid-naive patient being a chronic opioid user sharply increases. Even 1 day of opioid exposure carries with it a 6% chance of being on opioids 1 year later, increasing to 13.5% by 8 days and 29.9% by 31 days. [6] Among drug overdose deaths in the United States in 2014, 28,647, 61% involved an opioid. [7] The Centers for Disease Control and Prevention (CDC) reported that prescription opioid consumption and related deaths tripled from 1999 to 2010. [8] Opioids were involved in 75% of pharmaceutical overdose deaths in 2010, [9] and in 2015 over 22,000 deaths involving prescription opioids were recorded—an increase of 19,000 deaths over the previous year. [10]
Costs
The economic impact of the opioid epidemic was estimated to be nearly $56 billion in health and social costs in 2007, and since that time the problem has grown considerably. [11] Sales of prescription opioids in the United States nearly quadrupled from 1999 to 2014, [12] but without any overall change in the amount of pain patients reported. [13] Efforts aimed at curbing the opioids epidemic (including new prescribing guidelines, monitoring programs, enhanced access to treatment of opioid use disorder treatment, screening protocols, treatment contracts, urine testing, regulatory supervising of pain clinics, and law enforcement strategies) have failed to reduce rates of prescribing, misuse, and overdose. [7, 14, 15]
A pain management alternative: services provided by doctors of chiropractic
Little attention has been paid to the potential of nonpharmacologic pain treatment as an upstream strategy for addressing the opioids epidemic. The Institute of Medicine has recommended the use of nonpharmacologic therapies as effective alternatives to pharmacotherapy for patients with chronic pain. [16] Among U.S. adults prescribed opioids, 59% reported having back pain. [17] Recently published clinical guidelines from the American College of Physicians recommend nonpharmacologic treatment as the first-line approach to treating back pain, with consideration of opioids only as the last treatment option or if other options present substantial harm to the patient. [18] A recent systematic review and meta-analysis found that for treatment of acute low-back pain, spinal manipulation provides a clinical benefit equivalent to that of NSAIDs, with no evidence of serious harms. [19] Spinal manipulation is also shown to be an effective treatment option for chronic low-back pain. [20]
Association between utilization of chiropractic services and use of prescription opioids
A retrospective claims study of 165,569 adults found that utilization of services delivered by doctors of chiropractic was associated with reduced use of opioids. [21] More recently, it was reported that the supply of chiropractors as well as spending on spinal manipulative therapy is inversely correlated with opioid prescriptions in younger Medicare beneficiaries. [22] This finding suggests that increased availability and utilization of services delivered by doctors of chiropractic could lead to reductions in opioid prescriptions. It has been reported that services delivered by doctors of chiropractic may improve health behaviors [23] and reduce use of prescription drugs, [21] but it remains uncertain how the utilization of such services may influence patient use of opioid analgesics. Pain management services provided by doctors of chiropractic may allow patients to use lower or less frequent doses of opioids, leading to lower costs and reduced risk of adverse effects.
The objective of this investigation was to evaluate — among New Hampshire residents with low-back pain — the association between utilization of services provided by doctors of chiropractic and the use of prescription opioid medications. The authors chose New Hampshire because health claims data were readily available for research, and in 2015, New Hampshire had the second highest age-adjusted rate of drug overdose deaths in the United States, a 31% increase from the previous year and more than double the national rate. [7, 24] The opioid addiction crisis in New Hampshire crosses all socioeconomic levels, affecting the life of every resident, and has many "hidden" side effects in addition to overdose deaths. Opioid use can lead to self-neglect and neglect of loved ones, child and elder abuse, and newborn withdrawal, as well as unemployment and homelessness. Other associated ill-health effects include HIV, Hepatitis C, liver damage, and heart problems. [25]
Practical solutions to this societal crisis are urgently needed. The authors expected this study to generate the outcome that among patients with low-back pain, recipients of services delivered by doctors of chiropractic have a lower likelihood of using prescription opioids, compared with nonrecipients. Such a finding could exert a positive impact on the value of care for patients with low-back pain by pointing to a strategy for reducing unnecessary care, lowering costs, and improving safety.
Materials and Methods
The authors hypothesized that recipients of services delivered by doctors of chiropractic have a lower likelihood of filling a prescription for an opioid analgesic compared with nonrecipients of services delivered by doctors of chiropractic. To test this hypothesis, they used a retrospective cohort design to analyze health insurance claims data. The data source was the all payer claims database administered by the Department of Health and Human Services of the state of New Hampshire, which aggregates health claims data submitted by 26 private and public third-party payers, including preferred provider organizations, health maintenance organizations, and indemnity insurance plans. No Medicare or Medicaid claims were included in the database. This project was conducted subject to the terms of a data user agreement between the principal investigator and the state of New Hampshire. The research methods were reviewed and approved by the Institutional Review Board of the investigator’s university. All statistical analyses were performed using SAS (SAS Institute, Cary, NC).
The study population comprised New Hampshire residents aged 18–99 years, enrolled in a health plan in 2013 and 2014, and with at least two clinical office visits within 90 days for a primary diagnosis of low-back pain in 2013. (Subjects with more than one such 90-day period and those with more than two office visits per period were not excluded. Thus, the population included subjects with multiple office visits for low-back pain.) The authors excluded subjects with a diagnosis of cancer in 2013 or 2014. Among those included in the study population as defined above, they identified two cohorts of subjects:(1) recipients of services provided by doctors of chiropractic (recipients) were defined as subjects with at least two office visits for a primary diagnosis of low-back pain, for which the provider was a doctor of chiropractic.
(2) Nonrecipients were defined as subjects who received no services provided by a doctor of chiropractic.Following establishment of the cohorts with claims for low-back pain in 2013 data, the authors first compared the cohorts with regard to rates of prescription fills for opioids and associated charges in both 2013 and 2014. Next, they modeled for likelihood of opioid prescription fill in 2014 only to maintain the temporal relationship between inclusion in the cohort and measuring the outcomes. To reduce the potential for selection bias because the cohorts may have differed with regard to their disposition toward use of prescription medications, they used weighted propensity scoring to create equivalent cohorts for comparison. [26] The authors used multiple logistic regression to calculate the estimated probability of each subject to be in each cohort using sociodemographic measures (age, sex, and county of residence). After inversely weighting each subject by the propensity to be in the cohort, they used logistic regression to compare recipients to nonrecipients with regard to likelihood of opioid prescription fill in 2014. They controlled for patient demographics and health status through Charlson comorbidity scoring. Both univariate and multivariate logistic models were developed.
Results

Table 1
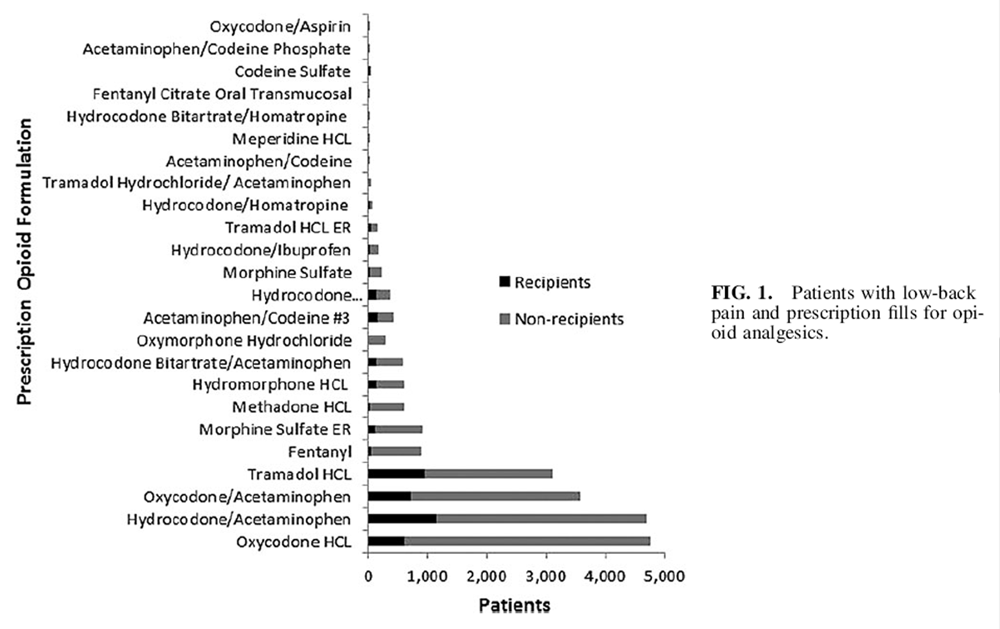
Figure 1

Table 2 Subject characteristics are tabulated in Table 1. The population was almost equally divided between recipients and nonrecipients of services provided by doctors of chiropractic. The cohorts did not differ by sex. Recipients included a larger proportion of young adults and a smaller proportion of middle-aged adults, compared with nonrecipients. The recipients’ cohort was healthier, as measured by Charlson comorbidity score.
The study population comprised 13,384 subjects,with roughly equivalent distribution between cohorts (Table 1). Among 6,868 recipients, 19% of subjects filled a prescription for a prescription opioid, compared with 35% of 6,516 nonrecipients. Figure 1 illustrates comparative proportions of subjects who filled prescriptions for opioid analgesics, by specific formulation. All categories of charges were significantly lower for recipients compared with nonrecipients (Table 2). In 2013, average annual charges per person for filling opioid prescriptions were 74% lower among recipients compared with nonrecipients. For clinical services provided at office visits for low-back pain, average annual charges per person in 2013 were 78% lower among recipients compared with nonrecipients. The authors found similar between-cohort differences in charges in 2014: annual charges per person were 78% lower for opioid prescriptions and 71% lower for clinical services among recipients compared with nonrecipients.
The adjusted likelihood of filling a prescription for an opioid analgesic in 2014 was 55% lower among recipients compared with nonrecipients (odds ratio 0.45; 95% confidence interval 0.40–0.47; p < 0.0001). The authors evaluated both univariate and multivariate logistic models. In models without the propensities and/or Charlson adjustment, they found only small changes in effect, suggesting that the strength of the association between exposure and outcome was independent of case mix.
Discussion
With regard to the use of prescription opioids as well as charges for both opioid prescriptions and clinical services for low-back pain, they found impressive between-cohort differences. However, they were only able to evaluate the correlation between the utilization of services provided by doctors of chiropractic and use of prescription opioids. It was not possible from the available data to infer whether or not utilization of services provided by doctors of chiropractic actually caused a reduction in the likelihood of filling an opioid prescription. The underlying cause of the negative correlation between utilization of chiropractic services and likelihood of opioid prescription fill is unknown.
Despite the use of propensity scoring to create equivalent cohorts for comparison, part of the reported effect upon likelihood of prescription fills may have resulted from the cohorts being drawn from different populations, that is, subject characteristics may have differed by cohort due to an unknown factor or factors that confounded the reported correlation. Recipients of services provided by doctors of chiropractic may differ from nonrecipients with regard to beliefs, attitudes, and predisposition to use prescription medications. In a recent national poll, 78% of U.S. adults indicated a preference for alternatives to prescription pain medication, and adults who had never seen a chiropractor were among those most likely to prefer pharmacologic pain treatments. [27] The underlying reasons for such patient preferences are unknown, and further evaluation of differences between patients who do and do not choose pharmacologic therapies for pain may point toward solutions to the opioids crisis. The preponderance of health outcomes result not from clinical interventions, but from personal health behaviors, as well as social and environmental determinants of health. Finally, it is unknown to what extent the effect of exposure to utilization of services provided by doctors of chiropractic may be modified by various aspects of care, including spinal manipulation and other treatments, the chiropractor’s recommendations regarding diet and exercise and other influences associated with chiropractic care. Certain limitations of the research dataset must also be acknowledged. In general, only a limited number of exposure variables were available. No fill dates or diagnoses were available in the pharmacy data. Finally, the authors emphasize that the safety of services provided by doctors of chiropractic was not assessed in this study.
Conclusion
Among New Hampshire adults with office visits for noncancer low-back pain, the adjusted likelihood of filling a prescription for an opioid analgesic was 55% lower for recipients of services provided by doctors of chiropractic compared with nonrecipients. The underlying cause of this correlation is unknown. Average charges per person for chiropractic users — for both opioids and office visits for low-back pain — were also significantly lower compared with nonusers over a 2-year period. Further investigation of these associations should be conducted through analysis of longitudinal data from multiple U.S. states to ascertain the generalizability of these findings and should use rigorous methods to minimize risk of bias.
Acknowledgments
This project was funded by the Council on Chiropractic Guidelines and Practice Parameters/Clinical Compass. Data for this research were supplied by The NH Insurance Department and NH Department of Health and Human Services. All the conclusions and recommendations of this publication are solely those of the authors.
Author Disclosure Statement
No competing financial interests exist.
References:
Centers for Disease Control and Prevention.
The Opioid Epidemic: By the Numbers
U.S. Department of Health and Human Services, 2016. Online document at:
https://www.hhs.gov/sites/default/files/Factsheet-opioids-061516.pdf
accessed April 17, 2017.Daubresse M, Chang HY, Yu Y, et al.
Ambulatory diagnosis and treatment of nonmalignant pain in the United States, 2000–2010.
Med Care 2013;51:870–878.Chou R, Turner JA, Devine EB, et al.
The effectiveness and risks of long-term opioid therapy for chronic pain: A systematic review for a National Institutes of Health Pathways to Prevention Workshop.
Ann Intern Med 2015;162:276–286.Prescription Opioids.
Centers for Disease Control and Prevention, 2016. Online document at:
https://www.cdc.gov/drugoverdose/opioids/prescribed.html
accessed April 18, 2017.Al-Tayyib AA, Koester S, Riggs P.
Prescription opioids prior to injection drug use: Comparisons and public health implications.
Addict Behav 2017;65:224–228.Shah A, Hayes CJ, Martin BC.
Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006–2015.
MMWR Morb Mortal Wkly Rep 2017;66:265–269.Rudd RA, Aleshire N, Zibbell JE, Gladden RM.
Increases in drug and opioid overdose deaths—United States, 2000–2014.
MMWR Morb Mortal Wkly Rep 2016;64:1378–1382.Figure 28.
Deaths Involving Opioid Analgesics.
Centers for Diseases Control and Prevention, Department of Health and Human Services, 2014.
Online document at:
www.cdc.gov/nchs/hus/chartbook.htm
accessed February 1, 2016.Opioids drive continued increase in drug overdose deaths. 2013.
Online document at:
www.cdc.gov/media/releases/2013/p0220_drug_overdose_deaths.html
accessed February 2, 2016.Opioid Data Analysis.
Centers for Diseases Control and Prevention, 2016. Online document at:
https://www.cdc.gov/drugoverdose/data/analysis.html
accessed May 1, 2017.Birnbaum HG, White AG, Schiller M, et al.
Societal costs of prescription opioid abuse, dependence, and misuse in the United States.
Pain Med 2011;12:657–667.Centers for Disease Control and Prevention (CDC).
Vital signs: Overdoses of prescription opioid pain relievers—United States, 1999—2008.
MMWR Morb Mortal Wkly Rep 2011;60:1487–1492.Chang HY, Daubresse M, Kruszewski SP, Alexander GC.
Prevalence and treatment of pain in EDs in the United States, 2000 to 2010.
Am J Emerg Med 2014;32:421–431.Deyo RA, Von Korff M, Duhrkoop D.
Opioids for low back pain.
BMJ 2015;350:g6380.Raji MA, Kuo Y, Chen N, et al.
Impact of laws regulating pain clinics on opioid prescribing and opioid-related toxicity among Texas Medicare Part D beneficiaries.
J Pharm Technol 2017;33 60–65.Institute of Medicine (IOM)
Relieving Pain in America: A Blueprint for Transforming Prevention,
Care, Education, and Research
Washington, DC: The National Academies Press, 2011.Hudson TJ, Edlund MJ, Steffick DE, et al.
Epidemiology of regular prescribed opioid use: Results from a national, population-based survey.
J Pain Symptom Manage 2008; 36:280–288.Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Paige NM, Myiake-Lye IM, Booth MS, et al.
Association of Spinal Manipulative Therapy with Clinical Benefit and Harm
for Acute Low Back Pain: Systematic Review and Meta-analysis
JAMA. 2017 (Apr 11); 317 (14): 1451–1460Rubinstein SM, van Middelkoop M, Assendelft WJ, et al.
Spinal manipulative therapy for chronic low-back pain.
Cochrane Database Syst Rev 2011;2:CD008112.Rhee Y, Taitel MS, Walker DR, Lau DT.
Narcotic drug use among patients with lower back pain in employer health plans: A retrospective analysis of risk factors and health care services.
Clin Ther 2007;29:2603–2612.Weeks WB, Goertz CM.
Cross-Sectional Analysis of Per Capita Supply of Doctors of Chiropractic
and Opioid Use in Younger Medicare Beneficiaries
J Manipulative Physiol Ther 2016 (May); 39 (4): 263–266Gray CM, Tan AW, Pronk NP, O’Connor PJ.
Complementary and alternative medicine use among health plan members. A cross-sectional survey.
Eff Clin Pract 2002;5:17–22.Hedegaard H, Warner M, Minino AM.
Drug overdose deaths in the United States, 1999–2015.
NCHS Data Brief 2017:1–8.Opioid Misuse Prevention, Treatment, and Recovery.
New Hampshire Department of Health and Human Services, 2017. Online document at:
https://www.dhhs.nh.gov/dcbcs/bdas/opioids.htm
accessed April 17, 2017.Weeks, WB, Tosteson, TD, Whedon, JM et al.
Comparing Propensity Score Methods for Creating Comparable Cohorts of Chiropractic Users and Nonusers
in Older, Multiply Comorbid Medicare Patients With Chronic Low Back Pain
J Manipulative Physiol Ther. 2015 (Nov); 38 (9): 620–628Gallup, Palmer College of Chiropractic.
Gallup-Palmer College of Chiropractic Annual Report
Americans’ Views of Prescription Pain Medication and Chiropractic Care.
Washington, DC: Gallup. Inc., 2017.
Return to LOW BACK PAIN
Return to THE OPIOID EPIDEMIC
Since 2-25-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |