

Exposure to a Motor Vehicle Collision and the Risk
of Future Back Pain: A Systematic Review and Meta-AnalysisThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Accident; Analysis and Prevention 2020 (May 18); 142: 105546 ~ FULL TEXT
OPEN ACCESS Paul S Nolet, Peter C Emary, Vicki L Kristman, Kent Murnaghan, Maurice P Zeegers, Michael D Freeman
Care and Public Health Research Institute,
Maastricht University,
Maastricht, Netherlands;
Department of Graduate Education and Research,
Canadian Memorial Chiropractic College,
Toronto, Ontario, Canada

Objective: The purpose of this study is to summarize the evidence for the association between exposure to a motor vehicle collision (MVC) and future low back pain (LBP).
Literature survey: Persistent low back pain (LBP) is a relatively common complaint after acute injury in a MVC, with a reported 1 year post-crash prevalence of at least 31 % of exposed individuals. Interpretation of this finding is challenging given the high incidence of LBP in the general population that is not exposed to a MVC. Risk studies with comparison control groups need to be examined in a systematic review.
Methodology: A systematic search of five electronic databases from 1998 to 2019 was performed. Eligible studies describing exposure to a MVC and risk of future non-specific LBP were critically appraised using the Quality in Prognosis Studies (QUIPS) instrument. The results were summarized using best-evidence synthesis principles, a random effects meta-analysis and testing for publication bias.
Synthesis: The search strategy yielded 1,136 articles, three of which were found to be at low to medium risk of bias after critical appraisal. All three studies reported a positive association between an acute injury in a MVC and future LBP. Pooled analysis of the results resulted in an unadjusted relative risk of future LBP in the MVC-exposed and injured population versus the non-exposed population of 2.7 (95 % CI [1.9, 3.8]), which equates to a 63 % attributable risk under the exposed.
Conclusions: There was a consistent positive association in the critically reviewed literature that investigated the risk of future LBP following an acute MVC-related injury. For the patient with chronic low back pain who was initially injured in a MVC, more often than not (63 % of the time) the condition was caused by the MVC. These findings are likely to be of interest to clinicians, insurers, patients, governments and the courts. Future studies from both general and clinical populations would help strengthen these results.
Keywords: Injury; Low back pain; Motor vehicle collision; Risk; Systematic review; Whiplash.
From the FULL TEXT Article:
Introduction
Low back pain (LBP) is common in the general population and globally is the leading cause of years lived with disability [Vos et al., 2012. LBP ranks six out of the 291 diseases in terms of total burden of health as measured by disability adjusted life years examined in the Global Burden of Disease study [Murray CJL et al., 2012]. In 2010, the global average point prevalence of LBP over all age groups was 9.4 %, and was slightly higher in men (10.1 %) than women (8.7 %) [Hoy et al., 2014]. In the adult general population, the annual incidence of LBP was 18.6 % with 1% rated as “intense” and 0.4 % resulting in disability [Cassidy et al., 2005]. The course of LBP in adults can be persistent (40.2 %) and have a high rate of recurrence at six months in individuals who had previously recovered (28.7 %) [Cassidy et al., 2005]. Unsurprisingly, the economic burden of LBP on health care systems is high [Hoy et al., 2014] and can impact health-related quality of life [Nolet et al., 2015].
Several large studies have demonstrated that low back sprain/strain is one of the most common injuries after a MVC. Based on a national study of >21,000 injury claims occurring the USA over a 2 week period, the Insurance Research Council report a 58 % rate of LBP after a MVC injury, second by only a small margin to neck pain after a MVC (66 %) [Insurance Research Council, 2008]. This was a similar low back injury rate reported in a cohort study in Saskatchewan, Canada, among individuals who reported an injury-producing traffic collision to an insurance company within 30 days (60.4 %) [Hincapié et al., 2010]. Recovery from LBP after a low back injury in a MVC is often prolonged or incomplete, with 31 % still having LBP 12 months after the acute injury [Cassidy et al., 2003]. Given the high incidence and prevalence of LBP in the non-MVC exposed population, it is reasonable for the clinician, insurer, or court presented with an individual with persisting LBP months or years after a traffic crash-related acute low back injury, to inquire as to the likelihood of the chronic LBP if the crash had not occurred. The answer to such a question is found within controlled observational studies, and the means to characterize the sum of the evidence is with systematic review and meta-analysis of the results. As no such review and analysis exists at the present time, the objective of the research presented herein is to estimate the difference in risk of future LBP among the population exposed to a MVC relative to the population that has not been exposed to a MVC.
Methods
Population
Epidemiologic studies with subjects aged 16 years of age and older who were involved in a prior MVC and which included an appropriate comparison group were included for review. LBP was defined as pain or discomfort below the costal margin (level of the lower ribs) and above the inferior gluteal folds, with or without referred leg pain [Duthey, 2013]. This systematic review included papers including participants with non-radicular LBP, radicular LBP and LBP with mid/upper back (thoracic) pain.
Exposure
The exposure was defined as subjects that had been involved in a MVC or injured in a MVC. Injury in a MVC could refer either to self-reported in a survey, reported to an insurer or associated with a diagnosis provided by a health care provider. The injury in a MVC can include injury to the neck region or injury to the back region and does not indicate injury to a specific tissue such as bone, disk, joint, ligament, muscle, or nerve.
Study designs
The review was restricted to cohort and case-control study designs that assessed the risk of a MVC on future non-specific LBP.
Inclusion criteria1) written in the English language;
2) published between January 1, 1998 to February 27, 2019;
3) published in a peer-reviewed journal;
4) examined the association between injury in a MVC (or involvement in a MVC) and future LBP;
5) used a case-control or cohort design;
6) included a study population including participants 16 years of age or older and if studies included a mixed population with individuals less than 16 years of age, results must have been stratified for adults 16 years of age and older.
Exclusion criteria1) publication types including: books and book chapters, commentaries, conference proceedings, consensus development statements, dissertations, editorials, government reports, guidelines, lectures and addresses, letters, meeting abstracts and unpublished manuscripts;
2) study designs including: systematic reviews and non-systematic reviews, cross-sectional studies and case studies;
3) studies with less than 20 human participants with LBP, or less than 20 participants at risk of LBP; and
4) LBP related to fractures or dislocations, infections, inflammatory joint disease, myelopathy, systematic disease, or tumors.
Data sources and searches
The search strategy was developed in consultation with a health sciences librarian. A second librarian was consulted using the Peer Review of Electronic Search Strategies (PRESS) checklist [McGowan et al., 2020]. The following electronic databases were systematically searched from January 1st, 1998 to February 27, 2019: PUBMED, EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL, SPORTDISCUS and MEDLINE (EBSCO). Search terms consisted of subject headings specific to each database (e.g. MeSH in MEDLINE) and free text words relevant to low back pain/back injuries, motor vehicle accidents, incidence, prevalence, and risk factors (Appendix A). Hand searched papers were included if they met the inclusion and exclusion criteria.
Study selection
Relevant citations were identified in a two stage process by two independent reviewers (PN and PE). In the first stage titles and abstracts were reviewed for relevant, possibly relevant and irrelevant citations. In the second stage, possibly relevant citations from stage one screening were reviewed in full text screening to determine if the papers were relevant. Disagreements between reviewers at either selection stages were discussed between the reviewers to try to reach consensus. Citations were screened by a third reviewer (MF) where consensus could not be reached or where a reviewer was an author on a paper being reviewed. The study selection process followed the methodology used in a previous systematic review and meta-analysis on exposure to a motor vehicle collision and future neck pain by the same authors [Nolet et al., 2019].
Assessment of risk of bias
Relevant studies were critically appraised by two reviewers (PN and PE) using the Quality in Prognosis Studies Appraisal Tool (QUIPS) [Hayden et al., 2013] that was modified to assess the internal validity of the risk studies. Studies where the first two reviewers could not reach consensus or where a reviewer was an author on a study were critically appraised by a third reviewer (MF). Studies with adequate internal validity and limited risk of bias were included in the best evidence synthesis and meta-analysis. Studies with limited risk of bias were classified according to their methodology into phases of risk [Hogg-Johnson et al., 2008]. Phase I studies are hypothesis generating studies that are exploratory describing crude associations between a history of injury in a MVC and future LBP. Phase II studies are exploratory using multivariable models or stratification to identify risk factors related to the onset of LBP and a history of injury in a MVC while adjusting for confounding (variables that could potentially affect both the MVC outcome and the injury outcome and result in a spurious relationship between the two). Phase III studies are confirmatory incidence studies that have a priori hypotheses which confirm independent risk factors for LBP after adjusting for confounding [Hogg-Johnson et al., 2008].
Data extraction and synthesis of results
Evidence tables were created by one reviewer (PN) using data from studies screened with the modified QUIPS tool and the tables were reviewed by a second reviewer (PE). The evidence was reported using a best evidence synthesis using qualitative synthesis with evidence statements [Slavin, 1995]. Summary statements were formulated using the evidence from the summary table to make comparisons and outline the best available evidence. Random effects meta-analysis was performed using data pooled from the studies.
Statistical analyses
Kappa coefficient (k) with 95 % confidence intervals (CI) were calculated for inter-rater reliability for the screening of citations. Classifying studies into high or low risk of bias following independent critical appraisal between reviewers was calculated using percentage agreement. Random effects meta-analysis for relative risk (RR) of the pooled studies and tests for heterogeneity (Cochran’s Q and I²) and absolute risk difference (ARD) used MedCalc Statistical Software, version 18.6. Tests for publication bias (Funnel plot and Egger regression) used Comprehensive Meta Analysis v3.3.070 software (2014). Attributable risk (AR) was calculated using results from the meta-analysis with the following formula: AR = RR-1/RR*100 %(15).
Reporting
This review complies with the Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [Moher et al., 2009]. The protocol for this review has been registered with the PROSPERO registry (CRD42019116359).
Results
Study selection
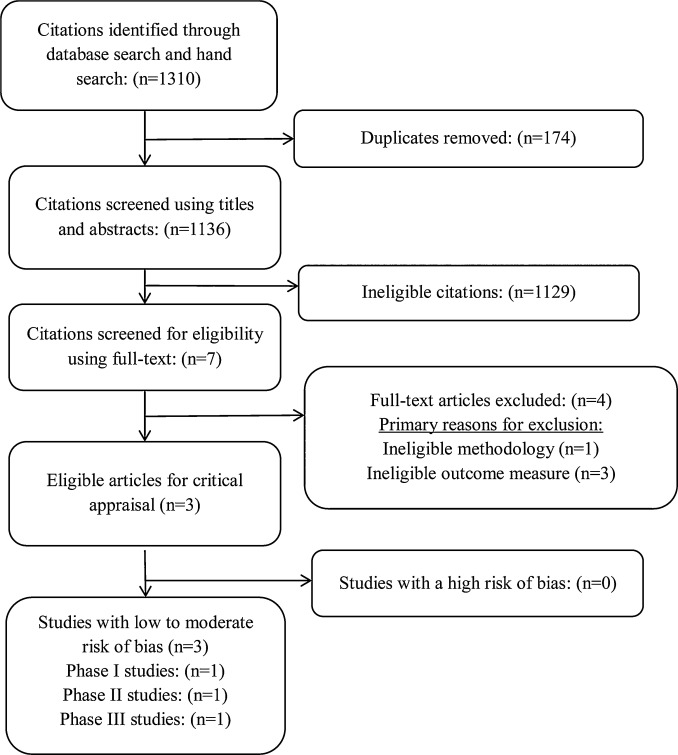
Figure 1 There were 1,310 citations identified, 174 duplicates removed, and 1,136 articles screened for eligibility (Figure 1). In stage one screening, 1,129 citations were deemed ineligible. In the 2nd stage of screening, seven full text papers were reviewed, and four articles were excluded as ineligible: ineligible outcome measures (n = 3) [Chou et al., 2004; Braddom et al., 2020; Odonkor et al., 2018] and ineligible methodology (n = 1) [Fujii and Matsudaira, 2013]. The inter-rater agreement for screening articles was substantial (Cohen’s Kappa = 0.75).
Three articles were critically appraised and all three articles had low to moderate risk of bias and were included in our evidence synthesis and meta-analysis [Berglund et al., 2001; Tournier et al., 2016; Nolet et al., 2018]. The reviewers had perfect agreement on the admissibility of studies (three agreements over three articles appraised).
Study characteristics

Table 1

Table 2 The studies included in the risk of bias analysis were all cohort studies. The studies were from two different types of source populations: insurance/injury databases (2/3 articles) [Berglund et al., 2001; Tournier et al., 2016] and a general population survey (1/3 articles) [Nolet et al., 2018] (Table 1). The duration of time between the MVC and the outcome varied across studies: unknown (1/3 articles) [Nolet et al., 2018], five years (1/3 articles) [Tournier et al., 2016], seven years (1/3 articles) [Berglund et al., 2001] (Table 2).
Exposure was defined in the cohort studies as: exposure to a rear-end collision without injury, exposure to a rear-end collision with neck/shoulder injury and low back injury (1/3 articles) [Berglund et al., 2001], exposure to a whiplash injury in a MVC (1/3 articles) [Tournier et al., 2016] and low back injury in a MVC (1/3 articles) [Nolet et al., 2018]. Exposure to a MVC was determined by: a question on self-reported low back injury in a MVC (1/3 articles) [Nolet et al., 2018], physician diagnosed injury in a public or private health facility (1/3 articles) [Tournier et al., 2016], and collision reported low back injury to an insurance company (1/3 articles) [Berglund et al., 2001]. The control groups were defined as: no prior self-reported low back injury in a MVC [Nolet et al., 2018], randomly selected insured drivers with no recorded prior MVC in the insurance database [Berglund et al., 2001] and other recorded injuries (no neck or low back injuries) in a MVC [Tournier et al., 2016].
The outcome of LBP was measured with: a self-reported question (2/3 articles) [Berglund et al., 2001; Tournier et al., 2016] or a validated questionnaire (1/3 articles) [Nolet et al., 2018]. Studies that controlled or stratified for confounding included: age, gender and other confounders (1/3 articles) [Nolet et al., 2018], age and gender (1/3 articles) [Berglund et al., 2001] and no control for confounding (1/3 articles) [Tournier et al., 2016]. The country the studies were conducted in were: Canada [Nolet et al., 2018], France [Tournier et al., 2016], and Sweden [Berglund et al., 2001].
Studies were classified according to the Task Force on Neck Pain and Its Associated Disorders into 3 phases of analysis for observational studies for risk of exposure to a MVC and LBP [Hogg-Johnson et al., 2008]. The three risk studies included one phase I hypothesis generating study (1/3 articles) [Tournier et al., 2016], one phase II exploratory study (1/3 articles) [Berglund et al., 2001] and one phase III confirmatory study [Nolet et al., 2018] (Table 1).
Assessment of risk of bias

Table 3 Studies with low to moderate risk of bias met the following criteria in six bias domains: study participation, study attrition, MVC exposure, LBP measurement, study confounding and statistical analysis and reporting. One study had low risk of bias in all six domains [Nolet et al., 2018]. The following limitations were noted from the risk assessment: 1) one study (1/3 articles) had moderate risk of bias in the study attrition domain [Tournier et al., 2016] two studies (2/3 articles) had moderate risk of bias in LBP measurement [Berglund et al., 2001; Tournier et al., 2016]; and 3) one study had moderate risk of bias when controlling for confounding (1/3 studies) [Berglund et al., 2001] and one study (1/3 articles) had high risk of bias as they did not control for confounding [Tournier et al., 2016] (Table 3).
Summary of the evidence
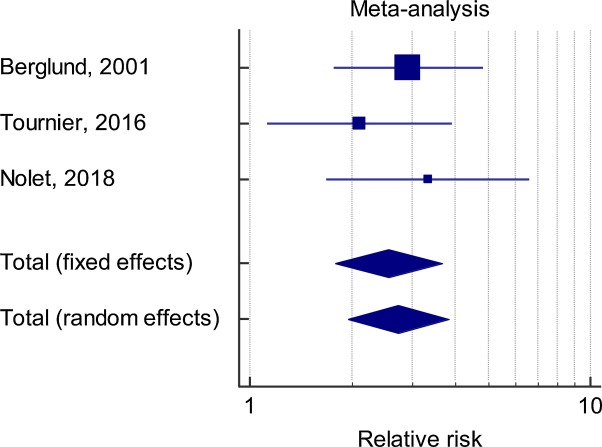
Figure 2 Exposure to an injury in a MVC Three risk studies examined the association between an injury in a MVC and future back pain [Berglund et al., 2001; Tournier et al., 2016; Nolet et al., 2018]. One phase I study found a positive association between a neck injury in a MVC and future back pain when compared to a control group with other MVC injuries: odds ratio (OR) = 2.28 (95 % CI [1.15–4.54]) and ARD = 7.7 % (95 % CI [1.5 %–13.9 %]) [Tournier et al., 2016]. They also found a graded response according to the Quebec classification of injury [Spitzer et al., 1995] between grade I injury (OR = 1.92, 95 % CI [0.76–4.89]) and grade II injury (OR = 3.35, 95 % CI [1.60–7.01]) [Tournier et al., 2016]. One phase II study found a positive association between a low back injury in a rear-end collision and future LBP seven years later when compared to a control group of insured drivers: adjusted RR = 2.9 (95 % CI [1.6–5.2]) and ARD = 22.6 % (95 % CI [6.0 %–39.1 %]) [Berglund et al., 2001]. One phase III study found a positive association between a low back injury in a MVC and future LBP when compared to controls who had not had a low back injury in a MVC: Hazard Rate Ratio (HRR) = 2.25 (95 % CI [1.11–4.56]) and ARD = 15.5 % (95 % CI [6.6 %–17.9 %]) [Nolet et al., 2018]. Random effects meta-analysis found a positive association between injury in a MVC on future LBP across the three studies (RR = 2.7, 95 % CI [1.9–3.8], p = 0.001) (Figure 2).
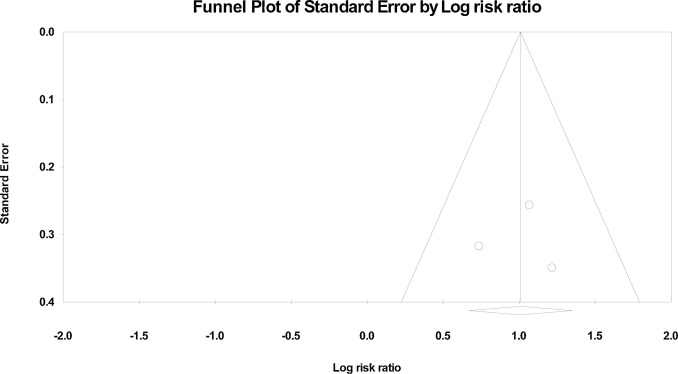
Figure 3 The combined subject count from the three studies in the meta-analysis was n = 265 in the injury group and n = 1918 in the control group. Tests for heterogeneity resulted in a Q of 1.23 (DF 2, p = 0.542) and I² of 0.0 % (95 % CI [0.0 %–94.5 %]) indicating low heterogeneity among the reviewed studies, but the wide confidence intervals may indicate the uncertainty inherent with the low number of studies that were pooled in the meta-analysis. Due to the low number of papers examined in the meta-analysis, further analysis into the potential of heterogeneity could not be examined. The RR of 2.7 (95 % CI [1.9–3.8]) was used to calculate an AR under the exposed of 63 % for individuals with ongoing LBP who had a previous history of injury in a MVC. Publication bias was tested using a funnel plot (Figure 3) and with Eggers regression (Intercept –0.0205, SE 4.71, 95 % CI [–59.8 to 59.8], t-value 0.004, df 1, p = 0.50) indicating no publication bias.
Exposure to a MVC One phase II risk study examined the association between an exposure to a rear-end collision and future LBP. This study did not find an association between exposure to a rear-end collision where the participants did not claim an injury to the insurance company compared to a control group of insured drivers (RR = 0.9, 95 % CI [0.5–1.6]) [Berglund et al., 2001].
Discussion
Summary of results
This study is the first systematic review and meta-analysis to estimate the pooled RR and AR of future LBP in a population of participants who have sustained an injury in a MVC. The evidence from three papers suggests that exposure to an injury in a MVC more than doubles the risk of developing future LBP. The pooled data in a random effects meta-analysis found a positive association between an injury in a MVC and future LBP (RR = 2.7, 95 % CI [1.9–3.8]). The AR among the exposed was determined to be 63 % which meets the legal standard of “more likely true than not” where more than 50 % of the current LBP in those patients previously injured in a MVC was attributable to the MVC [Freeman and Zeegers, 2015]. There was no increased risk of future LBP found in a study examining exposure to a rear-end collision where no claim for an injury was made to an insurance company.
The studies examined in this review selected subjects from different source populations such as the general population [Nolet et al., 2018], insurance and injury databases [Berglund et al., 2001; Tournier et al., 2016] (Table 1). It is important to have studies from different source populations and sampling frames to reduce the potential for misclassification bias of the exposure and increase the generalizability of the results [Guzman et al., 2008]. Injured participants in general population surveys may be missed from insurance and injury databases. Participants who were injured in a MVC may not seek care or report an injury to an insurance company. Conversely, participants responding to a general population survey may not remember their prior MVC injury.
The paper by Nolet et al. [2018] described a 55 % response rate in the baseline survey, but this did not result in substantial selection bias as the survey had low levels of differential response [Cassidy et al., 1998]. Studies can have low risk of selection bias with less than optimal response rates as long as there is no differential enrollment into the study between responders and non-responders [Carroll et al., 2009]. Berglund et al. [2001] had an acceptable response rate and non-responders did not differ with regard to age and gender. The response rate for participants with whiplash injury was 79 %, for participants without whiplash injury was 78 % and 77 % for unexposed control participants. They had a low risk of selection bias as they selected participants from the same population of persons covered by traffic insurance at Folksam [Berglund et al., 2001]. The paper by Tournier et al. [2016] captured participants who had a traffic accident in the Rhône administrative area and had been treated in one of the area hospitals [Tournier et al., 2016]. It is therefore unlikely that selection bias impacted the results of this review.
Studies with lower risk of bias from attrition all had adequate follow-up rates [Berglund et al., 2001; Nolet et al., 2018]. Two studies compared responders to non-responders for non-differential exposure to a MVC made them at low risk to suffer from attrition bias [Berglund et al., 2001; Nolet et al., 2018]. One study had a moderate risk of attrition bias, as only 64.5 % responded to the 5-year questionnaire [Tournier et al., 2016]. The response rates for the whiplash and non-whiplash groups were similar and responders in the whiplash group had similar response rates for both grade I and grade II injuries [Tournier et al., 2016]. It is therefore unlikely that attrition biased the findings of this review.
The measure of exposure to an injury in a MVC varied between studies, with one study using a question on history of self-reported low back injury in a MVC [Nolet et al., 2018], another study used a low back injury that was reported to an insurance company and a third study reported on whiplash associated disorder diagnosed in public or private health facilities in the Rhone region of France [Tournier et al., 2016]. It is possible that self-reported injuries could suffer from misclassification bias, although the reviewers’ consensus was that this risk was low. Some individuals may not remember if they were injured in a prior traffic collision, so the reliability and validity of such as question is important. Three studies reported moderate to substantial test-retest reliability of self-reported questions on a history of injury in a MVC (0.55 ≤ k≤0.80) [Koziol-McLain et al., 2000; Alonso et al., 2006; Pons-Villanueva and Segui-Gómez, 2010].
Further, the validity of self-reported questions on injuries three years earlier recorded in a health systems database was compared to police traffic crash records [Begg et al., 1999]. Participants were able to recall injuries three years earlier compared to a health system database and police traffic crash records: 86 % (95 % CI 68 %–96 %) for unintentional injury; 100 % for the type of car involved; 96 % for the speed limit; 84 % for number of years since the crash [Begg et al., 1999]. In addition, cohort studies, with their longitudinal course, reduce the possibility of differential exposure recall, therefore exposure misclassification in the cohort studies in this review would have resulted in conservative estimates of risk.
In the study by Tournier et al. [2016], subjects with a medically diagnosed neck injuries in a MVC were compared to participants with other medically diagnosed injuries in a MVC (excluding low back injuries). Some in the neck injury group may not have developed LBP which could result in an under-estimation of risk of LBP. This under-estimation of risk was seen in the study by Berglund et al. [2001] where those reporting a neck injury in a rear-end collision had a lower risk of LBP seven years later (adjusted RR = 1.7, 95 % CI [2.1–3.5]) as compared to the group reporting a low back injury in a rear-end collision and the risk of LBP seven years later (adjusted RR = 2.9, 95 % CI [1.6–5.2]) [Berglund et al., 2001]. Neck injury in a rear-end collision resulted in a slightly higher risk of upper/mid back pain seven years later (adjusted RR = 3.1, 95 % CI [2.0–4.8]) [Berglund et al., 2001] as compared to the risk of neck pain seven years after a neck injury in a rear-end collision (adjusted RR = 2.7, 95 % CI [2.1–3.5]) [Berglund et al., 2000].
In the present review, studies where individuals exposed to either a MVC or a MVC-caused acute injury were compared to a comparison group without exposure to a MVC. The recovery of those injured in a MVC can be prolonged but this needs to be interpreted in light of the background prevalence of pain [Carroll et al., 2008]. Those not exposed to a motor vehicle injury are also prone to LBP, so having an appropriate comparison group allows for a determination of excess risk of future prevalent or incident LBP associated with an injury in a MVC. The control group in one study was formed by those with no or mild LBP at baseline who reported no prior history of a low back injury in a MVC [Nolet et al., 2018]. In the study from an insurance database the control groups were selected from insured drivers who had not had a prior history of an injury in a MVC [Berglund et al., 2001] and the study from an injury database selected controls with Abbreviated Injury Scale (AIS) level 1 lesions such as ankle or shoulder sprain, superficial wounds or contusions or tendon tears [Tournier et al., 2016].
It is important in cohort studies to examine the effects of confounding on the association between the exposure to a MVC and the outcome of future LBP. Controlling for confounding in two studies did not have a marked effect on future LBP [Berglund et al., 2001; Nolet et al., 2018]. One of the studies in this review did not control for confounding which may have introduced bias into their results [Tournier et al., 2016]. One study controlled for age and gender using a Mantel-Haenszel technique and found no change between the crude (RR = 1.7, 95 % CI [1.2–2.4]) and age/gender adjusted results (RR = 1.7, 95 % CI [1.3–2.4]) on neck injury in a rear-end collision with LBP seven years later [Berglund et al., 2001]. In a study controlling for a priori confounding (sociodemographic, general health, comorbidities, depression and body mass index) in a Cox model reported some reduction of the association between low back injury in a MVC and future LBP between the crude HRR = 2.76 (95 % CI [1.42–5.39]) and the adjusted HRR = 2.25 (95 % CI [1.11–4.56]). This reduction was accounted for in the Cox model by the effect of self-reported arthritis [Nolet et al., 2018].
The outcome measurement of LBP varied between studies, with two studies having questions with face validity [Berglund et al., 2001; Tournier et al., 2016]. One study asked about LBP with a yes or no question [Tournier et al., 2016] and a second study asked about LBP often or always compared to never or occasionally [Berglund et al., 2001]. These questions could not differentiate the intensity of LBP or disability between the group exposed to an injury in a MVC and the control group. The third study from the general population measured LBP with a validated Chronic Pain Grade Questionnaire (CPQ). The CPQ measures the 6-month point prevalence of LBP and related disability. The outcome of troublesome LBP included participants with high pain intensity/low disability to participants with high disability/severely limiting LBP [Nolet et al., 2018].
The CPQ has been recommended as an outcome measure for pain measurement in surveys due to its established psychometric properties and prognostic implications [Guzman et al., 2008]. There was some variation in the timelines between the exposure to a MVC and the outcome of future LBP in the three studies. Two studies had fixed follow-up times between the exposure and measure of LBP of five years [Tournier et al., 2016] and seven years [Berglund et al., 2001]. One study examined a past history of low back injury in a MVC of an unknown duration prior to the baseline of the studies, following participants for one year [Nolet et al., 2018]. No trends were seen with the timelines between studies.
Two studies compared prevalent, as opposed to incident, LBP at follow-up, between the exposed group and the comparison group [Berglund et al., 2001; Tournier et al., 2016]. Prevalence studies can suffer from prevalence-incidence bias making it more difficult to determine temporality in the association of interest (for example, whether LBP resulted from an injury in a MVC or if LBP occurred prior to a MVC). The episodic nature of LBP makes it difficult to establish a new, incident case [Cassidy et al., 2005]. One study examined incident troublesome LBP in a population at risk with no or mild LBP [Nolet et al., 2018]. Excluding those at baseline with prevalent troublesome LBP, resulted in a more accurate estimate of risk for an incident episode of LBP. This study provides evidence for the causal nature of a LBP after an injury in a MVC, as the incident episode of troublesome LBP occurred sometime after the MVC. This study was unable to control for LBP prior to the MVC which could account for some of the LBP measured at six and 12 months follow-up [Nolet et al., 2018]. In a study examining pain prior to an injury in a MVC, those with more pre-MVC pain related diagnoses were more likely to have considerable neck pain a year after the MVC [Osterland et al., 2019].
Although, this risk maybe lower with LBP. In a prospective inception cohort study, in individuals who had recovered from LBP in the prior three month, the risk of a new episode of LBP (3/10 pain or higher lasting at least 24 h) over the following year increased by 4% with each prior episode of LBP (Hazard Rate 1.04 [95 % CI 1.02–1.07]) [Hancock et al., 2015]. The study by Nolet et al. [2018] minimized the effects of pre-MVC LBP by excluding those with prevalent troublesome LBP at the start of the study and by controlling for baseline LBP in their population at risk (those with no or mild LBP) [Nolet et al., 2018].
Strengths and limitations
This systematic review had several strengths. First, a comprehensive search strategy was used that was developed by a health sciences librarian in conjunction with a content expert and reviewed by an independent health sciences librarian using the PRESS Checklist [McGowan et al., 2020]. Second, the search strategy used several databases with predefined inclusion and exclusion criteria. Third, citations were screened and critically appraised by independent reviewers to reduce bias and error. Finally, trained reviewer used the QUIPS tool to critically appraise the selected studies. The QUIPS tool has moderate to substantial reliability (0.56 ≤ k≤0.82) and has been previously used in the evaluation of risk studies [Hayden et al., 2013].
There were potential limitations to the review, as well. The search was limited to English studies published in 1998 or later. It was not felt that this limitation biased our results, however, as the authors were not aware of any studies published in other languages or published prior to 1998 that would also meet the inclusion and exclusion criteria. Second, there were only three studies that met the criteria for our critical analysis, and this small body of literature may limit the generalizability of the results of the review. Finally, it is possible that reviewers had differences in scientific judgment during the critical appraisal of the studies. This possibility was minimized by the consensus process used to determine the internal validity of the studies along with our high inter-rater agreement (k = 0.75).
Conclusion
We examined the evidence from three studies on the association between exposure to a MVC and future LBP. The three critically appraised studies support the conclusion that there is an increased risk of future LBP in individuals who have been exposed to a prior injury in a MVC compared to individuals without a history of injury in a MVC. The pooled estimate from the studies in the meta-analysis was RR = 2.7 (95 % CI 1.9, 3.8). The estimate of AR from the pooled analysis suggests that for an individual presenting with chronic LBP that has had a past history of an acute MVC-related back injury with no intervening injury, 63 % of the LBP is attributable to the index crash. However, the reviewed literature does not support an association between exposure to a MVC and future LBP where no acute low back injury was reported. These results should help inform patients, clinicians, insurers, governments and the courts on the risk of a MVC on future LBP. Given that only three studies met the criteria for critical appraisal there is a need for additional risk studies, which will allow for more robust findings. Studies from various source populations, such as primary care and emergency departments, would improve the generalizability of the results as well.
CRediT authorship contribution statement
Paul S. Nolet: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing - original draft.
Peter C. Emary: Data curation, Formal analysis, Investigation, Writing - review & editing.
Vicki L. Kristman: Conceptualization, Methodology, Supervision, Writing - review & editing.
Kent Murnaghan: Data curation, Investigation, Writing - review & editing.
Maurice P. Zeegers: Conceptualization, Methodology, Supervision.
Michael D. Freeman: Conceptualization, Formal analysis, Methodology, Supervision, Writing - review & editing.
Declaration of Competing Interest
Dr. Michael D Freeman does medicolegal consultations pertaining to traffic crash-related injuries.
References
Alonso et al., 2006
A. Alonso, S. Laguna, M. Segui-Gomez
A comparison of information on motor vehicle crashes as reported by written or telephone interviews
Inj. Prev., 12 (2006), pp. 117-120Begg et al., 1999
D.J. Begg, J.D. Langley, S.M. Williams
Validity of self reported crashes and injuries in a longitudinal study of young adults
Inj. Prev., 5 (1999), pp. 142-144Berglund et al., 2000
A. Berglund, L. Alfredsson, J.D. Cassidy, I. Jensen, A. Nygren
The association between exposure to a rear-end collision and future neck or shoulder pain: a cohort study
J. Clin. Epidemiol., 53 (11) (2000), pp. 1089-1094Berglund et al., 2001
A. Berglund, L. Alfredsson, I. Jensen, J.D. Cassidy, A. Nygren
The association between exposure to a rear-end collision and future health complaints
J. Clin. Epidemiol., 54 (8) (2001), pp. 851-856Braddom et al., 2020
R.L. Braddom, L. Spitz, M.H. Rivner
Frequency of radiculopathies in motor vehicle accidents
Muscle Nerve, 39 (2009), pp. 545-547Carroll et al., 2008
Carroll LJ , Holm LW , Hogg-Johnson S , et al .
Course and Prognostic Factors for Neck Pain in Whiplash-associated Disorders (WAD):
Results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain
and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S83–92Carroll et al., 2009
Carroll LJ, Hurwitz EL, Cote P, Hogg-Johnson S, Carragee EJ, Nordin M, Holm LW, van der Velde G, Cassidy JD, Guzman J, et al.:
Research Priorities and Methodological Implications: The Bone and Joint Decade
2000-2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S214–S220Cote P, Cassidy JD, Carroll L.
The Saskatchewan Health and Back Pain Survey.
The Prevalence of Neck Pain and Related Disability in Saskatchewan Adults
Spine (Phila Pa 1976). 1998 (Aug 1); 23 (15): 1689–1698Cassidy et al., 2003
J.D. Cassidy, L.J. Carroll, P. Côté, A. Berglund, Å Nygren
Low back pain after traffic collisions: a population-based cohort study
Spine., 28 (10) (2003), pp. 1002-1009Cassidy et al., 2005
J.D. Cassidy, P. Côté, L.J. Carroll, V. Kristman
Incidence and course of low back pain episodes in the general population
Spine, 30 (24) (2005), pp. 2817-2823 2005Chou et al., 2004
L.H. Chou, C.W. Slipman, S.M. Bhagia, L. Tsaur, A.L. Bhat, et al.
Inciting events initiating injection-proven sacroiliac joint syndrome
Pain Med., 5 (1) (2004), pp. 26-32Duthey, 2013
B. Duthey
Background paper 6.24 low back pain
World Health Organisation (WHO) Priority Medicines for Europe and the World ‘A Public Health Approach to Innovation’ (2013)
GenevaFreeman and Zeegers, 2015
M.D. Freeman, M. Zeegers
Principles and applications of forensic epidemiology in the medicolegal setting
Law Probab. Risk (4) (2015), pp. 269-278Fujii and Matsudaira, 2013
T. Fujii, K. Matsudaira
Prevalence of low back pain and factors associated with disabling back pain in Japan
Eur. Spine J., 22 (2013), pp. 432-438Guzman J, Haldeman S, Carroll LJ, et al.
Clinical Practice Implications of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders:
From Concepts and Findings to Recommendations
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S199–S212Hancock et al., 2015
M.J. Hancock, C.M. Maher, P. Petocz, C.W. Lin, D. Steffens, A. Luque-Suarez, J.S. Magnussen
Risk factors for a recurrence of low back pain
Spine, 15 (11) (2015), pp. 2360-2368Hayden et al., 2013
J.A. Hayden, D.A. van der Windt, J.L. Cartwright, P. Côté, C. Bombardier
Assessing bias in studies of prognostic factors
Ann. Intern. Med., 158 (2013), pp. 280-286Hincapié et al., 2010
C.A. Hincapié, J.D. Cassidy, P. Côté, L.J. Carroll, J. Guzmán
Whiplash injury is more than neck pain: a population-based study of pain localization after traffic injury
J. Occup. Environ. Med., 52 (April (4)) (2010), pp. 434-440Hogg-Johnson, S, van der Velde, G, Carroll, LJ et al.
The Burden and Determinants of Neck Pain in the General Population: Results of the
Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S39–51Hoy et al., 2014
Hoy D, March L, Brooks P, et al.
The Global Burden of Low Back Pain: Estimates from the Global Burden of Disease 2010 study
Ann Rheum Dis. 2014 (Jun); 73 (6): 968–974Insurance Research Council, 2008
Insurance Research Council
Trends in Auto Injury Claims: Countrywide Patterns in Treatment, Cost, and Compensation
Malvern, Pa, USA (2008)Koziol-McLain et al., 2000
D. Koziol-McLain, D. Brand, D. Morgan, M. Leff, S.R. Lowenstein
Measuring injury risk factors: question reliability in a statewide sample
Inj. Prev., 6 (2000), pp. 148-150McGowan et al., 2020
J. McGowan, M. Sampson, D.M. Salzwedel, E. Cogo, V. Foerster, C. Lefebvre
PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement
J. Clin. Epidemiol., 75 (2016), pp. 40-46Moher et al., 2009
D. Moher, A. Liberati, J. Tatzlaff, D.G. Altman, P. Grp
Perferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement
Br. Med. J., 89 (9) (2009), pp. 873-880Murray CJL et al., 2012
C.J.L. Murray, T. Vos, R. Lozano, M. Naghavi, A.D. Flaxman, et al.
Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010
Lancet, 380 (2012), pp. 2197-2223Nolet et al., 2015
Nolet PS, Kristman VL, Cote P, et al.
Is Low Back Pain Associated With Worse Health-related Quality of Life 6 Months Later?
European Spine Journal 2015 (Mar); 24 (3): 458–466Nolet et al., 2018
Nolet PS, Côté P, Cassidy JD, Carroll LJ.
The Association Between a Lifetime History of a Neck Injury in a Motor Vehicle Collision
and Future Neck Pain: A Population-based Cohort Study
European Spine Journal 2010 (Jun); 19 (6): 972–981Nolet et al., 2019
P.S. Nolet, P. Emary, V.L. Kristman, K. Murnaghan, M.P. Zeegers, M.D. Freeman
Exposure to a Motor Vehicle Collision and the Risk of Future Neck Pain:
A Systematic Review and Meta-analysis
PM R. 2019 (Nov); 11 (11): 1228–1239Odonkor et al., 2018
C.A. Odonkor, Y. Chen, P. Adekoya, B.J. Marascalchi, H. Chaudhry-Richter, et al.
Inciting events associated with lumbar facet joint pain
Anesth. Analg., 126 (1) (2018), pp. 280-288Osterland et al., 2019
T.B. Osterland, H. Kasch, L. Frostholm, T. Bendix, T.S. Jensen, et al.
Precollision medical diagnoses predict chronic neck pain following acute whiplash trauma
Clin. J. Pain, 35 (2019), pp. 304-314Pons-Villanueva and Segui-Gómez, 2010
J. Pons-Villanueva, M. Segui-Gómez
Validation of self-reported motor vehicle crash and related work leave in multi-purpose prospective cohort
Int. J. Inj. Contr. Saf. Promot., 17 (4) (2010), pp. 223-230Slavin, 1995
R.E. Slavin
Best evidence synthesis: an intelligent alternative to meta-analysis
J Clin Epidmiol., 48 (1) (1995), pp. 9-18Tournier et al., 2016
C. Tournier, M. Hours, P. Charnay, L. Chossegros, H. Tardy
Five years after the accident, whiplash casualties still have poorer quality of life in the physical domain than other mildly injured casualties: analysis of the ESPARR cohort
BMC Public Health, 16 (2016), p. 13Vos et al., 2012
Vos T, Flaxman AD, Naghavi M, et al.
Years Lived with Disability (YLDs) for 1160 Sequelae of 289 Diseases and Injuries
1990-2010: A Systematic Analysis for the Global Burden of Disease Study 2010
Lancet. 2012 (Dec 15); 380 (9859): 2163–2196
Return to LOW BACK PAIN
Return to CHRONIC NECK PAIN
Since 5-30-2020


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |