

Efficacy of Manual and Manipulative Therapy in
the Perception of Pain and Cervical Motion in
Patients with Tension-type Headache:
A Randomized, Controlled Clinical TrialThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Chiropractic Medicine 2014 (Mar); 13 (1): 4—13 ~ FULL TEXT
OPEN ACCESS Espí-López Gemma V., PhD, PT, and Gómez-Conesa Antonia, PhD, PT
Professor, Physiotherapy Department,
University of Valencia, Spain.
OBJECTIVE: The purpose of this study was to evaluate the efficacy of manipulative and manual therapy treatments with regard to pain perception and neck mobility in patients with tension-type headache.
METHODS: A randomized clinical trial was conducted on 84 adults diagnosed with tension-type headache. Eighty-four subjects were enrolled in this study: 68 women and 16 men. Mean age was 39.76 years, ranging from 18 to 65 years. A total of 57.1% were diagnosed with chronic tension-type headache and 42.9% with tension-type headache. Participants were divided into 3 treatment groups (manual therapy, manipulative therapy, a combination of manual and manipulative therapy) and a control group. Four treatment sessions were administered during 4 weeks, with posttreatment assessment and follow-up at 1 month. Cervical ranges of motion pain perception, and frequency and intensity of headaches were assessed.
RESULTS: All 3 treatment groups showed significant improvements in the different dimensions of pain perception. Manual therapy and manipulative treatment improved some cervical ranges of motion. Headache frequency was reduced with manipulative treatment (P < .008). Combined treatment reported improvement after the treatment (P < .000) and at follow-up (P < .002). Pain intensity improved after the treatment and at follow-up with manipulative therapy (P < .01) and combined treatment (P < .01).
CONCLUSIONS: Both treatments, administered both separately and combined together, showed efficacy for patients with tension-type headache with regard to pain perception. As for cervical ranges of motion, treatments produced greater effect when separately administered.
KEYWORDS: Musculoskeletal manipulations; Pain perception; Range of motion; Rehabilitation; Spinal manipulation; Tension-type headache
From the FULL TEXT Article:
Introduction
Tension-type headache (TTH) is the most prevalent type of the primary headache categorized by the International Headache Society, [1] and it is a health problem with great socioeconomic impact. [2, 3] Both episodic tension-type headache (ETTH) and chronic tension-type headache (CTTH) have important repercussions on the quality of life, affecting the working and social spheres, as well as the activities of daily living. [4]
As for the treatments administered, Lenssinck et al [2] carried out a systematic review to assess the effectiveness of physiotherapy and spinal manipulation in the treatment of TTH and showed that there was no conclusive evidence of its effectiveness. However, later studies showed that treatment with manual therapy techniques combined may be effective in reducing the frequency, intensity, and duration of headaches and has a positive influence on the quality of life, disability, and global range of motion. [5–7]
There is evidence of the presence of active trigger points in suboccipital muscles in subjects with CTTH compared with healthy subjects. [8] There is also evidence of the connection between TTH and head-neck musculoskeletal disorders and of a higher intensity and frequency of pressure pain in trapezius muscles. [9] Likewise, the variations in head position are connected with cervical mobility in TTH patients. [10] It has been observed that central sensitization caused by prolonged periods of pain may lead to headache chronification. [11] Tension in suboccipital and neck muscles probably involves limitation of movement in the cervical region; and therefore, knowing the range of motion might be useful as a reference for the quality of neck muscles. The perception of pain and its different dimensions (ie, word descriptors for pain in headache) are aspects that should be assessed in patients with headache to better know the pain sensation experienced by the patient, as this can alter their quality of life.
The aim of this study was to evaluate the efficacy of the treatment with manual and manipulative therapy, administered separately and combined together, in patients with TTH through assessment of frequency, intensity, and perception of pain and cervical ranges of motion and, subsequently, to detect if changes after treatment are maintained at 1 month.
Methods
Four treatment sessions (1 session per week) were administered, with an interval of 7 days. Treatments were carried out by 2 physiotherapists with more than 10 years of experience in the treatment of headache with manual therapy. Each session lasted for approximately 20 minutes.
This study was supervised and approved by the research committee of the University of Murcia. Informed consent of patients was obtained before treatment, and all procedures were conduced according to the Declaration of Helsinki.
Subjects
Eighty-four subjects were initially enrolled in this study; 68 of them were women (81%), and 16 were men (19%). Mean age was 39.76 years (SD 11.38), ranging from 18 to 65 years. A total of 57.1% were diagnosed with CTTH and 42.9% with ETTH. Patients were recruited from January 2010 to December 2010. This study was carried out in a private clinic in Valencia (Spain) that specialized in the physiotherapy treatment of headache. Inclusion and exclusion criteria are shown in Fig 1.
Figure 1. Criteria for inclusion and exclusion in the study.
CTTH, chronic tension-type headache;
ETTH, episodic tension-type headache;
TTH, tension-type headache.
Inclusion criteria Exclusion criteria • Subjects aged between 18 and 65 y • Patients with infrequent ETTH, and patients with probable TTH in its frequent and infrequent forms. • Diagnosis of frequent ETTH and CTTH • Headache that is aggravated by head movements. • Having headache episodes on more than 1 d/mo • Metabolic or musculoskeletal disorders with symptoms similar to headache • Headache episodes lasting from 30 min to 7 d • Previous neck trauma • Headaches having at least 2 of the following characteristics: • Vertigo, dizziness, arterial hypertension. -Bilateral location of pain • Joint stiffness, arteriosclerosis, or advanced degenerative osteoarthritis -Pressing non pulsating quality • Patients with heart devices -Mild or moderate intensity • Patients in process of pharmacological adaptation -Not aggravated by physical activity • Excessive emotional tension • Sufferers may present photophobia, phonophobia, nausea, or vomiting • Neurological disorders • Headache may be associated with pericranial tenderness • Laxity of neck soft tissues • Suffering from TTH for over 3 mo • Radiological alterations • Subjects being under pharmacological control • General hypermobility or hyperlaxity • Joint instability • Pregnancy Study Design
The study was a 4 × 3 factorial, randomized, double-blinded, controlled trial. Allocation of patients to control and experimental groups was randomized using a computer-generated random sequence and was carried out by an assistant who was not informed about the treatments used and the objectives of the study and therefore was blinded to group assignment. The 2 physiotherapists provided the different treatments without knowing which group the patient formed part of. Because there were only 4 possible treatments, they could infer the treatment group; but this information was never provided to them by the researchers, and neither was the objective of the study nor the parameters that were being measured.
Subjects were divided into 4 groups:group 1 received manual therapy treatment,
group 2 received manipulative treatment,
group 3 received a combination of both treatments, and
group 4 received no treatment.All patients were assessed in the same conditions before the treatment, after the treatment (at 4 weeks), and at follow-up (after 8 weeks).
According to the nQuery Advisor program that provides power and sample size calculations, the sample size required in each group, for an analysis of variance (ANOVA) with 1 intersubject factor, with 4 groups, and assuming a 5% significance level for a large effect, is 19 subjects. In case of potential dropouts, 8 more subjects than the number recommended by the nQuery Advisor program were included in the study.
Interventions
Prior to each treatment session (in all 4 groups), the vertebral artery test was performed bilaterally, followed by a 2-minute gentle neck massage, without lubricants and with no therapeutic effect. Subsequently, each group received treatment according to allocation group:Manual therapy of suboccipital soft tissue inhibition is performed with patient in supine position. The patient's head leans against the physiotherapist's hands, which palpate suboccipital muscles by sliding fingertips until contacting posterior arch of atlas. At this point, a deep and progressive gliding pressure is applied for 10 minutes. The purpose of this technique is to release suboccipital muscle spasm, which can be responsible for the mobility dysfunction of the occiput-atlas-axis joint.
Occiput-atlas-axis joint manipulation is performed in the same position as the previous technique. It is bilaterally administered, and it consists of 2 phases:firstly, rotation with gentle head decompression with no flexoextension and slight lateral flexion is performed, followed by small circumductions aimed at increasing arterial viscoelasticity and searching for adequate joint barrier through selective tension;
secondly, a high-speed thrust manipulation in pure rotation towards the side to be manipulated is performed, with a head helicoidal movement, with the aim of restoring the mobility of joints between the occiput, atlas, and axis, which enables to correct a global joint dysfunction.The group receiving combined treatment received the 2 previous techniques exactly with the same sequence.
After the treatment, all 3 treatment groups stayed for 5 minutes in supine position with neutral ranges of neck flexion, extension, lateral flexion, and rotation.
The control group did not receive treatment but stayed in the supine position with neutral ranges for 10 minutes, that is, 5 minutes more than the treatment groups. The assessments were exactly in the same conditions than the rest of groups, including the daily register of pain.
Primary Outcome Assessment
Sociodemographic data and characteristics of headache were collected during the 4 weeks prior to the treatment through individual clinical interview carried out by a physiotherapist who did not participate in the outcome assessment or in the administration of treatments. It included age and sex, location of pain, side dominance of pain, type of pressure, connection with physical activity, frequency, severity of pain, associated symptoms, and pain intensity, rated by the patient on the 0 to 10 numeric pain scale (0 = no pain, 10 = most severe pain).
Secondary Outcome Assessment
Outcome assessment was carried out before the treatment, after the treatment period (at 4 weeks), and at follow-up (1 month later); and it included the following:Multidimensional perception of pain, assessed by the McGill Pain Questionnaire, [12] which includes the following aspects:
(a) sensory—description of pain in time-space terms;
(b) affective—description of pain in terms of stress, fear, and neurovegetative aspects; and
(c) evaluative—pain described in terms of general assessment.The McGill Pain Questionnaire is validated in the Spanish population [13, 14]; and it consists of 66 word descriptors divided into 20 groups, including in each group between 2 and 6 adjectives describing pain. Moreover, it includes a section in which patients register the intensity of pain with a pain scale. [15]
Cervical ranges of motion, measured with the cervical range of motion (CROM) device, which has demonstrated a good intratester reliability in previous studies (intraclass correlation coeffiecient > 0.80). [16] Other authors analyzed the correlation coefficients for intratester and intertester (0.92 and 0.99) [17], and the reliability of this instrument (0.89 to 0.98). [18] Before using the CROM device, we performed an intertester reliability analysis with our 2 examiners and 10 patients not participating in this study, which showed a Pearson correlation of 0.98. The CROM device combines a system of inclinometers and magnets set on a head mainframe with a nose-piece (positions like eyeglasses); and it measures angles of flexion, extension, lateral flexion, and rotation. As it includes a system of magnets, the CROM must not be used in subjects with heart devices.
Frequency and intensity of headache, assessed with a 7-register weekly. Patients recorded headache frequency as well as intensity of pain measured by the numeric pain scale. [15]
Statistical Analysis
Data were codified and analyzed using the statistical software SPSS for Windows (version 15.0; SPSS, Chicago, IL). Descriptive analyses were carried out on the sample as a whole and on each group, with frequencies, percentages, mean scores, standard deviation, and confidence interval. An ANOVA was performed on the pretest scores to test the homogeneity of the groups before beginning the treatment. In ANOVA-type analyses, the Levene test was used to test the assumption of homogeneity of variance. In the cases where it was significant, Welch and Brown-Forsythe F tests were performed. Likewise, t test for dependent samples was performed to compare pretest and posttest means, and pretest and follow-up means, as well as calculation and interpretation of standardized mean difference effect size index. In the t tests, the Kolmogorov-Smirnov test was used separately for each group and for each outcome measurement to test the normality assumption. When this assumption was violated, means were compared using the Wilcoxon test. The significance level was established at 5% in all analyses. As for the effect size, it was rated as follows: small (0.2-0.5), medium (0.5-0.8), or large (> 0.8).
Results
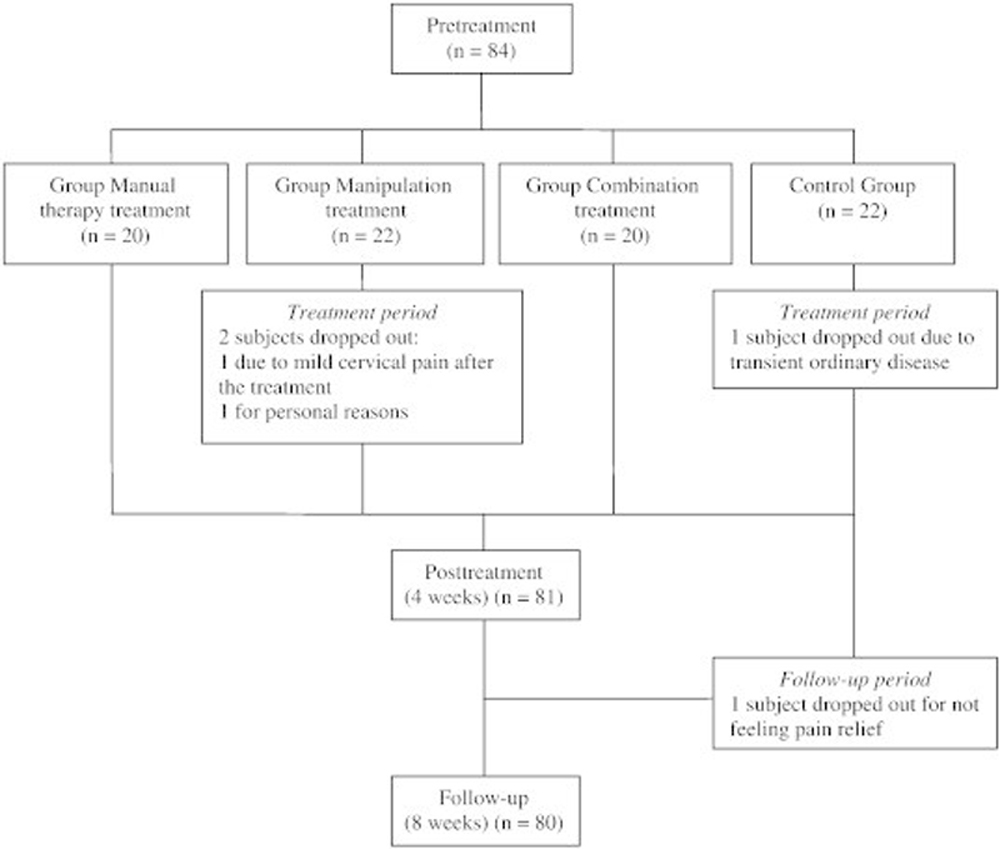
Figure 2 Out of the 84 subjects initially participating in the study, 4 participants dropped out for different reasons (2 subjects dropped out from the manipulation group: 1 because of mild cervical pain after the treatment and 1 for personal reasons. And 2 subjects dropped out from the control group: 1 subject was lost because of transient ordinary disease, and 1 subject was lost for not feeling pain relief), as shown in Figure 2. In the month prior to the study, average pain intensity was rated at 6.49 (SD 1.69). A total of 57.1% of subjects suffered from ETTH and 42.9% from CTTH. The characteristics of headache of subjects in the sample as a whole and by treatment groups, gathered in the clinical interview, are shown in Table 1.
Table 1. Characteristics of Headache in the Month Prior to the Treatment
Characteristics All Subjects
(N = 84)Manual Therapy
(n = 20)Manipulation
(n = 22)Combination
(n = 20)Control
(n = 22)Location of pain Occipital 31 (36.9) 7 (35) 6 (27.3) 8 (40) 10 (45.5) Interparietal 30 (35.7) 10 (50) 9(40.9) 4 (20) 7(31.8) Frontalis-temporalis 23 (27.4) 3 (15) 7 (31.8) 8(40) 5 (22.7) Lateral location Unilateral 2 (2.4) – 1 (4.5) 1 (5) – Bilateral 82 (97.6) 20 (100) 21 (95.5) 19 (95) 22 (100) Pressure Pulsating 16 (19) 5 (25) 4 (18.2) 2 (10) 5 (22.7) Nonpulsating 68 (81) 15 (75) 18 (81.8) 18 (90) 17 (77.3) Physical activity Not aggravating factor 60 (71.4) 13 (65) 15 (68.2) 13 (65) 19 (86.4) Aggravating factor 24 (28.6) 7 (35) 7 (31.8) 7 (35) 3 (13.6) Mild to moderate intensity 78 (92.9) 19 (95) 20 (90.9) 19 (95) 20 (90.9) Severity of pain Mild 11 (13.1) 1 (5) 6 (27.3) 1 (5) 3 (13.6) Moderate 56 (66.7) 17 (85) 11 (50) 13 (65) 15 (68.2) Severe 17 (20.2) 2 (10) 5 (22.7) 6 (30) 4 (18.2) Associated symptoms Photophobia or phonophobia 49 (58.3) 13 (65) 15 (68.2) 12 (60) 9 (40.9) Nausea or vomiting 29 (34.5) 7 (60) 9 (40.9) 6 (30) 9 (40.9) Pericranial tenderness 38 (45.2) 12 (60) 7 (31.8) 11 (55) 7 (31.8)
All results are presented as absolute frequency (percentage).
The perception of pain, assessed by the McGill Pain Questionnaire, showed significant changes in its 5 dimensions for all treatment groups, with the manipulative treatment being the most effective one, as it reported improvements after the treatment and at follow-up in all dimensions. After the treatment, the number of word descriptors for pain was also significantly reduced, as well as the intensity of pain. The control group showed significant differences in 3 dimensions in some of the moments assessed (Table 2).
Table 2. Results of McGill Pain Questionnaire
McGill Manual Therapy Manipulation Combination Control Sensory dimension Pretreatment 19.20 (8.48) 20.81 (10.45) 18.80 (9.76) 20.04 (9.37) Posttreatment 15.85 (9.44) 15.40 (11.74) 16.20 (8.18) 15.80 (9.49) Follow-up 13.95 (10.82) 12.70 (10.85) 14.25 (9.19) 13.95 (7.76) Pre/Posttreatment t = 1.35; P = .19 t = 2.38; P = .02a t = 1.85; P = .07 t = 3.31; P = .003b Pre/Follow-up z = − 2.31; P = .02a z = − 3.55; P = .000c z = − 2.20; P = .02a z = − 2.94; P = .003b Effect size 0.59 0.75 0.45 0.62 Affective dimension Pretreatment 2.80 (2.41) 2.68 (2.23) 3 (2.24) 2.27 (2.25) Posttreatment 1.75 (1.58) 1.55 (1.84) 1.85 (1.66) 1.95 (2.10) Follow-up 2.20 (2.44) 0.90 (1.59) 1.60 (2.19) 1.85 (2.25) Pre/Posttreatment t = 2.01; P = .05a t = 2.06; P = .05a t = 2.88; P = .01b t = 0.98; P = .33 Pre/Follow-up z = − 1.40; P = .15 z = − 2.88; P = .004b z = − 2.58; P = .01b z = − 1.25; P = .21 Effect size 0.24 0.77 0.6 0.18 Evaluative dimension Pretreatment 2.75 (0.91) 2.63 (1.00) 2.65 (0.87) 2.22 (0.97) Posttreatment 1.80 (1.19) 1.85 (0.98) 2.25 (0.96) (1.76-0.94) Follow-up 1.90 (0.79) 1.60 (0.99) 2.00 (1.03) 1.90 (0.91) Pre/Posttreatment t = 2.89; P = .009b t = 2.99; P = .007b t = 1.71; P = .10 t = 4.26; P = .000c Pre/Follow-up z = − 2.85; P = .004b z = − 3.37; P = .001b z = − 2.29; P = .02b z = − 1.73; P = .08 Effect size 0.91 1.00 0.71 0.33 Number of word descriptors Pretreatment 11.25 (4.55) 11.68 (5.03) 10.45 (4.53) 11.09 (4.70) Posttreatment 8.90 (4.82) 9.25 (5.52) 9.35 (4.68) 9.48 (5.50) Follow-up 8.10 (4.93) 7.00 (5.06) 7.70 (4.77) 8.80 (4.91) Pre/Posttreatment t = 1.94; P = .06 t = 2.39; P = .02a t = 1.78; P = .09 t = 2.83; P = .10 Pre/Follow-up z = − 2.63; P = .008b z = − 3.73; P = .000c z = − 2.99; P = .003b z = − 2.43; P = .47 Effect size 0.66 0.89 0.58 0.47 Intensity of pain Pretreatment 4.45 (2.11) 4.64 (2.12) 4.85 (2.00) 5.27 (2.22) Posttreatment 3.45 (2.52) 3.35 (2.25) 2.00 (1.55) 4.24 (2.54) Follow-up 2.55 (1.82) 2.50 (2.37) 1.50 (1.64) 3.85 (2.35) Pre/Posttreatment t = 1.96; P = .06 t = 2.10; P = .04a t = 4.35; P = .000c t = 1.70; P = .10 Pre/Follow-up t = 4.14; P = .001c t = 3.05; P = .007b t = 7.77; P = .000c t = 2.26; P = .03a Effect size 0.86 0.87 1.60 0.61 All results are presented as mean (SD) unless indicated otherwise.
z, Wilcoxon test; t, t test for 2 related samples.
a ≤ .05.b ≤ .01.c ≤ .001.
As for the cervical ranges of motion, flexion showed improvement in the group with manual therapy and in the control group; cervical extension improved in the groups with manual and manipulative therapy after the treatment, but not in the follow-up. After manipulative treatment, left lateral flexion showed improvement, which was maintained at follow-up. In the control group, differences were found in both lateral flexions at follow-up, but not after the treatment. All treatments improved left and right rotation; these improvements were maintained at 1-month follow-up for the groups with manual therapy and manipulative treatment (Table 3).
Table 3. Results of Cervical Ranges of Motion
Cervical Range of Motion Manual Therapy Manipulation Combination Control Cervical flexion Pretreatment 49.20 (12.53) 53 (10.23) 53.25 (12.39) 46.95 (9.03) Posttreatment 59.85 (11.61) 54.95 (9.86) 53.05 (11.24) 50.29 (9.81) Follow-up 56.85 (10.85) 52.30 (11.24) 52.75 (10.32) 49.40 (9.47) Pre/Posttreatment z = − 3.04; P = .002b z = − 1.22; P = .22 z = − 0.41; P = .67 z = − 2.40; P = .02a Pre/Follow-up z = − 2.26; P = .02a z = − 0.50; P = .61 z = − 0.18; P = .85 z = − 2.03; P = .04a Effect size 0.59 0.007 0.04 0.26 Cervical extension Pretreatment 50.90 (14.51) 49.36 (10.36) 53.40 (13.06) 51.82 (11.29) Posttreatment 57.05 (13.33) 56.35(11.85) 57.80 (14.53) 54.24 (11.44) Follow-up 54.15 (12.91) 53.50 (7.56) 57.85 (11.49) 55.10 (11.73) Pre/Posttreatmen t = − 2.34; P = .03a t = − 2.26; P = .03a t = − 1.94; P = .06 t = − 1.46; P = .15 Pre/Follow-up t = − 0.93; P = .36 t = − 1.67; P = .10 t = − 1.41; P = .17 t = − 1.71; P = .10 Effect size 0.21 0.38 0.33 0.28 Right lateral flexion Pretreatment 35.60 (14.36) 39.50 (6) 39.95 (8.67) 38.32 (6.22) Posttreatment 38.60 (8.13) 40.10 (10.73) 40.25 (8.06) 40.95 (8.25) Follow-up 38.05 (7.03) 41.70 (7.37) 39.85 (6.40) 40.70 (5.44) Pre/Posttreatment t = − 1.03; P = .31 t = − 0.43; P = .67 t = − 0.17; P = .86 t = − 1.55; P = .13 Pre/Follow-up t = − 0.86; P = .39 t = − 1.26;P = .22 t = − 0.05; P = .17 t = − 3.31;P = .04a Effect size 0.16 0.35 0.01 0.37 Left lateral flexion Pretreatment 38.15 (12.69) 39.54 (6.36) 41.45 (9.49) 38.27 (7.08) Posttreatment 41.35 (7.47) 44.05 (5.59) 41.05 (8.73) 41.14 (6.46) Follow-up 40.60 (7.70) 42.50 (5.74) 43.20 (6.95) 40.20 (5.81) Pre/Posttreatment z = − 1.71; P = .08 z = − 2.40; P = .01b z = − 0.03; P = .97 z = − 2.73; P = .06 Pre/Follow-up t = − 0.86; P = .39 z = − 1.96; P = .04a z = − 0.76; P = .44 z = − 1.52; P = .04a Effect size 0.19 0.45 0.18 0.40 Right rotation Pretreatment 59.85 (11.94) 61.05 (8.27) 63.10 (9.76) 58.73 (9.70) Posttreatment 64.35 (12.28) 68.70 (7.86) 67.95 (9.96) 61.86 (7.67) Follow-up 61.80 (12.24) 66.45 (7.51) 66.05 (10.84) 60.45 (7.87) Pre/Posttreatment z = − 2.34; P = .02a z = − 3.42; P = .000c z = − 2.02; P = .04a z = − 1.77; P = .07 Pre/Follow-up z = − 0.68; P = .49 z = − 2.69; P = .007b z = − 1.55; P = .12 z = − 0.28; P = .77 Effect size 0.16 0.63 0.29 0.17 Left rotation Pretreatment 56.50 (14.34) 64.45 (8.05) 63.45 (11.26) 62.36 (9.23) Posttreatment 66.83 (11.22) 64.15 (13.47) 71.50 (7.61) 68.10 (12.12) Follow-up 63.15 (10.79) 68.20 (9.14) 66.80 (11.76) 61.40 (9.74) Pre/Posttreatment t =−4.03; P = .000c t = − 3.07; P = .006b t =−2.40; P = .02a t = − 1.06; P = .30 Pre/Follow-up t = − 2.59; P = .02a t = − 2.33; P = .03a t = − 1.51; P = .14 t = − 0.89; P = .38 Effect size 0.45 0.45 0.29 0.10 All results are presented as mean (SD) unless indicated otherwise.
z, Wilcoxon test; t, t test for 2 related samples.
a≤ 0.05.b≤ 0.01.c≤ 0.001.
In the weekly register, the frequency of headaches in the group with combined treatment (manipulative and manual therapy) showed significant improvement until the end of the study; headache intensity was reduced in the groups with manipulative treatment, combined treatment, and control both after the treatment and at follow-up (Table 4). No adverse events were reported in this study.
Table 4. Results of Daily Register of Headache
Weekly Register Manual Therapy Manipulation Combination Control Frequency Week 1 3.25 (2.29) 2.90 (1.86) 3.80 (1.79) 3.24 (1.57) Week 4 2.60 (2.13) 1.70 (2.00) 1.55 (1.50) 2.45 (1.50) Week 7 2.45 (2.08) 2.15 (2.25) 1.65 (1.75) 2.85 (1.92) Week 1-4 t/z t = 1.68; P = .10 z = − 2.63; P = .008b z = − 3.64; P = .000c t = 1.89; P = .07 Week 1-7 t/z t = 1.59; P = .12 z = − 1.49; P = .13 z = − 3.03; P = .002b t = 0.55; P = .58 Effect size 0.34 0.39 1.15 0.24 Intensity Week 1 4.79 (2.26) 5.12 (1.95) 4.80 (1.68) 5.24 (1.80) Week 4 3.77 (2.51) 3.03 (2.80) 3.24 (2.72) 3.95 (2.12) Week 7 2.82 (2.20) 3.28 (2.39) 3.02 (2.60) 3.86 (2.00) Week 1-4 t/z t = 1.49; P = .15 t = 2.69; P = .014a z = − 2.21; P = .02a t = 2.34; P = .03a Week 1-7 t/z t = 1.30; P = .20 t = 2.86; P = .01b z = − 2.42; P = .01b t = 2.24; P = .03a Effect size 0.54 0.91 1.01 0.74 All results are presented as mean (SD) unless indicated otherwise.
z, Wilcoxon test; t, t test for 2 related samples.
a≤ 0.05.b≤ 0.01.c≤ 0.001.
Discussion
The results obtained in this study showed that TTH has specific pain characteristics, in accord with the classification of the International Headache Society [1] about TTH and its diagnosis developed in 2004. Regarding pain perception, manipulative treatment, manual therapy, and combined treatment have shown efficacy in reducing pain in all the dimensions assessed, although the group with manipulative treatment stood out from the others. Pain intensity also improved in all groups, even in the control group, although with less significant differences.
As for cervical flexion and extension, the treatment with manual therapy demonstrated more beneficial results. It is possible that the technique used induces relaxation of the suboccipital back muscles participating in extension and rotation of upper cervical vertebrae, which may have helped achieving greater flexion. The techniques used may have an influence on flexion and rotation muscles and, to a lesser extent, on lateral flexion muscles, which would explain the better results in these movements. Mobility in both rotations significantly improved after treatment in all experimental groups.
Both treatments when administered separately improved cervical mobility. Manual therapy showed better results for cervical flexion and extension; and manipulation was better for extension, left lateral flexion, and rotations. It is possible that joint manipulation in rotation can have a relaxation effect on this region, facilitating global mobility at this level. Combined treatment showed improvement only in rotation; and therefore, the use of manual therapy prior to joint manipulation was not more effective than joint manipulation on its own.
Other studies [19] provide data about cervical mobility assessment in a global way; however, the present study has assessed each cervical range of motion separately. We consider this assessment more comprehensive, allowing us to know which specific parameter changes after the treatment.
With regard to the weekly register on frequency and intensity of pain, these parameters showed significant improvement in the groups with manipulation and combined treatment both after the treatment at follow-up. The control group also reported significant differences at follow-up, but these differences were less important.
The administration of 2-minute massage with no therapeutic effect prior to the treatment was used in all groups. In other studies, [20, 21] massage was applied during the time required to achieve the effect of combined treatment with other techniques. It is possible that, if the technique used in this study had not been massage, the results would have been different. In the present study, it has been shown that the massage technique when rigorously applied may have had a positive impact on some aspects of headache. Moreover, manual contact (massage) may have greater impact on the patient than the administration of ultrasound (turned off) as a placebo. [22]
The treatments administered in the present study were beneficial, with significant results in most of the outcome assessments. Other studies [8, 23] have not shown conclusive results about the benefits of spinal manipulation, probably because these studies did not have a control group or had simple blind control.
In a review conducted in 2011 by Bryans et al [24] on the effectiveness of manipulative treatment, cranial-cervical manipulation was shown to be effective in the long term. Other authors [25] observed that the treatment with spinal manipulation at other levels (cervical or thoracic, depending on the dysfunction) was effective in pain perception. However, the manipulative treatment used in the current study is localized in a specific spinal segment to evaluate its effectiveness; moreover, it has been administered both separately and combined with another treatment to know its effectiveness, obtaining good results not only in intensity, frequency, and pain perception in each subscale of the questionnaire but also in variables like cervical mobility in 4 different parameters.
The studies assessing several techniques combined have obtained significant improvements in pain intensity and cervical ranges of motion. [9, 19, 26] However, although combined treatments were shown to be effective, none of these studies let us know if the effectiveness is mainly due to one of the treatments or to the combination of all treatments. To clarify this aspect, in the present study, each treatment has been administered individually and combined.
The results of manual therapy treatment have been positive for pain perception and for cervical flexion, extension, and rotation. In the current study, the treatment with manual therapy was chosen with the aim to reduce tension in suboccipital muscles, often responsible for the onset of headache; however, it was shown to be the least beneficial in the reduction of headache frequency and intensity in the affective scale and in cervical lateral flexion. These results might be because, with this soft tissue treatment, no joint movement is performed and patients may perceive this treatment as insufficient. For other authors, [2, 11] the use of soft tissue techniques involving joint movement induces relaxation of cervical muscles, thus reducing pain intensity and headache frequency. On the other hand, Toro-Velasco et al [22] studied the immediate effects of head and neck massage on the variability of heart rate, state of mind, and pressure pain threshold in patients with CTTH (11 patients) who received 1 single treatment session with the same soft tissue technique as the one used in the present study together with muscle-energy techniques on suboccipital muscles during 40 minutes or placebo with ultrasounds, showing an increase of the variability index in heart rate and a significant reduction of anxiety-tension, anger, and pain intensity; however, only 1 single session is administered, and the number of subjects is very small because it is a pilot study. In our study, outcome assessments were carried out in the short and long term on different aspects of pain perception, cervical joint mobility, and pain intensity and frequency; and the sample used was much larger.
The positive results of the current study found positive outcome assessments in the control group. This may be due to both the rigorous design, having taken into account the time of administration, and the fact that assessments were carried out exactly in the same conditions for all 4 groups, including the daily register of pain, which may have had a psychological beneficial effect. Other potential explanations for these results could be as follows: simple random variation, they improved because of the normal course of the disorder, or an observational effect (patients being observed may report better outcomes).
We consider that the treatments assessed in this study have shown efficacy in TTH, with positive results in perception, frequency, and intensity of pain and in cervical mobility. Therefore, we suggest that the treatments used in the present study may represent an alternative or addition to other treatments administered including physiotherapy, [2] osteopathic treatment, [5] craniocervical exercise, [6] chiropractic treatment, [24] or other techniques applied in combination. [26]
Limitations
The short follow-up period, lasting only 1 month after the treatment, and the small treatment groups are limitations of this study. It might have been desirable to have a longer follow-up period; but the outcome assessment performed at 8 weeks (4 weeks after finishing the treatment) already showed conclusive results regarding the maintenance of treatment effects, which were both statistically and clinically significant. The administration of the treatments used in this study was by experienced physiotherapists with experience in the treatment of headache with manual therapies. Therefore, the findings of this study may not necessarily apply to other therapies, practitioners, or clinical situations.
Conclusion
The findings of this study showed that treatment with manual therapy showed efficacy in most aspects of pain perception in TTH; however, manipulation and combined treatment were more beneficial. Treatment with manual therapy was better at improving cervical flexion, extension, and rotation, while manipulative treatment was better at improving extension, left lateral flexion, and rotation. The frequency of headache episodes decreased with the treatments including manipulation, maintaining this improvement at follow-up with the combined treatment. The manipulative treatment on its own or combined with manual therapy was more efficacious for reducing pain intensity.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
References:
Headache Classification Subcommittee of the International Headache Society
The international classification of headache disorders.
Cephalalgia. 2004;24(Suppl. 1):9–160Lenssinck M.L.B., Damen L., Verhagen A.P., Berber M.Y., Passchier J., Koes B.W.
The effectiveness of physiotherapy and manipulation patients with tension-type headache: a systematic review.
Pain. 2004;112:381–388Volcy-Gómez M.
The impact of migraine and other primary headaches on the health system and in social and economic terms.
Rev Neurol. 2006;43(4):228–235Stovner L.J., Andree C.
Prevalence of headache in Europe: a review for the Eurolight project.
J Headache Pain. 2010;11:289–299Anderson R.E., Seniscal C.
A comparison of selected osteopathic treatment and relaxation for tension-type headaches.
Headache. 2006;46(3):1273–1277van Ettekoven H., Lucas C.
Efficacy of physiotherapy including a craniocervical training programme for tension-type headache; a randomized clinical trial.
Cephalalgia. 2006;26:983–991Moraska A., Chandler C.
Pilot study of chronic tension type headache.
J Man Manipulative Ther. 2008;16(2):106–112Fernández-de-las-Peñas C., Alonso-Blanco C., Cuadrado M.L., Gerwin R.D., Pareja J.A.
Trigger Points in the Suboccipital Muscles and Forward Head Posture in Tension-Type Headache
Headache: J of Head and Face Pain 2006 (Mar); 46 (3): 454—460Couppe C., Torelli P., Fuglsang-Frederiksen A., Andersen K., Jensen R.
Myofascial trigger points are very prevalent in patients with chronic tension-type headache: a double-blinded controlled study.
Clin J Pain. 2007;23(1):23–27Fernández-de-las-Peñas C., Alonso-Blanco C., Cuadrado M.L., Pareja J.A.
Forward head posture and neck mobility in chronic tension-type headache: a blinded, controlled study.
Cephalalgia. 2006;26:314–319Buchgreitz L., Egsgaard L.L., Jensen R., Arendt-Nielsen L., Bendtsen L.
Abnormal pain processing in chronic tension-type headache: a high-density EEG brain mapping study.
Brain. 2008;131:3232–3238Melzack R.
The McGill Pain Questionnaire: major properties and scoring methods.
Pain. 1975;1(3):277–301Masedo A.I., Esteve R.
Some empirical evidence regarding the validity of the Spanish version of the McGill Pain Questionnaire (MPQ-SV)
Pain. 2000;85(3):451–456Lázaro C., Caseras X., Whizar-Lugo V.M.
Psychometric properties of a Spanish version of the McGill Pain Questionnaire in several Spanish-speaking countries.
Clin J Pain. 2001;17:365–374Williamson A., Hoggart B.
Pain: a review of three commonly used pain rating scales.
J Clin Nurs. 2005;14:798–804Tousignant M., de Bellefeuille L., O’Donoughue S., Grahovac S.
Criterion validity of the cervical range of motion (CROM) goniometer for cervical flexion and extension.
Spine. 2000;25(3):324–330Hall T., Robinson K.
The flexion-rotation test and active cervical mobility—a comparative measurement study in cervicogenic headache.
Man Ther. 2004;9:197–202Haynes M.J., Edmondston S.
Accuracy and reliability of a new, protractor-based neck goniometer.
J Manipulative Physiol Ther. 2002;25(9):579–586Demirturk F., Akarcali I., Akbayrak T., Citak I., Inan L.
Results of two different manual therapy techniques in chronic tension-type headache.
Pain Clin. 2002;14(2):121–128Taimela S., Takala E.P., Asklo¨f T., Seppa¨la¨ K., Parviainen S.
Active treatment of chronic neck pain. A prospective randomized intervention.
Spine. 2000;25(8):1021–1027Torelli P., Jensen R., Olesen J.
Physiotherapy for tension-type headache: a controlled study.
Cephalalgia. 2004;24(1):29–36Toro-Velasco C, Arroyo-Morales M, Fernandez-de-Las-Penas C, Cleland JA.
Short-Term Effects of Manual Therapy on Heart Rate Variability, Mood State, and
Pressure Pain Sensitivity in Patients With Chronic Tension-Type Headache:
A Pilot Study
J Manipulative Physiol Ther. 2011 (Jun); 34 (5): 274–289Astin J.A., Ernst E.
The effectiveness of spinal manipulation for the treatment of headache disorders: a systematic review of randomized clinical trials.
Cephalalgia. 2002;22:617–623Bryans R, Descarreaux M, Duranleau M, Marcoux H, Potter B, Ruegg R.
Evidence-Based Guidelines for the Chiropractic Treatment
of Adults With Headache
J Manipulative Physiol Ther. 2011 (Jun); 34 (5): 274–289Donkin R.D., Tech M., Parkin-Smith G.F., Tech M., Gomes A.N.
Possible effect of chiropractic manipulation and combined manual traction and manipulation on tension-type headache: a pilot study.
J Neuromusculoskelet Syst. 2002;10(3):89–97Castien, R. F., van der Windt, D. A., Grooten, A., & Dekker, J.
Effectiveness of Manual Therapy for Chronic Tension-type Headache:
A Pragmatic, Randomised, Clinical Trial
Cephalalgia. 2011 (Jan); 31 (2): 133–143
Return to CHRONIC TENSION HEADACHE
Since 3-21-2015


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |