The Comparative Prognostic Value of Directional Preference
and Centralization: A Useful Tool for Front-line Clinicians?This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manual Manip Therapy 2008; 16 (4): 248254 ~ FULL TEXT
OPEN ACCESS Audrey Long, BSc, PT, Stephen May, MSc, and Tak Fung, PhD
Senior Statistical Consultant,
University of Calgary,
Calgary AB, Canada.
A large number of prognostic factors have been associated with recovery from an episode of back pain, and much emphasis has been placed on psychosocial prognostic factors. The large number of prognostic factors and the lack of comparative analysis of different factors make use of these difficult in clinical practice. The aim of this study was to evaluate the comparative usefulness of a range of factors to predict outcome using data from a randomized controlled trial (RCT) in which 312 patients with sub-acute to chronic back pain received a mechanical evaluation and were sub-grouped based on the presence or absence of directional preference (DP). Patients were then randomized to treatment that was matched or unmatched to that DP.
Patients with a minimal reduction of 30% in Roland-Morris Disability Questionnaire (RMDQ) score were defined as the good outcome group. Seventeen baseline variables were entered into a step-wise logistic regression analysis for the ability to predict a good outcome. Of the patients, 84 met the good outcome criteria and had a mean RMDQ decrease of 58.2% (9.8 points) in 4 visits. Leg pain, work status, depression, pain location, chronicity, and treatment assignment were significant predictors of outcome in univariate analysis. Only leg bothersomeness rating and treatment assignment survived multivariate analysis. Subjects with DP/centralization who received matched treatment had a 7.8 times greater likelihood of a good outcome. Matching patients to their DP is a stronger predictor of outcome than a range of other biopsychosocial factors.
KEYWORDS: Centralization; McKenzie Method; Mechanical Low Back Pain; Multivariate Regression Analysis; Prognosis
From the FULL TEXT Article:
Introduction
Low back pain (LBP) is extremely common both in the general population and in those seeking healthcare. [18] Point prevalence estimates for LBP are at least 20% of the general population [2, 5, 6]; yearly prevalence estimates are at least 40% [14, 8]; and lifetime prevalence is around 60%. [2, 3, 6, 8] In contrast to earlier claims [9] of a relatively benign natural history for acute back pain, it is now clear that LBP is commonly both highly recurrent and frequently persistent [10, 11]. These systematic reviews on the topic noted that after initial improvements, there is little further improvement after 3 months, at which point approximately 50% are still experiencing activity limitation; in addition, 6675% of patients have at least one recurrence within 12 months [10, 11]. Not surprisingly, the direct and indirect costs associated with such a common, activity limiting, persistent, and episodic problem are vast in many developed countries. [1214] Treatments seem to have been largely ineffective at altering this 20th-century medical disaster. [15]
Given the now documented high prevalence rate, and the persistent and recurrent nature of LBP, there has been considerable recent interest in determining prognostic factors that might affect the outcome of an episode of LBP. Understanding prognostic factors would help to shape relevant management strategies and assist with early identification of individuals at high risk of developing chronic pain and disability. Ultimately, the goal would be to refine treatment approaches and permit the wiser allocation of scarce health care resources and the prevention of chronic problems. [16] Equally, identification of patients likely to have an uncomplicated recovery would help prevent overuse of healthcare resources by those who least need it. [16]

Table 1 For these reasons, a substantial volume of literature has been published on prognostic factors for LBP and sciatica. The 2004 European Guidelines for the Management of Acute Nonspecific Low Back Pain in Primary Care cited 74 articles on the topic. [17] This systematic review and numerous recent studies share a dominant theme: the prominence of psychosocial variables in the prediction models. [1824] However, the quantity of prognostic variables that have been identified as possible effectors of prognosis form a cumbersome and unrealistic list for clinicians to assess and address (Table 1).
This long list of potentially relevant prognostic factors also leaves many important issues unanswered. How can this information be translated into data for clinical use? For instance, which of these factors are most important, which should be used to make judgments about individual patients, and how can clinicians determine at assessment which patient is most likely to respond to a particular treatment? Such information may help to make treatment more selective rather than offering standardized treatment.
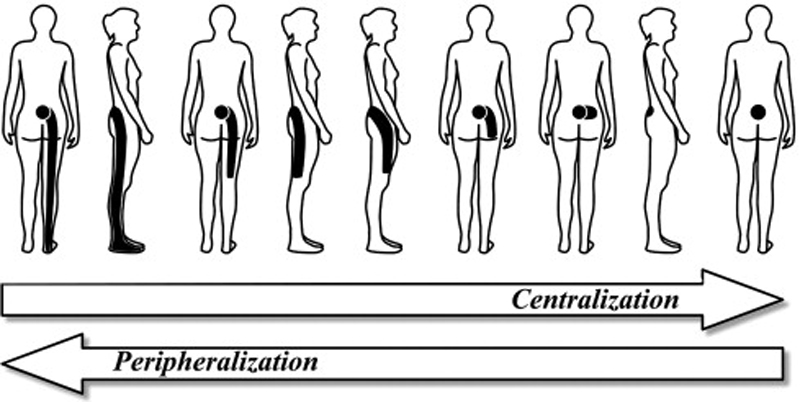
One prognostic sign that has been shown to be useful in guiding treatment is the centralization phenomenon. [27, 28] This physical examination finding refers to the abolition of local or distal pain emanating from the spine in response to repeated movements or sustained postures29. Centralization will always be accompanied by a directional preference (DP) describing the direction of spinal movement or posture that produces it. [28] However, DP may also be determined by a decrease in pain intensity, without the pain having changed location, and/or an increase in previously limited movement; thus, the terms are not synonymous but they are closely allied. A large number of studies have now shown that patients who demonstrate centralization at their initial evaluation will have better outcomes than non-centralizers [3037], and that matching patients to their DP exercise produces better outcomes than non-matched treatment. [27, 28]
The novel aspect of centralization is that it challenges the current trend in the evidence where psychosocial prognostic factors have dominated [1824] because it is a variable related to the physical examination. For the properly trained clinician, this finding, or lack of it, may be relatively easy to demonstrate, may be useful as a management guide, and may serve as a predictor of positive and negative outcomes.
What is not clear is whether centralization/non-centralization are more or less useful predictors of outcome than psychosocial variables. Prior studies have begun to shed light on this topic. Werneke and Hart [37] compared a range of baseline demographic, work-related, psychosocial and clinical findings in their ability to predict a range of healthcare-related outcomes at one year in 187 patients with LBP. Whereas leg pain, overt pain behaviors, non-organic physical signs, fear of work activities, perceived disability, and centralization/non-centralization were significant in the univariate analysis, only leg pain (0.004) and centralization/non-centralization classification (0.004 and <0.001 depending on outcome) survived the multivariate analysis. In a smaller study, George et al33 compared the predictive value of centralization and fear-avoidance beliefs at baseline to predict outcomes at 6 months. Both were significant predictors of disability at 6 months (0.004 and 0.27 respectively), but only centralization was a significant predictor of pain at 6 months (0.044).
These studies suggest that centralization may be as important a prognostic indicator as psychosocial factors. The purpose of the present secondary analysis of data from a previous randomized trial was to determine which factors were most likely to predict successful outcomes. A range of baseline biopsychosocial variables were analyzed to understand which individual items best predicted a good short-term prognosis.
Methods
The study design was a multivariate analysis of prognostic variables in patients with LBP. The subjects for the current analysis were 312 subjects, who were screened for participation in a previously published RCT, in which the methods were fully described. [28] Briefly, a mechanical diagnosis and therapy (MDT) assessment was used to subgroup candidates as having or not having DP/centralization. Each subgroup was then randomized to receive either matched or unmatched treatment. Matched treatment referred to exercises and advice that are based on MDT (McKenzie Method) principles. Unmatched treatment consisted of generic or commonly used LBP exercises that were not matched to DP and advice/reassurance consistent with current treatment guidelines. The 82 patients who did not demonstrate DP/centralization at baseline were randomized to receive one of two treatment protocols. The first group received further mechanical assessment on subsequent treatment sessions and if a DP emerged, they were given matched treatment (it has been demonstrated that 60% of those who are non-centralizers on day one become centralizers with further testing over subsequent sessions [38]). The second group received non-specific exercises and advice/reassurance consistent with current guidelines. The purpose of the current analysis is to determine which baseline variables from that earlier study were most predictive of a good outcome.
Descriptive statistics were reported for baseline variables. Pearson chi square test for categorical baseline variables and independent-sample t-tests for continuous baseline variables were used to compare subjects who had completed treatment and those who had dropped out. Within the original RCT protocol, subjects were allowed a maximum of 6 sessions in 2 weeks. At this point a good outcome was used to label those subjects reporting that as a result of the advice and prescribed exercises they felt their back pain problem was resolved and ready for discharge, or those who reported they felt better but required a few more sessions, and with a minimal reduction of 30% on their Roland-Morris Disability Questionnaire (RMDQ) score. Any patient reporting he or she was not changed much or worse was classified as having a poor outcome.
Seventeen variables were collected at baseline and entered into a step-wise logistic regression analysis for the ability to predict good outcome at 2 weeks.
Variables entered into the equation wereage,
gender,
marital status,
Quebec Task Force (QTF) category anatomic pain location,
QTF category acuity,
first or recurrent episode,
work status,
back and leg pain rating,
pain interference rating,
back and leg pain bothersomeness,DP status, and whether matched or un-matched to treatment (i.e., DP/centralization randomized to matched or unmatched treatment, or no DP/centralization at baseline randomized to further MDT assessments or generic exercises), RMDQ, medication, and Beck depression scale. Variables with p > 0.05 were excluded from further analysis while significantly associated variables (p < 0.05) survived subsequent steps in the regression analysis. Sensitivity, specificity, and odds ratios were calculated for the surviving variables in the model. Statistical analyses were performed using SPSS 14.0.
Results
Of 312 subjects, 44 (14%) did not complete treatment. Dropouts did not differ substantially on 12 of 17 baseline variables: gender, QTF anatomic pain location and acuity category, work status, back and leg pain rating, pain interference rating, back or leg bothersomeness ratings, presence/absence of DP/centralization, and RMDQ. Dropouts did tend to be younger (p=.043), single (p<.001), experiencing a first episode of LBP (p=.038), and taking more medication (p=.045), and they had higher depression scores (p=.002).

Table 2

Table 3

Table 4 A further 27 subjects (9%) were missing various data points: 3 were missing history of prior episodes, 9 marital status, 3 Beck Depression Inventory, and 2 activity interference rating at home and work. In addition, 10 gave conflicting dates for first episode and current episode so that the status of acute/sub-acute/chronic of the current episode could not be calculated. As a result, 241 subjects (77.2%) had complete data available at entry and discharge and formed the cohort for the current analysis.
Of the 241, 84 subjects (35%) met the good outcome criteria. In a mean of 4 visits over 2 weeks, these subjects' RMDQ scores were reduced by a mean 9.7 points (SE 0.69), or 58.2% (SE 3.2). In the poor outcome group, the mean change in the RMDQ scores was 0.45 (SE .33) or 2.06% change (SE 3.61).
Eight of the 17 baseline variables entered into the model (Table 2) were significantly correlated with good outcome (p < .05) and were carried forward in the regression analysis. Only two variables survived in the final model, the leg bothersomeness rating and treatment assignment, which included four subgroup/treatment combinations (i.e., DP/centralization randomized to matched or unmatched treatment, or no DP/centralization at baseline randomized to further MDT assessments or generic exercises). These two variables correctly predicted 77.6% of those with a good outcome within 2 weeks of care (mean 4 visits, range 16). Controlling for leg bothersomeness and other group variables, the treatment group representing the DP/centralization subgroup who received matched treatment were 7.8 times more likely to achieve a good outcome as defined by a minimal 30% decrease in RMDQ scores (Table 3). Sensitivity, specificity, and positive and negative predictive values are presented in Table 4.
Discussion
In this secondary analysis from a previous RCT [28], baseline variables were examined for the ability to predict a good outcome, which was defined by patients' report of resolved and ready for discharge or better but required a few more sessions and with a minimal reduction of 30% on their RMDQ score. According to this definition leg pain and leg bothersomeness ratings, leg pain rated higher than back pain, work status, depression, QTF anatomic pain location, and QTF acute/subacute/chronic categories, and treatment assignment were significant predictors of outcome in univariate analysis With multivariate analysis of these significant variables, only leg bothersomeness rating and treatment assignment survived.
Leg pain was negatively correlated with a good outcome, meaning that those with a lower leg pain score had better outcomes. Of the four treatment assignments, subjects with DP/centralization who received matched treatment had a 7.8 times greater likelihood of a good outcome finding not documented in prior trials was the finding that those with DP/centralization given unmatched exercises were negatively associated with a good outcome (i.e., the wrong exercise prescription may actually be detrimental).
Even those patients who did not appear to have a DP at the initial mechanical evaluation were 3.4 times more likely to have a good outcome if they were given further MDT evaluation and management along MDT guidelines at subsequent sessions. This finding requires further study to determine whether this represents cases where non-centralizers became centralizers over a few visits [38], or where non-centralizers responded favorably to a single direction exercise program rather than nonspecific exercises.
We conducted this secondary analysis to determine the comparative strength of a range of baseline variables to predict outcomes. Like others [33, 37], we found centralization to be a stronger predictor of outcomes than psychosocial variables. In this study, we used the variables of depression, marital status, and work status whereas in the other studies, variables such as overt pain behaviors, fear of work activity [37], and fear avoidance [33] were used. We found leg bothersomeness was predictive whereas Werneke and Hart [37] found leg pain only predicted one of five health related outcomes at one year. Subsequent analysis found that the QTF category was not useful at predicting long-term outcomes while centralization was40.

Table 5 Werneke and Hart38 found that two variables in acute predominantly worker's compensation subjects (non-centralization at discharge and baseline leg pain) were predictive of chronic pain and disability at one year. Treatment was matched to subgroup centralization/DP and Table 5 compares their findings to this current trial. Despite different study designs, similar predictive models were found. Most intriguing is that the surviving variables in both models were stronger predictors than a range of other biopsychosocial factors: age, gender, duration of back pain, prior history, baseline back and leg pain, baseline disability, work satisfaction, non-organic signs, fear avoidance, depression, and somatization. The fact that a physical examination finding survived in a predictive model over psychosocial factors is a rare finding worthy of further study since it challenges current guidelines, in which psychosocial factors dominate.
The findings from the original RCT [28] and from this secondary analysis emphasize the short-term positive prognostic finding of DP, as long as this is matched to appropriate directional exercises. Thus, both DP and centralization would appear to be important clinical findings that can be used as indicators of management strategies and good prognosis. Such findings are rare in physical examination items. However, Hahne et al [41] and Tuttle [42] also found that within session changes in pain intensity, pain site, and range of movement were predictive of short-term prognosis in back and neck pain patients. As these clinically derived responses match the changes that we would use to establish DP, these studies add further support to the prognostic validity of DP.

Table 6 The second variable surviving in our model, leg bothersomeness, has been identified previously as being associated with poorer outcomes. [4345] Indeed, leg bothersomeness has been suggested as a potentially important outcome measure. [39] Patrick et al [46] found that subjects with lower bothersomeness and sciatica frequency reported higher functional status, well-being, and fewer disability days. They also found that bothersomeness correlated well with baseline pain, disability, general health, and psychological health measures, therefore indicating good construct validity. Bothersomeness was also predictive of increased risk of work absence or health care consultations for LBP over 6 months. [47] The current trial adds support for the use of a bothersome rating in future trials. This simple rating may be an important part of a practical front-line screening tool for clinicians (Table 6).
Limitations
This study suffers from several weaknesses that should be recognized. It is a secondary analysis of data that was gathered for a RCT, and as such it lacks a number of methodological criteria that are recommended for prognostic studies. [48] For instance, the inception cohort was heterogeneous, the sample size was relatively small, and the follow-up was short-term. However, the sub-grouping was more important than the heterogeneity in our analysis, the sample size was enough to avoid a type II error, and though the follow-up was short-term, disability reduction early in the course of care clearly distinguished those with a good outcome from those reporting no change or worsening of their pain. The analysis was specific to our definition of success, which was 30% reduction in RMDQ. This amount of change has been derived as a rule for determining the minimally clinical important difference for the RMDQ. [49] This number allows patients with mild to severe problems to show improvement, compensates for the measurement error of the RMDQ, and has been recommended in clinical trials to detect clinical changes in health. [49] Furthermore, variables that have received increasing attention in recent years such as fear avoidance, patient expectations, distress, job satisfaction, and work place factors were not included.
The current analysis was used to prospectively predict early responsiveness to treatment. Whether this early improvement in pain and function yields long-term benefits requires further study. Brennan et al [27] suggested that early effective management may be a window of opportunity through improved decision-making, based on the use of subgroups, to optimize recovery and avoid persistent disability.
Conclusion
Pain duration, leg pain intensity, work status, depression, and QTF anatomic pain location (back pain vs. Sciatica) were all weak predictors of outcome. Weak is used here in the sense that these variables did not hold up when weighed against the variables of baseline leg bothersomeness and subgroup matched treatment (DP/centralization with matched treatment). Subgroup matched treatment appears to be a useful tool for front-line clinicians and an important factor that dominates other variables, including depression. As the science of LBP subgroups evolves, it may be possible to shorten the list of prognostic variables to those most amenable to change and those most important in preventing long-term disability.
References:
Croft, P., Macfarlane, G., Papageorgiou, A. (1998).
Outcome of low back pain in general practice:
A prospective study
British Medical Journal 1998 (May 2); 316 (7141): 13561359Hillman M, Wright A, Rajaratnam G, Tennant A, Chamberlain MA.
Prevalence of low back pain in the community: Implications for service provision in Bradford, UK.
J Epidem Comm Health. 1996;50:347352Leboeuf-Yde C, Klougart N, Lauritzen T.
How common is low back pain in the Nordic population? Data from a recent study on
a middle-aged general Danish population and four surveys previously conducted
in the Nordic countries.
Spine. 1996;21:15181526Linton SJ, Hellsing AL, Hallden K.
A population-based study of spinal pain among 3545-year-old individuals.
Spine. 1998;23:14571463Papageorgiou AC, Croft PR, Ferry S, Jayson MIV, Silman AJ.
Estimating the prevalence of low back pain in the general population.
Spine. 1995;20:18891894Skovron ML, Szpalski M, Nordin M, Melot C, Cukier D.
Sociocultural factors and back pain: A population-based study in Belgian adults.
Spine. 1994;19:129137Shekelle P.
The epidemiology of low back pain.
In: Giles LGF, Singer KP, editors.
Low Back Pain.
Oxford, UK: Butterworth Heineman; 1997. pp. 1831.Waxman R, Tennant A, Helliwell P.
A prospective follow-up study of low back pain in the community.
Spine. 2000;25:20852090Waddell. G..
A New Clinical Model For The Treatment Of Low-back Pain
Spine (Phila Pa 1976) 1987 (Sep); 12 (7): 632-644Abbott JH, Mercer SR.
The natural history of acute low back pain.
New Zealand J Physio. 2002;30:816.Pengel LHM, Herbert RD, Maher CG, Refshauge KM.
Acute low back pain: Systematic review of its prognosis.
Br Med J. 2003;327:323325Luo X, Pietrobon R, Sun SX, Liu GG, Hey L.
Estimates and Patterns of Direct Health Care Expenditures Among Individuals
With Back Pain in the United States
Spine (Phila Pa 1976) 2004 (Jan 1); 29 (1): 7986Maniadakis N, Gray A.
The economic burden of back pain in the UK.
Pain. 2000;84:95103van Tulder MW, Koes BW, Bouter LM.
A cost-of-illness study of back pain in the Netherlands.
Pain. 1995;62:233240Waddell G.
The Back Pain Revolution.
Edinburgh, UK: Churchill Livingstone; 1998.Bekkering G, Hendrix H, van Tulder M, et al.
Prognostic factors for low back pain in patients referred for physiotherapy.
Spine. 2005;30:18811886van Tulder M, Becker A, Bekkering T, Breen A, Carter T, Gil del Real MT.
European Guidelines for the Management of Acute Nonspecific Low Back Pain in Primary Care
European Spine Journal 2006 (Mar); 15 Suppl 2: S169191Dionne C, Bourbonnais R, Fremont P, Rossignol M, Stock SR.
A clinical return-to-work rule for patients with back pain.
Can Medical Assoc J. 2005;172:15591567Grotle M, Brox J, Veierod M, Glomsrod B, Lonn JH, Vollestad NK.
Clinical course and prognostic factors in acute low back pain: Patients consulting
primary care for the first time.
Spine. 2005;30:976982Hagen E, Svensen E, Eriksen H.
Predictors and modifiers of treatment effect influencing sick leave in subacute
low back pain patients.
Spine. 2005;30:27172723Pransky G, Verma S, Okurowski L, Webster B.
Length of disability prognosis in acute occupational low back pain:
Development and testing of a practical approach.
Spine. 2006;31:690697Steenstra I, Koopman F, Knol D, et al.
Prognostic factors for duration of sick leave due to low back pain in Dutch
health care professionals.
J Occup Rehab. 2005;15:591605Storheim K, Brox J, Holm I, Bo K.
Predictors for RTW in sick-listed acute LBP-with guideline-based treatment.
J Rehabil Med. 2005;37:365371Wessels T, van Tulder M, Sigl T, Ewert T, Limm H, Stucki G.
What predicts outcome in non-operative treatments of chronic low back pain?
A systematic review.
Eur Spine J. 2006;12:16331644Kjersti S, Brox J, Holm I, Bo K.
Predictors of return to work in patients sick-listed for sub-acute low back pain:
A 12-month follow-up study.
J Rehabil Med. 2005;37:365371Heneweer H, Aufdemkampe G, van Tulder Kiers H, Stappaerts KH.
Psychosocial variables in patients with (sub)acute low back pain: An inception cohort
in primary care physical therapy.
Spine. 2007;32:586592Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE.
Identifying subgroups of patients with acute/sub-acute non-specific low back pain.
Spine. 2006;31:623631Long A, Donelson R, Fung T.
Does it matter which exercise? A randomized control trial of exercise for low back pain.
Spine. 2004;29:25932602McKenzie R, May S.
The Lumbar Spine Mechanical Diagnosis and Therapy, 2nd ed.
Wainakae, New Zealand: Spinal Publications; 2003.Donelson R, Murphy K, Silva G.
Centralization phenomenon: Its usefulness in evaluating and treating referred pain.
Spine. 1990;15:211213Long A.
The centralization phenomenon: Its usefulness as a predictor of outcome
in conservative treatment of chronic low back pain.
Spine. 1995;20:25132521Karas R, McIntosh G, Hall H, Wilson L, Meles T.
The relationship between nonorganic signs and centralization of symptoms in the
prediction of return to work for patients with low back pain.
Phys Ther. 1997;77:354360George SZ. Bialosky JE, Donald DA.
The centralization phenomenon and fear-avoidance beliefs as prognostic factors for acute
low back pain: A preliminary investigation involving patients classified for
specific exercise.
J Orthop Sports Phys Ther. 2005;35:580588Skytte L, May S, Petersen P.
Centralization: Its prognostic value in patients with referred symptoms and sciatica.
Spine. 2005;30:E293E299Sufka A, Hauger B, Trenary M, et al.
Centralisation of low back pain and perceived functional outcome.
J Orthop Sports Phys Ther. 1998;27:205212Werneke M, Hart DL, Cook D.
A descriptive study of the centralisation phenomenon: A prospective analysis.
Spine. 1999;24:676683Werneke M, Hart DL.
Centralization phenomenon as a prognostic factor for chronic low back pain and disability.
Spine. 2001;26:758765Werneke M, Hart DL.
Discriminant validity and relative precision for classifying patients with non-specific
neck and back pain by anatomic pain patterns.
Spine. 2003;28:161166Deyo R, Battie M, Beurskens A, et al.
Outcome measures for low back pain research: A proposal for standardized use.
Spine. 1998;23:20032013Werneke M, Hart DL.
Categorizing patients with occupational low back pain by use of the Quebec Task Force
Classification system versus pain pattern classification procedures: Discriminant
and predictive validity.
Phys Ther. 2004;84:243254Hahne AJ, Keating JL, Wilson SC.
Do within-session changes in pain intensity and range of motion predict
between-session changes in patients with low back pain?
Aus J Physio. 2004;50:1723Tuttle N.
Do changes within a manual therapy treatment session predict between-session changes
for patients with cervical spine pain?
Aust J Physio. 2005;51:4348Cherkin DC, Deyo RA, Street JH, Barlow W.
Predicting poor outcomes for back pain seen in primary care using
patients' own criteria.
Spine. 1996;21:29002907Goertz MN.
Prognostic indicators for acute low back pain.
Spine. 1990;15:13071310Thomas E, Silman AJ, Croft PR, Papageorgiou AC, Jayson MI.
Predicting who develops chronic low back pain in primary care: A prospective study.
Br Med J. 1999;318:16621667Patrick D, Deyo R, Atlas S, Singer DE, Chapin A, Keller RB.
Assessing health-related quality of life in patients with sciatica.
Spine. 1995;20:18991909Dunn KM. Croft PR.
Classification of Low Back Pain in Primary Care: Using "Bothersomeness"
to Identify the Most Severe Cases
Spine (Phila Pa 1976). 2005 (Aug 15); 30 (16): 18871892McLean SM, May S, Klaber-Moffet J, Sharp DM, Gardiner E.
Prognostic factors for nonspecific neck pain: A systematic review.
Phys Ther Rev. 2007;12:207220.Jordan K, Dunn KM, Lewis M, Croft P.
A minimal clinically important difference was derived for the Roland-Morris Disability
Questionnaire for low back pain.
J Clin Epidemiol. 2006;59:4552
Return to McKENZIE METHOD
Since 5-16-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |