

A Randomized Trial of Chiropractic and Medical Care for Patients
with Low Back Pain: Eighteen-month Follow-up Outcomes
from the UCLA Low Back Pain StudyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Spine (Phila Pa 1976). 2006 (Mar 15); 31 (6): 611–621 ~ FULL TEXT
Eric L. Hurwitz, DC, PhD, Hal Morgenstern, PhD, Gerald F. Kominski, PhD,
Fei Yu, PhD, and Lu-May Chiang, MS
Department of Epidemiology,
UCLA School of Public Health,
Los Angeles, CA, USA.
STUDY DESIGN: Randomized clinical trial.
OBJECTIVES: To compare the long-term effectiveness of medical and chiropractic care for low back pain in managed care and to assess the effectiveness of physical therapy and modalities among patients receiving medical or chiropractic care.
SUMMARY OF BACKGROUND DATA: Evidence comparing the long-term relative effectiveness of common treatment strategies offered to low back pain patients in managed care is lacking.
METHODS: A total of 681 low back pain patients presenting to a managed-care facility were randomized to chiropractic with or without physical modalities, or medical care with or without physical therapy, and followed for 18 months. The primary outcome variables are low back pain intensity, disability, and complete remission. The secondary outcome is participants' perception of improvement in low back symptoms.
RESULTS: Of the 681 patients, 610 (89.6%) were followed through 18 months. Among participants not assigned to receive physical therapy or modalities, the estimated improvements in pain and disability and 18-month risk of complete remission were a little greater in the chiropractic group than in the medical group (adjusted RR of remission = 1.29; 95% CI = 0.80-2.07). Among participants assigned to medical care, mean changes in pain and disability and risk of remission were larger in patients assigned to receive physical therapy (adjusted RR = 1.69; 95% CI = 1.08-2.66). Among those assigned to chiropractic care, however, assignment to methods was not associated with improvement or remission (adjusted RR = 0.98; 95% CI = 0.62-1.55). Compared with medical care only patients, chiropractic and physical therapy patients were much more likely to perceive improvement in their low back symptoms. However, less than 20% of all patients were pain-free at 18 months.
CONCLUSIONS: Differences in outcomes between medical and chiropractic care without physical therapy or modalities are not clinically meaningful, although chiropractic may result in a greater likelihood of perceived improvement, perhaps reflecting satisfaction or lack of blinding. Physical therapy may be more effective than medical care alone for some patients, while physical modalities appear to have no benefit in chiropractic care.
Key words: low back pain, randomized trial, chiropractic, physical therapy, managed care.
From the Full-Text Article:
Background
Low back pain is one of the most common reasons for visiting a medical physician [1] or physical therapist [2] and is the leading complaint among persons accessing chiropractic care in the United States. [3] Indeed, chiropractic is the most frequently used alternative treatment for back problems [4] and is the most commonly used unconventional therapy in the United States. [5] Chiropractic care is now included in several managed-care plans, and the trend of managed-care organizations serving an increasing proportion of the population has continued up to the present. [6, 7]
Despite the high economic costs, disability, and lost productivity associated with low back pain in the United States and Europe, [8–11] and the development of several treatment guidelines, [12, 13] management of low back pain remains controversial and highly variable across professions and geographic regions. [14] Although several recent studies have compared chiropractic care with medical care and/or physical therapy for patients with low back pain, [15–22] ours is the only randomized clinical trial (RCT) to have been conducted entirely within a managed-care practice setting. [23] We previously reported that in the short-term (6 months), chiropractic and medical care for low back pain are comparable in their clinical effectiveness, but physical therapy may be marginally more effective than medical care alone for reducing disability in some patients. [23]
The purpose of this paper is to extend the analysis to participants followed through 18 months and to contrast and compare effect estimates from the primary (clinical) and secondary (perceived effectiveness) outcome measures. The three objectives are to compare the long-term clinical and perceived effectiveness of:1) medical and chiropractic care for low back pain patients in managed care,
2) physical therapy among medical patients, and
3) physical modalities among chiropractic patients.
Materials and Methods
Study Design and Source Population.
Low back pain patients presenting at 3 primary-care centers of a 100,000-member health-care network based in southern California were randomized in a balanced design to 4 treatment groups:chiropractic care with and without physical modalities, and
medical care with and without physical therapy.Follow-up questionnaires were mailed to participants at 2 and 6 weeks and at 6, 12, and 18 months. All study protocols and forms were approved by the institutional review boards (IRB) from UCLA and the healthcare network. Key design and protocol details are given below; additional methodologic information has been previously reported. [23]
Eligibility Criteria.
Patients were eligible for the clinical trial if they:1) were health maintenance organization members with the network chosen as their healthcare provider;
2) sought care at one of the 3 study sites from October 30, 1995 through November 9, 1998;
3) presented with pain in the region of the lumbosacral spine and its surrounding musculature;
4) had not received professional care for low back pain within the previous 1 month; and
5) were at least 18 years of age.Patients were excluded if they had pain due to fracture, tumor, infection, spondyloarthropathy, or other nonmechanical cause; had severe comorbidity; had a pacemaker or other electrical device; had a blood coagulation disorder or were on corticosteroids or anticoagulants; had progressive lower limb muscle weakness; had current signs or symptoms of cauda equina syndrome; had plans to move out of the area; could not be contacted by telephone; lacked the ability to read English; or had pending thirdparty liability or Workers’ Compensation cases.
Recruitment and Enrollment.
All patients presenting with symptoms consistent with low back pain were initially screened by the field coordinator and asked if they would be willing to participate in a study addressing the effectiveness of different types of care for low back pain. Patients received a brochure describing the study, its protocols, and the requirements of participation. A primary-care provider conducted a detailed history and physical examination on each eligible patient, and ordered imaging studies or additional diagnostic tests if necessary to rule out specific spinal pathology. Radiologic examinations were ordered on 9.5% of enrolled patients.
Patients meeting the eligibility criteria and agreeing to participate read and signed the IRB-approved informed consent form, which was administered by the field coordinator and witnessed by a third party.
Our statistician wrote a computer program to generate randomized treatment assignments in blocks of 12, stratified by site, and placed each assignment in a numbered security envelope. Each of the 3 sites had its own series of sequentially numbered sealed envelopes. On receiving consent, the field coordinator opened the appropriate envelope, informed the participant of the assignment, directed him or her to fill out the baseline questionnaire, and scheduled the same-day appointment with a medical or chiropractic provider.
InterventionsChiropractic Care Without Physical Modalities (DC Group) Participants randomized to the DC group received spinal manipulation or mobilization, instruction in strengthening and flexibility exercises, and instruction in proper back care.
Chiropractic Care With Physical Modalities (DCPm Group) In addition to chiropractic care (above), participants randomized to the DCPm group received heat or cold therapy, ultrasound, and/or electrical muscle stimulation (EMS), at the chiropractor’s discretion.
Medical Care Without Physical Therapy (MD Group) Participants randomized to the MD group received one or more of the following at the discretion of the medical provider: instruction in proper back care and strengthening and flexibility exercises; prescriptions for analgesics, muscle relaxants, or anti-inflammatories; and lifestyle recommendations.
Medical Care With Physical Therapy (MDPt Group) In addition to medical care (above), participants randomized to the MDPt group received instruction in proper back care and, at the discretion of the physical therapist, one or more of the following: heat or cold therapy, ultrasound, EMS, soft tissue and joint mobilization, traction, supervised therapeutic exercise, and strengthening and flexibility exercises. The interventions most commonly used on study participants were heat or cold therapy (71%), supervised therapeutic exercise (59.5%), ultrasound (45%), EMS (33.6%), and joint mobilization (19.9%).
Data Sources and CollectionBaseline Pain and Disability Data. The baseline questionnaire included items on low back pain and related disability. Intensity of most severe low back pain and average level of pain for the past week were measured with 0 to 10 numerical rating scales, where 0 = no pain and 10 = unbearable pain. These scales have been shown to have excellent reliability and validity for measuring back pain. [24] Current disability due to low back pain was measured with the previously validated 24-item Roland- Morris Low-Back Disability Questionnaire, [25–31] where 0 indicates no disability and 24 indicates severe disability due to low back pain.
We also asked participants several questions about their current and past episodes of low back pain, including the number of previous episodes, length of current episode, frequency of pain, disability days, and history of trauma.
Other Baseline Data. Sociodemographic and other possible prognostic factors were also queried at baseline. Sociodemographic variables included age, sex, race/ethnicity, education, household income, marital status, and current employment status. General health status was measured with 5 of 8 subscales of the previously validated Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36):1) limitations in physical activities because of physical or emotional problems;
2) limitations in usual role activities because of physical health problems;
3) limitations in usual role activities because of emotional health problems;
4) general health perceptions; and
5) general mental health. [32, 33]Follow-up Data. Follow-up questionnaires mailed to participants at 2, 6, 26, 52, and 78 weeks after their baseline visits addressed low back pain intensity, related disability, and perceived improvement. Pain status was measured with repeat 0 to 10 pain scales, and low back-related disability was measured with repeat Roland-Morris Low-Back Disability Questionnaires. Perceived improvement was assessed with scales of perception of change in low back symptoms during the preceding follow-up interval, with the following response options: “a lot worse,” “a little worse,” “about the same,” “a little better,” or “a lot better.” At each follow-up assessment, we also asked participants about the frequency of pain in the past week, number of disability days, and use of over-the-counter (OTC) and prescription medications to deal with their low back pain.
Outcome Variables. Four primary outcome variables were used to evaluate the effectiveness of assigned treatment group: average level of low back pain in the past week (0–10 scale), most severe low back pain in the past week (0–10 scale), current back-related disability score (0–24 Roland-Morris Questionnaire), and complete remission, defined as the first observation during follow-up in which the above outcome variables were zero (i.e., no low back pain in the past week and no related disability). Cutpoints of 2 or more points (vs.<2) on the 0 to 10 scales and 3 or more points (vs.<3) on the Roland-Morris scale were used as dichotomous outcomes. [8, 29] Differences between groups of 2+ and 3+ points on the pain and disability scales, respectively, were considered clinically relevant.
The secondary outcome was perceived improvement as measured by patients’ self-reports of their perceptions of change in low back pain symptoms during the preceding follow- up interval. Because of the small number of respondents reporting worsening of their symptoms, the response options “a lot worse” and “a little worse” were collapsed into one category; “a lot better” and “a little better” were left intact.
Data Analysis. To estimate treatment effects, we used intention- to-treat analyses and made 3 contrasts between treatment groups: DC versus MD, MDPt versus MD, and DCPm versus DC. Two statistical methods were used to estimate these 3 effects on the primary outcomes: The first involved treating each outcome variable as a continuous variable, whereas the second involved combining all 3 outcomes into a composite dichotomous measure, called complete remission. A third statistical method, polytomous logistic regression using a Markov (transition) model, was used to estimate treatment effects on perception of improvement. SAS 8.1 was used for data management and analysis. [34]
In the first method, applied separately to each outcome at all 6 observations, a mixed-effects linear model was fit to the data. [35, 36] To allow for heteroscedasticity in the variancecovariance matrix, we treated outcome values between individual subjects as independent, while outcome values within each subject were treated as correlated with a common unspecified variance-covariance structure. The other covariates in the model were follow-up time, age, sex, and 3 characteristics of the subject’s low back pain at baseline: duration of the current episode, number of previous episodes, and frequency of pain in the past week. Since the effects of treatment group were represented by the outcome changes (slopes) over follow-up time and it is unrealistic to assume linear treatment effects (constant slopes) for the entire 18-month follow-up period, linear splines for treatment effects (piece-wise linear slopes) at each follow-up time were used to allow outcome changes (slopes) to differ across follow-up intervals within each treatment group and to differ across treatment groups within each follow-up interval. To measure treatment effects for each outcome, we used the fitted model to estimate treatment-group differences (and 95% confidence intervals [CIs]) in mean outcome change between baseline and 6 months, baseline and 12 months, and baseline and 18 months. In addition, the adjusted means in each outcome by treatment group and follow-up time were graphed for the entire 18-month follow-up period. To reflect the adjusted mean in the population, each covariate was set equal to its mean value in the total sample.
In the second method, we observed the time to first complete remission after baseline. First complete remission for a given subject was defined as the first observation during follow-up in which all 3 outcome variables were zero (i.e., no low back pain in the past week and no related disability). Unconditional logistic regression was used to compare the 18-month probability (risk) of complete remission between treatment groups. Results of the fitted model were used to estimate risk ratios (and 95% CIs) for the same treatment-group contrasts described above. In addition to treatment group, other covariates in this model were age, sex, the 3 low back pain variables described above, and the baseline value of each outcome variable from which composite measure was derived. To estimate risk ratios for the treatment contrasts, each covariate was set equal to its mean value in the total sample. Because this method excluded 10% of all subjects lost to follow-up, we also used proportional hazards (survival) analysis to compare the remission rates between treatment groups. Since the results of these 2 methods were similar, we report here only the logistic regression results.
In the third method, we fit a first-order Markov transition model to estimate treatment effects on patient’s perception of low back pain improvement, recorded as “a lot better,” “a little better,” “about the same,” and “worse,” allowing for multiple categories by relating transition probabilities to covariates and previous outcomes through a polytomous logistic regression model with Markov structure. [37] In addition to treatment group and past outcomes, the other covariates were age, sex, duration of current episode at baseline, and 4 indicator variables reflecting follow-up times with 2 weeks as the reference category. All models used “about the same” as the reference response level. Estimated treatment effects are presented as odds ratios (ORs) with 95% CIs. The PHREG and GENMOD procedures in SAS were used for fitting the polytomous logistic regression models. [38] Additional details about the application of these models may be found elsewhere. [39]
Results
Recruitment, Enrollment, and Follow-up
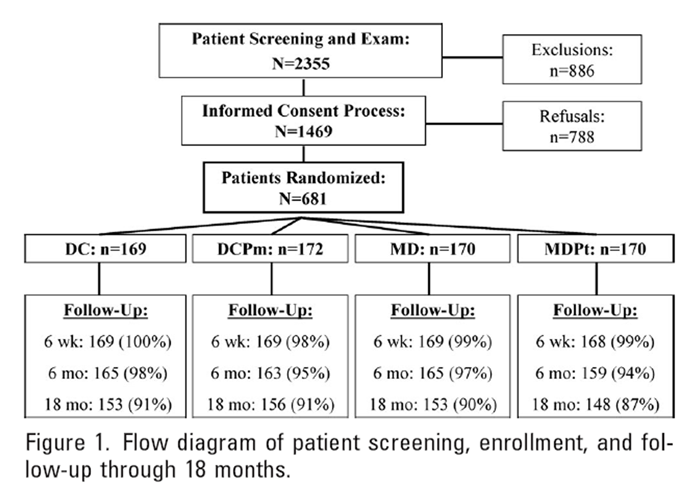
Figure 1 Figure 1 shows the flow of patients from initial screening through end of follow-up. A total of 886 (37.6%) of the 2,355 screened patients were excluded for the following reasons (number in parentheses):
recent treatment for low back pain (270),
lack of health maintenance organization insurance coverage (199),
symptoms inconsistent with low back pain (144),
third party liability or Workers’ Compensation case (55),
inability to read English (46),
less than 18 years old (43),
plans to move out of the area (18),
and inaccessible by telephone (4).Patients were also excluded for the following medical reasons:
low back pain due to fracture, tumor, or infection, ankylosing spondylitis, or other rheumatic disease (47),
severe comorbidity (37),
use of anticoagulants (13),
treatment with electrical device (5),
progressive lower limb muscle weakness (2),
abdominal aortic aneurysm (1),
blood coagulation disorder (1), and
signs or symptoms of possible cauda equina syndrome (1).Of the 1,469 eligible patients, 779 (53.0%) declined participation because of:
lack of interest (345),
inconvenience (137),
preference for medical care (116),
preference for chiropractic care (105),
desire for multiple treatment options (45), and
inability to afford copayments (31).Because of the apparent lack of understanding of the informed consent form, 9 additional otherwise eligible and willing prospective participants were not enrolled. We therefore enrolled 681 patients for an acceptance rate [number of enrollees/number of eligible patients] of 46.4%.
Two- and 6-week follow-up questionnaires were completed by 679 (99.7%) and 675 (99.1%) participants, respectively. Questionnaires at 6, 12, and 18 months were completed by 652 (95.7%), 629 (92.4%), and 610 (89.6%) participants, respectively.
Characteristics of Study Population

Table 1

Table 2 Table 1 shows the baseline distributions of sociodemographic and health-status variables by treatment group. Fifty-two percent of the participants are female, half are under age 50, 40% are nonwhite, and two thirds are currently employed. The SF-36 scores are lower than the U.S. general population norms, [32] although compatible with other back pain populations. [18, 40, 41]
Table 2 shows the baseline distributions of low back-related variables. Almost half of the participants had been in pain for longer than 1 year, and more than 80% reported prior episodes of low back pain. The median low back disability score of 11 reflects moderate disability, whereas the pain intensity scores indicate appreciable levels of pain perception. There are no clinically meaningful differences between treatment groups in the distributions of possible prognostic factors measured at baseline.
Utilization
Fifty-five percent of all low back-related patient visits took place within the first 6 weeks following randomization; 85% occurred within 6 months. In the initial 6 months, patients assigned to one of the chiropractic groups or the physical therapy group had, on average, almost twice as many visits (5.4 vs. 2.9) as patients assigned to medical care alone. Average visit duration was twice as long for physical therapy patients as for medical and chiropractic patients (31 vs. 15 minutes). Visit frequencies after 6 months did not appreciably differ between groups or providers. There were a total of 3 low back surgeries (one in each of the medical groups and one in the chiropractic care without physical modalities group), all performed between 6 and 18 months of follow-up.
Primary Outcomes

Table 3
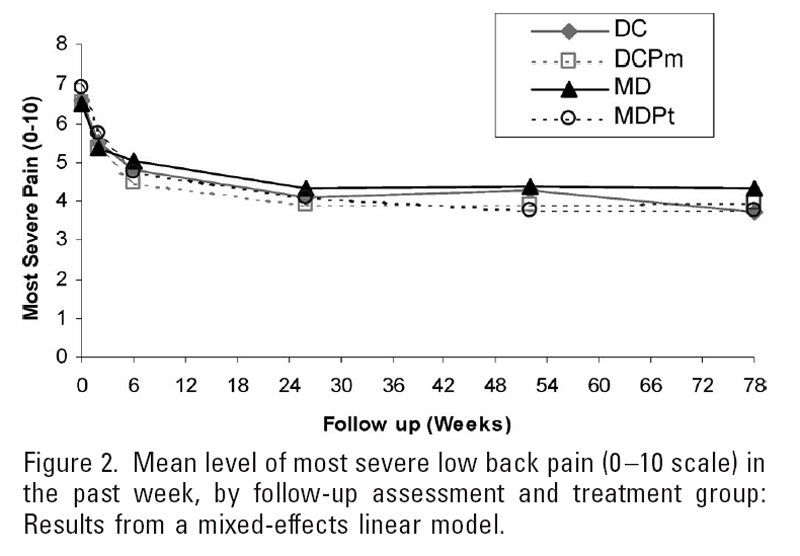
Figure 2

Figure 3
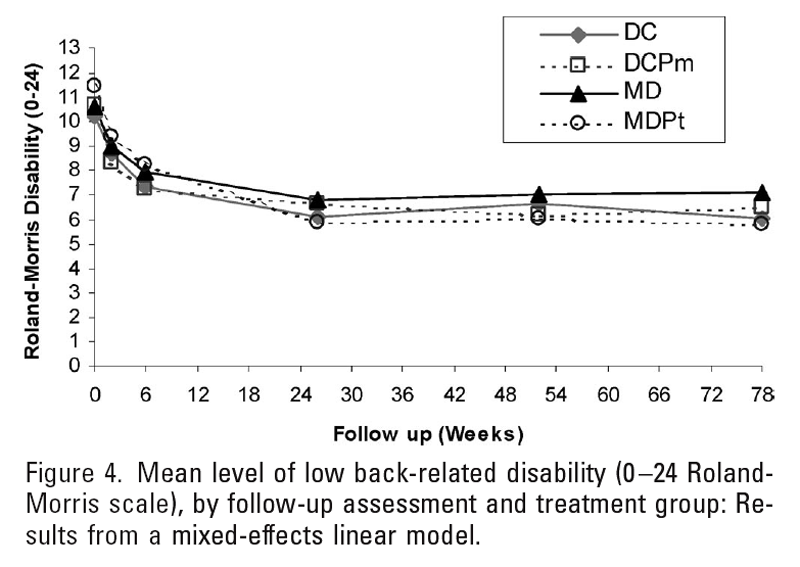
Figure 4

Table 4

Table 5 Table 3 shows the estimated effects from the mixed-effects linear models (adjusted differences in mean changes and 95% CIs) of chiropractic care only versus medical care only, medical care with physical therapy versus medical care only, and chiropractic care with physical modalities versus chiropractic care only on pain intensity and disability from baseline to 6, 12, and 18 months.
Figures 2 to 4 show the mean levels of pain and disability by follow-up assessment and treatment group. Although medical patients assigned to physical therapy had greater reductions in pain and disability than did medical patients not assigned to physical therapy, the differences are of marginal clinical significance at best. Using our a priori definitions of clinically relevant differences in pain and disability, none of the estimated effects would be considered clinically meaningful, although the estimated effects of DC versus MD and MDPt versus MD were relatively stronger after 18 months than after 6 months.
Table 4 shows the estimated adjusted 18-month risk ratio of clinical remission, by treatment-group contrast, from the logistic regression analysis. Twenty-three percent of all participants had complete remissions. Medical patients assigned to physical therapy were more likely than medical patients not assigned to physical therapy to remit during the 18-month follow-up period (RR = 1.69; 95% CI = 1.08–2.66). Chiropractic patients were also somewhat more likely than medical patients to remit (RR = 1.29; 95% CI = 0.80–2.07). Chiropractic with physical modalities did not result in any apparent benefit relative to chiropractic care without modalities (RR = 0.98; 95% CI = 0.62–1.55).
Secondary Outcomes
Table 5 shows the estimated adjusted treatment effects on perceived change in low back pain, from the transition polytomous logistic regression model. The odds of perceiving their pain as a little or a lot better (vs. perceiving no change) since the previous assessment were greater among patients assigned to chiropractic care without modalities (a lot better: OR = 1.83; 95% CI = 1.34–2.49; a little better: OR = 1.39; 95% CI = 1.08–1.79) and medical patients assigned to physical therapy (a lot better: OR = 1.67; 95% CI = 1.22–2.28; a little better: OR = 1.45; 95% CI = 1.13–1.87) than among medical patients not assigned to physical therapy. Chiropractic patients assigned to physical modalities were more likely than those not assigned to modalities to perceive their pain as worsening (vs. staying the same) since the previous assessment (OR = 0.63; 95% CI = 0.45–0.91).
Frequency of Pain, Disability Days, and Use of Medications
After 18 months of follow-up, 25% of all participants reported having low back pain most or all of the time in the past week; less than 20% reported having no pain. Participants in the medical care group were most likely to have pain most or all of the time (30%) and least likely to be pain-free (15%). The frequencies of disability days (cut-down and bed days) due to low back pain did not appreciably vary by treatment group. At each follow-up assessment, about 40% of all participants reported at least one cut-down day and 10% at least one bed day in the past month. There were no known treatment-related adverse events requiring IRB notification during the 18- month follow-up.
At each follow-up assessment, participants in the medical care groups were more likely to report prescription-pain medication use than were participants in the chiropractic groups (32% vs. 24% at 6 months; 29% vs. 20% at 12 months; 27% vs. 19% at 18 months). The most frequently prescribed drugs were nonsteroidal antiinflammatory drugs (NSAIDs), muscle relaxants, and narcotic analgesics. Patients assigned to chiropractic care were somewhat more likely than those assigned to medical care to report OTC-pain medication use at 6 months (56% vs. 49%) but not at 12 or 18 months (56% vs. 58% at 12 months; 53% vs. 51% at 18 months). Assignment to physical modalities or physical therapy among chiropractic and medical participants, respectively, did not appear to influence reported use of prescription or OTC medications.
Discussion
In a managed-care population comprised of mostly subacute and chronic low back pain patients, we observed relatively small differences in clinical outcomes between 4 popular low back pain management strategies during 18 months of follow-up. Larger differences were observed for patients’ perceptions of improvement. Among participants not assigned to receive physical therapy or modalities, there was slightly more improvement in the chiropractic group than in the medical group, and the estimated effects were somewhat stronger after 18 months than after 6 months. Chiropractic patients were much more likely than medical patients to perceive their pain as being a little or a lot better during the 18 months of follow-up, possibly reflecting, in part, satisfaction with care. [42] Among participants assigned to medical care, there was more remission and improvement in the physical therapy group, with relatively stronger effects observed after 18 months than after 6 months. These patients were also more likely to perceive their pain as being a little or a lot better during follow-up. As was also found in the short-term among participants assigned to chiropractic care, [43] no association was detected between physical modalities and low back pain outcome after 18 months, and patients assigned to modalities were actually more likely than patients not assigned to modalities to perceive their pain as getting worse.
The management approaches in our trial each include specific components, such as medications, exercises, spinal manipulative therapy, and advice, many of which have been the focus of recent systematic reviews. Published findings show that acetaminophen, [44] NSAIDs, [44–48] muscle relaxants, [45, 47, 49] conditioning exercises and certain aerobic activities, [50] and advice to stay active [51] may provide shortterm benefit for patients with acute low back pain; NSAIDs, [47] exercise therapy, [47, 48, 50, 52–55] massage, [56, 57] and cognitive behavioral or multidisciplinary biopsychosocial rehabilitation therapy [58, 59] may be of some benefit for patients with chronic low back pain; and that current evidence does not support bed rest [47, 60] or physical agents or modalities for acute or chronic low back pain. [47, 61] There is little or no support for the use of transcutaneous electrical nerve stimulation, [62] traction, [63] and specific exercise regimens [50, 53]; and despite more than 20 RCTs of acupuncture for acute and chronic back pain, evidence supporting the effectiveness of its use is unclear. [57] Guidelines for the treatment of low back pain of less than 3 months’ duration are consistent with the above findings, recommending the use of acetaminophen, NSAIDs, and aerobic activities, [12, 13] and recommending against bed rest, physical agents, and transcutaneous electrical nerve stimulation and other modalities. [12, 13]
Several RCTs and systematic reviews comparing chiropractic’s core procedure, spinal manipulation, with other interventions have reported favorable outcomes relative to both sham and active treatments in acute [47, 64] and chronic [47] low back pain, and guidelines support its use. [12, 13] Nevertheless, more recent findings suggest that spinal manipulation may not be more effective than conventional treatments for acute or chronic low back pain. [57, 65] In a meta-regression analysis of 39 RCTs, spinal manipulation was found to be superior only when compared with sham or therapies known to be ineffective, such as traction or bed rest. [65] However, the investigators of a systematic review and best evidence synthesis of 46 RCTs of spinal manipulative therapy for low back pain concluded that spinal manipulation is as effective as NSAIDs and may result in marginally better clinical outcomes relative to general practitioner care in the short-term and physical therapy in the long-term for patients with chronic pain. [66] The literature also indicates that analgesics and other medications given during the course of standard medical care are much more likely to be associated with adverse reactions than are comparator treatments, [12, 45, 46, 49, 66] and may delay recovery, [67] and that complications following spinal manipulation of the lumbar spine are very rare. [64, 66, 68, 69]
In addition to our trial, chiropractic care or spinal manipulative therapy has been compared with physical therapy and/or medical care in a few recent, well-conducted RCTs and observational studies. No clinically meaningful treatment-group differences in outcomes were found in the total study populations of the RCTs conducted by Meade et al, [16, 17]and Skargren et al, [20, 21] although certain subgroup differences were detected. Cherkin et al [19] also reported no meaningful differences between chiropractic and physical therapy outcomes, and their pain and disability outcomes were only slightly better than those observed in a group receiving only an educational booklet. An additional RCT comparing subacute-pain patients receiving 12 weeks of either osteopathic or routine medical care found comparable clinical outcomes but greater prescription-medication use in the medical group. [22]
Three observational studies are worth noting. Pain and disability outcomes were similar at 6 months among acute and subacute low back pain patients of primary care physicians, orthopedic surgeons, and chiropractors. [18] Acute and chronic low back pain patients of chiropractors enrolled in a large observational, practice-based study had better pain and disability outcomes after 1 year than did patients of medical physicians. [70] Among respondents of a national survey in the United States, persons visiting chiropractors for back or neck pain treatment in the past year were more than twice as likely as those visiting conventional providers to rate their care as “very helpful” (61% vs. 27%). [71] However, given the lack of randomization and evidence indicating that patients of chiropractors and medical physicians differ with respect to health status and other prognostic factors, [72, 73] findings from these observational studies are not easily interpretable.
Regardless of treatment, a large proportion of persons with low back pain do not become pain- and disability-free. In our trial, only about 20% of participants had absolutely no symptoms after 12 and 18 months, and more than 25% reported having pain most or all of the time. These figures are consistent with the findings from a review of low back pain in general patient populations, showing that up to 75% of patients still have pain 12 months later, and 60% of those who became pain-free relapsed within 12 months. [74] Similar findings have been reported in more recent long-term clinic- [70] and population- based studies. [75] Given this natural history of often persistent and recurring pain in a large segment of low back pain sufferers, even after one or more episodes of care, and the high prevalence of significant comorbidity, [76] it is apparent that focusing on the low back may not be the optimal strategy for long-term relief. Interventions that address behavior modification aiming for long-term benefits in general health and well-being, rather than back-specific treatment, may be more effective in ameliorating back pain and its many personal, social, and economic consequences. For example, promoting exercise and leisure-time physical activity may be an inexpensive, safe, and efficacious approach to reduce not only low back pain and associated work-loss days, [54, 77] but also psychologic distress and pain-related fear and anxiety. [55, 78] Consistent with findings from other recent RCTs showing the benefits of supervised exercise for patients with subacute and chronic low back pain, [79–81] the generally more favorable outcomes among physical therapy participants may be due to the therapists’ greater emphasis on active care. [82]
Although randomization and an 18-month follow-up rate of almost 90% likely preclude appreciable bias due to confounding or selective follow-up loss, findings from our clinical trial should be considered in light of the following limitations. First, because of the nature of the interventions, there could be no masking of participants or providers. Estimates of treatment effects could be biased by differential error in outcome measurement or by differential behavior of providers or participants during follow-up that might affect the outcome. The estimated effects of treatment on perceived changes in symptoms may be especially affected by lack of patient blinding. Second, if the eligible patients who declined to participate differed from participants on factors that modify treatment effects, then our effect estimates may not accurately reflect the results that would have been obtained from the total source population. Although this does not impact the study’s internal validity, generalizing the findings may be problematic. Third, generalizing the findings to patients in other settings or to those who receive their health care through different reimbursement mechanisms may not be appropriate. Healthcare practitioners in other environments may manage their low back pain patients in ways that affect treatment results, and fee-forservice and other reimbursement systems (e.g.,Workers’ Compensation, personal injury) may involve incentives that affect utilization and outcomes. Nevertheless, our study population is clinically similar to other ambulatory low back pain populations, [19, 25, 83–87] and we have no evidence that nonparticipants were systematically different from participants, or that treatment effects appreciably vary by baseline episode duration or other clinical subgroups.
Conclusion
Small differences in clinical outcomes were observed among low back pain patients randomized to chiropractic care with and without physical modalities, and medical care with and without physical therapy during 18 months of follow-up. The differences in pain and disability outcomes between medical and chiropractic care without physical therapy or modalities are not clinically meaningful, although patients of chiropractors are more likely to perceive improvement. Changes in reported pain and disability scores may reflect clinical outcomes, whereas perceived improvement may also reflect satisfaction with care or lack of blinding. Physical therapy may be more effective than medical care alone for some patients, whereas physical modalities used by chiropractors appear to have no effect. Regardless of treatment, a majority of each group had some degree of low back pain at the end of follow-up. Other promising multi-intervention strategies, such as coupling manual and behavioral therapies with the promotion of physical activity, may more favorably influence long-term prognosis and should be the focus of subsequent research.
Key Points
A randomized clinical trial was conducted among low back pain patients to compare the long-term effectiveness of medical and chiropractic care for low back pain and to assess the effectiveness of physical therapy and modalities in a managed-care practice setting.
A total of 681 patients presenting to a managedcare facility were randomized to medical care with and without physical therapy, and chiropractic care with and without physical modalities; 610 (89.6%) were followed up through 18 months.
The differences in pain and disability outcomes between medical and chiropractic care without physical therapy or modalities are not clinically meaningful, although patients of chiropractors are more likely to perceive improvement.
Physical therapy may be more effective than medical care alone for some patients, whereas physical modalities used by chiropractors appear to have no effect. Regardless of treatment, a majority of each group had some degree of low back pain at the end of follow-up.
Acknowledgments
The authors thank Friendly Hills HealthCare Network’ s executive officers for their initial interest, support, and commitment of resources; Gary Pirnat, former chairman of chiropractic services and manager of rehabilitation services, and the medical, chiropractic, and physical therapy providers for their cooperation during the study; and the clinic management teams from La Habra, Brea, and Buena Park and their front-office and health information personnel for their help with patient enrollment. The authors also thank UCLA personnel Karen Hemmerling and Stan Ewald for coordinating patient recruitment and follow-up efforts, Emerlinda Gonzalez and Silvia Sanz for assistance with patient enrollment and tracking, and He-Jing Wang for providing data management services at UCLA.
References:
Hing E, Middleton K.
National Hospital Ambulatory Medical Care Survey: 2002 outpatient department summary.
Adv Data Vital Health Stat 2004; 345.Feine JS, Lund JP.
An assessment of the efficacy of physical therapy and physical modalities for the control of chronic musculoskeletal pain.
Pain 1997;71:5–23.Barnes PM , Powell-Griner E , McFann K , Nahin RL:
Complementary and Alternative Medicine Use Among Adults:
United States, 2002
Advance Data 2004 (May 27); 343: 1–19Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC.
Trends in Alternative Medicine Use in the United States, 1990 to 1997:
Results of a Follow-up National Survey
JAMA 1998 (Nov 11); 280 (18): 1569–1575Druss BG, Rosenheck RA.
Association between use of unconventional therapies and conventional medical services.
JAMA 1999;282:651–6.Yelin E, Herrndorf A, Trupin L, et al.
A national study of medical care expenditures for musculoskeletal conditions: the impact of health insurance and managed care.
Arthritis Rheum 2001;44:1160–1169.Cherry DK, Burt CW, Woodwell DA.
National Ambulatory Medical Care Survey 2001 summary.
Adv Data Vital Health Stat 2003;337.Hashemi L, Webster BS, Clancy EA.
Trends in disability duration and cost of workers’ compensation low back pain claims (1988–1996).
J Occup Environ Med 1998;40:1110–9.Murphy PL, Volinn E.
Is occupational low back pain on the rise?
Spine 1999;247:691–7.Waddell G.
Low back pain: a twentieth century health care enigma.
Spine 1996;21:2820–5.Pai S, Sundarum LJ.
Low back pain: an economic assessment in the United States.
Orthop Clin North Am 2004;35:1–5.Bigos S, Bower O, Braen G, et al.
Acute Lower Back Problems in Adults. Clinical Practice Guideline No. 14.
Rockville, MD: Agency for Health Care Policy and Research,
Public Health Service, U.S. Department of Health and Human Services; 1994Royal College of General Practitioners.
Clinical Guidelines for the Management of Acute Low Back Pain
London: Royal College of General Practitioners; (1999)Waddell G.
The Back Pain Revolution.
Edinburgh: Churchill Livingston, 1998.Hurwitz EL.
The relative impact of chiropractic vs. medical management of low-back pain on health status in a multispecialty group practice.
J Manipulative Physiol Ther 1994;17:74–82.Meade TW, Dyer S, Browne W, et al.
Low Back Pain of Mechanical Origin: Randomised Comparison of Chiropractic and Hospital Outpatient Treatment
British Medical Journal 1990 (Jun 2); 300 (6737): 1431–1437Meade TW, Dyer S, Browne W, et al:
Randomised Comparison of Chiropractic and Hospital Outpatient Management for Low Back Pain:
Results from Extended Follow up
British Medical Journal 1995 (Aug 5); 311 (7001): 349–351Carey TS, Garrett J, Jackman A, et al.
The Outcomes and Costs of Care for Acute Low Back Pain Among Patients
Seen by Primary Care Practitioners, Chiropractors, and Orthopedic Surgeons
New England J Medicine 1995 (Oct 5); 333 (14): 913–917Cherkin DC, Deyo RA, Battie M, et al.
A Comparison of Physical Therapy, Chiropractic Manipulation, and Provision of an
Educational Booklet for the Treatment of Patients with Low Back Pain
New England Journal of Medicine 1998 (Oct 8); 339 (15): 1021-1029Skargren EI, Oberg BE, Carlsson PG, et al.
Cost and effectiveness analysis of chiropractic and physiotherapy treatment for low back and neck pain: sixmonth follow-up.
Spine 1997;22:2167–77.Skargren EI, Carlsson PG, Oberg BE.
One-year follow-up comparison of the cost and effectiveness of chiropractic and physiotherapy as primary management for back pain: subgroup analysis, recurrence, and additional health care utilization.
Spine 1998;23:1875–84.Andersson GBJ, Lucente T, Davis AM, et al.
A comparison of osteopathic spinal manipulation with standard care for patients with low back pain.
N Engl J Med 1999;341:1426–31.Hurwitz EL, Morgenstern H, Harber P, Kominski GF, Belin TR, Yu F, Adams AH
A Randomized Trial of Medical Care with and without Physical Therapy
and Chiropractic Care with and without Physical Modalities for
Patients with Low Back Pain: 6-month Follow-up Outcomes
From the UCLA Low Back Pain Study
Spine (Phila Pa 1976) 2002 (Oct 15); 27 (20): 2193–2204Strong J, Ashton R, Chant D.
Pain intensity measurement in chronic low back pain.
Clin J Pain 1991;7:209–18.Roland M, Morris R.
A study of the natural history of back pain: I. Development of a reliable and sensitive measure of disability in low-back pain.
Spine 1983;8:141–50.Deyo RA.
Comparative validity of Sickness Impact Profile and shorter scales for functional assessment in low-back pain.
Spine 1986;11:951–4.Deyo RA, Centor RM.
Assessing responsiveness of functional scales to clinical change: analogy to diagnostic test performance.
J Chronic Dis 1986;39: 897–906.Jensen MP, Strom SE, Turner JA, et al.
Validity of the Sickness Impact Profile Roland scale as a measure of dysfunction in chronic pain patients.
Pain 1992;50:157–62.Hsieh CJ, Phillips RB, Adams AH, et al.
Functional outcomes of low back pain: comparison of four treatment groups in a randomized controlled trial.
J Manipulative Physiol Ther 1992;15:4–9.Bouter LM, van Tulder MW, Koes BW.
Methodologic issues in low back pain research in primary care.
Spine 1998;23:2014–20.Ostelo RW, de Vet HC, Knol DL, et al.
24-item Roland-Morris Disability Questionnaire was preferred out of six functional status questionnaires for post-lumbar disc surgery.
J Clin Epidemiol 2004;57:268–76.Ware JE, Sherbourne CD.
The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection.
Med Care 1992;30: 473–83.McHorney CA, Ware JE.
Construction and validation of an alternate form general mental health scale for the Medical Outcomes Study Short-Form Health Survey.
Med Care 1995;33:15–28.SAS Institute Inc.
The SAS System for Windows 8.1.
Cary, NC: SAS Institute, 2000.Zeger SL, Liang K-Y.
Longitudinal data analysis for discrete and continuous outcomes.
Biometrics 1986;42:121–30.Liang K-Y, Zeger SL.
Longitudinal data analysis using generalized linear models.
Biometrika 1986;73:13–22.Diggle PJ, Liang K-Y, Zeger SL.
Analysis of Longitudinal Data.
New York: Oxford University Press, 1994.SAS Institute Inc.
SAS/STAT Software, version 8.
Cary, NC: SAS Institute, 2000.Yu F, Morgenstern H, Hurwitz EL, et al.
Use of a Markov transition model to analyse longitudinal low-back pain data.
Stat Methods Med Res 2003;12: 321–31.Hays RD, Brown JA, Spritzer KL, et al.
Member ratings of health care provided by 48 physician groups.
Arch Intern Med 1998;158:785–90.Coulter ID, Hurwitz EL, Adams AA, Genovese BJ, Hays R, Shekelle PG.
Patients Using Chiropractors in North America:
Who Are They, and Why Are They in Chiropractic Care?
Spine (Phila Pa 1976) 2002; 27 (3) Feb 1: 291–298Hertzman-Miller RP, Morgenstern H, Hurwitz EL, et al.
Comparing the Satisfaction of Low Back Pain Patients
Randomized to Receive Medical or Chiropractic Care:
Results From the UCLA Low-back Pain Study
Am J Public Health 2002 (Oct); 92 (10): 1628–1633Hurwitz EL, Morgenstern H, Harber P, et al.
The effectiveness of physical modalities among low-back pain patients randomized to chiropractic care: findings from the UCLA Low-Back Pain Study.
J Manipulative Physiol Ther 2002;25:10–20.Deyo RA.
Drug therapy for back pain: which drugs help which patients?
Spine 1996;21:2840–50.Cherkin DC, Wheeler KJ, Barlow W, et al.
Medication use for low back pain in primary care.
Spine 1998;23:607–14.Koes BW, Scholten RJPM, Mens JMA, et al.
Efficacy of non-steroidal antiinflammatory drugs for low back pain: a systematic review of randomised clinical trials.
Ann Rheum Dis 1997;56:214–23.van Tulder MW, Koes BW, Bouter LM.
Conservative treatment of acute and chronic nonspecific low back pain: a systematic review of randomized controlled trials of the most common interventions.
Spine 1997;22:2128–56.van Tulder MW, Scholten RJ, Koes BW, et al.
Nonsteroidal anti-inflammatory drugs for low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group.
Spine 2000;25:2501–13.van Tulder MW, Touray T, Furlan AD, et al.
Muscle relaxants for nonspecific low back pain: a systematic review within the framework of the Cochrane Collaboration.
Spine 2003;28:1978 –92.Abenhaim L, Rossignol M, Valat JP, et al.
The role of activity in the therapeutic management of back pain: report of the International Paris Task Force on Back Pain.
Spine 2000;25(suppl 4):1–33.Hagen KB, Hilde G, Jamtvedt G, et al.
The Cochrane review of advice to stay active as a single treatment for low back pain and sciatica.
Spine 2002;27: 1736–41.Faas A.
Exercises: which ones are worth trying, for which patients, and when?
Spine 1996;21:2874–9.van Tulder M, Malmivaara A, Esmail R, et al.
Exercise therapy for low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group.
Spine 2000;25:2784–96.Kool J, de Bie R, Oesch P, et al.
Exercise reduces sick leave in patients with non-acute non-specific low back pain: a meta-analysis.
J Rehabil Med 2004; 36:49–62.Rainville J, Hartigan C, Martinez E, et al.
Exercise as a treatment for chronic low back pain.
Spine J 2004;4:106–15.Furlan AD, Brosseau L, Imamura M, et al.
Massage for low-back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group.
Spine 2002;27:1896–910.Cherkin DC, Sherman KJ, Deyo RA, et al.
A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage therapy, and spinal manipulation for back pain.
Ann Intern Med 2003;138:898–906.van Tulder MW, Ostelo R, Vlaeyen JW, et al.
Behavioral treatment for chronic low back pain: a systematic review within the framework of the Cochrane Back Review Group.
Spine 2001;26:270–81.Karlalainen K, Malmivaara A, van Tulder M, et al.
Multidisciplinary biopsychosocial rehabilitation for subacute low back pain in working-age adults: a systematic review within the framework of the Cochrane Collaboration Back Review Group.
Spine 2001;26:262–9.Hagen KB, Hilde G, Jamtvedt G, et al.
The Cochrane review of bed rest for acute low back pain and sciatica.
Spine 2000;25:2932–9.Nordin M, Campello M.
Physical therapy. Exercises and the modalities: when, what and why?
Neurol Clin North Am 1999;17:75–89.Brosseau L, Milne S, Robinson V, et al.
Efficacy of the transcutaneous electrical nerve stimulation for the treatment of chronic low back pain: a metaanalysis.
Spine 2002;27:596–603.Harte AA, Baxter GD, Gracey JH.
The efficacy of traction for back pain: a systematic review of randomized controlled trials.
Arch Phys Med Rehabil 2003;84:1542–53.Shekelle PG, Adams AH, Chassin MR, et al.
Spinal manipulation for lowback pain.
Ann Intern Med 1992;117:590–8.Assendelft WJ, Morton SC, Yu EI, et al.
Spinal manipulative therapy for low back pain: a meta-analysis of effectiveness to other therapies.
Ann Intern Med 2003;138:871–81.Bronfort, G, Haas, M, Evans, RL, and Bouter, LM.
Efficacy of Spinal Manipulation and Mobilization for Low Back Pain and Neck Pain:
A Systematic Review and Best Evidence Synthesis
Spine J (N American Spine Soc) 2004 (May); 4 (3): 335–356Bernstein E, Carey TS, Garrett JM.
The use of muscle relaxant medications in acute low back pain.
Spine 2004;29:1346–51.Assendelft WJJ, Bouter LM, Knipschild PG.
Complications of spinal manipulation: a comprehensive review of the literature.
J Fam Pract 1996;42: 475–80.Assendelft WJJ, Koes BW, van der Heijden GJMG, et al.
The effectiveness of chiropractic for treatment of low back pain: an update and attempt at statistical pooling.
J Manipulative Physiol Ther 1996;19:499–507.Haas M, Goldberg B, Aickin M, Ganger B, Attwood M.
A Practice-Based Study of Patients With Acute and Chronic
Low Back Pain Attending Primary Care and Chiropractic
Physicians: Two-Week to 48-Month Follow-up
J Manipulative Physiol Ther 2004 (Mar); 27 (3): 160–169Wolsko PM, Eisenberg DM, Davis RB, Kessler R, Phillips RS:
Patterns and Perceptions of Care for Treatment of Back
and Neck Pain: Results of a National Survey
Spine (Phila Pa 1976) 2003 (Feb 1); 28 (3): 292–297Hurwitz EL, Morgenstern H.
The effects of comorbidity and other factors on medical versus chiropractic care for back problems.
Spine 1997;22: 2254– 64.Cote P, Cassidy JD, Carroll L.
The Treatment of Neck and Low Back Pain:
Seeks Care? Who Goes Where?
Med Care. 2001 (Sep); 39 (9): 956–967Hestbaek L, Leboeuf-Yde C, Manniche C.
Low Back Pain: What Is The Long-term Course?
A Review of Studies of General Patient Populations
European Spine Journal 2003 (Apr); 12 (2): 149–165Jacob T, Baras M, Zeev A, et al.
A longitudinal, community-based study of low back pain outcomes.
Spine 2004;29:1810–7.Hurwitz EL, Morgenstern H.
Correlates of back problems and back-related disability in the United States.
J Clin Epidemiol 1997;50:669–81.Macfarlane GJ, Thomas E, Croft PR, et al.
Predictors of early improvement in low back pain amongst consulters to general practice: the influence of pre-morbid and episode-related factors.
Pain 1999;80:113–9.Hurwitz EL, Morgenstern H, Chiao C.
Effects of Recreational Physical Activity and Back Exercises on Low Back Pain
and Psychological Distress: Findings from the UCLA Low Back Pain Study
Am J Public Health. 2005 (Oct); 95 (10): 1817–1824Frost H, Lamb SE, Klaber Moffett JA, et al.
A fitness programme for patients with chronic low back pain: 2-year follow-up of a randomised controlled trial.
Pain 1998;75:273–9.Moffett JK, Torgerson D, Bell-Syer S, et al.
Randomised controlled trial of exercise for low back pain: clinical outcomes, costs, and preferences.
BMJ 1999;319:279–83.Torstensen TA, Ljunggren AE, Meen HD, et al.
Efficiency and costs of medical exercise therapy, conventional physiotherapy, and self-exercise in patients with chronic low back pain: a pragmatic, randomized, single-blinded, controlled trial with 1-year follow-up.
Spine 1998;23:2616–24.Guccione AA.
Physical therapy for musculoskeletal syndromes.
Rheum Dis Clin North Am 1996;22:551–62.Burton AK, Tillotson KM, Main CJ, et al.
Psychosocial predictors of outcome in acute and subchronic low back trouble.
Spine 1995;20:722–8.Leclaire R, Esdaile JM, Suissa S, et al.
Back school in a first episode of compensated acute low back pain: a clinical trial to assess efficacy and prevent relapse.
Arch Phys Med Rehabil 1996;77:673–9.Malmivaara A, Hakkinen U, Aro T, et al.
The treatment of acute low back pain: bed rest, exercises, or ordinary activity?
N Engl J Med 1995;332: 351–5.Stratford PW, Binkley J, Solomon P, et al.
Defining the minimum level of detectable change for the Roland-Morris questionnaire.
Phys Ther 1996;76: 359–65.Stucki G, Liang MH, Fossel AH, et al.
Relative responsiveness of conditionspecific and general health status measures in degenerative lumbar spinal stenosis.
J Clin Epidemiol 1995;48:1369–78
Return to LOW BACK PAIN
Since 1-12-2007


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |