Chronic Low-Back Pain:
Is Infection a Common Cause?This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: ACA News ~ September 2013 ~ FULL TEXT
By Daniel Redwood, DC
Background:
A 2013 randomized trial by Hanne Albert and colleagues at the University of Southern Denmark, published in the European Spine Journal, [1] found that 100 days of treatment with a disc-penetrating antibiotic was significantly more effective than a placebo for relief of chronic low-back pain (CLBP) in people whose MRI exam showed Modic Type 1 changes, which are associated with degeneration and inflammation. If confirmed by other studies, this would mean that disc infection is a far more common cause of CLBP than previously known.
Rare indeed is the publication of a Research paper with the potential to overturn long-standing, fundamental assumptions about the nature of a disease. Virtually all clinical research is incremental in its expansion of our knowledge — by evaluating the effectiveness of treatment methods, demonstrating the conditions under which they are most likely to be beneficial and exploring the physical mechanisms through which they work. But every now and then, a study like Marshall and Warren’s 1982 discovery [2] of the association between the heliobacter pylori bacterium and peptic ulcers appears out of left field to upend what previously passed for conventional wisdom.
In recent years, arguably the only publication to trigger a major reorientation of our understanding in an area critical to chiropractic practice was the 2008 Cassidy et al. paper in Spine, [3] in which the investigators examined nine years of medical records in the Canadian province of Ontario (covering 100 million patient years) and were able to definitively demonstrate that the likelihood of a stroke is no greater if one visits a doctor of chiropractic (DC) than if one visits a medical doctor. Overnight, this study shifted our understanding of stroke vis-à-vis chiropractic, with the authors concluding: “The increased risks of VBA (vertebrobasilar artery) stroke associated with chiropractic and PCP (primary care physician) visits is likely due to patients with headache and neck pain from VBA dissection seeking care before their stroke. We found no evidence of excess risk of VBA stroke associated (with) chiropractic care compared to primary care.”
New Evidence on Infection and Low Back Pain: Must We Change Our Perspective?
Generations of DCs have been taught that infection, malignancy and fracture are “red flag” conditions that require referral for medical care. Until now, low-back pain identified as having an infectious etiology has been a rare enough occurrence that a doctor of chiropractic might go for years without seeing such a case.
This widespread view on the rarity of infection as a cause of CLBP — held by DCs and medical professionals alike — is sharply challenged by two 2013 papers [1, 4] in the European Spine Journal by Hanne Albert and colleagues at the University of Southern Denmark. Their work builds on previous studies, including one involving 247 people in which nuclear material taken from the intervertebral discs of people with lumbar disc herniations and other spinal disorders such as scoliosis, fracture and tumors was examined, and bacteria (i.e., primarily the anaerobic organism P. acnes) were present in 37 percent of cases involving disc herniation and 0 percent of non-disc cases. [5]
Albert’s group sought to determine whether previously nonresponsive CLBP with Modic Type 1 changes on MRI would respond to antibiotic therapy. The researchers’ European Spine Journal trial [1] clearly indicates that the answer is yes. But unlike the several-day course of antibiotics typically recommended for a bacterial infection of the upper respiratory tract, these intra-disc infections appear to require a much longer course of antibiotic therapy — 100 days in the Albert et al. study.
SIDEBAR:
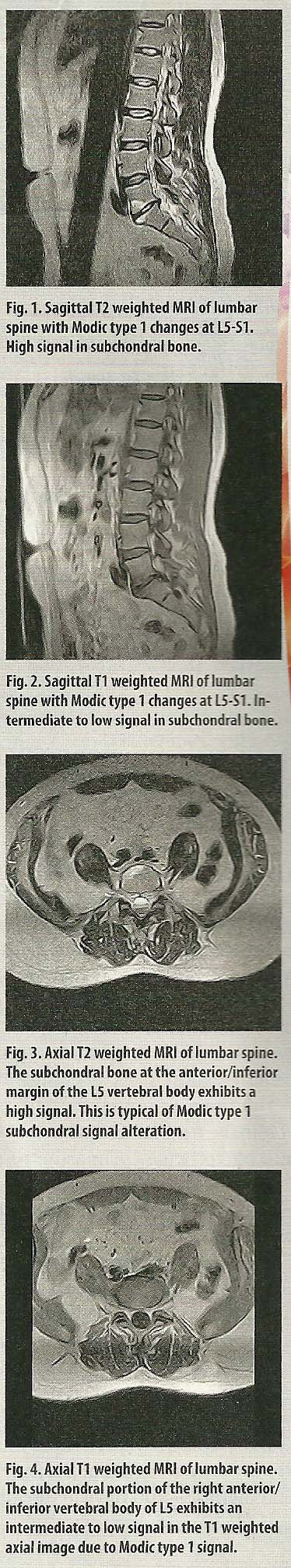
Modic changes, degeneration and chronic low-back pain In 1988, Modic et al. [6] described and validated an MRI-detected vertebral anomaly involving signal changes in the vertebral bone extending from the vertebral endplate. Modic changes (MCs) are strongly associated with disc degeneration [6] and low-back pain. [7] MCs are graded from 1 to 3, with Modic Type 1 the least severe and Type 3 the most severe. [8] On histologic examination, Type 1 involves fissured endplates and vascular granulation tissue adjacent to the endplate; Type 2 has disruption of the endplates and fatty degeneration of the adjacent bone marrow; [9] and Type 3 appears similar to the sclerosis of the bone marrow seen on plain-film radiographs. [6]
A 2008 systematic review [8] of the prevalence of MCs and their association with LBP estimated the median prevalence of MCs in clinical populations at 43 percent and showed that MCs are less common in nonclinical populations, with a median prevalence of 6 percent. In a 2012 study, [10] Wang, Videman and Battie found MCs in 56 percent of middle-aged men. Of these MCs, 64 percent were Type 2, 16 percent were Type 1, and 18 were mixed Type 1 and 2, with 2 percent Type 3 or mixed Type 2 and 3.
A 2012 study whose first two authors are chiropractic researchers at the University of Southern Denmark, Rikke Kryger Jensen and Charlotte Leboeuf-Yde, begins with the statement, “Clinical experience suggests that many patients with Modic changes have relatively severe and persistent low-back pain (LBP), which typically appears to be resistant to treatment.” In this study, Jensen and Leboeuf-Yde’s team found that exercise plus staying active (a guideline-recommended approach) was no more effective than rest and reduced load in patients with persistent CLBP and Modic changes.
In 2013, Albert et al. [1, 4] found that when treated with the disc-penetrating antibiotic Bioclavid (a combination of amoxicillin and clavulanic acid), people with chronic low-back pain and Modic Type 1 changes on MRI achieved levels of improvement far exceeding the placebo group to which their response was compared.
Media Coverage
Shortly after publication of Albert et al.’s research, stories on various mainstream news websites [12, 12] quoted a prominent British neurosurgeon’s opinion that Albert should win the Nobel Prize for medicine for this work. While this might be written off as hyperventilation in the excitement of the moment, it raises the question: When was the last time any study on low-back pain generated this level of interest?
To get a sense of how the story was reported in the press, consider this excerpt from the website of the Daily Mail, a major British newspaper: [12]Dr. Albert, working with colleagues from Birmingham, believes that often this persistent pain is caused not by damaged disc but by rogue bacteria that have infiltrated it. The researcher began by examining tissue taken from discs of people whose back pain was so bad they had had spinal surgery. Around half tested positive for bacteria, with a bug that normally causes acne predominant.
The researchers then allocated 162 men and women who were in “relentless” back pain to a 100-day course of the antibiotic Bioclavid or a placebo. In contrast to the placebo, the antibiotic greatly cut pain and disability. For instance, a year on, those who had taken the drug said they’d experienced 64 hours of pain in the previous month. Those on placebo had racked up 200 hours of pain. And those who had taken the drug took just 19 sick days – compared with 45 by those on placebo, the European Spine Journal reports.
Dr. Albert, of the University of Southern Denmark, described the improvement as “amazing” and said the patients were effectively cured. She added: “I can’t tell you how many people have given me hugs and told me I have given them their life back.”
Responses From Chiropractic Researchers
Jan Hartvigsen, DC, PhD, a professor and researcher in the chiropractic program at the University of Southern Denmark, the institution at which Albert and colleagues performed the antibiotic research, offers a measured response to the antibiotic study.“This is a very interesting result that raises more questions than it answers — which by the way is not unusual in research. Potentially, we have a new and effective treatment for a very specific subgroup of patients with chronic and unrelenting back pain, which is wonderful news. This is, however, only one small trial and before we begin awarding Nobel prizes and prescribing antibiotics on a large scale, the results should be replicated in other trials done by other groups. After all, two-thirds of the patients in the antibiotics group still had pain after the treatment.”
Cheryl Hawk, DC, PhD, dean of research at Logan College of Chiropractic, said of Albert’s study,
“What jumps out at me immediately is that this demonstrates that we’re thinking too narrowly when we call conditions ‘musculoskeletal.’ Nothing is only musculoskeletal, or only psychological, or only gastrointestinal, or only neurological, or only biochemical, etc. Everything in the body (and outside the body, for that matter) is integrated and interactive. From this study, it’s apparent that the immune system, diet and lifestyle contribute to low-back pain in ways we didn’t suspect. I can see that these data can actually have implications for an anti-inflammatory diet, for supporting one’s immune system, and more.”
Chronic low-back pain is challenging for all health professions that treat it. While the most influential current practice guidelines for LBP, [13] prepared jointly by the American College of Physicians and American Pain Society in 2007, recognize spinal manipulation as a non-pharmacologic method “with proven benefits” for CLBP, along with several other nondrug, nonsurgical methods in the chiropractic scope of practice (e.g., intensive interdisciplinary rehabilitation, exercise therapy, acupuncture, massage therapy and yoga), it is unfortunately true that neither manipulation nor any other method used by DCs, MDs or any other type of practitioner can be counted on to offer years-long relief in a majority of cases. For example, in a large (2,870 patients) practicebased study [14] on medical and chiropractic care for low-back pain, a team led by Mitch Haas, DC, at the University of Western States found that while chiropractic CLBP patients experienced somewhat greater relief than medical patients up to one year, exacerbation was common after that for both chiropractic and medical patients.
Questions Answered, Questions Raised
How should DCs respond to this new research, which appears to require at least some recalibration of our understanding of CLBP, a condition for which large numbers of people seek our services? First and foremost, we should cultivate openness to new information such as this, even if we find that it challenges long-held assumptions. Then, as chiropractic researcher Jan Hartvigsen advises, we should wait and see whether the conclusions reached by Albert’s group are confirmed in other studies.
But let’s assume that these results are confirmed, which seems reasonably likely. What would this mean? Should we feel threatened, particularly because the treatment of chronic lower back pain is one of the mainstays of chiropractic practice? What additional information might help us sort through these unexpected developments regarding the role of infection?
One of the questions chiropractic researchers could helpfully explore is the extent to which CLBP with Modic Type 1 changes responds to chiropractic care. Currently, a PubMed search with the terms “Modic” and “chiropractic OR spinal manipulation” yields no references. For purposes of discussion, let’s imagine that future research shows that CLBP cases with Modic changes respond relatively poorly to manual or other complementary care approaches. If so, this could conceivably be included in revised clinical prediction rules and case-management algorithms. That is, if Modic cases are much more likely to have a poor response to chiropractic care (presumably because of a persistent, low-grade disc infection), wouldn’t it be helpful to know the odds in advance if possible, rather than routinely pursuing a course of care in cases where the outcome is likely to be disappointing?
Such information would also have to be shared with patients to comply with informed consent guidelines. An upside of such improved triage is that it would almost certainly result in a much higher rate of success for DCs treating chronic low-back pain cases, because those most likely to fail would be directed elsewhere while those most likely to succeed would, ideally, be referred for chiropractic care.
Considering the Downsides
There are, of course, considerable downsides to substantially increasing the use of MRI and long-term antibiotic therapy, the two linchpins of Albert’s approach. With MRI, the known problems are largely financial. In this cost-conscious era, the private- and public-sector economic impacts of a substantial increase in the utilization of MRI must be given due consideration.
But far more serious are the long-term consequences that could ensue from major increases in antibiotic usage. Since the widespread use of antibiotics in humans and animals has already raised the proliferation of antibiotic-resistant pathogenic organisms to dangerous levels, anything that would accelerate this dangerous trend must be viewed with a critical eye by guideline writers and health policy decision makers. The issue is complex. On an individual basis, the quality of life for a patient suffering from intractable CLBP might be greatly helped by successful long-term antibiotic therapy. On a population basis, it could be a disaster. Such are the conundrums of public health policy.
Contributing to the development of antibioticresistant bacteria and fungi is not the only negative effect to be anticipated from widespread use of long-term antibiotic therapy. In addition, allergic or hypersensitivity reactions may occur in some individuals, including gastrointestinal reactions such as diarrhea, nausea or vomiting and dermatological reactions such as rashes, pruritus or urticaria.
The increased costs for MRI and adverse effects of increased antibiotic use will be operative even if medical practitioners ordering imaging studies and prescribing antibiotics do so judiciously, according to evidence-based guidelines. But such an assumption flies in the face of past experience. If antibiotic treatment for Modic Type 1 CLBP were to become the norm in severe cases, it would come as no surprise if it soon became the norm in less severe cases. We should be prepared for this kind of “mission creep,” aided and abetted by profit-seeking pharmaceutical manufacturers; we’ve seen it many times before. It is not difficult to picture CLBP patients with borderline Modic 1 diagnoses, or even without any Modic-related diagnosis, demanding 100-day antibiotic prescriptions from their medical physicians. Nor is it difficult to foresee many of those physicians succumbing to such strongly expressed patient preferences. It is also not that hard to imagine a second 100-day course of antibiotic therapy if the first one fails. Throughout the health care system in the United States, guidelines are voluntary and compliance is sporadic.
For now, the chiropractic community would do well to take the Albert et al. study seriously and at least begin discussions as to its possible implications. As we strive to embody an evidence-based perspective, we must do no less.
Daniel Redwood, DC, is a professor at Cleveland Chiropractic College–Kansas City. He is the editor-in-chief of Health Insights Today, associate editor of Topics in Integrative Healthcare and a member of the editorial board of the Journal of the American Chiropractic Association. Dr. Redwood’s website and health policy blog are at www.redwoodhealthspeak.com
The author wishes to acknowledge the help of the following people who reviewed earlier drafts of this manuscript: Jan Hartvigsen, DC, PhD; Cheryl Hawk, DC, PhD; William Meeker, DC, MPH; Gary Longmuir, DC, DACBR; Ray Conley, DC, DACBR and Michael Whitehead, DC, DACBR.
REFERENCES:
Albert HB, Sorensen JS, Christensen BS, Manniche C.
Antibiotic treatment in patients with chronic low back pain and vertebral bone edema
(Modic type 1 changes): a doubleblind randomized clinical controlled trial of efficacy.
Eur Spine J. Apr 2013;22(4):697-707.Marshall BJ, Armstrong JA, McGechie DB, Glancy RJ.
Attempt to fulfil Koch’s postulates for pyloric Campylobacter.
Med J Aust. Apr 15 1985;142(8):436-439.Cassidy JD, Boyle E, Cote P, et al.
Risk of Vertebrobasilar Stroke and Chiropractic Care: Results of a Population-based
Case-control and Case-crossover Study
Spine (Phila Pa 1976) 2008 (Feb 15); 33 (4 Suppl): S176–183Albert HB, Lambert P, Rollason J, et al.
Does nuclear tissue infected with bacteria following disc herniations lead to Modic changes
in the adjacent vertebrae?
Eur Spine J. Apr 2013;22(4):690-696.Stirling A, Worthington T, Rafiq M, Lambert PA, Elliott TS.
Association between sciatica and Propionibacterium acnes.
Lancet. Jun 23 2001;357(9273):2024-2025.Modic MT, Masaryk TJ, Ross JS, Carter JR.
Imaging of degenerative disk disease.
Radiology. Jul 1988;168(1):177-186.Kjaer P, Korsholm L, Bendix T, Sorensen JS, Leboeuf-Yde C.
Modic changes and their associations with clinical findings.
Eur Spine J. Sep 2006;15(9):1312-1319.Jensen TS, Karppinen J, Sorensen JS, Niinimaki J, Leboeuf-Yde C.
Vertebral endplate signal changes (Modic change): a systematic literature review of
prevalence and association with nonspecific low back pain.
Eur Spine J. Nov 2008;17(11):1407-1422.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR.
Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging.
Radiology. Jan 1988;166(1 Pt 1):193-199.Wang Y, Videman T, Battie MC.
Modic changes: prevalence, distribution patterns, and association with age in white men.
Spine J. May 2012;12(5):411-416.Sample I.
Antibiotics could cure 40% of chronic back pain patients: Scientists hail medical breakthrough
by which half a million UK sufferers could avoid major surgery and take antibiotics instead.
The Guardian (UK). 2013. Accessed 6/15/13.Macrae F.
How back pain can be beaten with antibiotics: Breakthrough could cure 40% of sufferers.
Daily Mail. 2013.
www.dailymail.co.uk/health/article-2320738/How-painbeaten-antibiotics-Breakthrough-
cure-40-sufferers.html
Accessed 6/15/13.Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr., Shekelle P, Owens DK:
Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline
from the American College of Physicians and the American Pain Society
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 478–491Haas M, Goldberg B, Aickin M, Ganger B, Attwood M.
A Practice-Based Study of Patients With Acute and Chronic Low Back Pain
Attending Primary Care and Chiropractic Physicians: Two-Week to 48-Month Follow-up
J Manipulative Physiol Ther 2004 (Mar); 27 (3): 160–169
Return to LOW BACK PAIN
Since 9-06-2013


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |