

Evidence-informed Management of Chronic
Low Back Pain with the McKenzie MethodThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Spine J. 2008 (Jan); 8 (1): 134-141
OPEN ACCESS Stephen May, MSca, Ronald Donelson, MD, MS
Faculty of Health and Wellbeing,
Sheffield Hallam University,
Sheffield, United Kingdom.
s.may@shu.ac.uk
The management of chronic low back pain (CLBP) has proven to be very challenging in North America, as evidenced by its mounting socioeconomic burden. Choosing among available nonsurgical therapies can be overwhelming for many stakeholders, including patients, health providers, policy makers, and third-party payers. Although all parties share a common goal and wish to use limited health-care resources to support interventions most likely to result in clinically meaningful improvements, there is often uncertainty about the most appropriate intervention for a particular patient. To help understand and evaluate the various commonly used nonsurgical approaches to CLBP, the North American Spine Society has sponsored this special focus issue of The Spine Journal, titled Evidence-Informed Management of Chronic Low Back Pain Without Surgery. Articles in this special focus issue were contributed by leading spine practitioners and researchers, who were invited to summarize the best available evidence for a particular intervention and encouraged to make this information accessible to nonexperts. Each of the articles contains five sections (description, theory, evidence of efficacy, harms, and summary) with common subheadings to facilitate comparison across the 24 different interventions profiled in this special focus issue, blending narrative and systematic review methodology as deemed appropriate by the authors. It is hoped that articles in this special focus issue will be informative and aid in decision making for the many stakeholders evaluating nonsurgical interventions for CLBP.
There are more articles like this @ our: SPINAL ALLIGNMENT/CERVICAL CURVE Page Page
From the FULL TEXT Article:
Description
“Everything I know I learnt from my patients. I did not set out to develop a McKenzie method. It evolved spontaneously over time as a result of clinical observation”. [1]
Terminology
The McKenzie method is a unique and comprehensive approach to chronic low back pain (CLBP) that includes both an assessment and an intervention component. The assessment component of the McKenzie method attempts to determine a classification for CLBP to inform management, and is also commonly referred to as mechanical diagnosis and therapy (MDT). [2] A common objective of this assessment is to elicit a pattern of pain response called “centralization,” which refers to the sequential and lasting abolition of all distal referred symptoms and subsequent abolition of any remaining spinal pain in response to a single direction of repeated movements or sustained postures. The assessment may also uncover a “directional preference,” which refers to a particular direction of lumbosacral movement or sustained posture that cause symptoms to centralize, decrease, or even abolish while the individual’s limited range of spinal movement simultaneously returns to normal. [3]
It should be noted here that many clinicians use the intervention component of the McKenzie method in isolation (eg, repeated or sustained flexion/extension exercises) without the McKenzie method assessment. It is preferable in such instances to identify the intervention descriptively (eg, repeated prone extension) rather than referring to them as McKenzie exercises, which denotes a more comprehensive assessment and matched intervention approach. This point is very important in light of the frequency with which McKenzie method care has mistakenly been equated with that of extension exercises, certainly related to the fact that the subset in need of extension is so large. Fortunately, such misunderstanding is becoming less common as the assessment component of the McKenzie method is more widely recognized.
History
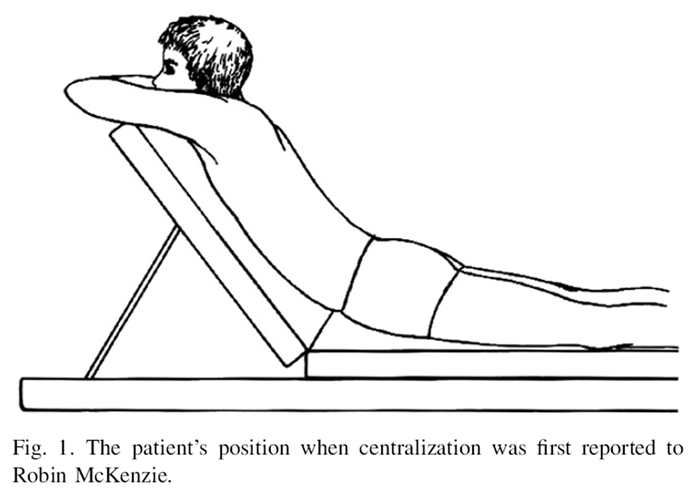
Figure 1 In a 1958 chance occurrence in a Wellington, New Zealand physiotherapy clinic, a patient with leg symptoms inadvertently lay prone in significant lumbar extension (Figure 1) for 10 minutes, after which he reported to the astounded clinician (McKenzie) that his leg had not felt this good for weeks. Impressed by the event, McKenzie began experimenting with the effect of sustained positions and repeated movements of the lumbar spine to end-range on spinal symptoms. During many years of experimentation, patterns of pain response to such positions and movements emerged, as did a system to classify many spinal pain problems. Based on his findings, McKenzie authored books for patients to manage their own pain; these books have been used worldwide for the past 25 years. Textbooks explaining the system for clinicians are also available. [4–6]
When addressing CLBP, most clinicians have their patients move only once into lumbar flexion and then once into lumbar extension. This often temporarily increases pain, leading the clinician to conclude that these movements are harmful. However, the diagnostic value of any single direction of movement frequently is not apparent unless repeated a number of times to end-range, after which this initially painful movement can become easier and less painful. More importantly, these beneficial changes can persist after the movements cease, leading to a treatment modality. Perhaps McKenzie’s greatest contribution to musculoskeletal medicine is his demonstrations of the great value in having patients perform repeated lumbar movements and sustained postures, both to end-range, while monitoring symptomatic and mechanical responses.
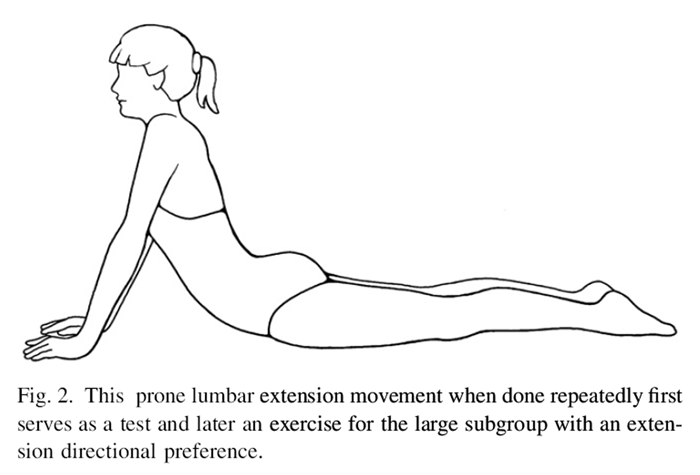
Figure 2 As long as each direction of lumbar movement is tested repetitively to end-range, McKenzie found that a single direction of testing would very commonly elicit these beneficial pain responses. Once such a directional preference is identified, treatment consists of having the patient frequently perform the single direction of end-range lumbar exercises that matches the patient’s directional preference. A common exercise for those with an extension directional preference is shown in Figure 2. Treatment also includes strict, temporary posture modifications to avoid loading the lumbar spine in the opposite direction for any length of time. The latter, when tested during the assessment, typically aggravates or reproduces the symptoms.
The overall objective of the McKenzie method is patient self-management that includes three important phases:1) demonstrating and educating patients about the beneficial effects of positions and end-range movements on their symptoms, and the aggravating effects of the opposite movements and postures;
2) educating patients in how to maintain the reduction and abolition of their symptoms; and
3) educating patients in how to restore full function to the lumbar spine without symptom recurrence.Research into the McKenzie method began in 1990 when the first diagnostic reliability study [7], randomized controlled trial (RCT) [8], and study of the concept of centralization [9] were published. Since then, the wealth of literature has expanded every year and now includes not only RCTs of the intervention components but also studies into the reliability and prognostic validity of the assessment components of the McKenzie method.
General description
The standardized McKenzie method assessment includes a medical history and physical examination in which responses to repeated lumbar movements are noted to enable the clinician to make a provisional classification of the patient’s condition. According to MDT, patients may be classified into one of three mechanical syndromes: derangement, dysfunction, or postural syndrome. The proportion of patients who could be classified has been generally high, with a mean of 87% across five studies. [1, 7, 10–12] For example, 83% of 607 patients were classified in one of the mechanical syndromes, with 78% classified as derangement. [13]
The derangement syndrome has the distinctive pain responses of centralization, which has been reported in 52% of 325 CLBP patients. [14] Directional preference was elicited in 74% of subjects in an RCT [15], of which 53% had symptoms duration greater than 7 weeks. The dysfunction syndrome is found only in patients with chronic symptoms, and is characterized by intermittent pain produced only at end-range in a single direction of restricted movement. Unlike derangement, there are no rapid changes in symptoms or range of motion as a result of performing repeated movements. Adherent nerve root is a particular type of dysfunction that typically follows an episode of radicular pain where the pain is now only elicited when the nerve root and its adhering scar tissue are placed on stretch. Postural syndrome is typically not seen in CLBP and is likewise intermittent, but pain is typically midline or symmetrical and produced only by sustained slouched sitting which is then abolished by posture correction (restoring the lumbar lordosis). This should be differentiated from very common postural “stresses,” where pain of other syndromes is aggravated and perpetuated by end-range postural or static loads. The minority of patients who do not demonstrate any of these responses over several sessions of MDT would be classified as “other.”
Management according to classification
Classification according to MDT is used to inform treatment. For derangement syndrome, the aim is to rapidly centralize and abolish all symptoms and restore all lumbar movement. For dysfunction syndrome, eliminating the symptoms requires treatment aimed at intentionally reproducing the symptoms at end-range as an indicator that the short, painful structure is being adequately stretched so it can heal, lengthen, and become pain-free over time. For postural syndrome, the pain is eliminated simply by improving posture to avoid prolonged tensile stress on normal structures. This is done through educating the patient in posture correction while (s)he experiences the beneficial effect on their pain.
Within each syndrome, MDT findings dictate further treatment considerations. For example, two patients might both be classified as derangement, but one centralizes and abolishes symptoms with extension exercises and the other with flexion exercises. Their treatment directions for their respective derangements are obviously opposite in terms of their exercises and posture strategies. It is important to note that there is no generic prescription of standardized McKenzie method exercises, which must be tailored to each patient. An important aspect of the McKenzie method is patient self-management. The clinician’s role is primarily as the assessor, classifier, and educator. With the clinician’s guidance and through each patient’s own experiential education, patients quickly and easily become empowered in how to first eliminate their own pain and then to become proactive with these same strategies to prevent its return.
The use of manual force
For a minority of patients, with CLBP, eliminating pain requires greater end-range force than they are able to generate themselves. In these cases, clinicians can provide manual pressure at end-range and even progress to spinal mobilization and manipulation in the patient’s direction of symptom preference. Brief and minimal forces are often all that is needed to gain the desired effect of centralization and pain elimination, after which most patients can selfmanage using end-range exercises under the clinicians’ guidance and education, with no further need for clinician- generated manual forces.
Practitioner, setting, and availability
The qualification of McKenzie method clinicians is structured, internationally standardized, and educationally validated. Four postgraduate courses and a credentialing exam complete basic training and for those who wish to pursue more advanced studies, a course, clinical mentorship, and examination are required to be recognized as a McKenzie Diplomat. In seeking competent McKenzie method clinicians for patient referral and research purposes, it is wise to first inquire about their educational credentials for assurance that the all-important assessment and classification process will be performed thoroughly and reliably. Typically, clinicians trained in the McKenzie method can be found in many in– and outpatient settings, departments in hospitals, and in private practice. The availability of certified McKenzie method practitioners can be verified with a web-based database for areas of the United States, Canada, and all other countries (www.mckenziemdt.org).
Reimbursement
Presently, there are no current procedural terminology (CPT) codes appropriate for care with the McKenzie method, especially for the performance of the extensive and highly informative assessment component. To be reimbursed at all, McKenzie method clinicians must use existing CPT codes for examination and manual or exercise therapy, and accept the same reimbursement paid for those CPT codes with far less extensive assessments.
Theory
Mechanism of action
Exercises are used to strengthen muscles, increase softtissue stability, restore range of movement, improve cardiovascular conditioning, increase proprioception, and reduce fear of movement as part of a cognitive behavioral or progressive exposure program. Most McKenzie method exercises are intended to directly and promptly diminish and eliminate patients’ symptoms [15] by providing beneficial and corrective mechanical directional end-range loads to the underlying pain generator. A discussion of the anatomic means by which these rapid pain changes might occur is beyond the scope of this article but is addressed at some length in an article by Wetzel and Donelson. [16]
Diagnostic testing required Because there are no specific contraindications or safety issues for the assessment component of the McKenzie method, no prior diagnostic testing is required before referral for this assessment. Of note, although this form of assessment does not identify the precise anatomic source of pain, such identification is fortunately only necessary when contemplating some invasive treatment (eg, surgery). Importantly, proper use of these assessment methods and the awareness of atypical and nonmechanical pain responses elicited with this form of testing quickly alerts the clinician to the possibility of serious pathology related to CLBP (eg, red flag). In such instances, prompt referral for further investigations is of course advised. [2]
Indications and contraindicationsCentralizers At least six studies have reported on the excellent prognosis for patients who were categorized as centralizers if treatment is directed by the patients’ directional preference. [9, 17–21] A systematic review similarly concludes that centralization, when elicited, predicts a high probability of a good treatment outcome, again as long as treatment is guided by the assessment findings. [14] These patients might be considered the most ideal patients to experience an excellent treatment response. Initial clues for potentially responsive patients emerge during the history taking and then are confirmed with the repeated end-range movement portion of the physical testing.
Recurrent low back pain Patients who report previous episodes of low back pain (LBP) that have resolved but keep recurring are routinely found to have a directional preference, are centralizers, and therefore also ideal treatment candidates. Furthermore, even if a patient has responded to some other form of treatment for past LBP but is frustrated with recurrences and in need of further treatment, they are often pleased with the ability to self-manage their pain with this intervention.
Mechanical low back pain Another indicator of patients who may be responsive to the McKenzie method are those whose symptoms are affected by changes in postures and activities (eg, pain made worse by sitting and bending, but better with walking or moving). Such a history is often indicative of a directional preference for extension, which can be confirmed during the repeated end-range testing of the physical examination. Such mechanical responsiveness to changes in posture and activity has been commonly reported. [8, 22–25]
Evidence of efficacy
Clinical guidelines

Table 1 Although the assessment component of the McKenzie method has been overlooked by most clinical guidelines (Denmark [26] is the exception), the intervention component has been mentioned in several clinical guidelines. It should be noted that most guidelines and systematic reviews incorrectly define the McKenzie method strictly as an intervention and often equate it with the performance of extension exercises without a preceding MDT assessment. Recommendations from guidelines are therefore deficient and flawed when related to the McKenzie method. As a treatment method for CLBP, the McKenzie method has been recommended by four guidelines (Table 1). [26–29]
Systematic reviews

Table 2 Two systematic reviews related to the McKenzie method have thus far been conducted (Table 2). [30, 31] Conclusions were similar and there was limited evidence relating to CLBP. Another systematic review examined the evidence regarding the effectiveness of physical therapy–directed exercise interventions after patients had been classified using symptom response methods. [32] This included mixed duration LBP (some chronic, but mostly subacute). Four out of five of the included studies related to the McKenzie method. All articles scored 6 or more by physiotherapy evidence database (PEDro) rating (suggesting high methodological quality), and four out of five found that a directed exercise program implemented according to patient response was significantly better than control or comparison groups. The authors noted a positive trend, but few studies have investigated this phenomenon.
Randomized controlled trials

Table 3

Table 4 Three RCTs are directly relevant to the treatment of CLBP using the McKenzie method. [15, 33, 34] Petersen et al. [33] compared care with the McKenzie method with strengthening exercises where 85% of subjects had symptoms more than 3 months. Miller et al. [34] compared care with the McKenzie method with stabilization exercises in CLBP (mean symptom duration of 26 months). Long et al. [15] had a mixed population, mostly subacute and chronic, with 53% having symptoms longer than 7 weeks. Results clearly favored the McKenzie method group at the short term in one study [15], showed a tendency to favor the McKenzie method group in another [33], or the two treatments were equal in the third (Table 3). [34] As described and discussed, the McKenzie method is a comprehensive system of assessment, classification, and management. Attempting to prove the efficacy of the intervention component alone is not reflective of practice [35]. Additional research has been conducted to examine evaluation, some of which is summarized in two key systematic reviews (Table 4). [14, 36]
Centralization studies
A systematic review concluded that centralization is not only a common clinical occurrence, but, with proper training, can be reliably detected and has important prognostic and management implications. [14] Its occurrence was consistently associated with good prognosis across six studies and it can be used to guide appropriate exercise or manual therapy prescription. The study concluded that centralization should be routinely monitored during spinal assessment and be used to guide treatment strategies.
Centralization and psychosocial factors
Two studies have demonstrated that centralization is a more important predictor of outcomes than fear-avoidance and work-related issues in terms of long-term pain, disability, and a range of other health-related outcomes. [21, 37] Conversely, failure to change the pain location during the baseline assessment (noncentralization) has been shown to be a strong predictor of a poor outcome and a predictor of a poor behavioral response to spine pain. [21]
When noncentralization was found, for example, the patient was 9 times more likely to have nonorganic signs, 13 times more likely to have overt pain behaviors, 3 times more likely to have fear of work, and 2 times more likely to have somatization. [38] Given these findings, in an effort to prevent the development of CLBP, the presence of noncentralization during a baseline McKenzie assessment in more acute LBP suggests that additional psychosocial screening may be useful.
Reliability studies
To have clinical utility, it is imperative that examination findings interpreted by different clinicians have high interexaminer reliability (eg, kappa values). Although several systematic reviews of reliability studies have been published recently, only one attempted to differentiate basic methods of physical examination. [36]
There would appear at first to be conflicting evidence regarding reliability of the McKenzie classification system from four studies, three of which are considered high quality. Two high-quality studies reported high reliability (kappa greater than 0.85) [1, 10] but the third reported low reliability (kappa 0.26). [11] However, clinicians involved in this latter study had little or no previous experience with the McKenzie method and errors could have resulted from this inexperience. In contrast, the first two used trained and experienced McKenzie method clinicians to classify and subclassify patients according to the MDT system, producing quite high kappa values of 0.7/0.96 [10], and 1.00/0.89. [1] A fourth study that also used trained McKenzie method clinicians likewise showed moderately high kappa values of 0.6/0.7. [3]
Ongoing studies
There are multiple planned and ongoing studies related to the McKenzie method, including subgroup determination in CLBP, RCTs of care with the McKenzie method in MDT subgroups versus placebo, comparative prognostic validity studies of centralization and clinical prediction rules, centralization and psychosocial factors, and anatomic studies to define the mechanism of pain centralization and directional preference.
Harms
There are no documented side effects or adverse events related to this intervention. It has been documented that failure to alter symptom distribution (noncentralization) is a strong predictor of negative outcomes [21] and poor behavioral responses to back pain. [38]
Summary
The McKenzie method has an important role to play in all patients with CLBP in terms of reliably classifying them into distinct, validated subgroups with distinctly different treatment needs. The reliability and prognostic validity of the assessment findings are well documented across multiple studies, along with more recent subgroup-specific RCTs showing the efficacy of classifying patients in this way. Subgroup classification of back pain and subgroup-specific management strategies appear to be a highly successful and objective way to improve the care of patients with CLBP, compared with the nonspecific, one-size-fits-all recommendations of most international guidelines to date.
The McKenzie method is first and most importantly a system of assessment and classification from which patient- specific treatments emerge. As described above, elements of the MDT classification system have consistently demonstrated substantially more reliability than any other alternative examination procedures. [36]
In addition, multiple studies have consistently identified the positive prognostic value of centralization [14] and reported that noncentralization is associated with a poor behavioral response. [21, 38] Intervention studies to date have demonstrated that the McKenzie method produces better short-term outcomes than nonspecific guidelinebased care [15] and equal or marginally better outcomes than stabilization or strengthening exercises for patients with CLBP. [33, 34]
This evidence indicates that the McKenzie method in the hands of an experienced clinician is a very powerful tool to determine the large subset of patients with CLBP who will respond in a straightforward manner using self-treatment methods, and conversely, the smaller group who will not respond and therefore are in need of either further investigations or a more involved psychosocial intervention.
Ideally, future RCTs need to shift away from studying patients with so-called nonspecific CLBP [35] by identifying subgroups of patients most likely to respond to the approach, and validating such predictions with prospective studies.
It is commonly stated that psychosocial issues dominate the evolution from acute LBP to CLBP and several recent studies have sought to test this theory, but many have failed to demonstrate clear superiority of a cognitive behavioral approach to exercise, manual therapy, or usual GP care. [39–43] Furthermore, there is no evidence that evaluating, subclassifying, or treating psychosocial factors in any way improves outcomes with CLBP. [43, 44] In fact, successfully addressing pain has been shown to resolve most accompanying psychosocial issues [21], even with the use of physical treatment. [15, 41]
More effort needs to be made in determining which subgroup of patients with CLBP actually needs a nonspecific psychosocial approach. The finding of noncentralization has been reported as a strong predictor of poor prognosis. This evidence suggests that the dominant role that many assign to the psychosocial element in CLBP has not been entirely appropriate. Further research to assist in dealing with this chronic subgroup should include the comparative prognostic validity of these different clinical findings, the degree to which psychosocial features are relevant to treatment decisions, and identifying reliable methods of evaluating and classifying subgroups in which these features may be dominant.
References:
Clare HA, Adams R, Maher CG. Reliability of McKenzie classification of patients with cervical or lumbar pain. J Manipulative Physiol Ther 2005;28:122–7.
McKenzie R, May S. The lumbar spine: mechanical diagnosis and therapy. 2nd ed. Waikanae, NZ: Spinal Publications New Zealand Ltd., 2003.
Kilpikoski S, Airaksinen O, Kankaanpaa M, Leminen P, Videman T, Alen M. Interexaminer reliability of low back pain assessment using the McKenzie method. Spine 2002;27:E207–14.
McKenzie RA. The lumbar spine: mechanical diagnosis and therapy. Waikanae, NZ: Spinal Publications New Zealand Ltd., 1981. [Ref Type: Generic].
McKenzie R, May S. The human extremities: mechanical diagnosis and therapy. Waikanae, NZ: Spinal Publications New Zealand Ltd., 2000.
McKenzie RA. The cervical and thoracic spine: mechanical diagnosis and therapy. Waikanae, NZ: Spinal Publications New Zealand Ltd., 1990.
Kilby J, Stigant M, Roberts A. The reliability of back pain assessment by physiotherapists, using a ‘McKenzie algorithm’. Physiotherapy 1990;76:579–83.
Stankovic R, Johnell O. Conservative treatment of acute low-back pain. A prospective randomized trial: McKenzie method of treatment versus patient education in “mini back school”. Spine 1990;15:120–3.
Donelson R, Silva G, Murphy K. Centralization phenomenon. Its usefulness in evaluating and treating referred pain. Spine 1990;15:211–3.
Razmjou H, Kramer JF, Yamada R. Intertester reliability of the McKenzie evaluation in assessing patients with mechanical low-back pain. J Orthop Sports Phys Ther 2000;30:368–83.
Riddle DL, Rothstein JM. Intertester reliability of McKenzie’s classifications of the syndrome types present in patients with low back pain. Spine 1993;18:1333–44.
Clare HA. Evaluation of the McKenzie method. Australia: University of Sydney, 2005.
May S. Classification by McKenzie mechanical syndromes: a survey of McKenzie-trained faculty. J Manipulative Physiol Ther 2006;29: 637–42.
Aina A, May S, Clare H. The centralization phenomenon of spinal symptomsda systematic review. Man Ther 2004;9:134–43.
Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine 2004;29: 2593–602.
Wetzel FT, Donelson R. The role of repeated end-range/pain response assessment in the management of symptomatic lumbar discs. Spine J 2003;3:146–54.
Long AL. The centralization phenomenon. Its usefulness as a predictor or outcome in conservative treatment of chronic law back pain (a pilot study). Spine 1995;20:2513–20.
Karas R, McIntosh G, Hall H, Wilson L, Melles T. The relationship between nonorganic signs and centralization of symptoms in the prediction of return to work for patients with low back pain. Phys Ther 1997;77:354–60.
Sufka A, Hauger B, Trenary M, et al. Centralization of low back pain and perceived functional outcome. J Orthop Sports Phys Ther 1998;27:205–12.
Werneke M, Hart DL, Cook D. A descriptive study of the centralization phenomenon. A prospective analysis. Spine 1999;24:676–83.
Werneke M, Hart DL. Centralization phenomenon as a prognostic factor for chronic low back pain and disability. Spine 2001;26:758–64.
BoissonnaultW, Fabio RP. Pain profile of patients with low back pain referred to physical therapy. J Orthop Sports Phys Ther 1996;24: 180–91.
Pengel LH, Refshauge KM, Maher CG. Responsiveness of pain, disability, and physical impairment outcomes in patients with low back pain. Spine 2004;29:879–83.
van Deursen LL, Patijn J, Durinck JR, Brouwer R, van Erven- Sommers JR, Vortman BJ. Sitting and low back pain: the positive effect of rotary dynamic stimuli during prolonged sitting. Eur Spine J 1999;8:187–93.
Van Deursen L, Snijders C, Patijn J. Influence of daily life activities on pain in patients with low back pain. J Orthopaedic Med 2002;24: 74–6.
Statens institut for medicinsk teknologivurdering. Low-back pain: frequency, management, and prevention from an HTA perspective. Denmark: Danish Institute for Health Technology Assessment, 1999.
Albright J, Allman R, Bonfiglio R, Conill A, Dobkin B, Guccione AA, et al. Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for low back pain. Phys Ther 2001;81:1641–74.
Rossignol M, Arsenault B. Clinique des Lombalgies Interdisciplinaire en Premiere Ligne. Guide de pratique. Montreal, Quebec, Canada: Reseau provincial de recherche en adaptation et en readaptation du Quebec (REPAR/FRSQ), 2006.
Mercer C, Jackson A, Hettinga D, Barlos P, Ferguson S, Greenhalgh S. Clinical guidelines for the physiotherapy management of persistent low back pain, Part 1: Exercise. London: Charted Society of Physiotherapy, 2006.
Clare HA, Adams R, Maher CG. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother 2004;50: 209–16.
Machado LA, de Souza MS, Ferreira PH, Ferreira ML. The McKenzie method for low back pain: a systematic review of the literature with a meta-analysis approach. Spine 2006;31:E254–62.
Cook C, Hegedus EJ, Ramey K. Physical therapy exercise intervention based on classification using the patent response method: a systematic review of the literature. J Manipulative Physiol Ther 2005;13: 152–62.
Petersen T, Kryger P, Ekdahl C, Olsen S, Jacobsen S. The effect of McKenzie therapy as compared with that of intensive strengthening training for the treatment of patients with subacute or chronic low back pain: a randomized controlled trial. Spine 2002;27:1702–9.
Miller ER, Schenk RJ, Karnes JL, Rouselle JG. A comparison of the McKenzie approach to a specific spine stabilization program for chronic low back pain. J Manipulative Physiol Ther 2005;13:103–12.
Spratt KF. Statistical relevance. In: Fardon DF, ed. Orthopaedic knowledge update spine. 2nd ed. Rosemont, IL: The American Academy of Orthopaedic Surgeons, 2002:497–505.
May S, Littlewood C, Bishop A. Reliability of procedures used in the physical examination of non-specific low back pain: a systematic review. Aust J Physiother 2006;52:91–102.
George SZ, Bialosky JE, Donald DA. The centralization phenomenon and fear-avoidance beliefs as prognostic factors for acute low back pain: a preliminary investigation involving patients classified for specific exercise. J Orthop Sports Phys Ther 2005;35:580–8.
Werneke MW, Hart DL. Centralization: association between repeated end-range pain responses and behavioral signs in patients with acute non-specific low back pain. J Rehabil Med 2005;37:286–90.
Hay EM, Mullis R, Lewis M, et al. Comparison of physical treatments versus a brief pain-management programme for back pain in primary care: a randomised clinical trial in physiotherapy practice. Lancet 2005;365:2024–30.
Kaapa EH, Frantsi K, Sarna S, Malmivaara A. Multidisciplinary group rehabilitation versus individual physiotherapy for chronic nonspecific low back pain: a randomized trial. Spine 2006;31:371–6.
Storheim K, Brox JI, Holm I, Koller AK, Bo K. Intensive group training versus cognitive intervention in sub-acute low back pain: shortterm results of a single-blind randomized controlled trial. J Rehabil Med 2003;35:132–40.
Smeets R, Vlaeyen J, Hidding A, et al. Active rehabilitation for chronic low back pain: cognitive-behavioral, physical, or both? First direct post-treatment results from a randomized controlled trial [ISRCTN22714229]. BMC Musculoskelet Disord 2006;7:5.
Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ 2006;332:1430–4.
Jellema P, van der Windt DA, van der Horst HE, Twisk JW, Stalman WA, Bouter LM. Should treatment of (sub)acute low back pain be aimed at psychosocial prognostic factors? Cluster randomised clinical trial in general practice. BMJ 2005;331:84.

Return to McKENZIE METHOD
Since 12-28-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |