

Overcoming Overuse Part 5:
Is Shared Decision Making Our Excalibur?This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Orthop Sports Phys Ther 2021 (Feb); 51 (2): 53-56 ~ FULL TEXT
Simon Décary, Joshua R Zadro, Mary O'Keeffe, Zoe A Michaleff, Adrian C Traeger, France Légaré
Tier 1 Canada Research Chair in Shared Decision Making
and Knowledge Translation,
Université Laval,
Quebec, Canada.
Shared decision making is recommended as a strategy to help patients identify what matters most to them and make informed decisions about musculoskeletal care. In part 5 of the Overcoming Overuse series, we look at the evidence supporting shared decision making as a strategy to help curb overuse. Using shared decision making in clinical consultations may help to reduce the overuse of options that are not beneficial and to increase use of care supported by evidence. Shared decision making could support clinicians in promoting uptake of active rehabilitation options with a favorable balance of benefits to harms. Shared decision making facilitates conversations about unnecessary tests or treatments and could be a key strategy for overcoming overuse.
Keywords: musculoskeletal; patient experience; preferences; value-based care; values.
From the FULL TEXT Article:
Backgroumd
Shared decision making (SDM) involves clinicians and patients collaborating on health care decisions after considering the best available evidence and patients’ values and preferences. [16] Shared decision making is increasingly promoted as a strategy to reduce overuse in health care, including in guidelines for musculoskeletal pain (eg, American Pain Society). [2, 12]
In the previous editorials, shared decision making offers a potential solution to “misaligned care” [13] and the beliefs and knowledge imbalances that drive supplier-induced demand. [14, 18] Excalibur was the legendary sword of King Arthur from the legends of fifth-century Britain that many believed to have magical properties and contributed greatly to victories in battle at the time. We believe that SDM could be our Excalibur in the fight against overuse if clinicians commit to learning how to wield it.
Shared Decision Making to Reduce Overuse in Health Care
The idea that SDM could reduce overuse gained traction after a Cochrane review on the effectiveness of patient decision aids—tools that help facilitate SDM in clinical consultations. [16] Using decision aids can reduce the use of some elective surgeries, [19] prevent unnecessary screening tests for prostate cancer, [16] and reduce antibiotic use for acute respiratory tract infections. [11] Decision aids may help increase uptake of options that are beneficial, such as diabetes medication. [16]
Evidence on the use of SDM for reducing invasive musculoskeletal care options is less certain. A comparative effectiveness trial of 2 decision aids for hip/knee osteoarthritis led to informed patientcentered decisions without reducing surgery rates. [15] A systematic review of decision aids for chronic musculoskeletal pain found that using these tools could improve knowledge and help to resolve decisional uncertainty, but 7 of 8 trials found no benefit of reducing the use of surgery for osteoarthritis. [3]
The impact of SDM on other aspects of musculoskeletal health care remains uncharted territory. Patients with musculoskeletal conditions face decisions concerning a plethora of low-value medical (eg, opioids, injections, imaging) and nonmedical options (eg, electrotherapy). Knowing whether SDM can reduce the use of some of these options starts by understanding the expected outcomes of SDM.
Shared Decision Making Outcomes Are Key to Understanding Overuse
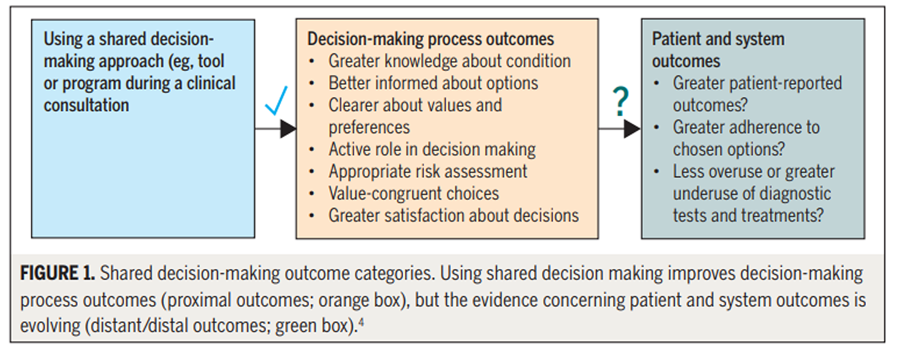
Figure Current theories about SDM outcomes can help us understand how SDM could impact overuse. Elwyn et al [4] categorized SDM outcomes as proximal, distal, or distant. Proximal outcomes are what happens as a direct result of using SDM (eg, increased knowledge of options, informed decisions) (FIGURE 1). Distal outcomes are what happens after a consultation (eg, alignment of treatment choice with preferred options). Distant outcomes are what happens in the longer term, after a treatment strategy has been decided (eg, utilization rates or health outcomes). Shared decision making has a ing distal and distant impacts of SDM continues to evolve.

Table The musculoskeletal community now has access to the Outcome Measures in Rheumatology (OMERACT) SDM core outcome domains17 (summarized in the TABLE), codesigned by patients, clinicians, and researchers. Knowledge and confidence in the chosen options are proximal outcomes, while alignment and satisfaction with the decision-making process are distal outcomes. The fifth domain, “adherence to the chosen option,” is a distant outcome measured after a consultation. Adherence to musculoskeletal rehabilitation is required to improve pain and function that may guard patients against overused options such as opioids or surgery.
Implementing Shared Decision Making in Musculoskeletal Rehabilitation
It is tempting to apply the findings from SDM studies of antibiotic use to other prescription medications for musculoskeletal pain. In the former, patients are typically faced with 2 options: take the antibiotic immediately or the wait-andsee approach, an acceptable option with few harms. When prescribing medications for acute and debilitating musculoskeletal pain, patients may be reluctant to accept treatment options that provide delayed symptom relief, such as exercise. [1] Using SDM for musculoskeletal conditions often requires a collaborative interdisciplinary approach between physicians, physical therapists, and patients.
A challenge to implementing SDM in musculoskeletal rehabilitation is that patients have diverse symptom severities, causes, and durations. Patients may have acute pain due to trauma or chronic pain that has flared up. The wait-and-see approach may be an acceptable option for conditions that often resolve naturally with advice and reassurance (eg, ankle sprain). For patients with chronic pain, tapering strong pain medicines (eg, opioids) may increase flare-ups, making it difficult to encourage a wait-and-see approach.
Decision aids for musculoskeletal pain also need to integrate and balance medication and rehabilitation options by specifically reporting on the benefits and harms, and levels of supporting evidence for each treatment option. [19] Providing many options increases the complexity of the decision and risks creating greater decision uncertainty for patients. Newer decision aids that use an online adaptive format that is based on patient phenotypes will help resolve this issue.
Not all patient decision aids are of high quality. Patient educational material is often mislabeled as a decision aid and fails to engage patients in SDM. In contrast, option grids present balanced information on benefits and harms and encourage active engagement of patients in the decision-making process. [6, 10]
Clinicians may need training in SDM to increase confidence and prevent potentially negative consequences. [9] Some clinicians may worry that discussing pain medication will threaten the clinicianpatient relationship. Patients may feel they are being stereotyped for preferring medication over sometimes costly and difficult-to-access rehabilitation. Communication skills are vital for navigating uncertainties concerning musculoskeletal rehabilitation. Clinicians need training to effectively use decision aids. [9]
Musculoskeletal rehabilitation clinicians, including physical therapists, have a central role to play in implementing SDM for musculoskeletal conditions. They have more time with patients, have regular follow-up during rehabilitation, and understand the benefits and harms of a range of treatment options. Clinicians can help patients reach better and informed decisions about musculoskeletal care. [5] While high-quality tools are being designed, clinicians can experiment with the SDM process in their clinical practice by using OMERACT’s 6-step process (FIGURE 2; also see https://www.youtube.com/watch?v=4OxXIXMfJAo).
Conclusion
Shared decision making enhances patient-clinician communication, improves patient knowledge about benefits and harms of care options, resolves uncertainies, and helps patients make decisions that best align with their values and preferences. In an era of misinformation, SDM could help patients and clinicians to more accurately compare the benefits and harms of musculoskeletal tests and treatments. [7, 8] Shared decision making represents a bright future where patients and clinicians truly collaborate and openly discuss high- and low-value care, helping patients to avoid overused options. The SDM sword has been drawn from the rock; now is the time to learn how to wield its power.
References:
Bishop MD, Mintken PE, Bialosky JE, Cleland JA.
Patient expectations of benefit from interventions for
neck pain and resulting influence on outcomes.
J Orthop Sports Phys Ther. 2013;43:457-465.
https://doi.org/10.2519/jospt.2013.4492Born KB, Coulter A, Han A, et al.
Engaging patients and the public in Choosing Wisely.
BMJ Qual Saf. 2017;26:687-691.
https://doi.org/10.1136/bmjqs-2017-006595Bowen E, Nayfe R, Milburn N, et al.
Do decision aids benefit patients with chronic
musculoskeletal pain? A systematic review.
Pain Med. 2020;21:951-969.
https://doi.org/10.1093/pm/pnz280Elwyn G, Frosch DL, Kobrin S.
Implementing shared decision-making:
consider all the consequences.
Implement Sci. 2016;11:114.
https://doi.org/10.1186/s13012-016-0480-9Elwyn G, Pickles T, Edwards A, et al.
Supporting shared decision making using an Option Grid for
osteoarthritis of the knee in an interface musculoskeletal clinic:
a stepped wedge trial.
Patient Educ Couns. 2016;99:571-577.
https://doi.org/10.1016/j.pec.2015.10.011Grande SW, Faber MJ, Durand MA, Thompson R, Elwyn G.
A classification model of patient engagement methods and
assessment of their feasibility in real-world settings.
Patient Educ Couns. 2014;95:281-287.
https://doi.org/10.1016/j.pec.2014.01.016Hoffmann TC, Del Mar C.
Clinicians’ expectations of the benefits and harms of
treatments, screening, and tests: a systematic review.
JAMA Intern Med. 2017;177:407-419.
https://doi.org/10.1001/jamainternmed.2016.8254Hoffmann TC, Del Mar C.
Patients’ expectations of the benefits and harms of treatments,
screening, and tests: a systematic review.
JAMA Intern Med. 2015;175:274-286.
https://doi.org/10.1001/jamainternmed.2014.6016Légaré F, Adekpedjou R, Stacey D, et al.
Interventions for increasing the use of shared decision making
by healthcare professionals.
Cochrane Database Syst Rev. 2018;7:CD006732.
https://doi.org/10.1002/14651858.CD006732.pub4Légaré F, Hébert J, Goh L, et al.
Do Choosing Wisely tools meet criteria for patient decision aids?
A descriptive analysis of patient materials.
BMJ Open. 2016;6:e011918.
https://doi.org/10.1136/bmjopen-2016-011918Légaré F, Labrecque M, Cauchon M, Castel J, Turcotte S, Grimshaw J.
Training family physicians in shared decision-making to reduce the overuse
of antibiotics in acute respiratory infections: a cluster randomized trial.
CMAJ. 2012;184:E726-E734.
https://doi.org/10.1503/cmaj.120568Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al.
What Does Best Practice Care for Musculoskeletal Pain Look Like?
Eleven Consistent Recommendations From High-quality
Clinical Practice Guidelines: Systematic Review
British J Sports Medicine 2020 (Jan); 54 (2): 79–86Michaleff ZA, Zadro JR, Traeger AC, O’Keeffe M, Décary S.
Overcoming Overuse Part 2: Defining and Quantifying
Health Care Overuse for Musculoskeletal Conditions
J Orthop Sports Phys Ther 2020 (Nov); 50 (11): 588-591O’Keeffe M, Traeger AC, Michaleff ZA, Décary S, Garcia AN, Zadro JR.
Overcoming Overuse Part 3: Mapping the Drivers
of Overuse in Musculoskeletal Health Care
J Orthop Sports Phys Ther 2020 (Dec); 50 (12): 657-660Sepucha K, Bedair H, Yu L, et al.
Decision support strategies for hip and knee osteoarthritis:
less is more: a randomized comparative effectiveness trial (DECIDE-OA Study).
J Bone Joint Surg Am. 2019;101:1645-1653.
https://doi.org/10.2106/JBJS.19.00004Stacey D, Légaré F, Lewis K, et al.
Decision aids for people facing health treatment or screening decisions.
Cochrane Database Syst Rev. 2017;4:CD001431.
https://doi.org/10.1002/14651858.CD001431.pub5Toupin-April K, Barton JL, Fraenkel L, et al.
OMERACT development of a core domain set of outcomes
for shared decision-making interventions.
J Rheumatol. 2019;46:1409-1414. https://doi.org/10.3899/jrheum.181071O’Keeffe M, Traeger AC, Michaleff ZA, Décary S, Garcia AN, Zadro JR.
Overcoming Overuse Part 4: Small Business Survival
J Orthop Sports Phys Ther 2021 (Jan); 51 (1): 1–4Zadro JR, Traeger AC, Décary S, O’Keeffe M.
Problem with patient decision aids.
BMJ Evid Based Med. In press.
https://doi.org/10.1136/bmjebm-2020-111371
Return to NON-PHARMACOLOGIC THERAPY
Since 3-15-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |