ABC of complementary medicine
The Manipulative Therapies:
Osteopathy and ChiropracticThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: British Medical Journal 1999 (Oct 30); 319 (7218): 1176-1179 ~ FULL TEXT
Andrew Vickers and Catherine Zollman

Osteopathy and chiropractic share a common origin. Their roots can be found in folk traditions of “bone setting,” and both were systematised in the late 19th century in the United States: Daniel D Palmer, the founder of chiropractic, is said to have met with Andrew Taylor Still, the founder of osteopathy, before setting up his own school. The therapies remain relatively similar, and many textbooks and journals are relevant to both. The term “manipulative therapy” refers to both osteopathy and chiropractic.
From the FULL TEXT Article:
Background
Osteopathy and chiropractic are therapies of the musculoskeletal system: practitioners work with bones, muscles, and connective tissue, using their hands to diagnose and treat abnormalities of structure and function.
The best known technique is the “high velocity thrust,” a short, sharp motion usually applied to the spine. This maneuver is designed to release structures with a restricted range of movement. High velocity thrusts often produce the sound of joint “cracking,” which is associated with manipulative therapy. There are various methods of delivering a high velocity thrust. Chiropractors are more likely to push on vertebrae with their hands, whereas osteopaths tend use the limbs to make levered thrusts. That said, osteopathic and chiropractic techniques are converging, and much of their therapeutic repertoire is shared.
Practitioners also use a range of soft tissue techniques that do not involve high velocity thrusts. For example, the “muscle energy techniques” (known as “proprioceptive neuromuscular facilitation” by physiotherapists) make use of post-isometric relaxation to increase restricted ranges of movement.
Osteopaths and chiropractors may also use what are termed “functional techniques,” such as treating hip pain by applying a gentle, prolonged pull to the leg while slowly rotating it in the hip joint. If a restriction is detected, however slight, the leg is held at the point of restriction until a release of muscle tension occurs. Techniques like these are based on an understanding of subtle neuromuscular behaviour, which conforms to mainstream theory. In practice, they also rely on finely developed palpatory skills.
Some osteopaths also practise a technique known as cranial osteopathy or craniosacral therapy. Practitioners place their hands on the cranium and sacrum and gently handle the bones of the skull. They say that, by feeling for and working with subtle rhythmic pulsations of the cerebrospinal fluid, they can correct disturbances in the neuromuscular system. There are some therapists, usually known as craniosacral therapists, who use similar techniques but who do not have an osteopathic background.
A relatively recent branch of chiropractic, the McTimoney school, has developed some of its own manipulative techniques that do not place as great an emphasis on high velocity thrusts as do osteopathy and mainstream chiropractic.
With the exception of cranial osteopathy, many of the treatment methods used by osteopaths and chiropractors are similar to techniques used by those physiotherapists with additional training in manipulative therapy. From a general practitioner's perspective, there are few important practical differences between the three types of practitioner.
What happens during a treatment?
Manipulative therapists take a history, palpate for significant changes in muscle tension and skin circulation, and look for any restricted movements in order to diagnose musculoskeletal abnormalities and “neuromuscular dysfunction” (such as “trigger points” or signs of “pain-spasm cycles”). Chiropractors may use x rays to assist diagnosis, whereas osteopaths do so largely only for the purposes of excluding serious pathology.
A typical treatment session lasts 15-30 minutes, although first consultations may take longer. A variety of the techniques described above will be used. Not more than four high velocity thrusts are usually given in a single treatment session. A course of chiropractic treatment for back pain might consist of six sessions, initially frequent and then at weekly intervals. Osteopaths are more likely than chiropractors to treat on an “as needed” basis.
Therapeutic scope
Both osteopathy and chiropractic were originally regarded as complete systems of medicine. For example, Andrew Taylor Still treated infectious diseases and blindness among a range of conditions. Interestingly, the treatment of back problems features only rarely in his writings. Similarly, early chiropractors believed that most diseases could be attributed to misalignments of the spine and were therefore amenable to treatment with chiropractic.
Contemporary practitioners have moved away from this position and concentrate primarily on musculoskeletal disorders. Low back pain is the most common presenting complaint. Guidelines from the Royal College of General Practitioners recommend physical therapy (any of the manipulative techniques) within six weeks of the start of persisting uncomplicated back pain.
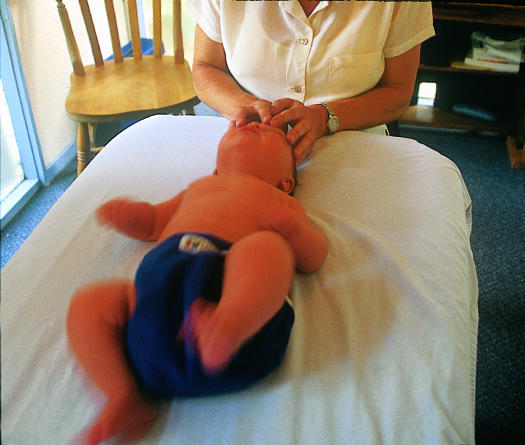
Other conditions often seen include neck and shoulder pain, sports injuries, repetitive strain disorders, and headache. Practitioners also treat various conditions such as arthritis; although they cannot affect disease pathology or progression, they claim to be able to treat secondary symptoms such as pain from associated muscle spasm. Cranial osteopathy has a particular reputation for treating children with conditions such as infantile colic, constant crying, and behavioural problems.
Research evidence
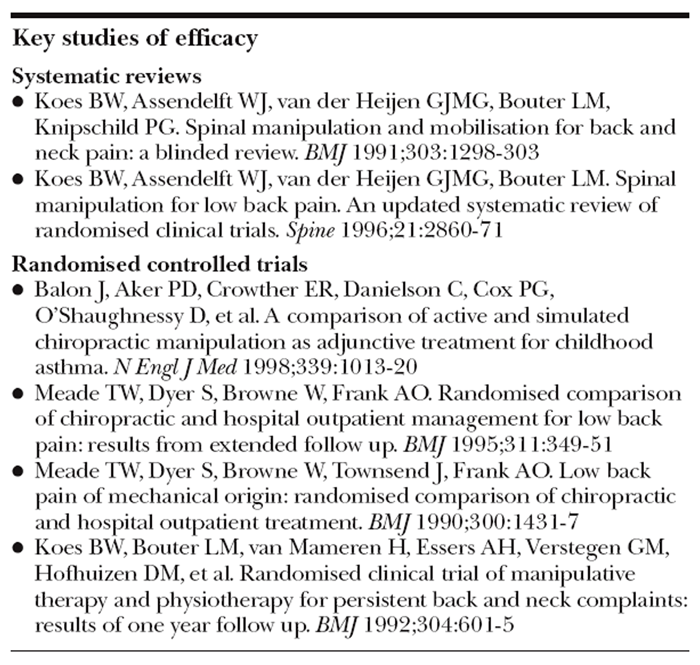
Key Studies of efficacyThere is considerable evidence from randomised controlled trials of the effectiveness of spinal manipulation for back and neck pain. Although this evidence is largely positive, it has been criticised for failing to exclude non-specific effects of treatment.
In the best known UK trial 741 patients with low back pain were randomised to chiropractic or hospital outpatient care. In both groups the treating practitioners were free to treat patients as they saw fit. The authors concluded that “chiropractic almost certainly confers worthwhile, long term benefit.” However, a recent systematic review of this and similar trials highlights methodological weaknesses, such as the fact that commonly used outcome measures such as pain and disability scores are assessed by patients and therefore unblinded.
In one trial that did involve blinded assessment of outcome, patients with back or neck pain were randomised to routine general practitioner care, placebo (deactivated heat treatment), physiotherapy, or manipulation. Physiotherapy and manipulation were superior to placebo and general practitioner care after six weeks, and manipulation was superior to physiotherapy at one year follow up.
In addition to effects on back and neck pain, randomised trials have also indicated that manipulative treatment is beneficial for headache, including migraine. However, the number of studies is small, so further work to confirm these results is needed. There is little or no reliable evidence of beneficial effects for many of the other musculoskeletal conditions that are commonly treated.
Apart from dysmenorrhoea, for which a small number of trials have shown a positive effect, current evidence suggests that manipulative therapy is not of benefit for problems related to smooth muscles or viscera, such as asthma and hypertension.
There has been little research on cranial osteopathy or McTimoney chiropractic.
Safety of osteopathy and chiropractic
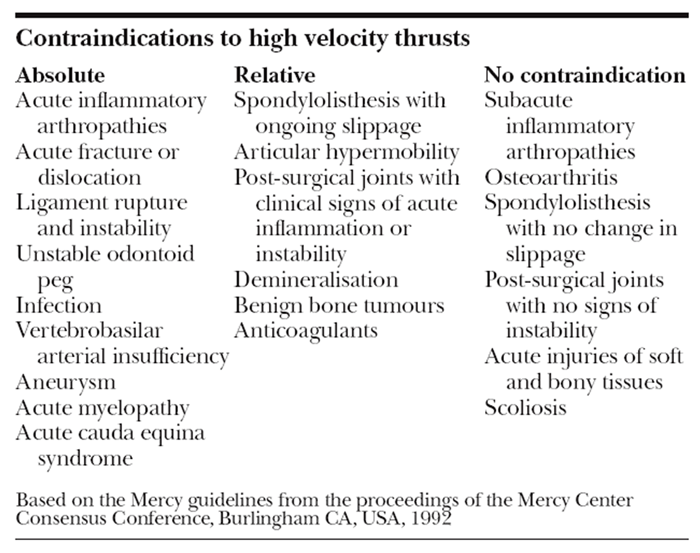
ContraindicationsThe most important potential adverse effects of osteopathy and chiropractic are stroke and spinal cord injury after cervical manipulation. Estimates of such severe adverse events vary widely, ranging from 1 in 20?000 patients undergoing cervical manipulation to 1 per million procedures. In recent years the osteopathic and chiropractic professions have shown greater appreciation of the risks of cervical manipulation, and it is possible that improved practice is leading to a reduction in the rate of severe complications.
More common adverse effects (25-50% of all patients) are mild pain or discomfort at the site of manipulation, slight headache, and fatigue; 75% or more of such complaints resolve within 24 hours. Contraindications to various manipulative techniques have been developed by the appropriate professional bodies, and practitioners are trained to screen patients and assess individual risk factors. Even when some techniques, such as high velocity thrusts, are contraindicated, other manipulative treatments may be safe.
Practitioners
Osteopathy and chiropractic are almost exclusively based in the community and in the private sector. Many practitioners work alone, often from converted rooms in their own homes. Others work in group clinics, in multidisciplinary practices, or in general practices. Some independent manipulative practitioners have established contracts with health authorities, fundholding practices, or primary care groups. Most private health insurance schemes now offer some cover for manipulative treatment.
Regulation
Osteopathy and chiropractic are the only two complementary therapies that are regulated by statute. Two acts of parliament passed in the mid-1990s established a General Osteopathic Council and a General Chiropractic Council with the aim of regulating the professions by the millennium. These organisations operate in a similar way to the General Medical Council and have the authority to remove practitioners from the register in disciplinary hearings.
Training
Most osteopaths take a four year, full time course leading to a BSc degree (BOst). Chiropractors undertake a four to five year, full time training, which includes a BSc in human sciences and chiropractic and a year of postgraduate training in an approved practice, leading to a diploma in chiropractic (DC). McTimoney and McTimoney Corley practitioners complete a four year, part time course. Biological and clinical sciences form a substantial component of all these training courses. Sometimes chiropractors are referred to as “doctors of chiropractic.” This is purely a courtesy title and has been used since chiropractic began. Several organisations run training courses in manipulative techniques specifically for conventional healthcare practitioners. The Manipulative Association of Chartered Physiotherapists runs and accredits postgraduate training in manipulation for physiotherapists. The British Institute of Musculoskeletal Medicine runs courses for medically qualified practitioners but is not a regulatory body. The London College of Osteopathic Medicine organises a one year, full time osteopathic training course for registered medical practitioners.
Acknowledgments
The pictures of manipulative techniques and of cranial osteopathy are reproduced with permission of BMJ/Ulrike Preuss. The picture of a physiotherapist is reproduced with permission of Science Photo Library.
Footnotes
The ABC of complementary medicine is edited and written by Catherine Zollman and Andrew Vickers. Catherine Zollman is a general practitioner in Bristol, and Andrew Vickers will shortly take up a post at Memorial Sloan-Kettering Cancer Center, New York. At the time of writing, both worked for the Research Council for Complementary Medicine, London. The series will be published as a book in Spring 2000.
Return to BMJs ABC'S OF CAM
Since 4-23-2003


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |