

A Revised Definition of Manipulation This section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2005 (Jan); 28 (1): 68–72 ~ FULL TEXT
OPEN ACCESS Howard Vernon, DC, PhD, John Mrozek, DC
We write this commentary to address a problem that we feel exists in the description of chiropractic theory regarding the definition of spinal manipulation. We will first outline the background of the problem and then state the problem as it exists currently. We will then propose a revised definition to more accurately describe spinal manipulation.
From the FULL TEXT Article:
Background
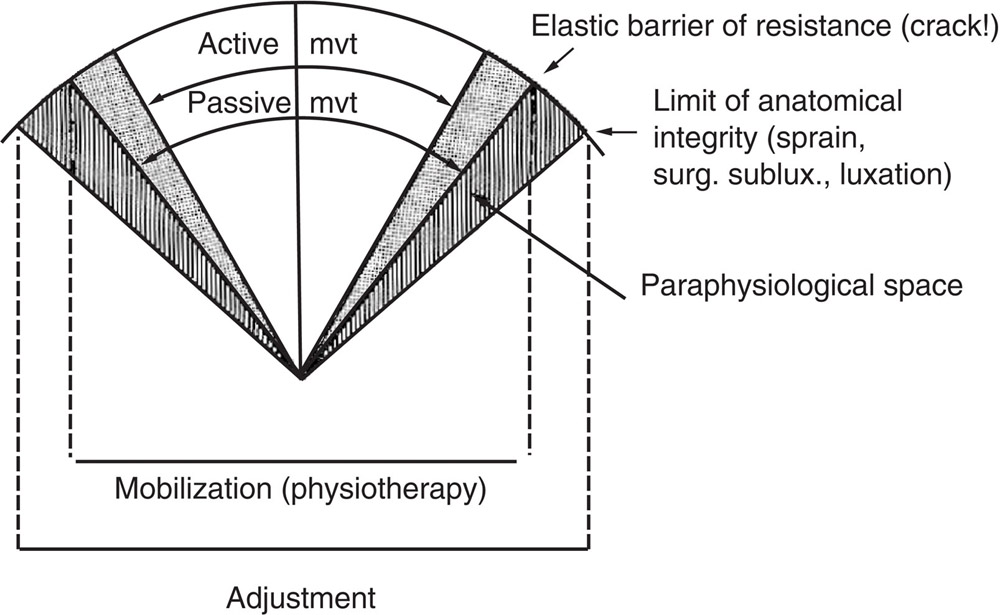
Figure 1
Sandoz modelIn 1976, Sandoz [1] published an important article entitled “Some physical mechanisms and effects of spinal adjustments.” In this article, Sandoz published a figure which was meant to describe the nature of joint manipulation with respect to where, in the total arc of the motion of a joint, manipulation was proposed to take place. Sandoz's figure is shown in Figure 1. The figure was particularly effective in identifying several phases of a joint's total motion, starting with the active range, defined as the range capable of being voluntarily produced by a person with their own motor power. Sandoz postulated that a further movement could be produced passively, either by the person themselves or by an external agent (ie, therapist), where ‘passive’ implied the imposition of externally applied force.
The outer margins of the figure represent the anatomic limit of motion of a joint, beyond which injury would occur to any of the holding elements and, with severe enough force, to the bony elements themselves. Active and passive motions are clearly shown to be less than, that is, within, the anatomic limit.
Sandoz postulated the presence of a “paraphysiological space,” beyond the passive range, but less than the anatomic limit. It was “into” this space that he postulated that a manipulation occurred. This “space” was described by others as a “zone of end-play,” [2] the “barrier,” [3] or “the capsular pattern.” [4] All of these terms are based on the notion that, at the end of “normal motion,” there exists a zone of elasticity in the joint which can be decreased in a joint which has lost some of its flexibility. The clinical term for this state has, as well, been given various names by all the schools of manipulation. Chiropractors have used the terms “subluxation” and “fixation” [5]: osteopaths use the term “somatic dysfunction”; medical and physiotherapeutic specialists use terms such as “dysfunction,” “barrier,” and “loss of end-play.” All of these terms contain the notion of “hypomobility.” We propose that the generic term for this problem is “joint dysfunction.”
This concept has been incorporated into the description of various palpatory procedures to assess joint motion. The palpatory experience which is proposed to match with normal joint motion is a feeling of smooth motion ending in a feeling of “play” or “spring” at the end of the passive range. Osteopaths used the term “ease” to describe this normal palpatory feel. An abnormal finding would be the feeling described in the term “blockage,” whereby the palpated motion is felt to stop before the expected end-range (perhaps as compared with the opposite side if it is healthy) and be accompanied by a “hard end-feel.” [4]
Before stating the problem alluded to in the introduction, it is timely to recognize that recent spinal biomechanics experts have introduced the term “neutral zone” to describe the zone within a joint's motion which produces little if no actual stress on the intrinsic tissues and within which minimal muscular activity is required for joint stabilization. [6] For example, Panjabi et al [6] determined that the neutral zone for C1-C2 rotation was approximately 28°, whereas the normal full active range is approximately 40°. The notion of an “elastic zone” has also been proposed [7] which is a zone in normal subjects which extends beyond the “neutral zone” and within which tissues undergo physiological levels of strain which increase but still remain less than sufficient to produce disruption or injury of tissues and within which higher levels of muscle recruitment occur for active stabilization. Klein et al [7] have described the situation of clinically restricted joint motion as “being stuck in the neutral zone.”
It is tempting to fit these 2 concepts into the model proposed by Sandoz. A rough equivalence might posit that the neutral zone lies within the “active” range, whereas the elastic zone might approximate the limit of the normal active zone.
The Problem

Figure 2 The problem we allude to can be appreciated from an inspection of Sandoz's original figure. In that figure, he placed manipulation as an “event” which took place at the upper limit of the passive range, presumably at the “barrier” or “paraphysiological space.” Figure 2 depicts this configuration with hypothetical percentage figures. Note that the anatomic limit of motion is considered to be 100%; therefore, the active range is considered to be approximately 80% of that maximum. Based upon our common clinical experience and the documented literature, [8, 9] we propose that the magnitude of the passive range is 10% to 15% of the active range. We also depict the “paraphysiological space” as no more than 1% to 2%, realizing that it has never been measured and is experienced by practitioners as no more than a “play” or “give” at the end of the passive range. Applying these percentages to Sandoz's model, we can see that manipulation is proposed to take place at upward of 90% to 95% of the total range of the joint in at least one of its operational ranges.
We state the problem as follows: manipulation is proposed to take place at the upper limit of the normal range of a joint, where the paraphysiological space approximates the limit of the anatomic range available to that joint in that particular plane of motion. This does not accord with the practical clinical circumstances in which manipulation is typically applied. Nor does it actually accord with the theory of hypomobility, as noted above. If hypomobility is the “joint state” associated with dysfunction, which, by definition, means it is the clinically important status of the joint, and if it is the purpose of manipulation to address dysfunction by improving mobility, then by definition, manipulation must be delivered to a joint with clinically significantly less-than-normal mobility, that is, not at the end of the normal range of motion.
Is this just a matter of words? Consider the definition of chiropractic in ‘Bill 46 - An act respecting the Regulation of the Profession of Chiropractic, in the Province of Ontario’ [10]: “moving the joints of the spine beyond a person's usual physiological range of motion using a fast low-amplitude thrust.”
Now consider the definition of manipulation which was recently used in a systematic review of spinal manipulation for headaches [1]: “low-amplitude, high-velocity thrusts in which vertebrae were carried beyond the normal physiological range of movement without exceeding the boundaries of anatomic integrity.” This quote was attributed to the team of Tuchin et al [12] who used it in their description of manipulation in their report on a clinical trial of spinal manipulation for migraine. Thus, we have a chiropractic group using this definition, which is then repeated verbatim by a nonchiropractic team who criticizes their work.
It would seem that the definition described above and attributed to the work of Sandoz has become firmly entrenched in the profession's consciousness. And yet, it is wrong!
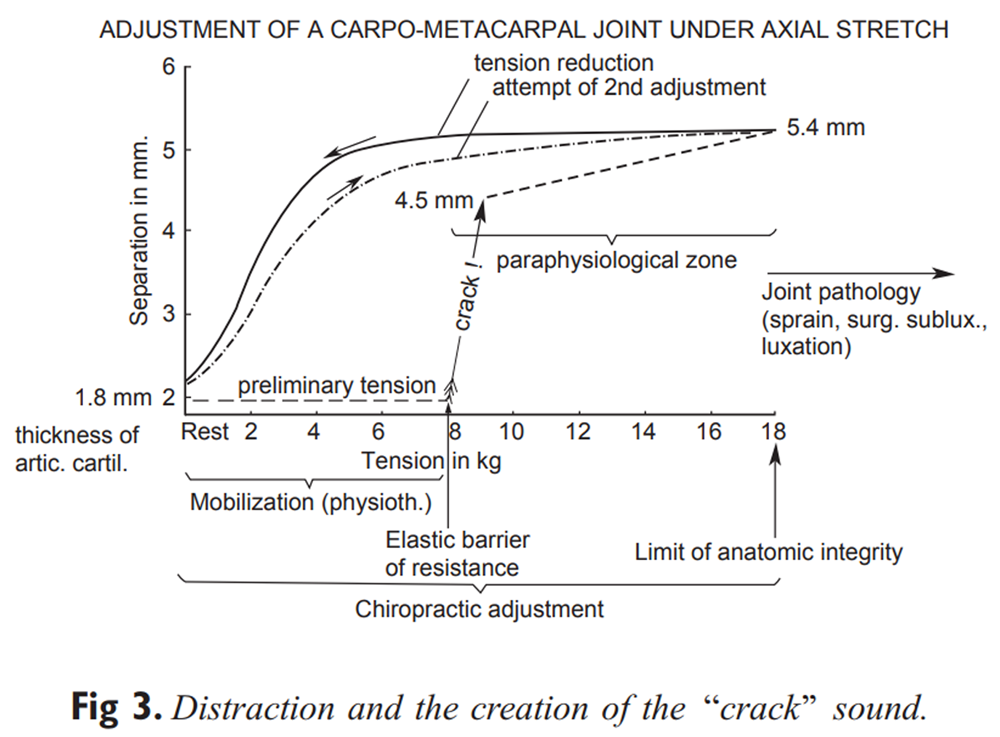
Figure 3 Another source of this problem could arise from a series of studies by Roston and Wheeler-Haines, [13] Unsworth et al, [14] and Miereau et al [15] which investigated joint cavitation in the metacarpal-phalangeal joint. The first 2 of these studies are mentioned by Sandoz, and the figure plotting the relationship between traction force on this joint versus distraction of the joint surfaces has become part of the theoretical “folklore” of the profession. The work of these authors shows where, in this plot of force versus distraction (Figure 3), a sudden increase of distraction is seen and is accompanied by a “crack.” Miereau et al even showed the vacuum phenomenon which occurred postcrack as evidence of the cavitation which was proposed to be responsible for the cracking sound.
These studies have been used to support the theoretical foundation of joint manipulation. The problem with these studies is that, although they do depict cavitation occurring at the extremes of normal joint motion, these joints were just that — normal. So the features of what appears to occur in a normal joint undergoing “manipulation” have osmosed to the circumstances of therapeutic manipulation to a clinically abnormal joint, without appreciation for the important differences between these 2 states.
Discussion
Figure 2 shows a hypothetical single normal spinal joint (ie, motion segment) in its plane of rotation. Regardless of the actual absolute amount of unilateral rotation at any specified joint (ie, at C1-C2 = 45°; at L5-S1 = 1°-2°), this range can be divided into the phases identified by Sandoz. As noted above, if the anatomic limit is defined as the point beyond which injury occurs, and if this is designated as 100%, then the active range is well below this limit and the passive range only approaches it. The upper end of the passive zone could probably be renamed the “nociceptive zone,” whereby forced movement into this zone would be painful, but not necessarily fully injurious. However, beyond the anatomic limit of motion, injury and pain would ensue. The “paraphysiological space” is represented in these figures as a 2% zone.
The critical point for our discussion is that Fig 2 represents the motion capacities of a normal joint. One now asks, is manipulation typically performed on such a joint? We would hope the answer is “no.” If the joint is normally mobile, why would one elect to perform a manipulation, when the purpose of that procedure is to impart force to the joint to increase its mobility? It should be noted here that the same argument could be made if, instead of motion, we selected the joint's alignment as the critical feature. If a joint is normally aligned, why perform manipulation?
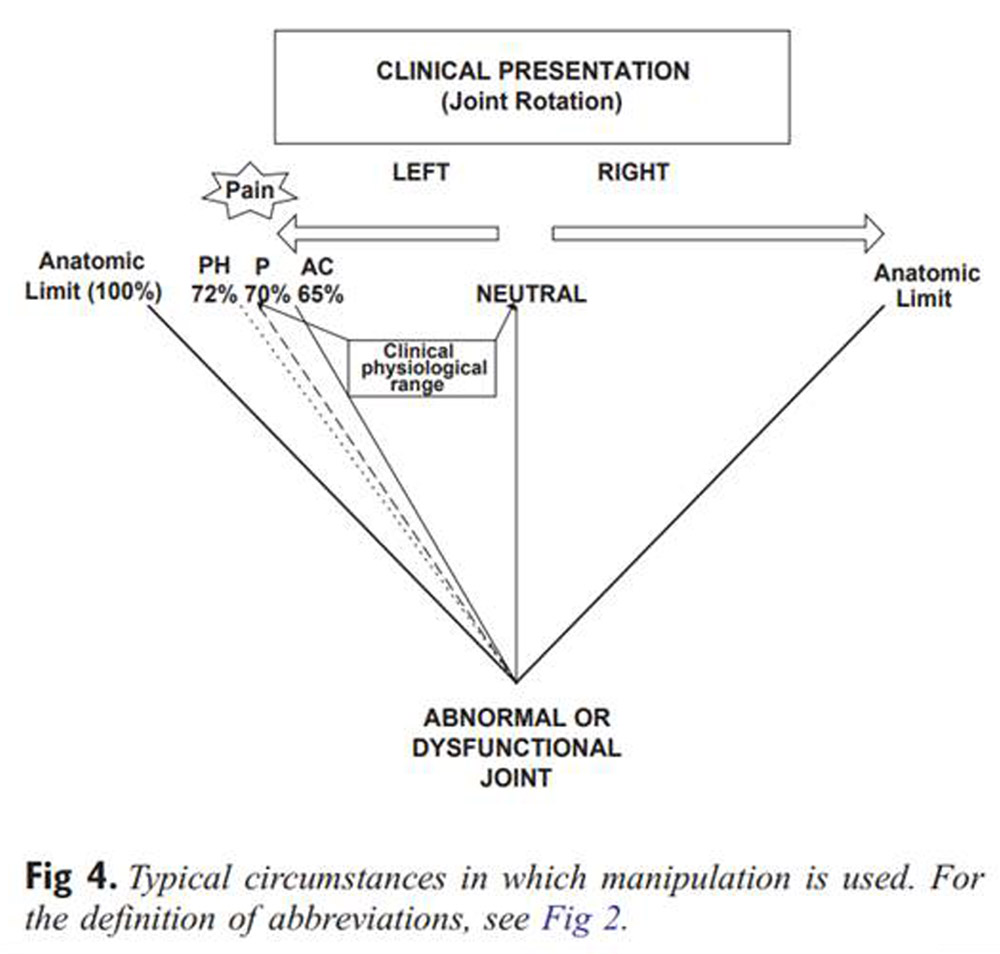
Figure 4

Figure 5
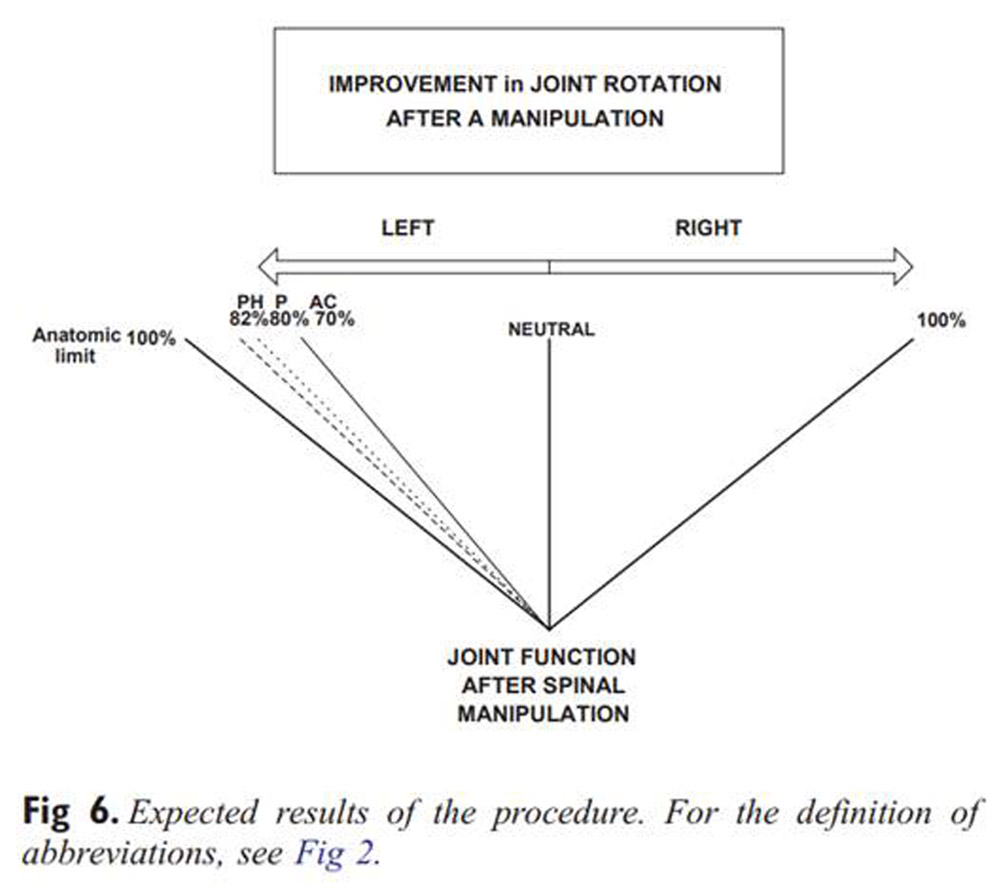
Figure 6 If the logic applied here is that manipulation is only performed on joints whose motion is not normal, by which we mean here that it is reduced (the problem of hypermobility or instability will be set aside for now), then Figure 4 depicts the typical circumstances in which manipulation is actually used. This figure is described as the “clinical situation,” not the normal situation. The range of motion available in the clinical situation is now called the “clinical physiological range.”
Figure 5 shows that manipulation is performed within the “clinical physiological” range. The figure attempts to show that the actual manipulation is not performed at the limit of the clinical physiological range, for that would provoke pain. Rather, it is performed at a point slightly before this range. The combination of subtle passive motions arranged by the chiropractor at that point creates what has been called the “closed pack” position. From this point on, we assume that a “paraphysiological” space is available within which the joint will cavitate and into which the impulse of the manipulative thrust is performed.
Figure 6 shows the expected result of this single procedure. The clinically restricted joint now has improved range of motion or less pain through more motion. This model has been confirmed by studies such as those by Cassidy et al, [16] Nansel et al, [17] and Whittingham and Nilsson [18] for range of motion increases after manipulation and by studies reviewed in Vernon [19] for decreases in pain after manipulation.
It should be noted here that this discussion has not addressed the potential mechanisms responsible for these changes. These may be mechanical or neurophysiological in nature or, as is likely, a combination of both of these.
As well, we recognize that this model presents an idealized version of joint motion in only one plane. We have not addressed the issue of the more complex, but realistic situation of joint dysfunction in several planes, whereby the actual “fixation” may be found in a 3-dimensional space which requires more careful and perhaps more subtle analysis by the practitioner.
Finally, we have completely ignored the issue of whether manual palpatory procedures can accurately and reliably identify the physical findings to which we allude in this discussion, particularly those hinted at in the paragraph above. These areas are fruitful directions for future thought and research.
Conclusion
We propose that what is described as the “Sandoz model” of joint dysfunction and manipulation requires revision. We have presented a revised model which presents the notion of a clinical physiological range of motion which more accurately defines the clinically important “joint state” or joint dysfunction, at least in one plane, and which also more accurately defines where in that state manipulation is applied. We hope this stimulates our readers and encourages their thoughtful critique.
Acknowledgments
The authors thank Tim Danson and Brian Foster for their encouragement in developing this commentary and Dr Jean Moss for her helpful comments.
References:
Sandoz, R.
Some physical mechanisms and effects of spinal adjustments.
Ann Swiss Chiropr Assoc. 1976; 6: 91–142Mennel, JM.
Joint pain.
Little Brown, Boston, MA; 1964Lewit, K.
Manipulative therapy in the rehabilitation of the locomotor system.
Butterworth's, London, England; 1991Cyriax, J.
Examination of the spinal column.
Physiotherapy. 1970; 56: 2–6Gillet, H and Liekens, M.
A further study of joint fixations.
Ann Swiss Chiropr Assoc. 1969; 4: 41–46Panjabi, M, Dvorak, J, Duranceau, J, Yamamoto, I, Greber, M, Rauschning, W et al.
Three-dimensional movements of the upper cervical spine.
Spine. 1988; 7: 726–730Klein, GN, Mannion, AF, Panjabi, MM, and Dvorak, J.
Trapped in the neutral zone: another symptom of whiplash-associated disorder?.
Eur Spine J. 2002; 11: 184–187Nilsson, N, Hartvigsen, J, and Christensen, HW.
Normal ranges of passive cervical motion in women and men 20-60 years old.
J Manipulative Physiol Ther. 1996; 19: 306–309Wong, A and Nansel, DD.
Comparisons of active vs passive end-range assessments in subjects exhibiting cervical range of motion asymmetries.
J Manipulative Physiol Ther. 1992; 15: 159–163Article 4, Subsection 2, Section 27,
Regulated Health Professions Act of Ontario; 1991.Astin, JA and Ernst, E.
The effectiveness of spinal manipulation for the treatment of headache disorders: a systematic review of randomized clinical trials.
Cephalalgia. 2002; 22: 617–623Tuchin PJ, Pollard H, Bonello R.
A Randomized Controlled Trial of Chiropractic Spinal Manipulative Therapy for Migraine
J Manipulative Physiol Ther 2000 (Feb); 23 (2): 91–95Roston, JB and Wheeler-Haines, R.
Cracking in the metacarpophalangeal joints.
J Anat. 1947; 81: 165–173Unsworth, A, Dawson, D, and Wright, V.
Cracking joints.
Ann Rheum Dis. 1971; 30: 348–358Miereau, D, Cassidy, JD, Bowen, V, Dupuis, P, and Noftall, F.
Manipulation and mobilization of the third metacarpophalangeal joint. A quantitative radiographic and range of motion study.
Man Med. 1988; 3: 135–140Cassidy, JD, Lopes, AA, and Yong-Hing, K.
The immediate effect of manipulation vs mobilization on pain and range of motion in the cervical spine: a randomized controlled trial.
J Manipulative Physiol Ther. 1992; 15: 570–575Nansel, DD, Peneff, A, and Quintoriano, J.
Effectiveness of upper vs lower cervical adjustments with respect to amelioration of passive rotational vs lateral-flexion end-range asymmetries in otherwise asymptomatic subjects.
J Manipulative Physiol Ther. 1992; 15: 99–105Whittingham, W and Nilsson, N.
Active range of motion of the cervical spine increases after spinal manipulation (toggle recoil).
J Manipulative Physiol Ther. 2001; 24: 552–555Vernon, H.
Qualitative Review of Studies of Manipulation-induced Hypoalgesia
J Manipulative Physiol Ther 2000 (Feb); 23 (2): 134–138
Return to ABOUT SPINAL ADJUSTING
Since 2-02-2005


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |