

Deconstructing the Placebo Effect
and Finding the Meaning ResponseThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Annals of Internal Medicine 2002 (Mar 19); 136 (6): 471–476 ~ FULL TEXT
Daniel E. Moerman, PhD, and Wayne B. Jonas, MD
Department of Anthropology,
University of Michigan-Dearborn,
6515 Cherry Hill Road,
Ypsilanti, MI 48198, USA.
dmoerman@umich.eduWe provide a new perspective with which to understand what for a half century has been known as the "placebo effect." We argue that, as currently used, the concept includes much that has nothing to do with placebos, confusing the most interesting and important aspects of the phenomenon. We propose a new way to understand those aspects of medical care, plus a broad range of additional human experiences, by focusing on the idea of "meaning," to which people, when they are sick, often respond. We review several of the many areas in medicine in which meaning affects illness or healing and introduce the idea of the "meaning response." We suggest that use of this formulation, rather than the fixation on inert placebos, will probably lead to far greater insight into how treatment works and perhaps to real improvements in human well-being.
From the FULL TEXT Article:
Introduction
[The cure for the headache] was a kind of leaf, which required to be accompanied by a charm, and if a person would repeat the charm at the same time that he used the cure, he would be made whole; but that without the charm the leaf would be of no avail.”
— Socrates, according to Plato [1]There is a renewed interest in placebos and the placebo effect — on their reality, their ethics, their place in medicine, or not, both in and out of the clinic and academy. The U.S. National Institutes of Health recently sponsored a large conference called “Science of the Placebo”. [2] At least five serious books on the subject [3-7] plus a book of poetry [8] and a novel [9] — each titled Placebo Effect — have been published since 1997. In the past 10 years, the National Library of Medicine has annually listed an average of 3972 scholarly papers with the keywords “placebo,” “placebos,” or “placebo effect,” with a low of 3362 papers in 1992 and a high of 4814 in 2000. During the fall of 2000, a discussion of the effect of new “drag free” suits, which might give an edge to Olympic swimmers, appeared in US News and World Report: “[S]wimming officials aren’t convinced this is anything more than the placebo effect. Swimmers excel because they think they’ve got an edge”. [10] One widely reported study, which concluded that placebos were powerless [11], or represented the Wizard of Oz [12], occasioned a blizzard of criticism [13-26] and some support. [27] It’s in the papers. [28, 29] It’s in the air.
Yet the most recent serious attempt to try logically to define the placebo effect failed utterly. [30] Given the ways people have gone about it, this seems unsurprising. Arthur K. Shapiro, MD, who spent much of his career as a psychiatrist studying the placebo effect, recently wrote:A placebo is a substance or procedure . . . that is objectively without specific activity for the condition being treated . . .
The placebo effect is the . . . therapeutic effect produced by a placebo. [31]If we replace the word “placebo” in the second sentence with its definition from the first, we get: “The placebo effect is the therapeutic effect produced by [things] objectively without specific activity for the condition being treated.” This makes no sense whatsoever. Indeed, it flies in the face of the obvious. The one thing of which we can be absolutely certain is that placebos do not cause placebo effects. Placebos are inert and don’t cause anything.
Moreover, people frequently expand the concept of the placebo effect very broadly to include just about every conceivable sort of beneficial biological, social, or human interaction that doesn’t involve some drug wellknown to the pharmacopoeia. A narrower form of this expansion includes identifying “natural history” or “regression to the mean” (as we might observe them in a randomized, controlled trial) as part of the placebo effect. But natural history and regression occur not only in the control group. Nothing in the theory of regression to the mean [31] hints that when people are selected for being extreme on some measure (blood pressure or cholesterol, for example), they are immune to regression if they receive active treatment. Such recipients are as likely (or unlikely) to move toward homeostasis as are control group patients. So, regression to the mean is in no meaningful way a “placebo effect.” Ernst and Resch [32] took an important step in trying to clarify this situation by differentiating the “true” from the “perceived” placebo effect. But “true placebo effect” hasn’t really caught on as a viable concept.
The concept of the placebo effect has been expanded much more broadly than this. Some attribute the effects of various alternative medical systems, such as homeopathy [33] or chiropractic [34], to the placebo effect. Others have described studies that show the positive effects of enhanced communication, such as Egbert’s [35], as “the placebo response without the placebo”. [7]
No wonder things are confusing.
MEANING AND MEDICINE
We suggest thinking about this issue in a new way.
A group of medical students was asked to participate in a study of two new drugs, one a tranquilizer and the other a stimulant (36). Each student was given a packet containing either one or two blue or red tablets; the tablets were inert. The students’ responses to a questionnaire indicated that1) the red tablets acted as stimulants while the blue ones acted as depressants and
2) two tablets had more effect than one. The students were not responding to the inertness of the tablets.Moreover, these responses cannot be easily accounted for by natural history, regression to the mean, or physician enthusiasm (presumably the experimenters were as enthusiastic about the reds as the blues). Instead, they can be explained by the “meanings” in the experiment:
1) Red means “up,” “hot,” “danger,” while blue means “down,” “cool,” “quiet” and
2) two means more than one. These effects of color [37-40] and number [41, 42] have been widely replicated.In a British study, 835 women who regularly used analgesics for headache were randomly assigned to one of four groups. [43] One group received aspirin labeled with a widely advertised brand name (“one of the most popular” analgesics in the United Kingdom that had been “widely available for many years and supported by extensive advertising”). The other groups received the same aspirin in a plain package, placebo marked with the same widely advertised brand name, or unmarked placebo. In this study, branded aspirin worked better than unbranded aspirin, which worked better than branded placebo, which worked better than unbranded placebo. Among 435 headaches reported by branded placebo users, 64% were reported as improved 1 hour after pill administration compared with only 45% of the 410 headaches reported as improved among the unbranded placebo users. Aspirin relieves headaches, but so does the knowledge that the pills you are taking are “good” ones.
In a study of the benefits of aerobic exercise, two groups participated in a 10-week exercise program. One group was told that the exercise would enhance their aerobic capacity, while the other group was told that the exercise would enhance aerobic capacity and psychological well-being. Both groups improved their aerobic capacity, but only the second group improved in psychological well-being (actually “self-esteem”). The researchers called this “strong evidence . . . that exercise may enhance psychological well-being via a strong placebo effect”. [44]
In the red versus blue pill study, we can correctly (if not very helpfully) classify the responses of the students as “placebo effects” because they did indeed receive inert tablets; it seems clear, however, that they responded not to the pills but to their colors. In the second study, the presence of the brand name enhanced the effect of both the inert and the active drug. It doesn’t seem reasonable to classify the “brand name effect” as a “placebo effect” because no placebos are necessarily involved. Meanwhile, calling the consequences of authoritative instruction to the exercisers a “placebo effect” could come only from someone who believes that words do not affect the world, someone who has never been told “I love you” or who has never read the reviews of a rejected grant proposal. It seems reasonable to label all these effects (except, of course, of the aspirin and the exercise) as “meaning responses,” a term that seeks, among other things, to recall Dr. Herbert Benson’s “relaxation response”. [45] Ironically, although placebos clearly cannot do anything themselves, their meaning can.
We define the meaning response as the physiologic or psychological effects of meaning in the origins or treatment of illness; meaning responses elicited after the use of inert or sham treatment can be called the “placebo effect” when they are desirable and the “nocebo effect” [46] when they are undesirable. This is obviously a complex notion with several terms that would be challenging to unpack (“desirable,” “effect,” “meaning,” “treatment,” “illness”) — an exercise that cannot be carried out here. Note that this definition excludes several elements that are usually included in our understanding of the placebo effect, such as natural history, regression, experimenter or subject bias, and error in measurement or reporting. Note as well that the definition is not phrased in terms of “nonspecific” effects; although many elements of the meaning response or placebo effect may seem nonspecific, they are often quite specific in principle after they are understood.
Meaning Permeates Medical Treatment
Insofar as medicine is meaningful, it can affect patients, and it can affect the outcome of treatment. [47-49] Most elements of medicine are meaningful, even if practitioners do not intend them to be so. The physician’s costume (the white coat with stethoscope hanging out of the pocket) [50], manner (enthusiastic or not), style (therapeutic or experimental), and language [51] are all meaningful and can be shown to affect the outcome; indeed, we argue that both diagnosis [52] and prognosis [53] can be important forms of treatment.
Many studies can be cited to document aspects of the therapeutic quality of the practitioner’s manner. [54] In one, a strong message of the effect of a drug (an inert capsule) substantially reduced the patients’ report of the pain of mandibular block injection compared with the pain after a weak message. Patients who received the weak message reported less pain than a group that received no placebos and no message at all. [55] In another study, 200 patients with symptoms but no abnormal physical signs were randomly assigned to a positive or a negative consultation. In a survey of patients 2 weeks later, 64% of patients in the positive consultation group said they were all better, while only 39% of those who had negative consultations thought they were better. [56]
Although there is strong evidence for such “physician effects,” little evidence shows that “patient effects” are very important. A mass of research in the 1970s designed to identify “placebo reactors” produced only inconsistent and contradictory findings. [57-59]
Meaning Can Have Substantial Physiologic Action
Placebo analgesia can elicit the production of endogenous opiates. Analgesia elicited with an injection of saline solution can be reversed with the opiate antagonist naloxone and enhanced with the opiate agonist proglumide. [60] Likewise, acupuncture analgesia can be reversed with naloxone in animals [61] and people. [62] To say that a treatment such as acupuncture “isn’t better than placebo” does not mean that it does nothing.
Meaning and Surgery
The classic example of the meaningful effects of surgery comes from two studies of ligation of the bilateral internal mammary arteries as a treatment for angina. [63, 64] Patients receiving sham surgery did as well — with 80% of patients substantially improving — as those receiving the active procedure in the trials or in general practice. Although the studies were small, the procedure was no longer performed after these reports were published. Of note, these effectiveness rates (and those reported by the proponents of the procedure at the time) are much the same as those achieved by contemporary treatments such as coronary artery bypass or β-blockers.
Some observers have suggested that the success of transmyocardial laser revascularization, a procedure without a clear mechanism, may be explained by what they call the placebo effect [65] but what we call the meaning response. This is a plausible interpretation of a recent trial showing dramatic improvement in very sick people in both participant groups of a control trial of transmyocardial laser revascularization (Leon MB, Baim DS, Moses JW, Laham RJ, Knopf W. A randomized blinded clinical trial comparing percutaneous laser myocardial revascularization [using Biosense LV Mapping] vs. placebo in patients with refractory coronary ischemia. Presented at American Heart Association Scientific Session, 12–15 November 2000).
Surgery is particularly meaningful: Surgeons are among the elite of medical practitioners; the shedding of blood is inevitably meaningful in and of itself. In addition, surgical procedures usually have compelling rational explanations, which drug treatments often do not. The logic of arthroscopic surgery (“we will clean up a messy joint”) is much more sensible and understandable (and even effective [66]), especially for people in a culture rich in machines and tools, than is the logic of nonsteroidal anti-inflammatory drugs (which “inhibit the production of prostaglandins which are involved in the inflammatory process,” something no one would ever tell a patient). Surgery clearly induces a profound meaning response in modern medical practice. [67-69]
MEANING, CULTURE, AND MEDICINE
Anthropologists understand cultures as complex webs of meaning, rich skeins of connected understandings, metaphors, and signs. Insofar as1) meaning has biological consequence and
2) meanings vary across cultures, we can anticipate that biology will differ in different places, not because of genetics but because of these entangled ideas;we can anticipate what Margaret Lock has called “local biologies” [70, 71]; Lock has shown dramatic cross-cultural variation in the existence and experience of “menopause”. [70, 71] Moreover, Phillips has shown that “Chinese Americans, but not whites, die significantly earlier than normal (1.3 to 4.9 y) if they have a combination of disease and birth year which Chinese astrology and medicine consider ill fated”. [72]
Among Chinese Americans whose deaths were attributed to lymphatic cancer (n = 3041), those who were born in “Earth years” — and consequently were deemed by Chinese medical theory to be especially susceptible to diseases involving lumps, nodules, or tumors — had an average age at death of 59.7 years. In contrast, among those born in other years, age at death of Chinese Americans with lymphatic cancer was 63.6 years — nearly 4 years longer. Similar differences were also found for various other serious diseases. No such differences were evident in a large series of “whites” who died of similar causes in the same period.
The intensity of the effect was shown to be correlated with “the strength of commitment to traditional Chinese culture.” These differences in longevity (up to 6% or 7% difference in length of life!) are not due to having Chinese genes but to having Chinese ideas, to knowing the world in Chinese ways. The effects of meaning on health and disease are not restricted to placebos or brand names but permeate life.
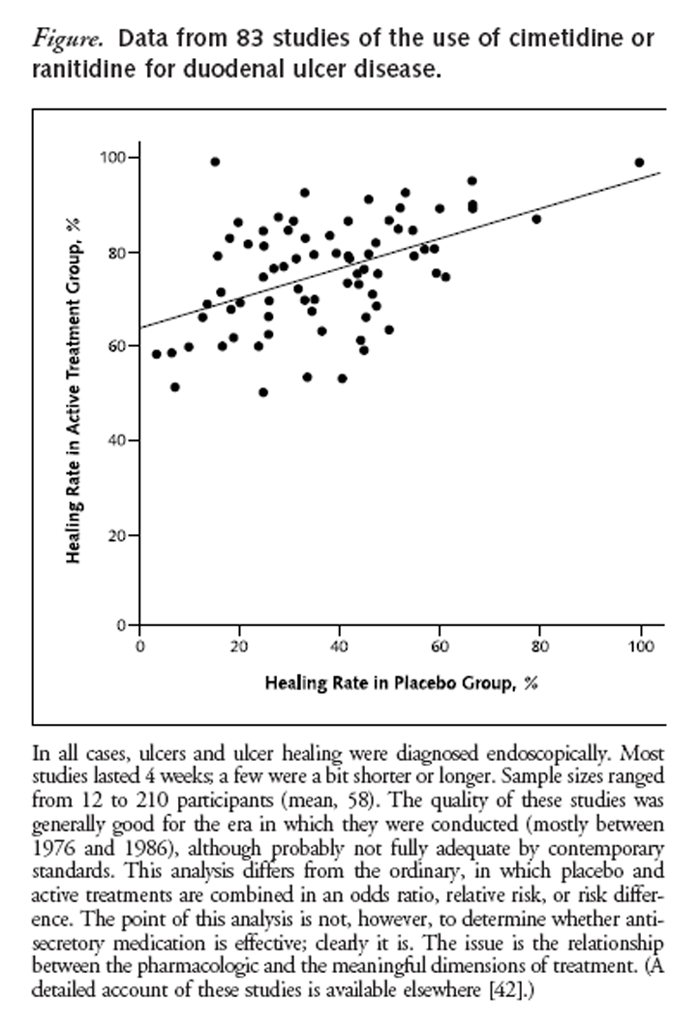
Figure One of us has shown variation in the response of control groups to inert medication in diverse cultures for the same conditions (ulcers, hypertension, and anxiety). [42] The Figure shows the relationship between control group and active treatment group healing for endoscopically diagnosed duodenal ulcer treated with antisecretory medication. Control group healing and active treatment group healing seem functionally related in these studies.
The correlation between control and active healing rates is 0.49; as the placebo group’s healing rate increases, so does the rate of the active treatment group. Although the average control group healing rate in five German studies has been 62.4%, the healing rate was 16.7% in three studies from neighboring Denmark and the Netherlands. The number needed to treat for benefit (NNTB), to obtain ulcer healing, can be calculated; for ulcer patients treated with placebo, the NNTB for those who are German (not Danish or Dutch) is 2.
CONCLUSIONS
Practitioners can benefit clinically by conceptualizing this issue in terms of the meaning response rather than the placebo effect. Placebos are inert. You can’t do anything about them. For human beings, meaning is everything that placebos are not, richly alive and powerful. However, we know little of this power, although all clinicians have experienced it. One reason we are so ignorant is that, by focusing on placebos, we constantly have to address the moral and ethical issues of prescribing inert treatments [73, 74], of lying [75], and the like. It seems possible to evade the entire issue by simply avoiding placebos. One cannot, however, avoid meaning while engaging human beings. Even the most distant objects—the planet Venus, the stars in the constellation Orion—are meaningful to us, as well as to others. [76]
Yet, a huge puzzle remains: Obviously the meaning response is of great value to the sick and the lame. For example, eliciting the meaning response requires remarkably little effort (“You will be fine, Mr. Smith”). So why doesn’t this happen all the time? And why can’t you do it to yourself? Psychologist Nicholas Humphrey has suggested that this conundrum may have evolutionary roots: Healing has its benefits but also its costs. [77] (For example, relieving pain may encourage premature activity, which could exacerbate the injury. Moreover, immune activity is metabolically very demanding on an injured system.) Perhaps only when a friend, relative, or healer indicates some level of social support (for example, by performing a ritual) is the individual’s internal economy able to act. Moreover, as we have clarified, routinized, and rationalized our medicine, thereby relying on the salicylates and forgetting about the more meaningful birches, willows, and wintergreen from which they came — in essence, stripping away Plato’s “charms” — we have impoverished the meaning of our medicine to a degree that it simply doesn’t work as well as it might any more. Interesting ideas such as this are impossible to entertain when we discuss placebos; they spring readily to mind when we talk about meaning.
Grant Support:
In part by a grant from the National Science Foundation to Dr. Moerman (NSF SBR-9421128).
References:
Jowett B.
Dialogues of Plato.
Chicago: Univ Chicago Pr; 1952.
“The Science of the Placebo: Toward an Interdisciplinary Research Agenda.”National Institutes of Health,
Bethesda, Maryland, 19–20 November 2000.
Available at placebo.nih.gov. Accessed on 25 January 2002.Harrington A, ed.
The Placebo Effect: An Interdisciplinary Exploration.
Cambridge, MA: Harvard Univ Pr; 1997.Shapiro AK, Shapiro E.
The Powerful Placebo: From Ancient Priest to Modern Physician.
Baltimore: Johns Hopkins Univ Pr; 1997.Spiro HM.
The Power of Hope: a Doctor’s Perspective.
New Haven: Yale Univ Pr; 1998.Kirsch I, ed.
How Expectancies Shape Experience.
Washington, DC:
American Psychological Association; 1999.Brody H, Brody D.
The Placebo Response: How You Can Release the Body’s Inner Pharmacy for Better Health.
New York: Cliff Street Books; 2000.Beaumont JM.
Placebo Effects: Poems.
New York: W.W. Norton; 1997.Russell G.
Placebo Effect.
New York: BBC Worldwide Americas; 1998.Clark K, Milliken R.
Today, it’s “May the best swimsuit win.”
US News and World Report. 21 August 2000:55.Hrobjartsson A, Gotzsche PC.
Is the placebo powerless? An analysis of clinical trials comparing placebo with no treatment [Review].
N Engl J Med. 2001;344:1594-602. [PMID: 11372012]Bailar JC 3rd.
The powerful placebo and the Wizard of Oz.
N Engl J Med. 2001;344:1630-2. [[PMID: 11372017]Beldoch M.
Is the placebo powerless?
N Engl J Med. 2001;345:1278; discussion 1278-9. [PMID: 11680460]DiNubile MJ.
Is the placebo powerless?
N Engl J Med. 2001;345:1278; discussion 1278-9. [PMID: 11680459]MISSING FROM ARTICLE
Kupers R.
Is the placebo powerless?
N Engl J Med. 2001;345:1278; discussion 1278-9. [PMID: 11680457]Einarson TE, Hemels M, Stolk P.
Is the placebo powerless?
N Engl J Med. 2001;345:1277; discussion 1278-9. [PMID: 11680456]Kaptchuk TJ.
Is the placebo powerless?
N Engl J Med. 2001;345:1277; discussion 1278-9. [PMID: 11680455]Miller FG.
Is the placebo powerless?
N Engl J Med. 2001;345:1277; discussion 1278-9. [PMID: 11680454]Lilford RJ, Braunholtz DA.
Is the placebo powerless?
N Engl J Med. 2001; 345:1277-8; discussion 1278-9. [PMID: 11680453]Spiegel D, Kraemer H, Carlson RW.
Is the placebo powerless?
N Engl J Med. 2001;345:1276; discussion 1278-9. [PMID: 11680452]Ader R.
Much ado about nothing.
Advances in Mind-Body Medicine. 2001; 17:293-95.Brody H, Weismantel D.
A challenge to core beliefs.
Advances in Mind-Body Medicine 2001;17:296-8.Greene PJ, Wayne PM, Kerr CE, Weiger WA, Jacobson E, Goldman P, et al.
The powerful placebo: doubting the doubters.
Advances in Mind-Body Medicine. 2001;17:298-307.Kirsch I, Scorboria A.
Apples, oranges, and placebos: heterogeneity in a meta-analysis of placebo effects.
Advances in Mind-Body Medicine 2001;17:307-9.Wickramasekera I.
The placebo efficacy study: problems with the definition of the placebo and the mechanisms of placebo efficacy.
Advances in Mind-Body Medicine. 2001;17:309-12.McDonald CJ.
Is the placebo powerless?
N Engl J Med. 2001;345:1276-7; discussion 1278-9. [PMID: 11680451]Talbot M.
The placebo prescription.
New York Times Magazine. 9 January 2001: 34-9, 44, 58-60.Rubin R.
‘Eat one. You’ll feel better.’
USA Today. 16 January 2001:D1.Gøtzsche PC.
Is there logic in the placebo?
Lancet. 1994;344:925-6. [PMID: 7934350]McDonald CJ, Mazzuca SA, McCabe GP Jr.
How much of the placebo ‘effect’ is really statistical regression?
Stat Med. 1983;2:417-27. [PMID: 6369471]Ernst E, Resch KL.
Concept of true and perceived placebo effects.
BMJ. 1995;311:551-3. [PMID: 7663213]Ernst E, Pittler MH.
Efficacy of homeopathic arnica: a systematic review of placebo-controlled clinical trials.
Arch Surg. 1998;133:1187-90. [PMID: 9820349]Curtis P.
Spinal manipulation: does it work?
Occup Med. 1988;3:31-44. [PMID: 2963390]Egbert LD, Battit GE, Welch CE, Bartlett MK.
Reduction of postoperative pain by encouragement and instruction of patients. A study of doctor-patient rapport.
N Engl J Med. 1964;270:825-7.Blackwell B, Bloomfield SS, Buncher CR.
Demonstration to medical students of placebo responses and non-drug factors.
Lancet. 1972;1:1279-82. [PMID: 4113531]Schapira K, McClelland HA, Griffiths NR, Newell DJ.
Study on the effects of tablet colour in the treatment of anxiety states.
Br Med J. 1970;1:446-9. [PMID: 5420207]Honzak R, Horackova E, Culik A.
Our experience with the effect of placebo in some functional and psychosomatic disorders.
Activa Nervosa Superior (Prague). 1971;13:190-1.Cattaneo AD, Lucchilli PE, Filippucci G.
Sedative effects of placebo treatment.
Eur J Clin Pharmacol. 1970;3:43-5.de Craen AJ, Roos PJ, Leonard de Vries A, Kleijnen J.
Effect of colour of drugs: systematic review of perceived effect of drugs and of their effectiveness.
BMJ. 1996;313:1624-6. [PMID: 8991013]de Craen AJ, Moerman DE, Heisterkamp SH, Tytgat GN, Tijssen JG, Kleijnen J.
Placebo effect in the treatment of duodenal ulcer.
Br J Clin Pharmacol. 1999;48:853-60. [PMID: 10594490]Moerman DE.
Cultural variations in the placebo effect: ulcers, anxiety, and blood pressure.
Med Anthropol Q. 2000;14:51-72. [PMID: 10812563]Branthwaite A, Cooper P.
Analgesic effects of branding in treatment of headaches.
Br Med J (Clin Res Ed). 1981;282:1576-8. [PMID: 6786566]Desharnais R, Jobin J, Coˆte´ C, Le´vesque L, Godin G.
Aerobic exercise and the placebo effect: a controlled study.
Psychosom Med. 1993;55:149-54. [PMID: 8475229]Benson H, Klipper MZ.
The Relaxation Response.
New York: Wings Books; 1992.Hahn RA.
The nocebo phenomenon: concept, evidence, and implications for public health.
Prev Med. 1997;26:607-11. [PMID: 9327466]Levi-Strauss C.
The Effectiveness of Symbols. Structural Anthropology.
Garden City, NY: Anchor Books; 1967.Moerman DE.
Anthropology of symbolic healing.
Current Anthropology. 1979;20:59-80.Kirmayer LJ.
Healing and the invention of metaphor: the effectiveness of symbols revisited.
Cult Med Psychiatry. 1993;17:161-95. [PMID: 7693395]Blumhagen DW.
The doctor’s white coat. The image of the physician in modern America.
Ann Intern Med. 1979;91:111-6. [PMID: 88917]Uhlenhuth EH, Rickels K, Fisher S, Park LC, Lipman RS, Mock J.
Drug, doctor’s verbal attitude and clinic setting in the symptomatic response to pharmacotherapy.
Psychopharmacologia. 1966;9:392-418. [PMID: 4872909]Brody H, Waters DB.
Diagnosis is treatment.
J Fam Pract. 1980;10:445-9. [PMID: 7354290]Christakis NA.
Death Foretold: Prophecy and Prognosis in Medical Care.
Chicago: Univ Chicago Pr; 1999.Gracely RH.
Charisma and the art of healing: can nonspecific factors be enough?
In: Devor M, Rowbotham MC, Wiesenfeld-Hallin Z, eds.
Proceedings of the 9th World Congress on Pain.
Seattle: IASP Pr; 2000:1045-67.Gryll SL, Katahn M.
Situational factors contributing to the placebos effect.
Psychopharmacology (Berl). 1978;57:253-61. [PMID: 97705]Thomas KB.
General practice consultations: is there any point in being positive?
Br Med J (Clin Res Ed). 1987;294:1200-2. [PMID: 3109581]Moerman DE.
Edible symbols: the effectiveness of placebos.
Ann N Y Acad Sci. 1981;364:256-68.Fisher S.
The placebo reactor: thesis, antithesis, synthesis, and hypothesis.
Dis Nerv Syst. 1967;28:510-5. [PMID: 6048413]Liberman RP.
The elusive placebo reactor.
In: Brill H, ed. Neuro-Psycho-Pharmacology:
Proceedings of the Fifth International Congress of the Collegium
Internationale Neuro-Psycho-Pharmacologicum.
Amsterdam: Excerpta Medica Foundation. 1967:557-66.Benedetti F, Amanzio M.
The neurobiology of placebo analgesia: from endogenous opioids to cholecystokinin.
Prog Neurobiol. 1997;52:109-25. [PMID: 9185235]Pomeranz B, Chiu D.
Naloxone blockade of acupuncture analgesia: endorphin implicated.
Life Sci. 1976;19:1757-62. [PMID: 187888]Mayer DJ, Price DD, Rafii A.
Antagonism of acupuncture analgesia in man by the narcotic antagonist naloxone.
Brain Res. 1977;121:368-72. [PMID: 832169]Cobb L, Thomas GI, Dillard DH, Merendino KA, Bruce RA.
An evaluation of internal-mammary artery ligation by a double blind technic.
N Engl J Med. 1959;260:1115-8.Dimond EG, Kittle CF, Crockett JE.
Comparison of internal mammary ligation and sham operation for angina pectoris.
Am J Cardiol. 1960;5:483-6.Lange RA, Hillis LD.
Transmyocardial laser revascularization [Editorial].
N Engl J Med. 1999;341:1075-6. [PMID: 10502599]Moseley JB Jr, Wray NP, Kuykendall D, Willis K, Landon G.
Arthroscopic treatment of osteoarthritis of the knee: a prospective, randomized, placebo-controlled trial.
Results of a pilot study.
Am J Sports Med. 1996;24:28-34. [PMID: 8638750]Beecher HK.
Surgery as placebo. A quantitative study of bias.
JAMA. 1961; 176:1102-7.Johnson AG.
Surgery as a placebo.
Lancet. 1994;344:1140-2. [PMID: 7934500]Kaptchuk TJ, Goldman P, Stone DA, Stason WB.
Do medical devices have enhanced placebo effects?
J Clin Epidemiol. 2000;53:786-92. [PMID: 10942860]Lock MM.
Encounters with Aging: Mythologies of Menopause in Japan and North America.
Berkeley: Univ California Pr; 1993.Lock M.
Menopause: lessons from anthropology.
Psychosom Med. 1998;60: 410-9. [PMID: 9710286]Phillips DP, Ruth TE, Wagner LM.
Psychology and survival.
Lancet. 1993; 342:1142-5. [PMID: 7901476]Macklin R.
The ethical problems with sham surgery in clinical research.
N Engl J Med. 1999;341:992-6. [PMID: 10498498]Reynolds T.
The ethics of placebo-controlled trials.
Ann Intern Med. 2000; 133:491. [PMID: 10975985]Evans M.
Justified deception? The single blind placebo in drug research.
J Med Ethics. 2000;26:188-93. [PMID: 10860211]McCleary TP.
The Stars We Know. Crow Indian Astronomy and Lifeways.
Prospect Heights, IL: Waveland Pr; 1997.Humphrey N.
Great expectations: The evolutionary psychology of faithhealing and the placebo response.
In: Humphrey N, ed. The Mind Made Flesh: Essays from the Frontiers of Evolution and Psychology.
Oxford: Oxford Univ Pr; 2002: Chapter 19.
Return to PLACEBOS
Since 3-01-2020


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |